Abstract
Purpose
The study aims to examine the factors that impact vaccination uptake and additional protective behavior during the fourth wave of the pandemic in Israel, whereas the “pandemic fatigue” phenomenon has been identified as a hurdle to adherence to protective health behaviors against coronavirus disease 2019 (COVID‐19).
Design
A cross‐sectional, structured questionnaire was utilized for this investigation in September 2021, during the fourth wave of the pandemic.
Methods
A sample of the adult (18+) Israeli population was employed for the study. Recruiting participants for the study was conducted through an online internet panel company that consists of over 100,000 members, representing all geographic and demographic sectors of the Israeli population.
Results
Our findings indicate that pandemic fatigue has begun to have cascading effects on vaccination efforts. In particular, this study found that at this stage of the COVID‐19 pandemic, trust in authorities, and even threat perception components, such as concern and fear of contracting the disease, are incapable of predicting vaccination uptake. Instead, perception of the importance of the vaccine and its effectiveness are predictive of vaccination uptake.
Conclusion
The findings indicate that at this stage of the pandemic, focusing on the robustness of the science behind the vaccine is more important than trying to regain public trust. The findings also suggest that risk communication employing fear tactics is losing its capacity to generate motivation for vaccination.
Clinical Relevance
The findings of this study reveal lessons learned from the COVID‐19 global pandemic. Specifically, the study reveals how in times of prolonged crisis, we can currently and, in the future, prepare improved strategies for public communication in order to promote uptake of protective health behavior, such as vaccination.
Keywords: attitudes, COVID‐19, pandemic, pandemic fatigue, vaccination uptake
INTRODUCTION
Since the onset of the coronavirus disease 2019 (COVID‐19) pandemic, a variety of policies have been enacted by governments worldwide in an effort to contain the outbreak (Hale et al., 2021). Early in the pandemic, prior to the extensive availability of vaccines, governments relied on non‐pharmaceutical interventions (NPIs) to reduce virus transmission within their respective populations with the aim of delaying the timing of the epidemic peak (Flaxman et al., 2020; Lai et al., 2020). Health measures focused on minimizing interpersonal contact to reduce the risk of person‐to‐person transmission, through mobility restrictions, mask wearing, and social distancing (such as school closures and gathering bans), alongside strategies of testing and contact tracing (Flaxman et al., 2020; Lai et al., 2020). While the stringency of measures has varied throughout the outbreak and across geographical regions, the measures have been in place in many countries, for well over a year (Hale et al., 2021).
Alongside multi‐pronged countermeasures, vaccination rollout campaigns were integrated in late 2020 in order to suppress COVID‐19 transmission (Shilo, Rossman, & Segal, 2021). In the case of Israel, a country of 9.3 million, a supply of the Pfizer‐BioNTech vaccine was obtained and inoculation began on December 20, 2020 among healthcare staff, individuals aged 60 years and older, and those with additional risks (e.g., immunodeficiency, chronic lung disease, diabetes, etc.) and gradually expanded to include all eligible individuals (including most recent children over the age of 5 on November 23, 2021) (Alpert, Herbst, Abramovich, Strugo, & Jaffe, 2021; Wilf‐Miron, Myers, & Saban, 2021). The vaccination drive was orchestrated by the Ministry of Health and conducted by four national health maintenance organizations (HMOs), which provide insurance for all citizens and ensured easy access throughout the country (Alpert et al., 2021; Wilf‐Miron et al., 2021). Despite early success and momentum in the vaccination campaign, a moderate, yet the notable level of vaccine hesitancy in the Israeli general population was observed (Dror et al., 2020). Globally, widespread immunization has been hampered by the reluctance of large sectors of the public to receive recommended available vaccines which, in part may be due to the fast‐tracked new technology involved with the development of COVID‐19 vaccines, and these, along with the well‐established concerns of vaccine opponents (Wilf‐Miron et al., 2021). This phenomenon may be propagated by a spectrum of held views concerning vaccination, spanning from vigilant acceptors to complete deniers (Rosen, Waitzberg, Israeli, Hartal, & Davidovitch, 2021). Anti‐vaccination groups with a strong social media platform presence have contributed to growing anxieties concerning vaccination worldwide (Rosen et al., 2021).
To incentivize vaccination in an attempt to reach “herd immunity,” Israel, had implemented a “green pass” certificate which would provide access to social, cultural, sports events, gyms, hotels, and restaurants. It also provides exemptions from isolation upon contact with a confirmed COVID‐19 case or upon returning from international travel for those who were deemed to have achieved “immunity,” whether based on those who had recovered from COVID‐19 or by being fully vaccinated (Wilf‐Miron et al., 2021). In spite of progress in clinical care for patients and findings in Israel and around the globe indicating the effectiveness of the vaccine through the marked declines in the incidence of SARS‐CoV‐2 infections, hospitalizations, and deaths, as presented by Haas et al. (2021), the management of the pandemic, has been aggravated by the findings that vaccinated individuals can serve as asymptomatic carriers, the evolution and emergence of new, highly transmissible variants (such as the Delta and Omicron variants), alongside the hurdles of different durations of effective immunity or “time‐limited immunity” (Haas et al., 2021; Kosinski, 2020; Puri, Coomes, Haghbayan, & Gunaratne, 2020; Reis et al., 2021). These elements may play a contributing factor in vaccine hesitancy and disbelief in the efficacy of the vaccine. Following the notable decline in immune protection following the two‐dose regime, the health authorities in Israel launched a campaign for vaccinating all those eligible with a third “booster” shot after a 5‐month elapsed period from the second dose of inoculation (Mahase, 2021a; Mahase, 2021b; Porat et al., 2021) Currently, discussions are underway in the government regarding a population‐wide fourth dose vaccination drive (Times of Israel, 2021). Other countries have similarly provided incentive schemes for the public to vaccinate, where governments have proposed or implemented “digital health passes” to provide proof of vaccination and allow for a gradual reopening of the economy, where key sectors such as food, retail, entertainment, and travel could be reinvigorated (Dror et al., 2020; Wilf‐Miron et al., 2021). Some states and countries such as Indonesia, Greece, and Austria, while morally and ethically problematic, have invoked vaccination mandates (Gostin, Cohen, & Shaw, 2021; The Guardian, 2021)..
