Abstract
Background
This study examined whether COVID‐19‐related maternal mental health changes contributed to changes in adolescent psychopathology.
Methods
A community sample of 226 adolescents (12 years old before COVID‐19) and their mothers were asked to complete COVID‐19 surveys early in the pandemic (April–May 2020, adolescents 14 years) and approximately 6 months later (November 2020–January 2021). Surveys assessed pandemic‐related stressors (health, financial, social, school, environment) and mental health.
Results
Lower pre‐pandemic family income‐to‐needs ratio was associated with higher pre‐pandemic maternal mental health symptoms (anxiety, depression) and adolescent internalizing and externalizing problems, and with experiencing more pandemic‐related stressors. Pandemic‐related stressors predicted increases in maternal mental health symptoms, but not adolescent symptoms when other variables were covaried. Higher maternal mental health symptoms predicted concurrent increases in adolescent internalizing and externalizing. Maternal mental health mediated the effects of pre‐pandemic income and pandemic‐related stressors on adolescent internalizing and externalizing problems.
Conclusions
Results indicate that adolescent mental health is closely tied to maternal mental health during community‐level stressors such as COVID‐19, and that pre‐existing family economic context and adolescent symptoms increase risk for elevations in symptoms of psychopathology.
Keywords: adolescent, internalizing, externalizing, maternal mental health, COVID‐19 pandemic
Introduction
The COVID‐19 pandemic resulted in families experiencing a range of unprecedented stressors, including disrupted structure and routine, increased health concerns, and financial loss (Gruber et al., 2020). Many families experienced restricted access to resources and support systems, and some families were faced with substantial financial difficulties due to containment measures, social distancing, and economic lockdown (Carroll et al., 2020; Fegert, Vitiello, Plener, & Clemens, 2020). For youth who were restricted from attending school and extra‐curricular activities, these containment measures limited their relationships with other adults and peers, potentially disrupting their social support networks. In this context of limited contact with sources of support outside of the home, the family context might have taken on relatively greater importance. Given that COVID‐19 pandemic‐related disruptions are known to have resulted in increased mental health problems in children and adolescents (Calvano et al., 2021; Gruber et al., 2020; Racine, McArthur, et al., 2021), it is critical to understand the factors that contributed to increased risk. This study examined the extent to which maternal mental health symptoms accounted for the effects of pandemic‐related stressors on adolescent psychopathology.
Children and adolescents have demonstrated elevated levels of anxiety and depression since the COVID‐19 outbreak (Magson et al., 2021; Racine, McArthur, et al., 2021; Wright, Hill, Sharp, & Pickles, 2021). Understanding factors that contribute to the effects of the COVID‐19 pandemic on youth’s psychopathology is important and may inform intervention targets. In particular, family factors are critical to consider in relation to adolescent psychopathology during the pandemic. Youth were spending increased amounts of time with their families as a result of social distancing, and parents reported more frequent interactions with their children (Gadermann et al., 2021). These changes may heighten youth’s susceptibility to family and parental risk factors for adverse mental health, especially with limited access to social support and resources.
Maternal mental health is recognized as a central risk factor for children’s psychopathology (Goodman et al., 2011). Past research on natural or community level disasters (Green et al., 1991; Kerns et al., 2014; Kılıç, Kılıç, & Aydın, 2011), as well as research on the effects of the COVID‐19 pandemic (Russell, Tomkunas, Hutchison, Tambling, & Horton, 2021; Westrupp et al., 2021) suggest parental mental health and emotional reactions to such stressors are significant predictors of children’s adjustment response. If a parent reports more distress as a sequela to a disaster, the child is also likely to report more distress than parent–child dyads experiencing the same disaster who report lower levels of distress (Norris et al., 2002). These relations are observed even when children are less exposed to the disaster than their parents, highlighting the influence of caregiver mental health (Juth, Silver, Seyle, Widyatmoko, & Tan, 2015). In addition, research suggests that parental stress may mediate the relations of disaster experiences on children’s distress (Proctor et al., 2007) and predict the persistence of children’s emotional and behavioral problems after exposure to a disaster (Swenson et al., 1996).
With regard to the COVID‐19 pandemic, there is consistent evidence of elevated mental health problems among parents (e.g., Cameron et al., 2020; Racine, Eirich, et al., 2021), and that worsening parental mental health from prior to the pandemic to several months into it was shown to co‐occur with worsening behavioral health in children (Patrick et al., 2020), highlighting the importance of examining concurrent and prospective relations of symptoms across parents and children. For example, changes in maternal mental health during the pandemic predicted changes in young children’s adjustment (Thompson et al., 2022). Further, financial deprivation and prior mental health problems in both parents and children, along with pandemic‐related stressors, were associated with poorer parent and child functioning during the pandemic (Bryson et al., 2021; Westrupp et al., 2021). This study uniquely adds to this literature by examining not only the changes in both maternal and youth mental health from pre‐pandemic to early in the pandemic, but also across several months of the pandemic.
