Abstract
The determinants of vaccine hesitancy remain complex and context specific. Betrayal aversion occurs when an individual is hesitant to risk being betrayed in an environment involving trust. In this pre-registered vignette experiment, we show that betrayal aversion is not captured by current vaccine hesitancy measures despite representing a significant source of unwillingness to be vaccinated. Our survey instrument was administered to 888 United States residents via Amazon Mechanical Turk in March 2021. We find that over a third of participants have betrayal averse preferences, resulting in an 8–26% decline in vaccine acceptance, depending on the betrayal source. Interestingly, attributing betrayal risk to scientists or government results in the greatest declines in vaccine acceptance. We explore an exogenous message intervention and show that an otherwise effective message acts narrowly and fails to reduce betrayal aversion. Our results demonstrate the importance of betrayal aversion as a preference construct in the decision to vaccinate.
Supplementary Information
The online version contains supplementary material available at 10.1007/s10439-022-02975-4.
Keywords: Health behavior, Persuasive messages, COVID-19
Introduction
While vaccinations are important in protecting public health, many individuals are vaccine hesitant, delaying or refusing available vaccines. The 3C model18,20 measures the prevalence of three factors of vaccine hesitancy: confidence (trust in safety and effectiveness), convenience (physical and psychological constraints), and complacency (perceived risks of disease are low). Recent work suggests that individual differences in information processing and social preferences also influence hesitancy.4 Nonetheless, the determinants of vaccine hesitancy remain complex and context specific.20
Betrayal aversion is a decision-making preference that occurs when people avoid situations involving trust in order to avoid disutility associated with the negative emotions experienced when being betrayed.1,2,5,14 A bad trust outcome carries with it both lost utility relative to the desired outcome and disutility from being betrayed, with betrayal aversion capturing aversion to negative emotional disutility related to the latter. Importantly, betrayal aversion is distinct from a preference for avoiding outcome risk in trust environments. When choosing between safety products like vaccines, betrayal averse individuals may accept lower levels of protection from the primary risk in order to avoid a relatively small secondary risk of being harmed by the safety product itself. People were significantly more likely to choose to purchase airbags and smoke alarms, and marginally more likely to choose vaccines, when the potential risks of the products involved no betrayal.14 Levels of betrayal aversion also decline in contexts that dampen emotional responses.11
Current measures of vaccine hesitancy capture overall beliefs about the safety of vaccines without disassociating the source of the assumed risks,17,25,26 hence, are unable to determine whether betrayal aversion represents an additional, currently unmeasured, source of hesitancy. In this work, we seek to establish the importance of betrayal aversion as a preference construct in the decision to vaccinate. We developed a pre-registered vignette experiment involving a highly infectious hypothetical disease to measure willingness to become vaccinated across different betrayal scenarios while holding the overall risk level constant. We hypothesized that willingness to become vaccinated is lower when there is an additional risk of betrayal (death due to side effects) compared to a non-betrayal risk. We found evidence confirming this hypothesis.
During pandemics, information about the disease and available vaccines develops rapidly. The nature of communication and spread of information can have significant influences on vaccine hesitancy.6,19,21–23,27,28 Learning that President Obama had his daughters vaccinated, for example, was positively associated with willingness to get vaccinated against H1N1 influenza.27 Recent studies on COVID-19 vaccination approval reported a positive impact of messaging stressing the importance of herd immunity30 as well as endorsements by the director of the National Institute of Allergy and Infectious Diseases.6 On the other hand, misinformation around COVID-19 caused a decline in vaccination intent.19 In this study, we investigate whether a message that primes regret for not getting the vaccine increases willingness to vaccinate and, separately, whether it decreases betrayal aversion. Willingness to become vaccinated was greater among responders exposed to our messaging intervention. Contrary to our pre-registered hypothesis, the prevalence of betrayal aversion did not decline after message exposure. To identify the channels by which the messaging treatment operates on vaccination intent, we administered another pre-registered survey to another group of responders that reported the motives for getting the vaccine, and found exposure to the message treatment increased the intent to protect others.
The COVID-19 pandemic has served as an illustration that many potential factors connect betrayal aversion and vaccine hesitancy. To explore some of these factors, in addition to our two pre-registered studies, we designed an exploratory study (not pre-registered) to investigate betrayal aversion and vaccine hesitancy when the risk of betrayal is brought about by (1) a chance of the vaccine weakening the immune system, (2) a partisan government approving the vaccine rapidly, overlooking certain safety measures, or (3) scientists approving the vaccine rapidly, overlooking certain safety measures. Betrayal aversion was higher when a partisan government or scientists actively contribute to the associated risk. However, betrayal sensitivity was dampened when the political party of the government developing the vaccine was aligned with an individual’s own preferences. This result demonstrates that political polarization can yield and/or amplify differences in vaccination intent.6,13,15,31
Materials and Methods
We administered an online survey via Amazon Mechanical Turk (MTurk). The final sample includes 595 participants for our pre-registered hypotheses (https://osf.io/4peuy) (from registered studies 1 and 2) and 293 additional participants to test our exploratory hypotheses (study 3) (see Electronic Supplementary Material: Appendix A for MTurk exclusion criteria and Appendix B for sample characteristics in Table A1). All of our procedures were approved by Virginia Tech Institutional Review Board and all participants provided informed consent.
