Summary
The coronavirus disease 2019 (COVID‐19) pandemic is a global health crisis with the potential to elicit and worsen psychiatric symptoms, particularly post‐traumatic stress disorder (PTSD) symptoms. Identifying modifiable protective factors is critical for preventing and treating PTSD symptoms both during and following the COVID‐19 pandemic. The present study examined associations of self‐reported sleep quality and anticipatory threat appraisals of the pandemic with PTSD symptoms 6 months later in a sample enriched for pre‐pandemic trauma exposure and PTSD. The sample included 590 adults (mean age 38.2 years) who completed a baseline survey in August/September 2020 and follow‐up survey in March/April 2021. The sample was recruited from a pool of participants interested in a prior study about traumatic stress. Participants self‐reported sleep quality and pandemic‐related anticipatory threat appraisals at baseline. PTSD symptoms were assessed at baseline and follow‐up. Baseline sleep quality was associated with PTSD symptoms at follow‐up controlling for baseline PTSD symptoms (B = −2.49, p = 0.001). Perceived anticipatory threat of the pandemic moderated this association such that worse sleep quality was related to more severe PTSD symptoms at follow‐up for participants with higher (B = −4.07, p < 0.001) but not lower (B = −0.43, p = 0.679) anticipatory threat about the COVID‐19 pandemic. These findings suggest that poor sleep quality may enhance vulnerability to later PTSD symptoms during the pandemic, particularly among those individuals who perceived the pandemic as threatening for their future. Treatments that address sleep problems may be beneficial for reducing trauma‐related symptoms during and following the global health crisis.
Keywords: coronavirus disease 2019 (COVID‐19), Post‐traumatic stress disorder (PTSD), sleep, threat
1. INTRODUCTION
Post‐traumatic stress disorder (PTSD) is a debilitating condition with long‐term consequences. The ongoing coronavirus disease 2019 (COVID‐19) global pandemic has claimed over 4 million lives worldwide to date, heightening concern for post‐traumatic sequelae; recent data suggests PTSD has been especially prevalent among women and those experiencing economic instability during the pandemic (Di Crosta et al., 2020). Identifying modifiable risk factors for PTSD will inform interventions to prevent or ameliorate PTSD symptoms in the context of both the ongoing COVID‐19 pandemic in particular and stressful circumstances in general.
Sleep quality is an important risk factor for PTSD. Short sleep duration has been associated with PTSD symptoms during the COVID‐19 pandemic in cross‐sectional studies (Tang et al., 2020) and longitudinal studies have identified sleep disturbance as a risk factor for PTSD prior to and immediately after traumatic events (Neylan et al., 2021). Poor sleep is a treatable condition even with short‐term interventions (Germain & Buysse, 2011), making sleep an ideal potential target for reducing or preventing PTSD symptoms during and following the pandemic.
Another potential pandemic‐related risk factor for worsening PTSD is perceived threat, which underlies and maintains many PTSD symptoms (Piotrkowski & Brannen, 2002). Anticipatory threat appraisals may be particularly potent in determining the psychological and biological sequelae of stressors (O’Donovan et al., 2012). Given that poor sleep influences threat perception (Zenses et al., 2020) and fear processing (Colvonen et al., 2019), poor sleep quality may be especially salient in the context of high threat. To our knowledge, no study has explored the combined impact of sleep quality and perceived anticipatory threat on PTSD symptoms during the COVID‐19 pandemic.
We conducted a survey‐based study in a United States community sample enriched for trauma exposure and PTSD symptoms (n = 590). We assessed self‐reported sleep quality and anticipatory threat appraisals of the pandemic in August/September 2020 and PTSD symptoms in March/April 2021. The present study aimed to: (1) examine if self‐reported sleep quality early in the pandemic was associated with PTSD symptoms several months later; and (2) examine if the relationship between sleep quality and PTSD symptoms varied with levels of anticipatory threat appraisals. We hypothesised that individuals with poor sleep quality in the initial months of the pandemic would have higher PTSD symptoms several months later, with particularly strong effects among those who had higher pandemic‐related anticipatory threat appraisals.
