Abstract
Myopia has reached epidemic levels in recent years. Stopping the development and progression of myopia is critical, as high myopia is a major cause of blindness worldwide. This overview aims at finding the association of time spent outdoors (TSO), near work (NW), and physical activity (PA) with the incidence, prevalence, and progression of myopia in children. Literature search was conducted in PubMed, Scopus, Cumulative Index to Nursing and Allied Health Literature, Cochrane Database of Systematic Reviews, ProQuest, and Web of Science databases. Systematic reviews (SR) and meta-analyses (MA) on the TSO, NW, and PA in relation to myopia were reviewed. Methodological nature of qualified studies were evaluated utilizing the Risk of Bias in Systematic Review tool. We identified four SRs out of which three had MA, which included 62 unique studies, involving >1,00,000 children. This overview found a protective trend toward TSO with a pooled odds ratio (OR) of 0.982 (95% confidence interval (CI) 0.979–0.985, I2 = 93.5%, P < 0.001) per extra hour of TSO every week. A pooled OR 1.14 (95% CI 1.08–1.20) suggested NW to be related to risk of myopia. However, studies associating myopia with NW activities are not necessarily a causality as the effect of myopia might force children to indoor confinement with more NW and less TSO. PA presented no effect on myopia. Though the strength of evidence is less because of high heterogeneity and lack of clinical trials with clear definition, increased TSO and reduced NW are protective against myopia development among nonmyopes.
Keywords: Indoor activity, myopia, near work, physical activity, time spent outdoor
Myopia is the most common disorder with a wide variation in prevalence concerning age, race, ethnicity, urbanization, occupation, and education level.[1] In the South-East Asian population, myopia prevalence of more than 80% has been documented, with the prevalence of high myopia exceeding 20%,[1,2,3,4] while the prevalence is increasing among the Western population.[2,5,6,7]
The rising prevalence of myopia is a significant public health issue,[1,8,9] as high myopia imposes lifelong medical care due to increased risk of degenerative retinal conditions, primary open-angle glaucoma, early-onset cataract, and retinal detachment.[1,3,4,10] Moreover, though myopia management is simple with corrective lenses, its negative economic, social, and educational impact have been well documented.[10]
Various clinical trials have shown changes in refractive error when eyes are exposed to form deprivation, hyperopic defocus, alteration of the daily light level, and also lifestyle changes like duration of near work (NW), time spent outdoors (TSO), and physical activity (PA) during childhood. Rise in the incidence and progression of myopia has shown genetic influence along with environmental factors.[11,12,13,14,15,16,17,18,19]
Among environmental factors, the interventional effect of PA, TSO, and NW against myopia has been documented. However, there is a lack of evidence on the interrelation between these factors concerning myopia development and progression.[2,9,20]
Furthermore, during the COVID-19 pandemic, many of the world population were restricted at home confinement with a sedentary life. Toddlers, children, and teenagers got exposed to an unusual amount of indoor time. Additionally, online classes for students have added to the burden of NW and digital screen time (television, smartphones, etc.), sparking concerns that these children may have an even higher risk of myopia development and progression.[21]
Thus, the main aim of this review is to gather evidence from existing systematic review (SR)/meta-analysis (MA) on the influence of TSO, PA, and NW on the incidence, prevalence, and progression of myopia.
Methods
Preferred Reporting Items for Systematic Reviews and Meta-Analysis guidelines has been followed in this SR.[22] The protocol of current review is registered in the International Prospective Register of Systematic Reviews (CRD42018096186).
Search strategy
Two independent reviewers (KKS, PM) searched for articles in various databases with a week’s gap. Articles indexed in PubMed, Scopus, Cumulative Index to Nursing and Allied Health Literature, Cochrane Database of Systematic Reviews, ProQuest, and Web of Science were considered for this SRs. On January 31, 2019 last search was done. The search terms used were (“Myopia” OR “myopic” OR “near-sightedness” OR “myopia*” OR “short sight” OR “short-sighted” OR “short-sightedness” OR “short sight” OR “short sighted” OR “short sightedness” OR “near-sight” OR “near-sighted” OR “near-sightedness” OR “near sight” OR “near sighted” OR “near sightedness” OR “refractive errors” OR “refract*”) AND (“exercise” OR “physical activity” OR “physical activities” OR “motor activity” OR “exercises” OR “motor activities” OR “outdoor*” OR “outside” OR “leisure Activities” OR “sport*” OR “hobby*” OR “environment” OR “time spent outdoor” OR “near activity” OR “near work” OR “studying” OR “reading” OR “reading distance” OR “working distance” OR “outdoor activity” OR “indoor activity” OR “sunlight exposure” OR “darkness” OR “dark”). The search strategy used for the keywords in PubMed is described and cumulated in Appendix-Table A1. The articles searched were restricted to only English language.
Study selection
Two reviewers independently (KKS, PM) accessed each article’s title and abstract based on the association between myopia and TSO, NW, and PA to include in the current review. In addition, references were searched manually for yielded articles to include relevant SRs in this current study. Further, the full-text review was performed by (ADL, PM) reviewers independently. The screening of articles was done using Covidence to ensure the blinding in both phases. If there was any conflict while selecting articles, it was resolved with the mutual discussion between the authors (ADL, AN, KKS, and PM). The exclusion criteria were as follows (1) not available in English, (2) published in books or gray literature, conference abstracts, and (3) studies with inappropriate and/or insufficient quality.
Data extraction
Two reviewers (ADL, PM) independently extracted for (1) the general data: title of the study article, author names, year of publication, (2) article related data: study design, sample size, (3) participant data, (4) type of intervention, (5) age (mean, standard deviation; range), (6) sex (% men and % women), (7) study location, (8) any other specific population (if any), (9) visual acuity effect estimate with 95% confidence interval or standard error, (10) confounding factor adjusted for data management, and (11) study outcome (odds, risk, refractive error, axial length change, proportion developing myopia, and progressing).
Assessment of methodological quality and risk of bias
Critical appraisal tool “Risk of Bias in Systematic Review (ROBIS)” was used to assess the quality of the articles included in full-text review (Appendix-Table A4).[23]
The list of index articles in qualified SR/MA was looked into to recognize those contained in two or more reviews (Appendix-Tables A2 and A3).
Statistical analysis
STATA version 12.0 software (STATA Corporation, College Station, TX, USA) was used to perform statistical analysis. Pooled odds ratio (OR) and Mantel–Haenszel random-effects model with 95% CI was used to analyze dichotomous outcome data and data for MA, respectively. I2 test was used to assess statistical heterogeneity; high heterogeneity was considered if I2 ≥50%. MA and heterogeneity calculation were done only to estimate prevalence of myopia in association with TSO. The MA was done after removing the duplicates to avoid repetition of data. There were six overlaps, and finally, it was 14 primary study data used for MA after removing duplicates. As the number of included data were minimum, duplicates were removed manually. Standardized effect estimated values of included papers have been incorporated in the MA of current study.
Results
Literature search
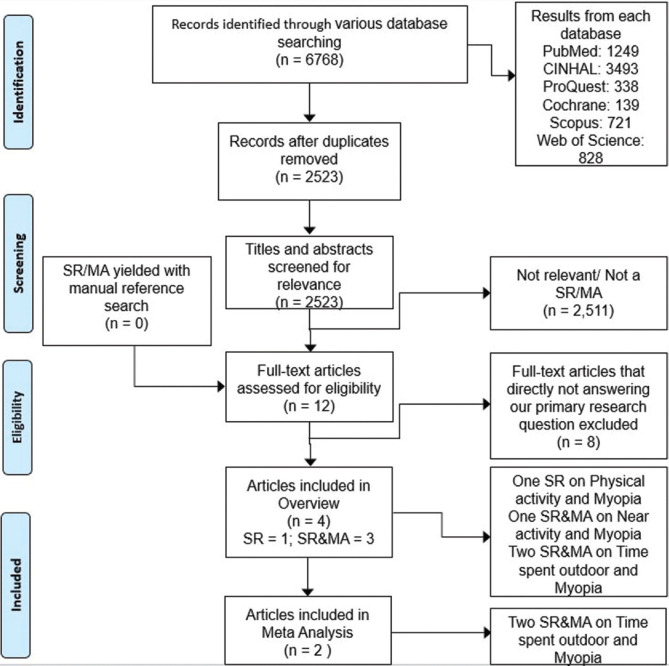
We identified 6768 articles from the various databases. After removing the duplicates and screening of the articles for eligibility, we identified four SRs out of which three had MA included for review. The included SRs had 62 unique studies. [Table 1 and Appendix-Tables A4–A6]; details mentioned in Fig. 1.
Table 1.
Summary of results of studies included in the review
| Review & type of study | Aim of study | No. of primary studies (sample size) | Types of studies included in the review | Ethnicity/ Location | Age range (years) | Definition of myopia (in Diopter sphere) | Intervention | Measuring tool | Conclusion |
|---|---|---|---|---|---|---|---|---|---|
| Anne-SuhrThykjær, et al. (2016) SR | To examine the association between physical activity and the development and progression of myopia | 9 (17,634) | Cross-sectional, cohort, case control | Ireland, Britain, Netherlands, Australia, Finland, Singapore, USA, Jordan | 7-20 years, 33-37 years | -0.25, -0.50, -0.75, -1.00 | Physical activity | Subjective and objective utilities to quantify amount of PA (Questionnaire and accelerometer) | No evidence of physical activity having any effect on myopia |
| Justin C. Sherwin et al. (2012) SR and MA | To summarize relevant evidence investigating the association between time spent outdoors and myopia in children and adolescents | 23 (33,926) | Cross-sectional, cohort, randomized controlled trial | East Asian and Non east Asian (USA, Singapore, Australia, Jordan, China) | 6-18 years, 11-20 years, and 6-72 months | -0.25 DS | Time spent outdoors | The sum of general activities, leisure activities, and sports performed outdoors | Increasing time spent outdoors is a simple strategy to reduce the risk of developing myopia and its progression |
| ShuyuXiong, et al. (2017) SR and MA | To evaluate the evidence for association between time outdoors and the prevalence, incidence, and progression of myopia | 52 (66,379) | Cross-sectional, cohort, randomized, and controlled clinical trial | East Asia, Australia, French, UK, USA, and Turkey | 6-18 years, 18-24 years, 6-72 months, and aged 50 years or older | -0.25 DS | Time spent outdoors | Subjective and objective utilities to quantify amount of time spent outdoors (Questionnaire and accelerometer) | Increased time outdoors is effective in preventing the onset of myopia, but ineffective in reducing progression in existing myopes |
| Hsiu-Mei Huang et al. (2015) SR and MA | To quantify the effect of near work activities on myopia in children | 27 (25,110) | Cohort, cross-sectional | Asia, North America, Australia, Europe, and Middle East | -0.50 DS and above | Near activity | Near activity in questionnaires completed by parents, children or both. | Near work activities were associated with myopia and that increased diopter-hours of near work might increase myopia prevalence |
SR: systematic review, MA: meta-analysis
Figure 1.
