Abstract
Purpose
The objective of this study was to assess perceptions, health behaviors, and disruptions related to the COVID‐19 pandemic in a largely rural, Midwestern state, and to examine differences between rural and urban respondents.
Methods
A questionnaire was mailed August 2020 to a sample of 10,009 registered voters in Iowa ages 18‐100 years, with oversampling from 6 select rural counties. Previously validated and tested items assessed COVID‐19 precautions, health care disruptions, emotional reactions, health behavior changes, telehealth and experiences with the internet, and demographic characteristics.
Findings
There were 4,048 respondents (40% response rate); 65% were rural and 35% were urban residents. The average age of respondents was 58.3 years and 45% of respondents identified as female. Rural respondents reported less concern about COVID‐19 in their community (29% vs 40%, P<.001) and lower perceived importance of social distancing (51% vs 64%, P<.001). Urban respondents more often reported experiencing disruption to daily living, stronger negative emotional reactions, and displayed more pronounced behavior change compared to their rural counterparts. For example, urban respondents reported more pandemic‐related job losses (6% vs 4%, P = .05), disruptions to daily activities (48% vs 35%, P<.001), and use of telehealth services during the pandemic (24% vs 16%, P<.001).
Conclusions
The majority of respondents reported disruptions to normal activities, medical appointment cancellations, and emotional distress during the first 6 months of the pandemic. The impact of the pandemic on urban residents appeared to be greater than for rural respondents. Timing of pandemic spread and varying beliefs are potential explanations.
Keywords: behaviors, COVID‐19, experiences, rural, urban
INTRODUCTION
The COVID‐19 pandemic has altered how we engage in health behaviors, interact with others, and access health care. 1 COVID‐19 is a highly contagious illness caused by the SARS‐COV‐2 virus that has infected more than 79 million individuals and resulted in the death of more than 950,000 individuals in the United States as of March 4, 2022. 2 During peak COVID‐19 infections in the United States, businesses closed or implemented restrictions to reduce person‐to‐person spread of the virus. 3 These closures (eg, to gyms, clinics, and outpatient facilities) have prevented individuals from maintaining healthy behaviors and seeking health care; 3 , 4 , 5 , 6 , 7 combined with the impact of COVID‐19 on the mental health of Americans, 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 we suspected a resulting decrease in individuals engaging in healthy behaviors to prevent chronic illnesses, and a potential differential impact on those living in rural counties compared to urban ones.
It has been well demonstrated that rural and urban populations have differences in health‐related behaviors to begin with, making it difficult to anticipate the potential impacts of COVID‐19 on each group. 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 For example, adult residents of rural areas have higher average caloric intake, higher body mass index, and lower diet quality across all age groups, and also have greater odds for cigarette smoking. 16 , 17 , 18 , 19 , 20 , 21
Studies have also assessed differences in rural and urban populations regarding mental health and telehealth services prior to the COVID‐19 pandemic. Compared to urban residents, rural residents attend fewer mental health visits for similar conditions, rural nursing home residents are less likely to be diagnosed with mental health conditions, and rural individuals (particularly veterans) are less likely to utilize telehealth services. 27 , 28 , 29 , 30 An exception was observed among a Medicaid beneficiary sample, where rural respondents were more likely to use telehealth services. 31 Since mental health care and telehealth services have been crucial during the pandemic, recognizing these pre‐existing differences is helpful in understanding how the pandemic has impacted rural and urban populations.
Several surveys implemented on a national scale aimed to understand the impacts of the pandemic. 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 These surveys assessed a wide range of impacts, from mental and physical health to employment and childcare disruptions to changes in socioeconomic status. Of these, 8 surveys specifically assessed the impact of the pandemic on rural communities. 8 , 9 , 10 , 11 , 12 , 34 , 61 , 62 , 63 Three compared health behaviors between rural and urban respondents, and found that those in rural counties were less likely to engage in COVID‐19 prevention behaviors, such as wearing a mask, maintaining at least 6 feet distance in public, and avoiding dine‐in restaurants. 61 , 62 , 63 Others assessed the impact of the pandemic exclusively among rural populations of Latinx farmworkers, Black churchgoers, and high school students. 8 , 9 , 10 , 11 , 12 , 34 Despite existing efforts, there remains a gap in population‐based surveys comprehensively assessing differences between rural and urban populations during the early months of the COVID‐19 pandemic.
We aimed to assess the impact of the COVID‐19 pandemic and associated restrictions on the perceptions, behaviors, and health care experiences of a population‐based sample, and how these factors differed between rural and urban respondents. Given the increased importance of telehealth and online information seeking during the pandemic, we also assessed differences in the ability of rural and urban populations to engage in video conferencing with health providers, comfortability in using telehealth services, and ability to obtain health‐related information on the internet. We hypothesized that the pandemic may have been less disruptive for behavior and lifestyle changes in rural areas, but could have created more challenges related to technology‐based implications of the pandemic.
METHODS
Study population
In August 2020, we mailed a cross‐sectional questionnaire to a stratified random sample of 10,009 Iowans from the 2018 voter registration file. Individuals eligible for inclusion in survey participation were those ages 18‐100 who were registered to vote in Iowa in 2018, and could communicate in English and/or Spanish. During initial participant selection, cases that were undeliverable or were found to live outside of the state, country, or assigned strata were replaced with a random individual in the desired strata selected from the 2018 voter registration file.
Strata
Target recipients were sampled from 7 geographic areas: 557 people from each of 6 highly rural counties located throughout Iowa as indicated by Rural‐Urban Continuum Codes (RUCCs) 7 through 9 (Adair, Appanoose, Buena Vista, Mahaska, Wayne, and Winneshiek counties) and 6,667 from the rest of the state. Representatives from Critical Access Hospitals (hospitals designated were those at least 35 miles from other hospitals chosen with the goal of improving local health care services) located in these 6 highly rural counties had been involved in a previous qualitative study designed to elicit barriers and challenges to prioritizing cancer prevention and control in their communities. 64 Their representatives had expressed the need for more locally relevant data on cancer risk factors and access to health care.
