Abstract
Objective
The purpose of this study was to develop a standardized rounding tool for use on the general paediatric ward and to determine if its use can improve quality of rounds as well as patient and parent satisfaction.
Methodology
The study used a pre- and post-intervention prospective observational methodology. The intervention consisted of the implementation of a Checklist Rounding Tool (CRT) entitled the ‘Paediatric Inpatient Rounding Checklist (PIRC)’ which outlined items deemed essential to discuss during rounds for all patients admitted to the paediatric ward. The PIRC was created by the research team after reviewing the literature and it was peer reviewed by a panel of expert paediatricians. Performance on rounds based on discussion of checklist items as well as patient and parent satisfaction were evaluated by an external observer both pre- and post-PIRC implementation.
Results
Four of the five less frequently addressed checklist items were discussed significantly more post-intervention. The Rounds Quality Score was significantly improved after checklist implementation, the pre- and post-intervention scores being 8.24 and 9.61/10, respectively (P-value <0.001). Patient and parent satisfaction were rated higher with the use of the checklist. There was no difference in the duration of rounds between the pre- and post-implementation phases.
Conclusion
In summary, utilization of a standardized rounding tool on an inpatient paediatric ward led to improvement in quality of rounds as well as patient and parent satisfaction.
Keywords: Bedside rounds, Checklist, Communication, Patient safety, Rounding tool, Teaching rounds
Most standardized checklist approaches in medicine have been studied in the adult population (1–4). Almost all studies concerning the use of checklists in paediatrics were performed in paediatric or neonatal intensive care units (PICU or NICU) (5–12). Use of safety checklists in the PICU has been shown to improve quality of care (5,7,10) but few studies have been conducted on standardization of actual rounds presentation (6,11,12). A few studies have shown that use of a standardized rounding structure leads to a higher level of awareness of problems listed and daily goals for each patient (11), increased family satisfaction with rounds (12) and improvement in all aspects of the rounding process (6) with minimal increase in rounds duration. Most items of these rounding tools were specifically applicable to critically ill patients.
The ‘Family-centered rounds (FCR) checklist intervention’ by Cox et al. (13), is the only study that examined the impact of a rounding checklist on a general paediatric ward. Their checklist partially structured rounds to outline items related to family engagement, promoting effective FCR and patient safety.
As none of the tools described above could be used to completely structure rounds on a general paediatric ward, the goal of this study was to develop a checklist rounding tool (CRT) specifically applicable to the general paediatric ward. Our primary aim was to assess if implementation of a standardized CRT could improve the quality of rounds on a general paediatrics ward. The secondary aim was to explore whether families’ satisfaction with rounds improved with the use of a standardized CRT. We hypothesized that our intervention would accomplish those two objectives.
METHOD
Literature review
The literature was extensively reviewed. Studies discussing standardized rounds, rounds improvement, checklist use, and rounding tools were included. Of the 38 articles selected, most relevant ones were observational studies measuring impact of rounds standardization. Only six studies proposed actual rounding tools (3,6,7,11–13), none of which were designed to completely structure rounds on a general paediatric ward. There was no Cochrane review found on this subject.
Study design, setting, and participants
This study used a pre- and post-intervention prospective observational methodology. It was conducted on the general paediatric ward of Kingston General Hospital (KGH, Ontario) from March to May 2019 and involved a total of 59 paediatric patients and 21 medical team members (attending physicians, residents, and medical students). For the pre- and post-intervention phases, a convenience sample was used of all patients admitted to the general paediatric ward over a 10- and 8-day period, respectively. Eighty-four and 52 observations were conducted during the pre- and post-intervention phases, respectively. Formal sample size calculations were not done, as the parameters needed to estimate power and sample size did not yet exist. Given that Altman (14) indicates that a sample size of 50 is adequate for testing associations or drawing inferences, we felt that this sample was adequate for testing differences in the number of times key topics were addressed during rounds. A convenience sample was also used for the enrollment of the medical team members. The study was approved by Queen’s University Health Sciences & Affiliated Teaching Hospitals Research Ethics Board (HSREB # 6025408).
