Abstract
Purpose:
To observe the effects of caffeine intake on vessel densities in macular and peripapillary regions and to analyze the correlations of vascular properties of these two interlinked regions in healthy volunteers using optical coherence tomography angiography (OCTA).
Methods:
In this prospective randomized, double-masked, placebo-controlled study, 120 participants were grouped into two groups: sixty subjects as a study group, which received caffeine and sixty subjects as a placebo group, which received a placebo. OCTA imaging was performed at baseline and 1 h after drug intake. Changes in macular and radial peripapillary capillary (RPC) vessel densities (VD) and foveal avascular zone (FAZ) parameters and correlation of these parameters were analyzed.
Results:
Baseline macular and RPC VD and FAZ parameters showed no significant difference between study and placebo groups (P > 0.05 for all). VD parameters in all segments of superficial and deep macular regions and peripapillary region showed a statistically significant decrease after caffeine intake (P < 0.001 for all). All macular superficial VD parameters showed a positive correlation with deep perifovea VD (P < 0.05 for all). Also, superficial perifovea VD was positively correlated with all deep macular VD parameters except deep fovea VD (P < 0.05 for all).
Conclusion:
We show that caffeine causes a decrease in macular and peripapillary vessel densities in healthy subjects, and correlations were observed between macular and peripapillary VD parameters. We believe that future studies are needed to support the effect of caffeine on peripapillary VD and the idea of using deep perifovea VD as the main parameter to estimate superficial macular parameters.
Keywords: Caffeine, deep macular vessel density, foveal avascular zone vessel density, radial peripapillary capillary vessel density, superficial macular vessel density
Caffeine, which is found in chocolate, fruits, and some of the common beverages like tea and coffee, is the most commonly used neurostimulant worldwide.[1] One cup of coffee contains about 30 to 175 mg of caffeine, and 200 mg to 300 mg intake a day is expressed as moderate coffee intake.[1,2,3,4] Caffeine reaches maximum plasma concentration in 20–120 min; its half-life is 3–6 h. Besides central nervous system stimulation, caffeine causes diuresis, myocardial stimulation, smooth muscle relaxation, and an increase of vascular resistance through vasoconstriction.[5] Caffeine may cause intraocular pressure to rise temporarily in normal and glaucomatous subjects after intake.[6,7] Some studies reported decreased cerebral and ocular blood flow including the macula, optic nerve head, and choroid.[7,8,9,10,11]
Optical coherence tomography angiography (OCTA) is a non-invasive, dye-free imaging technique that allows us to evaluate microcirculation in seconds, taking into account both structural and functional (i.e., blood flow) data based on the red blood cell movement.[12] OCTA provides angiographic images and volumetric data with clinical capacity that helps specifically localize and identify the disease.
To our knowledge, there are no studies that have evaluated the effect of caffeine on peripapillary region vascularity or the relationship of both macular and peripapillary region vascular density. The aim of the current study is to observe the effects of acute caffeine ingestion on vessel densities in macular and peripapillary regions and to analyze the correlations of vascular properties of these two interlinked regions in healthy subjects using OCTA.
Methods
This prospective randomized, double-masked, placebo-controlled study took place in the Department of Ophthalmology at Kocaeli University between June 2020 and July 2020 with approval from the Institutional Review Board of the Kocaeli University. Our study was conducted following the tenets of the Declaration of Helsinki. Informed consent was obtained from all participants. All subjects were told to avoid beverages or foods containing caffeine and not to smoke for 24 h before the dose of the drug or placebo. There were two groups in the study; group 1 got a 200-mg caffeine tablet, and group 2 got a placebo.
Exclusion criteria at study entry included: (1) best-corrected visual acuity (BCVA) <20/20 in either eye, (2) any pathology on biomicroscopic and fundus examination, (3) any retinal and choroidal pathology observed on optical coherence tomography (OCT) of the macula and enhanced-depth imaging (EDI) OCT of the choroid, (4) presence of systemic disease which may influence ocular microcirculation like diabetes, hypertension, and cardiovascular disease, (5) two or more cups of coffee consumption per day, and (6) systemic drug or alcohol use.
A complete ophthalmologic examination, including best-corrected visual acuity (BCVA), slit-lamp biomicroscopy, IOP measurement with Goldmann applanation tonometry, axial eye length (AL) measurement using an IOLMaster (ver. 3.02; Carl Zeiss, Meditec, Jena, Germany), spherical equivalent (SE formula = Cylindrical power/2 + Spherical power), dilated fundus examination were performed for all participants. Before fundus examination, a combination of 1% tropicamide and 2.5% phenylephrine was used to dilate pupils. Baseline systolic blood pressure (SBP), diastolic blood pressure (DBP), IOP measurement, retinal nerve fiber layer thickness (RNFL), central macular thickness (CMT), subfoveal choroidal thickness (CT) by SD-OCT (Heidelberg Engineering GmbH, Heidelberg, Germany) and data of OCTA were noted. Data were collected from the right eye of each participant. The measurements were repeated 1 h after oral caffeine or placebo ingestion. The subjects were told not to drink or eat anything or exercise during this period in order not to affect the retinal microcirculation.
Optical Coherence Tomography Angiography
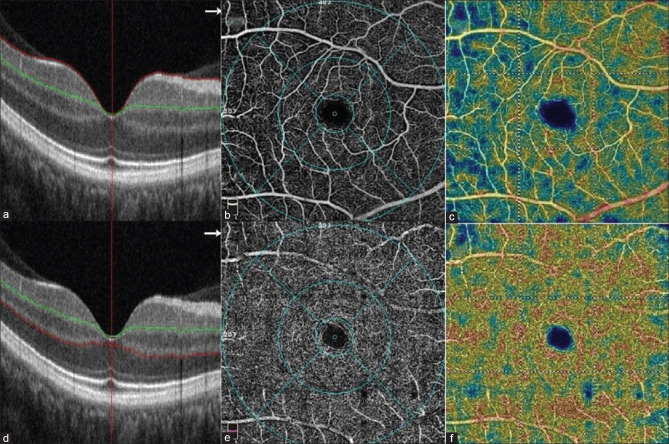
In the current study, the Optovue AngioVue system based on decorrelation angiography (RTVue XR Avanti; Optovue Inc., Fremont, CA, USA) was used for evaluating the macular, peripapillary, and foveal avascular zone (FAZ) regions. Optovue AngioVue system is an angiographic program that includes an SD-OCT providing both thickness and vascular density. High-density Angio Retina 6 × 6-mm2 protocol was performed to assess the macular region to cover the whole macular area. Macular superficial vessel density (msVD) was measured from the inner limiting membrane (ILM) to the inner plexiform layer (IPL) [Fig. 1a]. Macular deep vessel density (mdVD) was measured from IPL to OPL (outer plexiform layer) [Fig. 1d]. FAZ density was measured from ILM to OPL [Fig. 2a]. The internal software (Optovue Inc., software version: 2018.0.0.14) calculated the whole-image vessel density (wiVD), the parafoveal vessel density (ParaVD) (centered on the fovea-inner diameter of 1 mm and the outer diameter of 3 mm), and perifoveal vessel density (PeriVD) (centered on the parafovea-inner diameter of 3 mm and the outer diameter of 6 mm), vessel density values of all segments [Fig. 1b and e] and FAZ parameters [the area of FAZ, the perimeter of FAZ and FAZ density-300 mm (FD-300) (vessel density around the 300-mm width of the FAZ region)] [Fig. 2b and c].