Participants received $2 compensation for the task, which took an average of 19 min to complete. After answering questions about our hypothetical disease scenario (described below and in Tables 1, 2, 3 and 4), participants reported their real-world experiences with vaccines,7 including those related to COVID-19. In particular, the first group of surveys asked about participants’ general attitudes toward vaccination (5 questions) and toward COVID-19 (3 questions). Other study measures included a survey of demographic characteristics and two widely used vaccine hesitancy surveys adopted from 1) the Parental Attitudes About Childhood Vaccines questionnaire25,26 (the 5-question PACV-short version24,26) and the Vaccine Confidence Index questionnaire (the 4-question VCI core survey,16,17 see Online Appendix A for indices’ scoring). These comprehensive measures allow us to establish the robustness of the findings reported in Section 5 using multiple linear regression and controlling for individual characteristics (gender, age, ethnicity, race, education, work status, political orientation), extent of vaccine hesitancy (PACV or VCI), and the responder’s geographic region. Note that data was collected in the United States during the COVID-19 pandemic between March 30th, 2021 and April 8th, 2021. In the United States, by March 30th, the cumulative number of reported COVID-19 cases surpassed 29 million and the number of the associated deaths was 543,003.8 By this time more than 130 million COVID-19 vaccines had been administered.7 The vignette conditions (summarized in Tables 1, 2, 3 and 4) and subsequent questionnaire are available in Online Appendix C.
Table 1.
Caption: summary of vignette treatments.
| Study 1 | Study 2 | Study 3 | |||||
|---|---|---|---|---|---|---|---|
| Treatment | Side-effectsa | Risk-only | Risk-only w/Message | Side-effects w/Messagea | Vaccine is counter-productivea | Governmenta | Scientistsa |
| Participants | 198 | 103 | 97 | 197 | 97 | 102 | 94 |
Table 2.
Caption: study 1 treatments: non-betrayal vs side-effects betrayal.
| “a 1% chance that people treated with the vaccine will contract the virus and die as a result.” and “an additional one chance in 10,000 (0.01%) that someone who is treated with the vaccine will die due to [source of risk below] | ||
|---|---|---|
| Treatment | Source of risk | Participants |
| Non-betrayal (control) | … problems unrelated to the vaccine.” | 198 |
| Betrayal: side-effects | …vaccine-induced complications (side effects).” | |
Table 3.
Caption: Study 2 treatment conditions: no message vs message in risk-only treatment and in betrayal side-effects treatment.
|
Message (prime feelings of regret): “There is no chance you will regret getting the vaccine, but, if you don’t get it then you may either get sick and might die or may get other people sick meaning that they might die, and you could regret it. Imagine how you would feel if you passed the virus to someone else. Just try to imagine how that would feel. Now tell us that you should not do a lot to prevent that terrible feeling of regret that you didn’t get the vaccination earlier.” | ||
|---|---|---|
| Treatment | Source of risk | Participants |
| Study 2A | ||
| Risk-Only | “a 1.01% chance that people treated with the vaccine will contract the virus and die as a result.” | 103 |
| Risk-Only w/ Message | 97 | |
| Study 2B | ||
| Side-effectsb | “a 1% chance that people treated with the vaccine will contract the virus and die as a result.” and “an additional one chance in 10,000 (0.01%) that someone who is treated with the vaccine will die due to vaccine-induced complications (side effects).” | 198a |
| Side-effectsb w/Message | 197 | |
aSame participants as Study 1
bDenotes treatments involving betrayal. Participants assigned to a betrayal treatment completed both the betrayal condition (source of risk as outlined in the table) and a non-betrayal scenario (control) condition (source of risk: “…problems unrelated to the vaccine”, see Table 2)
Table 4.
Caption: Study 3 treatment conditions: side-effects betrayal vs alternative betrayal sources (counter-productivity, government, scientists).
| “a 1% chance that people treated with the vaccine will contract the virus and die as a result.” and “an additional one chance in 10,000 (0.01%) that someone who is treated with the vaccine will die due to [source of risk below] | ||
|---|---|---|
| Treatment | Source of risk | Participants |
| Study 3A | ||
| Counter-productivityb | …the vaccine lowering the recipient’s immunity making them more prone to catching the virus.” | 97 |
| Side-effectsb | …vaccine-induced complications (side effects).” | 198a |
| Study 3B | ||
| Governmentb | …a [XYZ] government in charge that approved the vaccine too rapidly, overlooking certain safety concerns.” |
102 (“XYZ” read “Democrat” or “Republican”, order counterbalanced) |
| Side-effectsb | …vaccine-induced complications (side effects).” | 198a |
| Study 3C | ||
| Scientistsb | …scientists who work for [XYZ] developing the vaccine too rapidly, overlooking certain safety concerns.” |
94 (“XYZ” read “the government” or “pharmaceutical companies”, order counterbalanced) |
| Side-effectsb | …vaccine-induced complications (side effects).” | 198a |
aSame participants as Study 1
bDenotes treatments involving betrayal. Participants assigned to a betrayal treatment completed both the betrayal condition (source of risk as outlined in the table) and a non-betrayal scenario (control) condition (source of risk: “…problems unrelated to the vaccine”, see Table 2)
Study 1: Betrayal Aversion Related Vaccine Hesitancy
In the vignette experiment, participants read a hypothetical scenario about a novel future disease described as both highly infectious and deadly, with an available free and easy-to-take vaccine. To investigate betrayal aversion, we modify Koehler and Gershoff’s safety product task (which did not explore general vaccine hesitancy and found marginal results on vaccine betrayal) to create a within-subject design with greater power to detect betrayal aversion to vaccines.11,14 Participants were told that the unvaccinated face a 2% risk of death. Those who are vaccinated face a 1.01% risk of death, where 1% was due to the virus, while the explanation for the remaining 0.01% varies across treatments. By measuring changes in willingness to become vaccinated across treatments while holding the probability of death constant, we explore how the causes of betrayal aversion affect its severity.
