Introduction
Anxiety and depressive disorders pose significant public health issues across the world. Depression and other depressive disorders are mental illnesses characterised by a profound and persistent feeling of sadness or despair and a loss of interest in formerly pleasurable activities. Disturbances in sleep, appetite and cognitive processes are common symptoms. Globally, 5% of adults are estimated to suffer from the disorder.1 Anxiety disorder is a chronic condition characterised by excessive and persistent apprehension, with physical symptoms such as sweating, palpitations, feelings of stress and increased blood pressure. Baxter and colleagues’ meta-analysis of 87 studies from 44 countries indicated that the global prevalence of this disorder has fluctuated between 0.9% and 28.3%.2 3 These prevalent and debilitating mental disorders can seriously impact daily life, including school performance, work productivity, family and friend interpersonal relationships, and community participation.4 5 Many studies also show strong relationships between these disorders and physical health problems such as tuberculosis, cardiovascular disease, disturbed concentration, sleep disorder and appetite.6–9 Individuals from all countries—young and old, rich and poor—suffer from these conditions. Previous research findings indicate that women, persons with higher education, and urban-dwelling individuals are more likely to have depression and anxiety than men, illiterate individuals, and villagers living in rural communities.10 11
Despite the increased international focus on mental health-related problems and their explicit mention in the World Health Organization (WHO) New Health Plan 2010, many aspects of mental disorders have not been thoroughly investigated. Although the aetiology of these mood disorders has been examined extensively at the individual level in various kinds of research, the population-level characteristics have not received as much attention, including socioeconomic aspects.12 Therefore, this study aimed to evaluate the relationship between the Human Development Index (HDI) elements—life expectancy at birth, education and gross national income per 1000 capita—and anxiety and depressive disorder prevalence worldwide.
Materials and methods
This ecological study examined the prevalence of anxiety and depression in 181 countries based on the 2019 HDI ranking. The HDI is a mathematical index applied to estimate a country’s overall success in social and economic dimensions. HDI includes several primary measures: life expectancy at birth, mean years of education and gross national income per capita. The value of this index is between 0 and 1. The closer it is to 1, the higher the level of development. Our research compiled the countries’ HDI scores to classify their socioeconomic status.13
We first gathered data about anxiety and depression prevalence from the 181 countries or territories listed in the 2019 WHO database (https://www.who.int/health-topics/depression).1 Next, we collected the HDI-2019 data for the 181 listed countries from the World Bank website (https://databank.worldbank.org/Human-development-index). Our analysis included only those countries for which data about anxiety and depressive disorders and HDI were available.
The relative concentration index (RCI) was used to measure socioeconomic inequality in the prevalence of anxiety and depressive disorders. The RCI is a relative index derived from a concentration curve (CC), which measures socioeconomic inequality in ordinal variables and groups. For example, in the CC, the proportion of anxiety and depressive disorder prevalence (y-axis) was plotted against the cumulative proportion of the population ranked by the HDI (x-axis). The CC begins with the lowest HDI levels on the left and ends with the highest HDI levels on the right. This relative measure ranges from +1 (depression and anxiety wholly concentrated among countries with high HDI) to −1 (depression and anxiety wholly concentrated among countries with low HDI). The 0 value in this index indicates the absence of inequality. When the RCI equals 0, there is no socioeconomic inequality in the anxiety and depression prevalence across countries with different levels of HDI. When the CC rises over the diagonal, the RCI is negative, indicating the outcome is concentrated between countries with low levels of HDI. When the CC falls under the diagonal line, the RCI is positive, indicating the outcome is disproportionately concentrated among countries with higher levels of HDI.14 A linear regression model was used to investigate the relationship between HDI and the prevalence of anxiety and depression. In the regression model, the β coefficient is the degree of decrease or increase in anxiety and depressive disorder prevalence for every 1 unit increase in the HDI level. The level of 0.05 was considered statistically significant. Data were analysed using Stata software V.16.