Mailing procedures
Approval for this study was received from the University of Iowa Institutional Review Board. A postcard was mailed to all individuals on August 7, 2020 to inform them of the subsequent arrival of their survey packet, a method reported to increase survey response rates. 65 Packets containing a study information and consent form, questionnaire booklet, online survey link, postage‐paid business reply envelope, and $5 cash incentive were then mailed 1 week later. Invitees were given the option of completing the paper survey or using an online survey link included in the survey packet. In cases where an individual's address changed and was within the same stratum, updated addresses were gathered and packets were remailed. A follow‐up mailing was sent to nonrespondents on October 1, 2020. The majority of completed surveys (80%) were received between August 16 and September 7, 2020, and nearly all completed surveys (98%) were received by December 31, 2020. The last survey included was returned in April 2021.
Measures
The survey was created using a combination of previously validated and newly developed/pretested Likert‐type and multiple choice items. 66 , 67 , 68 Items captured COVID‐19 symptoms and testing experience, concern regarding the pandemic, social distancing behaviors, changes in health behaviors after COVID‐19 restrictions were implemented, access to telehealth services, and delays in or lack of health care. Additional items assessed the influence of the pandemic in the following domains: emotional and physical reactions, disruption to daily activities, financial hardship, perceived benefits, social support, ability to manage stress, and concerns about medical care. 69 RUCCs were used to categorize counties as either rural (codes 4‐9) or urban (codes 1‐3). 70
Items assessing COVID‐19 symptoms and testing experience asked respondents about testing experience, symptoms, hospitalizations, and recent close physical contact with individuals who have COVID‐19 and/or respiratory symptoms with yes/no/not sure response options. Concern about the pandemic was assessed as a 5‐scale Likert item from “not at all concerned” to “very concerned.” Questions about social distancing behaviors included items on staying home, not having others come into their home, staying 6 feet away from others in public, and wearing a face covering when indoors and/or outdoors with yes/no response options. An additional item assessed perceived importance of social distancing on a 4‐point Likert‐scale from “not important” to “very important.”
Experiences with the internet and telehealth were assessed using either yes/no/not sure or Likert‐scale items. Respondents were asked if they owned a device that would allow them to video conference with a health care provider (yes/no), and if yes, whether they would be comfortable using telehealth to video conference with a provider (yes/no). Experiences with telehealth were assessed by asking if respondents had participated in video conferencing (yes/no) and if yes, whether they felt comfortable doing so (yes/no). Items assessed overall confidence in getting information on medical topics and confidence in getting medical information specifically from the internet (both on 5‐point Likert scales from “completely confident” to “not confident at all”), experience going online to access the internet (yes/no), and frustration/concern getting needed information from the internet (both on 4‐point Likert scales from “strongly agree” to “strongly disagree”).
Health care appointment cancellations were assessed using multiple‐choice items. Respondents were asked if a medical appointment was cancelled or closed because of COVID‐19 (yes/no/not applicable), if they cancelled an appointment to avoid being around others (yes/no/not applicable), and if they were unable to receive prescription medications, nonprescription medications, treatment for substance use issues, and/or mental health care counseling (able to obtain/unable to obtain/did not need). Physical barriers, such as transportation, insurance, and cost, were assessed in reference to medical appointments and mental health care or counseling.
Health behaviors and changes in these behaviors were assessed in multiple ways. Items borrowed from the validated Behavioral Risk Factor Surveillance System questionnaire and the Health Information National Trends Survey asked respondents to indicate the frequency of physical activity (30 minutes of at least moderate intensity), fruit intake, vegetable intake, and alcohol consumption in the 30 days prior to survey completion. 66 , 67 They were also asked to indicate if they had used any smoking/tobacco products in 30 days prior to completion (yes/no), and if they did, which types were used (cigarettes, cigars, chewing tobacco, electronic cigarettes or other vaping products, other products, none of the above). Use of alternative therapies was asked as a yes/no question for the use of complementary, alternative, or unconventional therapies, such as vitamins, minerals, herbal supplements, or homeopathy in the 12 months prior to survey completion. For each of the behaviors listed above, respondents were also asked to indicate whether they have changed the amount of the behavior compared to before the COVID‐19 pandemic (more than before the pandemic, less than before the pandemic, same amount as before the pandemic, did not use the product during or before the pandemic).
Demographic information included age in years, sex assigned at birth (male or female, prefer not to answer), identified gender (male, female, transgender, nonbinary, prefer not to answer), weight (in pounds), height (in feet and inches), race (White, Black, American Indian or Alaska Native, Asian, Native Hawaiian/Pacific Islander, other), ethnicity (Mexican, Chicano/a, Puerto Rican, Cuban, other Hispanic/Latinx/Spanish origin, or not of Hispanic/Latinx/Spanish origin), household income (categorized into 9 levels), education level (less than 8th grade, 8th‐11th grade, high school diploma or GED, vocational or technical school, some college, college graduate, postgraduate), insurance coverage (employer‐provided, private coverage, Medicare, Medicaid, TRICARE/Veterans Affairs/Military, Alaska Native/Indian Health Service/Tribal Health Services, other), marital status (single/never married, married, not married but living with a romantic partner, separated, divorced, widowed), and employment status (employed for wages, self‐employed, out of work, homemaker, student, retired).
Returned surveys were logged, manually edited, scanned using TeleForm Scan Station, reviewed using TeleForm Verifier software, and exported to an MS SQL Server database. Research team members attempted to contact respondents who skipped entire pages of the survey. If the respondent provided a phone number in the survey, a research team member attempted to call the respondent, offering to collect responses via phone; otherwise, contact was attempted via mail.
