Abstract
Swellings in medial canthal area in eye most often involve the lacrimal sac, the commonest aetiology being chronic dacryocystitis. Very rarely, there is a deviation in the routine diagnosis when the pathology comes out to be a lacrimal sac tumour. We report the case of a young man who presented with a medial canthal mass not extending above the medial canthal ligament. The clinical presentation was typical for a lacrimal sac mucocele, however on histopathological evaluation was diagnosed as a rare case of solitary fibrous tumour of lacrimal sac. We recommend radiological investigation in medial canthal masses where there is negative regurgitation on pressure over lacrimal sac area to avoid misdiagnoses.
Keywords: Ophthalmology, Pathology, Surgical oncology
Background
Solitary fibrous tumours are mesenchymal neoplasms first described in pleura and mediastinum. They are rarely seen in orbit and lacrimal apparatus accounting for just seven cases reported in the literature. Owing to their clinical and radiological findings similar to that of lacrimal sac mucoceles, they can readily be mistaken for chronic dacryocystitis and its sequelae. Complete excision and histopathological correlation are the primary modality of treatment of these lesions. Careful follow-up is necessary for averting recurrence.
Case presentation
A young man in his 30s presented to our ophthalmology clinic with chief reports of epiphora and watery discharge from his left eye for 1-year duration. It was associated with off and on swelling in the lacrimal sac area below the medial canthal ligament. He gave a history of regurgitation of mucoid material on compression of the lacrimal sac lately but the present episode showed negative regurgitation test. The swelling was non-tender, firm in consistency, smooth with well-defined margins without any erythema, pulsation or fluid thrill (figure 1). Right eye examination was within normal limits. There was no similar history in the past, nor any remarkable previous medical or surgical history. He was a teacher by profession, belonging to medium socioeconomic background.
Figure 1.

Clinical photograph showing left-sided lacrimal sac swelling with well-defined margins and healthy overlying skin of size 2×1×2 centimetres.
Based on the above clinical findings, our provisional diagnosis was lacrimal sac retention mucocele of left side. Contrast-enhanced CT of orbits and paranasal sinuses was requested to rule out lacrimal sac mass, nasal polyps or sinusitis.
Investigations
Contrast-enhanced CT scan of orbit showed an enlarged lacrimal sac extending into the nasolacrimal duct, without any bony erosion (figure 2). The clinical and radiological findings were consistent with mucocele of the lacrimal sac precluding any tumour pathology. Routine preoperative blood investigations were carried out for planning dacryocystorhinostomy.
Figure 2.

Contrast-enhanced CT scan of orbit showed an enlarged lacrimal sac extending into the nasolacrimal duct, without any bony erosion.
Treatment
We proceeded to perform dacryocystorhinostomy with insertion of Crawford tube. During the surgical step of fashioning of sac flaps, to our utter surprise, we could visualise a mass with smooth margins involving whole of the sac with a small conical extension into the nasolacrimal duct. We were in a dilemma whether to continue with the osteotomy and complete the mucosal anastomosis. However, we decided to excise the mass in toto, send for histopathology and wait for the reports. The mass was well circumscribed of size of 2.5×2.4×1.2 cm, highly vascular, reddish colour, solid and firm in consistency (figure 3). The dacryocystectomy specimen containing the mass was sent for histopathological examination.
Figure 3.
Excised lacrimal sac mass of size of 2.5×2.4×1.2 centimetres, solid, well circumscribed, highly vascular, reddish colour and firm in consistency.