As the 2‐year mark has approached since the commencement of the COVID‐19 pandemic (November 2019) during which a “wax and wane” battle trajectory has been observed almost globally and afflicted most of the human‐life domains, the concept of “pandemic fatigue” has gained both academic and popular lexicon traction. Pandemic fatigue defined by the WHO as “distress which can result in demotivation to follow recommended protective behaviors, emerging gradually over time and affected by a number of emotions, experiences, and perceptions” has been identified as an additional hurdle and risk factor to adherence to health‐protective behavior by the public (Ala'a, Tarhini, & Akour, 2021). Given the ability to continue to mitigate adverse consequences of the pandemic relies on the public's compliance with health regulations, the phenomenon may have implications for jeopardizing the epidemiological status curves of countries (Ala'a et al., 2021; Bodas & Peleg, 2021). To achieve public health benefits from the various implemented measures, the public's cooperation is crucial (Bodas & Peleg, 2021; Kaim et al., 2021b; Kaim, Jaffe, Siman‐Tov, Khairish, & Adini, 2020). Throughout various phases of the pandemic, it has been identified that among various additional factors—trust, perceived fear, susceptibility, severity of disease, and efficacy of measures play a key role in the mediation process of compliance to protective behavior (Bodas & Peleg, 2020; Kaim et al., 2020; Kaim et al., 2021a; Seale et al., 2020). In the context of Israel, as described by Bodas and Peleg (2021), the various measures taken by the government such as prolonged shutdowns of businesses and school systems and confinements of people to their homes have taken a substantial toll on the public. In light of this information and the evolving conditions of the pandemic, understanding the public's mediation process of compliance to directed protective behavior alongside receptivity of a booster vaccine is essential for the purpose of mitigating the consequences of this ongoing emergency and future such outbreaks. The purpose of the current study was to examine the factors that impact vaccination uptake and additional protective behavior through a cohort study assessing public attitudes during the fourth wave of the pandemic in Israel.
METHODS AND MATERIALS
Study design
The study was conducted during the fourth wave of the pandemic in Israel, in September 2021. A sample of the Israeli population (N = 940) was employed to assess uptake of the third dose of the vaccine (booster) as well as factors implicated in compliance. Recruiting participants for the study was conducted through iPanel, an online internet panel company that consists of over 100,000 members, representing all geographic and demographic sectors of the Israeli population. A stratified sampling method was used, based on data published by the Israeli Central Bureau of Statistics in regard to age, gender, religiosity, and geographic zones.
Participants
The sample size was determined based on The OpenEpi online calculator (https://www.openepi.com/SampleSize), requiring 384 respondents. This was calculated based on the size of the Israeli population, accounting for 9.3 million people, as presented by the Israeli Bureau of Statistics. The study was conducted using a random internet sample of 940 participants who consented to participate voluntarily in the research. To partake in the study, the participants had to confirm their willingness to voluntarily participate in the study. The data were collected anonymously, following the approval of the Ethics Committee of the Tel Aviv University (number 0003846–1 from September 2, 2021).
The study tool
The study was based on a structured questionnaire that included items and indices that were developed specifically for this study, given no prior work had evaluated vaccine uptake for a third dose, as was the case in Israel. The newly developed components of the questionnaire were designed based on a literature review conducted as well as consultation with experts in the field of the behavior of civil society. The questionnaire was validated by five content experts and pilot tested on 20 individuals prior to its dissemination.
Vaccination/illness status
One item assessed vaccination status (“Have you been vaccinated against corona?”) by a multiple‐choice question with possible answers (a) Yes, I got three shots, (b) Yes, I got two shots, (c) Yes, I got one shot, (d) I set a date for a vaccine, (e) I was not vaccinated. One item assessed history of illness diagnosis with COVID‐19 (Yes/No).
Level of compliance to protective measures and attitudes (social distancing and mask wearing)
Two items assessed the level of compliance to protective measures of social distancing and mask wearing in enclosed spaces (“Given the observed increase in the number of infected with COVID‐19 among vaccinated and unvaccinated, to what extent are you now taking care to maintain the following steps compared to the previous waves of the outbreak:”) by a 5‐point Likert scale, scaling from 1 = much more careful, to 5 = much less careful. One item assessed the level of perceived effectiveness of the protective measures of social distancing and mask wearing in enclosed spaces (“To what extent do you think the following measures are effective against COVID‐19”) by a 5‐point Likert scale, scaling from 1 = to a very small extent, to 5 = to a very large extent.
Attitudes toward COVID‐19/vaccine
One item assessed concern regarding the coronavirus (“To what extent are you concerned about the coronavirus outbreak?”) on a 5‐point Likert scale, from 1 = not at all, to 5 = to a very large extent. One item assessed apprehension from getting infected with the coronavirus (“How afraid are you to be infected with the coronavirus?”) on a 5‐point Likert scale, from 1 = to a very small extent, to 5 = to a very large extent). Four items assessed perceived personal threats from the economic, health, security, and political situation in Israel (“In the current situation, how would you rate each of the following situations as threatening to you personally?”) on a 5‐point Likert scale, from 1 = not at all threatening, to 5 = to a very large extent threatening.