2. METHODS
2.1. Sample
Community‐dwelling adults residing in the United States were recruited from a prior PTSD‐focussed study conducted in 2017–2018 (Niles et al., 2020). Participants were recruited from all 50 States via Craigslist advertisements and Reddit forums related to trauma or post‐traumatic stress. Craigslist and Reddit are online communities that allow for recruitment of a broad sample of online users. Participants (n = 3631) who expressed interest in the 2017–2018 study were contacted about participating in a follow‐up study regarding psychological experiences during the COVID‐19 pandemic (Nishimi et al., 2022, under review). Of the 3631 individuals, 896 eligible individuals provided electronic consent and completed an online Qualtrics survey in August/September 2020. Between March 9–April 14, 2021, 892 (four individuals opted out) of these individuals were invited to participate in a follow‐up online Qualtrics survey regarding the COVID‐19 pandemic. Of those invited, 609 (68.3%) individuals completed at least part of the follow‐up survey. Individuals received a $5 Amazon e‐gift card for each completed survey. Current analyses included data from August/September 2020 (baseline) and March/April 2021 (follow‐up). There were 590 individuals with complete data on relevant measures. This study was approved by the Institutional Review Board at the University of California, San Francisco, CA, USA.
2.2. Measures
2.2.1. PTSD symptoms
PTSD symptoms were assessed at baseline and follow‐up. Past 30‐day PTSD symptom severity in relation to one’s worst trauma was assessed with the 20‐item PTSD Checklist‐5 (PCL‐5; Weathers et al., 2013).
2.2.2. Sleep quality
Past 30‐day sleep quality was assessed at baseline (5‐point scale from “very poor” to “very good”).
2.2.3. Pandemic‐related anticipatory threat appraisals
At baseline, participants rated threat of the COVID‐19 pandemic to multiple domains of life including work and finances, education and training, social relationships inside and outside the home, and physical and emotional health (5‐point scale from “no threat” to “extreme threat”) in the next 12 months, as per Niles and O’Donovan (2018). A mean score of all threat items was created for analyses.
2.3. Data analysis
Linear regression was used to test the aims of this study. All analyses controlled for baseline PTSD symptoms. First, we examined baseline sleep quality as a predictor of PTSD symptoms at follow‐up. Second, we examined the main effect of baseline sleep quality, the main effect of baseline perceived future threat of the COVID‐19 pandemic, and the interaction between baseline sleep quality and perceived future threat of the COVID‐19 pandemic on PTSD symptoms at follow‐up. Significant interactions were followed‐up with simple slopes analyses. The simple slopes were derived from the interaction equation fit and examined the effect of the independent variable at one standard deviation (SD) above and below the mean. An alpha level of p < 0.05 was used for all analyses. All analyses were conducted in R, version 4.0.3.
3. RESULTS
Among the participants (n = 590), three‐quarters identified as women (75.9%), 21.4% identified as men, and 2.7% identified as a gender other than man or woman. The mean (SD) age of the sample was 38.2 (11.0) years. Race and ethnicity were largely representative of the United States general population with 12.9% identifying as Black, 10.7% as Asian, 10.2% as Latinx, 62.7% as non‐Hispanic White, and 3.6% as other race or more than one race. Two‐thirds (66.6%) of the sample had a 4‐year college degree or more, and over half (57.3%) of the sample reported full‐time employment. Additional demographic and clinical characteristics are reported in Table 1.
TABLE 1.
