Abstract
Purpose
To report a novel case of unilateral peripheral facial nerve palsy manifesting as a complication of Herpes simplex keratitis.
Observations
A 51-year-old immunocompetent male presented with severe eye pain for 3 weeks. He was found to have Herpes simplex keratitis in the left eye and started on valacyclovir 3g per day for 10 days. At three weeks his pain and blurred vision resolved. He returned 2.5 months later with worsening of vision and five days of unilateral facial numbness and weakness. Ocular evaluation revealed a visual acuity of 20/25 in the left eye, which showed mid-stromal corneal edema bordered by several keratoprecipitates. Both the keratitis and Bell's palsy markedly improved with valacyclovir, topical prednisolone, and a 10-day course of oral prednisone.
Conclusions and Importance
This is the first reported case of Bell's palsy accompanying disciform keratitis. Both entities have been observed to be caused by Herpes simplex, however they have not been described together in one patient. Knowledge that these conditions may present simultaneously allows for earlier identification and treatment, resulting in decreased morbidity.
Keywords: Herpes simplex, Bell's palsy, Disciform keratitis, Herpes simplex keratitis
1. Introduction
Bell's palsy is an acute unilateral facial paralysis caused by dysfunction of the peripheral portion of cranial nerve VII. It is an idiopathic process which is, by definition, a diagnosis of exclusion. It is a lower motor neuron process; it can be distinguished from upper motor neuron disease by involvement of the frontalis. In upper motor neuron disease, the upper face would be spared, however in Bell's palsy all facial muscles of expression may be affected, causing incomplete closure of the eyelids and exposure keratopathy. Although Bell's palsy often resolves without treatment, current recommendations suggest treating with systemic steroids and/or acyclovir, even though most cases resolve even without treatment.1
Herpes simplex virus can cause disease in any area of the eye. There is a >50% seroprevalence of HSV-1 in United States adults.2 With regard to the cornea, the virus can manifest in many ways. HSV-1 affects ocular tissue more commonly than other serotypes.2 Early in the disease process, virus enters the corneal epithelium and stroma via sensory nerves. If untreated it can continue to infect additional parts of the cornea. Stromal keratitis is also very common, especially in recurrent disease. Findings include stromal edema and haze. Immune reaction to the herpes virus is effective in destroying the virus but leads to damage of the cornea as well.3
The endothelium may become involved as well. In endothelialitis, keratic precipitates collect on the endothelial surface. It is believed that this may be caused by active viral infection of the endothelium, or it may be an inflammatory response to the endothelium itself. Similarly, disciform keratitis is a specific pattern of endothelialitis, frequently observed as a circular zone of stromal edema within the central cornea accompanied by keratic precipitates.3 Both forms of endothelialitis may be effectively treated with topical steroids and oral antivirals.4
2. Case report
A 51-year-old male presented to the eye clinic with severe left-sided eye pain and blurring of vision which had been worsening for weeks. He had no known past medical or ocular history, and had recently been in another country where he sought care for his developing eye pain. He reported that a doctor had removed a foreign body from the left eye and he was prescribed tobramycin/dexamethasone drops four times per day for two weeks. Despite the medical treatment, he noted that his pain and blurring had worsened three days prior to presentation.
On physical examination, the patient's vision was 20/20 in the right eye and 20/80 in the left eye. Intraocular pressure was 11 mmHg OD and 10 mmHg OS, and there was no relative afferent pupillary defect. On slit lamp examination he had moderate conjunctival injection and two large dendritic lesions with prominent terminal bulbs on the left cornea (Fig. 1). Fundus evaluation was unremarkable. He was started on oral valacyclovir 1 g three times per day for fourteen days and switched from tobramycin/dexamethasone to topical moxifloxacin four times per day. Herpes simplex titers were obtained; HSV 1 and HSV 2 IgM negative, HSV 1 IgG 52.70, HSV 2 IgG negligible.