Development of the Checklist Rounding Tool and Patient and Parents Satisfaction surveys
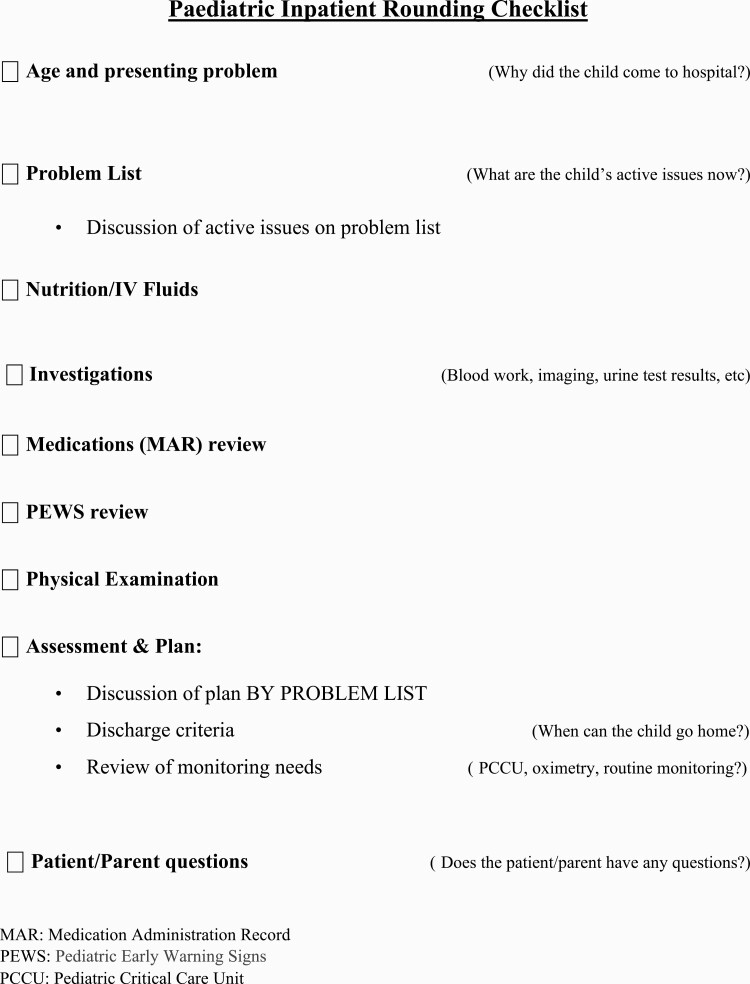
The CRT entitled the Paediatric Inpatient Rounding Checklist (PIRC) was developed by the research team (Figure 1). The items on the PIRC were selected from the Structured interdisciplinary bedside rounds (SIBR) by Stein et al. (3), the ‘CERTAINp’ study (6), ‘WE CARE 4 KIDS’ tool (7), and the survey results from Holton et al. (15). The PIRC was peer reviewed by an expert panel of three paediatricians who were not on service during the study. The content of the checklist was approved by the panel and some modifications to the phrasing of the items were made to ensure complete understanding by junior trainees (see italicized questions on PIRC).
Figure 1.
The Paediatric Inpatient Rounding Checklist (PIRC).
The Patient and Parents Satisfaction survey (Supplementary Appendix 1) was developed through focus groups with parents to identify issues most valued by them during rounds. Our survey was also inspired from patient appreciation surveys in the literature and the survey results described by Holton et al. (15).
Pre-intervention
During the pre-intervention phase, a research assistant (RA) provided direct in-person observation of rounds which were conducted at the bedside and involved one attending physician, one senior and one junior paediatric resident and two to four off-service residents and medical students. The RA assessed the quality of rounds by identifying which items on the PIRC were discussed for each patient. The medical team was blinded to the PIRC content.
Intervention
The medical team was educated about the PIRC and were encouraged to use it to structure their patient’s presentation during rounds.
Post-intervention
Rounds were observed by the RA the same way as during the pre-intervention phase. However, this time, the medical team was using the PIRC to structure their rounds presentation. The composition of the medical team for the post-intervention phase was the same as during the pre-intervention phase (i.e., Medical students, residents, attending staff); however, the individual members were different.
