Abstract
Aim
To identify groups of nurses engaging in coronavirus disease (COVID‐19) care who are most in need of organizational support.
Background
Overwhelming stress and susceptibility to burnout have been reported in nurses during the COVID‐19 pandemic.
Methods
Nurses working at five hospitals that accepted COVID‐19 patients answered the questionnaire. The Tokyo Metropolitan Distress Scale for Pandemic, Self‐Diagnosis Check List for Assessment of Workers' Accumulated Fatigue and Japanese Burnout Scale were evaluated. Multiple regression analysis was performed to examine the relationship between engaging in COVID‐19 care and psychosocial/physical burden.
Results
In total, 895 questionnaires were analysed. With experience in caring for COVID‐19 patients as the independent variable, nurses caring for suspected cases had significantly higher standardized Tokyo Metropolitan Distress Scale for Pandemic scores for ‘concerns for infection’ (standardized partial regression coefficient β = .921, P = .004), Assessment of Workers' Accumulated Fatigue (β = .445, P = .022) and Japanese Burnout Scale ‘emotional exhaustion’ (β = .136, P = .021) than those caring for confirmed cases.
Conclusions
Nurses caring for suspected COVID‐19 patients have the highest psychological/physical burden and propensity for burnout.
Implications for Nursing Management
Extensive support systems are required for nurses caring for confirmed and suspected COVID‐19 cases.
Keywords: burnout, COVID‐19, nurses, occupational health, pandemic
1. BACKGROUND
Nurses play a critical role in patients' care during the coronavirus disease (COVID‐19) pandemic. Nurses caring for COVID‐19 patients must wear personal protective equipment (PPE) in enclosed, highly infective environments. This allows them to provide treatment to patients without anxiety, fear and tension of getting infected at work (Zhan et al., 2020). They also face discrimination and prejudice for offering care to COVID‐19 patients and struggle in their responsibilities and sense of duty as professionals supporting medical care (Japanese Nursing Association, 2020). Compared with other professionals, nurses have a higher workload that can overwhelm them. In the COVID‐19 era, nurses are challenged by having to work in a new context and setting and are exhausted due to heavy workloads and long work shifts, and they have to manage relationships with patients' families (Adachi et al., 2005; Mori & Kageyama, 1995), alongside the fear of becoming infected and infecting others. Thus, nurses are burdened by significant work pressure and stress due to the COVID‐19 pandemic, in addition to those due to the usual clinical practice (Kim et al., 2021; Kuo et al., 2020). This burden on the mental health of nurses and the importance of support for nurses have been noted since the early days of the COVID‐19 pandemic (Galanis et al., 2021; Hammond et al., 2021; Hendy et al., 2020; Hoseinabadi et al., 2020; Zhang et al., 2020). Burnout of nurses is a significant problem (Adachi et al., 2005; Kowalczuk et al., 2019; Liao et al., 2020; Mori & Kageyama, 1995). Chronic stress further increases the risk of burnout and predisposes the affected nurses to severe symptoms of depression (Kim et al., 2021; Kubo, 2007; Setou et al., 2020).
During the course of the prolonged threat of COVID‐19, nurses play an important role in responding to the COVID‐19 spread and providing care to patients (Ke et al., 2021). It is thus essential to prevent nurses from resigning from their jobs to ensure sufficient staffing. To achieve this goal, it is crucial to protect nurses' mental and physical health, help them feel fulfilled in their work and prevent vulnerability to burnout through organizational initiatives (Labrague & de Los Santos, 2021). Thus, it is necessary to share data on the severity of the psychosocial and physical burdens experienced by nurses during the pandemic with hospital management. However, studies on nursing tasks related to COVID‐19 in Japan are limited. Although nurses caring for COVID‐19 patients are vulnerable to burnout (Matsuo et al., 2020), there is limited knowledge available on what kind of support would help prevent this burnout.
As a public hospital organization, the Kanagawa Prefectural Hospital Organization responded rapidly to the request of the Kanagawa Prefecture to allocate beds for and accept COVID‐19 patients. The Kanagawa Prefectural Hospital Organization comprises five hospitals (1692 beds in total), each of which provides specialized healthcare services and continues to provide routine care while accommodating confirmed and suspected COVID‐19 patients. This organization was therefore suitable for conducting a comprehensive survey of nurses caring for COVID‐19 patients. This study surveyed nurses caring for COVID‐19 patients to evaluate and compare their stress, fatigue and burnout levels. Furthermore, we aimed to identify the groups that would benefit most from organizational support and to explore the elements of effective support tailored to the group characteristics. This study aimed to show the status of stress among nurses providing COVID‐19 care and identify the group with the highest potential for burnout. Our findings provide information to other medical care facilities with various degrees of involvement in providing efficient COVID‐19 care.
2. METHODS
2.1. Study participants
A questionnaire‐based survey was administered from 1 to 14 March 2021 to 1622 nurses working at the five hospitals of the Kanagawa Prefectural Hospital Organization, namely, the General Hospital, Cardiovascular & Respiratory Center, Cancer Center, Children's Medical Center and Psychiatric Center. The General Hospital and the Cardiovascular & Respiratory Center accepted COVID‐19 patients with moderate disease severity (requiring oxygen therapy), whereas the other three hospitals accepted those with mild or suspected COVID‐19, needing specialized care. The inclusion criteria for this study were being a full‐time nursing staff in any of the above five hospitals. Those who were unable to receive the questions because they were on leave during the survey period were excluded.