Figure 1.
Superficial macular density was evaluated in the region extending from inner limiting membrane (ILM) (red line) to the inner plexiform layer (IPL) (green line) (a), subdivisions of the parafoveal and perifoveal ring into four quadrants in the superficial layer (b), color image of the superficial macular region (c). Deep macular density was evaluated in the region extending from the inner plexiform layer (IPL) (green line) to the outer plexiform layer (OPL) (red line) (d), subdivisions of the parafoveal and perifoveal ring into four quadrants in the deep layer (e), color image of the deep macular region (f)
Figure 2.
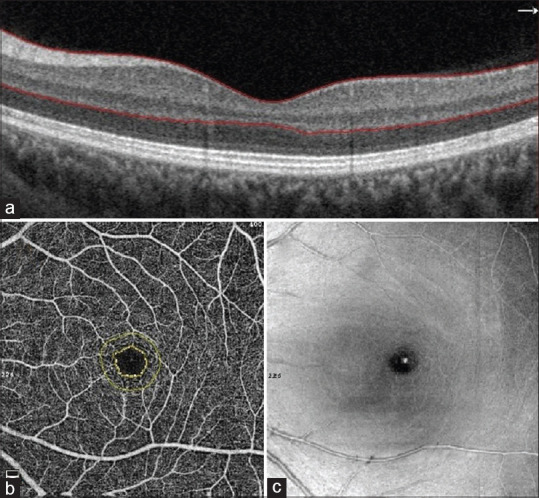
Foveal avascular zone (FAZ) was evaluated in the region extending from internal limiting membrane (ILM) to outer plexiform layer (OPL) (red line to red line) (a) image of FAZ measurements (yellow lines) (b), C-scan (en-face) image of FAZ (c)
High-density Angio Disc 4.5 × 4.5-mm protocol was performed to assess the peripapillary region. Vessels were analyzed from ILM to the posterior boundary of the RNFL [Fig. 3a]. Internal software calculates radial peripapillary capillary (RPC) vessel density (VD) automatically. ONH-centered annular region of interest (ROI) was over imposed onto the peripapillary OCTA scan [Fig. 3b]. The percentage of the whole area filled with the vessels was expressed as VD [Figs. 1c, f and 3c]. Poor-quality images with 1) low scan quality <8/10, 2) poor clarity, 3) motion or vitreous floater artifacts, and 4) segmentation errors, were not included.
Figure 3.
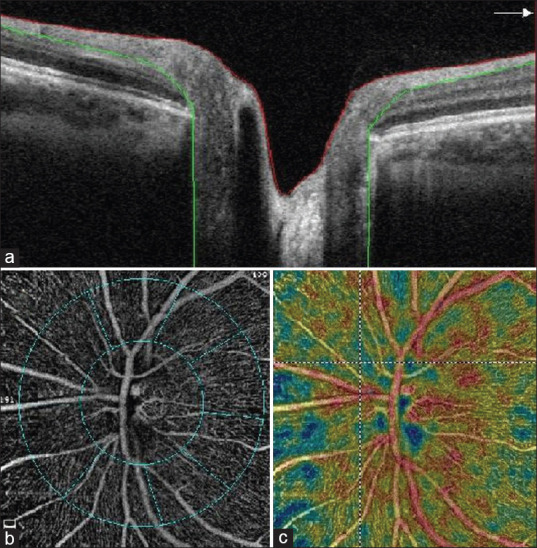
Peripapillary retinal nerve fiber layer was evaluated in the region extending from ILM (red line) to nerve fiber layer (NFL) (green line) (a), subdivisions of the peripapillary region (b), color image of the peripapillary region (c)
Statistical analysis
IBM SPSS for Windows version 20.0 (SPSS, Chicago, IL, USA) was used to perform all statistical analyses. The assumption of normality was tested with the Kolmogorov-Smirnov test. Continuous variables with normal distribution were presented as mean ± standard deviation; continuous variables with no normal distribution were presented as median (25th-75th percentile). Counts (percentages) represented categorical variables. Independent samples t-test/Mann–Whitney U test was performed to compare continuous variables between groups, whichever was appropriate. Before-after drug comparisons were analyzed by paired-samples t-test/Wilcoxon signed ranks test, whichever was appropriate. Spearman correlation analyses were used to determine the associations between continuous variables. Interobserver reproducibility was determined using the intraclass correlation coefficient. All statistical analyses were performed with 5% significance and a two-sided P value <0.05 was considered as statistically significant.
Results
Demographic and clinical parameters
We recruited 60 participants (60 eyes) in the caffeine group (16 men and 44 women) and 60 participants (60 eyes) in the placebo group (16 men and 44 women) between October 2020–November 2020. The median age was 36.50 (26–50) and 39.50 (18–51) in the caffeine and placebo groups, respectively. The median SE was −0.5 (−3.0–1.25) D, the median AL was 23.61 (22.07–26.35) mm, the median SBP was 105 (90–140) mmHg, the median DBP was 70 (50–80) mmHg, and the median IOP was 14 (9–20) mmHg in the study group. The median SE was − 0.5 (−3.0–2.75) D, the median AL was 23.55 (21.15–25.27) mm, the median SBP was 110 (90–140) mmHg, the median DBP was 70 (60–80) mmHg, and the median IOP was 15 (10–21) mmHg in the placebo group. No significant difference was seen in demographic and clinical parameters between the two groups (P > 0.05, for all) [Table 1]. SBP, DBP, and IOP did not show significant difference in placebo group (P = 0.996, P = 0.697, and P = 0.093, respectively) and in caffeine group (P = 0.097, P = 0.358, and P = 0.215, respectively) after drug intake.
Table 1.