The COVID‐19 pandemic has had universal but not equivalent impacts across individuals and families (Calvano et al., 2021; Rosenfeld et al., 2021). It is clear that socioeconomic disadvantage increases the likelihood of mental health symptoms in general (Adler & Ostrove, 1999), during community level disasters (Purtle, 2012), and in particular, during the COVID‐19 pandemic (Fancourt, Steptoe, & Bu, 2021; Purtle, 2020). Factors such as household density, potential work exposure to the virus, job loss, as well as a family member’s infection, all of which are more prevalent among lower income families, correlated with symptoms of anxiety and depression during the COVID‐19 lockdown (Pakenham et al., 2020). Similarly, a cumulative risk index capturing parental job loss, income loss, increased caregiver burden, and household illness predicted parental mental health early in pandemic (Gassman‐Pines, Ananat, & Fitz‐Henley, 2020). These contexts may therefore account for increases in mental health symptoms during the pandemic. In one study examining maternal mental health in general, the context of risk, rather than maternal mental health, was shown to account for youth symptoms (Pelham et al., 2020). Taken together, these literatures highlight the need to consider contextual factors as potential cascading predictors of mental health in a disaster.
This study tested whether pandemic‐related changes in maternal mental health partially accounted for changes in psychopathology in adolescents. Based on prior evidence that economic disadvantage is related to more stressors during a disaster and during the COVID‐19 pandemic in particular, we expected that pandemic‐related stressors would be higher among families with lower income before the pandemic and would account for increases in maternal and adolescent mental health symptoms early in the pandemic from pre‐pandemic levels, over and above the effects of pre‐pandemic family income. Given prior evidence of the impact of maternal mental health on youth response to disasters and COVID‐19, we hypothesized that increases in maternal mental health symptoms would predict concurrent and prospective levels of adolescent internalizing and externalizing problems, above the effects of pandemic‐related stressors. Further, we hypothesized that maternal mental health would mediate the effects of both pre‐pandemic income and pandemic‐related stressors on adolescent psychopathology. Accounting for the pre‐pandemic family income‐to‐needs ratio, maternal mental health and adolescent psychopathology, the study examined the effects of (a) pandemic‐related stressors on increases in maternal mental health symptoms and adolescent psychopathology, (b) changes in maternal mental health on changes in adolescent psychopathology during the pandemic, and (c) whether maternal mental health mediated the effects of pre‐pandemic income and pandemic‐related stressors on adolescent psychopathology.
Methods
Participants
Participants in this study (N = 226) were a subset of a larger community‐based sample of 306 children and their mothers who were assessed at multiple time points across childhood. The subset of 226 participants participated in an age‐12 assessment, capturing adjustment before the pandemic. Participants from the parent study were excluded from age‐12 assessments based on the following criteria: moved out‐of‐area, IQ < 80, active substance dependence, psychosis, or the presence of pervasive developmental disorder.
All subjects who participated in the age‐12 assessment were invited to complete COVID‐19 surveys. Of those, 143 adolescents (63%, 62 females, mean age = 14.33, SD = .48) and a caregiver completed online questionnaires between April and May of 2020, early in the COVID‐19 pandemic (spring 2020), and 152 youth (67%, 72 female, mean age 14.87, SD = .49), and a caregiver completed questionnaires online between November 2020 and January 2021 (winter 2020–21). Some participants completing the second survey had not completed the first one, and vice versa, resulting in a total of 161 survey respondents across the two surveys. Of those participants, 105 (65%) identified as White, 19 (12%) as Black, 17 (11%) as Latinx, 14 (9%) as Asian, and 6 (4%) as another race or ethnicity.
Missingness analyses
Participants completing both the spring 2020 and winter 2020–21 surveys were compared with those who did not complete either of the surveys. Variables were compared across participants missing and not missing COVID‐19 survey data using t‐tests of mean differences between the group with complete data and that with missing data (Tabachnick & Fidell, 2013). Families who did not complete the COVID‐19 surveys did not differ significantly from the families who completed the survey on age‐12 income‐to‐needs, maternal mental health or on child internalizing or externalizing problems, indicating that it was unlikely that missing data introduced bias in the model estimates, and missing data would likely have minimal impact on parameter estimates (Collins et al., 2001; Dong & Peng, 2013). Full‐information maximum likelihood estimation (FIMLE) was considered appropriate under these conditions and consistently produces less biased parameter estimates and greater statistical power (e.g., Enders & Bandalos, 2001).
Procedures
When youth were 12 years old, families were assessed in offices on the university campus. All procedures for this assessment were approved by the University of Washington Human Subjects Institutional Review Board, and all procedures performed were in accordance with the ethical standards of the institutional committee. Both active, informed parental consent and child assent were obtained from all participants prior to data collection. Parents and children completed questionnaire measures, and families were compensated $75 for participating. During the pandemic, pandemic‐related stressors, maternal and adolescent mental health were assessed in two online surveys administered to families in spring 2020, and approximately 6 months later in winter 2020–21. COVID‐19 survey procedures were approved by the Institutional Review Board at Harvard University where the surveys were conducted. For the COVID‐19 survey, legal guardians provided informed consent and children provided assent via electronic signature obtained using Qualtrics (Provo, UT). Parents and adolescents were provided separate RedCap survey links. If youth had trouble completing the surveys on their own, an experimenter called, read the questions aloud to the adolescent, and recorded their responses.
Measures
Income‐to‐needs
At the age‐12 assessment, mothers reported on household income from all sources on a 14‐point scale (e.g., 1 = $14,570 or less, 2 = $14,571–$18,310, 3 = $18,311–22,050.). The income‐to‐needs ratio was calculated by dividing the family’s income by the federal poverty threshold for a family of that size in 2017, with values less than one indicating income below the poverty line. The median and mean income in this sample was $75–100K, with an average income‐to‐needs ratio of 3.587 (SD = 1.808, range = 0.143–7.603).