Details about selection of articles. Note: SR – systematic review; MA – meta-analysis
Physical activity and myopia
Among two prospective cohort studies, one with 9109 children, extreme levels of PA had borderline association with incident myopia (≥ -1.0 DS), (OR: 0.88, 95% CI: 0.76–1.01, P = 0.062). Similarly, myopia had a higher risk (HR: 1.17, 95% CI: 1.10–1.24) related to sedentary time (accelerometer).[11] Another questionnaire-based study with 151 medical students (mean age 23.1 years) showed that nonmyopic students had more PA than their myopic counterparts (60 vs 51 min/day, P = 0.049). The increase prevalence of myopia (≥ -0.50 DS) was from 37 to 42.7% within 2 years of study span [Table 1 and Appendix-Table A6].[24]
Among six cross-sectional studies (8242 children), comparison between children with PA (>3 h/week) vs sedentary lifestyle revealed that self-reported PA was associated with lower prevalence of myopia (≥ -0.50 DS) (OR: 0.46, 95% CI: 0.23–0.90, P = 0.027).[25] Results with PA measured using wrist-worn accelerometers and myopia (≥ -0.75 DS); the mean difference in the PA levels between the emmetropic and myopic participants was not significant (P = 0.14).[26] Questionnaire-based studies demonstrated myopic children spent less time playing sports than emmetropes ([1.87 vs 4.04 hours/day, P < 0.0001],[27] [0.72 vs 0.85 h/day, P = 0.007],[28] and [7.4 vs 9.7 h/week]).[29] Protective effect (questionnaire-based) on myopia was found with daily PA and sports (OR: 0.89, 95% CI: 0.86–0.93)[27] and weekly PA (OR: 0.94, 95% CI: 0.89–0.98, P = 0.0045).[29] Questionnaire-based PA assessment demonstrated myopic refraction which is least (+0.56 DS, 95% CI: 0.38–0.75, P = 0.04) in participants with high levels of outdoor activity and low levels of NW.[30] The association of outdoor sports was high with reduced myopia prevalence (OR: 0.90, 95% CI: 0.84–0.96, P = 0.004) and indoor PA failed to show any such association.[28] However, participants with low levels of outdoor activity and high levels of NW demonstrated myopic refraction more (+0.27 DS, 95% CI: 0.02–0.52, P = 0.06).[30]
One case-control study (131 adult men) investigating childhood effect of PA and myopia (≥ -0.25 DS) concluded that myopic adults recollected being less interested in PA during their childhood compared to the nonmyopic adults (25% vs 5.7%, P < 0.03) [Table 1 and Appendix-Table A6].[31]
Time spent outdoors and myopia
Three clinical trials[32,33,34] (2865 children) demonstrated protective effect on incident myopia (risk ratio (RR): 0.536, 95% CI: 0.338–0.850, I2 = 87.7%, Pheterogeneity < 0.001) with increasing TSO during school recess. On excluding He et al.[32] study for sensitivity analysis, two clinical trials showed lower risk (RR: 0.435, 95% CI: 0.344–0.550, I2 = 0%, Pheterogeneity = 0.829) without any heterogeneity when pooled [Table 1 and Appendix-Table A6].[35]
Three cohort studies[11,36,37] (4064 children) reported significantly reduced risk of incident myopia associated with high TSO levels (RR: 0.574, 95% CI: 0.395–0.834, I2 = 70.9%, Pheterogeneity = 0.032). For sensitivity analysis, only the removal of younger cohort by French et al.[36,37] study showed higher risk (RR: 0.693, 95% CI: 0.548–0.877, I2 = 0%, Pheterogeneity = 0.933) with no heterogeneity [Table 1 and Appendix-Table A6].[35]
Thirteen cross-sectional studies[28,29,38,39,40,41,42,43,44,45,46,47,48] (23,112 children) investigated the effect of TSO on incident myopia and found an OR of 0.964, 95% CI: 0.945–0.982, I2 = 93.2%, Pheterogeneity < 0.001). Although the overall OR did not change substantially on exclusion of any study (OR: 0.960–0.984), exclusion of Guo et al.[47] reduced the heterogeneity from 93.2 to 39.8% [Table 1 and Appendix-Table A6].[35]
Seven studies[11,32,33,37,49,50,51] (8437 children) studied the dose–response relationship of TSO with myopia. The dose–response curve between incident myopia risk and TSO was linear, with an inverse relationship (R2 = 0.586). The linear equation relating TSO and myopia (y = -0.189 ln(x) + 0.9136), showed TSO of 1 h/day (7 h/week) reduces incident myopia by 45% compared to controls, while 76 min/day (8.9 h/week) showed 50% [Table 1 and Appendix-Table A6].[35] Dividing the TSO into tertiles shows the lowest tertile (≤13.5–16 h/week) had significantly (P < 0.01) higher OR for incident myopia than the highest tertile (>22.5–23 h/week).
Three clinical trials[32,33,34] (2865 children) estimated the risk of myopia progression or shift concerning the TSO and had a weighted mean difference of -0.30 D, 95% CI: -0.18 to -0.41D, I2 = 58.6%, and Pheterogeneity = 0.089 [Table 1 and & Appendix-Table A6].[35]
Six studies[51,52,53,54,55,56] (3956 children) evaluated dose–response between myopia progression and TSO and failed to find any relationship (R2 = 0.00064).[35] Only one study showed protective treatment effect on myopia progression (mean difference between test and control eye -0.14 D, 95% CI: -0.22 to -0.06).[52] Other studies had no statistically significant effect (range -0.12 D to 0.013 D) [Table 1 and Appendix-Table A6].
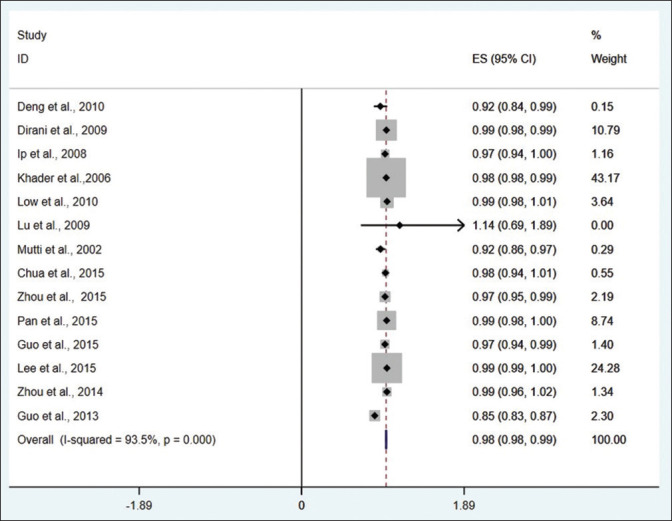
On analyzing the data available for TSO and myopia prevalence, we calculated the pooled OR to be 0.982 (95% CI: 0.979–0.985, I2 = 93.5%, Pheterogeneity < 0.001) per additional hour of TSO/week [Fig. 2].
Figure 2.
Forest plot corresponding to main random-effects meta-analysis performed to quantify the relationship between the time spent on outdoor activities and the prevalence of myopia. Note: ES – effect size
Near work and myopia
Among 15 cross-sectional studies examining the prevalence of myopia and the effect of NW, 10 studies[27,29,38,40,47,57,58,59,60] (9076 children) reported increased prevalence myopia with increased NW among 6–18 years old children. Myopic children had more NW compared to the nonmyopic (2.7 ± 0.7 vs 2.3 ± 1 h/day, P = 0.0027).[59] Additionally, reading two or more books/week were associated with higher odd (OR: 1.43 of SE ≤ -0.50D and OR: 3.05 of SE ≤ -3D) of developing myopia than those reading less than two books/week.[58] Moreover, continuous reading (>30 min) and close reading distance (<30 cm) increased the risk of myopia by 1.5 times (95% CI: 1.05–2.10) and 2.5 times (95% CI: 1.7–4.0), respectively.[40] The multivariate risk of myopia in children in terms of 1 diopter-h of NW/week is estimated to be 1.02.[29,57] Myopic children were also found to watch more television (12.78 ± 9.28 vs 8.91 ± 5.95 h/week, P = 0.02) compared to the nonmyopes.[38] Longer hour of reading (>5 h per day) was associated with the higher prevalence of myopia (43.1% vs 28.6%, P < 0.001).[57] Others reported an increase in odds of having myopia for every additional hour spent reading, writing, studying, or computer work by 16–38% [Table 1 and Appendix-Table A6].[27,47]
The other five studies[30,39,61,62,63] (7297 children) failed to show any association between NW and myopia even after factors adjusted for age, sex, and parental education. There was weak or no correlation between myopia and NW such as watching television, computer, reading, and writing.[61] Myopic and nonmyopic children spent similar time on NW activities like personal reading (23.8 ± 24.7 vs 20.7 ± 21.2 diopter-h/week, P = 0.12), computer use and playing video games (18.9 ± 24.9 vs. 21.8 ± 24.7 diopter-h/week, P = 0.11), homework (35.3 ± 25.9 vs. 34 ± 24.4 diopter-h/week, P = 0.62), and watching television (6.8 ± 5.3 versus 6.2 ± 5.2 diopter-h/week, P = 0.22).[39] Furthermore, prevalence of myopia among children spending various levels of NW (0–2, 1.6–3.1, and >2.6–3.0 h/day) were also similar (P > 0.05) among different age groups (6 and 12-year olds).[30] Similarly, other levels of NW (<2.79, 2.79–3.85, and 3.86–8 h/day) reported similar refraction in children (6–12 and 13–17-year olds).[62] However, the prevalence of myopia was lower in Sydney (3.3%) than in Singapore (29.1%) [Table 1, Appendix-Table A6].[63]
The pooled OR from cross-sectional studies resulted in 1.14 (95% CI: 1.08–1.20) indicating the association of NW with myopia risk. However, the studies MA explained the influence of small-study effect and potential publication bias in the studies with the asymmetrical distribution of the studies in their funnel plot (P = 0.003). Subgroup analysis reported myopia’s likelihood with children performing more NW (OR: 1.85, 95% CI: 1.31–2.62, I2 = 85%) with an additional 2% increased risk of myopia for 1 diopter-hour of NW/week.[20]
Six cohort studies[11,37,49,50,51,64] estimated the association between incidence of myopia and NW. The increase in prevalence of myopia in association with NW was reported in only two studies (3432 children).[37,64] The myopic group had 3 diopter-hours/week of NW more than the nonmyopic group, which increased by 1.7 diopter-hours/week, compared to the previous year when the eyes were nonmyopic.[64] Also, younger children (6-year-old) who became myopic significantly performed more NW than those who did not become myopic (19.4 vs 17.6 h/week, P = 0.02).[37] Although not significant, similar results with higher risk of developing myopia (HR: 1.22, 95% CI: 0.96–1.55, P = 0.098) were obtained for children spending >3 h/day in reading in comparison with less than 3 h/day.[11] Distinctively, multivariate RR of 0.99 (95% CI: 0.97–1.01) per diopter-hour/week of NW was reported.[49] Similarly, a 5-year follow-up on children revealed that newly myopic and nonmyopic children spent similar time (39.49 ± 20.79 vs 39.22 ± 19.67 diopter-h/week, P = 0.90) on NW activity.[50] After adjusting for the recess period outside the classroom, NW like painting, reading, computer use, writing, playing piano, or watching television does not affect the risk of developing myopic in school children.[51] The pooled OR from the cohort studies gave a RR of 1.00 (95% CI: 0.99–1.01, I2 = 43%) for every diopter-hour of increasing NW [Table 1, Appendix-Table A6].[20]
Among six longitudinal studies[52,53,56,65,66,67] evaluating the relationship between myopia progression and NW activity among children, two studies (355 children) reported a higher risk of myopia progression associated with NW.[66,67] However, the other four (1547 children) did not support this conclusion showing any relationship between the two.[52,53,56,65] In group where myopia progression was faster (-2.9 ± 0.6D), it was reported to have a significantly closer reading distance (22 ± 3.8 vs 24.1 ± 4.3 cm) and more NW activity (3.5 ± 0.9 vs 2.9 ± 0.8 h/day) in comparison with the group with slower myopia progression (-0.5 ± 0.3 D).[66] A higher proportion of children (48.8%) with 6 h/day of reading and NW had myopia progression compared to a lower proportion of children (18.9%) in the control group.[67] Interestingly, there is a reported significant difference in myopia progression (0.52 ± 0.19 D vs 0.38 ± 0.15 D, P < 0.01) among the intervention group performing less near and middle vision work (<30 h/week) and more outdoor activity (>14–15 h/week) compared to the control group (>30 h/week and <14–15 h/week). Although the time spent in NW were found to be similar among the two groups, the intervention group had significantly higher outdoor activity (13.7 ± 2.4 vs 6.2 ± 1.6 h/week, P < 0.01).[52] Linear regression analysis of cycloplegic refraction changes over 2 years in children also yielded no statistically significant association with NW activities.[53] Likewise, it was reported that there is no association between myopia progression per year and hours of NW activity. Others said a 2% increase (nonsignificant, P = 0.07) in risk of myopia progression among children performing each additional hour of NW.[65] Due to varying definition of myopia progression and different outcomes, the MA could not combine their results [Table 1, Appendix-Table A6].