Demographic and clinical features of the caffeine and placebo group
| Caffeine Group (n: 60) | Control Group (n: 60) | P | |
|---|---|---|---|
| Age (years) | 36.50 (26-50) | 39.50 (18-51) | 0.231* |
| Sex (Male/female) | 16 (26.7%)/44 (73.3%) | 16 (26.7%)/44 (73.3%) | 1.000† |
| IOP (mmHg) | 14.0 (9.0-20.0) | 15.0 (10.0-21.0) | 0.371* |
| SE (D) | -0.5 [-3.0- (+1.25)] | -0.5 [-3.0- (+2.75)] | 0.340* |
| AL (mm) | 23.61 (22.07-26.35) | 23.55 (21.15-25.27) | 0.385* |
| SBP (mmHg) | 105.0 (90.0-140.0) | 110.0 (90.0-140.0) | 0.204* |
| DBP (mmHg) | 70.0 (50.0-80.0) | 70.0 (60.0-80.0) | 0.834* |
IOP: intraocular pressure; SE: Spherical Equivalent; AL: Axial Length; SBP: Systolic Blood Pressure; DBP: Diastolic Blood Pressure. *Mann-Whitney U test used for comparison, †Chi-square test used for comparison
Macular, radial peripapillary capillary vessel densities and foveal avascular zone parameters
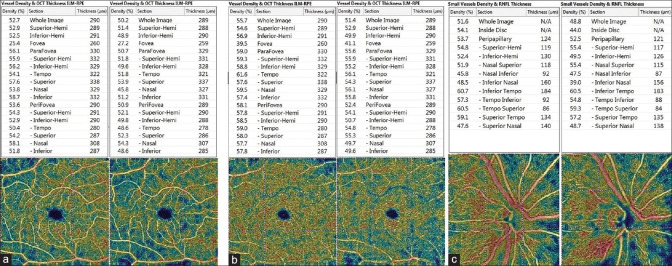
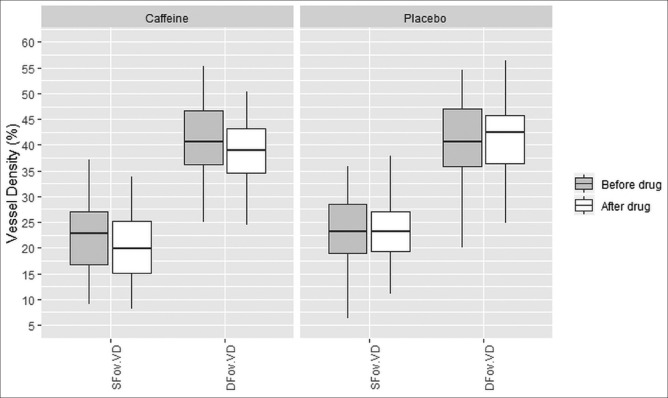
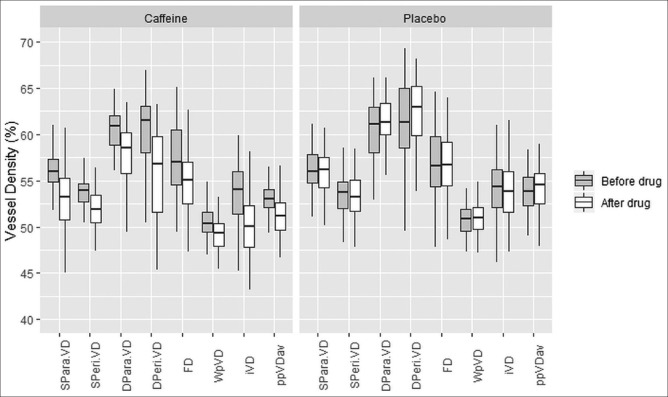
The intraclass correlation coefficient of the interobserver reproducibility for measurement of superficial whole macular VD was 0.977 (95% confidence interval 0.871–0.993). Baseline vascular parameters including superficial and deep macular VD, RPC VD, and FAZ were shown in Table 2. All baseline parameters showed no significant difference between the caffeine and placebo groups (P > 0.05). In the study group, vessel density in all segments of superficial and deep macular regions and peripapillary region showed a statistically significant decrease after oral caffeine intake (P < 0.001 for all) [Table 3 and Fig. 4]. In terms of FAZ parameters, while FAZ area and FAZ perimeter did not change (P = 0.724 and P = 0.818, respectively), FD 300 decreased significantly after caffeine intake (P < 0.001) [Table 3]. Vessel density in all segments of superficial and deep macular regions, peripapillary region, and FAZ revealed no significant difference 1 h after placebo intake compared to baseline (P > 0.05, for all) [Table 4]. Figs. 5 and 6 show the changes in some main superficial and deep macular VD, RPC VD, and FAZ parameters of the caffeine and placebo groups after drug intake.
Table 2.
Baseline superficial and deep macular and radial peripapillary capillary vessel density, foveal avascular zone, and optic nerve head parameters of caffeine and placebo group
| Caffeine Group (n=60) | Placebo Group (n=60) | P | |
|---|---|---|---|
| Superficial Macular Vessel Density (VD) (%) | |||
| wiVD | 53.00 (52.05-53.97) | 52.75 (51.02-53.90) | 0.278† |
| Sup hemi VD | 52.90 (52.00-53.77) | 53.20 (52.02-54.60) | 0.271† |
| Inf hemi VD | 53.30 (52.20-54.20) | 53.20 (51.22-54.55) | 0.485† |
| Fovea | 22.14±6.78 | 23.24±7.05 | 0.386* |
| Parafovea | 55.95 (54.67-57.30) | 56.00 (54.65-58.02) | 0.522† |
| Para sup hemi | 55.85±2.64 | 56.22±3.13 | 0.915* |
| Para inf hemi | 56.15 (54.40-57.00) | 56.00 (54.47-58.02) | 0.596† |
| Para superior | 56.75 (55.02-58.50) | 56.80 (54.90-59.30) | 0.611† |
| Para nasal | 55.10 (53.70-56.57) | 55.40 (53.02-57.60) | 0.733† |
| Para inferior | 56.50 (55.50-58.00) | 56.80 (55.00-58.77) | 0.793† |
| Para temporal | 55.65 (53.62-57.27) | 56.05 (53.82-57.82) | 0.490† |
| Perifovea | 53.90 (52.70-54.67) | 53.72 (51.94-54.89) | 0.637† |
| Peri sup hemi | 53.80 (52.80-54.67) | 53.40 (51.70-55.15) | 0.416† |
| Peri inf hemi | 54.00 (52.90-54.90) | 54.05 (51.87-56.05) | 0.906† |
| Peri superior | 53.95 (52.30-55.25) | 53.70 (52.45-55.15) | 0.669† |
| Peri nasal | 57.65 (56.22-58.60) | 57.80 (55.62-59.77) | 0.620† |
| Peri inferior | 54.00 (52.60-55.62) | 54.50 (52.37-56.32) | 0.490† |
| Peri temporal | 50.40 (49.25-51.65) | 50.60 (48.82-52.70) | 0.285† |
| Deep Macular Vessel Density (VD)(%) | |||
| wiVD | 59.50 (56.15-61.47) | 59.30 (55.85-62.75) | 0.551† |
| Sup hemi VD | 58.90 (56.52-61.30) | 58.05 (53.42-60.65) | 0.078† |
| Inf hemi VD | 59.80 (56.30-61.55) | 59.90 (55.52-63.47) | 0.372† |
| Fovea | 40.90 (36.15-47.27) | 40.70 (35.62-47.15) | 0.867† |
| Parafovea | 60.95 (58.55-62.07) | 61.10 (57.82-62.97) | 0.700† |
| Para sup hemi | 61.10 (58.85-62.40) | 61.15 (57.50-63.05) | 0.773† |
| Para inf hemi | 61.30 (58.82-62.37) | 60.90 (57.70-63.40) | 0.914† |
| Para superior | 60.55 (58.42-62.10) | 60.25 (57.02-62.30) | 0.673† |
| Para nasal | 62.35 (60.42-63.57) | 62.10 (58.75-63.77) | 0.426† |
| Para inferior | 60.15 (58.02-61.60) | 58.45 (55.40-61.52) | 0.052† |
| Para temporal | 61.60 (59.82-62.75) | 61.90 (58.80-63.50) | 0.648† |
| Perifovea | 61.55 (57.95-63.10) | 61.10 (57.42-64.97) | 0.497† |
| Peri sup hemi | 60.95 (58.00-62.90) | 59.45 (54.55-62.47) | 0.051† |
| Peri inf hemi | 61.50 (58.35-63.70) | 61.85 (56.67-65.60) | 0.224† |
| Peri superior | 60.15 (57.92-63.27) | 59.00 (54.75-62.67) | 0.089† |
| Peri nasal | 60.55 (57.50-63.37) | 60.75 (54.62-64.27) | 0.948† |
| Peri inferior | 62.20 (58.77-64.65) | 62.65 (57.37-66.35) | 0.277† |
| Peri temporal | 62.40 (59.67-63.20) | 61.60 (58.25-64.85) | 0.956† |