Statistical analysis
All data were cleaned and analyzed using SAS 9.4 software (SAS Institute, Cary, NC). To account for oversampling in the 6 rural county strata, data were weighted based on the sampling rate and proportion of the state the county represented. Frequencies were generated for all questions by strata and for composite weighted estimates for the entire state. Chi‐square tests were run to assess respondent differences in the state's rural counties compared to urban counties.
RESULTS
Demographics
The survey yielded a 40% response rate with 4,048 responses (Figure 1). Our analytic dataset contained 2,347 respondents in rural counties (65.1%) and 1,258 respondents in urban counties (34.9%) after weighting for oversampling. Rural respondents were significantly older, and more likely to be white, married, straight/heterosexual, retired, and have lower average income and educational attainment compared to urban respondents (Table 1). Those in rural counties more frequently identified commuting to work (72.4% vs 64.0%, P = .001) as opposed to working from home (17.7% vs 38.6%, P<.001). Rural respondents less frequently identified being in excellent or very good health (48.6% vs 53.8%, P = .01) and less frequently reported having had a routine checkup in the past year compared to those in urban counties (10.5% vs 13.2%, P = .04).
FIGURE 1.
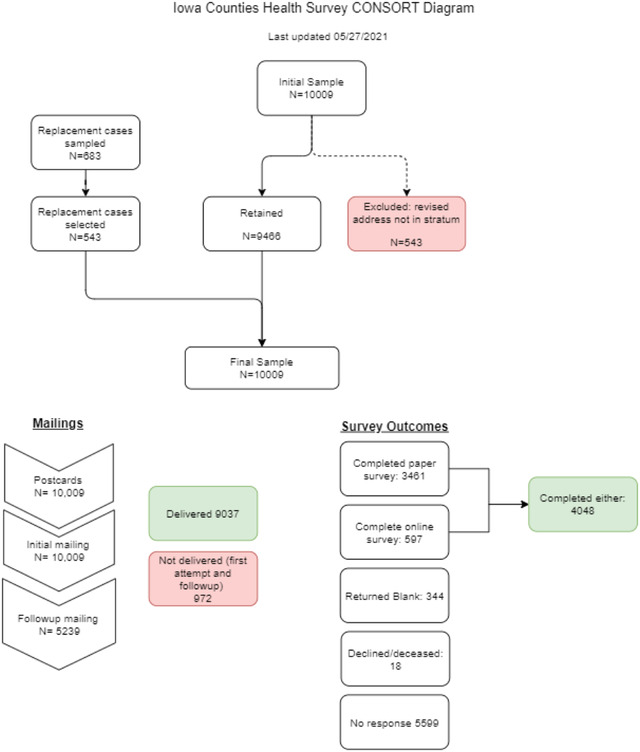
CONSORT flow diagram outlining participant sampling, mailing, and survey completion
TABLE 1.
Characteristics of survey respondents stratified by rural/urban county residence
| Respondent location | |||
|---|---|---|---|
| Characteristic | Rural (n = 2,347) | Urban (n = 1,278) | P |
| Age | .002 | ||
| <50 | 22.7% | 28.6% | |
| 50‐64 | 28.2% | 28.2% | |
| 65‐74 | 26.1% | 24.8% | |
| 75+ | 23.0% | 18.4% | |
| White race | 99.1% | 96.6% | <.001 |
| Hispanic ethnicity | 1.2% | 1.9% | .17 |
| Identified gender | .43 | ||
| Female | 44.9% | 42.0% | |
| Male | 55.1% | 57.7% | |
| Transgender or none of the above | 0.0% | 0.3% | |
| Marital status | .006 | ||
| Single, not married | 8.1% | 10.7% | |
| Married/living with a romantic partner | 72.2% | 69.0% | |
| Separated, divorced, widowed | 19.7% | 20.4% | |
| Sexual orientation | <.001 | ||
| Straight/heterosexual | 96.3% | 94.4% | |
| Gay/lesbian | 0.4% | 1.8% | |
| Bisexual | 3.0% | 1.5% | |
| Male height in inches, mean (SD) | 70.3 (0.1) | 70.5 (0.1) | |
| Female height in inches, mean (SD) | 64.8 (0.1) | 64.6 (0.1) | |
| Male weight in pounds, mean (SD) | 208.5 (2.0) | 200.9 (1.9) | |
| Female weight in pounds, mean (SD) | 173.8 (1.8) | 168.8 (1.6) | |
| Household income | <.001 | ||
| <$50,000 | 40.4% | 28.8% | |
| $50,000‐$99,999 | 38.3% | 38.2% | |
| $100,000+ | 21.3% | 33.0% | |
| Education | <.001 | ||
| High school/GED or less | 34.2% | 23.8% | |
| Some college or technical/vocational school | 32.0% | 29.2% | |
| College degree or more | 33.6% | 47.0% | |
| Employment status | <.001 | ||
| Employed for wages | 40.2% | 43.9% | |
| Self‐employed | 11.3% | 6.9% | |
| Out of work | 1.5% | 3.2% | |
| Homemaker | 3.3% | 3.3% | |
| Student | 0.9% | 1.3% | |
| Retired | 42.8% | 41.3% | |
| Commuted to work | 72.4% | 64.0% | <.001 |
| Worked from home | 17.7% | 38.6% | <.001 |
| Health insured | 94.6% | 94.9% | .92 |
| Self‐reported excellent/very good health | 48.6% | 53.8% | .01 |
| Had a routine check‐up in the past year | 10.5% | 13.2% | .04 |
Experiences with the internet and telehealth
A significantly lower proportion of rural respondents reported owning a device that would allow them to video conference with a health care provider (73.4% vs 83.3%, P<.001) (Table 2). Among those who reported owning a device, comfort levels for video conferencing with their health provider were generally high and there was no difference between urban and rural respondents in anticipated level of comfort with telehealth. A significantly lower proportion of the rural population reported that they had engaged in a video conference with their health care provider (16.0% vs 24.4%, P<.001). Among those who had engaged in a video conference, comfort was generally high and there was no difference in comfort level between urban and rural respondents. Although internet use in both groups was relatively high, a smaller proportion of rural respondents reported using the internet compared to urban respondents (75.1% vs 85.3%, P<.001). Similarly, a smaller proportion of rural respondents indicated that they felt confident in using information from the internet to make health decisions (30.5% vs 35.1% for strongly agree and agree responses, P<.001) and were able to seek information to address concerns related to the pandemic (58.3% vs 62.5%, P = .02).