Sociodemographic and clinical characteristics of the sample (N = 590)
| Characteristic | Value |
|---|---|
| Socio‐demographic factors | |
| Age, years, mean (SD) | 38.2 (11.0) |
| Gender, n (%) | |
| Man | 126 (21.4) |
| Woman | 448 (75.9) |
| Non‐binary, transgender, other | 16 (2.7) |
| Race/Ethnicity, n (%) | |
| Non‐Hispanic White | 370 (62.7) |
| Black | 76 (12.9) |
| Asian | 63 (10.7) |
| Latinx | 60 (10.2) |
| Other or more than one race | 21 (3.6) |
| Educational attainment, n (%) | |
| High school or less | 36 (6.1) |
| Some College/2‐years College Degree | 160 (27.1) |
| 4‐years College Degree or Graduate School | 393 (66.6) |
| Employment status, n (%) | |
| Employed (full‐time) | 338 (57.3) |
| Employed (part‐time) | 91 (15.4) |
| Unemployed | 109 (18.5) |
| Student | 26 (4.4) |
| Retired | 15 (2.5) |
| Furlough | 10 (1.7) |
| Annual household income, n (%) | |
| ≤$50,000/year | 208 (35.3) |
| $50,001–$100,000/year | 257 (43.6) |
| $100,001–$150,000/year | 81 (13.7) |
| >$150,000/year | 43 (7.3) |
| Clinical factors, n (%) | |
| PTSD symptoms at baseline, mean score (SD) | 22.1 (19.7) |
| PTSD symptoms at follow‐up, mean score (SD) | 23.4 (20.5) |
| Sleep quality at baseline, mean score (SD) | 2.9 (1.0) |
| Perceived anticipatory threat of pandemic scale at baseline, mean score (SD) | 1.7 (0.9) |
PTSD, post‐traumatic stress disorder; SD, standard deviation.
A comparison of participants included in the analytical sample with those who were lost to follow‐up indicated that the samples had similar demographic characteristics. Participants with complete datasets were slightly older (mean [SD] age, 38.2 [11.0] versus 34.7 [11.0] years), more educated (high school or less: 6.1% versus 17.6%, some college/2‐years college degree: 27.1% versus 27.1%, 4‐years college degree or graduate school: 66.6% versus 55.2%), and had higher annual income (≤$50,000/year: 35.3% versus 53.6%, $50,001–$100,000/year: 43.6% versus 31.4%, $100,001–$150,000/year: 13.7% versus 9.2%, >$150,000/year: 7.3% versus 5.9%).
The severity of PTSD symptoms was similar at baseline (mean [SD] 22.1 [19.7] points) and follow‐up (mean [SD] 23.4 [= 20.5] points), t(551) = 0.188, p = 0.851, but change over time was highly variable ranging from −57 to +80 points (mean [SD] change 0.34 [17.16] points). On average, participants rated their sleep quality as “fair” at baseline (mean [SD] 2.9 [1.0] points). Overall, participants reported mild to moderate anticipatory threat appraisals of the COVID‐19 pandemic at baseline (mean [SD] 1.7 [0.9] points). Compared with participants excluded from the analytical sample, participants included in the analysis had similar anticipatory threat appraisals, less severe PTSD symptoms (mean [SD]: 22.1 [19.7] versus 30.3 [19.8] points), and better sleep quality (mean [SD]: 2.9 [1.0] versus 2.6 [1.0] points).
Worse baseline sleep quality was associated with more severe PTSD symptoms at follow‐up, adjusting for baseline PTSD symptoms, B = −2.49, t(549) = −3.29, p = 0.001. This finding indicates that for each unit decrease in sleep quality, PTSD symptoms as measured by the PCL‐5 increased by ~2.5 points.
The interaction between baseline sleep quality and perceived future threat of the COVID‐19 pandemic was significantly related to PTSD symptoms at follow‐up, controlling for baseline PTSD symptoms, F(1, 546) = 7.23, p = 0.007. Simple slopes (Figure 1) indicated that worse sleep quality was associated with more severe PTSD symptoms at follow‐up for participants with higher anticipatory threat related to the COVID‐19 pandemic, B = −4.07, t(549) = −4.11, p < 0.001, but not among those with lower COVID‐19 pandemic anticipatory threat, B = −0.43, t(549) = −0.41, p = 0.679. In other words, during the pandemic, worse sleep quality was associated with increasing PTSD severity for those with high but not low anticipatory threat appraisals of the pandemic.