| Radial peripapillary capillary vessel density (RPC VD) | |||
| wpVD | 50.48±2.06 | 50.70±2.06 | 0.564* |
| iVD | 53.32±3.74 | 53.97±4.09 | 0.367* |
| ppVD average | 53.00 (52.10-54.15) | 53.85 (52.25-55.45) | 0.138† |
| ppVD sup hemi | 53.33±2.13 | 53.22±2.59 | 0.797* |
| ppVD inf hemi | 53.26±2.40 | 53.44±2.87 | 0.718* |
| ppVD superior | 53.30±2.70 | 53.20±3.21 | 0.854* |
| ppVD nasal | 50.00 (48.25-52.00) | 51.00 (48.00-52.00) | 0.581† |
| ppVD inferior | 55.00 (53.25-57.00) | 54.00 (50.25-57.00) | 0.092† |
| ppVD temporal | 56.00 (53.00-57.75) | 55.00 (53.00-57.00) | 0.455† |
| Foveal avscular zone (FAZ) parameters | |||
| FAZ area (mm2) | 0.27±0.09 | 0.30±0.12 | 0.097* |
| FAZ perimeter (mm) | 2.06 (1.71-2.23) | 2.07 (1.86-2.36) | 0.265† |
| FD-300 | 57.05 (54.58-60.49) | 56.48 (54.10-59.77) | 0.229† |
wiVD: whole image vessel density, para: parafovea, peri: perifovea, sup hemi: superior hemifield, inf hemi: inferior hemifield, wpVD: whole papillary vessel density, İVD: inside disk vessel density, ppVD: peripapillary vessel density, FD: FAZ density. *Student t-test was used for comparison, †Mann-Whitney U test used for comparisons
Table 3.
Superficial and deep macular and radial peripapillary capillary vessel density, foveal avascular zone, and optic nerve head parameters of caffeine group at baseline and 1 h after caffeine intake
| Caffeine Group baseline (n=60) | 1 h After Caffeine Intake (n=60) | P | |
|---|---|---|---|
| Superficial Macular Vessel Density (VD)(%) | |||
| wiVD | 53.00 (52.05-53.97) | 51.10 (49.70-52.67) | <0.001† |
| Sup hemi VD | 52.90 (52.00-53.77) | 51.20 (49.55-52.30) | <0.001† |
| Inf hemi VD | 53.30 (52.20-54.20) | 51.05 (49.52-52.62) | <0.001† |
| Fovea | 22.14±6.78 | 20.07±6.66 | <0.001* |
| Parafovea | 55.95 (54.67-57.30) | 53.20 (50.80-55.35) | <0.001† |
| Para sup hemi | 56.10 (54.35-57.22) | 53.05 (51.22-55.47) | <0.001† |
| Para inf hemi | 56.15 (54.40-57.00) | 53.40 (50.42-55.25) | <0.001† |
| Para superior | 56.57±2.63 | 53.30±4.21 | <0.001* |
| Para nasal | 55.10 (53.70-56.57) | 52.65 (51.05-54.62) | <0.001† |
| Para inferior | 56.50 (55.50-58.00) | 54.00 (49.52-55.87) | <0.001† |
| Para temporal | 55.36±2.85 | 52.20±3.84 | <0.001* |
| Perifovea | 53.90 (52.70-54.67) | 51.95 (50.35-53.47) | <0.001† |
| Peri sup hemi | 53.80 (52.80-54.67) | 51.70 (50.32-53.17) | <0.001† |
| Peri inf hemi | 53.86±2.44 | 51.43±3.09 | <0.001* |
| Peri superior | 53.95 (52.30-55.25) | 52.10 (49.92-53.37 | <0.001† |
| Peri nasal | 57.65 (56.22-58.60) | 55.60 (53.72-57.10) | <0.001† |
| Peri inferior | 54.30 (52.60-55.62) | 52.10 (49.75-53.87) | <0.001† |
| Peri temporal | 50.40 (49.25-51.65) | 47.65 (45.70-49.67) | <0.001† |
| Deep Macular Vessel Density (VD)(%) | |||
| wiVD | 58.44±3.99 | 54.07±5.03 | <0.001* |
| Sup hemi VD | 58.42±3.83 | 53.82±5.05 | <0.001* |
| Inf hemi VD | 59.80 (56.30-61.55) | 55.20 (49.22-58.82) | <0.001† |
| Fovea | 41.43±7.72 | 38.63±6.86 | <0.001* |
| Parafovea | 60.95 (58.55-62.07) | 58.55 (55.72-60.60) | <0.001† |
| Para sup hemi | 60.72±2.40 | 57.85±3.22 | <0.001* |
| Para inf hemi | 61.30 (58.82-62.37) | 57.90 (54.87-59.90) | <0.001† |
| Para superior | 60.24±2.73 | 57.03±3.57 | <0.001* |
| Para nasal | 62.35 (60.42-63.57) | 59.30 (56.70-60.87) | <0.001† |
| Para inferior | 60.15 (58.02-61.60) | 56.25 (52.77-59.40) | <0.001† |
| Para temporal | 61.60 (59.82-62.75) | 59.35 (56.92-60.67) | <0.001† |
| Perifovea | 61.55 (57.95-63.10) | 56.70 (51.30-59.85) | <0.001† |
| Peri sup hemi | 60.24±4.11 | 55.45±5.46 | <0.001* |
| Peri inf hemi | 61.50 (58.35-63.70) | 56.30 (50.57-60.15) | <0.001† |
| Peri superior | 60.15 (57.92-63.27) | 55.15 (50.42-59.20) | <0.001† |
| Peri nasal | 60.55 (57.50-63.37) | 54.95 (49.35-58.97) | <0.001† |
| Peri inferior | 62.20 (58.77-64.65) | 56.75 (50.72-60.67) | <0.001† |
| Peri temporal | 62.40 (59.67-63.20) | 58.25 (54.82-60.35) | <0.001† |
| Radial peripapillary capillary vessel density (RPC VD) | |||
| wpVD | 50.48±2.06 | 48.99±2.12 | <0.001* |
| iVD | 53.32±3.74 | 49.82±4.34 | <0.001* |
| ppVD average | 53.00 (52.10-54.15) | 51.15 (49.60-52.75 | <0.001† |
| ppVD sup hemi | 53.33±2.13 | 51.19±2.34 | <0.001* |
| ppVD inf hemi | 53.26±2.40 | 50.84±2.53 | <0.001* |
| ppVD superior | 53.00 (51.25-55.00) | 50.00 (48.00-53.00) | <0.001† |
| ppVD nasal | 50.00 (48.25-52.00) | 49.00 (47.00-50.00) | <0.001† |
| ppVD inferior | 55.00 (53.25-57.00) | 51.00 (50.00-54.00) | <0.001† |
| ppVD temporal | 55.45±3.11 | 53.43±2.90 | <0.001* |
| Foveal avscular zone (FAZ) parameters | |||
| FAZ area (mm2) | 0.27±0.09 | 0.27±0.09 | 0.724* |
| FAZ perimeter (mm) | 2.06 (1.70-2.23) | 2.08 (1.70-2.23 | 0.818† |
| FD-300 | 57.33±3.52 | 54.61±4.04 | <0.001* |
wiVD: whole image vessel density, para: parafovea, peri: perifovea, sup hemi: superior hemifield, inf hemi: inferior hemifield, wpVD: whole papillary vessel density, İVD: inside disk vessel density, ppVD: peripapillary vessel density, FD: FAZ density. *student t-test was used for comparison, †Mann-Whitney U test used for comparison
Figure 4.