Results
The association of HDI and its components with anxiety and depression prevalence was assessed by a linear regression model and presented in table 1. This model indicated that the prevalence of anxiety and depressive disorders significantly increased as life expectancy at birth, mean years of education, gross national income and HDI level increased (all p-values<0.05). The scatter plots displayed in figure 1 showed the positive relationship between the countries’ HDI rankings and anxiety and depressive disorder prevalence, indicating the tendency for higher prevalence of these mental disorders in countries with higher HDI rankings.
Table 1.
The association between anxiety and depressive disorder prevalence and the Human Development Index (HDI) and its components
| Variables | Anxiety prevalence | Depression prevalence | ||||
| β* | CI | P value | β* | CI | P value | |
| Life expectancy at birth | 0.82 | 0.60 to 1.03 | <0.001 | 0.46 | 0.31 to 0.62 | <0.001 |
| Mean years of education | 1.52 | 0.97 to 2.06 | <0.001 | 1.32 | 0.96 to 1.68 | <0.001 |
| Gross national income | 0.0001 | 0.00008 to 0.0003 | <0.001 | 0.0001 | 0.00004 to 0.00017 | 0.002 |
| HDI | 37.46 | 26.79 to 48.14 | <0.001 | 25.79 | 18.37 to 33.23 | <0.001 |
p<0.05=statistical significance.
*β coefficient=the degree of decrease or increase in anxiety and depressive disorder prevalence for every 1 unit increase in the HDI level.
Figure 1.
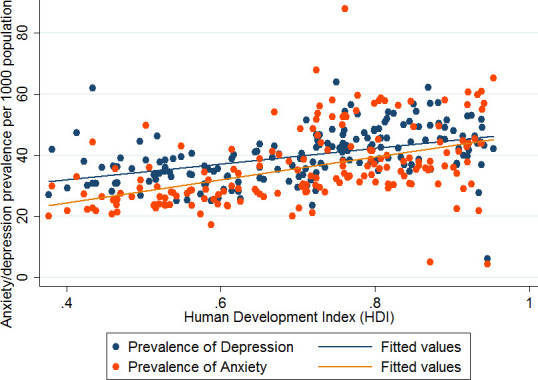
Scatter plots for the relationship between the Human Development Index (HDI) and anxiety/depressive disorder prevalence (0=lowest HDI; 1=highest HDI).
The CC results that examined socioeconomic disparity in the outcomes assessed in this research were shown in figure 2. In this figure, the horizontal axis represents the cumulative percentage of the countries ranked by HDI. A score of 0 indicates the lowest HDI rating, and a score of 1 indicates the highest HDI rating. The vertical axis indicates the percentage of anxiety and depression prevalence corresponding to the cumulative percentage of the HDI. The RCI and 95% CI were 0.43 (0.04 to 0.82) for anxiety disorder and 0.45 (0.03 to 0.86) for depressive disorder. The positive value of the RCI and the position of the CCs under the equity line indicated that anxiety and depression disorders are concentrated in countries with a high HDI ranking. According to figure 1, 20% of the world’s population that ranked lowest in HDI accounted for approximately 15% of anxiety and depressive disorders worldwide. On the other hand, 20% of the world’s population in the highest-ranked HDI accounted for more than 30% of these two disorders worldwide (ie, more than two times the prevalence of the low HDI countries). Alternatively, the poorest 30% of the world’s population accounted for 18% of global anxiety and depressive disorders.
Figure 2.
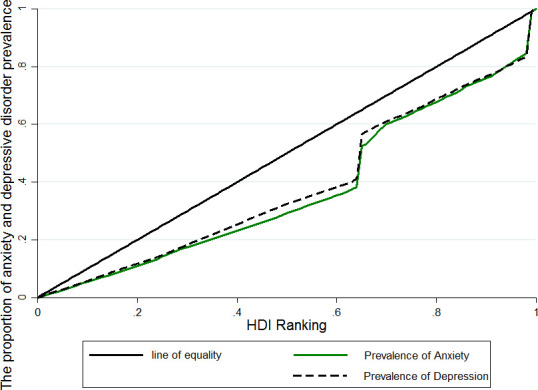
Concentration curve for measuring socioeconomic inequality in the prevalence of anxiety and depressive disorders ranked by Human Development Index (HDI) cumulative percentage of the countries worldwide.