2.2. Data collection
Data on the participants' age, sex, nursing experience, hospital, department, position, department and individual experience in caring for COVID‐19 patients, marital status, cohabitation status and answers to survey questions related to the types of support they needed were collected using questionnaires. The questionnaires were distributed to each nursing unit by the nursing department staff. The nurses who responded to the questionnaire placed the answered questionnaire in a prepared envelope, sealed, and placed it in a collection box. The nursing department staff could not ascertain who had or had not responded. Four scales were used to evaluate the burden, propensity for burnout and coping strategies of the participants. Psychological and social burdens were evaluated using nine items in the Tokyo Metropolitan Distress Scale for Pandemic (Shiwaku et al., 2021). Physical burden was evaluated using the 20‐item Self‐Diagnosis Check List for Assessment of Workers' Accumulated Fatigue (Ministry of Health, 2008), a tool developed for self‐assessment of accumulated fatigue by workers. The propensity for burnout was evaluated using 17 items in the Japanese Burnout Scale comprising three subscales, namely, ‘emotional exhaustion’, ‘depersonalization’ and ‘personal accomplishment’ (Kubo, 2014; Kubo & Tao, 1994). Coping was assessed using 18 items in the Brief Scales of Coping Profile comprising six subscales ‘active solution’, ‘avoidance and suppression’, ‘changing mood’, ‘changing point of view’, ‘seeking help for solution’ and ‘emotional expression involving others’ (Kageyama et al., 2004). The total score of the subscales were used for the Tokyo Metropolitan Distress Scale for Pandemic. A score of ≥14 points, the cut‐off for detecting moderate or severe symptoms of depression and anxiety, was defined as Tokyo Metropolitan Distress Scale for Pandemic‐positive (Shiwaku et al., 2021). Workers' accumulated fatigue scores were calculated by combining the scores of the questions related to subjective symptoms and work status, according to the specified methods of the scale (Ministry of Health, 2008). The total Japanese Burnout Scale and Brief Scales of Coping Profile scores were purposefully not analysed; rather, only the subscale scores were used for analysis.
2.3. Evaluation of nurses' mental stress
Tokyo Metropolitan Distress Scale for Pandemic, Japanese Burnout Scale subscale and Assessment of Workers' Accumulated Fatigue scores were used to evaluate the mental status of nurses. The Tokyo Metropolitan Distress Scale for Pandemic is a simple tool used to detect depression and anxiety by comprehensively assessing psychosocial factors that may affect the mental health and motivation of healthcare workers during the COVID‐19 pandemic (Shiwaku et al., 2021). It includes the following questions.
During the PAST TWO WEEKS, how frequently were you concerned about the following?
COVID‐19 infection of oneself
You have no control over whether you have COVID‐19 or not.
People around you avoid you because of your occupation.
These three scores were evaluated based on the participants' involvement in COVID‐19 care. Next, it was described using the following categorical variables: ‘department acceptance of COVID‐19 patients’ and ‘individual experience caring for COVID‐19 patients’. As none of the participating facilities were designated COVID‐19 hospitals, departments within the hospitals have different practices to prevent the spread of COVID‐19 infection to patients staying at the hospitals for other diseases. We assessed this as an important variable for describing the role in COVID‐19 care. However, providing COVID‐19 patient care often requires flexibility among workers and performance of tasks beyond their usual job description. This would limit department acceptance of COVID‐19 as an accurate measure of participant experience in providing COVID‐19 care, which necessitated the addition of this item to the questionnaire. Neither variable was binomially classified by whether they worked in a COVID‐19 care unit, but into three classes, including caring for suspected patients. Caring for suspected COVID‐19 patients exposed nurses to levels of various burdens comparable to that for confirmed patients, which was taken into consideration, as high infectivity demands equivalent caution and preventive measures for infection in initial care. Therefore, COVID‐19 patient care was divided into the following classes at the department level: ‘accepting confirmed COVID‐19 patient’, ‘accepting suspected COVID‐19 patients only’ and ‘not accepting either confirmed or suspected COVID‐19 patients’. At the individual level, data were analysed using the following classes: ‘experience caring for confirmed COVID‐19 patients’, ‘experience caring for suspected COVID‐19 patients only’ and ‘no experience in caring for either confirmed or suspected COVID‐19 patients’. The Tokyo Metropolitan Distress Scale for Pandemic has not been adequately evaluated for reliability and validity because it was developed after the 2020 COVID‐19 pandemic. However, in studies conducted by the group that developed the scale, it was found to be correlated with the Patient Health Questionnaire‐9 (PHQ‐9) (Kroenke et al., 2001) and the Generalized Anxiety Disorder‐7 Scale (GAD‐7) (Spitzer et al., 2006) (Matsumoto et al., 2021; Shiwaku et al., 2021). The validity and reliability of the other two scales were described elsewhere (Kubo, 2007; Sasaki et al., 2005, 2007; Xue et al., 2008). Both scales were mainly developed and validated in Japanese populations, especially in the occupational health field.
2.4. Ethical approval
This study was approved by the Institutional Review Boards of the authors' institutions. The aims and methods of the study were explained to the participants prior to handing out the questionnaire. The submission of the questionnaire was interpreted as consent to participate in the study. This study complied with the STrengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines.
2.5. Statistical analysis
To evaluate the effects of involvement in COVID‐19 care on the primary outcome, a multiple regression analysis was performed with the two variables describing involvement in COVID‐19 care as the independent variables for the separate regression equations, with the total Assessment of Workers' Accumulated Fatigue, Tokyo Metropolitan Distress Scale for Pandemic and Japanese Burnout Scale subscale scores as the dependent variables. Age, nursing experience, department, hospital, marital status (yes/no), living with children (yes/no) and the Brief Scales of Coping Profile subscale were used as adjustment factors. In all statistical analyses, the statistical software R Version 3.6.1. (Ihaka & Gentleman, 1996) was used, and a two‐tailed test with a significance level of .05 was performed. Detailed information about the statistical analysis performed in this study is included in the supplemental information.
3. RESULTS
3.1. Study participants
Of the 1622 nurses surveyed, 998 (61.5%) returned the questionnaires, and the responses of 103 nurses (10.3%) were excluded because of missing data. Thus, we analysed questionnaire data of 895 nurses. A total of 88.5% participants were women, and most were in their 20s (30.4%). Approximately half (45.7%) had at least 15 years of nursing experience. Furthermore, 33.1% of the participants worked in departments that accepted COVID‐19 patients, whereas 23.8% worked in those that accepted suspected cases only. Overall, 37.5% of the participants had experience of providing care for COVID‐19 patients, and 23.9% had experience of caring for suspected cases only. Of these, 22.6% worked in hospitals that accepted patients with up to moderate COVID‐19 disease severity, and 77.4% worked in those that only accepted mild COVID‐19 cases. Details of participant demographics are shown in Table 1.