In our benchmark (control) Non-Betrayal treatment, the 0.01% chance of death faced by those who get the vaccine was described as “problems unrelated to the vaccine” (Table 2). The cause of the 0.01% chance of death in our Side-Effects treatments involved active betrayal, and was described as “vaccine-induced complications (side effects).” We asked participants (N = 395) to indicate their willingness to become vaccinated (single 7-point Likert question with response alternatives ranging from “Definitely reject” at 1 to “Definitely accept” at 7) under both scenarios, with the order of scenarios presented counterbalanced across participants. By subtracting an individual’s willingness to become vaccinated in the Side-Effects treatments from their willingness in the Non-Betrayal treatment, we get an individual level measurement of betrayal aversion. Note that we designed the Non-Betrayal scenario to represent general risk by highlighting clearly its unrelatedness to the vaccine in question, intentionally not providing contextualized details that could have confounded our measure and lengthened the instructions (such as getting into a car accident on the way to the vaccination clinic, etc).
Study 2: Messaging, Vaccine Hesitancy and Betrayal Aversion
Our second study explores the influence of messaging on willingness to become vaccinated with and without the possibility of betrayal using Dan’s Ariely’s message suggestion, which primes feelings of regret for not getting the vaccine.10 Here is the exact wording of the message:
There is no chance you will regret getting the vaccine, but, if you don’t get it then you may either get sick and might die or may get other people sick meaning that they might die, and you could regret it. Imagine how you would feel if you passed the virus to someone else. Just try to imagine how that would feel. Now tell us that you should not do a lot to prevent that terrible feeling of regret that you didn’t get the vaccination earlier.
The Risk-Only treatment (N = 103) involves the same probabilities as above, 1.01% with and 2% chance of death without the vaccine, but no chance of betrayal. In the Risk-Only w/Message treatment (N = 97), we presented the message prior to participants making decisions in the Risk-Only treatment (Table 3, study 3A). By comparing the responses to five vaccine uptake questions in both treatments,19 the causal role of the regret message on vaccine hesitancy is identified while also investigating the motives behind vaccination intent and hesitancy. Participants reported their benchmark willingness to become vaccinated, their willingness to become vaccinated in order to protect oneself, and separately, their willingness to become vaccinated to protect others (family, friends, and at-risk groups). Responders also indicated their willingness to wait and see how the vaccine is working before getting vaccinated and their willingness to become vaccinated only if it was required by their work or school (7-point Likert questions). Moreover, to identify the effect of the message on betrayal aversion, the Side-Effects w/Message treatment (N = 197) involves presenting the message prior to participants making decisions in both the Non-Betrayal and Side-Effects treatment frameworks (Table 3, study 3B).
Study 3: Source of Betrayal and Vaccine Hesitancy
The last study focuses on our exploratory treatments, where we manipulated the source of betrayal (Table 4, studies 4A–4C). In all of the three conditions with varied sources of betrayal, participants also made decisions in a Non-Betrayal condition as well (order counter-balanced across subjects). In the Counter-Productivity treatment (N = 97), we elicited willingness to become vaccinated in an active betrayal condition where the 0.01% risk was caused by the vaccine lowering the recipient’s general immunity making them more prone to catching the virus. Concerns about the vaccine overloading the immune system has been one of the most stated reasons behind vaccine hesitancy.29 In the Government treatment (N = 102), we elicited willingness to become vaccinated when the 0.01% risk of active betrayal is caused by having either a Democrat or a Republican government overseeing an accelerated vaccine approval process that overlooks potential safety concerns. Note that in this condition, participants were presented with three different conditions (order counter-balanced, see Online Appendix A): Non-Betrayal, Democrat Government, and Republican Government. The Scientists treatment (N = 94) investigates betrayal aversion when the active betrayal is attributed to the behavior of scientists (working for pharmaceutical companies or for the government) (see Online Appendix A for additional details).