TABLE 2.
Experiences with the internet and telehealth
| Respondent location | |||
|---|---|---|---|
| Characteristic | Rural (n = 2,347) | Urban (n = 1,278) | P |
| Owns a device that would allow them to video conference with their health care provider | 73.4% | 83.3% | <.001 |
| Would feel comfortable communicating with their health care provider in a video conference format through a device | 74.8% | 80.0% | .12 |
| Had engaged in a video conference visit with any of their health care providers | 16.0% | 24.4% | <.001 |
| Felt comfortable communicating with their health care provider in a video conference visit | 89.3% | 93.9% | .07 |
| Goes online to access the internet or world wide web, or to send and receive email | 75.1% | 85.3% | <.001 |
| How much do you agree or disagree with this statement? “I feel confident in using information from the Internet to make health decisions” | <.001 | ||
| Strongly agree | 5.0% | 6.7% | |
| Agree | 25.5% | 28.4% | |
| Undecided | 43.1% | 37.4% | |
| Disagree | 17.2% | 18.6% | |
| Strongly disagree | 9.2% | 8.8% | |
| Feels they are able to seek information and plan accordingly to address concerns over the pandemic | 58.3% | 62.5% | .02 |
Effects and concerns during the pandemic
Reported impacts of COVID‐19 were greater in urban counties than in rural ones (Table 3). Urban respondents more frequently reported losing their job or primary source of income compared to rural respondents (6.2% vs 4.0%, P = .05), though rural respondents more frequently reported finding it difficult or very difficult to get by on their household's income at the time of survey response (12.7% vs 10.0%, P = .009). Urban respondents more frequently identified having conflict with household members (19.3% vs 14.7%, P = .004), having difficulty doing their job well due to needing to care for others in their home (6.9% vs 3.4%, P<.001), having to take over teaching or instructing a child (11.3% vs 7.1%, P = .02), having difficulty taking care of children in their home (3.3% vs 1.9%, P = .01), and balancing their child's needs with other responsibilities (10.2% vs 7.4%, P = .005). Urban respondents also more frequently identified experiencing disruptions in day‐to‐day activities (72.1% vs 61.4%, P<.001) and an inability to follow daily routines (34.5% vs 47.4%, P<.001). However, more urban respondents reported receiving tangible support from loved ones when needed (24.6% vs 19.9%, P = .005).
TABLE 3.
Effects and concerns during COVID‐19 pandemic
| Respondent location | |||
|---|---|---|---|
| Characteristic | Rural (n = 2,347) | Urban (n = 1,278) | P |
| Lost job or primary source of income due to COVID‐19 | 4.0% | 6.2% | .05 |
| Lost primary source of insurance due to COVID‐19 | 0.5% | 1.0% | .08 |
| Found it difficult or very difficult to get by on household income | 12.7% | 10.0% | .009 |
| Had difficulty purchasing or obtaining basic necessities | 19.4% | 20.0% | .37 |
| Worked in close contact with people who might be infected with COVID‐19 | 16.1% | 18.8% | .32 |
| Since the outbreak of the COVID‐19 pandemic: | |||
| Experienced conflict with household members | 14.7% | 19.3% | .004 |
| Had a hard time doing their job well due to needing to care for others in their home | 3.4% | 6.9% | <.001 |
| Had trouble adequately taking care of family members or friends they provide for | 9.1% | 11.2% | .11 |
| Took over teaching or instructing a child | 7.1% | 11.3% | .02 |
| Had difficulty taking care of children in the home | 1.9% | 3.3% | .01 |
| Had difficulty taking care of their children's needs and/or balancing their needs with other responsibilities | 7.4% | 10.2% | .005 |
| Moved or relocated due to COVID‐19 | 0.5% | 0.8% | .05 |
| Experienced disruptions in day‐to‐day activities with family and/or friends | 61.4% | 72.1% | <.001 |
| Was unable to follow daily routines | 34.5% | 47.4% | <.001 |
| General medical care has been disrupted or delayed | 67.0% | 64.3% | .09 |
| Clinic, doctor's office, or dental practice closed or cancelled an appointment due to COVID‐19 | 56.3% | 60.7% | .14 |
| Respondent cancelled a clinic, doctor, or dental appointment to avoid being around others | 27.4% | 30.2% | .24 |
| Received tangible support from family or friends when needed | 19.9% | 24.6% | .005 |
| Felt social distancing is very important during COVID‐19 | 50.8% | 63.6% | <.001 |
| Reported great concern about COVID‐19 in their community | 28.9% | 40.0% | <.001 |
Concerns about the pandemic
Rural respondents reported great concern about COVID‐19 in their community less often than urban respondents (28.9% vs 40.0% P<.001) (Table 3). Additionally, a lower proportion of rural respondents reported feeling that social distancing during COVID‐19 was very important compared to urban respondents (50.8% vs 63.6%, P<.001).