TABLE 1.
Characteristics of nurses participating in the study (N = 895)
| Total | General Hospital | Cardiovascular & Respiratory Center | Cancer Center | Children's Medical Center | Psychiatric Center | |
|---|---|---|---|---|---|---|
| (N = 895) | (n = 121, 13.5%) | (n = 81, 9.0%) | (n = 268, 29.9%) | (n = 279, 31.1%) | (n = 146, 16.3%) | |
| Severity of accepted COVID‐19 patients | Moderate | Moderate | Mild | Mild | Mild | |
| Sex | ||||||
| Male | 103 (11.5) | 6 (5.0) | 7 (8.6) | 15 (5.6) | 22 (7.9) | 53 (36.3) |
| Female | 792 (88.5) | 115 (95.0) | 74 (91.4) | 253 (94.4) | 257 (92.1) | 93 (63.7) |
| Age, years | ||||||
| 20–29 | 272 (30.4) | 28 (23.1) | 23 (28.4) | 98 (36.6) | 103 (36.9) | 20 (13.7) |
| 30–39 | 193 (21.6) | 25 (20.7) | 10 (12.3) | 64 (23.9) | 73 (26.2) | 21 (14.4) |
| 40–49 | 220 (24.6) | 32 (26.4) | 24 (29.6) | 63 (23.5) | 54 (19.4) | 47 (32.2) |
| 50–59 | 184 (20.6) | 29 (24.0) | 20 (24.7) | 41 (15.3) | 45 (16.1) | 49 (33.6) |
| 60–69 | 26 (2.9) | 7 (5.8) | 4 (4.9) | 2 (0.7) | 4 (1.4) | 9 (6.2) |
| Nursing work experience, years | ||||||
| <1 | 49 (5.5) | 6 (5.0) | 4 (4.9) | 20 (7.5) | 18 (6.5) | 1 (0.7) |
| 1–3 | 113 (12.6) | 13 (10.7) | 5 (6.2) | 48 (17.9) | 42 (15.1) | 5 (3.4) |
| 3–6 | 107 (12.0) | 12 (9.9) | 7 (8.6) | 29 (10.8) | 46 (16.5) | 13 (8.9) |
| 6–9 | 80 (8.9) | 8 (6.6) | 10 (12.3) | 18 (6.7) | 25 (9.0) | 19 (13.0) |
| 9–15 | 137 (15.3) | 14 (11.6) | 13 (16.0) | 45 (16.8) | 46 (16.5) | 19 (13.0) |
| ≥15 | 409 (45.7) | 68 (56.2) | 42 (51.9) | 108 (40.3) | 102 (36.6) | 89 (61.0) |
| Position | ||||||
| Nursing staff | 615 (68.7) | 75 (62.0) | 54 (66.7) | 206 (76.9) | 199 (71.3) | 81 (55.5) |
| Chief | 240 (26.8) | 39 (32.2) | 22 (27.2) | 55 (20.5) | 68 (24.4) | 56 (38.4) |
| Section head | 32 (3.6) | 6 (5.0) | 3 (3.7) | 6 (2.2) | 9 (3.2) | 8 (5.5) |
| Nurse manager | 8 (0.9) | 1 (0.8) | 2 (2.5) | 1 (0.4) | 3 (1.1) | 1 (0.7) |
| Department | ||||||
| Ward | 674 (75.3) | 86 (71.1) | 58 (71.6) | 174 (64.9) | 227 (81.4) | 129 (88.4) |
| Outpatient | 107 (12.0) | 19 (15.7) | 11 (13.6) | 55 (20.5) | 16 (5.7) | 6 (4.1) |
| Operation room | 50 (5.6) | 3 (2.5) | 6 (7.4) | 22 (8.2) | 19 (6.8) | 0 (0) |
| Other | 64 (7.2) | 13 (10.7) | 6 (7.4) | 17 (6.3) | 17 (6.1) | 11 (7.5) |
| Marital status | ||||||
| Married | 403 (45.0) | 60 (49.6) | 39 (48.1) | 99 (36.9) | 107 (38.4) | 98 (67.1) |
| Not married | 492 (55.0) | 61 (50.4) | 42 (51.9) | 169 (63.1) | 172 (61.6) | 48 (32.9) |
| Cohabitation status | ||||||
| Yes | 572 (63.9) | 87 (71.9) | 51 (63.0) | 160 (59.7) | 159 (57.0) | 115 (78.8) |
| No | 323 (36.1) | 34 (28.1) | 30 (37.0) | 108 (40.3) | 120 (43.0) | 31 (21.2) |
| Living with children | ||||||
| Yes | 295 (33.0) | 53 (43.8) | 29 (35.8) | 71 (26.5) | 65 (23.3) | 77 (52.7) |
| No | 600 (67.0) | 68 (56.2) | 52 (64.2) | 197 (73.5) | 214 (76.7) | 69 (47.3) |
| Departments acceptance of COVID‐19 patients | ||||||
| None | 386 (43.1) | 38 (31.4) | 21 (25.9) | 98 (36.6) | 163 (58.4) | 66 (45.2) |
| Suspected cases | 213 (23.8) | 30 (24.8) | 18 (22.2) | 93 (34.7) | 32 (11.5) | 40 (27.4) |
| Confirmed cases | 296 (33.1) | 53 (43.8) | 42 (51.9) | 77 (28.7) | 84 (30.1) | 40 (27.4) |
| Experience in caring for COVID‐19 patients | ||||||
| None | 345 (38.5) | 27 (22.3) | 8 (9.9) | 75 (28.0) | 193 (69.2) | 42 (28.8) |
| Suspected cases | 214 (23.9) | 10 (8.3) | 13 (16.0) | 119 (44.4) | 44 (15.8) | 28 (19.2) |
| Confirmed cases | 336 (37.5) | 84 (69.4) | 60 (74.1) | 74 (27.6) | 42 (15.1) | 76 (52.1) |
Note: Data are presented as n (%).