FIGURE 1.
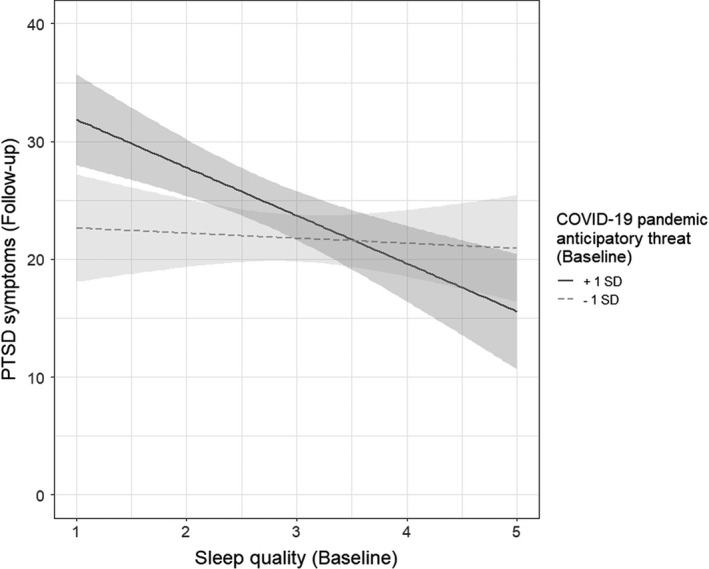
Simple slopes of the interaction between baseline sleep quality and baseline perceived anticipatory threat of the coronavirus disease 2019 (COVID‐19) pandemic with post‐traumatic stress disorder (PTSD) symptoms at follow‐up. The grey shading denotes the standard error of the simple slopes
4. DISCUSSION
To our knowledge, this is the first study to examine the longitudinal impact of sleep quality and anticipatory threat on PTSD symptoms during the global COVID‐19 pandemic. In our United States‐based community sample enriched for trauma exposure and PTSD symptoms, poor sleep quality at baseline in the early months of the pandemic predicted more severe PTSD symptoms at follow‐up several months later. Additionally, we observed the relationship between poor sleep and PTSD depended on perceived pandemic‐related threat, such that poor sleep quality was associated with more severe PTSD symptoms at follow‐up only in those who perceived the pandemic as especially threatening. Thus, poor sleep quality was associated with increased vulnerability to increasing PTSD symptoms over time in the context of high anticipatory threat appraisals.
Consistent with our hypotheses, poor sleep quality at baseline predicted more severe PTSD symptoms several months later, even controlling for baseline PTSD symptoms. This finding extends previous literature on the COVID‐19 pandemic linking short sleep duration with more severe PTSD when examined cross‐sectionally (Tang et al., 2020). Additionally, our results are consistent with other longitudinal studies identifying disrupted sleep as a risk factor for worsening PTSD symptoms (Neylan et al., 2021). Sleep disruption leads to impairments in fear processing (Colvonen et al., 2019), which in turn underlies many symptoms of PTSD. This study adds to the growing body of research suggesting that targeting sleep problems with focussed interventions may improve PTSD symptoms.
Results also supported our hypothesis that poor sleep quality would be most closely associated with worsening of PTSD in those who were experiencing greater anticipatory threat. This finding is in line with evidence that fear reinstatement is associated with more severe PTSD symptoms but only among individuals with poor sleep (Zuj et al., 2018). Additionally, poor baseline sleep quality has been shown to interfere with trauma‐focussed treatment among Veterans with PTSD and traumatic brain injury (Sullan et al., 2021). Taken together, these findings suggest that poor sleep may not be a stand‐alone risk factor but may act as a vulnerability factor to reduce capacity to cope with other stressors.