Data collection
Demographic data, American Society of Anesthesiologists (ASA) score, daily Paediatric Early Warning System (PEWS) score, length of stay, most responsible diagnosis, checklist items discussed during rounds and total duration of rounds were collected for all recruited patients pre- and post-intervention. Satisfaction surveys were distributed to patients and/or parents during both pre- and post-intervention phases after every rounds observation.
Data analysis
Descriptive statistics, including means, standard deviations and medians for continuous data, and frequencies and percentages for categorical data, were used to analyze patient demographic characteristics. Data collected regarding items discussed during rounds were analyzed initially using frequencies. Comparisons between pre- and post-intervention data were performed with inferential statistics including independent samples t-tests, and the Pearson chi-square or Fisher’s Exact test as appropriate. The Rounds Quality Score (RQS) was designed by this research team and inspired from the ‘Total checklist compliance score’ from Hulyalkar et al (6), to give an overview of rounds performance. Every item discussed was worth one point. The total number of points obtained for one patient’s presentation was divided by the number of checklist items and multiplied by 10. Data obtained from the score were analyzed with the independent samples t-test, as were the data from the patient and parent satisfaction daily surveys. Twenty and 15 patients were assessed more than once, pre- and post-intervention respectively. The association of observation number (1, 2, 3, and 4+) with the items discussed during rounds was assessed using the Pearson chi-square test. Finally, the associations between PEWS of the day, ASA and the RQS were assessed overall, and pre and post separately, using the Spearman correlation.
RESULTS
Population demographic data
As shown in Table 1, the patients’ mean age was between 5 and 6 years for both pre- and post-intervention phases. Sex distribution showed a slight predominance of male patients. Most patients had an ASA score of 1 or 2. For most patients, the most responsible diagnosis for admission was a respiratory or gastrointestinal condition.
Table 1.
Pre- and post-intervention demographic data
| Characteristics | Time observation | Std. deviation | |||||
|---|---|---|---|---|---|---|---|
| Age: mean in years | Pre | 5.41 | 5.88 | ||||
| Post | 5.99 | 5.68 | |||||
| Male | Female | Other | |||||
| Sex: absolute (%) | Pre | 18 (50) | 17 (47.2) | 1 (2.8) | |||
| Post | 13 (56.5) | 10 (43.5) | 0 (0) | ||||
| 1 | 2 | 3 | 4 | ||||
| ASA score: absolute (%) | Pre | 15 (41.7) | 19 (52.8) | 2 (5.6) | 0 (0) | ||
| Post | 8 (34.8) | 11 (47.8) | 3 (13.0) | 1 (4.3) | |||
| Respiratory | GI | Neuro | Trauma/Incident | Endo | Other | ||
| Most responsible diagnosis: Absolute (%) | Pre | 15 (41.7) | 6 (16.7) | 3 (8.3) | 1 (2.8) | 3 (8.3) | 8 (22.2) |
| Post | 7 (30.4) | 9 (39.1) | 2 (8.7) | 2 (8.7) | 1 (4.3) | 2 (8.7) |
Quality of rounds
As outlined in Table 2, frequency statistical analysis showed that before our intervention, Nutrition, IV Access, Medication, Physical Exam, and Discharge were the items most omitted during rounds, being discussed less than 80% of the time. After the implementation of the checklist all those items, except for IV Access, were significantly more addressed during rounds. PEWS, discussed relatively often without the PIRC, was more frequently mentioned post-intervention. Most Responsible Diagnosis, Active Issues, Plan and Patient/Parents’ questions answered were initially discussed more than 90% of the time and their frequency of discussion remained the same post-intervention.
Table 2.