Abbreviation: COVID‐19, coronavirus disease.
3.2. Tokyo Metropolitan Distress Scale for Pandemic, Japanese Burnout Scale and Brief Scales of Coping Profile
According to the exploratory factor analysis, the number of factors detected for the Tokyo Metropolitan Distress Scale for Pandemic, Japanese Burnout Scale and Brief Scales of Coping Profile scales were 3, 3, and 6, respectively, showing the expected internal consistency of the subscales (Figures S1–S3, Tables S1–S3). Cronbach's α coefficients of reliability for the Tokyo Metropolitan Distress Scale for Pandemic, Japanese Burnout Scale and Brief Scales of Coping Profile were .75, .87 and .77, respectively. The mean Tokyo Metropolitan Distress Scale for Pandemic score of the included participants was 14.04 points (SD: 4.92), with 50.9% of the participants scoring ≥14 points (95% confidence interval [CI], 47.6%–54.3%).
The total mean Tokyo Metropolitan Distress Scale for Pandemic scores were compared among nurses at the departmental (stratified by acceptance of COVID‐19 cases: none, suspected cases only, confirmed cases only) and individual levels (stratified by experience in caring for COVID‐19 patients based on disease severity) (Figure 1). Nurses who worked in departments accepting confirmed cases had the highest total mean Tokyo Metropolitan Distress Scale for Pandemic score (14.67 points), and those who had experience in caring for suspected COVID‐19 patients scored the highest (15.43 points). For determining the involvement in COVID‐19 care at the department or individual level, one‐way analysis of variance (ANOVA) was performed among the following three levels: no acceptance at all, acceptance of suspected cases and acceptance of suspected and confirmed cases; it showed significant differences (P < .001 for all comparisons). The Tukey–Kramer tests of comparison between the two groups resulted in a difference of 1.37 points between the departments accepting confirmed cases and those not accepting any COVID‐19 cases (P < .001) and a difference of 1.21 points between the departments accepting suspected cases and those not accepting any COVID‐19 cases (P = .11). There was no significant difference between the departments accepting confirmed cases only and those accepting suspected cases only (P = .92). Regarding the nurses' work experience, nurses with experience in caring for suspected cases scored the highest (P < .01). No difference was noted between the nurses with no experience and those with experience in caring for confirmed cases (P = .17).
FIGURE 1.
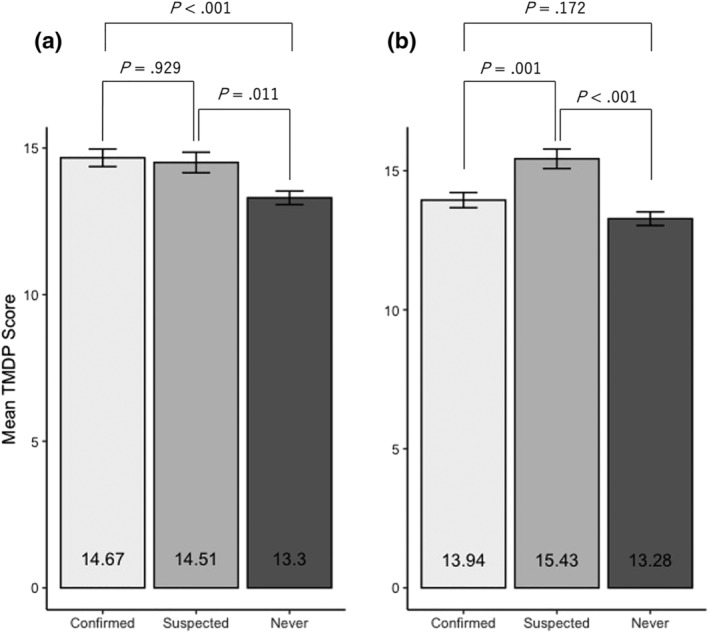
Mean Tokyo Metropolitan Distress Scale for Pandemic (TMDP) total score of nurses. The total score of the Tokyo Metropolitan Distress Scale for Pandemic stratified by the departments' acceptance status of coronavirus disease (COVID‐19) patients (a) and nurse experience in caring for COVID‐19 patients (b). The labels under the bars represent the COVID‐19 patient care classes: ‘confirmed COVID‐19 patients’, ‘suspected COVID‐19 patients only’ and ‘not accepting or no experiences in caring for either confirmed or suspected COVID‐19 patients’. Error bars represent standard errors. To avoid over‐detection of multiple testing, the Tukey–Kramer test was used to compare each group after significant differences were confirmed among the three groups by one‐way analysis of variance (ANOVA). The P‐values shown in this figure are calculated by Tukey–Kramer test
3.3. Involvement in COVID‐19 care and Tokyo Metropolitan Distress Scale for Pandemic, Japanese Burnout Scale and Brief Scales of Coping Profile scores
Multiple regression analysis revealed that the adjusted standardized scores for Tokyo Metropolitan Distress Scale for Pandemic subscales ‘concerns for infection’ (standardized partial regression coefficient β = −.542, P = .044) and ‘social stress’ (β = −.652, P = .001) were significantly lower in nurses working in non‐COVID‐19 departments than those in departments accepting confirmed COVID‐19 patients (Table 2). Nurses working in departments that only accepted suspected cases had significantly lower standardized scores for ‘social stress’ than those in departments accepting confirmed cases (β = −.522, P = .017).
TABLE 2.