Two items assessed the perceived importance of the COVID‐19 vaccine. (“I believe it is important that I be vaccinated against the coronavirus in order to preserve my well‐being, the well‐being of my dear ones, and the well‐being of others in society”) and (“I believe it is important that I get vaccinated against the coronavirus because my family members (or close acquaintances) have been vaccinated or intend to get vaccinated”) on a 5‐point Likert scale, ranging from 1 = do not agree at all, to 5 = agree very much. Trust in the vaccine was assessed by one item (“I believe in the published information about the effectiveness and safety of the corona vaccine”), on a 5‐point Likert scale, ranging from 1 = do not agree at all, to 5 = agree very much. One item assessed “whether fact that the vaccine is effective in preventing severe hospitalizations and mortality is sufficient enough to recommend that the public be vaccinated, even if the vaccine is less effective against infection” on a 4‐point Likert scale, ranging from 1 = Definitely yes, to 4 = Definitely not.
Attitudes toward authorities
One item assessed trust in four organizational authorities (National Ambulance Service, the Health Fund, Ministry of Health, Home Front Command) “To what extent do you trust the following authorities regarding coping with the coronavirus” on a 5‐point Likert scale, from 1 = do not trust at all, to 5 = trust very much.
Demographics
Demographics were assessed by 10 items including gender, year of birth, place of residence, marital status, number of children, number of dependents, education, religion, degree of religiosity, and income.
Statistical analysis
Descriptive statistics were used to analyze the characteristics of the sample. Chi‐square tests were used to evaluate the association between vaccine uptake and threat perception and attitudes toward COVID‐19. Ordinal logistic regression was used for determining the factors affecting vaccination. ANOVA test was used to identify variability between vaccination groups (No dose, 1 dose, two doses, three doses of inoculation). All statistical analyses were performed using SPSS software version 27. p‐values lower than 0.05 were considered to be statistically significant.
RESULTS
The final sample for this study included 940 participants, of which 50.6% (n = 476) were females. The mean age of participants was 40.41 years (14.47 SD), with a minimum age of 18 and maximum age of 70. One hundred thirty‐seven participants (14.6%) reported they were confirmed COVID‐19 cases. The complete socio‐demographic breakdown of the sample is provided in Table 1.
TABLE 1.
Socio‐demographic distribution of studied sample
| Variable | N (%) |
|---|---|
| Gender | |
| Female | 476 (50.6%) |
| Male | 464 (49.4%) |
| Age (mean 40.41, SD 14.47) | |
| 18–35 | 411 (43.7%) |
| 36–55 | 340 (36.2%) |
| 56–70 | 189 (20.1%) |
| Religion | |
| Jewish | 746 (79.4%) |
| Muslim | 122 (13.0%) |
| Druze | 29 (3.1%) |
| Christian | 36 (3.8%) |
| Other | 7 (0.7%) |
| Religiosity | |
| Secular | 384 (40.9%) |
| Traditional | 350 (37.2%) |
| Religious | 120 (12.8%) |
| Ultra‐Orthodox | 81 (8.6%) |
| Other | 5 (0.5%) |
| Place of residence | |
| Haifa & North | 333 (35.4%) |
| Tel‐Aviv & Center | 249 (26.5%) |
| South and Coastline Plain | 195 (20.7%) |
| Greater Jerusalem | 78 (8.3%) |
| HaSharon Region | 85 (9.0%) |
| Family status | |
| Coupled with children | 534 (56.8%) |
| Coupled without children | 143 (15.2%) |
| Single with children | 69 (7.3%) |
| Single without children | 194 (20.6%) |
| Children (under 18 years) | |
| Yes | 422 (44.8%) |
| No | 181 (19.3%) |
| Missing | 337 (35.9%) |
| Education | |
| Up to (including) 8 years | 12 (1.3%) |
| Up to (including) 12 years | 280 (29.8%) |
| Vocational degree | 194 (20.6%) |
| Academic degree | 454 (48.3%) |
| Income | |
| Much below average | 295 (31.4%) |
| Below average | 200 (21.3%) |
| Average | 199 (21.2%) |
| Above average | 129 (13.7%) |
| Much above average | 45 (4.8%) |
| Missing | 72 (7.7%) |
The distribution of the vaccine uptake in the sample was as follows: 453 (48.2%) participants received three doses of the Pfizer (BioNTech) vaccine, 327 (34.8%) received two doses, 47 (5.0%) received a single dose, and 113 (12.0%) participants were unvaccinated. Of those vaccinated with three doses, only 1.8% reported being previously confirmed for COVID‐19. Of those vaccinated with two doses, this figure rose to 12.8%, and among unvaccinated to 41.1%. Forty (85%) of those vaccinated with a single dose were confirmed with COVID‐19, in line with the policy to provide a single dose to those recovered from COVID‐19.
Participants vaccinated with two doses (N = 380) were asked if they would be willing to take the third dose. Ninety‐four (24.7%) replied they will surely get it, 110 (28.9%) indicated they would probably get it, 132 (34.7%) indicated they would probably not get it, and 44 (11.6%) said they will surely refuse it. Of the 170 unvaccinated participants, three (2.8%) said they will surely get the vaccine, 23 (21.5%) indicated they would probably get it, an additional 23 (21.5%) indicated they would probably not get it, and 58 (54.2%) said they will surely refuse it.
Participants were asked if the fact that the vaccine is effective in reducing severe morbidity and mortality, even if it does not entirely prevent infection is sufficient for recommending it to the public. While 64% of those vaccinated with three doses replied “Yes, for sure,” only 32% of participants who received two doses and 3% of the unvaccinated replied the same. More than half (55%) of the unvaccinated indicated that it is “surely not” sufficient to recommend vaccination.
Analysis for socio‐demographic differences between individuals vaccinated, once, twice, three times, or not vaccinated with the COVID‐19 vaccine yielded the following results. There was no statistically significant difference in the distribution of gender between the groups (p = 0.052). Age was associated with higher vaccine uptake. The mean age of unvaccinated participants (35.91 ± 12.79 SD) and those vaccinated with two doses (35.58 ± 12.33 SD) was lower than those vaccinated with three doses (45.62 ± 12.66 SD), according to the ANOVA test (F = 59.30, df = 2, p < 0.001).