Discussion
This ecological study was conducted to assess socioeconomic inequality in anxiety and depressive disorder prevalence based on HDI ranking. Our results indicated that the prevalence of anxiety and depressive disorders increased as HDI and its components increased. This disproportionately concentrated prevalence of anxiety and depressive disorders in regions with high HDI can be attributed to the high degree of accessibility to mental healthcare services and, consequently, the accurate recording of high rates of anxiety and depressive disorders. On the other hand, in countries with low HDI, the limited access to diagnostic services, screening tests for mental disorders, and medical care may lead to fewer documented cases of anxiety and depressive disorders. Moreover, most low-income and middle-income countries’ disease recording and reporting systems are imprecise, leading to the under-reporting of illnesses, especially those disorders such as mental illness, which are socially stigmatised.15 16
Life expectancy at birth is one of the measures of HDI. Increased life expectancy in a society indicates an increase in the elderly population. Numerous research studies have reported a higher incidence and prevalence of anxiety and depressive disorders among the ageing population. In older people, chronic diseases, various infections, psychosocial problems, economic poverty, disability, isolation, and deprivation increase the susceptibility to depression and anxiety in already vulnerable older adults.17
The results from the linear regression model indicated that an increase in the mean years of education led to a rise in the prevalence of anxiety and depressive disorders. We can justify this finding by saying that the prevalence rate may increase with increasing health knowledge, awareness of initial signs of the disease and early detection.18
There were some limitations in this study. First, exposure is measured at an aggregate level, so we must be careful to interpret the results on the aggregate level, not at the individual level, to avoid ecological fallacies.19 The second limitation is the shortcoming of not measuring the impact of confounding variables in this study. Due to these limitations, this study’s results cannot be used for causal relationships, but they can guide hypotheses. The third limitation was the lack of access to sex and age data; thus, we could not adjust the RCI based on these variables. However, the most important strength of this study was that it was conducted at the global level and analysed information from more than 90% of the world’s countries.
Conclusion
This study showed that the prevalence of anxiety and depressive disorders is mainly concentrated in countries with a higher level of HDI, which would indicate that these mental illnesses become more pervasive as the countries become more highly developed. However, the confounding relationship between socioeconomic inequality and the prevalence of these two mental disorders should be prioritised in further investigations and given special attention by global health policymakers to understand this conundrum better. Notably, the prevalence rates of anxiety and depressive disorders across developing countries suffer from under-reporting due to poor health education, difficulties in seeking healthcare, delayed identification of mental illness and misdiagnosis. In addition, the identification and reporting of anxiety and depressive disorders vary according to HDI levels because of the intense stigma attached to diagnostic labels and seeking mental healthcare in the poor HDI quintiles of the low-income and lower middle-income countries. In the future, individual-level studies designed with different analytical methodologies should be used for low-income and lower middle-income countries to more accurately measure the overall prevalence of mental disorders and their relationship to socioeconomic status.
Biography
Dr Fatemeh Shahbazi obtained a master degree in Epidemiology with honours from Shahid Beheshti University of Medical Sciences in Iran in 2018. Her basic education was in public health from Arak University of Medical Sciences in Iran. She is currently a PhD candidate in Epidemiology in the College of Public Health at Hamadan University of Medical Sciences, Hamadan, Iran. In 2022, she was recognized as a top research student in the country. Her main research interests include social epidemiology, types of meta-analysis, prediction models, and research of non-communicable diseases.
Footnotes
Contributors: FS contributed to the study concept and design, acquisition, analysis and interpretation of data, and to drafting of the manuscript. JP contributed to the study concept and design and revising the manuscript. MS contributed to data preparation and preparation of the first draft of the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
This research did not involve direct human participants; the data were extracted from the WHO website and the World Bank dataset.