Maternal mental health
Symptoms of generalized anxiety were measured with the 7‐item Generalized Anxiety Disorder‐7 (GAD‐7) scale, which assesses anxiety symptoms occurring in the last 2 weeks. Items are scored on a Likert scale (0–3). The GAD‐7 has good reliability and validity (Spitzer, Kroenke, Williams, & Löwe, 2006) and demonstrated good internal consistency at all time‐points in this study (α = .86–.90). Depression symptoms were measured with the 9‐item Patient Health Questionnaire‐9 (PHQ‐9), which assesses depression symptoms occurring in the last 2 weeks using a Likert scale (0–3). The PHQ‐9 has good reliability and validity (Kroenke, Spitzer, & Williams, 2001) and good internal consistency at all time‐points in this study (α = .84–.88). These measures were correlated .51, .76, and .74 at each time point and were averaged into a single measure of maternal mental health symptoms.
Adolescent internalizing and externalizing problems
Internalizing and externalizing problems prior to the pandemic were assessed using youth report on the Youth Self‐Report (YSR; Achenbach & Rescorla, 2001). In the COVID‐19 assessments, adolescents completed the 25‐item Strengths and Difficulties Questionnaire (SDQ; Goodman, 2001), selected to reduce participant burden, as it has substantially fewer items than the YSR. The SDQ has good reliability and validity (Dickey & Blumberg, 2004; Goodman, Lamping, & Ploubidis, 2010) and correlates strongly with the CBCL/YSR(Goodman & Scott, 1999).
Pandemic‐related stressors
Adolescents and caregivers reported on questions assessing health, financial, social, school, and physical environment stressors that occurred within the month prior to the first COVID‐19 assessment (Weissman et al., 2021). Seven of the stressors were related to the health of participants or close others (e.g., contracting COVID‐19); four were related to financial impacts of COVID‐19 (e.g., parent lost a job); four were related to disruptions to social life; and three related to household noise and crowding. Scores were the count of risk factors endorsed. Adolescent and parent reports were correlated r = .588 and were averaged to capture both perspectives (see Table S1).
Analytic plan
A path model was estimated using FIMLE in Mplus to test whether pandemic‐related stressors predicted changes in maternal and adolescent mental health from before the pandemic to early in the pandemic, and whether changes in maternal mental health early in the pandemic predicted adolescent internalizing and externalizing problems and mediated the effects of pandemic‐related stressors on adolescent psychopathology (see Figure 1). The model was specified such that: (a) maternal mental health and adolescent internalizing and externalizing problems when youth were aged 12 were regressed on age‐12 family income‐to‐needs ratio, to account for the families’ pre‐existing context of economic risk; (b) maternal mental health and adolescent internalizing and externalizing problems assessed in spring 2020 of the pandemic were regressed on age‐12 mental health measures and pandemic‐related stressors, testing the extent to which pandemic‐related stressors predicted changes in maternal and adolescent mental health from pre‐pandemic to its start; and (c) adolescent psychopathology assessed in winter 2020–21 of the pandemic was regressed on spring 2020 and winter 2020–21 maternal mental health and spring 2020 adolescent psychopathology to test whether changes in maternal mental health during the pandemic predicted changes in youth psychopathology during the pandemic. Adolescent sex was covaried in all analyses. Tests of indirect effects were used to evaluate whether maternal mental health mediated the effects of pandemic‐related stressors on adolescent psychopathology.
Figure 1.
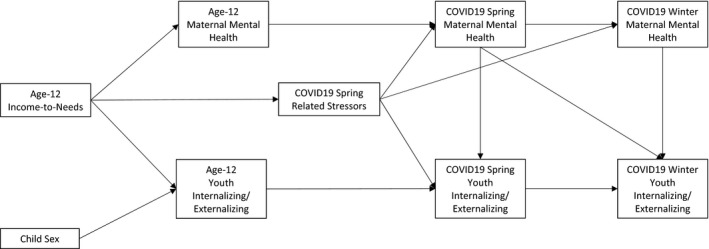
Conceptual model testing changes in parent and child mental health from before the COVID‐19 pandemic to its start, and across 6 months of the pandemic
Results
Descriptive statistics for all study measures are reported in Table 1. The originally specified path model demonstrated adequate fit to the data ( 2(27) = 40.161, p = .0495, CFI = 0.977, RMSEA = .047, RMSEA 90% CI = .002–.075, SRMR = .054, average residual correlation |r| = .160). All estimated path coefficients are reported in Table 2.
Table 1.
Descriptive statistics for study measures
| Pre‐COVID‐19 | Spring 2020 COVID‐19 | Winter 2020‐21 COVID‐19 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| M | SD | Min‐Max | M | SD | Min‐Max | M | SD | Min‐Max | |
| Age 12 Income‐to‐Needs | 3.587 | 1.808 | 0.143–7.602 | ||||||
| Pandemic‐Related Stressors | 2.391 | 1.537 | 0–7 | ||||||
| Mother Mental Health | 3.278 | 2.562 | 0–15.670 | 5.198 | 4.125 | 0.000–16.000 | 7.418 | 4.820 | 0.000–21.000 |
| YSR Internalizing | 10.867 | 7.662 | 0–41 | ||||||
| YRS Externalizing | 7.615 | 5.226 | 0–30 | ||||||
| SDQ Internalizing | 4.210 | 3.367 | 0.000–16.000 | 5.414 | 3.971 | 0.000–17.000 | |||
| SDQ Externalizing | 5.500 | 3.287 | 0.000–16.000 | 5.861 | 3.671 | 0.000–14.000 | |||
The Youth Self Report was used as the pre‐pandemic measure of adolescent internalizing and externalizing; the Strengths and Difficulties Questionnaire was used in the pandemic surveys.