On analyzing myopes and nonmyopes for the time spent on NW activities, it was found that myopic children spend 0.66 h/week more on reading (95% CI: 0.16–1.17) concerning nonmyopes. NW such as watching television, playing computer games, and studying were not associated with myopia.[20]
Age
Analyzing the effect of age on the risk of myopia and TSO in cohort studies, it was found that younger age groups (6-year-olds) have more protective effect against myopia (RR: 0.380, 95% CI: 0.259–0.558) than older kids (11–12-years). In case of cross-sectional studies, there was no significant difference between the groups of myopia prevalence (<20%, 20–80%, >80%) or between age groups (<6, 6–18, >18-years) on the protective effect of TSO [Table 1, Appendix: Table A6].[35]
Gender
Studies after adjusting for age, initial refraction, and NW show a significant association between increasing TSO with reduced myopic progression with no reduced final spherical equivalent in females but in males.[9]
Geographical location represented in studies
In all the four review papers,[2,9,20,35] wide geographical locations have been selected [Table 1].
Definition of myopia
The various definitions of myopia have been described in the literature and included in Table 1, which ranged spherical equivalent less than from -0.25 to -1.00 DS.[2,9,20,35]
Discussion
The current systematic overview aimed to summarize all relevant evidence concerning TSO, NW, and PA related to myopia development and progression [Table 2a and 2b]. At younger ages, myopia progression is rapid.[20] Therefore, the current review included articles that studied population aged ≤20 years. The studies found a general relation of lower risk of myopia and PA without any associated effect or trend of the study population, ethnicity, or age connecting the two. Most children of 7–15 years were the participants with exception in few studies where students aged 11–20,[28] adults with mean age of 23.1 years,[24] and even 33–37 years men[31] were included.
Table 2a.
Primary outcomes from the articles
| Outcome | Comparison | Number of subjects (no. of primary studies) | Measure of effect (95% Confidence interval) | Direction of effect |
|---|---|---|---|---|
|
| ||||
| Physical activity and myopia | ||||
| Estimation of risk | Daily PA | 17352 (7) | OR=0.88-0.90 | Protective against myopia |
| PA >3 h/week | 661 (1) | OR=0.46 (0.23-0.90) | Protective against myopia | |
| Per hour sedentary time | 9109 (1) | HR=1.17 (1.10-1.24) | Increased risk of myopia | |
| Changes in Refractive error | NA | NA | NA | NA |
| Change in axial length | NA | NA | NA | NA |
| Proportion (%) developing myopia | Reduced hours of PA per week (51 vs. 60 min/day) | 151 (1) | 5.7% | Increased risk of myopia |
| Proportion (%) with progressive myopia | NA | NA | NA | No effect |
| Time spent in PA | Myopic vs. nonmyopic children | 1713 (3) | 43-112 vs. 51-242 min/day | Protective against myopia |
|
| ||||
| Time spent outdoors and myopia | ||||
|
| ||||
| Estimation of risk | Every additional hour | 39472 (24) | OR=0.928 (0.979-0.985) | Protective against myopia |
| Changes in Refractive error | Dose-response relationship | 6821 (9) | MD = -0.30 D to +0.013 D | No effect |
| Change in axial length | NA | NA | NA | NA |
| Proportion (%) developing myopia | Increasing TSO by 60-76 min/day | 8437 (5) | Incident myopia reduced by 45% to 50% | Protective against myopia |
| Proportion (%) with progressive myopia | NA | NA | NA | NA |
| Time spent outdoors (hours) | Myopic vs. nonmyopic children | 5962 (6) | 3.05-7.98 vs. 5.7-13.75 h/week | Protective against myopia |
OR: odds ratio, RR: relative risk, HR: hazard ratio, MD: mean deviation, PA: physical activity, NW: near work, TSO: time spent outdoors, NA: not available
Table 2b.
Primary outcomes from the articles
| Outcome | Comparison | Number of subjects (no. of primary studies) | Measure of effect (95% confidence interval) | Direction of effect |
|---|---|---|---|---|
| Near work | ||||
| Estimation of risk | More vs. less near work | 6921 (6) | OR=1.85 (1.31-2.62) | Increased risk of myopia |
| Every 1 diopter-hour more of NW per week | 3463 (5) | OR=1.02 (1.01-1.03) | Increased risk of myopia | |
| Incidence of myopia with increasing diopter-hours spent in NW | 10617 (3) | RR=1.00 (0.99-1.01) | No effect | |
| More than 3 h/day reading | 9109 (1) | HR=1.22 (0.96-1.55) | Increased risk of myopia | |
| Reading more than 2 books/week | 2103 (2) | OR=1.43-3.05 | Increased risk of myopia | |
| Close reading distance (<30 cm) and continuous reading (>30 min) | 2353 (1) | OR=2.5 (1.74-4.0) and 1.5 (1.05-2.10) | Increased risk of myopia | |
| Changes in refractive error | NA | NA | NA | NA |
| Changes in axial length | NA | NA | NA | NA |
| Proportion (%) developing myopia | NA | NA | NA | NA |
| Proportion (%) with progressive myopia | 6 h/day of reading and NW vs. control group | 117 (1) | 48.8% vs. 18.9% | Increased risk of myopia |
| Time spent in near work | ||||
| Reading time | NA Myopic vs. non-myopic children | NA 2919 (4) | MD=0.66 (0.16-1.17) | Increased risk of myopia |
| Watching television | MD = -0.22 (-0.96 to 0.51) | No effect | ||
| Computer or video games | MD=0 (-0.60 to 0.57) | No effect | ||
| Studying | MD = -0.01 (-0.60 to 0.57) | No effect |
OR: odds ratio, RR: relative risk, HR: hazard ratio, MD: mean deviation, PA: physical activity, NW: near work, TSO: time spent outdoors, NA: not available
Physical activity
The physiological pathway behind how PA protects against myopia is not confirmed. Theories have hypothesized that increased blood flow causing choroidal layer expansion might reduce axial length. On the other hand, animal studies proved reduction of eye growth with increased thickness and blood flow.[68,69]
Physical activity measurement method
Most of the studies measured PA using questionnaire and interviews, thus paving recall bias risking both over or underestimation of myopia. Only Jacobsen et al.[24] did retesting of questionnaires to increase the validity. Although accelerometers are more objective than questionnaires but not suitable for all kinds of exercises. Moreover, the results might be influenced by the type of exercise, the intensity and duration. Besides, the placement of accelerometer in wrist vs waist is also important and it is recommended to place it at core of body as back or waist for better results.
Questionnaire approach was subjective in all the studies that relied on answers from the child or parents and even recollected from their childhood. Jacobsen et al.[24] used a closed-ended questionnaire (yes/no) to reduce the bias and error. This helped to reduce the misinterpretation, recall bias, and interview bias. The repeated test results of the questionnaires had high correlations coefficient (0.97) in a subgroup of participants. Some studies used a comprehensive questionnaire to determine time spent indoors and outdoors accurately.[28,30,70]
Both outdoor leisure time and outdoor sports showed a protective effect over indoor sports, thus, suggesting the associated element to be TSO rather than sports. Also, the wording “Sports” might have led to misinterpretation by the participants who categorized only exercise and games as sports and not cycling, walking and falsely categorized them in leisure time. Many studies failed to distinguish between TSO and PA, also to quantify different degrees of PA. Some studies lack record on PA whether performed indoor or outdoor.[24,25]
Refractive and visual acuity measurements
The visual measurement methods and cycloplegia usage varied across the studies with some using cycloplegia, whereas others were not using it. However, cycloplegic refraction is important while studying young subjects considering their ability for accommodation.[71] Use of a retinoscope or an autorefractometer to assess the refractive status[72,73] using different kinds of visual acuity charts (Snellen, logMAR, etc.) affects the outcome.[74] Another important factor is the variation in the myopia definition as some studies defined myopia as -1.0 DS, which underestimates myopia, as most studies use -0.50 DS definition of myopia. Hence, prevalence of myopia across studies should be carefully compared.
Study design
In the prospective cohort studies, there were many missing data (14%) and dropouts (8.3%).[2] In studies with large number of children, the number of children tested in each visit varied. This may somewhat limit the representation of general population.
In cross-sectional studies, study participants were from respective local areas and mostly from schools representing the general population. Some studies were small;[26] rest were large with sample size ranging from 366 to 4088,[25,27,28,29,30] which might overestimate the intervention effects. Perhaps it might not be the lesser PA resulting in myopia. The inability to distinguish between exposure and outcome is a limitation of cross-sectional study. A child’s refraction and need for spectacle might have denied sports engagement in myopic children.
Among risk factors, other than PA, studies also assessed potential risk factors like amount of NW (computer usage, writing, watching television, and reading), refractive status of the parents, and cognitive skills with factors confounding like higher likelihood of reading among myopes, urban lifestyle, and better cognitive test results were taken care of.[24,25,27] However, including participants of different age has complicated our understanding as age, and high level of education are confounders of myopia. It was demonstrated that the TSO is the most important protective factor. Since, mostly PA is likely to occur outdoors, there is a possibility of confounding.
In the only case-control study included to study PA and myopia, the sample size was low (n = 65), with more men than women. Different tables in the study presented discrepancies throughout the study, suggesting that several subjects left the questionnaire unfinished. However, it is the only study in the presence of exposures (e.g., PA) that considered possible confounders while comparing the risk of myopia.[31]
Time spent outdoors
The Sydney Myopia Study by Rose et al.[30,75] was the earliest study to propose the protective effect of outdoor activity on developing myopia against PA and time spent on indoor activity.[30,75] This protective effect of TSO on myopia have been confirmed recently in two large randomized controlled trials (RCT).[32,51] Additionally, three studies supported TSO over PA’s effect on myopia.[11,28,75]
The studies on degree of myopia and axial length and PA were not conflicting; instead, PA was more active outdoors than indoors. However, PA could be an important and independent element with different theoretical pathogenic pathways. Most of the questionnaire-based studies reported that PA has a protective association on development and progression of myopia and vice versa.[25,27,28,29,30] Studies evaluating PA using accelerometers found that myopia in correlation with other factors might be linked to PA.[11,26]
The protective effect of TSO on myopia may be due to several mechanisms working individually or in conjunction, starting from release of retinal dopamine due to sunlight, ultraviolet radiation, increased depth of focus, decreased image blur, low accommodative demand, and also the resultant reduced NW (substitution effect).[30,38,76,77,78,79,80]
Studies demonstrated TSO to have a protective effect on the onset of myopia but not on myopia progression. Similarly, the dose–response curve indicates that, although exposure to outdoors may decrease the chances of developing myopia, it was not protective in myopia progression in prediagnosed myopes.[9,35]
Dose–response analysis results in a linear curve indicating a linear relationship between TSO and the risk of myopia onset. However, it should be noted that the studies included for this analysis had an increase in TSO ranging from 1 to 9.8 h/week[36,37,49] and does not determine the effect of TSO more than this upper limit used. Hence, we need to determine the effect of TSO beyond 9.8 h/week on myopia. Likewise, the threshold TSO to prevent the onset of myopia is unknown.[50,62]
Cross-sectional studies had high heterogeneity, but sensitivity analysis reduced the heterogeneity. Participants in the control group playing together with the children from intervention group might have potential contamination. Also, removing studies using noncycloplegic refraction reduced heterogeneity as the results were an overestimated myopia prevalence due to classifying children with emmetropia inappropriately and low hyperopia as myopia.[47,71,81,82] However, cross-sectional studies have a fundamental limitation of inability to distinguish between exposure and outcome and nonexclusion of reverse causality.
TSO is more effective on younger children (6 years) than older children (11–12 years) because ocular growth patterns are more sensitive and mature more in younger children.[35] Analysis of the studies shows that TSO has a greater protective effect on nonmyopic eyes in preventing the onset than on already myopic eyes in progression. However, only one study which demonstrated a significant protective effect of TSO and myopia progression was designed to instruct the children to perform less NW and more outdoor activities, thus signifying the effect as combination of both. Summarizing, these findings suggest that the effect of increased TSO is limited to prevent myopia onset and progression among nonmyopic children.