Results
Study 1 Results: Betrayal Aversion Related Vaccine Hesitancy
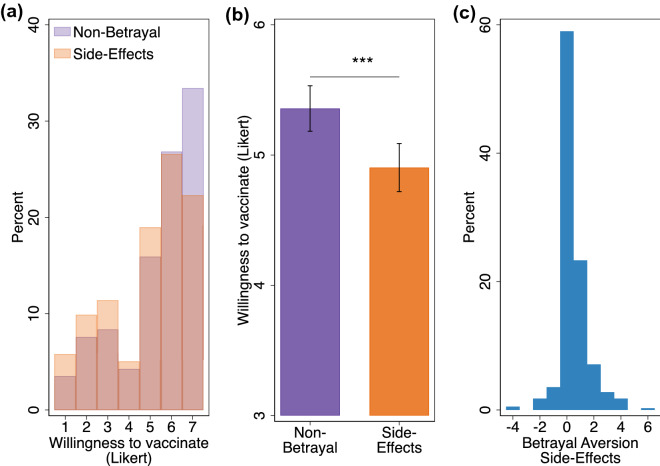
We first compare willingness to become vaccinated when the 0.01% additional risk was due to vaccine-induced complications (Side-Effects treatments) instead of unrelated problems (Non-Betrayal treatment). Participants reported a significantly lower willingness to vaccinate when the risk associated with vaccination was due to side effects (= 0.453; Wilcoxon signed-rank test, p < 0.001) (Figs. 1a and 1b). Next, we compute a binary measure of vaccine hesitancy by collapsing the Likert responses for each treatment into two categories: vaccine hesitant (score < 5) or vaccine non-hesitant (score 5). When the additional risk was caused by side-effects, 8.4% more people were identified as vaccine hesitant (McNemar test, p < 0.001).
Figure 1.
Willingness to vaccinate and betrayal aversion. (a) Distribution of willingness to vaccinate responses across Non-Betrayal and Side-Effects treatments (see Table 2). (b) Average willingness to vaccinate across betrayal treatments. (c) Betrayal aversion distribution (Difference in willingness to vaccinate across treatments). =395 (Side-Effects + Side-Effects w/Message). Error bars denote 95% confidence intervals. Two-sided paired t-tests: ***p < 0.01, **p < 0.05, *p < 0.1, N.S. not significant.
To derive an individual-level measure of betrayal aversion, we calculated the difference between willingness to become vaccinated in the Non-Betrayal and Side-Effects treatments. As shown in Fig. 1c, the distribution of betrayal aversion is skewed to the right with more than 30% of responders classified as betrayal averse (positive level of betrayal aversion). Taken together these results support our pre-registered hypothesis and indicate that betrayal aversion is likely influencing the willingness of individuals to vaccinate. This result is consistent with previous studies,1,2,5,14 demonstrating a substantial portion of the population is betrayal averse.
Study 2 Results: Messaging, Vaccine Hesitancy and Betrayal Aversion
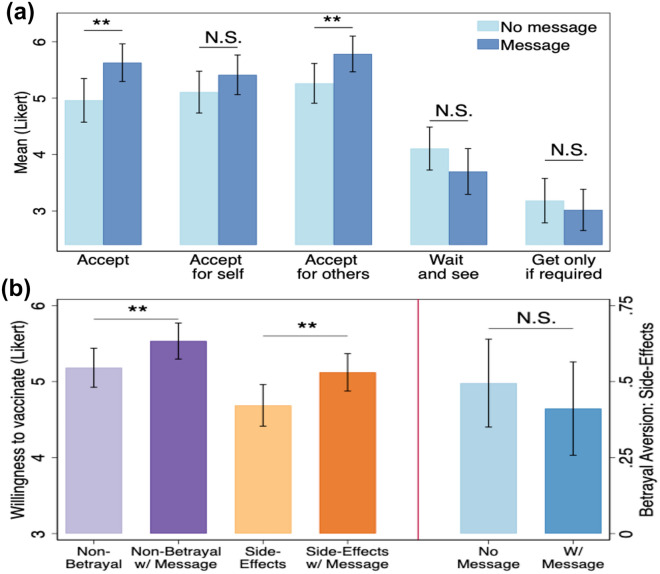
Similar to other studies that explored vaccine hesitancy and communication,19,21–23,27 participants exposed to our message treatment in the Risk Only w/Message condition reported higher willingness to become vaccinated relative to the group that did not receive the message ( = 0.668; Two-sample Wilcoxon rank-sum test, p = 0.009) (Fig. 2a). The channel through which the message appears to work is social—our regret messaging increased willingness to become vaccinated to protect others ( = 0.522; Two-sample Wilcoxon rank-sum test, p = 0.022; Fig. 2a) rather than protecting oneself. After collapsing the Likert responses into a binary measure of vaccine hesitancy as before, exposure to the message reduced vaccine hesitancy by about 11.7% (One-sided Fisher’s exact test, p = 0.032). Confirming the social channel of the message, the likelihood of accepting the vaccine to protect others was 14.8% higher among participants exposed to the message compared to the control group (One-sided Fisher’s exact test, p = 0.008).
Figure 2.
Message exposure, willingness to vaccinate, and betrayal aversion. (a) Willingness to get the vaccine, and associated motives with undivided probabilities across message and no message treatments (see Table 3; = 103; NRisk-Only w/message = 97). (b) Willingness to get the vaccine with divided probabilities across message treatments (see Table 3; = 198; NSide-Effects w/message = 197) and the corresponding average betrayal aversion across message treatments. Error bars denote 95% confidence intervals. Two-sided t tests: ***p < 0.01, **p < 0.05, *p < 0.1, N.S. non-significant.