Table 2.
Standardized regression coefficients (standard errors) from the path model testing the effects of pre‐COVID‐19 income‐to‐needs, maternal and youth mental health on changes in mental health during the pandemic
| Pre‐COVID‐19 | Spring 2020 COVID‐19 | Winter 2020‐21 COVID‐19 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mother Mental Health | Child Internal | Child External | Pandemic Related Stressors | Mother Mental Health | Child Internal | Child External | Mother Mental Health | Child Internal | Child External | |
| Pre‐COVID‐19 | ||||||||||
| Child Sex | .137* (.064) | .065 (.066) | .203** (.063) | – | −.427*** (.064) | −.085 (.064) | .231** (.067) | .012 (.093) | −.089 (.079) | .007 (.086) |
| Age 12 Income‐to‐Needs | −.242*** (.063) | −.147* (.065) | −.163* (.064) | −.313*** (.071) | −.027 (.075) | −.029 (.062) | .062 (.065) | .039 (.087) | .074 (.073) | −.020 (.074) |
| Age 12 Mother Mental Health | .175* (.074) | – | – | |||||||
| Age 12 Child Internalizing | – | .191** (.058) | – | |||||||
| Age 12 Child Externalizing | – | – | .161** (.061) | |||||||
| COVID‐19 Spring 2020 | ||||||||||
| Pandemic Related Stressors | .276*** (.073) | .099 (.064) | .054 (.067) | .228* (.093) | ||||||
| Spring 2020 Mother Mental Health | – | .612*** (.058) | .708*** (.058) | .212* (.106) | .048 (.104) | .182 (.108) | ||||
| Spring 2020 Child Internalizing | .509*** (.076) | – | ||||||||
| Spring 2020 Child Externalizing | – | .468*** (.076) | ||||||||
| COVID‐19 Winter 2020–21 | ||||||||||
| Winter 2020–21 Mother Mental Health | .167* (.074) | .082 (.074) | ||||||||
*<.05, **<.01, ***<.001.
A lower pre‐pandemic income‐to‐needs ratio predicted higher pre‐pandemic maternal mental health symptoms and higher adolescent internalizing and externalizing.
Lower income‐to‐needs predicted more spring‐2020 pandemic‐related stressors, and in turn, pandemic‐related stressors were associated with higher concurrent maternal mental health symptoms, but not adolescent internalizing or externalizing when the other variables in the model were covaried. Pandemic‐related stressors were related to rank order increases in maternal mental health symptoms from spring 2020 to winter 2020–21.
Maternal mental health in spring 2020 was strongly related to concurrent adolescent internalizing and externalizing problems above the effects of pre‐pandemic income‐to‐needs, internalizing and externalizing problems, and above pandemic‐related stressors, indicating that it was predicting rank order increases from pre‐pandemic levels of psychopathology. There was a significant concurrent association of winter 2020–21 maternal mental health symptoms with adolescent internalizing, controlling for spring 2020 maternal mental health, indicating that rank order increases in maternal mental health symptoms were associated with increases in adolescent psychopathology.
Given the substantial proportion of missing COVID‐19‐survey data, sensitivity analyses were conducted to compare the FIMLE results with analyses conducted using listwise deletion (see Table S2). The magnitudes of associations were essentially unchanged, although three associations became nonsignificant (i.e., age‐12 maternal mental health predicting spring 2020 maternal mental health, and spring 2020 maternal mental health predicting winter 2020‐21 adolescent internalizing and externalizing), likely as a result of the lower sample size, considering that the differences in magnitudes of the effects were very small (.025–.034).
Tests of indirect effects were used to assess whether maternal mental health mediated the effects of pre‐pandemic income‐to‐needs and pandemic‐related stressors on adolescent psychopathology. There were significant indirect effects of age‐12 income‐to‐needs on winter 2020–21 youth internalizing and externalizing through pandemic‐related stressors, spring 2020 maternal mental health, and spring 2020 adolescent internalizing (β = −.027, SE = .011, p = .013) and externalizing (β = −.029 SE = .012, p = .013). The portion of this indirect effect reflecting the effects of pandemic‐related stressors on winter 2020–21 internalizing (β = .086 SE = .028, p = .002) and externalizing (β = .091 SE = .030, p = .002) were also significant. Power to detect mediating effects was determined using Fritz and MacKinnon’s (2007) simulation results. In this study, with 2 and 3 mediating steps of the effects of income‐to‐needs on youth adjustment, power estimates are not readily available. In order to use the available simulations, the effect of income‐to‐needs on pandemic‐related stressors was considered the “a” path (β = −.313, moderate effect), and the joint effects of pandemic‐related stressors on maternal mental health, and in turn, youth adjustment were calculated and treated as the “b” path (β = .09, small effect). Based on Fritz and MacKinnon (2007), we were not adequately powered to detect small mediating effects (e.g., a*b where the “a” path is medium and the “b” path is small), which would require a sample size of ≥400, but we had sufficient power (.80) to detect medium indirect effects (e.g., a*b where the “a” path was medium and the “b” path was half‐way between small and medium), which would require a sample of ≥125.