Multiple regression analysis
| TMDP | JBS | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Concerns of infection | Social stress | AWAF | Emotional exhaustion | Depersonalization | Personal accomplishment | |||||||
| β | SE | β | SE | β | SE | β | SE | Β | SE | β | SE | |
| Departments acceptance of COVID‐19 patients | ||||||||||||
| Confirmed | ||||||||||||
| Suspected | −.106 | .316 | −.106* | .316 | −.106 | .316 | .105 | .061 | −.004 | .045 | −.002 | .038 |
| Never | −.542* | .269 | −.542** | .269 | −.542 | .269 | .014 | .053 | −.068 | .039 | −.028 | .033 |
| R 2 | .124 | .445 | .211 | .267 | .280 | .223 | ||||||
| Adjusted R 2 a | .111 | .089 | .197 | .256 | .268 | .210 | ||||||
| Experience in caring for COVID‐19 patients | ||||||||||||
| Confirmed | ||||||||||||
| Suspected | .921** | .316 | .196 | .226 | .445* | .193 | .136* | 0.059 | .038 | .046 | .032 | .039 |
| Never | .158 | .299 | −.317 | .208 | .089 | .182 | .067 | 0.052 | −.012 | .043 | −.034 | .036 |
| R 2 | .129 | .092 | .213 | .277 | .225 | .129 | ||||||
| Adjusted R 2 a | .115 | .082 | .199 | .266 | .212 | .115 | ||||||
AWAF, Assessment of Workers' Accumulated Fatigue; COVID‐19, coronavirus disease; JBS, Japanese Burnout Scale; R 2, coefficient of determination; SE, standard error; TMDP, Tokyo Metropolitan Distress Scale for Pandemic; β, standardized partial regression coefficient.
Adjusted for age, department, hospital, marital status, living with children and the six subscales of Brief Scales for Coping Profiles.
P < .05.
P < .01.
P < .001.
However, different trends were noted when we used COVID‐19 nursing experience as the independent variable. Nurses who only cared for suspected cases had significantly higher standardized scores for Tokyo Metropolitan Distress Scale for Pandemic ‘concerns for infection’ (β = .921, P = .004), Assessment of Workers' Accumulated Fatigue (β = .445, P = .022) and Japanese Burnout Scale ‘emotional exhaustion’ (β = .136, P = .021) than those for confirmed cases. No other statistically significant differences were found for the other scales. The variance inflation factor was adequately low for all regression equations used (Tables S4–S7).
3.4. Correlation among Tokyo Metropolitan Distress Scale for Pandemic, Japanese Burnout Scale and Brief Scales of Coping Profile scores
Significant positive correlations were observed among all subscales (P < .001). High correlations were noted between the Japanese Burnout Scale subscales ‘emotional exhaustion’ and ‘depersonalization’ (.710, P < .001). A correlation was also observed between the Assessment of Workers' Accumulated Fatigue and Japanese Burnout Scale subscale ‘emotional exhaustion’ (.671, P < .001) (Table 3).
TABLE 3.
Correlation matrix (N = 896)
| TMDP | AWAF | JBS | |||||
|---|---|---|---|---|---|---|---|
| Concerns for infection | Social stress | Emotional exhaustion | Depersonalization | Personal accomplishment | |||
| TMDP | Concerns for infection | ||||||
| Social stress | 0.302*** | ||||||
| AWAF | 0.384*** | 0.375*** | |||||
| JBS | Emotional exhaustion | 0.392*** | 0.327*** | 0.671*** | |||
| Depersonalization | 0.29*** | 0.373*** | 0.49*** | 0.71*** | |||
| Personal accomplishment | 0.121*** | 0.155*** | 0.234*** | 0.313*** | 0.295*** | ||
Note: The values indicate Pearson's correlation coefficients.
Abbreviations: AWAF, Assessment of Workers' Accumulated Fatigue; JBS, Japanese Burnout Scale; TMDP, Tokyo Metropolitan Distress Scale for Pandemic.
P < .001.
4. DISCUSSION
4.1. High‐stress group providing COVID‐19 care
In this study, nurses who cared for COVID‐19 patients were under high stress according to the Tokyo Metropolitan Distress Scale for Pandemic scores. This is consistent with the findings of previous studies that reported stress among nurses providing COVID‐19 care; high stress status was reported among the nurses caring for COVID‐19 patients evaluated by various scoring systems, such as Self‐rating Anxiety Scale (SAS) and PHQ‐9 (Hoseinabadi et al., 2020; Zhang et al., 2020). Thus, nurses offering care to COVID‐19 patients suffer high stress and require optimal support. Of note, nurses caring for suspected COVID‐19 patients scored high in the Tokyo Metropolitan Distress Scale for Pandemic subscale ‘concerns about infection’, in this study, showing that support for nurses offering care to suspected patients is a priority.
In contrast to confirmed patients who are treated in a specialized ward by specialized professionals, suspected patients are often accepted in general wards. Nurses managing their care are required to practise infection measures similar to those of caring for confirmed patients while following stringent zoning to isolate them from general patients to avoid infection outbreaks (Ingram et al., 2021). This places them under constant stress and pressure, likely subjecting them to added psychological stress. Furthermore, uncertain situations are closely linked to tolerance to uncertainty and are noted as a common component of various mental health problems, such as anxiety and depression (Carleton, 2016; Grupe & Nitschke, 2013). Repeatedly working with suspected patients only who may or may not be infected may be a factor contributing to high scores (Carleton, 2016). To our knowledge, this is the first study to consider the type of nurses' roles in COVID‐19 care. This topic has not been investigated in the context of other infectious diseases, such as severe acute respiratory syndrome (SARS) and novel influenza virus infections.
4.2. Risk of burnout
Previous studies have shown that nurses providing COVID‐19 patient care were at a high risk of burnout (Hoseinabadi et al., 2020; Matsuo et al., 2020; Setou et al., 2020; Zhang et al., 2020); the present study found that nurses caring for suspected COVID‐19 patients were at an even higher risk of burnout. The strong correlations noted among the Tokyo Metropolitan Distress Scale for Pandemic, Japanese Burnout Scale and Brief Scales of Coping Profile scores suggested that the accumulation of psychological and social burden and fatigue contributed to burnout.