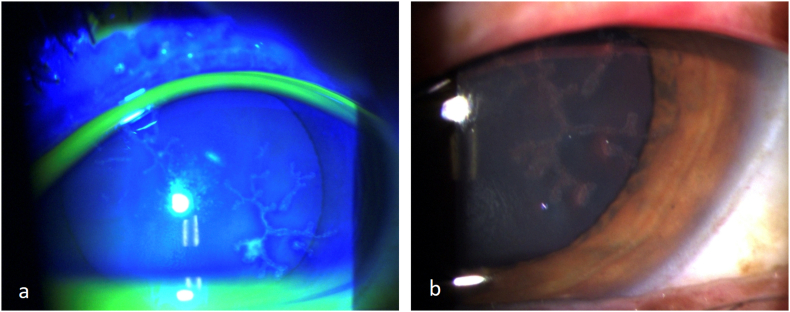
Fig. 1.
a,b. Slit lamp photos showing dendritic figures with (a) and without fluorescein (b).
Eight days later the patient presented for follow up. At this time his pain had completely resolved, but he continued to have blurred vision with visual acuity of 20/80 in the affected eye. On slit lamp examination the dendrites had been replaced by a severe confluent superficial punctate keratitis. The moxifloxacin was stopped and switched to preservative-free artificial tears four to six times per day with erythromycin ointment at night.
Seventeen days after initial presentation he returned to clinic having completed the course of valacyclovir. He had been using preservative-free artificial tears and erythromycin ointment as prescribed. His vision had returned to 20/20 in the affected eye, and the epithelial changes had resolved. He was advised to stop all drops and ointment and return in two weeks.
The patient returned two months and fifteen days later reporting five days of blurred vision in the left eye accompanied by numbness of the left side of his face. His vision was 20/20 in the right eye and 20/25 in the left eye. Examination of the face revealed a decrease in sensation of the upper and lower left face with subtle drooping of the upper and lower left face. He had no difficulty with closing the left eye, despite a slight lagophthalmos with asymmetry of his smile and poor forehead wrinkling. Slit lamp examination revealed endothelialitis of the left eye with fine filamentary keratic precipitates in the center of the cornea (Fig. 2). He was prescribed another ten-day course of valacyclovir 1 g three times per day and started on oral prednisone 60 mg for seven days for Bell's palsy. Preservative-free artificial tears were ordered.
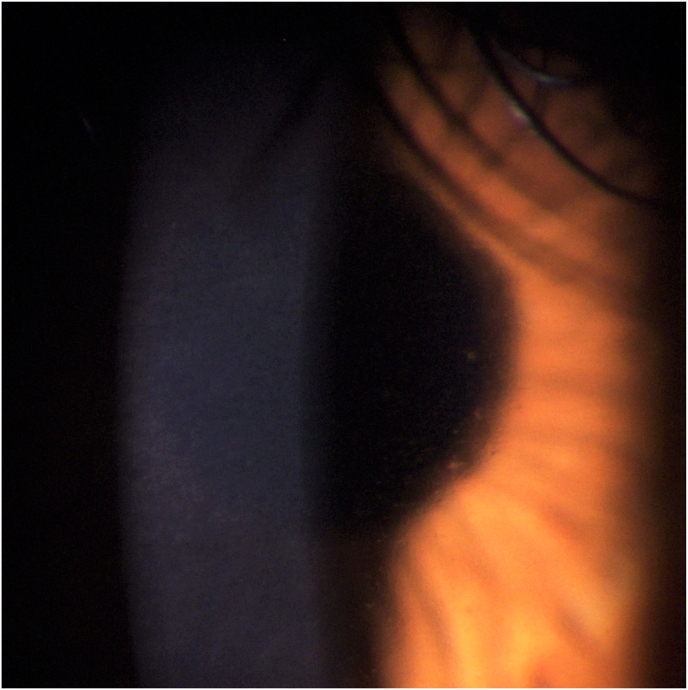
Fig. 2.
Slit lamp photo showing endotheliialitis as fine, filamentary keratic precipitates best seen at pupillary edge and in center of the cornea.