Measurement of optical coherence tomography angiography parameters on a superficial (a), deep capillary plexus (b) and peripapillary region (c). Left columns represent vessel density parameters (top) and color map images of the patient (bottom) before caffeine intake. Right columns represent vessel density parameters (top) and color map images of the patient (bottom) after caffeine intake. Note the decrease of parameters related to caffeine intake
Table 4.
Superficial and deep macular and radial peripapillary capillary vessel density, foveal avascular zone, and optic nerve head parameters of control group at baseline and 1 h after placebo intake
| Control Group baseline (n=60) | 1 h After Placebo Intake (n=60) | P | |
|---|---|---|---|
| Superficial Macular Vessel Density (VD)(%) | |||
| wiVD | 52.75 (51.02-53.90) | 52.10 (50.90-54.05) | 0.199† |
| Sup hemi VD | 53.20 (52.02-54.60) | 53.25 (51.52-54.77) | 0.310† |
| Inf hemi VD | 53.20 (51.22-54.55) | 52.80 (51.17-54.20) | 0.189† |
| Fovea | 23.24±7.05 | 22.82±7.43 | 0.276* |
| Parafovea | 56.00 (54.65-58.02) | 56.05 (54.22-57.50) | 0.303† |
| Para sup hemi | 56.45 (54.52-58.37) | 55.85 (54.37-57.97) | 0.416† |
| Para inf hemi | 56.00 (54.47-58.02) | 56.50 (54.30-57.95) | 0.505† |
| Para superior | 56.80 (54.90-59.30) | 56.35 (54.75-58.07) | 0.310† |
| Para nasal | 55.40 (53.02-57.60) | 55.80 (52.70-57.97) | 0.971† |
| Para inferior | 56.80 (55.00-58.77) | 56.75 (54.02-58.62) | 0.401† |
| Para temporal | 56.05 (53.82-57.82) | 55.70 (54.12-57.20) | 0.347† |
| Perifovea | 53.72 (51.94-54.89) | 53.17 (51.62-55.09) | 0.168† |
| Peri sup hemi | 53.40 (51.70-55.15) | 53.05 (51.40-55.17) | 0.381† |
| Peri inf hemi | 53.92±2.58 | 53.16±3.50 | 0.107* |
| Peri superior | 53.70 (52.45-55.15) | 53.70 (52.02-56.42) | 0.616† |
| Peri nasal | 57.74±2.56 | 57.21±3.02 | 0.212* |
| Peri inferior | 54.37±2.78 | 53.64±3.35 | 0.123* |
| Peri temporal | 50.60 (48.82-52.70) | 50.80 (48.70-52.47) | 0.211† |
| Deep Macular Vessel Density (VD)(%) | |||
| wiVD | 59.30 (55.85-62.75) | 60.70 (56.92-62.95) | 0.567† |
| Sup hemi VD | 58.05 (53.42-60.65) | 58.60 (54.70-61.10) | 0.363† |
| Inf hemi VD | 59.90 (55.52-63.47) | 61.20 (57.77-63.30) | 0.363† |
| Fovea | 40.70 (35.62-47.15) | 42.45 (36.15-45.97) | 0.777† |
| Parafovea | 61.10 (57.82-62.97) | 61.35 (59.80-63.45) | 0.101† |
| Para sup hemi | 61.15 (57.50-63.05) | 61.25 (59.65-63.50) | 0.094† |
| Para inf hemi | 60.90 (57.70-63.40) | 61.60 (59.35-63.50) | 0.085† |
| Para superior | 60.25 (57.02-62.30) | 61.30 (58.62-62.87) | 0.172† |
| Para nasal | 62.10 (58.75-63.77) | 62.45 (60.72-64.70) | 0.074† |
| Para inferior | 58.45 (55.40-61.52) | 59.55 (57.10-61.67) | 0.086† |
| Para temporal | 61.90 (58.80-63.50) | 62.30 (60.10-64.07) | 0.154† |
| Perifovea | 61.10 (57.42-64.97) | 62.90 (59.37-65.25) | 0.219† |
| Peri sup hemi | 59.45 (54.55-62.47) | 60.50 (57.30-63.05) | 0.208† |
| Peri inf hemi | 61.85 (56.67-65.60) | 63.80 (59.65-65.47) | 0.367† |
| Peri superior | 59.00 (54.75-62.67) | 60.45 (57.90-63.30) | 0.291† |
| Peri nasal | 60.75 (54.62-64.27) | 60.65 (57.47-64.07) | 0.476† |
| Peri inferior | 62.65 (57.37-66.35) | 64.05 (61.00-65.70) | 0.516† |
| Peri temporal | 61.60 (58.25-64.85) | 62.90 (60.62-65.50) | 0.062† |
| Radial peripapillary capillary vessel density (RPC VD) | |||
| wpVD | 50.90 (49.45-51.97) | 51.00 (49.70-52.10) | 0.901† |
| iVD | 53.97±4.09 | 53.34±4.12 | 0.120* |
| ppVD average | 53.85 (52.25-55.45) | 54.55 (52.50-55.87) | 0.188† |
| ppVD sup hemi | 53.22±2.59 | 53.64±2.97 | 0.192* |
| ppVD inf hemi | 54.10 (51.62-55.25) | 54.45 (51.87-56.07) | 0.524† |
| ppVD superior | 53.00 (51.00-56.00) | 54.00 (51.00-57.00) | 0.053† |
| ppVD nasal | 51.00 (48.00-52.00) | 51.00 (48.25-53.00) | 0.615† |
| ppVD inferior | 54.00 (50.25-57.00) | 55.00 (52.00-58.00) | 0.050† |
| ppVD temporal | 55.00 (53.00-57.00) | 55.00 (53.25-57.00) | 0.565† |
| Foveal avscular zone (FAZ) parameters | |||
| FAZ area (mm2) | 0.30±1.2 | 0.30±1.2 | 0.777* |
| FAZ perimeter (mm) | 2.11±0.43 | 2.12±0.44 | 0.365* |
| FD-300 | 56.48 (54.10-59.77) | 56.66 (54.07-59.15) | 0.860† |
wiVD: whole image vessel density, para: parafovea, peri: perifovea, sup hemi: superior hemifield, inf hemi: inferior hemifield, wpVD: whole papillary vessel density, İVD: inside disk vessel density, ppVD: peripapillary vessel density, FD: FAZ density. *Student t-test was used for comparison, †Mann-Whitney U test used for comparisons
Figure 5.