With evidence that messaging is effective at reducing overall vaccine hesitancy, we now explore whether the message also decrease betrayal aversion. This is measured by contrasting decisions in the Side-Effects treatment (N = 198) to that from the Side-Effects w/Message treatment (N = 197) that involves displaying the treatment message prior to presenting participants with the Non-Betrayal and Side-Effects treatment frameworks. As shown in Fig. 2b (right panel), betrayal aversion, on average, was not statistically significantly lower for participants exposed to the message treatment ( = 0.084; Two-sample Wilcoxon rank-sum test; ). Failure of the message to decrease betrayal aversion could arise either from similar changes of vaccine hesitancy in both treatments or from a lack of change of vaccine hesitancy in both the Non-Betrayal and Side-Effects treatments due to the message. Fig. 2b (left panel) shows that relative to the no message comparison treatment groups, participants exposed to the message treatment reported higher willingness to vaccinate under both Non-Betrayal ( = 0.351; Two-sample Wilcoxon rank-sum test, p = 0.028) and Side-Effects condition ( = 0.435; Two-sample Wilcoxon rank-sum test, p = 0.034). These results suggest that while regret messaging is effective at reducing vaccine hesitancy, it is acting orthogonally to betrayal aversion related vaccine hesitancy. Consequently, this result seems to be consistent with the evidence from the Risk-Only and Risk-Only w/Message treatments that suggested the messages were acting to increase willingness to become vaccinated to protect others. In particular, the effect of the message operates through an external/other focused channel while betrayal aversion would be expected to be an emotional/internal focused channel.11
Our results exploring messaging’s effects on vaccine hesitancy using the Risk-Only and Risk-Only w/Message treatments are robust to exploring the data with a multiple linear regression analysis with vaccine acceptance as the dependent variable while controlling for individual characteristics (see “Materials and Methods” section and Online Appendix A), measures of vaccine hesitancy and geographic region in fixed effects linear regression models (Effect on benchmark acceptance: > 0.660, p < 0.050; Effect on acceptance to protect others: > 0.278, p < 0.050; Online Appendix B Tables A2 and A3). For these regression analyses, and subsequent tables in the Online Appendix B, we standardize all 7-Likert scale measures at the responder level, prior to calculating betrayal aversion, and use the z-scores in model estimation. Importantly, when betrayal aversion is modelled instead, the null effect of the message treatment on betrayal aversion persisted ( when controlling for PACV; when controlling for VCI; (Online Appendix B Table A4). Note that the coefficients for the commonly used vaccine hesitancy measures (PACV and VCI) are not significantly associated with betrayal aversion () and seem to move in the opposite direction. We obtain an identical result when we include each of the four measures in the VCI separately in the regression17 (available upon request). Moreover, the finding that the message increased willingness to become vaccinated in both treatments (Non-Betrayal and Side-Effects) holds in our regression analysis (>0.250, p < 0.050; Online Appendix B Table A5). Even though the null result of the effect of the message on betrayal aversion related vaccine hesitancy is in conflict with our pre-registered hypothesis that vaccine hesitancy reducing messages would mitigate betrayal aversion, our findings suggest that the current measures of vaccine hesitancy, and potentially messaging interventions, seem to fall short in accounting for an important preference construct that influences the vaccination decision.
Study 3 Results: Source of Betrayal and Vaccine Hesitancy
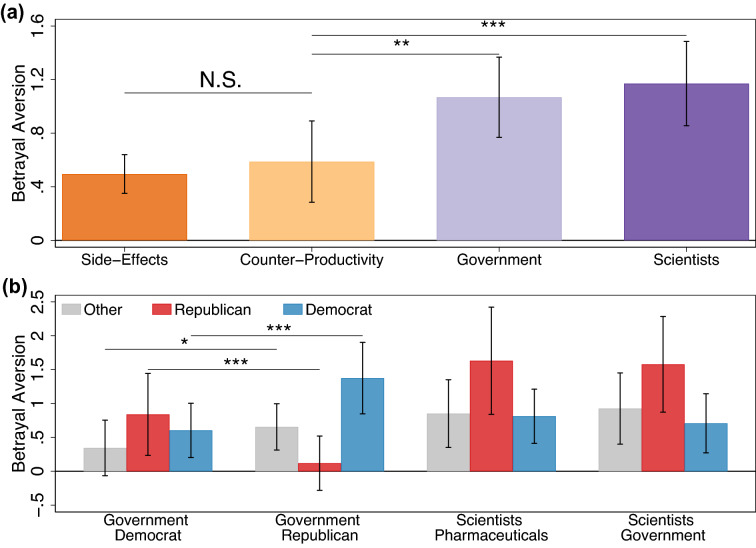
We compared whether the level of betrayal aversion differs when active betrayal comes from side effects (Side-Effects treatment) or when due to the vaccine causing an individual to suffer weakened immunity that makes them more prone to catching the virus (Counter-Productivity treatment). There was no discernable difference in betrayal aversion between these two types of active betrayals ( = 0.093; Two-sample Wilcoxon rank-sum test, ; Fig. 3a).
Figure 3.