He returned one month and twenty-six days later with decreased vision and persistent Bell's palsy. He had completed the course of valacyclovir and prednisone and was using preservative-free artificial tears as prescribed. His left-sided facial weakness had mostly recovered, though he continued to show a slight decrease in sensation of the left upper eyelid and cheek. Visual acuity was 20/20 in the right eye and 20/50 in the left eye. The endothelialitis had developed into a disciform keratitis with corneal edema and haze (Fig. 3). At this time the patient was prescribed valacyclovir 3 g per day for ten days, followed by prophylactic valacyclovir 1 g per day. He was also prescribed prednisolone acetate 1% eight times per day for four days then four times per day for two weeks duration and slowly tapered.
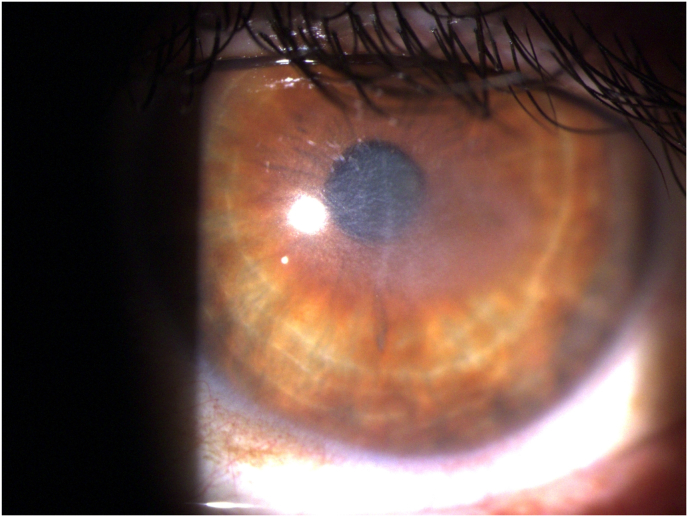
Fig. 3.
Disciform keratitis with corneal haze, edema, and filamentary keratic precipitates on the endothelium.
The patient is still recovering from the disciform keratitis and his Bell's palsy has completely resolved. At this follow up his vision was 20/20 in the right eye and 20/40 in the left eye. The corneal haze, edema, and endothelialitis have significantly improved. He is currently on prednisolone acetate 1% four times per day while continuing valacyclovir 1 g daily.
3. Discussion
Herpes simplex keratitis is a common and sight-threatening disease, estimated to affect 500,000 people in the United States alone.5 HSV1 and HSV2 have both been proven to cause lesions in the cornea, though HSV1 is the most common cause of HSV keratitis.2 HSV characteristically may result in ocular lesions in the eye after trauma like the reported foreign body in our patient, especially when treated with corticosteroids. Herpes simplex virus can present in numerous ways, including dendritic and disciform keratitis as seen in our patient, or more subtly as blepharoconjunctivitis or as a progressive ulceration centrally or peripherally.6
Two-thirds of acute facial weakness is known to be caused by Bell's palsy. This condition is caused by weakness of the peripheral facial nerve.7 The role that HSV plays in causing Bell's palsy is controversial. Several studies show evidence that HSV reactivation in the facial nerve is linked to the development of Bell's palsy. One such study found HSV1 in 11 of 14 patients' endoneurial ‘fluid of the facial nerve that was obtained during decompression surgery of patients with Bell's palsy.8 However, no clear cause has been determined, and it therefore remains a diagnosis of exclusion. It is often self-limited, however many patients continue to have residual deficits even after treatment. Studies have been done to determine the best treatment approach for Bell's palsy, and the consensus is that antivirals in addition to steroids are more effective than steroids alone.9
A similar presentation of facial nerve palsy was reported in a patient with Herpes zoster ophthalmicus.10 The patient had vesicular lesions of the trigeminal dermatome with involvement of the distribution of the ophthalmic branch, with pseudodendrites on the cornea. Three weeks later he displayed symptoms of Bell's palsy of the ipsilateral face. This case offers further evidence that Herpesviruses may be causative of Bell's palsy. Our patient's elevated HSV 1 IgG levels and corneal findings suggest Herpes simplex activation in temporal proximity to his development of Bell's palsy.