Discussion
This study demonstrated that changes in maternal mental health from before COVID‐19 to early in the pandemic, as well as changes in maternal mental health symptoms across several months of the pandemic, predicted changes in adolescent psychopathology. Further, maternal mental health accounted for the effects of family income and pandemic‐related stressors on adolescent outcomes. Previous studies showed substantial increases in psychopathology in parents and youth during the COVID‐19 pandemic (Racine, Eirich, et al., 2021; Racine, McArthur, et al., 2021). The results of this study elaborate on those findings by demonstrating the effects of a family context of stress and maternal mental health on changes adolescent psychopathology, providing information about which adolescents were likely to be more vulnerable to increased psychopathology. The results of this study indicate that adolescents whose families were lower in income before the pandemic experienced greater pandemic‐related stressors, which in turn predicted greater maternal mental health symptoms. When mothers experienced greater symptoms related to COVID‐19, adolescents were significantly more likely to show increases in psychopathology.
Consistent with prior research on disasters and community level stressors (e.g., Kerns et al., 2014; Kılıç et al., 2011), parents’ mental health in response to the pandemic was a substantial predictor of youth psychopathology during COVID‐19 (e.g., Russell et al., 2021; Thompson et al., 2022). In this study, increases in mothers’ anxiety and depression early in the pandemic predicted parallel changes in adolescent psychopathology and mediated the effects of pandemic‐related stressors. Mothers showed increases in mental health symptoms when they experienced a greater number of pandemic‐related stressors. These effects were above the effects of pre‐pandemic levels of family income and consistent with findings from other studies of the COVID pandemic (e.g., Westrupp et al., 2021). Interestingly, pandemic‐related stressors did not have direct effects on adolescent psychopathology when other family contextual factors were considered, but rather demonstrated significant indirect effects through maternal mental health. This study adds to the literature on adolescent mental health during COVID‐19 by showing that maternal mental health changes were closely tied to changes in adolescent psychopathology. Further, prior research indicates that parental distress following a disaster predicts persistence of children's emotional and behavioral problems afterward (Swenson et al., 1996), suggesting that parental mental health symptoms following the COVID‐19 pandemic could contribute to protracted symptoms for youth. This highlights the importance of supporting parental mental health to prevent psychopathology in youth (Miller et al., 2012). In particular, targeting youth mental health alone without also supporting parental mental health may be insufficient to mitigate the impact of the COVID‐19 pandemic on long‐term youth outcomes.
Adolescents in families who had lower pre‐pandemic income demonstrated higher internalizing and externalizing prior to the pandemic, which were related to higher levels of symptoms at the start of the pandemic. Adolescents living in low income contexts and/or those who were already demonstrating higher levels of psychopathology prior to the pandemic were at greatest risk for adjustment problems during the pandemic and might be at greater risk for persistence of psychopathology emerging from the pandemic. Given the stability of low income or increased economic strain related to the pandemic (Gruber et al., 2020), it is likely that adolescents in lower income households would be more likely to demonstrate protracted symptom elevations after the pandemic. For example, following Hurricane Katrina, long‐term health and mental health consequences were most severe for low‐income mothers who experienced more hurricane‐related stressors and loss, and who had fewer resources (Rhodes et al., 2010). In considering youth responses to disasters or prolonged stressors, attention to providing resources and mental health support to youth in lower‐income families is critical to addressing the adverse impact of such events.
The results of this study highlight a cascading effect of low income on youth mental health during the pandemic, as evidenced by the significant indirect effect of pre‐pandemic family income‐to‐needs ratio on youth internalizing and externalizing problems several months into the pandemic. The family economic context was associated with increased stressors during the pandemic, which prospectively predicted increases in maternal mental health symptoms, representing a cascading effect of pre‐pandemic income and pandemic‐related stressors on youth psychopathology. The implications of this are profound when considering that nearly one in six children in the United States, where this study was conducted, are living in poverty, and one in six children worldwide are living in extreme poverty (Silwal, Engilbertsdottir, Cuesta, Newhouse, & Stewart, 2020). Estimates indicate that 77% of families in low‐ and middle‐income countries suffered economic losses, food insecurity, and inability to access medicine as a consequence of the pandemic (Josephson, Kilic, & Michler, 2021), making these children and families particularly vulnerable to mental health problems when community‐level stressors or disasters strike. Supporting low‐income families financially, materially, socially, and emotionally during disasters is critical for preventing persistent mental health problems in youth.
Strengths of this study included the longitudinal design which incorporated pre‐pandemic measures as well as multiple assessments during the pandemic. In addition, measures were obtained from both parents and adolescents, reducing the likelihood that associations were accounted for by reporter bias. Several limitations are also noted. First, the overall sample responses to the COVID‐19 survey were relatively low, with only 71% of the sample completing at least one of the surveys, although it appears that little bias was introduced by missing data. Additional limitations are the inclusion of only one parent respondent, and in particular, not being able to account for both maternal and paternal mental health in our models.