Similar to any questionnaire-based data, the reported TSO have source of bias, inaccurate reporting, and recall bias. Thus, questionnaires require validation against TSO’s objective measures as light meters, Actigraph, GPS-based systems, and biomarkers such as vitamin D and conjunctival ultraviolet autofluorescence.[2,35]
Despite the high heterogeneity among the studies due to differences in study design, ethnicity, and age of the participants, there is an established protective effect of TSO in most studies. Conversion of TSO from per day to per week in hours may be erroneous as only a few studies provide the actual difference between weekdays and weekends.[11,28,38,42]
Near work
The strength of evidence (rating) for clinical recommendation regarding decreased NW based on the available evidences are category II, level B.[20] This indicates that there is adequate literature to support the recommendation on reducing the risk of children developing myopia with decreased time spent reading though there is a lack qualities for solid support. The quality of evidence it lacks is that most were observational studies with only one RCT.[20]
SRs and MA have estimated 2% increased risk of myopia among children involved per additional diopter-hour of NW per week. They appropriately used 6–18 years age group children among whom the development and progression of myopia are the highest.[20]
The primary studies of the included review studied myopia development and progression of population from various ethnicity. These studies found eastern countries to have more myopic population compared with western countries.[2,9,20,35] However, we should also remember that academic pressure, peer pressure, and educational system are different among the eastern (Asian) and western countries. Eastern parents pay more attention to academic, NW, and TSO, whereas in the western side, parents pay more attention to PA and TSO. This might result in high prevalence of myopia in Asia and less in western countries. Moreover, after school tutorials popular in Asian countries might increase the NW and associated with a high prevalence of myopia.[83]
Calculating with a factual example, if a child spends four hours a day for NW (at 33 cm) after school hours, he or she is likely to have myopia by 120%. On one hand, the MA indicated an 80% higher risk of myopia in children performing NW. On the other hand, the behavioral pattern indicated myopic children reading more than nonmyopic children with similar levels of computer, watching television, and other NW. This might be possibly explaining that reading alone is providing the effect of NW on myopia.[20] It should be borne in mind that although activities such as NW and reading show an association with myopia, they are not necessarily causal in nature. A reverse causality or the effect of myopia might actually force children to do more NW and less outdoor activity. This might be a confounder in the studies associating NW with myopia.
The number of prospective studies and RCT on myopia incidence and progression are minimal. In addition to this, other factors which might be giving such inconsistent conclusions are different study designs: ethnicity studied, myopia and NW definition, inaccuracy, and bias in self- or parent-reported questionnaire, to name a few. Importantly, the effect of lighting on myopia, text size used to read, break in reading, and cumulative effect over time were not considered, affecting the results.[20] Further prospective evidence in preventing myopia is a mandate to elucidate the balance and relationship of NW with outdoor activities.
To our knowledge, this is the first overview of SR and MA on the effect of TSO, PA, and NW on the prevalence, incidence, and progression of myopia. We were able to identify and synthesize the evidence available so far, estimated the overlap of index publications in the included reviews. However, there are certain limitations to this overview. First of all, the high heterogeneity among the primary studies in the overview restricted our MA only to TSO and myopia. Likewise, the topic of NW activity and PA concerning myopia is relatively new. There is a lack of MA on those topics, which further reduced our ability to analyze further data. Including the limited number SR/MA on PA has a high risk of bias. Other limitations are the difference in study designs: ethnicity studied, small sample size, subjectivity and effect of recall bias in questionnaires, lack of adjustment for confounding factors, and lack of information on participants who were lost of follow-up, which we have discussed before in the relevant sections. However, despite the limitations, we can find an association between the TSO, NW, and myopia.
Future studies will need objective measurement with wrist-worn accelerometers to get more accurate estimation of the PA. An enhanced version of the existing questionnaire is needed to eliminate recall bias about PA. The questionnaires need to be accurate in differentiating and quantifying the time spent on various indoor and outdoor settings. Additionally, participants’ fitness tests (physical status) should be used as a further confirmation (indirect measure).
RCT with longitudinal follow-up of refractive error/axial length progression on children with varying degrees of PA would give the highest level of evidence. Such studies concentrating on childhood would be more practical considering the crucial period for ocular development.[1] However, this would be a huge and difficult task to perform considering recruitment, ethical considerations, and compliance. As mentioned, a clear distinction between PA and outdoor activity is a mandate without overlap in future studies.
Conclusion
From the overview, we can conclude that there is evidence suggesting that an increase in the TSO and decrease in NW has a protective effect in reducing myopia among nonmyopes. Although several activities like NW show an association with myopia, they are not necessarily causal. PA is not an independent factor affecting myopia. However, none of the factors had any effect on reducing the progression of myopia in existing myopes. Nevertheless, a distinct difference between the outdoor activity and PA is needed to study their individual effect on myopia accurately. RCT looking at incidence of myopia and myopic progression as primary endpoints is required to study further the dose–duration response of TSO, PA, and NW.
The COVID-19 pandemic has increased the risk of myopia onset and progression with increased NW and digital screen time and reduced the TSO drastically, thus multiplying the risk several times with the continuation of home confinement, especially for children at large. Recommendations for digital screen time are needed to reduce further myopia development and progression.[21] Methodologically, rigorous clinical research is critical to draw a clearer picture and achieve the required consensus. We recommend more RCT with large sample sizes and long-term follow-up to investigate the physical relationship between myopia and its risk factors.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
We would like to thank Ms. Vidyut Rajhans, PhD Student, Manipal College of Health Professions, Manipal Academy of Higher Education, Manipal, for helping us in preparation of protocol and data extraction sheet. Mr. Nagarajan T, Assistant Professor, Manipal College of Health Professions, Manipal Academy of Higher Education, Manipal and Mrs Radhika Poojary, Assistant Professor, Manipal College of Health Professions, Manipal Academy of Higher Education, Manipal for helping during protocol preparation.
Appendix
Table A1.
MEDLINE search strategy (searched on January 31, 2019)
| Search no | Query | Results |
|---|---|---|
| #S1 | Search ((((((((((((((((((Myopia[Title/Abstract]) OR Myopia[Text Word]) OR myopia[MeSH Terms])) OR ((myopic[Title/Abstract]) OR myopic[Text Word])) OR ((nearsightedness[Title/Abstract]) OR nearsightedness[Text Word])) OR ((myopi*[Title/Abstract]) OR myopi*[Text Word])) OR ((short-sighted[Title/Abstract]) OR short-sighted[Text Word])) OR ((short-sightedness[Title/Abstract]) OR short-sightedness[Text Word])) OR ((shortsight[Title/Abstract]) OR shortsight[Text Word])) OR ((short sighted[Title/Abstract]) OR short sighted[Text Word])) OR ((short sightedness[Title/Abstract]) OR short sightedness[Text Word])) OR ((near-sight[Title/Abstract]) OR near-sight[Text Word])) OR ((near-sighted[Title/Abstract]) OR near-sighted[Text Word])) OR ((near-sightedness[Title/Abstract]) OR near-sightedness[Text Word])) OR ((near sighted[Title/Abstract]) OR near sighted[Text Word])) OR ((near sightedness[Title/Abstract]) OR near sightedness[Text Word])) OR (((refractive errors[Title/Abstract]) OR refractive errors[Text Word]) OR refractive errors[MeSH Terms])) OR ((refract*[Title/Abstract]) OR refract*[Text Word]) | 199065 |
| #S2 | Search ((((((((((((((((((((((((((exercise[Title/Abstract]) OR exercise[Text Word]) OR exercise[MeSH Terms])) OR (((physical activity[Title/Abstract]) OR physical activity[Text Word]) OR physical activity[MeSH Terms])) OR (((physical activities[Title/Abstract]) OR physical activities[Text Word]) OR physical activities[MeSH Terms])) OR (((motor activity[Title/Abstract]) OR motor activity[Text Word]) OR motor activity[MeSH Terms])) OR (((exercises[Title/Abstract]) OR exercises[Text Word]) OR exercises[MeSH Terms])) OR (((motor activities[Title/Abstract]) OR motor activities[Text Word]) OR motor activities[MeSH Terms])) OR ((outdoor*[Title/Abstract]) OR outdoor*[Text Word])) OR ((outside[Title/Abstract]) OR outside[Text Word])) OR ((Leisure Activities[Title/Abstract]) OR Leisure Activities[Text Word])) OR ((sport*[Title/Abstract]) OR sport*[Text Word])) OR ((hobb*[Title/Abstract]) OR hobb*[Text Word])) OR ((Environment[Title/Abstract]) OR Environment[Text Word])) OR ((Time spent outdoor[Title/Abstract]) OR Time spent outdoor[Text Word])) OR ((Near activity[Title/Abstract]) OR Near activity[Text Word])) OR ((near work[Title/Abstract]) OR near work[Text Word])) OR ((studying[Title/Abstract]) OR studying[Text Word])) OR (((reading[Title/Abstract]) OR reading[Text Word]) OR reading[MeSH Terms])) OR ((reading distance[Title/Abstract]) OR reading distance[Text Word])) OR ((working distance[Title/Abstract]) OR working distance[Text Word])) OR ((Outdoor activity[Title/Abstract]) OR Outdoor activity[Text Word])) OR ((Indoor activity[Title/Abstract]) OR Indoor activity[Text Word])) OR ((sunlight exposure[Title/Abstract]) OR sunlight exposure[Text Word])) OR ((Darkness[Title/Abstract]) OR Darkness[Text Word])) OR ((Dark[Title/Abstract]) OR Dark[Text Word]) | 1583807 |
| #S1 AND S2 | Search ((((((((((((((((((((((((((((exercise[Title/Abstract]) OR exercise[Text Word]) OR exercise[MeSH Terms])) OR (((physical activity[Title/Abstract]) OR physical activity[Text Word]) OR physical activity[MeSH Terms])) OR (((physical activities[Title/Abstract]) OR physical activities[Text Word]) OR physical activities[MeSH Terms])) OR (((motor activity[Title/Abstract]) OR motor activity[Text Word]) OR motor activity[MeSH Terms])) OR (((exercises[Title/Abstract]) OR exercises[Text Word]) OR exercises[MeSH Terms])) OR (((motor activities[Title/Abstract]) OR motor activities[Text Word]) OR motor activities[MeSH Terms])) OR ((outdoor*[Title/Abstract]) OR outdoor*[Text Word])) OR ((outside[Title/Abstract]) OR outside[Text Word])) OR ((Leisure Activities[Title/Abstract]) OR Leisure Activities[Text Word])) OR ((sport*[Title/Abstract]) OR sport*[Text Word])) OR ((hobb*[Title/Abstract]) OR hobb*[Text Word])) OR ((Environment[Title/Abstract]) OR Environment[Text Word])) OR ((Time spent outdoor[Title/Abstract]) OR Time spent outdoor[Text Word])) OR ((Near activity[Title/Abstract]) OR Near activity[Text Word])) OR ((near work[Title/Abstract]) OR near work[Text Word])) OR ((studying[Title/Abstract]) OR studying[Text Word])) OR (((reading[Title/Abstract]) OR reading[Text Word]) OR reading[MeSH Terms])) OR ((reading distance[Title/Abstract]) OR reading distance[Text Word])) OR ((working distance[Title/Abstract]) OR working distance[Text Word])) OR ((Outdoor activity[Title/Abstract]) OR Outdoor activity[Text Word])) OR ((Indoor activity[Title/Abstract]) OR Indoor activity[Text Word])) OR ((sunlight exposure[Title/Abstract]) OR sunlight exposure[Text Word])) OR ((Darkness[Title/Abstract]) OR Darkness[Text Word])) OR ((Dark[Title/Abstract]) OR Dark[Text Word]))) AND (((((((((((((((((((Myopia[Title/Abstract]) OR Myopia[Text Word]) OR myopia[MeSH Terms])) OR ((myopic[Title/Abstract]) OR myopic[Text Word])) OR ((nearsightedness[Title/Abstract]) OR nearsightedness[Text Word])) OR ((myopi*[Title/Abstract]) OR myopi*[Text Word])) OR ((short-sighted[Title/Abstract]) OR short-sighted[Text Word])) OR ((short-sightedness[Title/Abstract]) OR short-sightedness[Text Word])) OR ((shortsight[Title/Abstract]) OR shortsight[Text Word])) OR ((short sighted[Title/Abstract]) OR short sighted[Text Word])) OR ((short sightedness[Title/Abstract]) OR short sightedness[Text Word])) OR ((near-sight[Title/Abstract]) OR near-sight[Text Word])) OR ((near-sighted[Title/Abstract]) OR near-sighted[Text Word])) OR ((near-sightedness[Title/Abstract]) OR near-sightedness[Text Word])) OR ((near sighted[Title/Abstract]) OR near sighted[Text Word])) OR ((near sightedness[Title/Abstract]) OR near sightedness[Text Word])) OR (((refractive errors[Title/Abstract]) OR refractive errors[Text Word]) OR refractive errors[MeSH Terms])) OR ((refract*[Title/Abstract]) OR refract*[Text Word])) AND (Review[ptyp]) | 1249 |
Table A2.