Urban respondents reported stronger emotional reactions to COVID‐19 (Table 4). Compared to rural respondents, urban respondents more frequently reported feeling nervous, anxious, or on edge (40.0% vs 30.4%, P<.001), feeling anxious about getting COVID‐19 (42.0% vs 35.2%, P<.001), being concerned about a friend or family member getting or dying from COVID‐19 (68.8% vs 61.9%, P<.001), and being concerned about dying from COVID‐19 (33.7% vs 26.3%, P<.001). Urban respondents also more often reported experiencing changes in their sleep, eating, concentration, feelings of sadness/depression and negativity about the future, and feelings of social isolation or loneliness (all P<.001). However, urban respondents also more frequently reported receiving emotional support than rural respondents (62.8% vs 52.5%, P<.001). Rural and urban respondents did not significantly differ in feeling lack of control over how COVID‐19 will impact their life (P = .09).
TABLE 4.
Emotional reactions to COVID‐19
| Respondent location | |||
|---|---|---|---|
| Since the COVID‐19 pandemic, respondents reported agreement/strong agreement with: | Rural (n = 2,347) | Urban (n = 1,278) | P |
| Feeling nervous, anxious, or on edge | 30.4% | 40.0% | <.001 |
| Feeling anxious about getting COVID‐19 | 35.2% | 42.0% | <.001 |
| Worrying about possibly infecting others | 39.9% | 44.4% | .002 |
| Being concerned about a family member or close friend getting or dying from COVID‐19 | 61.9% | 68.8% | <.001 |
| Worrying about the possibility of dying from COVID‐19 | 26.3% | 33.7% | <.001 |
| Feeling they have no control over how COVID‐19 will impact their life | 41.7% | 46.2% | .09 |
| Experiencing feelings of sadness or depression | 29.2% | 38.8% | <.001 |
| Feeling negative about the future | 21.4% | 26.0% | <.001 |
| Experiencing changes in their sleep | 19.3% | 25.8% | <.001 |
| Experiencing changes in their eating | 17.2% | 24.6% | <.001 |
| Experiencing difficulty concentrating | 16.0% | 21.7% | <.001 |
| Experiencing feelings of social isolation or loneliness | 33.2% | 40.9% | <.001 |
| Has received emotional support from family or friends when needed | 52.5% | 62.8% | <.001 |
| Feels a greater appreciation for family and friends since the onset of COVID‐19 | 71.1% | 77.5% | <.001 |
| Feels a greater appreciation for life since the onset of COVID‐19 | 64.4% | 68.5% | .05 |
Health behaviors
Key differences emerged in health behaviors between rural and urban respondents reported from before the pandemic to time of survey response (Table 5). Urban respondents more frequently reported decreased engagement in physical activity (26.5% vs 17.5%, P<.001) and weight gain (23.3% vs 17.2%, P<.001) compared to rural respondents. However, they also more often met daily recommendations for vegetable consumption (3.3% vs 1.9%, P = .003) and more frequently reported an increase in their fruit and vegetable consumption (6.7% vs 4.6%, P = .03). Urban respondents reported more frequent alcohol consumption in the 30 days prior to survey response (P<.001) as well as more frequently reported COVID‐related increases in levels of alcohol consumption compared to rural respondents (14.2% vs 7.5%, P<.001). Rural and urban respondents reported similar physical activity frequency over the past 30 days, lifetime cigarette use, change in smoking/tobacco use, and use of complementary/alternative therapies.
TABLE 5.
Changes in health behaviors from before to during COVID‐19
| Respondent location | |||
|---|---|---|---|
| Characteristic | Rural (n = 2,347) | Urban (n = 1,278) | P |
| Physical activity frequency in the last 30 days | .17 | ||
| 0 days | 18.4% | 15.8% | |
| 1‐10 days | 49.2% | 53.6% | |
| 11‐20 days | 15.5% | 15.3% | |
| 21‐30 days | 17.0% | 15.3% | |
| Change in physical activity compared to before the pandemic | <.001 | ||
| Less activity | 17.5% | 26.5% | |
| Same amount of activity | 73.6% | 58.7% | |
| Increased activity | 9.0% | 14.8% | |
| Weight changed compared to before the pandemic | <.001 | ||
| Increased weight | 17.2% | 23.3% | |
| Same weight | 69.8% | 60.8% | |
| Decreased weight | 13.0% | 15.8% | |
| Met daily recommendations (4 servings) for fruit consumption in the past 30 days | 3.5% | 3.4% | .76 |
| Met daily recommendations (5 servings) for vegetable consumption in the past 30 days | 1.9% | 3.3% | .003 |
| Change in fruit/vegetable consumption compared to before the pandemic | .03 | ||
| Decreased consumption | 4.6% | 6.7% | |
| Same consumption | 88.1% | 84.5% | |
| Increased consumption | 7.3% | 8.8% | |
| Have smoked at least 100 cigarettes in their lifetime | 37.1% | 37.4% | .81 |
| Change in smoking/tobacco use compared to before the pandemic | .44 | ||
| Increased use | 2.4% | 3.3% | |
| Same amount of use | 11.6% | 8.9% | |
| Decreased use | 2.7% | 3.1% | |
| Did not use these products before or during the pandemic | 83.3% | 84.7% | |
| Alcohol consumption in the past 30 days | <.001 | ||
| 0 days | 47.6% | 38.1% | |
| 1‐10 days | 31.4% | 34.9% | |
| 11‐20 days | 9.9% | 13.2% | |
| 21‐30 days | 11.1% | 13.7% | |
| Change in alcohol consumption compared to before the pandemic | <.001 | ||
| Increased consumption | 7.5% | 14.2% | |
| Same amount of consumption | 46.5% | 46.3% | |
| Decreased consumption | 3.6% | 5.6% | |
| Did not use these products before or during the pandemic | 42.3% | 33.9% | |
| Used complementary/alternative therapies in the past 12 months | 48.4% | 45.1% | .07 |
| Change in complementary/alternative therapies compared to before the pandemic | .07 | ||
| Increased use | 5.1% | 5.9% | |
| Same amount of use | 34.8% | 37.8% | |
| Decrease use | 0.6% | 0.7% | |
| Did not use these products before or during the pandemic | 59.5% | 55.5% | |
DISCUSSION
The majority of respondents in our survey, which was administered 6 months into the pandemic, reported experiencing disruptions to their normal activities, having medical appointments cancelled due to the pandemic, and feeling concern about a family member or friend getting or dying from COVID‐19. A considerable portion of respondents reported working closely to persons who might be infected with COVID‐19, experiencing negative changes in their sleep, eating, ability to concentrate, and outlook for the future. More respondents in our survey reported negative pandemic‐related behavior change (decreased physical activity, increased tobacco and other smoking product use, and increased alcohol consumption) than positive pandemic‐related behavior change (increased physical activity, decreased tobacco use and alcohol consumption).