A critical future direction will be to continue to assess youth mental health in the aftermath of the COVID‐19 pandemic to understand which youth exhibit protracted elevations in psychopathology. In addition to the effects of family income, prior symptoms, and parental mental health, family factors potentially relevant to adolescent responses to community level disasters to consider include family conflict, cohesion, and parenting. Family dysfunction has been observed in twice as many families following a disaster (McDermott & Cobham, 2012) and in the COVID‐19 pandemic in particular (Calvano et al., 2021). In addition, evidence suggests that the quality of parenting practices following traumatic events mediate the relations of trauma and youth adjustment (Cobhan & McDermott, 2014) pointing to the potential importance of parenting during the pandemic.
Conclusions
In the context of the COVID‐19 pandemic, adolescent mental health was closely connected to maternal mental health. The results of this study imply that targeted intervention and prevention efforts in response to a disaster or community level stressor should consider factors that increase youth risk for psychopathology, including pre‐existing contextual risk factors such as the family economic situation, along with stressors that arise in relation to the event. In particular, addressing parents' mental health in conjunction with direct support for adolescents’ is critical to reducing youth psychopathology.
Supporting information
Table S1. Within and across reporter correlations of adolescent, mother and combined reports of COVID‐19‐related stressors and mother and adolescent mental health.
Table S2. Standardized regression coefficients from the path model testing the effects of pre‐COVID‐19 income‐to‐needs, maternal, and youth mental health on changes in mental health during the pandemic using observed (listwise) data.
Acknowledgements
This work was supported by the Bezos Family Foundation (to A.M.), National Institute of Mental Health (R01 MH106482 to K.A.M.) and National Institute of Child Health and Human. Development (R01 HD054465 to L.J.L.). The authors have declared that they have no competing or potential conflicts of interest.
Key points.
The COVID‐19 pandemic is associated with increases in both parental and youth mental health problems.
Changes in maternal mental health in response to the pandemic predicted changes in youth psychopathology during the pandemic and mediated the effects of family income and pandemic‐related stressors on psychopathology.
Providing support for parents' mental health along with support for youth is critical to reducing the impact of community‐level stressors like the COVID‐19 pandemic on youth psychopathology.
Conflict of interest statement: No conflicts declared.
References
- Achenbach, T.M. , & Rescorla, L.A. (2001). Manual for the ASEBA school‐age forms & profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families. [Google Scholar]
- Adler, N.E. , & Ostrove, J.M. (1999). Socioeconomic status and health: What we know and what we don't. Annals of the New York Academy of Sciences, 896, 3–15. [DOI] [PubMed] [Google Scholar]
- Bryson, H. , Mensah, F. , Price, A. , Gold, L. , Mudiyanselage, S.B. , Kenny, B. , … & Goldfeld, S. (2021). Clinical, financial and social impacts of COVID‐19 and their associations with mental health for mothers and children experiencing adversity in Australia. PLoS One, 16, e0257357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calvano, C. , Engelke, L. , Di Bella, J. , Kindermann, J. , Renneberg, B. , & Winter, S.M. (2021). Families in the COVID‐19 pandemic: Parental stress, parent mental health and the occurrence of adverse childhood experiences—results of a representative survey in Germany. European Child & Adolescent Psychiatry, 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cameron, E.E. , Joyce, K.M. , Delaquis, C.P. , Reynolds, K. , Protudjer, J.L.P. , & Roos, L.E. (2020). Maternal psychological distress & mental health service use during the COVID‐19 pandemic. Journal of Affective Disorders, 276, 765–774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll, N. , Sadowski, A. , Laila, A. , Hruska, V. , Nixon, M. , Ma, D.W. , & Haines, J. (2020). The impact of COVID‐19 on health behavior, stress, financial and food security among middle to high income Canadian families with young children. Nutrients, 12, 2352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cobham, V.E. , & McDermott, B. (2014). Perceived parenting change and child posttraumatic stress following a natural disaster. Journal of Child and Adolescent Psychopharmacology, 24(1), 18–23. [DOI] [PubMed] [Google Scholar]
- Collins, L.M. , Schafer, J.L. , & Kam, C.‐M. (2001). A comparison of inclusive and restrictive strategies in modern missing data procedures. Psychological Methods, 6(4), 330–351. 10.1037/1082-989X.6.4.330 [DOI] [PubMed] [Google Scholar]
- Dickey, W.C. , & Blumberg, S.J. (2004). Revisiting the factor structure of the Strengths and Difficulties Questionnaire: United States, 2001. Journal of the American Academy of Child and Adolescent Psychiatry, 43, 1159–1167. [DOI] [PubMed] [Google Scholar]
- Dong, Y. , & Peng, C.Y.J. (2013). Principled missing data methods for researchers. SpringerPlus, 2, 1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enders, C.K. , & Bandalos, D.L. (2001). The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Structural Equation Modeling, 8(3), 430–457. [Google Scholar]