Quality of rounds: Comparison between pre- and post-intervention
| Rounding tool’s Items |
Time | Items addressed, frequency (%) | Chi-square | P-value |
|---|---|---|---|---|
| Most responsible diagnosis | Pre | 92.8 | 3.934 | 0.082* |
| Post | 100 | |||
| Active issues | Pre | 97.6 | 1.257 | 0.524* |
| Post | 100 | |||
| Nutrition | Pre | 72 | 14.773 | < 0.001 |
| Post | 98.1 | |||
| IV access | Pre | 76.2 | 0.980 | 0.443 |
| Post | 87.5 | |||
| Medication† | Pre | 48.8 | 29.896 | < 0.001 |
| Post | 94.2 | |||
| PEWS‡ | Pre | 84.1 | 7.001 | 0.03 |
| Post | 98.1 | |||
| PE§ | Pre | 66.7 | 16.243 | < 0.001 |
| Post | 96.2 | |||
| Plan | Pre | 100 | 1.627 | 0.382* |
| Post | 98.1 | |||
| Discharge discussed | Pre | 65.4 | 4.698 | 0.03 |
| Post | 82.7 | |||
| Patient/Parents’ questions answered | Pre | 90.5 | 2.957 | 0.228 |
| Post | 92.3 |
*Corrected P-value (Fisher’s Exact test)
†MAR directly reviewed
‡PEWS sheet directly reviewed
§Physical exam findings discussed, or Physical exam stated as not done
Rounding time
The mean rounding time per patient was 0.21 and 0.22 hour during the pre- and post-intervention phases respectively (P-value 0.705).
Rounds Quality Score (RQS) and influencing factors
For the pre- and post-intervention phase, the mean RQSs were 8.24/10±1.36 and 9.61/10±0.61 respectively (P-value < 0.001). This shows a significant improvement in quality of rounds with the CRT.
With repeated presentations for the same patient during a hospital admission, a decrease in rounds quality, especially regarding discussion of Most Responsible Diagnosis, Nutrition and Physical Exam, was observed pre-intervention, but not post-intervention. From the first observation to the fourth for a same patient, Most responsible diagnosis was discussed from 100% to 75% of time (P-value 0.027), Nutrition from 85.7% to 45.5% (P-value 0.035) and Physical exam from 83.3% to 50% (P-value 0.02).
For the pre-intervention phase exclusively, a significant correlation between PEWS and quality of rounds was observed (P-value 0.024). Higher PEWS were associated with greater quality of rounds.
Regarding the ASA score, the only significant observation was that Medication was more often discussed for patients with an ASA score of 2 or 3 in comparison to 1, during the pre-intervention phase. Complete omission of medication was observed 37% of time with ASA 1 patients compared to 4% and 0%, respectively with ASA 2 and 3 patients (P-value 0.001).
It was not possible to assess the influence of the diagnosis type on quality of rounds given the small sample of each diagnosis type.
Patient and parent satisfaction
The Patient and Parents Satisfaction survey (Supplementary Appendix 1) was completed 20 times by patients and 52 by parents during the pre-intervention phase and 7 times by patients and 42 by parents during the post-intervention phase. Almost all surveys distributed were completed.
As provided in Table 3, understanding of discharge timing achieved the lowest level of satisfaction pre-intervention, which improved from a mean of 6.48 to 8.67/10, (P-value < 0.001) post-intervention. The items A, B, D, and E improved significantly post-intervention. Finally, the only item for which there was no difference in satisfaction pre- and post-intervention was the perception of rounding time, with a mean score of approximately 5, meaning just the right duration.
Table 3.
Parents and patients’ rounds satisfaction survey results
| Questions | Time | Mean | Std.-deviation | P-value |
|---|---|---|---|---|
| A. Important information discussed* | Pre | 9.03 | 1.98 | 0.010 |
| Post | 9.78 | 0.507 | ||
| B. Understand the plan* | Pre | 8.81 | 1.95 | 0.002 |
| Post | 9.72 | 0.784 | ||
| C. Understandtiming of discharge* | Pre | 6.48 | 3.25 | < 0.001 |
| Post | 8.67 | 2.135 | ||
| D. Felt included* | Pre | 8.78 | 2.13 | 0.002 |
| Post | 9.76 | 0.591 | ||
| E. No unanswered questions* | Pre | 8.93 | 2.02 | 0.014 |
| Post | 9.70 | 0.953 | ||
| F. Rounding time perception† | Pre | 4.90 | 1.01 | 0.283 |
| Post | 5.06 | 0.240 |
*The first five statements were ranked from 1 to 10, 1 being completely disagree and 10 completely agree.