Betrayal aversion across betrayal sources. (a) Betrayal aversion across betrayal source conditions (see Table 4; = 395; = 97; = 102; = 94). For Government (Scientists), the lowest willingness to get the vaccine between Democrat or Republican governments (Pharmaceutical or Government scientists) is used to calculate betrayal aversion. Betrayal aversion was greater in both the Government and Scientists conditions in comparison to the Side-Effects condition (p < 0.010; asterisks omitted for clarity). (b) Betrayal aversion by participants’ political orientation for the two betrayal treatments: Government ( = 29; = 25; = 48) and Scientists ( = 27; = 19; = 48). Error bars denote 95% confidence intervals. Two-sided t tests (paired tests in (b) only): ***p < 0.01, **p < 0.05, *p < 0.1, N.S. non-significant.
On the other hand, betrayal aversion was higher in conditions involving either politicians or scientists actively contributing to the betrayal risk. For the Government (Scientists) treatment, the lowest willingness to become vaccinated between Democrat or Republican government (Pharmaceutical or Government scientists) was used to derive betrayal aversion. Relative to the active betrayal treatment (Counter-Productivity), betrayal aversion to vaccination was significantly higher when betrayal was channeled through the government ( = 0.481; Two-sample Wilcoxon rank-sum test, ) or scientists ( = 0.583; Two-sample Wilcoxon rank-sum test, ; Fig. 3a). We confirm that betrayal aversion is greater in the government or scientists treatments relative to the Side-Effects treatment from study 1 instead (Government = 0.574; Scientists = 0.675; Two-sample Wilcoxon rank-sum tests, and respectively). In addition, we confirm these results using regression analysis that controls for individual characteristics, measures of vaccine hesitancy and region fixed effects (, ; Online Appendix B Table A6).
When the additional risk of betrayal was caused by Counter-Productivity, vaccine acceptance was reduced by about 12.4% (McNemar test, p = 0.008). This decline is again comparable to the 8.4% decline in vaccine acceptance reported in Study 1 for betrayal caused by Side-Effects. On the other hand, vaccine acceptance was reduced more steeply by 20.6% and 25.6% when the additional risk of betrayal was caused by the government or the scientists (McNemar tests, p < 0.001), respectively.
Participants reported lower willingness to vaccinate when the betrayal source was a Republican led government compared to a Democrat led government ( = 0.275; Wilcoxon signed-rank test, . Interestingly, betrayal aversion to a vaccine developed by a Democrat or Republican led government is modulated by political orientation. Here, responders who self-identified as Democrats were more betrayal averse to a vaccine from a Republican led government compared to a Democrat led government ( = 0.771; Wilcoxon signed-rank test, ) (Fig. 3b). Analogously, Republicans were more sensitive to betrayal when the vaccine risk was brought about by a Democrat led government instead of a Republican led government ( = 0.720; Wilcoxon signed-rank test, ). Willingness to become vaccinated for self-identified Republicans in the Non-Betrayal scenario was not significantly different from that in the scenario involving the Republican government as a proxy cause of betrayal ( = ; Wilcoxon signed-rank test, ). On the other hand, betrayal aversion persisted for self-identified Democrats who reported higher willingness to become vaccinated in the Non-Betrayal scenario relative to that involving the Democrat government as a proxy cause of betrayal ( = 0.604; Wilcoxon signed-rank test, ). Responders who self-identified as neither Republicans nor Democrats were marginally more betrayal averse when the source of betrayal involved a Republican led government instead of a Democrat led government ( = 0.310; Wilcoxon signed-rank test: ).
Willingness to vaccinate did not differ significantly when the betrayal source involved either pharmaceutical company scientists or government employed scientists ( = 0.043; Wilcoxon signed-rank test, . Moreover, betrayal aversion to vaccines developed rapidly by pharmaceutical company or government employed scientists were not differentiated by political affiliation ( < 0.105; Wilcoxon signed-rank tests, ). Interestingly, however, we find that Republican responders, relative to Democrat responders, were significantly more betrayal averse to vaccines from government employed scientists ( = 0.871; Two-sample Wilcoxon rank-sum test, ) and marginally more averse to betrayal from vaccines developed by pharmaceutical company employed scientists ( = 0.819; Two-sample Wilcoxon rank-sum test, ).
Discussion
Betrayal aversion is an important preference that influences decision-making in situations where trust can be broken. Despite their potential to reduce the overall risk of harm, safety products with small chances of causing the very same harm they are expected to prevent are often less preferred.1,11,14 In this study, we demonstrate that betrayal aversion is an important preference construct in the decision to vaccinate and is one not accounted for by widely used vaccine hesitancy measures.
In addition, the observed level of betrayal aversion depended on the source of betrayal. In comparison to the levels observed when the source of betrayal was a vaccine side effect, betrayal aversion was amplified when the government or scientists may be at fault. Since our design held the objective probability of harm constant (0.01%) across all betrayal scenarios, this finding may be due to stronger emotional responses when potential betrayals involve institutions or personnel that were expected to prevent harm. In the case of vaccine development, while risks such as side effects are inevitable with any vaccine, pressure to develop and approve a vaccine quickly during an epidemic or pandemic could magnify the perceived risk of betrayal due to concerns that sufficient testing was not conducted, or that safety concerns were overlooked. Thus, the active involvement of the government or scientists in breaking the trust may have compounded betrayal aversion to the safety product itself. Interestingly, Democrats (Republicans) were more sensitive to betrayal by a Republican (Democrat) government. Thus, betrayal aversion seems to further amplify political polarization in vaccination decisions.3,6,13,15,31
We explore a messaging intervention that increased overall willingness to vaccinate but did not ameliorate betrayal aversion. The messaging intervention primes feelings of regret for not getting the vaccine via phrases like “Imagine how you would feel if you passed the virus to someone else.” The message operated through other regarding preferences, such as altruism, enhancing receivers’ willingness to vaccinate to protect friends, family members, and at-risk groups. Since the message was not targeted at reducing concerns about betrayal, we were not surprised that it failed to decrease hesitancy through that channel. In fact, in a sense the message’s ineffectiveness in reducing betrayal aversion underscores the importance of treating betrayal aversion as a unique preference construct so that it is not overlooked in health communications and behavioral interventions.