The results indicate that vaccination uptake is negatively associated with the level of religiosity. Among those vaccinated with three doses, half defined themselves as secular, and half as non‐secular (religious and traditional). However, among those vaccinated with two doses and those who are unvaccinated, non‐secular individuals account for 63% and 74%, respectively (χ 2 = 24.58, df = 2, p < 0.001). The higher level of education is associated with vaccination uptake, as well. The ratio of academics to non‐academics among those vaccinated with three doses is 55%–45%, respectively, whereas among those vaccinated with two doses this ratio changes to 46%–54%, and among unvaccinated individuals, the representation is 30% academics versus 70% non‐academic (χ 2 = 23.81, df = 2, p < 0.001). Furthermore, unvaccinated individuals also reported lower income compared to the vaccinated groups (data not shown).
As expected from their relative distribution in the Israeli population, in all three vaccination uptake groups, the portion of Jews is larger than that of the Arab population. However, as the vaccination uptake increases, the relative portion of the Arabs decreases: 14% among those vaccinated with three doses, 26% among those vaccinated in two doses, and 31% among those unvaccinated are Arab. Notably, Arabs comprise approximately 20% of the Israeli population according to Israel's Central Bureau of Statistics.
Compared to unvaccinated and vaccinated with two doses, participants who received three doses of vaccine were more worried about COVID‐19 (F = 12.833, p < 0.001), more scared of contracting the disease (F = 11.898, p < 0.001), more inclined to be threatened by the economic (p < 0.001) and political situation (p = 0.022), and to demonstrate higher levels of trust in authorities (F = 172.701, p < 0.001), in the vaccine (F = 115.603, p < 0.001) and in the vaccine importance (F = 269.353, p < 0.001)—all according to the ANOVA test. See complete figures in Figure 1.
FIGURE 1.
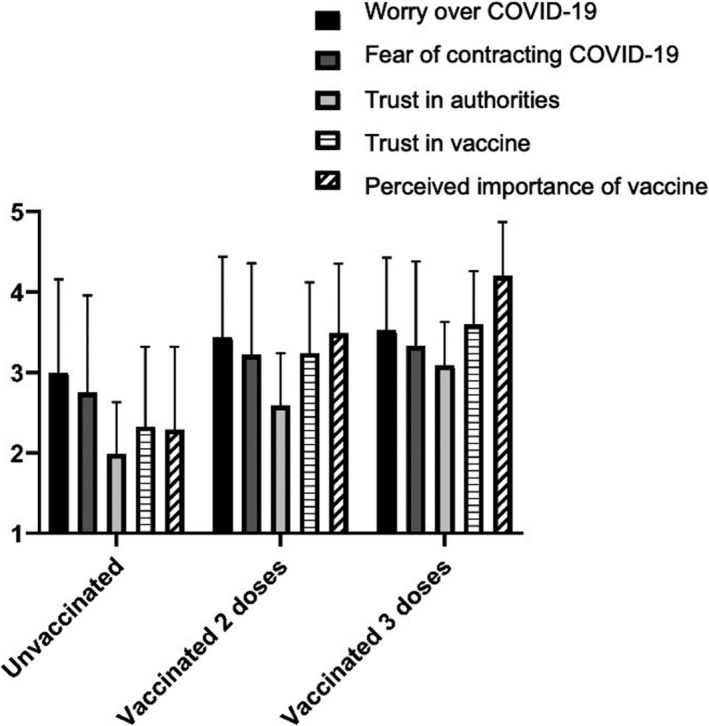
Attitudes (means and standard deviations) toward COVID‐19 outbreak and vaccine according to vaccination uptake status (N = 940). Source: Authors' analysis of data from iPanel
Vaccine uptake is also associated with compliance with other COVID‐19 related health regulations. Close to 86% of participants vaccinated with three doses indicated they complied with mask wearing during the fourth wave more than during previous waves, compared to 79% and 63% among those vaccinated with two doses and unvaccinated, respectively (χ 2 = 16.52, df = 2, p < 0.001). Similarly, two‐thirds (67%) of participants vaccinated with three doses indicated they complied more with maintaining social/physical distance from others during the fourth wave than during previous waves, compared to 53% and 50% reported by those vaccinated with two doses and unvaccinated, respectively (χ 2 = 10.88, df = 2, p = 0.004).
Despite the relatively high compliance rate to health recommendations, all three groups tended to view the efficacy of mask wearing and social distancing on COVID‐19 prevention as limited. Nevertheless, perception of efficacy increased to a certain degree with vaccination uptake. For example, the mean score for the perceived efficacy of mask wearing among participants vaccinated with three doses was 2.75 (±0.58 SD), compared to 2.51 (±0.78 SD) and 2.23 (±0.83 SD) among those vaccinated with two doses and unvaccinated (ANOVA F = 28.25, df = 2, p < 0.001).
An ordinal logistic regression analysis to investigate the effect of variables on vaccine uptake was conducted. The predictor variables were tested a priori to verify there was no multicollinearity. The full model was a significant improvement in fit over the null model (χ 2 = 166.47, df = 24, p < 0.001) and explains 35.4% of the total variance of the dependent variable. The results of the regression analysis indicate that the odds of participants perceiving the vaccine as important to accept more doses of the vaccine were 2.624 (95% CI: 1.812, 3.798) times that of participants who perceive the importance of the vaccine as low, a statistically significant effect, Wald χ 2(1) = 26.117, p < 0.001. An increase in age was associated with an increase in the odds of vaccine dose uptake, with an odds ratio of 1.043 (95% CI: 1.024, 1.062), Wald χ 2(1) = 19.833, p < 0.001. The results also suggest that non‐Jewish participants were 0.536 (95% CI: 0.310, 0.925) times less likely to comply with vaccination, compared with the Jewish participants, and those non‐academic participants were 0.621 (95% CI: 0.388, 0.994) times less likely to accept the vaccine, compared with academic participants. The complete results of the regression analysis are provided in Table 2.