The boxplot analysis representing foveal vessel density changes in the study and placebo group after drug intake. (SFov.VD: superficial fovea vessel density, DFov.VD: deep fovea vessel density)
Figure 6.
The boxplot analysis representing vessel density changes in the macular and radial peripapillary region in study and placebo group after drug intake. (SPara.VD: superficial parafovea vessel density, SPeri.VD: superficial perifovea vessel density, DPara.VD: deep parafovea vessel density, DPeri.VD: deep perifovea vessel density, FD: density, wpVD: whole peripapillary vessel density, iVD: inside disc vessel density, ppVDav: peripapillary vessel density average)
Correlations of vessel density parameters
Correlations between percent change in superficial and deep macular vessel density and FAZ density parameters in the study group 1 h after caffeine intake are presented in Table 5. Positive correlations were seen between superficial and deep wiVD, sup hemi VD, and inf hemi VD (r value ranges from 0.364 to 0.452, P < 0.00 1 for all). Superficial perifovea VD was correlated with deep perifovea VD (r = 0.384, P = 0.002). All macular superficial vessel density parameters showed a positive correlation with deep perifovea VD (P < 0.05, for all). Also, superficial perifovea VD was correlated with all deep macular vessel density parameters except deep fovea VD (P < 0.05, for all).
Table 5.
Correlations between percent change in radial peripapillary capillary vessel density parameters and change in macular parameters of caffeine group after caffeine intake
| Swi VD | Ssuphem VD | Sinfhemi VD | SFov.VD | SPara.VD | SPeri.VD | Dwi VD | Dsuphemi VD | Dinfhemi VD | DFov.VD | DPara.VD | DPeri.VD | FD | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| wpVD | 0.206 | 0.139 | 0.203 | 0.358† | 0.245 | 0.212 | 0.301* | 0.271* | 0.168 | 0.151 | 0.099 | 0.340† | 0.021 |
| iVD | 0.025 | −0.075 | −0.076 | 0.024 | 0.058 | 0.010 | 0.160 | 0.133 | −0.025 | 0.093 | 0.100 | 0.118 | 0.002 |
| ppVDav | 0.147 | 0.091 | 0.136 | 0.247 | 0.243 | 0.108 | 0.290* | 0.198 | 0.113 | 0.210 | 0.262* | 0.323* | −0.010 |
| ppVDsh | −0.085 | −0.071 | −0.076 | 0.119 | 0.083 | −0.049 | 0.207 | 0.227 | −0.030 | 0.251 | 0.198 | 0.231 | −0.052 |
| ppVDih | 0.259* | 0.194 | 0.259* | 0.268* | 0.354† | 0.230 | 0.260* | 0.175 | 0.139 | 0.119 | 0.131 | 0.251 | 0.080 |
| ppVDsup | −0.069 | −0.104 | −0.003 | 0.159 | −0.058 | −0.055 | 0.160 | 0.150 | −0.048 | 0.310* | 0.078 | 0.168 | 0.057 |
| ppVDnas | 0.109 | 0.032 | −0.015 | −0.001 | 0.174 | 0.102 | 0.159 | 0.141 | 0.001 | 0.046 | 0.156 | 0.200 | 0.019 |
| ppVDinf | 0.093 | 0.071 | 0.154 | 0.129 | 0.182 | 0.056 | 0.210 | 0.147 | 0.135 | 0.204 | 0.181 | 0.238 | −0.004 |
| ppVDtemp | −0.085 | −0.158 | −0.046 | 0.147 | −0.014 | −0.105 | 0.046 | 0.149 | −0.095 | -0.066 | 0.020 | 0.060 | −0.202 |
SwiVD: superficial whole image vessel density, SsuphemVD: superficial superior hemifield vessel density, SinfhemVD: superficial inferior hemifield vessel density, SFov.VD: superficial fovea vessel density, SPara.VD: superficial parafovea vessel density, SPeri.VD: superficial perifovea vessel density, DwiVD: deep whole image vessel density, DsuphemVD: deep superior hemifield vessel density, DinfhemVD: deep inferior hemifield vessel density, DFov.VD: Deep fovea vessel density, DPara.VD: deep parafovea vessel density, Peri.VD: perifovea vessel density, FD: FAZ density, wpVD: whole peripapillary vessel density, iVD: inside disc vessel density, ppVDav: peripapillary vessel density average, ppVDsh: peripapillary vessel density superior hemifield, ppVDih: peripapillary vessel density inferior hemifield, ppVDsup: peripapillary vessel density superior, ppVDnas: peripapillary vessel density nasal, ppVDinf: peripapillary vessel density inferior, ppVDtemp: peripapillary vessel density temporal. SDS: Standard deviation score *Significant correlations were written in bold in the submitted form of table 5 and 6 as table 1. May be they were written in bold
Correlations between percent change in RPC VD parameters and change in macular parameters of study group 1 h after caffeine intake are presented in Table 6. wpVD was correlated with superficial fovea VD (P < 0.01), deep wiVD (P < 0.05), deep sup hemi VD (P < 0.05), and deep perifovea VD (P < 0.01). ppVD average showed a positive correlation with deep wiVD, deep parafovea VD, and deep perifovea VD (P < 0.05, for all). ppVD inf hemi was positively correlated with superficial wiVD (P < 0.05), superficial inf hemi VD (P < 0.05), superficial fovea VD (P < 0.05), superficial parafovea VD (P < 0.01), and deep wiVD (P < 0.05) macular vessel density parameters. A positive correlation was found between ppVD sup and deep fovea VD (r = 0.310, P = 0.016).
Table 6.
Correlations between percent change in superficial and deep macular vessel density and foveal avascular zone density parameters of caffeine group 1 h after caffeine intake
| DwiVD | DsuphemVD | DinfhemVD | DFov.VD | DPara.VD | DPeri.VD | FD | |
|---|---|---|---|---|---|---|---|
| SwiVD | 0.407† | 0.355† | 0.452† | 0.166 | 0.209 | 0.409† | 0.244 |
| SsuphemVD | 0.364† | 0.347† | 0.399† | 0.147 | 0.173 | 0.329* | 0.221 |
| SinfhemVD | 0.427† | 0.407† | 0.400† | 0.294* | 0.210 | 0.420† | 0.225 |
| SFov.VD | 0.190 | 0.214 | 0.235 | 0.105 | 0.016 | 0.275* | 0.000 |
| SPara.VD | 0.350† | 0.291* | 0.336† | 0.061 | 0.215 | 0.383† | 0.124 |
| SPeri.VD | 0.442† | 0.353† | 0.485† | 0.187 | 0.277* | 0.384† | 0.248 |
| FD | 0.264* | 0.202 | 0.322* | 0.317* | -0.007 | 0.219 | 1.000 |
SwiVD: superficial whole image vessel density, SsuphemVD: superficial superior hemifield vessel density, SinfhemVD: superficial inferior hemifield vessel density, SFov.VD: superficial fovea vessel density, SPara.VD: superficial parafovea vessel density, SPeri.VD: superficial perifovea vessel density, FD: FAZ density, DwiVD: deep whole image vessel density, DsuphemVD: deep superior hemifield vessel density, DinfhemVD: deep inferior hemifield vessel density, DFov.VD: deep fovea vessel density, DPara.VD: deep parafovea vessel density, DPeri.VD: deep perifovea vessel density. SDS: Standard deviation score *Correlation is significant at the 0.05 level. †Correlation is significant at the 0.01 level
Discussion
Caffeine has a constrictive effect on vessels and increases peripheral vascular resistance with the adenosine receptor antagonist effect.[13] Studies have shown the effects of caffeine on blood flow in some areas of the human body. Acute elevation of systolic and diastolic blood pressure could be seen after caffeine ingestion. In a study, acute 75 mg of caffeine intake led to decreases in cerebral blood flow.[14] Abdel Wahed et al.[15] reported that caffeine causes significant changes in superior mesenteric artery blood flow measurements reflecting a significant reduction in perfusion in preterms. Also, Namdar et al.[16] concluded that caffeine impairs exercise-induced hyperaemic myocardial blood flow response in the study group.