Numerous studies have reported that work overload aggravates stress and is closely linked to the onset of burnout (Galanis et al., 2021; Hendy et al., 2020; Kuo et al., 2020; Zhan et al., 2020). COVID‐19 care places an additional workload on nurses (Zhan et al., 2020), including coordinating unexpected acceptance of patients and transport for transfers, wearing and removing PPE, other reinforced infection measures, medical care assistance and nursing care for patients whose conditions deteriorate rapidly. In addition, nurses have to keep their contact time with patients short to avoid getting themselves infected. Nursing is founded on paying individualized attention to patients to holistically treat them and respecting individual dignity through healing and staying by the patient's side (Ogiwara et al., 2020). The combination of powerlessness that nurses feel when they are prevented from delivering such holistic care and pressures related to infection measures compounded with anxiety seemed to worsen their emotional and physical exhaustion from the heavy workload. Furthermore, departments that accept confirmed cases operate with adequate nurse staffing and better conditions to account for the additional and more difficult tasks that nurses must perform. In contrast, departments that only accept suspected cases continue to carry out routine care while accommodating COVID‐19 patients with the same level of nurse staffing, which increases the workload of nurses (Furubayashi, 2021). Nurses working in departments converted into COVID‐19 units cannot decide who to accept at their discretion, which may make them feel fatigued rather than fulfilled. This likely results in even greater exhaustion in nurses, which requires closer monitoring for burnout (Kubo, 2007).
4.3. Support for nurses providing COVID‐19 care
Our findings showed that support is equally important for nurses caring for confirmed and suspected COVID‐19 patients. It is ideal to establish specialized wards for the care of suspected cases. Otherwise, clarifying zoning and patient assignment is vital to alleviate nurses' anxiety and stress. A safe and secure support programme implemented to that end should be based on expert knowledge and information on infection measures, guidance on techniques, evaluation and monitoring (Setou et al., 2020). Experts in psychiatry and clinical psychology should also be included in the establishment of such support programmes to provide mental support to nurses. Finally, work should be clearly allocated and regularly modified with planned rotations to allow for advanced preparation (Chemali et al., 2019; Kubo & Tao, 1994).
5. LIMITATIONS
This study had some limitations. First, because we used a questionnaire survey design, the outcomes may be affected by selection bias. Second, although the cross‐sectional design showed similarities among participants, causality could not be determined as we did not conduct any follow‐up survey. Third, we did not evaluate the pre‐COVID‐19 conditions; thus, changes in stress and fatigue over time could not be compared. A follow‐up or interventional study is required to confirm our findings and develop interventional methods adapted for various group characteristics. Fourth, a comparison of the nurses with more experience in COVID‐19 care (in terms of number of patients with COVID‐19 cared for) and nurses with a small experience would be beneficial. We did not include information in this regard in this study (e.g. number of patients with COVID‐19 cared for or duration of experience in COVID‐19 care). Thus, future studies evaluating this difference are warranted.
6. CONCLUSIONS
Our findings revealed that nurses providing care for COVID‐19 patients are subjected to heavy mental and social burdens. Nurses caring for suspected patients had the highest levels of mental and social burden, fatigue accumulation and emotional exhaustion and were at the highest risk of burnout. Therefore, they require adequate support equivalent to that provided to nurses caring for confirmed COVID‐19 patients.
7. IMPLICATIONS FOR NURSING MANAGEMENT
Management of nursing care for COVID‐19 should be implemented with a broad perspective that considers not only care for confirmed cases but also for suspected cases, which is more burdensome in some regards. Extensive support systems are required for nurses caring for suspected cases, even if they have never cared for confirmed cases.
CONFLICT OF INTEREST
All authors have no conflict of interests.
ETHICAL APPROVAL
This study was approved by the Institutional Review Boards of the Kanagawa Prefectural Hospital Organization (2020‐epidemiology‐1) Kanagawa Psychiatric Center (202007) and the Kanagawa Cancer Center (2020‐epidemiology‐151).
AUTHOR CONTRIBUTIONS
HK was responsible for conceptualizing the study, conducting the survey and writing the main part of the manuscript. KW was responsible for statistical analysis, interpretation of the data and writing the section on statistics and results, preparing all figures and tables. SN and HT critically reviewed the results of the analyses and the manuscript and provided expert advice. HN was involved in all stages of the study and provided overall supervision. All authors read and approved the final manuscript.
Supporting information
Table S1. Factor Loadings of Factor Analysis of Tokyo Metropolitan Distress Scale for Pandemic (TMDP)
Table S2. Factor Loadings of Factor Analysis of Japanese Burnout Scale (JBS)
Table S3. Factor Loadings of Factor Analysis of Brief Scale for Coping Profile (BSCP)
Table S4. Single Regression Analysis
Table S5. Multiple Regression Analysis (Department's Acceptance of COVID‐19 Patients)
Table S6. Multiple Regression Analysis (Experience in Caring for COVID‐19 Patients)
Table S7. Variance Inflation Factor
Figure S1. Parallel Analysis Scree Plots of Tokyo Metropolitan Distress Scale for Pandemic (TMDP)
Figure S2. Parallel Analysis Scree Plots of Japanese Burnout Scale (JBS)
Figure S3. Parallel Analysis Scree Plots of Brief Scale for Coping Profile (BSCP)
ACKNOWLEDGMENT
The authors would like to thank Editage (https://www.editage.jp) for English‐language editing.