There are limitations of the present study that are worth noting. Results were based on survey data from two time‐points, and 302 participants did not provide follow‐up data (~34%), raising concern about the generalisability of the findings. Although those lost to follow‐up had worse PTSD severity and sleep quality at baseline, they had similar anticipatory threat appraisals. Additionally, we assessed sleep via a self‐reported item focussed on global sleep quality. Although there is support for the use of a single‐item measures of sleep quality (Snyder et al., 2018), future studies should include fuller assessments of sleep quality based on subjective and objective data, which will provide more information about which aspects of disrupted sleep are the most salient. Finally, this sample was recruited from an unknown population of Craigslist and Reddit users, which limits generalisability. The participants in this study were also more likely to be exposed to traumatic events than the general population. These findings may not generalise beyond individuals with a history of trauma exposure.
In summary, we found poor sleep quality was associated with worsening PTSD symptoms, but only among those individuals who perceived the pandemic to be especially threatening. Studies such as this one provide the opportunity to inform interventions to reduce or prevent PTSD, which is especially important given the large potential for post‐traumatic sequelae in the aftermath of the COVID‐19 pandemic.
CONFLICT OF INTEREST
None.
AUTHOR CONTRIBUTION
Conceptualization: LDS, EAD, KN, TCN, AOD; Methodology: LDS, EAD, KN, TCN, AOD; Writing – Original Draft: LDS, EAD; Writing – Reviewing and Editing: LDS, EAD, KN, TCN, AOD; Statistical analysis: EAD; Resources: TCN, AOD; Data curation: KN; Funding Acquisition: AOD.
Straus, L. D. , Dolsen, E. A. , Nishimi, K. , Neylan, T. C. , & O’Donovan, A. (2022). Worse sleep, worsening post‐traumatic stress disorder (PTSD): Poor sleep quality associated with increases in PTSD symptoms amongst those experiencing high threat of the COVID‐19 pandemic. Journal of Sleep Research, 00, e13568. 10.1111/jsr.13568
Laura D. Straus and Emily A. Dolsen contributed equally towards first authorship for this study
Funding information
This work was supported by the University of California, San Francisco (UCSF), Department of Psychiatry Rapid Award (Aoife O’Donovan), the National Institutes of Mental Health (Aoife O’Donovan; K01MH109871), the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development (Laura D. Straus; IK2CX002032), a Mental Illness Research and Education Clinical Center fellowship of the United States Veterans Health Administration at the San Francisco VA Healthcare System (Emily A. Dolsen), and a VA Data Science Fellowship at the San Francisco VA Healthcare System (Kristen Nishimi).
Contributor Information
Laura D. Straus, Email: laura.straus@ucsf.edu.
Emily A. Dolsen, Email: emily.dolsen@ucsf.edu.
DATA AVAILABILITY STATEMENT
Research data are not shared.
