CASE PRESENTATION
A previously healthy 2-year-old girl presented to the Emergency Department with 2-day history of vomiting, lethargy, fever, and poor oral intake. On initial presentation she was tachycardic with intermittent irritability. She also had dry mucous membranes, pallor, and mild dehydration. Glasgow Coma Scale (GCS) score was 13, with eye, verbal, and motor scores of 4, 4, and 5, respectively. Bloodwork revealed a significant iron deficiency anemia with hemoglobin of 70 g/L, thrombocytosis, and mild leukocytosis. Additional routine bloodwork and coagulation profile were unremarkable. On history, her dietary intake consisted of 2% cow’s milk (72 oz daily) with intake of few solids. Patient was admitted for further workup, parenteral hydration, analgesia, and iron supplementation.
Additional investigations including COVID swab, blood, and urine cultures were negative. She remained irritable throughout her hospital stay. She began to deteriorate neurologically with GCS between 10 and 11, although no focal neurological deficits were present. On examination, she was persistently moaning and lethargic. A CT scan of the brain revealed the underlying diagnosis.
DIAGNOSIS: CEREBRAL VENOUS SINUS THROMBOSIS
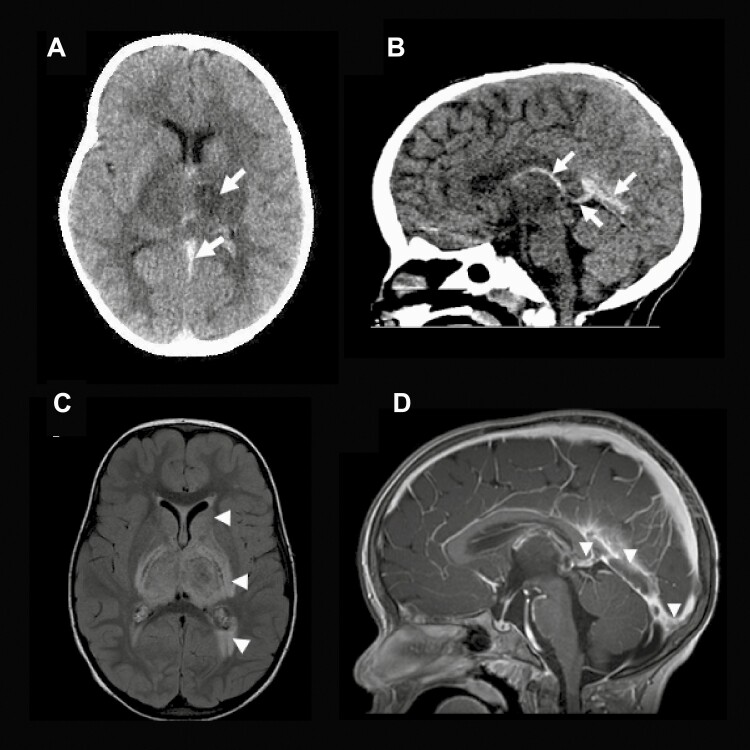
The noncontrast CT scan (Figure 1) revealed a hyperdense straight sinus, vein of Galen, and internal cerebral vein, as well as diffuse hypodensities in the thalami and basal ganglia bilaterally suggestive of venous congestion and raising the strong likelihood of a deep system cerebral sinus vein thrombosis (CSVT). Following imaging the patient received a packed red blood cell transfusion, as hemoglobin levels continued to drop to 57 g/L and the patient was transferred to the intensive care unit of tertiary paediatric hospital. A repeat CT scan revealed further progression of parenchymal hypodensities, while CT venography demonstrated intraluminal filling defects in the above-mentioned venous structures thereby confirming the diagnosis of CSVT. Thereafter, heparin was initiated. In subsequent days, follow-up brain MRIs (Figure 1) with contrast were performed to monitor CSVT progression. Following improvement in level of consciousness, a mild right-sided hemiparesis due to asymmetric thalamic venous infarction became evident. The patient was subsequently transferred to a paediatric rehabilitation hospital for inpatient rehabilitation.
Figure 1.
Brain images of 2-year-old girl with iron deficiency anemia, demonstrating cerebral sinus venous thrombosis. CT head demonstrates a hypodense left thalamus, a high attenuating density present within the straight sinus (SS), favored vein of Galen (VoG), and internal cerebral vein consistent with CVST, seen in the axial (Panel A) and sagittal views (Panel B). (Arrows). (Panel C) The MRI FLAIR-weighted axial image depicts increased signal in the bilateral thalamus, globus pallidus, genu and posterior limbs of the internal capsule, putamen, and the trigones suggestive of extensive edema. Also, a mild ventriculomegaly is evident. (Panel D) The sagittal enhanced T1-weighted image shows the intraluminal thrombus filling the torcula, SS, and VoG (Arrow heads).