TABLE 2.
Results of ordinal logistic regression analysis to predict vaccine doses uptake (N = 940)
| Parameter | B | Std. error | Wald chi‐Square | Sig. | Exp (B) | 95% Wald confidence interval for Exp (B) | |
|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||
| Threshold | |||||||
| Unvaccinated | 2.312 | 0.9303 | 6.175 | 0.013 | 10.094 | 1.630 | 62.512 |
| Vaccinated with 2 doses | 5.506 | 0.9733 | 32.009 | 0.000 | 246.257 | 36.554 | 1658.958 |
| Gender = female | −0.205 | 0.2401 | 0.726 | 0.394 | 0.815 | 0.509 | 1.305 |
| Gender = male (Ref.) | 1 | ||||||
| Religion = non‐Jewish | −0.624 | 0.2788 | 5.014 | 0.025 | 0.536 | 0.310 | 0.925 |
| Religion = Jewish (Ref.) | 1 | ||||||
| Religiosity = religious | −0.299 | 0.2471 | 1.464 | 0.226 | 0.742 | 0.457 | 1.204 |
| Religiosity = secular (Ref.) | 1 | ||||||
| Education = non‐academic | −0.477 | 0.2402 | 3.942 | 0.047 | 0.621 | 0.388 | 0.994 |
| Education = academic (Ref.) | 1 | ||||||
| Worry over COVID‐19 = 1 | −1.308 | 0.7947 | 2.710 | 0.100 | 0.270 | 0.057 | 1.283 |
| Worry over COVID‐19 = 2 | −0.691 | 0.5542 | 1.553 | 0.213 | 0.501 | 0.169 | 1.485 |
| Worry over COVID‐19 = 3 | 0.036 | 0.4416 | 0.007 | 0.934 | 1.037 | 0.436 | 2.465 |
| Worry over COVID‐19 = 4 | −0.289 | 0.3884 | 0.553 | 0.457 | 0.749 | 0.350 | 1.604 |
| Worry over COVID‐19 = 5 (Ref.) | 1 | ||||||
| Fear of infection = 1 | 1.120 | 0.6367 | 3.092 | 0.079 | 3.064 | 0.880 | 10.673 |
| Fear of infection = 2 | −0.065 | 0.4876 | 0.018 | 0.895 | 0.938 | 0.361 | 2.438 |
| Fear of infection = 3 | 0.361 | 0.4265 | 0.715 | 0.398 | 1.434 | 0.622 | 3.309 |
| Fear of infection = 4 | 0.630 | 0.3996 | 2.482 | 0.115 | 1.877 | 0.858 | 4.107 |
| Fear of infection = 5 (Ref.) | 1 | ||||||
| Vaccine is sufficiently effective = 1 | −0.622 | 0.6602 | 0.888 | 0.346 | 0.537 | 0.147 | 1.958 |
| Vaccine is sufficiently effective = 2 | 0.071 | 0.3984 | 0.032 | 0.859 | 1.073 | 0.492 | 2.344 |
| Vaccine is sufficiently effective = 3 | −0.139 | 0.2760 | 0.253 | 0.615 | 0.870 | 0.507 | 1.495 |
| Vaccine is sufficiently effective = 4 (Ref.) | 1 | ||||||
| Social distance = comply much less | 0.580 | 0.6050 | 0.918 | 0.338 | 1.785 | 0.545 | 5.845 |
| Social distance = comply less | 0.205 | 0.4774 | 0.185 | 0.667 | 1.228 | 0.482 | 3.130 |
| Social distance = comply more | −0.096 | 0.3304 | 0.085 | 0.771 | 0.908 | 0.475 | 1.736 |
| Social distance = comply much more (Ref.) | 1 | ||||||
| Mask wearing = comply much less | −0.378 | 0.6108 | 0.383 | 0.536 | 0.685 | 0.207 | 2.268 |
| Mask wearing = comply less | −0.486 | 0.4846 | 1.006 | 0.316 | 0.615 | 0.238 | 1.590 |
| Mask wearing = comply more | 0.128 | 0.3122 | 0.169 | 0.681 | 1.137 | 0.617 | 2.097 |
| Mask wearing = comply much more (Ref.) | 1 | ||||||
| Age (cont.) | 0.042 | 0.0094 | 19.833 | 0.000 | 1.043 | 1.024 | 1.062 |
| Trust in authorities (cont.) | 0.283 | 0.2581 | 1.206 | 0.272 | 1.328 | 0.801 | 2.202 |
| Vaccine importance (cont.) | 0.965 | 0.1887 | 26.117 | 0.000 | 2.624 | 1.812 | 3.798 |
Bold values are significant at p‐value < 0.05 (two‐tailed).
DISCUSSION
The fourth wave of the COVID‐19 outbreak in Israel and the massive “booster” vaccination campaign provided a valuable setting for evaluating the effect of the pandemic fatigue on compliance with vaccination. At the time of conducting the study, the virus has impacted Israeli and global communities for close to 2 years. As Israel was the first country to initiate a massive “booster” vaccination campaign, this investigation offers the setting of evaluating the pandemic fatigue effect on vaccination efforts.