†The sixth statement was ranked from 1 to 10, 1 being too short, 5 just right and 10 too long regarding rounding time perception.
The qualitative analysis of comments on the survey showed general appreciation (42% and 64% of the comments, respectively pre- and post-intervention) and comments regarding negative experiences or suggestions for improvement (33% and 36%, respectively pre- and post-intervention). Few comments mentioned confusion regarding discharge timing and miscommunication amongst team members during the pre- (3 comments) and post-intervention phases (2 comments).
Discussion
The primary outcome of this study was to assess if the quality of daily inpatient paediatric rounds, which was defined as discussing all items deemed essential for patient care, could be improved by using a standardised rounding tool. In light of our results, using the PIRC improved quality of rounds, without affecting rounding efficiency. Indeed, the RQS showed a significant improvement in global quality of rounds post-intervention. Furthermore, the pre-intervention phase clearly identified important items that were regularly not discussed during rounds: Nutrition, IV Access, Medication, Physical Exam, and Discharge. The use of the PIRC led to significant improvements in addressing these items except for IV Access. Strategies that might improve the addressing of IV access during rounds include assigning an individual on the team to remind team members to use the PIRC during rounds. Idahosa and Kahn (2) observed that encouragement to use a tool by the supervising staff resulted in better uptake of the tool, making omission of rounding items less likely. As time management is a real challenge in all medical units, it is even more interesting that those results were obtained without prolonging rounding time. We can postulate that use of the PIRC helps structure patient presentation on rounds, allowing the team to discuss more topics in a time efficient manner.
The secondary outcome of this study was to explore if patient and parent satisfaction with rounds could be improved with the use of a standardized rounding tool. After comparative analysis of pre- and post-checklist implementation survey data, improved satisfaction was noted, especially with regards to understanding discharge planning. Knowing that discharge criteria is one of the most sought-after pieces of information for a patient/parent (15), use of the PIRC clearly improves the patient/family-centred approach to care.
Some factors were identified as influencing the quality of rounds during pre-intervention observations. Patients’ length of stay and quality of rounds were inversely proportional with respect to discussion of Most Responsible Diagnosis, Nutrition and Physical Exam. These items were progressively more omitted throughout the same patient’s admission. An association between higher PEWS and increased quality of rounds was observed in the pre-implementation phase. Although this is positive, all patients, irrespective of their acuity, deserve all aspects of their care discussed. Using the PIRC controls for these influencing factors and allows higher quality of rounds for all patients, regardless of their acuity or length of stay.
There were some limitations to this study. First, quality of rounds was arbitrarily defined as discussion of all items outlined on the PIRC, without studying the impact of omitting a certain item. Further, the PIRC developed by the research team was not a validated tool; however, we tried to overcome this by incorporating items from other rounding tools in the literature which had been previously validated. The PIRC was also peer reviewed by a panel of general paediatricians. In a future study, it would be interesting to assess the real impact of the checklist on patients’ care such as rates of medical errors and critical incidents, as well as length of stay and re-admission. Second, the RA was not blinded as to whether the rounding tool was being used or not, as the medical team used physical copies of the tool and members were encouraged to use the tool by the senior resident if it was forgotten. We did however ensure the RA was rigorously trained to identify items discussed during rounds that were consistent with the PIRC items. Third, with respect to the secondary outcome of assessing patient and parent satisfaction with rounds, the patient/parent sample size was small. It would be interesting to repeat the study with a greater sample of patients to confirm or invalidate our results. Finally, the impact of the checklist was studied in a teaching hospital, where good communication is often challenging given multiple professionals and learners involved in patient care. We would expect similar outcomes in other teaching hospitals. In the community setting however, its applicability may not be as strong as a single physician typically rounds alone, reducing the need for structured rounds presentation. In that situation, the checklist could be used as a reminder to prevent overlooking important components of patient care, rather than using it as a communication tool. The research team is happy to report that the original version of the PIRC continues to be in use with good uptake from staff physicians at KGH.
In sum, this study suggests that use of a standardized rounding tool can improve quality of rounds on a general paediatric ward. It showed significant improvement in terms of addressing all items deemed essential to discuss during daily rounds for optimal patient care and led to increased patient and parent satisfaction with rounds, without impacting rounding time.