Outcome and follow-up
The patient did well after en-bloc excision of the tumour. Histopathological examination revealed capsulated tumour with cellular neoplasm composed of spindloid to oval cells with mild degree of nuclear atypia arranged in sheets and fascicular pattern suggestive of solitary fibrous tumour of lacrimal sac (figure 4). Further immunohistochemistry (IHC) was suggested for better characterisation of tumour. IHC showed strong cytoplasmic and membranous positivity for CD34 (figure 5A), CD99, STAT-6, BCL-2 and weak to moderate positivity for smooth muscle actin (SMA). The tumour cells were negative for S-100, TLE-1, CD117, DOG-1 and EMA. The MIB-1 labelling index (K-67) was 10% (figure 5B). As the K-67 index was higher than average, we advised him for adjuvant radiation therapy. External beam radiation therapy was advised for 60 grey in 30 fractions over 6 weeks, but the patient deferred any further treatment and opted for watchful observation. He was advised for follow-up clinically every 3 months and with MRI yearly to look for any recurrence. He is on regular follow-up with us for last 3 years without any reports of epiphora and rerecurrence.
Figure 4.
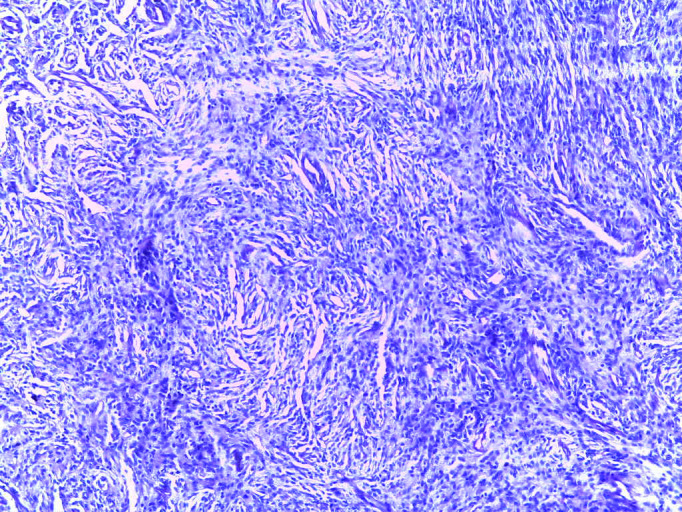
Histopathology showing cellular neoplasm composed of spindloid to oval cells with mild degree of nuclear atypia arranged in sheets and fascicular pattern.
Figure 5.
(A) Immunohistochemical staining showing strong positivity for CD34. (B) MIB-1 pattern.
Discussion
Lacrimal sac tumours are rare with only 775 cases reported worldwide.1 In a case series of acquired dacryocystoceles, Bothra et al have described just five cases over 5-year period in which they found only one case of solitary fibrous tumour of lacrimal sac.2 Kuo CY et al, in their retrospective case series over a period of 23 years, found 65 cases of lacrimal sac tumours, out of which 70% were benign and 30% were malignant.3
Lacrimal sac tumours are classified as epithelial (75%) or non-epithelial (25%).4 5 Benign epithelial tumours (papilloma, oncocytoma, adenoma and cylindromas) arise from pre-existing inflammation while malignant epithelial tumours (squamous cell carcinoma, transitional cell carcinoma, oncocytic adenocarcinoma) arise de novo. Non-epithelial tumours are divided into lymphoproliferative, melanocytic and mesenchymal tumours. The last variant of mesenchymal tumours comprises 12%–14% of lacrimal sac tumours.6–8 Benign mesenchymal tumours include fibrous histiocytoma (most common), fibroma, solitary fibrous tumour, haemangioma, haemangiopericytoma, angiofibroma, lipoma and leiomyoma. Malignant mesenchymal tumours of the lacrimal sac include Kaposi sarcoma and rhabdomyosarcoma.9–12
Clinical presentation mimics chronic dacryocystitis and complete ophthalmic examination, including lacrimal probing and syringing should be done. Per nasal evaluation should also be performed in all cases of chronic dacryocystitis to rule out any deviated nasal septum and nasal polyps. Our patient had similar reports of epiphora and swelling at medial canthal mass. The important differentiating feature from encephalocele/dermoid cyst/any other soft tissue mass is that the extension of the mass should not cross above the medial canthal ligament. The swelling at medial canthus in our patient was also below medial canthal ligament, hence we did not suspect any tumour pathology; however, we did a CT scan to confirm our findings which again showed deceptive findings. CT scan of the orbit and paranasal sinuses help to identify bony invasion while MRI delineates soft tissue infiltration better. Moriyama et al have suggested an endoscopic-modified medial maxillectomy for a solitary fibrous tumour of lacrimal sac with extension to the nasolacrimal duct.13 Other diagnostic modalities like CT dacryocystography shows lacrimal sac filling defect, however does not delineate soft tissue well.14–16 Ultrasonography with Doppler has also been suggested a diagnostic modality in a case report by Kurdi et al.17
We do not recommend aspiration prior to giving surgical incision in such cases of suspicious lacrimal sac swellings since they may underlie a tumour and accidental haemorrhage, infection can occur. Instead, they should be carefully explored intraoperatively to rule out any tumour pathology and then proceed with dacryocystectomy whenever indicated and sent for histopathological evaluation.