Vignette experiments are a valuable first step in a multi-method research agenda where many observations are needed and circumstances preclude other data collection strategies (e.g., ethical issues are present).9 At the same time, we acknowledge that research using survey methods may have reduced external validity when compared with some other approaches because participants do not experience the scenario and decisions are not consequential. Nevertheless, an external validity check revealed a positive and significant correlation between willingness to get COVID-19 vaccination and willingness to become vaccinated in the vignette experiment ( Online Appendix B Table A7).
The results of this study motivate future research on vaccine betrayal aversion. First, betrayal aversion might be added to measures of vaccine hesitancy to augment their accuracy. Next, research on interventions to increase vaccination rates should address the betrayal aversion channel of vaccine hesitancy, which we show is less malleable to some messaging. Emotion regulation interventions,12 however, may be a potential candidate to mitigate betrayal aversion to vaccination. Finally, we believe that, with additional research and perhaps including a field or randomized controlled study, results from this study may shed light on how to reduce COVID-19-related vaccine hesitancy.
Supplementary Information
Below is the link to the electronic supplementary material.
Author Contributions
All authors contributed to conception and design of the study. AA and ED authors collected the data and organized the database. AA performed the statistical analysis and wrote the first draft of the manuscript. All authors wrote sections of the manuscript, contributed to manuscript revision, and read and approved the submitted version.
Funding
Funding provided by the National Science Foundation (Grant #1541105).
Data and Code Availability
Data reported in this study and code generating the results will be made available via the Open Science Framework upon publication: https://osf.io/4peuy.
Conflict of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Contributions that do not Justify Authorship
Not applicable.
Informed Consent
This study was approved by the Institutional Review Board at Virginia Tech in the United States and participants provided informed consent.
Technical Help
Not applicable.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Aimone J, Ball S, King-Casas B. The betrayal aversion elicitation task: an individual level betrayal aversion measure. PLoS ONE. 2015;10:e0137491. doi: 10.1371/journal.pone.0137491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aimone JA, Houser D. What you don’t know won’t hurt you: a laboratory analysis of betrayal aversion. Exp. Econ. 2012;15:571–588. doi: 10.1007/s10683-012-9314-z. [DOI] [Google Scholar]
- 3.Betsch C, Korn L, Böhm R. Reply to Weisel: from polarization to vaccination and back. Proc. Natl. Acad. Sci. 2021;118:e2102717118. doi: 10.1073/pnas.2102717118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Betsch C, Schmid P, Heinemeier D, Korn L, Holtmann C, Böhm R. Beyond confidence: development of a measure assessing the 5C psychological antecedents of vaccination. PLoS ONE. 2018;13:e0208601. doi: 10.1371/journal.pone.0208601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bohnet I, Greig F, Herrmann B, Zeckhauser R. Betrayal aversion: evidence from Brazil, China, Oman, Switzerland, Turkey, and the United States. Am. Econ. Rev. 2008;98:294–310. doi: 10.1257/aer.98.1.294. [DOI] [Google Scholar]
- 6.Bokemper SE, Huber GA, Gerber AS, James EK, Omer SB. Timing of COVID-19 vaccine approval and endorsement by public figures. Vaccine. 2021;39:825–829. doi: 10.1016/j.vaccine.2020.12.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.COVID Data Tracker Weekly Review for March 26, 2021. Centers for Disease Control and Prevention: https://www.cdc.gov/coronavirus/2019-ncov/covid-data/covidview/past-reports/03262021.html, 2021.
- 8.COVID-19 Weekly Epidemiological Update, March 30 2021. World Health Organization: https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---31-march-2021, 2021.
- 9.Erfanian F, Latifnejad Roudsari R, Heydari A, Noghani Dokht Bahmani M. A narrative on the use of vignette: its advantages and drawbacks. J. Midwifery Reprod. Health. 2020;8:2134–2145. [Google Scholar]
- 10.Ferreri, E. To Convince Vaccine Skeptics, Use Empathy, Information and a Re-Start, Experts Say. https://today.duke.edu/2020/12/convince-vaccine-skeptics-use-empathy-information-and-re-start-experts-say, 2020
- 11.Gershoff AD, Koehler JJ. Safety first? The role of emotion in safety product betrayal aversion. J. Consumer Res. 2011;38:140–150. doi: 10.1086/658883. [DOI] [Google Scholar]
- 12.Gross JJ. Emotion regulation: current status and future prospects. Psychol. Inquiry. 2015;26:1–26. doi: 10.1080/1047840X.2014.940781. [DOI] [Google Scholar]
- 13.Hamel, L., A. Kirzinger, C. Muñana, and M. Brodie. KFF COVID-19 Vaccine Monitor: December 2020. https://www.kff.org/coronavirus-covid-19/report/kff-covid-19-vaccine-monitor-december-2020/, 2020.