There were marked differences between urban and rural respondents in levels of emotional distress and concern about the pandemic and perceived importance of social distancing behaviors, with those in rural communities being significantly less concerned about COVID‐19 in their community and less likely to think social distancing is important to prevent the spread of COVID‐19. This trend is reflected in other observed rural/urban differences; urban respondents more often reported experiencing disruption to their daily living, stronger negative emotional reactions, and displayed more pronounced behavior change compared to their rural counterparts.
Our findings are largely consistent with studies during COVID‐19 in rural communities. For surveys that compare rural and urban community members, those in rural communities were less likely to participate in social distancing behaviors (76% vs 82%). 61 , 62 , 63 This was consistent in our survey, where a lower proportion of rural residents identified social distancing as very important (50.8% vs 63.6%). Additionally, respondents in rural communities less frequently identified concern about COVID‐19 in their community compared to rural respondents (28.9% vs 40.0%). However, this could reflect the timing of survey implementation and the pandemic impacting urban communities earlier than rural ones.
In some ways, our findings reflect those of studies assessing rural/urban differences in health behaviors prior to the COVID‐19 pandemic. Prior studies have identified that obesity rates are typically higher in rural areas, which was consistent with our findings. 16 , 17 Despite having similar average heights, rural males weighed 8 pounds higher on average compared to urban males, and rural women weighed 5 pounds higher on average compared to urban women. One survey found that those in rural communities were less likely to meet physical activity recommendations; 61 while 3% more rural respondents in our survey indicated having not engaged in physical activity in the month prior to survey completion, this difference was not significant compared to urban respondents. Our item on physical activity frequency in the 30 days prior to survey completion suggests that rural and urban residents report similar levels of prior physical activity (P = .17) though our measures may have not been sufficiently precise to detect smaller differences or differences at the lowest end of the activity scale.
Alcohol use and abuse has been linked to young adults in advantaged and more educated urban areas, 26 which is consistent with our finding of urban adults drinking more days in a 30‐day period compared to rural adults (P<.001). The finding from the previous study could also provide some insight on our finding where individuals in urban areas more frequently reporting increased consumption of alcohol compared to before the COVID‐19 pandemic.
Our survey also had significant departures from studies assessing rural/urban differences in health behaviors prior to the COVID‐19 pandemic. While prior studies have reported greater odds for cigarette smoking among adults in rural counties, 21 , 22 we found no difference between the rural and urban respondents who did not use tobacco products during or before the pandemic. The frequency of rural and urban respondents who have smoked at least 100 cigarettes in their lifetime was also similar between rural and urban respondents. Additionally, our results demonstrated that among individuals who owned a device allowing them to participate in telehealth visits, there was no difference between rural and urban residents in their comfortability in doing so (P = .12). 29
Prior surveys that focused exclusively on rural communities found respondents had significant concerns regarding finances, mental health, and employment. 8 , 9 , 10 , 11 , 12 In our survey, 13% of rural respondents reported difficulties getting by on their present household income and less than half of respondents reported living comfortably on their current income. Additionally, while rural respondents in our survey had less pronounced emotional responses compared to urban respondents, there were still one‐third of rural respondents who indicated feeling anxious about getting COVID‐19, worrying about possibly infecting others, experiencing feelings of sadness or depression, and feeling nervous, anxious, or on edge.
There are several factors that could contribute to the observed differences between rural and urban residents in our results. As this survey was administered from August to December 2020, respondents in rural counties may not have been impacted by the pandemic. A previous study reported that 84% of confirmed COVID‐19 cases resided in urban counties, and another reported that the incidence rate was higher in urban counties compared to rural ones in the first 2 surges of the pandemic (April‐June 2020 and June‐September 2020). 71 , 72 This could support our finding of urban residents reporting stronger emotional reactions and more disruptions to childcare, work schedules, and daily activities. Another theory is that stoicism (the “tough it out” mentality) differentially impacted how rural and urban counties responded to the pandemic. Previous studies have found that stoicism and perceived stigma independently predicted lower odds of seeking mental and physical health services, and were more frequently identified among rural residents. 73 , 74 , 75 In addition, a number of polls have indicated that political affiliation is associated with differing perspectives on COVID‐19, and rural districts in Iowa tend to be more conservative than urban districts. 76
There were several strengths of our study. This was a large population‐based survey in which we received a 40% response rate. In addition, we used a sampling strategy that allowed us to oversample select rural counties to describe their experiences. Often, the experiences of rural respondents are not well represented in surveys; 65% of the respondents in our weighted sample lived in rural counties. Additionally, our questionnaire used previously validated items from other surveys and was offered in multiple modalities (paper and online) in 2 languages (English and Spanish), and used a modified Dillman method to encourage increased participant response.