References
- 1.World Health Organization . Comprehensive mental health action plan 2013-2030, 2022. World Health Organization. Available: https://www.who.int/health-topics/depression#tab=tab_1
- 2.Baker A, Simon N, Keshaviah A, et al. Anxiety symptoms questionnaire (ASQ): development and validation. Gen Psychiatr 2019;32:e100144. 10.1136/gpsych-2019-100144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baxter AJ, Scott KM, Vos T, et al. Global prevalence of anxiety disorders: a systematic review and meta-regression. Psychol Med 2013;43:897–910. 10.1017/S003329171200147X [DOI] [PubMed] [Google Scholar]
- 4.Alenko A, Girma S, Abera M, et al. Children emotional and behavioural problems and its association with maternal depression in Jimma town, southwest Ethiopia. Gen Psychiatr 2020;33:e100211. 10.1136/gpsych-2020-100211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McLaughlin KA. The public health impact of major depression: a call for interdisciplinary prevention efforts. Prev Sci 2011;12:361–71. 10.1007/s11121-011-0231-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vadher S, Desai R, Panchal B, et al. Burden of care in caregivers of patients with alcohol use disorder and schizophrenia and its association with anxiety, depression and quality of life. Gen Psychiatr 2020;33:e100215. 10.1136/gpsych-2020-100215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim JA, Choi S, Choi D, et al. Pre-existing depression among newly diagnosed dyslipidemia patients and cardiovascular disease risk. Diabetes Metab J 2020;44:307–15. 10.4093/dmj.2019.0002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Molla A, Mekuriaw B, Kerebih H. Depression and associated factors among patients with tuberculosis in Ethiopia: a cross-sectional study. Neuropsychiatr Dis Treat 2019;15:15. 10.2147/NDT.S208361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Oh KH, Choi H, Kim EJ, et al. Depression and risk of tuberculosis: a nationwide population-based cohort study. Int J Tuberc Lung Dis 2017;21:804–9. 10.5588/ijtld.17.0038 [DOI] [PubMed] [Google Scholar]
- 10.Geerlings MI, Schoevers RA, Beekman AT, et al. Depression and risk of cognitive decline and Alzheimer's disease. Results of two prospective community-based studies in the Netherlands. Br J Psychiatry 2000;176:568–75. 10.1192/bjp.176.6.568 [DOI] [PubMed] [Google Scholar]
- 11.Husain N, Gater R, Tomenson B, et al. Social factors associated with chronic depression among a population-based sample of women in rural Pakistan. Soc Psychiatry Psychiatr Epidemiol 2004;39:618–24. 10.1007/s00127-004-0781-1 [DOI] [PubMed] [Google Scholar]
- 12.Ben-Zeev D, Young MA, Corrigan PW. DSM-V and the stigma of mental illness. J Ment Health 2010;19:318–27. 10.3109/09638237.2010.492484 [DOI] [PubMed] [Google Scholar]
- 13.Watson D. Rethinking the mood and anxiety disorders: a quantitative hierarchical model for DSM-V. J Abnorm Psychol 2005;114:522–36. 10.1037/0021-843X.114.4.522 [DOI] [PubMed] [Google Scholar]
- 14.Shahbazi F, Khazaei S. Socioeconomic inequality in global incidence and mortality rates from coronavirus disease 2019: an ecological study. New Microbes New Infect 2020;38:100762. 10.1016/j.nmni.2020.100762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Henkelmann J-R, de Best S, Deckers C, et al. Anxiety, depression and post-traumatic stress disorder in refugees resettling in high-income countries: systematic review and meta-analysis. BJPsych Open 2020;6:e68. 10.1192/bjo.2020.54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Uthman OA, Magidson JF, Safren SA, et al. Depression and adherence to antiretroviral therapy in low-, middle- and high-income countries: a systematic review and meta-analysis. Curr HIV/AIDS Rep 2014;11:291–307. 10.1007/s11904-014-0220-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Alexopoulos GS. Depression in the elderly. The Lancet 2005;365:1961–70. 10.1016/S0140-6736(05)66665-2 [DOI] [PubMed] [Google Scholar]
- 18.Pinto-Foltz MD, Logsdon MC, Myers JA. Feasibility, acceptability, and initial efficacy of a knowledge-contact program to reduce mental illness stigma and improve mental health literacy in adolescents. Soc Sci Med 2011;72:2011–9. 10.1016/j.socscimed.2011.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Szklo M, Nieto FJ. Basic study designs in analytical epidemiology, in epidemiology beyond the basic. United States of America: Jones & bartlett learning publisher, 2019. [Google Scholar]