In this study, we show that vaccine hesitancy remains to be a major barrier to full population inoculation, where even among those that received the initial two doses of the vaccine when asked about their willingness to receive a third booster dose, over 45% indicated they would probably not get it or said they will surely refuse it. Of those unvaccinated, over 75% indicated the same. Arguably, the vaccine hesitancy of the “booster vaccine” observed among those that received the initial two doses can be attributed to the “pandemic fatigue” phenomenon. In the context of this population, the reluctance perhaps does not reflect a conscious refusal of the vaccine as the previous inoculation was observed, but rather fatigue from the politicization of the issue where the swarming of arguments from both sides results in bewilderment and lack of uptake (Lewis, 2020). As discussed by Lewis (2020), the subject of the pandemic has become highly politicized, with partisanship impacting attitudes regarding uptake of protective behavior, the validity of COVID‐19 statistics, as well as with respect to the development of the vaccine (Abbas, 2021). Additionally, the booster vaccination campaigns may have predictably further heightened the resistance of individuals who are unvaccinated with initial doses turning them into “hard‐core refusers” as the campaign may have brought into question the effectiveness of the vaccine in the first place (Hoffman, 2021).
In line with previous findings throughout the H1N1 pandemic and precursory stages of the COVID‐19 outbreak (Al‐Amer et al., 2022; Kaim et al., 2021b; Lazarus et al., 2021; Seale et al., 2010; Wang et al., 2020), the bivariate analysis shows a significant association between vaccine uptake and threat perception of COVID‐19, the political and economic situation, levels of trust in authorities, vaccine importance and uptake of additional health regulations and the perception of their efficacy. However, in the multivariate analysis, most of these associations are nullified where the predictors that remain are sociodemographic (age, religion, and academic status) and the perception of the importance and efficacy of the vaccine. These findings effectively demonstrate “pandemic fatigue” at play where the background noise about trust and fear tactics to motivate the public is no longer relevant. Instead, the findings indicate that at this stage of the pandemic, focusing on the robustness and the rigorous science behind the vaccine is more promising regarding effectiveness than trying to regain public trust.
The findings also suggest that risk communication employment of fear tactics is losing its capacity to generate motivation for vaccination (Dermody et al., 2021). As previously used effective messaging dwindles its influence on protective behavior, reinvigorating tactics must be sought after that identify priority population groups and test new initiatives that make careful consideration of new understandings of drivers and barriers to compliance. High‐ quality, evidence‐informed, tailored communication should be directed to key population groups.
Policy implications of vaccination in light of these findings indicate the need for decision‐making regarding vaccination to be made on objective criteria and create structural conditions for health equity. Consistency in messaging is a key component for improving vaccination uptake, where recommendations should always be in line with epidemiological risk, and consistent with other implemented responses and recommendations to avoid mixed messaging by various stakeholders. Furthermore, communication as part of vaccination campaigns must employ transparency and rationale for recommendations, while also acknowledging the limits of science and the government in predicting the development of the pandemic and what vaccination measures may be necessary at any later stage. The scientific soundness of the vaccination, its efficacy and importance should be relayed to the public by trustworthy figures, namely physicians and researchers, as opposed to politicians and government representatives (Topf & Williams, 2021; Falcone & Sapienza, 2020). As the pandemic becomes a chronic threat and is normalized into our daily lives, the type of information that interests the public changes as well. In earlier stages of the pandemic, information concerning preventive measures to avoid contracting the disease was most sought after (Sulistyawati et al., 2021); however, at this point in time, such information is less demanded by the public and attention to risk cues decreases, as is vivid in the reduction in levels of concern (author's unpublished data – under review). The results of this study suggest that under such circumstances, making information accessible to the public requires focusing the message on the science behind the vaccine and its safety, efficacy, and importance. Providing valid, effective, efficient, and continuous information is of crucial importance (Sulistyawati et al., 2021).
The findings lastly highlight the importance of tailor‐making the risk communication and information messaging to target groups. In particular, minorities, those of younger age, unvaccinated and non‐booster vaccinated individuals should be targeted with different risk communication approaches that take into consideration the unique features of each group. Alternatively put, simply relaying scientific information the to the public is not sufficient. Messages need to be adapted, to accommodate specific concerns and hesitations demonstrated by these distinct groups. Future research may be warranted to identify these modalities more clearly.
This study offers important insights into understanding the mediation process of the public during a fourth wave of the COVID‐19 ongoing crisis where the effects of pandemic fatigue have begun to cascade on vaccination efforts. In particular, this study found that fear and trust in authorities are no longer relevant for motivating uptake of vaccination, rather it is advisable that the evidence for the efficacy of the vaccine must be available and provided to the public. The socio‐demographic predictor data also shows that sectors of the population are more hesitant than others, such as those of younger age, more religious backgrounds, and of non‐academic status, and that targeted interventions for these populations must be considered to increase compliance with vaccination measures.
LIMITATIONS
This study has several limitations. First, this study employs the use of non‐validated tools that were designed for the purpose of this research. Although efforts have been made to make the tool reliable through experts' consultations, the conclusions of this study should be taken with caution. Second, this study utilized an online panel to collect responses. While this option provides immediate access to a diverse sample of the population on a wide geographic distribution, it may limit the generalization of the conclusion to people with high digital literacy. Third, although this study was able to capture a sizeable portion of unvaccinated participants, it is difficult to assess whether or not these participants are representative of this group. It is reasonable to assume that additional archetypes of unvaccinated people may have been excluded from this study based on the enrollment process through an online panel. Lastly, a conclusion of the study was that younger age was associated with lower uptake of vaccination, however, it must be taken into consideration that young people started getting vaccinated at a later point in time due to the gradual opening of the vaccination campaign, thus fewer were eligible for a third vaccine at the time of the study, potentially impacting on our findings.
CONCLUSIONS
The results of this study suggest that at the stage of the COVID‐19 pandemic, characterized by pandemic fatigue, trust in authorities, and even threat perception components, such as concern and fear of contracting the disease, are incapable of predicting vaccination uptake. Instead, perception of the importance of the vaccine and its effectiveness are predictive of vaccination uptake. The findings indicate that at this stage of the pandemic, focusing on the robustness of the science behind the vaccine is more important than trying to regain public trust. The findings also suggest that risk communication employing fear tactics is losing its capacity to generate motivation for vaccination.