- 14.Koehler JJ, Gershoff AD. Betrayal aversion: when agents of protection become agents of harm. Organ. Behav. Hum. Decis. Process. 2003;90:244–261. doi: 10.1016/S0749-5978(02)00518-6. [DOI] [Google Scholar]
- 15.Kreps S, Prasad S, Brownstein JS, Hswen Y, Garibaldi BT, Zhang B, Kriner DL. Factors associated with US adults’ likelihood of accepting COVID-19 vaccination. JAMA Netw. Open. 2020;3:e2025594–e2025594. doi: 10.1001/jamanetworkopen.2020.25594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Larson, H., A. de Figueiredo, E. Karafillakis, and M. Rawal. State of vaccine confidence in the EU 2018. Luxembourg: Publications Office of the European Union 10:241099, 2018.
- 17.Larson HJ, De Figueiredo A, Xiahong Z, Schulz WS, Verger P, Johnston IG, Cook AR, Jones NS. The state of vaccine confidence 2016: global insights through a 67-country survey. EBioMedicine. 2016;12:295–301. doi: 10.1016/j.ebiom.2016.08.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Larson HJ, Jarrett C, Eckersberger E, Smith DM, Paterson P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007–2012. Vaccine. 2014;32:2150–2159. doi: 10.1016/j.vaccine.2014.01.081. [DOI] [PubMed] [Google Scholar]
- 19.Loomba S, de Figueiredo A, Piatek SJ, de Graaf K, Larson HJ. Measuring the impact of COVID-19 vaccine misinformation on vaccination intent in the UK and USA. Nat. Hum. Behav. 2021;5:337–348. doi: 10.1038/s41562-021-01056-1. [DOI] [PubMed] [Google Scholar]
- 20.MacDonald NE. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33:4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 21.Milkman KL, et al. A megastudy of text-based nudges encouraging patients to get vaccinated at an upcoming doctor’s appointment. Proc. Natl. Acad. Sci. USA. 2021;118:e2101165118. doi: 10.1073/pnas.2101165118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nyhan B, Reifler J, Richey S, Freed GL. Effective messages in vaccine promotion: a randomized trial. Pediatrics. 2014;133:e835–e842. doi: 10.1542/peds.2013-2365. [DOI] [PubMed] [Google Scholar]
- 23.Odone A, Ferrari A, Spagnoli F, Visciarelli S, Shefer A, Pasquarella C, Signorelli C. Effectiveness of interventions that apply new media to improve vaccine uptake and vaccine coverage: a systematic review. Hum. Vacc. Immunother. 2015;11:72–82. doi: 10.4161/hv.34313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Oladejo O, Allen K, Amin A, Frew PM, Bednarczyk RA, Omer SB. Comparative analysis of the Parent Attitudes about Childhood Vaccines (PACV) short scale and the five categories of vaccine acceptance identified by Gust et al. Vaccine. 2016;34:4964–4968. doi: 10.1016/j.vaccine.2016.08.046. [DOI] [PubMed] [Google Scholar]
- 25.Opel DJ, Taylor JA, Mangione-Smith R, Solomon C, Zhao C, Catz S, Martin D. Validity and reliability of a survey to identify vaccine-hesitant parents. Vaccine. 2011;29:6598–6605. doi: 10.1016/j.vaccine.2011.06.115. [DOI] [PubMed] [Google Scholar]
- 26.Opel DJ, Taylor JA, Zhou C, Catz S, Myaing M, Mangione-Smith R. The relationship between parent attitudes about childhood vaccines survey scores and future child immunization status: a validation study. JAMA Pediatrics. 2013;167:1065–1071. doi: 10.1001/jamapediatrics.2013.2483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Quinn SC, Parmer J, Freimuth VS, Hilyard KM, Musa D, Kim KH. Exploring communication, trust in government, and vaccination intention later in the 2009 H1N1 pandemic: results of a national survey. Biosecur. Bioterror. 2013;11:96–106. doi: 10.1089/bsp.2012.0048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Romaniuc, R., A. Guido, N. Mai, E. Spiegelman, and A. Sutan. Increasing vaccine acceptance and uptake: a review of the evidence. Available at SSRN 3839654, 2021.
- 29.Salmon DA, Moulton LH, Omer SB, DeHart MP, Stokley S, Halsey NA. Factors associated with refusal of childhood vaccines among parents of school-aged children: a case-control study. Arch. Pediatrics Adolesc. Med. 2005;159:470–476. doi: 10.1001/archpedi.159.5.470. [DOI] [PubMed] [Google Scholar]
- 30.Trueblood, J. S., A. B. Sussman, and D. O’Leary. The role of general risk preferences in messaging about COVID-19 vaccine take-up. Available at SSRN 3649654, 2020.
- 31.Weisel, O. Vaccination as a social contract: the case of COVID-19 and US political partisanship. Proc. Natl. Acad. Sci. 118: 2021. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data reported in this study and code generating the results will be made available via the Open Science Framework upon publication: https://osf.io/4peuy.