Primary studies contained within systematic reviews
| Sn | Primary Study |
|---|---|
| 1 | O’Donoghue L, Kapetanankis VV, McClelland JF, et al. Risk factors for childhood myopia: findings from the NICER study. Invest Ophthalmol Vis Sci 2015;56: 1524-1530. |
| 2 | Guggenheim JA, Northstone K, McMahon G, et al. Time outdoors and physical activity as predictors of incident myopia in childhood: a prospective cohort study. Invest Ophthalmol Vis Sci 2012;53: 2856-2865. |
| 3 | Jacobsen N, Jensen H, Goldschmidt E. Does the level of physical activity in university students influence development and progression of myopia?-a 2-year prospective cohort study. Invest Ophthalmol Vis Sci 2008;49: 1322-1327. |
| 4 | Read SA, Collins MJ, Vincent SJ. Light exposure and physical activity in myopic and emmetropic children. Optom Vis Sci 2014;91: 330-341 |
| 5 | Parssinen O, Leskinen AL, Era P, Heikkinen E. Myopia, use of eyes, and living habits among men aged 33-37 years. Acta Ophthalmol (Copenh) 1985;63: 395-400 |
| 6 | Dirani M, Tong L, Gazzard G, et al.: Outdoor activity and myopia in Singapore teenage children. Br J Ophthalmol 2009;93: 997-1000 |
| 7 | Mutti DO, Mitchell GL, Moeschberger ML, et al. Parental myopia, near work, school achievement, and children’s refractive error. Invest Ophthalmol Vis Sci 2002;43: 3633-3640 |
| 8 | Khader YS, Batayha WQ, Abdul-Aziz SM, Al-Shiekh-Khalil MI. Prevalence and risk indicators of myopia among schoolchildren in Amman, Jordan. East Mediterr Health J 2006;12: 434-439 |
| 9 | Rose K, Smith W, Morgan I, Mitchell P. The increasing prevalence of myopia: implications for Australia. Clin Exp Ophthalmol 2001;29: 116-120 |
| 10 | He M, Xiang F, Zeng Y et al. Effect of time spent outdoors at school on the development of myopia among children in China: a randomized clinical trial. JAMA 2015;314: 1142-1148 |
| 11 | Jin JX, Hua WJ, Jiang X et al. Effect of outdoor activity on myopia onset and progression in school-aged children in northeast China: the Sujiatun Eye Care Study. BMC Ophthalmol 2015; 15: 73 |
| 12 | Wu PC, Tsai CL, Wu HL, et al. Outdoor activity during class recess reduces myopia onset and progression in school children. Ophthalmology 2013;120: 1080-1085 |
| 13 | Yi JH, Li RR. [Influence of near-work and outdoor activities on myopia progression in school children]. Zhongguo Dang Dai Er Ke Za Zhi 2011; 13: 32-35 |
| 14 | French AN, Morgan IG, Mitchell P, Rose KA. Patterns of myopigenic activities with age, gender and ethnicity in Sydney schoolchildren. Ophthamic Physiol Opt 2013; 33: 318-28 |
| 15 | Saw SM, Shankar A, Tan SB, et al. A cohort study of incident myopia in Singaporean children. Invest Ophthalmol Vis Sci 2006;47: 1839-1844 |
| 16 | Chua SY, Ikram MK, Tan CS et al. Relative contribution of risk factors for early-onset myopia in young Asian children. Invest Ophthalmol Vis Sci 2015;56: 8101-8107 |
| 17 | Zhou Z, Morgan IG, Chen Q, et al. Disordered sleep and myopia risk among Chinese children. PLoS ONE 2015;10: e0121796 |
| 18 | Lee YY, Lo CT, Sheu SJ, Yin LT. Risk factors for and progression of myopia in young Taiwanese men. Ophthalmic Epidemiol 2015;22: 66-73 |
| 19 | Pan CW, Chen Q, Sheng X et al. Ethnic variations in myopia and ocular biometry among adults in a rural community in China: the yunnan minority eye studies. Invest Ophthalmol Vis Sci 2015;56: 3235-3241 |
| 20 | Guo K, Yang DY, Wang Y et al. Prevalence of myopia in schoolchildren in Ejina: the Gobi Desert children eye study. Invest Ophthalmol Vis Sci 2015;56: 1769-1774 |
| 21 | Zhou R, Zhang WF, Yang Y, et al. Analysis of myopia prevalence and influencing factors among primary school students in the urban area of Lanzhou city. Int Eye Sci 2014; 14: 903-907 |
| 22 | Guo Y, Liu LJ, Xu L, et al. Outdoor activity and myopia among primary students in rural and urban regions of Beijing. Ophthalmology 2013;120: 277-283 |
| 23 | Low W, Dirani M, Gazzard G et al. Family history, near work, outdoor activity, and myopia in Singapore Chinese preschool children. Br J Ophthalmol 2010; 94: 1012-1016 |
| 24 | Deng L, Gwiazda J, Thorn F Children’s refractions and visual activities in the school year and summer. Optom Vis Sci 2010; 87: 406-413 |
| 25 | Lu B, Congdon N, Liu X, et al. Associations between near work, outdoor activity, and myopia among adolescent students in rural China: the Xichang Pediatric Refractive Error Study report no. 2. Arch Ophthalmol 2009;127: 769-775. |
| 26 | Ip JM, Saw SM, Rose KA, et al. Role of near work in myopia: findings in a sample of Australian school children. Invest Ophthalmol Vis Sci 2008; 49: 2903-2910 |
| 27 | Oner V, Bulut A, Oruc Y, Ozgur G Influence of indoor and outdoor activities on progression of myopia during puberty. Int Ophthalmol 2015; 36: 121-125 |
| 28 | Li SM, Li H, Li SY, et al. Time outdoors and myopia progression over 2 years in chinese children: the Anyang childhood eye study. Invest Ophthalmol Vis Sci 2015; 56: 4734-4740 |
| 29 | Jones-Jordan LA, Mitchell GL, Cotter SA et al. Visual activity before and after the onset of juvenile myopia. Invest Ophthalmol Vis Sci 2011; 52: 1841-1850 |
| 30 | Jones-Jordan LA, Sinnott LT, Cotter SA, et al. Time outdoors, visual activity, and myopia progression in juvenile-onset myopes. Invest Ophthalmol Vis Sci 2012; 53: 7169-7175 |
| 31 | Saw SM, Nieto FJ, Katz J, et al. Factors related to the progression of myopia in Singaporean children. Optom Vis Sci 2000; 77: 549-554 |
| 32 | Zadnik K, Sinnott LT, Cotter SA et al. Prediction of juvenile-onset myopia. JAMA Ophthalmol 2015; 133: 683-689 |
| 33 | Onal S, Toker E, Akingol Z, et al. Refractive errors of medical students in Turkey: one year follow-up of refraction and biometry. Optom Vis Sci 2007;84: 175-180 |
| 34 | Peckham CS, Gardiner PA, Goldstein H. Acquired myopia in 11-year-old children. Br Med J 1977; 1: 542-545 |
| 35 | Saxena R, Vashist P, Tandon R, et al. Prevalence of myopia and its risk factors in urban school children in Delhi: the North India Myopia Study (NIM Study). PLoS ONE 2015; 10: e0117349 |
| 36 | Ramessur R, Williams KM, Hammond CJ. Risk factors for myopia in a discordant monozygotic twin study. Ophthalmic Physiol Opt 2015;35: 643-651. |
| 37 | Wen XF, Zhang J, Zhao Y. Analysis of poor vision conditions and risk factors of myopia in primary school He’xi district of Sanya. Int Eye Sci 2015; 15: 684-686 |
| 38 | Han X, Miao HL, Huang D. Investigation of junior school student myopia in high-altitude Tibetan areas in Qinghai Province. Int Eye Sci 2014; 14: 913-915. |
| 39 | Lin Z, Vasudevan B, Jhanji V et al. Near work, outdoor activity, and their association with refractive error. Optom Vis Sci 2014; 91: 376-382. |
| 40 | Cheng CY, Huang W, Su KC, et al. Myopization factors affecting urban elementary school students in Taiwan. Optom Vis Sci 2013;90: 400-406 |
| 41 | Xie HL, Xie ZK, Zhou F, Hu L. [Myopia prevalence and influencing factor analysis of primary and middle school students in our country]. Zhonghua yi xue za zhi 2013;93: 999-1002 |
| 42 | Sherwin JC, Hewitt AW, Coroneo MT, et al. The association between time spent outdoors and myopia using a novel biomarker of outdoor light exposure. Invest Ophthalmol Vis Sci 2012;53: 4363-4370 |
| 43 | Wu PC, Tsai CL, Hu CH, Yang YH Effects of outdoor activities on myopia among rural school children in Taiwan. Ophthalmic Epidemiol 2010; 17: 338-342 |
| 44 | Zhang M, Li L, Chen L et al. Population density and refractive error among Chinese children. Invest Ophthalmol Vis Sci 2010; 51: 4969-4976 |
| 45 | Ma MM, Zhang ZW, Song JG, et al. An epidemiological survey of refractive error and associated factors among middle school students in Deqing County of Zhejiang Province, China. Fudan Univ J Med Sci 2010; 37: 680-684 |
| 46 | Rose KA, Morgan IG, Ip J, et al. Outdoor activity reduces the prevalence of myopia in children. Ophthalmology 2008;115: 1279-1285 |
| 47 | Rose KA, Morgan IG, Smith W, et al. Myopia, lifestyle, and schooling in students of Chinese ethnicity in Singapore and Sydney. Arch Ophthalmol 2008;126: 527-530 |
| 48 | Saw SM, Zhang MZ, Hong RZ, et al. Near-work activity, night-lights, and myopia in the Singapore- China study. Arch Ophthalmol 2002;120: 620-627 |
| 49 | Saw SM, Hong RZ, Zhang MZ, et al. Near-work activity and myopia in rural and urban schoolchildren in China. J Pediatr Ophthalmol Strabismus 2001;38: 149-155 |
| 50 | Tan GJ, Ng YP, Lim YC, Ong PY, et al. Cross-sectional study of near-work and myopia in kindergarten children in Singapore. Ann Acad Med Singapore 2000;29: 740-744 |
| 51 | Wu LJ, Wang YX, You QS, et al. Risk factors of myopic shift among primary school children in Beijing, China: a prospective study. Int J Med Sci 2015;12: 633-638 |
| 52 | Scheiman M, Zhang Q, Gwiazda J, et al. Visual activity and its association with myopia stabilisation. Ophthalmic Physiol Opt 2014; 34: 353-361 |
| 53 | Parssinen O, Kauppinen M, Viljanen A. The progression of myopia from itsonset at age 8-12 to adulthood and the influence of heredity and external factors on myopic progression. A 23-year follow-up study. Acta Ophthalmol 2014; 92: 730-739 |
| 54 | Guo Y, Liu LJ, Xu L, et al. Myopic shift and outdoor activity among primary school children: one-year follow-up study in Beijing. PLoS ONE 2013; 8: e75260. |
| 55 | Parssinen O, Lyyra AL. Myopia and myopic progression among schoolchildren: a three-year follow-up study. Invest Ophthalmol Vis Sci 1993; 34: 2794-2802 |
| 56 | Jones LA, Sinnott LT, Mutti DO, et al. Parental history of myopia, sports and outdoor activities, and future myopia. Invest Ophthalmol Vis Sci 2007; 48: 3524-3532 |
| 57 | Saw S-M, Chua W-H, Hong C-Y, et al. Nearwork in Early-Onset Myopia. Invest Ophthalmol Vis Sci 2002;43:332-9. |
| 58 | French AN, Morgan IG, Mitchell P, Rose KA. Risk Factors for Incident Myopia in Australian Schoolchildren: The Sydney Adolescent Vascular and Eye Study. Ophthalmology. 2013; 120:2100-8. |
| 59 | Mavracanas TA, Mandalos A, Peios D, et al. Prevalence of myopia in a sample of Greek students. Acta Ophthalmol Scand 2000; 78:656-9. |
| 60 | Hepsen IF, Evereklioglu C, Bayramlar H. The effect of reading and near-work on the development of myopia in emmetropic boys: a prospective, controlled, three-year follow-up study. Vision Res 2001; 41:2511-20 |
| 61 | Yingyong P. Risk factors for refractive errors in primary school children (6-12 years old) in Nakhon Pathom province. JMed Assoc Thai 2010; 93:1288-93. |
| 62 | Wu P-C, Tsai C-L, Wu H-L, et al. Outdoor Activity during Class Recess Reduces Myopia Onset and Progression in School Children. Ophthalmology 2013;120:1080-5 |
Table A3.