REFERENCES
- Colvonen, P. J. , Straus, L. D. , Acheson, D. , & Gehrman, P. (2019). A review of the relationship between emotional learning and memory, sleep, and PTSD. Current Psychiatry Reports, 21(1), 2. 10.1007/s11920-019-0987-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Crosta, A. , Palumbo, R. , Marchetti, D. , Ceccato, I. , La Malva, P. , Maiella, R. , … & Di Domenico, A. (2020). Individual differences, economic stability, and fear of contagion as risk factors for PTSD symptoms in the COVID‐19 emergency. Frontiers in Psychology, 11, 2329. 10.3389/fpsyg.2020.567367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Germain, A. , & Buysse, D. J. (2011). Brief behavioral treatment of insomnia. In: Perlis, M., Aloia, M., & Kuhn, B. (Eds.) Behavioral Treatments for Sleep Disorders (pp. 143–150). New York, NY: Academic Press. 10.1016/B978-0-12-381522-4.00015-8 [DOI] [Google Scholar]
- Neylan, T. C. , Kessler, R. C. , Ressler, K. J. , Clifford, G. , Beaudoin, F. L. , An, X. , … McLean, S. A. (2021). Prior sleep problems and adverse post‐traumatic neuropsychiatric sequelae of motor vehicle collision in the AURORA study. Sleep, 44(3), zsaa200. 10.1093/sleep/zsaa200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niles, A. N. , & O’Donovan, A. (2018). Personalizing affective stimuli using a recommender algorithm: An example with threatening words for trauma exposed populations. Cognitive Therapy and Research, 42(6), 747–757. 10.1007/s10608-018-9923-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niles, A. N. , Woolley, J. D. , Tripp, P. , Pesquita, A. , Vinogradov, S. , Neylan, T. C. , & O’Donovan, A. (2020). Randomized controlled trial testing mobile‐based attention‐bias modification for posttraumatic stress using personalized word stimuli. Clinical Psychological Science, 8(4), 756–772. 10.1177/2167702620902119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nishimi, K. , Borsari, B. , Marx, B. P. , Tripp, P. , Woodward, E. , Rosen, R. C. , … O’Donovan, A. (2022). Posttraumatic stress symptoms associated with protective and risky behaviors for COVID‐19. Health Psychology. in press. 10.1037/hea0001157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Donovan, A. , Tomiyama, A. J. , Lin, J. , Puterman, E. , Adler, N. E. , Kemeny, M. , … Epel, E. S. (2012). Stress appraisals and cellular aging: A key role for anticipatory threat in the relationship between psychological stress and telomere length. Brain, Behavior, and Immunity, 26(4), 573–579. 10.1016/j.bbi.2012.01.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piotrkowski, C. S. , & Brannen, S. J. (2002). Exposure, threat appraisal, and lost confidence as predictors of PTSD symptoms following September 11, 2001. American Journal of Orthopsychiatry, 72(4), 476–785. 10.1037/0002-9432.72.4.476 [DOI] [PubMed] [Google Scholar]
- Snyder, E. , Cai, B. , DeMuro, C. , Morrison, M. F. , & Ball, W. (2018). A new single‐item sleep quality scale: Results of psychometric evaluation in patients with chronic primary insomnia and depression. Journal of Clinical Sleep Medicine, 14(11), 1849–1857. 10.5664/jcsm.7478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullan, M. J. , Crocker, L. D. , Thomas, K. R. , Orff, H. J. , Davey, D. K. , Jurick, S. M. , … Jak, A. J. (2021). Baseline sleep quality moderates symptom improvement in veterans with comorbid PTSD and TBI receiving trauma‐focused treatment. Behaviour Research and Therapy, 143, 103892. [DOI] [PubMed] [Google Scholar]
- Tang, W. , Hu, T. , Hu, B. , Jin, C. , Wang, G. , Xie, C. , … Xu, J. (2020). Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID‐19 epidemic in a sample of home‐quarantined Chinese university students. Journal of Affective Disorders, 274, 1–7. 10.1016/j.jad.2020.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers, F. W. , Litz, B. T. , Keane, T. M. , Palmieri, P. A. , Marx, B. P. , & Schnurr, P. P. (2013). The ptsd checklist for dsm‐5 (pcl‐5). Scale available from the National Center for PTSD at Retrieved from www.ptsd.va.gov, 10. [Google Scholar]
- Zenses, A. K. , Lenaert, B. , Peigneux, P. , Beckers, T. , & Boddez, Y. (2020). Sleep deprivation increases threat beliefs in human fear conditioning. Journal of Sleep Research, 29(3), e12873. 10.1111/jsr.12873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuj, D. V. , Palmer, M. A. , Malhi, G. S. , Bryant, R. A. , & Felmingham, K. L. (2018). Greater sleep disturbance and longer sleep onset latency facilitate SCR‐specific fear reinstatement in PTSD. Behaviour Research and Therapy, 110, 1–10. 10.1016/j.brat.2018.08.005 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Research data are not shared.