- Fancourt, D. , Steptoe, A. , & Bu, F. (2021). Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID‐19 in England: A longitudinal observational study. The Lancet Psychiatry, 8, 141–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fegert, J.M. , Vitiello, B. , Plener, P.L. , & Clemens, V. (2020). Challenges and burden of the Coronavirus 2019 (COVID‐19) pandemic for child and adolescent mental health: A narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child and Adolescent Psychiatry and Mental Health, 14, 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fritz, M.S. , & Mackinnon, D.P. (2007). Required sample size to detect the mediated effect. Psychological Science, 18, 233–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gadermann, A.C. , Thomson, K.C. , Richardson, C.G. , Gagné, M. , McAuliffe, C. , Hirani, S. , & Jenkins, E. (2021). Examining the impacts of the COVID‐19 pandemic on family mental health in Canada: Findings from a national cross‐sectional study. British Medical Journal Open, 11, e042871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gassman‐Pines, A. , Ananat, E.O. , & Fitz‐Henley, J. (2020). COVID‐19 and parent‐child psychological well‐being. Pediatrics, 146, e2020007294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman, A. , Lamping, D.L. , & Ploubidis, G.B. (2010). When to use broader internalising and externalising subscales instead of the hypothesised five subscales on the Strengths and Difficulties Questionnaire (SDQ): Data from British parents, teachers and children. Journal of Abnormal Child Psychology, 38, 1179–1191. [DOI] [PubMed] [Google Scholar]
- Goodman, R. (2001). Psychometric properties of the Strengths and Difficulties Questionnaire. Journal of the American Academy of Child and Adolescent Psychiatry, 40, 1337–1345. [DOI] [PubMed] [Google Scholar]
- Goodman, R. , & Scott, S. (1999). Comparing the Strengths and Difficulties Questionnaire and the Child Behavior Checklist: Is small beautiful? Journal of Abnormal Child Psychology, 27, 17–24. [DOI] [PubMed] [Google Scholar]
- Goodman, S.H. , Rouse, M.H. , Connell, A.M. , Broth, M.R. , Hall, C.M. , & Heyward, D. (2011). Maternal depression and child psychopathology: A meta‐analytic review. Clinical Child and Family Psychology Review, 14, 1–27. [DOI] [PubMed] [Google Scholar]
- Green, B.L. , Korol, M. , Grace, M.C. , Vary, M.G. , Leonard, A.C. , Gleser, G.C. , & Smith‐Cohen, S. (1991). Children and disaster: Age, gender, and parental effects on PTSD symptoms. Journal of the American Academy of Child and Adolescent Psychiatry, 30, 945–951. [DOI] [PubMed] [Google Scholar]
- Gruber, J. , Prinstein, M.J. , Clark, L.A. , Rottenberg, J. , Abramowitz, J.S. , Albano, A.M. , … & Forbes, E.E. (2020). Mental health and clinical psychological science in the time of COVID‐19: Challenges, opportunities, and a call to action. American Psychologist, 76, 409–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Josephson, A. , Kilic, T. , & Michler, J.D. (2021). Socioeconomic impacts of COVID‐19 in low‐income countries. Nature Human Behaviour, 5, 557–565. [DOI] [PubMed] [Google Scholar]
- Juth, V. , Silver, R.C. , Seyle, D.C. , Widyatmoko, C.S. , & Tan, E.T. (2015). Post‐disaster mental health among parent–child dyads after a major earthquake in Indonesia. Journal of Abnormal Child Psychology, 43, 1309–1318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerns, C.E. , Elkins, R.M. , Carpenter, A.L. , Chou, T. , Green, J.G. , & Comer, J.S. (2014). Caregiver distress, shared traumatic exposure, and child adjustment among area youth following the 2013 Boston Marathon bombing. Journal of Affective Disorders, 167, 50–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kılıç, C. , Kılıç, E.Z. , & Aydın, İ.O. (2011). Effect of relocation and parental psychopathology on earthquake survivor‐children's mental health. The Journal of Nervous and Mental Disease, 199, 335–341. [DOI] [PubMed] [Google Scholar]
- Kroenke, K. , Spitzer, R.L. , & Williams, J.B.W. (2001). The PHQ‐9. Journal of General Internal Medicine, 16, 606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magson, N.R. , Freeman, J.Y. , Rapee, R.M. , Richardson, C.E. , Oar, E.L. , & Fardouly, J. (2021). Risk and protective factors for prospective changes in adolescent mental health during the COVID‐19 pandemic. Journal of Youth and Adolescence, 50, 44–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDermott, B.M. , & Cobham, V.E. (2012). Family functioning in the aftermath of a natural disaster. BMC psychiatry, 12(1), 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller, P.A. , Roberts, N.A. , Zamora, A.D. , Weber, D.J. , Burleson, M.H. , Robles, E. , & Tinsley, B.J. (2012). Families coping with natural disasters: Lessons from wildfires and tornados. Qualitative Research in Psychology, 9, 314–336. [Google Scholar]
- Norris, F.H. , Friedman, M.J. , Watson, P.J. , Byrne, C.M. , Diaz, E. , & Kaniasty, K. (2002). 60,000 disaster victims speak: Part I. An empirical review of the empirical literature, 1981–2001. Psychiatry, 65, 207–239. [DOI] [PubMed] [Google Scholar]