Citation matrix
| Primary Study | Type of Primary study | Anne Suhr Thykjaer, et al., 2016 | Shuyu Xiong, et al., 2017 | Justin C Sherwin, et al., 2012 | Hsiu-MeiHuang, et al., 2015 | Total number of reviews |
|---|---|---|---|---|---|---|
| O’Donoghue L et al., 2015 | Cross-sectional | 1 | 1 | |||
| Guggenheim JA, et al., 2012 | Cohort Prospective | 1 | 1 | 1 | 3 | |
| Jacobsen N, et al., 2008 | Cohort Prospective | 1 | 1 | |||
| Read SA, et al., 2014 | Cross-sectional | 1 | 1 | 2 | ||
| Parssinen O, et al., 1985 | Case control | 1 | 1 | |||
| Dirani M, et al., 2009 | Cross-sectional | 1 | 1 | 1 | 3 | |
| Mutti DO, et al., 2002 | Cross-sectional | 1 | 1 | 1 | 1 | 4 |
| Khader YS, et al., 2006 | Cross-sectional | 1 | 1 | 1 | 3 | |
| Rose K, et al., 2001 | Cross-sectional | 1 | 1 | |||
| He M, et al., 2015 | RCT | 1 | 1 | |||
| Jin JX, et al., 2015 | RCT | 1 | 1 | |||
| Wu PC, et al., 2013 | RCT | 1 | 1 | |||
| Yi JH et al., 2011 | RCT | 1 | 1 | 1 | 3 | |
| French AN, et al., 2013a | Cohort prospective | 1 | 1 | |||
| Saw SM, et al., 2006 | Cohort prospective | 1 | 1 | 1 | 3 | |
| Chua SY, et al., 2015 | Cross sectional | 1 | 1 | |||
| Zhou Z, et al., 2015 | Cross sectional | 1 | 1 | |||
| Lee YY, et al., 2015 | Cross sectional | 1 | 1 | |||
| Pan CW, et al., 2015 | Cross sectional | 1 | 1 | |||
| Guo K, et al., 2015 | Cross sectional | 1 | 1 | |||
| Zhou R, et al., 2014 | Cross sectional | 1 | 1 | |||
| Guo Y, et al., 2013a | Cross sectional | 1 | 1 | 2 | ||
| Low W, et al., 2010 | Cross sectional | 1 | 1 | 2 | ||
| Deng L, et al., 2010 | Cross sectional | 1 | 1 | 1 | 3 | |
| Lu B, et al., 2009 | Cross sectional | 1 | 1 | 1 | 3 | |
| Ip JM, et al., 2008 | Cross sectional | 1 | 1 | 1 | 3 | |
| Oner V, et al., 2015 | Cohort prospective | 1 | 1 | |||
| Li SM, et al., 2015 | Cohort prospective | 1 | 1 | |||
| Jones-Jordan LA, et al., 2011 | Cohort prospective | 1 | 1 | 1 | 3 | |
| Jones-Jordan LA, et al., 2012 | Cohort prospective | 1 | 1 | 2 | ||
| Saw SM, et al., 2000 | Cohort prospective | 1 | 1 | 1 | 3 | |
| Zadnik K, et al., 2015 | Cohort prospective | 1 | 1 | |||
| Onal S, et al., 2007 | Cohort prospective | 1 | 1 | 2 | ||
| Peckham CS, et al., 1977 | Cohort prospective | 1 | 1 | 2 | ||
| Saxena R, et al., 2015 | Cross sectional | 1 | 1 | |||
| Ramessur R, et al., 2015 | Cross sectional | 1 | 1 | |||
| Wen XF et al., 2015 | Cross sectional | 1 | 1 | |||
| Han X, et al., 2014 | Cross sectional | 1 | 1 | |||
| Lin Z, et al., 2014 | Cross sectional | 1 | 1 | 2 | ||
| Cheng CY, et al., 2013 | Cross sectional | 1 | 1 | |||
| Xie HL, et al., 2013 | Cross sectional | 1 | 1 | |||
| Sherwin JC, et al., 2012 | Cross sectional | 1 | 1 | |||
| Wu PC, et al., 2010 | Cross sectional | 1 | 1 | 1 | 3 | |
| Zhang M, et al., 2010 | Cross sectional | 1 | 1 | 2 | ||
| Ma MM, et al., 2010 | Cross sectional | 1 | 1 | 2 | ||
| Rose KA, et al., 2008a | Cross sectional | 1 | 1 | 1 | 3 | |
| Rose KA, et al., 2008b | Cross sectional | 1 | 1 | 1 | 3 | |
| Saw SM, et al., 2002 | Cross sectional | 1 | 1 | 1 | 3 | |
| Saw SM, et al., 2001 | Cross sectional | 1 | 1 | 1 | 3 | |
| Tan GJ, et al., 2000 | Cross sectional | 1 | 1 | 2 | ||
| Wu LJ, et al., 2015 | Cohort prospective | 1 | 1 | |||
| Scheiman M, et al., 2014 | Cohort prospective | 1 | 1 | 2 | ||
| Parssinen O, et al., 2014 | Cohort prospective | 1 | 1 | |||
| Guo Y, et al., 2013b. | Cohort prospective | 1 | 1 | |||
| Parssinen O et al., 1993 | Cohort prospective | 1 | 1 | 1 | 3 | |
| Jones LA, et al., 2007 | Cohort prospective | 1 | 1 | 1 | 3 | |
| Saw S-M, et al., 2002 | Cross sectional | 1 | 1 | |||
| French AN, et al., 2013b | Cohort prospective | 1 | 1 | 2 | ||
| Mavracanas TA, et al., 2000 | Cross sectional | 1 | 1 | |||
| Hepsen IF, et al., 2001 | Longitudinal | 1 | 1 | |||
| Yingyong P. 2010 | Cross sectional | 1 | 1 | |||
| Wu P-C, et al., 2013 | Cohort prospective | 1 | 1 |
Corrected covered area (CCA)= 26.34%
Table A4.
Methodological quality of included systematic reviews and meta-analyses based on ROBIS tool
| Review and Year | ROBIS Assessment | ||||
|---|---|---|---|---|---|
|
| |||||
| Domain 1: Study eligibility criteria | Domain 2: Identification and selection of studies | Domain 3: Data collection and study appraisal | Domain 4: Synthesis and findings | Risk of bias | |
| Anne Suhr Thykjaer, et al., 2016 | LOW | LOW | UNCLEAR | HIGH | HIGH |
| Shuyu Xiong, et al., 2017 | LOW | LOW | LOW | LOW | LOW |
| Justin C Sherwin, et al., 2012 | LOW | LOW | LOW | LOW | LOW |
| Hsiu-MeiHuang, et al., 2015 | LOW | LOW | LOW | LOW | LOW |
Table A5.
Excluded studies after full text review
| Selected for review | Reason for exclusion |
|---|---|
| Wilson, A., & Woo, G. (1989). A review of the prevalence and causes of myopia. Singapore medical journal, 30 (5), 479-484. | Nonsystematic review |
| Rudnicka, A. R., Kapetanakis, V. V., Wathern, A. K., Logan, N. S., Gilmartin, B., Whincup, P. H., . & Owen, C. G. (2016). Global variations and time trends in the prevalence of childhood myopia, a systematic review and quantitative meta-analysis: implications for aetiology and early prevention. British Journal of Ophthalmology, 100 (7), 882-890. | Topic not directly relevant |
| Walline, J. J., Lindsley, K. B., Vedula, S. S., Cotter, S. A., Mutti, D. O., Ng, S. M., & Twelker, J. D. (2020). Interventions to slow progression of myopia in children. Cochrane Database of Systematic Reviews, (1). | Topic not directly relevant |
| Hobday, R. (2016). Myopia and daylight in schools: a neglected aspect of public health?. Perspectives in public health, 136 (1), 50-55. | Nonsystematic review |
| Walline, J. J. (2016). Myopia control: a review. Eye & contact lens, 42 (1), 3-8. | Nonsystematic review |
| Saw, S. M., Chua, W. H., Wu, H. M., Yap, E., Chia, K. S., & Stone, R. A. (2000). Myopia: gene-environment interaction. Annals of the Academy of Medicine, Singapore, 29 (3), 290. | Nonsystematic review |
| Lagrèze, W. A., & Schaeffel, F. (2017). Preventing myopia. Deutsches Ärzteblatt International, 114 (35-36), 575. | Nonsystematic review |
| Wang, J., He, X. G., & Xu, X. (2018). The measurement of time spent outdoors in child myopia research: a systematic review. International journal of ophthalmology, 11 (6), 1045. | Topic not directly relevant |
Appendix Table 6.