CLINICAL RESOURCES
-
Analysis: Pandemic Fatigue makes the case for boosters a harder sell (Source: Reuters)
-
Pandemic fatigue—reinvigorating the public to prevent COVID‐19: policy framework for supporting pandemic prevention and management: revised version November 2020 (Source: World Health Organization)
SOURCE OF SUPPORT
This work did not receive any external funding.
CONFLICT OF INTERESTS
The authors declare they have no competing interests.
Bodas, M. , Kaim, A. , Velan, B. , Ziv, A. , Jaffe, E. & Adini, B. (2022). Overcoming the effect of pandemic fatigue on vaccine hesitancy—Will belief in science triumph?. Journal of Nursing Scholarship, 00, 1–10. 10.1111/jnu.12778
Moran Bodas and Arielle Kaim are joined first authors.
Funding information
This research received no external funding.
REFERENCES
- Abbas, A. H. (2021). Politicizing COVID‐19 vaccines in the press: A critical discourse analysis. International Journal for the Semiotics of Law‐Revue internationale de Sémiotique juridique, 1–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al‐Amer, R. , Maneze, D. , Everett, B. , Montayre, J. , Villarosa, A. R. , Dwekat, E. , & Salamonson, Y. (2022). COVID‐19 vaccination intention in the first year of the pandemic: A systematic review. Journal of Clinical Nursing, 31(1–2), 62–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ala'a, B. , Tarhini, Z. , & Akour, A. (2021). A swaying between successive pandemic waves and pandemic fatigue: Where does Jordan stand? Annals of Medicine and Surgery, 65, 102298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alpert, E. A. , Herbst, R. , Abramovich, I. , Strugo, R. , & Jaffe, E. (2021). Mass COVID‐19 vaccination of residents in geriatric facilities by emergency medical services: The Israeli experience. The Lancet Healthy Longevity, 2(4), e189–e190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodas, M. , & Peleg, K. (2020). Self‐isolation compliance in the covid‐19 era influenced by compensation: Findings from a recent survey in Israel: Public attitudes toward the covid‐19 outbreak and self‐isolation: A cross sectional study of the adult population of Israel. Health Affairs, 39(6), 936–941. [DOI] [PubMed] [Google Scholar]
- Bodas, M. , & Peleg, K. (2021). Pandemic fatigue: The effects of the COVID‐19 crisis on public trust and compliance with regulations in Israel: The study examines the effects of the COVID‐19 crisis on public trust and compliance with regulations in Israel. Health Affairs, 40(8), 1225–1233. [DOI] [PubMed] [Google Scholar]
- Dermody, T. S. , DiMaio, D. , & Enquist, L. W. (2021). Vaccine safety, efficacy, and trust take time. Annual Review of Virology, 8, iii–iv. [DOI] [PubMed] [Google Scholar]
- The Guardian . (2021). Do covid vaccine mandates work? Retrieved December 18, 2021, from https://www.theguardian.com/world/2021/dec/03/do‐covid‐vaccine‐mandates‐work
- Dror, A. A. , Eisenbach, N. , Taiber, S. , Morozov, N. G. , Mizrachi, M. , Zigron, A. , Srouji, S. , & Sela, E. (2020). Vaccine hesitancy: The next challenge in the fight against COVID‐19. European Journal of Epidemiology, 35(8), 775–779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falcone, R. , & Sapienza, A. (2020). How COVID‐19 changed the information needs of Italian citizens. International Journal of Environmental Research and Public Health, 17(19), 6988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flaxman, S. , Mishra, S. , Gandy, A. , Unwin, H. J. T. , Mellan, T. A. , Coupland, H. , Whittaker, J. , Zhu, H. , Berah, T. , Eaton, W. E. , Monod, M. , Imperial College COVID‐19 Response Team , Ghani, A. C. , Donnelly, C. A. , Riley, S. , Vollmer, M. A. C. , Ferguson, N. M. , Okell, L. C. , & Bhatt, S. (2020). Estimating the effects of non‐pharmaceutical interventions on COVID‐19 in Europe. Nature, 584(7820), 257–261. [DOI] [PubMed] [Google Scholar]
- Gostin, L. O. , Cohen, I. G. , & Shaw, J. (2021). Digital health passes in the age of COVID‐19: Are “vaccine passports” lawful and ethical? JAMA, 325(19), 1933–1934. [DOI] [PubMed] [Google Scholar]
- Haas, E. J. , Angulo, F. J. , McLaughlin, J. M. , Anis, E. , Singer, S. R. , Khan, F. , Brooks, N. , Smaja, M. , Mircus, G. , Pan, K. , Southern, J. , Swerdlow, D. L. , Jodar, L. , Levy, Y. , & Alroy‐Preis, S. (2021). Impact and effectiveness of mRNA BNT162b2 vaccine against SARS‐CoV‐2 infections and COVID‐19 cases, hospitalisations, and deaths following a nationwide vaccination campaign in Israel: An observational study using national surveillance data. The Lancet, 397(10287), 1819–1829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hale, T. , Angrist, N. , Goldszmidt, R. , Kira, B. , Petherick, A. , Phillips, T. , Webster, S. , Cameron‐Blake, E. , Hallas, L. , Majumdar, S. , & Tatlow, H. (2021). A global panel database of pandemic policies (Oxford COVID‐19 government response tracker). Nature Human Behaviour, 5(4), 529–538. [DOI] [PubMed] [Google Scholar]
- The Times of Israel . (2021). Health minister suggests fourth vaccine dose amid rising fears of Fifth covid wave. Retreived December 18, 2021, from https://www.timesofisrael.com/health‐minister‐suggests‐fourth‐vaccine‐dose‐amid‐rising‐fears‐of‐fifth‐covid‐wave//