- Pakenham, K.I. , Landi, G. , Boccolini, G. , Furlani, A. , Grandi, S. , & Tossani, E. (2020). The moderating roles of psychological flexibility and inflexibility on the mental health impacts of COVID‐19 pandemic and lockdown in Italy. Journal of Contextual Behavioral Science, 17, 109–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick, S.W. , Henkhaus, L.E. , Zickafoose, J.S. , Lovell, K. , Halvorson, A. , Loch, S. , … & Davis, M.M. (2020). Well‐being of parents and children during the COVID‐19 pandemic: A national survey. Pediatrics, 146, e2020016824. [DOI] [PubMed] [Google Scholar]
- Pelham, W.E., III , West, S.G. , Lemery‐Chalfant, K. , Goodman, S.H. , Wilson, M.N. , Dishion, T.J. , & Shaw, D.S. (2020). Depression in mothers and the externalizing and internalizing behavior of children: An attempt to go beyond association. Journal of Abnormal Psychology, 130, 60–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Proctor, L.J. , Fauchier, A. , Oliver, P.H. , Ramos, M.C. , Rios, M.A. , & Margolin, G. (2007). Family context and young children’s responses to earthquake. Journal of Child Psychology and Psychiatry, 48, 941–949. [DOI] [PubMed] [Google Scholar]
- Purtle, J. (2012). Racial and ethnic disparities in post‐disaster mental health: Examining the evidence through a lens of social justice. Washington and Lee Journal of Civil Rights and Social Justice, 19, 31–55. [Google Scholar]
- Purtle, J. (2020). COVID‐19 and mental health equity in the United States. Social Psychiatry and Psychiatric Epidemiology, 55, 969–971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Racine, N. , Eirich, R. , Cookee, J. , Zhu, J. , Pador, P. , Dunnewold, N. , & Madigan, S. (2021). When the bough breaks: A systematic review and meta‐analysis of mental health symptoms in mothers of young children during the COVID‐19 pandemic. PsyArXiv. 10.31234/osf.io/u8pnh [DOI] [PMC free article] [PubMed] [Google Scholar]
- Racine, N. , McArthur, B.A. , Cooke, J.E. , Eirich, R. , Zhu, J. , & Madigan, S. (2021). Global prevalence of depressive and anxiety symptoms in children and adolescents during COVID‐19: A meta‐analysis. JAMA Pediatrics, 175, 1142–1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes, J. , Chan, C. , Paxson, C. , Rouse, C.E. , Waters, M. , & Fussell, E. (2010). The impact of hurricane Katrina on the mental and physical health of low‐income parents in New Orleans. American Journal of Orthopsychiatry, 80, 237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenfeld, D.L. , Balcetis, E. , Bastian, B. , Berkman, E.T. , Bosson, J.K. , Brannon, T.N. , … & Tomiyama, A.J. (2021). Psychological science in the wake of COVID‐19: Social, methodological, and meta‐scientific considerations. Perspectives on Psychological Science, 17, 311–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell, B.S. , Tomkunas, A.J. , Hutchison, M. , Tambling, R.R. , & Horton, A.L. (2021). The protective role of parent resilience on mental health and the parent‐child relationship during COVID‐19. Child Psychiatry & Human Development, 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silwal, A.R. , Engilbertsdottir, S. , Cuesta, J. , Newhouse, D. , & Stewart, D. (2020). Global estimate of children in monetary poverty. World Bank and UNICEF Report. [Google Scholar]
- Spitzer, R.L. , Kroenke, K. , Williams, J.B.W. , & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD‐7. Archives of Internal Medicine, 166, 1092–1097. [DOI] [PubMed] [Google Scholar]
- Swenson, C.C. , Saylor, C.F. , Powell, M.P. , Stokes, S.J. , Foster, K.Y. , & Belter, R.W. (1996). Impact of a natural disaster on preschool children: Adjustment 14 months after a hurricane. American Journal of Orthopsychiatry, 66, 122–130. [DOI] [PubMed] [Google Scholar]
- Tabachnick, B. , & Fidell, L. (2013). Using multivariate statistics, 6th ed. Boston, MA: Pearson. [Google Scholar]
- Thompson, S.F. , Shimomaeda, L. , Calhoun, B. , Moini, N. , Smith, M.R. , & Lengua, L.J. (2022). Maternal mental health and child adjustment problems in response to the COVID‐19 pandemic in families experiencing economic disadvantage. Research on Child and Adolescent Psychopathology. 10.1007/s10802-021-00888-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman, D.G. , Rodman, A.M. , Rosen, M.L. , Kasparek, S.W. , Mayes, M. , Sheridan, M. , … & McLaughlin, K.A. (2021). Contributions of emotion regulation and brain structure and function to adolescent internalizing problems and stress vulnerability during the COVID‐19 pandemic: A longitudinal study. Biological Psychology: Global Open Sceince, 1, 272–282. 10.31234/osf.io/jfxd4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westrupp, E.M. , Bennett, C. , Berkowitz, T. , Youssef, G.J. , Toumbourou, J.W. , Tucker, R. , & Sciberras, E. (2021, September 30). Child, parent, and family mental health and functioning in Australia during COVID‐19: Comparison to pre‐pandemic data. European Child & Adolescent Psychiatry, 1–14. 10.31234/osf.io/ydrm9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright, N. , Hill, J. , Sharp, H. , & Pickles, A. (2021). Interplay between long‐term vulnerability and new risk: Young adolescent and maternal mental health immediately before and during the COVID‐19 pandemic. JCPP Advances, 1, e12008. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Within and across reporter correlations of adolescent, mother and combined reports of COVID‐19‐related stressors and mother and adolescent mental health.
Table S2. Standardized regression coefficients from the path model testing the effects of pre‐COVID‐19 income‐to‐needs, maternal, and youth mental health on changes in mental health during the pandemic using observed (listwise) data.