Previous studies have demonstrated the effect of caffeine on retinal microcirculation. In a study performed in healthy participants using a laser speckle tissue analyzer, a 6% decrease in blood flow velocity was determined 60 min after oral caffeine intake.[10] Ozkan et al.[17] studied with color Doppler ultrasonography to evaluate the effect of 300-mg caffeine on the resistive index of the ophthalmic, central retinal, and posterior nasal ciliary artery. Resistive indexes of these arteries were significantly increased 1 h after caffeine ingestion. In the study conducted with 12 healthy subjects using the blue field stimulation technique, they showed a 13% decrease in retinal blood flow after 200-mg caffeine intake.[4]
In all studies mentioned above, none of the techniques used to assess ocular blood flow was sufficient to evaluate peripapillary and macular microcirculation with the desired precision. Also, none of them were used in regular clinical practice due to various limitations such as invasiveness, reliability, stability, reproducibility. With the introduction of OCTA, a very precise, rapid, high-resolution, and noninvasive evaluation of both the peripapillary and macular microcirculation was begun to be obtained in the retinal circulation. In a recent study, Karti et al.[18] used OCTA to assess the effect of caffeine on macular microcirculation. They concluded that caffeine decreases macular superficial, deep, and choriocapillaris flow area and vessel density in healthy subjects 1 h after caffeine intake. In the current study, additionally, we evaluated vascular parameters of the peripapillary area and possible changes of them after caffeine or placebo intake and compared them with macular parameters. We observed that 200-mg caffeine intake significantly decreased macular superficial and deep layer vessel density. Furthermore, the current study revealed uniquely that radial peripapillary capillary vessel density parameters using OCTA showed a significant decrease after caffeine intake in normal subjects in concordance with the change in blood flow in the previous studies.
Our current study further demonstrates that the decrease of macular superficial and deep vessel density after caffeine intake showed correlation with each other and also the change in radial peripapillary capillary vessel density parameters showed correlation with some of macular vessel density parameters. Especially, deep perifoveal vessel density showed correlation with all superficial macular vessel density parameters. Also, superficial perifoveal vessel density was correlated with all deep macular vessel density parameters except deep foveal vessel density. In the light of these findings, it may be possible to suggest that deep perifoveal vessel density may be used as the main reference parameter to estimate superficial macular parameters.
Studies examining the effect of caffeine on intraocular pressure have yielded different results with some studies noting an increase in IOP after caffeine intake,[6,7,19] others observing no change.[17,20,21] Avisar et al.[7] investigated the effect of 180-mg caffeine on subjects with normotensive glaucoma and ocular hypertension. Both groups were assessed at 30, 60, and 90 min after coffee intake. Both normotensive glaucoma patients and ocular hypertensive patients revealed a statistically significant increase in IOP. Adams and Brubaker[20] conducted a study regarding the change in aqueous humor flow after 400-mg caffeine intake. They reported that aqueous flow measured hourly from 1 to 4 h after the intake showed no significant difference. Also, IOP measured 4 h after caffeine intake revealed no statistically significant difference. In Ozkan et al.[17] study evaluating the effect of 300-mg caffeine on retrobulbar blood flow, they did not observe a statistically significant change in IOP after caffeine intake. The findings of this study support the studies like the latter one that do not show IOP change.
In studies observing the effect of caffeine intake on systolic and diastolic blood pressure, some investigators reported an increase in blood pressure,[4,6] others not.[10,17,20] In Papakonstantinou et al.[22] study focusing on acute effects of coffee consumption in healthy individuals, they concluded that coffee consumption significantly increased BP 3 h post-consumption, within the healthy physiological levels. Ajayi and Ukwade[6] measured IOP and blood pressure of the caffeinated coffee and decaffeinated coffee groups 0, 30, 60, and 90 min after the caffeine intake. An increase in SBP and DBP was noted in the caffeinated group and no change in blood pressure was noted in the control group. Ozkan et al.[17] measured systolic and diastolic blood pressure in healthy subjects 1 h after caffeine intake. No difference was observed in blood pressure values. In the current study, we also did not observe any change in systolic and diastolic blood pressure after caffeine intake.
Previous studies revealed that OCTA can quantify the layers of the retinal microvasculature with high intra-session repeatability and inter-session reproducibility.[23,24,25] The interobserver agreement was high for measurement of superficial whole macular VD [intraclass correlation coefficient 0.977 (95% confidence interval 0.871–0.993)]. Furthermore, evaluation of the control group at baseline and 1 h after placebo intake revealed no significant difference at all OCTA parameters. This finding also supports the intrasession repeatability in the previous studies and strengthens our results that decreased vessel density in the macula and peripapillary area was related to caffeine intake. Overall, the repeatability and reproducibility of quantitative assessment were in line with the previous studies. Moreover, the strengths of our study include exclusion of subjects using any medication, high-frequency caffeine consumers, and smokers. Also, measurement of the effect of caffeine on radial peripapillary vascular density and examination of the correlation of macular and peripapillary densities which were not performed in previous studies made our study more valuable.
The young median age and limited sample size of the study and placebo groups can be considered as limitations of our study. Another limitation was that there was not any study in the literature reporting deep perifoveal vascular density represents drug effect on superficial macular vessel density and thus, the results of our study could not be supported and compared. Further studies can be performed to evaluate the correlation of vessel density parameters with each other after drug intake.
Conclusion
In summary, our results provide clear evidence that caffeine administration also decreases peripapillary vessel densities in addition to macular densities in healthy volunteers, and correlations were observed between macular and peripapillary vessel density parameters. Future studies are needed to support the effect of caffeine on peripapillary vessel density and idea using deep perifoveal vessel density as the main parameter to estimate superficial macular parameters.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Local ethic committee registration number of this study is KAEK 11.4.
T.C. SAĞLIK BAKANLIĞI Türkiye İlaç ve Tıbbi Cihaz Kurumu Klinik Araştırma [20-AKD-118].