- Hoffman J. (2021). Boosters are complicating efforts to persuade the unvaccinated to get shots. The New York Times. Retreived December 18, 2021, from https://www.nytimes.com/2021/10/11/health/covid‐boosters‐unvaccinated.html
- Kaim, A. , Jaffe, E. , Siman‐Tov, M. , Khairish, E. , & Adini, B. (2020). Impact of a brief educational intervention on knowledge, perceived knowledge, perceived safety, and resilience of the public during COVID‐19 crisis. International Journal of Environmental Research and Public Health, 17(16), 5971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaim, A. , Siman‐Tov, M. , Jaffe, E. , & Adini, B. (2021a). Effect of a concise educational program on COVID‐19 vaccination attitudes. Frontiers in Public Health, 9, 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaim, A. , Siman‐Tov, M. , Jaffe, E. , & Adini, B. (2021b). Factors that enhance or impede compliance of the public with governmental regulation of lockdown during COVID‐19 in Israel. International Journal of Disaster Risk Reduction, 66, 102596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kosinski, R. J. (2020). The influence of time‐limited immunity on a COVID‐19 epidemic: A simulation study. MedRxiv, 1, 1–9. [Google Scholar]
- Lai, S. , Ruktanonchai, N. W. , Zhou, L. , Prosper, O. , Luo, W. , Floyd, J. R. , Wesolowski, A. , Santillana, M. , Zhang, C. , Du, X. , Yu, H. , & Tatem, A. J. (2020). Effect of non‐pharmaceutical interventions to contain COVID‐19 in China. Nature, 585(7825), 410–413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus, J. V. , Ratzan, S. C. , Palayew, A. , Gostin, L. O. , Larson, H. J. , Rabin, K. , & El‐Mohandes, A. (2021). A global survey of potential acceptance of a COVID‐19 vaccine. Nature Medicine, 27(2), 225–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis, J. R. (2020, November). What is driving the decline in people's willingness to take the COVID‐19 vaccine in the United States?. In JAMA Health Forum (Vol. 1, No. 11, p. e201393). American Medical Association. [DOI] [PubMed] [Google Scholar]
- Mahase, E. (2021a). Covid‐19 booster vaccines: What we know and who’s doing what. British Medical Association, 374, n2082. [DOI] [PubMed] [Google Scholar]
- Mahase, E. (2021b). Covid‐19: Booster vaccine to be rolled out in autumn as UKsecures 60m more Pfizer doses. British Medical Association, 373(1116), 10–1136. [DOI] [PubMed] [Google Scholar]
- Porat, T. , Burnell, R. , Calvo, R. A. , Ford, E. , Paudyal, P. , Baxter, W. L. , & Parush, A. (2021). “Vaccine passports” may backfire: Findings from a cross‐sectional study in the UKand Israel on willingness to get vaccinated against COVID‐19. Vaccine, 9(8), 902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puri, N. , Coomes, E. A. , Haghbayan, H. , & Gunaratne, K. (2020). Social media and vaccine hesitancy: New updates for the era of COVID‐19 and globalized infectious diseases. Human Vaccines & Immunotherapeutics, 16(11), 2586–2593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reis, B. Y. , Barda, N. , Leshchinsky, M. , Kepten, E. , Hernán, M. A. , Lipsitch, M. , Dagan, N. , & Balicer, R. D. (2021). Effectiveness of BNT162b2 vaccine against delta variant in adolescents. New England Journal of Medicine, 385(22), 2101–2103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosen, B. , Waitzberg, R. , Israeli, A. , Hartal, M. , & Davidovitch, N. (2021). Addressing vaccine hesitancy and access barriers to achieve persistent progress in Israel's COVID‐19 vaccination program. Israel Journal Health Policy Research, 10(1), 1–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seale, H. , Dyer, C. E. , Abdi, I. , Rahman, K. M. , Sun, Y. , Qureshi, M. O. , Dowell‐Day, A. , & Islam, M. S. (2020). Improving the impact of non‐pharmaceutical interventions during COVID‐19: Examining the factors that influence engagement and the impact on individuals. BMC Infectious Diseases, 20(1), 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seale, H. , Heywood, A. E. , McLaws, M. L. , Ward, K. F. , Lowbridge, C. P. , Van, D. , & MacIntyre, C. R. (2010). Why do I need it? I am not at risk! Public perceptions towards the pandemic (H1N1) 2009 vaccine. BMC Infectious Diseases, 10(1), 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shilo, S. , Rossman, H. , & Segal, E. (2021). Signals of hope: Gauging the impact of a rapid national vaccination campaign. Nature Reviews Immunology, 21(4), 198–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sulistyawati, S. , Rokhmayanti, R. , Aji, B. , Wijayanti, S. P. M. , Hastuti, S. K. W. , Sukesi, T. W. , & Mulasari, S. A. (2021). Knowledge, attitudes, practices and information needs during the covid‐19 pandemic in Indonesia. Risk Management and Healthcare Policy, 14, 163–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Topf, J. M. , & Williams, P. N. (2021). COVID‐19, social media, and the role of the public physician. Blood Purification, 50(4–5), 595–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, J. , Jing, R. , Lai, X. , Zhang, H. , Lyu, Y. , Knoll, M. D. , & Fang, H. (2020). Acceptance of COVID‐19 vaccination during the COVID‐19 pandemic in China. Vaccine, 8(3), 482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilf‐Miron, R. , Myers, V. , & Saban, M. (2021). Incentivizing vaccination uptake: The “green pass” proposal in Israel. JAMA, 325(15), 1503–1504. [DOI] [PubMed] [Google Scholar]