CSVT is a form of ischemic stroke where a clot develops in the dural venous sinuses that drain blood from the brain, with an incidence of 0.4 to 0.7 per 100,000 children (1). Although clinical manifestations can be life-threatening and lead to long-term neurological sequelae, diagnosis is frequently delayed or missed, as symptoms and signs are often nonspecific (1,2). Paediatric CVST has been associated with various etiologies including dehydration, infection, head trauma, hematological disorders, malignancy, and acquired and rarely inherited prothrombotic disorders (1). Among hematological disorders, iron deficiency anemia (IDA) is important to identify as it is a relatively common condition in developed countries, with a peak prevalence of 4% to 8% in children between 12 and 36 months of age (2). In fact, studies have demonstrated that previously healthy children with ischemic stroke were 10 times more likely to have IDA compared to healthy children without ischemic stroke (2). In addition, children with IDA accounted for more than half of all stroke cases in children without an underlying medical condition (2).
Signs and symptoms of CSVT are typically nonspecific (1). A majority of cases are acute/subacute in onset, presenting with signs and symptoms of raised intracranial pressure such as decreased level of consciousness, papilledema, false localizing sixth nerve palsy, and bulging fontanelle in infants (1). Other clinical manifestations include seizures, encephalopathy, focal neurologic deficits (hemiparesis and hemisensory losses), and diffuse neurologic symptoms (headache, nausea, emesis) (1).
In general, unenhanced CT imaging may occasionally detect deep venous thrombosis, although this imaging is rarely diagnostic (1). Ideally, contrast enhanced CT or CT venography is needed to definitively diagnose CSVT, although CT scans with contrast still miss the diagnosis in up to 40% of cases (1). Therefore, the preferred modality to confirm the diagnosis of CVST is brain MRI and MR venography to demonstrate the infarct and the clot within the vessels (1). Once diagnosed, children are often treated with iron supplementation (in cases of IDA), and anticoagulation including treatment with heparin or low-molecular weight heparin (LMWH) initially followed by a minimum of 3 months of LMWH or a vitamin K antagonist (3–5). In general, anticoagulated children are more likely to have good cognitive outcomes (1,5).
In conclusion, CSVT is an under recognized condition in children with significant neurological consequences, which can present with nonspecific signs and symptoms. If risk factors for CVST are present (such as severe iron deficiency anemia) in the setting of altered neurological examination, further definitive contrast-based neuroimaging should be performed if there is a high level of clinical suspicion. Furthermore, cases of severe IDA, in which excess milk intake is a common cause, should be actively monitored for risk of developing CSVT and treated promptly.
CLINICAL PEARLS
Paediatric cerebral sinus venous thrombosis (CSVT) is a rare condition that can present nonspecifically with headache, lethargy, altered level of consciousness, seizures, hemiparesis, cranial nerve abnormalities, and coma.
Iron deficiency anemia is a common condition in children which can result in CSVT and stroke.
When there is a high degree of suspicion, neuroimaging with contrast enhanced CT head, CT venography, or brain MRI (preferred modality) should be done promptly to confirm the diagnosis.
Informed Consent
Written consent was obtained from the patient’s family for publication of this case.
Funding
This research received no specific grant from any funding agency.
Potential Conflicts of Interest
There are no conflicts to disclose. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Dlamini N, Billinghurst L, Kirkham FJ. Cerebral venous sinus (sinovenous) thrombosis in children. Neurosurg Clin N Am 2010;21(3):511–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Maguire JL, deVeber G, Parkin PC. Association between iron-deficiency anemia and stroke in young children. Pediatrics 2007;120(5):1053–7. [DOI] [PubMed] [Google Scholar]
- 3. Monagle P, Chan AKC, Goldenberg NA, et al. Antithrombotic therapy in neonates and children: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 2012;141(2 Suppl):e737–801S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Saposnik G, Barinagarrementeria F, Brown RD Jr, et al. ; American Heart Association Stroke Council and the Council on Epidemiology and Prevention . Diagnosis and management of cerebral venous thrombosis: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2011;42(4):1158–92. [DOI] [PubMed] [Google Scholar]
- 5. Monagle P, Cuello CA, Augustine C, et al. American Society of Hematology 2018 Guidelines for management of venous thromboembolism: treatment of pediatric venous thromboembolism. Blood Adv 2018;2(22):3292–316. [DOI] [PMC free article] [PubMed] [Google Scholar]