Limitations include that the study was conducted in 1 state and may not be generalizable to other states/regions. Additionally, our sample was drawn from a relatively rural area of the United States with above average educational attainment, which may further limit generalizability to other samples. Data were drawn from a voter registry file in this state, which has been shown to underrepresent minority populations; only 3% of our overall dataset self‐identified as racial minorities, which is lower than the 2019 population estimate (9%) for the state. 77 The mean age of respondents in our survey was 61 years of age; this is higher than the 2019 state average of 39 years of age. 78 A fourth limitation in our study was the inability to follow up with those who had undeliverable surveys. If surveys were returned with a forwarding address, we were able to resend the survey to the updated address; we were unable to do the same for undeliverable surveys. Due to the cross‐sectional nature of the study, our results are subject to recall bias from respondents. We attempted to minimize the latter limitation by using specific as well as shorter recall time frames (eg, “last 7 days” and “last 30 days”) and asking few questions that required participants to remember information from longer than 1 month prior to survey completion.
Our findings provide important insight regarding the experiences of rural Iowans during COVID‐19 and how these compare to their urban counterparts. Assessing impacts of the COVID‐19 pandemic is important in understanding its effects on rural populations, and how to better tailor services to fit the needs of those who may be experiencing increased difficulties due to the pandemic. The impacts of COVID‐19 in the early parts of the pandemic varied by population density, geographic area, political affiliations of leaders, and behaviors of the communities before the pandemic. Further research using common data items should assess the effects of the pandemic in diverse areas to reveal true differences between rural and urban community members. Additionally, these observed differences in behaviors and health care access call for further research to assess the impact of COVID‐19 on long‐term health outcomes of rural populations.
DISCLOSURES
The authors of this manuscript do not have any conflicts of interest to disclose.
ACKNOWLEDGMENTS
The authors of this manuscript would like to acknowledge the funding sources for this study, as listed below. We would also like to extend our gratitude to Nicholas Rudzianski and Savannah Borman at the University of Iowa for their time in formatting, mailing, processing, and verifying survey data. Special thanks to the representatives at Critical Access Hospitals in the selected rural counties for their time and assistance with testing survey items, and to Miriam Vélez‐Bermúdez, MS, MPH (doctoral candidate at the University of Iowa), as well as Janeth I. Sanchez, PhD, MPH and Michelle Doose, PhD, MPH, (fellows at the National Cancer Institute) for their assistance in translating survey items from English to Spanish.
Greteman BB, Garcia‐Auguste CJ, & Gryzlak BM, et al. Rural and urban differences in perceptions, behaviors, and health care disruptions during the COVID‐19 pandemic. J Rural Health. 2022;1‐13. 10.1111/jrh.12667
Funding information
The project was supported in part by the University of Iowa Holden Comprehensive Cancer Center 3P30CA086862 as well as by the University of Iowa Holden Comprehensive Cancer Center COVID‐19 Supplement Grant 3P30CA086862‐19S5. Research reported in this publication was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Number UL1TR002537. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
REFERENCES
- 1. World Health Organization . Impact of COVID‐19 on People's Livelihoods, Their Health and Our Food Systems. Statement. 2020. Available at https://www.who.int/news/item/13‐10‐2020‐impact‐of‐covid‐19‐on‐people%27s‐livelihoods‐their‐health‐and‐our‐food‐systems. Accessed February 12, 2022.
- 2. Centers for Disease Control and Prevention . CDC COVID Data Tracker. Available at https://covid.cdc.gov/covid‐data‐tracker/#cases_casesper100klast7days. Accessed March 4, 2022.
- 3. IHSRA . The Global Health & Fitness Association. Fitness Industry Still Feels COVID's Negative Impact. 2021. Available at https://www.ihrsa.org/improve‐your‐club/fitness‐industry‐still‐feels‐covids‐negative‐impact/. Accessed February 12, 2022.
- 4. Levy JJ, Tarver TL, & Douglas, HR . Examining the impact of gym closures due to the COVID‐19 pandemic on combat sport athletes’ mental health. J Clin Psychol. 2021;15(4):289‐305. [Google Scholar]
- 5. Kaur H, Singh T, & Arya, YK , et al. Physical fitness and exercise during the COVID‐19 pandemic: a qualitative enquiry. Brief research report. Front Psychol. 2020;11. https://www.frontiersin.org/articles/10.3389/fpsyg.2020.590172/full [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Corallo B, Tolbert JKKF. Impact of Coronavirus on Community Health Centers. 2020. Available at https://www.kff.org/coronavirus‐covid‐19/issue‐brief/impact‐of‐coronavirus‐on‐community‐health‐centers/. Accessed February 12, 2022.
- 7. Mehotra A, Chernew M & Linetsky, D et al. Commonwealth Fund. The Impact of the COVID‐19 Pandemic on Outpatient Visits: A Rebound Emerges. Available at https://www.commonwealthfund.org/publications/2020/apr/impact‐covid‐19‐outpatient‐visits. Accessed February 12, 2022.