Solitary fibrous tumours are composed of clusters of spindle to oval-shaped cells admixed with collagen bands around a prominent vasculature. Similar histopathology can be seen in haemangiopericytoma, neural tumours, smooth muscle tumours, fibrous histiocytoma and nodular fasciitis, which can be differentiated by the typical immunohistochemical staining pattern for vimentin, BCL-2 and CD-34. Our patient showed strong positivity for CD34, CD99, STAT-6, BCL-2 and negative for S-100, TLE-1, CD117, DOG-1 and EMA due to which helped in ruling out other pathologies. Ten to fifteen percent of cases are aggressive in nature and characterised by hypercellularity, high mitoses.17 18 Our patient had a MIB 1 index of 10%, which suggested aggressive pathology and, therefore, we advised him for adjuvant radiotherapy. Favourable prognostic factors include early-stage tumour, benign characterisation on histopathology, short duration and early intervention with complete excision of tumour mass. Poor prognostic factors include malignant transformation, incomplete excision and bony invasion. Long-term follow-up is necessary to check for recurrence.
Patient’s perspective.
I am very much indebted to the chief oculoplastic surgeon who did a wise and early decision to operate on my tumour. She had explained to me very clearly about the aggressiveness of the tumour and advised further treatment with radiation therapy. I am in constant follow-up with her for the last 3 years without any recurrence of symptoms.
Learning points.
Solitary fibrous tumour of lacrimal sac is a very rare tumour and can mimic chronic dacryocystitis.
Radiological imaging should be done in lacrimal swellings, which show negative result on regurgitation, even if they do not extend beyond medial palpebral ligament.
Complete excision of the tumour is mandatory and histopathological confirmation with immunohistochemical staining always clinch to the diagnosis.
Long-term follow-up is advisable to prevent recurrence.
Acknowledgments
We acknowledge Dr. Ashok Kumar Nanda, Medical director of Kar Vision eye Hospital, Bhubaneswar who helped in the patient care.