Informed consent
Informed consent was obtained from all individual participants included in the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1. Gilbert RM. Caffeine consumption. Prog Clin Biol Res. 1984;158:185–213. [PubMed] [Google Scholar]
- 2. Zengin MO, Cinar E, Karahan E, Tuncer I, Kucukerdonmez C. The effect of caffeine on choroidal thickness in young healthy subjects. Cutan Ocul Toxicol. 2015;34:112–6. doi: 10.3109/15569527.2014.912659. [DOI] [PubMed] [Google Scholar]
- 3. Daly JW, Fredholm BB. Caffeine--An atypical drug of dependence. Drug Alcohol Depend. 1998;51:199–206. doi: 10.1016/s0376-8716(98)00077-5. [DOI] [PubMed] [Google Scholar]
- 4. Lotfi K, Grunwald JE. The effect of caffeine on the human macular circulation. Invest Ophthalmol Vis Sci. 1991;32:3028–32. [PubMed] [Google Scholar]
- 5. Bunker ML, McWilliams M. Caffeine content of common beverages. J Am Diet Assoc. 1979;74:28–32. [PubMed] [Google Scholar]
- 6. Ajayi OB, Ukwade MT. Caffeine and intraocular pressure in a Nigerian population. J Glaucoma. 2001;10:25–31. doi: 10.1097/00061198-200102000-00006. [DOI] [PubMed] [Google Scholar]
- 7. Avisar R, Avisar E, Weinberger D. Effect of coffee consumption on intraocular pressure. Ann Pharmacother. 2002;36:992–5. doi: 10.1345/aph.1A279. [DOI] [PubMed] [Google Scholar]
- 8. Casiglia E, Bongiovì S, Paleari CD, Petucco S, Boni M, Colangeli G, et al. Haemodynamic effects of coffee and caffeine in normal volunteers:A placebo-controlled clinical study. J Intern Med. 1991;229:501–4. doi: 10.1111/j.1365-2796.1991.tb00385.x. [DOI] [PubMed] [Google Scholar]
- 9. Sasaki H, Hirasawa A, Washio T, Ogoh S. Acute effect of coffee drinking on dynamic cerebral autoregulation. Eur J Appl Physiol. 2016;116:879–84. doi: 10.1007/s00421-016-3345-7. [DOI] [PubMed] [Google Scholar]
- 10. Okuno T, Sugiyama T, Tominaga M, Kojima S, Ikeda T. Effects of caffeine on microcirculation of the human ocular fundus. Jpn J Ophthalmol. 2002;46:170–6. doi: 10.1016/s0021-5155(01)00498-1. [DOI] [PubMed] [Google Scholar]
- 11. Ross A, Ross AH, Mohamed Q. Review and update of central serous chorioretinopathy. Curr Opin Ophthalmol. 2011;22:166–73. doi: 10.1097/ICU.0b013e3283459826. [DOI] [PubMed] [Google Scholar]
- 12. Chansangpetch S, Lin SC. Optical coherence tomography angiography in glaucoma care. Curr Eye Res. 2018;43:1067–82. doi: 10.1080/02713683.2018.1475013. [DOI] [PubMed] [Google Scholar]
- 13. Smits P, Thien T, van't Laar A. Circulatory effects of coffee in relation to the pharmacokinetics of caffeine. Am J Cardiol. 1985;56:958–63. doi: 10.1016/0002-9149(85)90412-6. [DOI] [PubMed] [Google Scholar]
- 14. Kennedy DO, Haskell CF. Cerebral blood flow and behavioural effects of caffeine in habitual and non-habitual consumers of caffeine:A near infrared spectroscopy study. Biol Psychol. 2011;86:298–306. doi: 10.1016/j.biopsycho.2010.12.010. [DOI] [PubMed] [Google Scholar]
- 15. Abdel Wahed MA, Issa HM, Khafagy SM, Abdel Raouf SM. Effect of caffeine on superior mesenteric artery blood flow velocities in preterm neonates. J Matern Fetal Neonatal Med. 2019;32:357–61. doi: 10.1080/14767058.2017.1378337. [DOI] [PubMed] [Google Scholar]
- 16. Namdar M, Schepis T, Koepfli P, Gaemperli O, Siegrist PT, Grathwohl R, et al. Caffeine impairs myocardial blood flow response to physical exercise in patients with coronary artery disease as well as in age-matched controls. PLoS One. 2009;4:e5665. doi: 10.1371/journal.pone.0005665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ozkan B, Yüksel N, Anik Y, Altintas O, Demirci A, Cağlar Y. The effect of caffeine on retrobulbar hemodynamics. Curr Eye Res. 2008;33:804–9. doi: 10.1080/02713680802344708. [DOI] [PubMed] [Google Scholar]
- 18. Karti O, Zengin MO, Kerci SG, Ayhan Z, Kusbeci T. Acute effect of caffeine on macular microcirculation in healthy subjects:An optical coherence tomography angiography study. Retina. 2019;39:964–71. doi: 10.1097/IAE.0000000000002058. [DOI] [PubMed] [Google Scholar]
- 19. Okimi PH, Sportsman S, Pickard MR, Fritsche MB. Effects of caffeinated coffee on intraocular pressure. Appl Nurs Res. 1991;4:72–6. doi: 10.1016/s0897-1897(05)80058-8. [DOI] [PubMed] [Google Scholar]
- 20. Adams BA, Brubaker RF. Caffeine has no clinically significant effect on aqueous humor flow in the normal human eye. Ophthalmology. 1990;97:1030–1. doi: 10.1016/s0161-6420(90)32468-5. [DOI] [PubMed] [Google Scholar]
- 21. Chandrasekaran S, Rochtchina E, Mitchell P. Effects of caffeine on intraocular pressure:The Blue Mountains eye study. J Glaucoma. 2005;14:504–507. doi: 10.1097/01.ijg.0000184832.08783.be. [DOI] [PubMed] [Google Scholar]
- 22. Papakonstantinou E, Kechribari I, Sotirakoglou K, Tarantilis P, Gourdomichali T, Michas G, et al. Acute effects of coffee consumption on self-reported gastrointestinal symptoms, blood pressure and stress indices in healthy individuals. Nutr J. 2016;15:26. doi: 10.1186/s12937-016-0146-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Mihailovic N, Brand C, Lahme L, Schubert F, Bormann E, Eter N, et al. Repeatability, reproducibility and agreement of foveal avascular zone measurements using three different optical coherence tomography angiography devices. PLoS One. 2018;13:e0206045. doi: 10.1371/journal.pone.0206045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Lei J, Durbin MK, Shi Y, Uji A, Balasubramanian S, Baghdasaryan E, et al. Repeatability and reproducibility of superficial macular retinal vessel density measurements using optical coherence tomography angiography en face images. JAMA Ophthalmol. 2017;135:1092–8. doi: 10.1001/jamaophthalmol.2017.3431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lee JC, Grisafe DJ, Burkemper B, Chang BR, Zhou X, Chu Z, et al. Intrasession repeatability and intersession reproducibility of peripapillary OCTA vessel parameters in non-glaucomatous and glaucomatous eyes. Br J Ophthalmol. 2021;105:1534–41. doi: 10.1136/bjophthalmol-2020-317181. [DOI] [PMC free article] [PubMed] [Google Scholar]