Supplementary Material
ACKNOWLEDGEMENTS
We appreciate the help of Wilma Hopman, statistician at KHSC, who helped us with the study design, statistical analysis and data interpretation, and Dr. Kimberly Dow, neonatologist at KHSC, who helped us reviewing the manuscript prior to our initial submission. We recognize the valuable participation of all the members of the medical team who were observed during this project. Finally, we especially want to thank all patients who agreed to take part in this study, as well as their parents.
Funding: There are no funders to report for this submission.
Potential Conflicts of Interest: All authors: No reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Collins S, Hurley AC, Chang FY, et al. Content and functional specifications for a standards-based multidisciplinary rounding tool to maintain continuity across acute and critical care. J Am Med Inform Assoc 2014;21(3):438–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Idahosa O, Kahn JM. Beyond checklists: using clinician prompts to achieve meaningful ICU quality improvement. Crit Care 2012;16(1):305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Stein J, Payne C, Methvin A, et al. Reorganizing a hospital ward as an accountable care unit. J Hosp Med 2015;10(1):36–40. [DOI] [PubMed] [Google Scholar]
- 4. O’Leary KJ, Killarney A, Hansen LO, et al. Effect of patient-centred bedside rounds on hospitalised patients’ decision control, activation and satisfaction with care. BMJ Quality & Safety 2016;25(12):921–8. [DOI] [PubMed] [Google Scholar]
- 5. Sharma S, Peters MJ. “Safety by DEFAULT”: Introduction and impact of a paediatric ward round checklist. Critical Care 2013;17:R232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hulyalkar M, Gleich SJ, Kashyap R, et al. Design and α-testing of an electronic rounding tool (CERTAINp) to improve process of care in pediatric intensive care unit. J Clin Monit Comput 2017;31(6):1313–20. [DOI] [PubMed] [Google Scholar]
- 7. Ganesan R, Rajakumar P, Fogg L, Silvestri J, Kane JM. WE CARE 4 KIDS: Use of a rounding tool in the Pediatric Intensive Care Unit. Pediatr Qual Saf 2017;2(6):e044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Chuo J, Graysib S, Hufnal C, Carroll J, Jani G. Results from implementing medical checklist “rounding tool” into care practices in a large Neonatal Intensive Care Network. Pediatrics 2018;142: 364. [Google Scholar]
- 9. Arriaga Redondo M, Sanz López E, Rodríguez Sánchez de la Blanca A, et al. Mejorando la seguridad del paciente: utilidad de las listas de verificación de seguridad en una unidad neonatal [Improving patient safety: Usefulness of safety checklists in a neonatal unit]. An Pediatr (Barc) 2017;87(4):191–200. [DOI] [PubMed] [Google Scholar]
- 10. Mckelvie BL, Mcnally JD, Menon K, Marchand MGR, Reddy DN, Creery WD. A PICU patient safety checklist: Rate of utilization and impact on patient care. International Journal for Quality in Health Care 2016;28(3):371–5. [DOI] [PubMed] [Google Scholar]
- 11. Seigel J, Whalen L, Burgess E, et al. Successful implementation of standardized multidisciplinary bedside rounds, including daily goals, in a pediatric ICU. Joint Commission Journal on Quality and Patient Safety 2014;40(2):83, AP1–90,AP2. [DOI] [PubMed] [Google Scholar]
- 12. Lopez M, Vaks Y, Wilson M, et al. Impacting satisfaction, learning, and efficiency through structured interdisciplinary rounding in a pediatric intensive care unit: A quality improvement project. Pediatric Quality & Safety 2019;4(3):e176–e176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Cox ED, Jacobsohn GC, Rajamanickam VP, et al. A family-centered rounds checklist, family engagement, and patient safety: a randomized trial. Pediatrics 2017;139(5):e20161688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Altman DG. Practical Statistics for Medical Research. London: Chapman and Hall; 1991:456. [Google Scholar]
- 15. Holton R, Patel R, Eggebrecht M, et al. Rounding on rounds: Creating a checklist for patient- and family-centered rounds. Am J Med Qual 2015;30(5):493. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.