Details of the studies included in the review
| Author, year of publication | Aim of study | Type of included study | Databases searched | last date of literature search | Type of intervention | Outcomes measured |
|---|---|---|---|---|---|---|
| Anne Suhr Thykjær et al., 2016 | To perform a systematic literature review, to examine the association between PA, and the development and progression of myopia | 6 cross-sectional, 2 cohorts and 1 case-control study | PubMed/Medline and Embase, manual reference, and author search | 2015 | Physical activity- indoor, outdoor (time spent outdoor) | Physical activity - Accelerometer (CPM), Cycle ergometer test, refractive error (D), questionnaire |
| Hsiu-MeiHuang et al., 2015 | To quantify the effect of near work activities on myopia in children | 15 Cross sectional, 6 cohort, 6 longitudinal | MEDLINE, Embase, the Cochrane Library, and the citation lists were reviewed | 2014 | Nearwork was defined as the sum of activities with short working distance such as reading, studying, writing, doing homework, watching TV, or playing video games, etc. | Near work activities, myopia incidence or progression |
| Justin C. Sherwin et al., 2012 | To summarize relevant evidence investigating the association between times spent outdoors and myopia in children and adolescents (up to 20 years). | 7 cross-sectional studies for meta-analysis. A further 16 studies (8 cross-sectional not meeting criteria for meta-analysis; 7 prospective cohort studies; 1 RCT) | Medline, Embase, Web of Science, and Cochrane Central Register of Controlled Trials [CENTRAL] and reference lists | 2011 | Time spent outdoors, confounding factors and latitude of the study location | Time spent outdoors, definition of myopia, confounding factors were adjusted for and latitude of the study location |
| Shuyu Xiong, et al., 2017 | To evaluate the evidence for association between time outdoors and (1) risk of onset of myopia (incident/prevalent myopia); (2) risk of a myopic shift in refractive error and (3) risk of progression in myopes only. | 4 Clinical trials, 18 cohort studies and 30 cross-sectional studies | PubMed, EMBASE, and the Cochrane Library | 2015 | Outdoor time spent | (1) Risk of incident/prevalent myopia from pooled estimates and dose-response analysis; (2) Risk of a myopic shift in refractive error (both myopes and nonmyopes) from pooled estimates; and (3) Risk of progression of myopia (in myopic eyes) from dose- response analysis |
References
- 1. Morgan IG, Ohno-Matsui K, Saw SM. Myopia. Lancet. 2012;379:1739–48. doi: 10.1016/S0140-6736(12)60272-4. [DOI] [PubMed] [Google Scholar]
- 2. Suhr Thykjaer A, Lundberg K, Grauslund J. Physical activity in relation to development and progression of myopia-A systematic review. Acta Ophthalmol. 2017;95:651–9. doi: 10.1111/aos.13316. [DOI] [PubMed] [Google Scholar]
- 3. Lin LLK, Shih YF, Hsiao CK, Chen CJ. Prevalence of myopia in taiwanese schoolchildren:1983 to 2000. Ann Acad Med Singapore. 2004;33:27–33. [PubMed] [Google Scholar]
- 4. Jung SK, Lee JH, Kakizaki H, Jee D. Prevalence of myopia and its association with body stature and educational level in 19-year-old male conscripts in Seoul, South Korea. Investig Ophthalmol Vis Sci. 2012;53:5579–83. doi: 10.1167/iovs.12-10106. [DOI] [PubMed] [Google Scholar]
- 5. Morgan I, Rose K. How genetic is school myopia? Prog Retin Eye Res. 2005;24:1–38. doi: 10.1016/j.preteyeres.2004.06.004. [DOI] [PubMed] [Google Scholar]
- 6. Rose K, Smith W, Morgan I, Mitchell P. The increasing prevalence of myopia:Implications for Australia. Clin Exp Ophthalmol. 2001;29:116–20. doi: 10.1046/j.1442-9071.2001.00389.x. [DOI] [PubMed] [Google Scholar]
- 7. Vitale S, Sperduto RD, Ferris FL. Increased prevalence of myopia in the United States between 1971-1972 and 1999-2004. Arch Ophthalmol. 2009;127:1632–9. doi: 10.1001/archophthalmol.2009.303. [DOI] [PubMed] [Google Scholar]
- 8. Ward DS, Evenson KR, Vaughn A, Rodgers AB, Troiano RP. Accelerometer use in physical activity:Best practices and research recommendations. Med Sci Sports Exerc. 2005;37((Suppl 11)):S582–8. doi: 10.1249/01.mss.0000185292.71933.91. [DOI] [PubMed] [Google Scholar]
- 9. Sherwin JC, Reacher MH, Keogh RH, Khawaja AP, MacKey DA, Foster PJ. The association between time spent outdoors and myopia in children and adolescents:A systematic review and meta-analysis. Ophthalmology. 2012;119:2141–51. doi: 10.1016/j.ophtha.2012.04.020. [DOI] [PubMed] [Google Scholar]
- 10. Prousali E, Mataftsi A, Ziakas N, Fontalis A, Brazitikos P, Haidich AB. Interventions to control myopia progression in children:Protocol for an overview of systematic reviews and meta- analyses. BMC Syst Rev. 2017;6:188. doi: 10.1186/s13643-017-0580-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Guggenheim JA, Northstone K, McMahon G, Ness AR, Deere K, Mattocks C, et al. Time outdoors and physical activity as predictors of incident myopia in childhood:A prospective cohort study. Investig Ophthalmol Vis Sci. 2012;53:2856–65. doi: 10.1167/iovs.11-9091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Loman J, Quinn GE, Kamoun L, Ying G-S, Maguire MG, Hudesman D, et al. Darkness and near work. Ophthalmology. 2002;109:1032–8. doi: 10.1016/s0161-6420(02)01012-6. [DOI] [PubMed] [Google Scholar]
- 13. Quinn GE, Shin CH, Maguire MG, Stone RA. Myopia and ambient lighting at night. Nature. 1999;399:113–4. doi: 10.1038/20094. [DOI] [PubMed] [Google Scholar]
- 14. Fulk GW, Cyert LA, Parker DE. A randomized trial of the effect of single-vision vs. bifocal lenses on myopia progression in children with esophoria. Optom Vis Sci. 2000;77:395–401. doi: 10.1097/00006324-200008000-00006. [DOI] [PubMed] [Google Scholar]
- 15. Gwiazda JE. Progressive-addition lenses versus single-vision lenses for slowing progression of myopia in children with high accommodative lag and near esophoria. Investig Ophthalmol Vis Sci. 2011;52:2749–57. doi: 10.1167/iovs.10-6631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Phillips JR. Monovision slows juvenile myopia progression unilaterally. Br J Ophthalmol. 2005;89:1196–200. doi: 10.1136/bjo.2004.064212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Vannas AE, Ying GS, Stone RA, Maguire MG, Jormanainem V, Tervo T. Myopia and natural lighting extremes:Risk factors in Finnish army conscripts. Acta Ophthalmol Scand. 2003;81:588–95. doi: 10.1046/j.1395-3907.2003.0151.x. [DOI] [PubMed] [Google Scholar]
- 18. Czepita D, Gosławski W, Mojsa A, Muszyńska-Lachota I. Role of light emitted by incandescent or fluorescent lamps in the development of myopia and astigmatism. Med Sci Monit. 2004;10:CR168–71. [PubMed] [Google Scholar]
- 19. Gwiazda J, Hyman L, Hussein M, Everett D, Norton TT, Kurtz D, et al. A randomized clinical trial of progressive addition lenses versus single vision lenses on the progression of myopia in children. Investig Ophthalmol Vis Sci. 2003;44:1492–500. doi: 10.1167/iovs.02-0816. [DOI] [PubMed] [Google Scholar]
- 20. Huang HM, Chang DST, Wu PC. The association between near work activities and myopia in children-A systematic review and meta-analysis. PLoS One. 2015;10:e0140419. doi: 10.1371/journal.pone.0140419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Nagata JM, Abdel Magid HS, Pettee Gabriel K. Screen time for children and adolescents during the COVID-19 pandemic. Obesity (Silver Spring) 2020;28:1582–3. doi: 10.1002/oby.22917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Moher D, Liberati A, Tetzlaff J, Altman DG, Altman DG, PRISMA Group Preferred reporting items for systematic reviews and meta-analyses:The PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Whiting P, Savović J, Higgins JP, Caldwell DM, Reeves BC, Shea B, et al. ROBIS:a new tool to assess risk of bias in systematic reviews was developed. Journal of clinical epidemiology. 2016;69:225–34. doi: 10.1016/j.jclinepi.2015.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Jacobsen N, Jensen H, Goldschmidt E. Does the level of physical activity in university students influence development and progression of myopia?--A 2-year prospective cohort study. Invest Ophthalmol Vis Sci. 2008;49:1322–7. doi: 10.1167/iovs.07-1144. [DOI] [PubMed] [Google Scholar]
- 25. O'Donoghue L, Kapetanankis VV, McClelland JF, Logan NS, Owen CG, Saunders KJ, et al. Risk factors for childhood myopia:Findings from the NICER study. Invest Ophthalmol Vis Sci. 2015;56:1524–30. doi: 10.1167/iovs.14-15549. [DOI] [PubMed] [Google Scholar]
- 26. Read SA, Collins MJ, Vincent SJ. Light exposure and physical activity in myopic and emmetropic children. Optom Vis Sci. 2014;91:330–41. doi: 10.1097/OPX.0000000000000160. [DOI] [PubMed] [Google Scholar]
- 27. Khader YS, Batayha WQ, Abdul-Aziz SM, Al-Shiekh-Khalil MI. Prevalence and risk indicators of myopia among schoolchildren in Amman, Jordan. East Mediterr Health J. 2006;12:434–9. [PubMed] [Google Scholar]
- 28. Dirani M, Tong L, Gazzard G, Zhang X, Chia A, Young TL, et al. Outdoor activity and myopia in Singapore teenage children. Br J Ophthalmol. 2009;93:997–1000. doi: 10.1136/bjo.2008.150979. [DOI] [PubMed] [Google Scholar]
- 29. Mutti DO, Mitchell GL, Moeschberger ML, Jones LA, Zadnik K. Parental myopia, near work, school achievement, and children's refractive error. Invest Ophthalmol Vis Sci. 2002;43:3633–40. [PubMed] [Google Scholar]
- 30. Rose KA, Morgan IG, Ip J, Kifley A, Huynh S, Smith W, et al. Outdoor activity reduces the prevalence of myopia in children. Ophthalmology. 2008;115:1279–85. doi: 10.1016/j.ophtha.2007.12.019. [DOI] [PubMed] [Google Scholar]
- 31. Pärssinen O, Leskinen A-L, Era P, Heikkinen E. Myopia, use of eyes, and living habits among men aged 33–37 years. Acta Ophthalmol. 1985;63:395–400. doi: 10.1111/j.1755-3768.1985.tb01551.x. [DOI] [PubMed] [Google Scholar]
- 32. He M, Xiang F, Zeng Y, Mai J, Chen Q, Zhang J, et al. Effect of time spent outdoors at school on the development of myopia among children in China:A randomized clinical trial. JAMA Ophthalmol. 2015;314:1142–8. doi: 10.1001/jama.2015.10803. [DOI] [PubMed] [Google Scholar]
- 33. Jin J-X, Hua W-J, Jiang X, Wu X-Y, Yang J-W, Gao G-P, et al. Effect of outdoor activity on myopia onset and progression in school-aged children in northeast China:The Sujiatun eye care study. BMC Ophthalmol. 2015;15:73. doi: 10.1186/s12886-015-0052-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Wu L-J, Wang Y-X, You Q-S, Duan J-L, Luo Y-X, Liu L-J, et al. Risk factors of myopic shift among primary school children in Beijing, China:A prospective study. Int J Med Sci. 2015;12:633–8. doi: 10.7150/ijms.12133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Xiong S, Sankaridurg P, Naduvilath T, Zang J, Zou H, Zhu J, et al. Time spent in outdoor activities in relation to myopia prevention and control:A meta-analysis and systematic review. ACTA Ophthalmol. 2017;95:551–66. doi: 10.1111/aos.13403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. French AN, Morgan IG, Mitchell P, Rose KA. Patterns of myopigenic activities with age, gender and ethnicity in Sydney school children. Ophthalmic Physiol Opt. 2013;33:318–28. doi: 10.1111/opo.12045. [DOI] [PubMed] [Google Scholar]