Despite the fact that disciform keratitis and Bell's palsy are known complications of HSV infection, to date there have been no case reports demonstrating a patient with simultaneous development of disciform keratitis and Bell's palsy symptoms. Based on the evidence, we recommend treating disciform keratitis associated with Bell's palsy with oral antivirals, topical steroids, and systemic steroids. The keratitis should be treated, as it may lead to sight-threatening complications, and even though Bell's palsy typically resolves on its own, prevention of residual deficits should be in the patient's best interest.
In conclusion, we report a novel case of Bell's palsy associated with HSV1-induced disciform keratitis. The patient described above has had complete resolution of his Bell's palsy symptoms, and his disciform keratitis has markedly improved with treatment. The presence of HSV1 in association with Bell's palsy does not appear to be related to the prognosis of the disease,11 however the knowledge that HSV1 is implicated in a patient's disease may help clinicians be more vigilant in examining eyes for Herpes simplex keratitis and lead to earlier treatment with lower morbidity.
Patient consent
Consent to publish this case was not obtained. This report does not contain any personal information that could lead to the identification of the patient.
Funding
No funding or grant support.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Declaration of competing interest
The following authors have no financial disclosures: PF, TW, PW, MM, HP.
Acknowledgements
None.
References
- 1.Mavrikakis I. Facial nerve palsy: anatomy, etiology, evaluation, and management. Orbit. 2008;27(6):466–474. doi: 10.1080/01676830802352543. [DOI] [PubMed] [Google Scholar]
- 2.Rowe A., St Leger A., Jeon S., et al. Herpes simplex. Prog Retin Eye Res. 2013;32C:88–101. doi: 10.1016/j.preteyeres.2012.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liesegang T.J. Ocular herpes simplex infection: pathogenesis and current therapy. Mayo Clin Proc. 1988;63(11):1092–1105. doi: 10.1016/s0025-6196(12)65504-9. [DOI] [PubMed] [Google Scholar]
- 4.Liesegang T.J. Herpes simplex virus epidemiology and ocular importance. Cornea. 2001;20(1):1–13. doi: 10.1097/00003226-200101000-00001. [DOI] [PubMed] [Google Scholar]
- 5.Azher T.N., Yin X.T., Tajfirouz D., et al. Herpes simplex keratitis: challenges in diagnosis and clinical management. Clin Ophthalmol. 2017;11:H1. doi: 10.2147/OPTH.S80475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Valerio G.S., Lin C.C. Ocular manifestations of herpes simplex virus. Curr Opin Ophthalmol. 2019;30(6):525–531. doi: 10.1097/ICU.0000000000000618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kennedy P. Herpes simplex virus type 1 and Bell's palsy - a current assessment of the controversy. J Neurovirol. 2010;16:1–5. doi: 10.3109/13550284.2010.522868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Murakami S., Mizobuchi M., Nakashiro Y., et al. Bell palsy and herpes simplex virus: identification of viral DNA in endoneurial fluid and muscle. Ann Intern Med. 1996;124:27–30. doi: 10.7326/0003-4819-124-1_part_1-199601010-00005. [DOI] [PubMed] [Google Scholar]
- 9.Kim Y., Doo J., Chon J., et al. Steroids plus antiviral agents are more effective than steroids alone in the treatment of severe Bell's palsy patients over 40 years of age. Int J Immunopathol Pharmacol. 2021;35:1–9. doi: 10.1177/20587384211042124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wakil S.M., Ajlan R., Arthurs B. Herpes zoster ophthalmicus complicated by ipsilateral isolated Bell's palsy: a case report and review of the literature. Can J Ophthalmol. 2020;47(4):339–343. doi: 10.1016/j.jcjo.2012.04.007. [DOI] [PubMed] [Google Scholar]
- 11.Ordoñez G., Vales O., Pineda B., et al. The presence of herpes simplex-1 and varicella zoster viruses is not related with clinical outcome of Bell's Palsy. Virology. 2020;549:85–88. doi: 10.1016/j.virol.2020.07.020. [DOI] [PubMed] [Google Scholar]