Footnotes
Contributors: BP, SV designed the study, drafted the manuscript, BP revised the manuscript. MB provided scientific contribution and SR contributed to the initial drafting of the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Case reports provide a valuable learning resource for the scientific community and can indicate areas of interest for future research. They should not be used in isolation to guide treatment choices or public health policy.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Consent obtained directly from patient(s)
References
- 1.Krishna Y, Coupland SE. Lacrimal Sac Tumors-A Review. Asia Pac J Ophthalmol 2017;6:173–8. 10.22608/APO.201713 [DOI] [PubMed] [Google Scholar]
- 2.Bothra N, Wagh RD, Ali MJ. Masquerades of acquired Dacryocystocele. Clin Ophthalmol 2020;14:1855–8. 10.2147/OPTH.S261098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kuo C-Y, Tsai C-C, Kao S-C, et al. Comparison of clinical features and treatment outcome in benign and malignant lacrimal sac tumors. Biomed Res Int 2020;2020:3545839 10.1155/2020/3545839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Flanagan JC, Stokes DP. Lacrimal sac tumors. Ophthalmology 1978;85:1282–7. 10.1016/S0161-6420(78)35554-8 [DOI] [PubMed] [Google Scholar]
- 5.Pe'er JJ, Stefanyszyn M, Hidayat AA. Nonepithelial tumors of the lacrimal sac. Am J Ophthalmol 1994;118:650–8. 10.1016/S0002-9394(14)76580-8 [DOI] [PubMed] [Google Scholar]
- 6.Ashton N, Choyce DP, Fison LG. Carcinoma of the lacrimal sac. Br J Ophthalmol 1951;35:366–76. 10.1136/bjo.35.6.366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Radnót M, Gáll J. [Tumors of the lacrimal sac]. Ophthalmologica 1966;151:2–22. [PubMed] [Google Scholar]
- 8.Stefanyszyn MA, Hidayat AA, Pe'er JJ, et al. Lacrimal sac tumors. Ophthalmic Plast Reconstr Surg 1994;10:169–84. 10.1097/00002341-199409000-00005 [DOI] [PubMed] [Google Scholar]
- 9.YW B, Chen RJ, XP L. Clinical and pathological analysis of primary lacrimal sac tumors. Zhonghua Yan Ke Za Zhi 2007;43:499–504. [PubMed] [Google Scholar]
- 10.Kishimoto I, Shinohara S, Fujiwara K, et al. [A case of intraorbital solitary fibrous tumor resected successfully with preoperative arterial embolization]. Nihon Jibiinkoka Gakkai Kaiho 2014;117:1477–82. 10.3950/jibiinkoka.117.1477 [DOI] [PubMed] [Google Scholar]
- 11.Pe'er JJ, Stefanyszyn M, Hidayat AA. Nonepithelial tumors of the lacrimal sac. Am J Ophthalmol 1994;118:650–8. 10.1016/S0002-9394(14)76580-8 [DOI] [PubMed] [Google Scholar]
- 12.Anderson NG, Wojno TH, Grossniklaus HE. Clinicopathologic findings from lacrimal sac biopsy specimens obtained during dacryocystorhinostomy. Ophthalmic Plast Reconstr Surg 2003;19:173–6. 10.1097/01.IOP.0000066646.59045.5A [DOI] [PubMed] [Google Scholar]
- 13.Moriyama M, Kodama S, Hirano T, et al. Endoscopic-modified medial maxillectomy and its limitation for a solitary fibrous tumor of the lacrimal sac and nasolacrimal duct. Auris Nasus Larynx 2017;44:370–4. 10.1016/j.anl.2016.07.010 [DOI] [PubMed] [Google Scholar]
- 14.Kim HJ, Shields CL, Langer PD. Lacrimal sac tumors: diagnosis and treatment. In: Black EH, Nesi FA, Cavana CJ, eds. Smith and Nesi’s Ophthalmic Plastic and Reconstructive Surgery. New York: Springer, 2012: 609–14. [Google Scholar]
- 15.Bi Y-W, Chen R-J, Li X-P. [Clinical and pathological analysis of primary lacrimal sac tumors]. Zhonghua Yan Ke Za Zhi 2007;43:499–504. [PubMed] [Google Scholar]
- 16.Kim HJ, Kim H-J, Kim Y-D, et al. Solitary fibrous tumor of the orbit: CT and MR imaging findings. AJNR Am J Neuroradiol 2008;29:857–62. 10.3174/ajnr.A0961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kurdi M, Allen L, Wehrli B, et al. Solitary fibrous tumour of the lacrimal sac presenting with recurrent dacryocystitis. Can J Ophthalmol 2014;49:e108–10. 10.1016/j.jcjo.2014.05.011 [DOI] [PubMed] [Google Scholar]
- 18.Sciot R, Goffin J, Fossion E, et al. Solitary fibrous tumour of the orbit. Histopathology 1996;28:188–91. 10.1046/j.1365-2559.1996.284330.x [DOI] [PubMed] [Google Scholar]