Kishi, H. , Watanabe, K. , Nakamura, S. , Taguchi, H. , & Narimatsu, H. (2022). Impact of nurses' roles and burden on burnout during the COVID‐19 pandemic: Multicentre cross‐sectional survey. Journal of Nursing Management, 1–9. 10.1111/jonm.13648
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- Adachi, H. , Inoue, M. , & Inaba, R. (2005). Stress management among hospital nurses application to nurses of stress & stress‐coping scale (SSCQ) (in Japanese). Sangyō Eiseigaku Zasshi, 47, 1–10. 10.1539/sangyoeisei.47.1 [DOI] [PubMed] [Google Scholar]
- Carleton, R. N. (2016). Into the unknown: A review and synthesis of contemporary models involving uncertainty. Journal of Anxiety Disorders, 39, 30–43. 10.1016/j.janxdis.2016.02.007 [DOI] [PubMed] [Google Scholar]
- Chemali, Z. , Ezzeddine, F. L. , Gelaye, B. , Dossett, M. L. , Salameh, J. , Bizri, M. , Dubale, B. , & Fricchione, G. (2019). Burnout among healthcare providers in the complex environment of the Middle East: A systematic review. BMC Public Health, 19(1), 1337. 10.1186/s12889-019-7713-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furubayashi, C. (2021). Practice as a nurse manager in accepting patients with new coronavirus infections and future issues: Approaches at Nagoya City eastern medical center (in Japanese). Nursing Manegement, 31(1), 58–64. [Google Scholar]
- Galanis, P. , Vraka, I. , Fragkou, D. , Bilali, A. , & Kaitelidou, D. (2021). Nurses' burnout and associated risk factors during the COVID‐19 pandemic: A systematic review and meta‐analysis. Journal of Advanced Nursing, 77(8), 3286–3302. 10.1111/jan.14839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grupe, D. W. , & Nitschke, J. B. (2013). Uncertainty and anticipation in anxiety: An integrated neurobiological and psychological perspective. Nature Reviews Neuroscience, 14(7), 488–501. 10.1038/nrn3524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammond, N. E. , Crowe, L. , Abbenbroek, B. , Elliott, R. , Tian, D. H. , Donaldson, L. H. , Fitzgerald, E. , Flower, O. , Grattan, S. , Harris, R. , Sayers, L. , & Delaney, A. (2021). Impact of the coronavirus disease 2019 pandemic on critical care healthcare workers' depression, anxiety, and stress levels. Australian Critical Care, 34(2), 146–154. 10.1016/j.aucc.2020.12.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendy, A. , Abozeid, A. , Sallam, G. , Abboud Abdel Fattah, H. , & Ahmed Abdelkader Reshia, F. (2020). Predictive factors affecting stress among nurses providing care at COVID‐19 isolation hospitals at Egypt. Nursing Open, 8(1), 498–505. 10.1002/nop2.652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoseinabadi, T. S. , Kakhki, S. , Teimori, G. , & Nayyeri, S. (2020). Burnout and its influencing factors between frontline nurses and nurses from other wards during the outbreak of coronavirus disease‐COVID‐19‐in Iran. Investigación Y Educación en Enfermería, 38(2). 10.17533/udea.iee.v38n2e03 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ihaka, R. , & Gentleman, R. (1996). R: A language for data analysis and graphics. Journal of Computational and Graphical Statistics, 5(3), 299–314. 10.1080/10618600.1996.10474713 [DOI] [Google Scholar]
- Ingram, C. , Downey, V. , Roe, M. , Chen, Y. , Archibald, M. , Kallas, K. A. , Kumar, J. , Naughton, P. , Uteh, C. O. , Rojas‐Chaves, A. , Shrestha, S. , Syed, S. , Cléirigh Büttner, F. , Buggy, C. , & Perrotta, C. (2021). COVID‐19 prevention and control measures in workplace settings: A rapid review and meta‐analysis. International Journal of Environmental Research and Public Health, 18(15). 10.3390/ijerph18157847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Japanese Nursing Association . (2020). Survey on nursing staffs deal with novel coronavirus infection (in Japanese). Retrieved from https://www.nurse.or.jp/nursing/practice/covid_19/research/index.html?utm_source=whats_new&utm_campaign=20200908
- Kageyama, T. , Kobayashi, T. , Kawashima, M. , & Kanamaru, Y. (2004). Development of the brief scales for coping profile (BSCP) for workers: Basic information about its reliability and validity. Sangyō Eiseigaku Zasshi, 46(4), 103–114. 10.1539/sangyoeisei.46.103 [DOI] [PubMed] [Google Scholar]
- Ke, Q. , Chan, S. W. , Kong, Y. , Fu, J. , Li, W. , Shen, Q. , & Zhu, J. (2021). Frontline nurses' willingness to work during the COVID‐19 pandemic: A mixed‐methods study. Journal of Advanced Nursing, 77(9), 3880–3893. 10.1111/jan.14989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim, S. C. , Quiban, C. , Sloan, C. , & Montejano, A. (2021). Predictors of poor mental health among nurses during COVID‐19 pandemic. Nursing Open, 8(2), 900–907. 10.1002/nop2.697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kowalczuk, K. , Krajewska‐Kułak, E. , & Sobolewski, M. (2019). Factors determining work arduousness levels among nurses: Using the example of surgical, medical treatment, and emergency wards. BioMed Research International, 2019, 6303474. 10.1155/2019/6303474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke, K. , Spitzer, R. L. , & Williams, J. B. (2001). The PHQ‐9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613. 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kubo, M. (2007). The factorial and construct validity of the Japanese burnout scale. The Journal of Science of Labour, 83, 39–53. [Google Scholar]
- Kubo, M. (2014). The factorial and construct validity of the Japanese burnout scale among service workers. Shinrigaku Kenkyu: The Japanese Journal of Psychology, 85(4), 364–372. 10.4992/jjpsy.85.13214 [DOI] [PubMed] [Google Scholar]
- Kubo, M. , & Tao, M. (1994). Burnout among nurses: The relationship between stresses and burnout. Japanese Journal of Experimental Social Psychology, 34(1), 33–43. 10.2130/jjesp.34.33 [DOI] [Google Scholar]