- 37. French AN, Morgan IG, Mitchell P, Rose KA. Risk factors for incident myopia in Australian schoolchildren:The Sydney adolescent vascular and eye study. Ophthalmology. 2013;120:2100–8. doi: 10.1016/j.ophtha.2013.02.035. [DOI] [PubMed] [Google Scholar]
- 38. Deng L, Gwiazda J, Thorn F. Children's refractions and visual activities in the school year and summer. Optom Vis Sci. 2010;87:406–13. doi: 10.1097/OPX.0b013e3181da8a85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Lu B, Congdon N, Liu X, Choi K, Lam DSC, Zhang M, et al. Associations between near work, outdoor activity, and myopia among adolescent students in rural China:The Xichang Pediatric Refractive Error Study report no. 2. Arch Ophthalmol. 2009;127:769–75. doi: 10.1001/archophthalmol.2009.105. [DOI] [PubMed] [Google Scholar]
- 40. Ip JM, Saw S-M, Rose KA, Morgan IG, Kifley A, Wang JJ, et al. Role of near work in myopia:Findings in a sample of Australian school children. Invest Ophthalmol Vis Sci. 2008;49:2903–10. doi: 10.1167/iovs.07-0804. [DOI] [PubMed] [Google Scholar]
- 41. Chua SYL, Ikram MK, Tan CS, Lee YS, Ni Y, Shirong C, et al. Relative contribution of risk factors for early-onset myopia in young Asian children. Invest Ophthalmol Vis Sci. 2015;56:8101–7. doi: 10.1167/iovs.15-16577. [DOI] [PubMed] [Google Scholar]
- 42. Zhou Z, Morgan IG, Chen Q, Jin L, He M, Congdon N. Disordered sleep and myopia risk among Chinese Children. PLoS One. 2015;10:e0121796. doi: 10.1371/journal.pone.0121796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Pan C-W, Chen Q, Sheng X, Li J, Niu Z, Zhou H, et al. Ethnic variations in myopia and ocular biometry among adults in a rural community in China:The Yunnan minority eye studies. Invest Ophthalmol Vis Sci. 2015;56:3235–41. doi: 10.1167/iovs.14-16357. [DOI] [PubMed] [Google Scholar]
- 44. Guo K, Yang DY, Wang Y, Yang XR, Jing XX, Guo YY, et al. Prevalence of myopia in schoolchildren in Ejina:The Gobi desert children eye study. Investig Ophthalmol Vis Sci. 2015;56:1769–74. doi: 10.1167/iovs.14-15737. [DOI] [PubMed] [Google Scholar]
- 45. Lee Y-Y, Lo C-T, Sheu S-J, Yin L-T. Risk factors for and progression of myopia in young Taiwanese men. Ophthalmic Epidemiol. 2015;22:66–73. doi: 10.3109/09286586.2014.988874. [DOI] [PubMed] [Google Scholar]
- 46. Zhou R, Zhang WF, Yang Y, Ting Y. Analysis of myopia prevalence and influencing factors among primary school students in the urban area of Lanzhou city. Int Eye Sci. 2014;14:903–7. [Google Scholar]
- 47. Guo Y, Liu LJ, Xu L, Lv YY, Tang P, Feng Y, et al. Outdoor activity and myopia among primary students in rural and urban regions of Beijing. Ophthalmology. 2013;120:277–83. doi: 10.1016/j.ophtha.2012.07.086. [DOI] [PubMed] [Google Scholar]
- 48. Low W, Dirani M, Gazzard G, Chan Y-H, Zhou H-J, Selvaraj P, et al. Family history, near work, outdoor activity, and myopia in Singapore Chinese preschool children. Br J Ophthalmol. 2010;94:1012–6. doi: 10.1136/bjo.2009.173187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Saw S-M, Shankar A, Tan S-B, Taylor H, Tan DTH, Stone RA, et al. A cohort study of incident myopia in Singaporean children. Invest Ophthalmol Vis Sci. 2006;47:1839–44. doi: 10.1167/iovs.05-1081. [DOI] [PubMed] [Google Scholar]
- 50. Jones LA, Sinnott LT, Mutti DO, Mitchell GL, Moeschberger ML, Zadnik K. Parental history of myopia, sports and outdoor activities, and future myopia. Invest Ophthalmol Vis Sci. 2007;48:3524–32. doi: 10.1167/iovs.06-1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Wu P-C, Tsai C-L, Wu H-L, Yang Y-H, Kuo H-K. Outdoor activity during class recess reduces myopia onset and progression in school children. Ophthalmology. 2013;120:1080–5. doi: 10.1016/j.ophtha.2012.11.009. [DOI] [PubMed] [Google Scholar]
- 52. Yi J-H, Li R-R. [Influence of near-work and outdoor activities on myopia progression in school children] Zhongguo Dang Dai Er Ke Za Zhi. 2011;13:32–5. [PubMed] [Google Scholar]
- 53. Saw SM, Nieto FJ, Katz J, Schein OD, Levy B, Chew SJ. Factors related to the progression of myopia in Singaporean children. Optom Vis Sci. 2000;77:549–54. doi: 10.1097/00006324-200010000-00009. [DOI] [PubMed] [Google Scholar]
- 54. Li S-M, Li H, Li S-Y, Liu L-R, Kang M-T, Wang Y-P, et al. Time outdoors and myopia progression over 2 years in Chinese children:The Anyang childhood eye study. Invest Ophthalmol Vis Sci. 2015;56:4734–40. doi: 10.1167/iovs.14-15474. [DOI] [PubMed] [Google Scholar]
- 55. Öner V, Bulut A, Oruç Y, Özgür G. Influence of indoor and outdoor activities on progression of myopia during puberty. Int Ophthalmol. 2016;36:121–5. doi: 10.1007/s10792-015-0091-5. [DOI] [PubMed] [Google Scholar]
- 56. Jones-Jordan LA, Sinnott LT, Cotter SA, Kleinstein RN, Manny RE, Mutti DO, et al. Time outdoors, visual activity, and myopia progression in juvenile-onset myopes. Invest Ophthalmol Vis Sci. 2012;53:7169–75. doi: 10.1167/iovs.11-8336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Yingyong P. Risk factors for refractive errors in primary school children (6-12 years old) in Nakhon Pathom Province. J Med Assoc Thai. 2010;93:1288–93. [PubMed] [Google Scholar]
- 58. Saw S-M, Chua W-H, Hong C-Y, Wu H-M, Chan W-Y, Chia K-S, et al. Nearwork in early-onset myopia. Invest Ophthalmol Vis Sci. 2002;43:332–9. [PubMed] [Google Scholar]
- 59. Saw SM, Hong RZ, Zhang MZ, Fu ZF, Ye M, Tan D, et al. Near-work activity and myopia in rural and urban schoolchildren in China. J Pediatr Ophthalmol Strabismus. 2001;38:149–55. doi: 10.3928/0191-3913-20010501-08. [DOI] [PubMed] [Google Scholar]
- 60. Mavrakanas TA, Mandalos A, Peios D, Golias V, Megalou K, Gregoriadou A, et al. Prevalence of myopia in a sample of Greek students. Acta Ophthalmol Scand. 2000;78:656–9. doi: 10.1034/j.1600-0420.2000.078006656.x. [DOI] [PubMed] [Google Scholar]
- 61. Wu P-C, Tsai C-L, Hu C-H, Yang Y-H. Effects of outdoor activities on myopia among rural school children in Taiwan. Ophthalmic Epidemiol. 2010;17:338–42. doi: 10.3109/09286586.2010.508347. [DOI] [PubMed] [Google Scholar]
- 62. Lin Z, Vasudevan B, Jhanji V, Mao GY, Gao TY, Wang FH, et al. Near work, outdoor activity, and their association with refractive error. Optom Vis Sci. 2014;91:376–82. doi: 10.1097/OPX.0000000000000219. [DOI] [PubMed] [Google Scholar]
- 63. Rose KA, Morgan IG, Smith W, Burlutsky G, Mitchell P, Saw S-M. Myopia, lifestyle, and schooling in students of Chinese ethnicity in Singapore and Sydney. Arch Ophthalmol (Chicago, Ill 1960) 2008;126:527–30. doi: 10.1001/archopht.126.4.527. [DOI] [PubMed] [Google Scholar]
- 64. Jones-Jordan LA, Mitchell GL, Cotter SA, Kleinstein RN, Manny RE, Mutti DO, et al. Visual activity before and after the onset of juvenile myopia. Invest Ophthalmol Vis Sci. 2011;52:1841–50. doi: 10.1167/iovs.09-4997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Scheiman M, Zhang Q, Gwiazda J, Hyman L, Harb E, Weissberg E, et al. Visual activity and its association with myopia stabilisation. Ophthalmic Physiol Opt. 2014;34:353–61. doi: 10.1111/opo.12111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Pärssinen O, Lyyra AL. Myopia and myopic progression among schoolchildren:A three-year follow-up study. Invest Ophthalmol Vis Sci. 1993;34:2794–802. [PubMed] [Google Scholar]
- 67. Hepsen IF, Evereklioglu C, Bayramlar H. The effect of reading and near-work on the development of myopia in emmetropic boys:A prospective, controlled, three-year follow-up study. Vision Res. 2001;41:2511–20. doi: 10.1016/s0042-6989(01)00135-3. [DOI] [PubMed] [Google Scholar]
- 68. Fitzgerald MEC, Wildsoet CF, Reiner A. Temporal relationship of choroidal blood flow and thickness changes during recovery from form deprivation myopia in chicks. Exp Eye Res. 2002;74:561–70. doi: 10.1006/exer.2002.1142. [DOI] [PubMed] [Google Scholar]
- 69. Nickla DL. Transient increases in choroidal thickness are consistently associated with brief daily visual stimuli that inhibit ocular growth in chicks. Exp Eye Res. 2007;84:951–9. doi: 10.1016/j.exer.2007.01.017. [DOI] [PubMed] [Google Scholar]
- 70. Lougheed T. Myopia:The evidence for environmental factors. Environ Health Perspect. 2014;122:A12–9. doi: 10.1289/ehp.122-A12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Morgan IG, Iribarren R, Fotouhi A, Grzybowski A. Cycloplegic refraction is the gold standard for epidemiological studies. Acta Ophthalmol. 2015;93:581–5. doi: 10.1111/aos.12642. [DOI] [PubMed] [Google Scholar]
- 72. Rotsos T, Grigorious D, Kokkolaki A, Manios N. A comparison of manifest refractions, cycloplegic refractions and retinoscopy on the RMA-3000 autorefractometer in children aged 3 to 15 years. Clin Ophthalmol. 2009;3:429–31. doi: 10.2147/opth.s5145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Funarunart P, Tengtrisorn S, Sangsupawanich P, Siangyai P. Accuracy of noncycloplegic refraction in primary school children in southern Thailand. J Med Assoc Thai. 2009;92:806–11. [PubMed] [Google Scholar]
- 74. Kaiser PK. Prospective evaluation of visual acuity assessment:A comparison of Snellen versus ETDRS charts in clinical practice (an aos thesis) Trans Am Ophthalmol Soc. 2009;107:311–24. [PMC free article] [PubMed] [Google Scholar]
- 75. Rose KA, Ip J, Robaei D, Huynh SC, Kifley A, Smith W, et al. Near–work and outdoor activities and the prevalence of myopia in Australian school students aged 12–13 years:The Sydney myopia study Invest Ophthalmol Vis Sci 2006. 47 5453 17122136 [Google Scholar]
- 76. French AN, Ashby RS, Morgan IG, Rose KA. Time outdoors and the prevention of myopia. Exp Eye Res. 2013;114:58–68. doi: 10.1016/j.exer.2013.04.018. [DOI] [PubMed] [Google Scholar]
- 77. McCarthy CS, Megaw P, Devadas M, Morgan IG. Dopaminergic agents affect the ability of brief periods of normal vision to prevent form-deprivation myopia. Exp Eye Res. 2007;84:100–7. doi: 10.1016/j.exer.2006.09.018. [DOI] [PubMed] [Google Scholar]
- 78. Mehdizadeh M, Nowroozzadeh MH. Outdoor activity and myopia. Ophthalmology. 2009;116:1229–30. doi: 10.1016/j.ophtha.2009.02.015. author reply 1230. [DOI] [PubMed] [Google Scholar]
- 79. Mutti DO, Cooper ME, Dragan E, Jones-Jordan LA, Bailey MD, Marazita ML, et al. Vitamin D receptor (VDR) and group-specific component (GC, Vitamin D–binding protein) polymorphisms in myopia. Invest Ophthalmol Vis Sci. 2011;52:3818–24. doi: 10.1167/iovs.10-6534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Prepas SB. Light, literacy and the absence of ultraviolet radiation in the development of myopia. Med Hypotheses. 2008;70:635–7. doi: 10.1016/j.mehy.2007.07.023. [DOI] [PubMed] [Google Scholar]
- 81. Guo Y, Liu LJ, Xu L, Tang P, Lv YY, Feng Y, et al. Myopic shift and outdoor activity among primary school children:One-year follow-up study in Beijing. PLoS One. 2013;8:e75260. doi: 10.1371/journal.pone.0075260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Hu YY, Wu JF, Lu TL, Wu H, Sun W, Wang XR. Effect of cycloplegia on the refractive status of children:The Shandong children eye study. PLoS One. 2015;10:e0117482. doi: 10.1371/journal.pone.0117482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Morgan IG, Rose KA. Myopia and international educational performance. Ophthalmic Physiol Opt. 2013;33:329–38. doi: 10.1111/opo.12040. [DOI] [PubMed] [Google Scholar]