- Kuo, F. L. , Yang, P. H. , Hsu, H. T. , Su, C. Y. , Chen, C. H. , Yeh, I. J. , Wu, Y. H. , & Chen, L. C. (2020). Survey on perceived work stress and its influencing factors among hospital staff during the COVID‐19 pandemic in Taiwan. The Kaohsiung Journal of Medical Sciences, 36(11), 944–952. 10.1002/kjm2.12294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Labrague, L. J. , & de Los Santos, J. A. A. (2021). Fear of COVID‐19, psychological distress, work satisfaction and turnover intention among frontline nurses. Journal of Nursing Management, 29(3), 395–403. 10.1111/jonm.13168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liao, R. W. , Yeh, M. L. , Lin, K. C. , & Wang, K. Y. (2020). A hierarchical model of occupational burnout in nurses associated with job‐induced stress, self‐concept, and work environment. Journal of Nursing Research, 28(2), e79. 10.1097/jnr.0000000000000348 [DOI] [PubMed] [Google Scholar]
- Matsumoto, Y. , Fujino, J. , Shiwaku, H. , Miyajima, M. , Doi, S. , Hirai, N. , Jitoku, D. , Takagi, S. , Tamura, T. , Maruo, T. , Shidei, Y. , Kobayashi, N. , Ichihashi, M. , Noguchi, S. , Oohashi, K. , Takeuchi, T. , Sugihara, G. , Okada, T. , Fujiwara, T. , & Takahashi, H. (2021). Factors affecting mental illness and social stress in hospital workers treating COVID‐19: Paradoxical distress during pandemic era. Journal of Psychiatric Research, 137, 298–302. 10.1016/j.jpsychires.2021.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsuo, T. , Kobayashi, D. , Taki, F. , Sakamoto, F. , Uehara, Y. , Mori, N. , & Fukui, T. (2020). Prevalence of health care worker burnout during the coronavirus disease 2019 (COVID‐19) pandemic in Japan. JAMA Network Open, 3(8), e2017271. 10.1001/jamanetworkopen.2020.17271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministry of Health, Labour and Welfare, Japan . (2008). Self‐diagnosis check list for assessment of workers' accumulated fatigue; check list for AWAF (in Japanese). Retrieved from https://www.mhlw.go.jp/topics/2004/06/tp0630-1.html
- Mori, T. , & Kageyama, T. (1995). A cross‐sectional survey on mental health and working environment of hospital nurses. Journal of Occupational Health, 37(2), 135–142. 10.1539/sangyoeisei.37.2_135 [DOI] [PubMed] [Google Scholar]
- Ogiwara, N. , Mito, Y. , & Kim, S. (2020). Concept analysis of “holistic care” in nursing in Japan. Japanese Journal of Nursing Art and Science, 19, 83–91. [Google Scholar]
- Sasaki, T. , Iwasaki, K. , Mori, I. , Hisanaga, N. , & Shibata, E. (2005). Examination of the reliability and validity of the “Self‐Diagnosis Check List for Assessment of Workers Accumulated Fatigue”. Sangyō Eiseigaku Zasshi, 47(Special), 759. 10.1539/sangyoeisei.KJ00003804390 [DOI] [Google Scholar]
- Sasaki, T. , Iwasaki, K. , Mori, I. , Hisanaga, N. , & Shibata, E. (2007). Overtime, job stressors, sleep/rest, and fatigue of Japanese workers in a company. Industrial Health, 45(2), 237–246. 10.2486/indhealth.45.237 [DOI] [PubMed] [Google Scholar]
- Setou, N. , Takebayashi, Y. , & Maeda, M. (2020). Mental health support for healthcare workers during a novel coronavirus infection (COVID‐19) epidemic: A literature review on psychosocial support for staff dealing with infected patients (in Japanese). Job Stress Research, 27(3), 351–361. [Google Scholar]
- Shiwaku, H. , Doi, S. , Miyajima, M. , Matsumoto, Y. , Fujino, J. , Hirai, N. , Jitoku, D. , Takagi, S. , Tamura, T. , Maruo, T. , Shidei, Y. , Kobayashi, N. , Ichihashi, M. , Noguchi, S. , Oohashi, K. , Takeuchi, T. , Sugihara, G. , Okada, T. , Fujiwara, T. , & Takahashi, H. (2021). Novel brief screening scale, Tokyo metropolitan distress scale for pandemic (TMDP), for assessing mental and social stress of medical personnel in COVID‐19 pandemic. Psychiatry and Clinical Neurosciences, 75(1), 24–25. 10.1111/pcn.13168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer, R. L. , Kroenke, K. , Williams, J. B. , & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD‐7. Archives of Internal Medicine, 166(10), 1092–1097. 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- Xue, X. L. , Wang, T. F. , & Yu, C. G. (2008). Estimation on the reliability and validity of the fatigue self‐assessment scale. Zhongguo Zhong Xi Yi Jie he Za Zhi, 28(6), 550–554. [PubMed] [Google Scholar]
- Zhan, Y. , Ma, S. , Jian, X. , Cao, Y. , & Zhan, X. (2020). The current situation and influencing factors of job stress among frontline nurses assisting in Wuhan in fighting COVID‐19. Frontiers in Public Health, 8, 579866. 10.3389/fpubh.2020.579866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, Y. , Wang, C. , Pan, W. , Zheng, J. , Gao, J. , Huang, X. , Cai, S. , Zhai, Y. , Latour, J. M. , & Zhu, C. (2020). Stress, burnout, and coping strategies of frontline nurses during the COVID‐19 epidemic in Wuhan and Shanghai, China. Frontiers in Psychiatry, 11, 565520. 10.3389/fpsyt.2020.565520 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Factor Loadings of Factor Analysis of Tokyo Metropolitan Distress Scale for Pandemic (TMDP)
Table S2. Factor Loadings of Factor Analysis of Japanese Burnout Scale (JBS)
Table S3. Factor Loadings of Factor Analysis of Brief Scale for Coping Profile (BSCP)
Table S4. Single Regression Analysis
Table S5. Multiple Regression Analysis (Department's Acceptance of COVID‐19 Patients)
Table S6. Multiple Regression Analysis (Experience in Caring for COVID‐19 Patients)
Table S7. Variance Inflation Factor
Figure S1. Parallel Analysis Scree Plots of Tokyo Metropolitan Distress Scale for Pandemic (TMDP)
Figure S2. Parallel Analysis Scree Plots of Japanese Burnout Scale (JBS)
Figure S3. Parallel Analysis Scree Plots of Brief Scale for Coping Profile (BSCP)
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