- 8. Mueller JT, McConnell K, Burow PB, et al. Impacts of the COVID‐19 pandemic on rural America. Proc Natl Acad Sci U S A. 2021;118(1):2019378118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Quandt SA, LaMonto NJ, Mora DC, et al. COVID‐19 pandemic among Latinx farmworker and nonfarmworker families in North Carolina: knowledge, risk perceptions, and preventive behaviors. Int J Environ Res Public Health. 2020;17(16):5786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Quandt SA, LaMonto NJ, Mora DC, et al. COVID‐19 pandemic among immigrant Latinx farmworker and non‐farmworker families: a rural‐urban comparison of economic, educational, healthcare, and immigration concerns. New Solut. 2021;31(1):30‐47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Williams LB, Fernander AF, Azam T, et al. COVID‐19 and the impact on rural and black church congregants: results of the C‐M‐C project. Res Nurs Health. 2021.44(5), 767–775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Strobel S, Danzi B, Puumala S, et al. Attitudes, and needs: assessing the COVID‐19 impact in rural America. S D Med. 2020;73(11):536‐539. [PubMed] [Google Scholar]
- 13. Kecojevic A, Basch CH, Sullivan M, et al. The impact of the COVID‐19 epidemic on mental health of undergraduate students in New Jersey, cross‐sectional study. PLoS ONE. 2020;15(9):e0239696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Moriarty T, Bourbeau K, Fontana F, et al. The relationship between psychological stress and healthy lifestyle behaviors during COVID‐19 among students in a US Midwest university. Int J Environ Res Public Health. 2021;18(9):4752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wang X, Hegde S, Son C, et al. Investigating mental health of US college students during the COVID‐19 pandemic: cross‐sectional survey study. J Med Internet Res. 2020;22(9):e22817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Befort CA, Nazir N, Perri MG. Prevalence of obesity among adults from rural and urban areas of the United States: findings from NHANES (2005–2008). J Rural Health. 2012;28(4):392‐397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Cohen SA, Greaney ML, Sabik NJ. Assessment of dietary patterns, physical activity and obesity from a national survey: rural‐urban health disparities in older adults. PLoS ONE. 2018;13(12):e0208268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Euler R, Jimenez EY, Sanders S, et al. Rural‐urban differences in baseline dietary intake and physical activity levels of adolescents. Prev Chronic Dis. 2019;16:E01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Liu JH, Jones SJ, Sun H, Probst JC, Merchant AT, Cavicchia P. Diet, physical activity, and sedentary behaviors as risk factors for childhood obesity: an urban and rural comparison. Child Obes. 2012;8(5):440‐448. [DOI] [PubMed] [Google Scholar]
- 20. Robertson MC, Song J, Taylor WC, Durand CP, Basen‐Engquist KM. Urban‐rural differences in aerobic physical activity, muscle strengthening exercise, and screen‐time sedentary behavior. J Rural Health. 2018;34(4):401‐410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Coughlin LN, Bonar EE, Bohnert KM, et al. Changes in urban and rural cigarette smoking and cannabis use from 2007 to 2017 in adults in the United States. Drug Alcohol Depend. 2019;205:107699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Cepeda‐Benito A, Doogan NJ, Redner R, et al. Trend differences in men and women in rural and urban U.S. settings. Prev Med. 2018;117:69‐75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Mantey DS, Omega‐Njemnobi O, Barroso CS. Secondhand smoke exposure at home and/or in a vehicle: differences between urban and non‐urban adolescents in the United States, from 2015 to 2018. Nicotine Tob Res. 2021;23(8):1327‐1333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Warren JC, Smalley KB, Barefoot KN. Perceived ease of access to alcohol, tobacco and other substances in rural and urban US students. Rural Remote Health. 2015;15(4):3397. [PMC free article] [PubMed] [Google Scholar]
- 25. Mumford EA, Stillman FA, Tanenbaum E, et al. Regional rural‐urban differences in e‐cigarette use and reasons for use in the United States. J Rural Health. 2019;35(3):395‐404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Slutske WS, Deutsch AR, Piasecki TM. Neighborhood contextual factors, alcohol use, and alcohol problems in the United States: evidence from a nationally representative study of young adults. Alcohol Clin Exp Res. 2016;40(5):1010‐1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kirby JB, Zuvekas SH, Borsky AE, Ngo‐Metzger Q. Rural residents with mental health needs have fewer care visits than urban counterparts. Health Aff (Millwood). 2019;38(12):2057‐2060. [DOI] [PubMed] [Google Scholar]
- 28. Dobalian A, Tsao JC, Radcliff TA. Diagnosed mental and physical health conditions in the United States nursing home population: differences between urban and rural facilities. J Rural Health. 2003;19(4):477‐483. [DOI] [PubMed] [Google Scholar]
- 29. Chen X, Orom H, Hay JL, et al. Differences in rural and urban health information access and use. J Rural Health. 2019;35(3):405‐417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Connolly SL, Miller CJ, Koenig CJ, et al. Veterans' attitudes toward smartphone app use for mental health care: qualitative study of rurality and age differences. JMIR Mhealth Uhealth. 2018;6(8):e10748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Talbot JA, Burgess AR, Thayer D, Parenteau L, Paluso N, Coburn AF. Patterns of telehealth use among rural Medicaid beneficiaries. J Rural Health. 2019;35(3):298‐307. [DOI] [PubMed] [Google Scholar]
- 32. Ahlers‐Schmidt CR, Hervey AM, Neil T, et al. Concerns of women regarding pregnancy and childbirth during the COVID‐19 pandemic. Patient Educ Couns. 2020;103(12):2578‐2582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Whitaker KM, Hung P, Alberg AJ, et al. Variations in health behaviors among pregnant women during the COVID‐19 pandemic. Midwifery. 2021;95:102929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Campbell K, Weingart R, Ashta J, et al. COVID‐19 knowledge and behavior change among high school students in semi‐rural Georgia. J Sch Health. 2021;91(7):526‐534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Patrick SW, Henkhaus LE, Zickafoose JS, et al. Well‐being of parents and children during the COVID‐19 pandemic: a national survey. Pediatrics. 2020;146(4):e2020016824. [DOI] [PubMed] [Google Scholar]
- 36. Baptist AP, Lowe D, Sarsour N, et al. Asthma disparities during the COVID‐19 pandemic: a survey of patients and physicians. J Allergy Clin Immunol Pract. 2020;8(10):3371‐3377.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Islam JY, Vidot DC, Camacho‐Rivera M. Determinants of COVID‐19 preventive behaviours among adults with chronic diseases in the USA: an analysis of the nationally representative COVID‐19 impact survey. BMJ Open. 2021;11(2):e044600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Wolf MS, Serper M, Opsasnick L, et al. Awareness, attitudes, and actions related to COVID‐19 among adults with chronic conditions at the onset of the U.S. outbreak: a cross‐sectional survey. Ann Intern Med. 2020;173(2):100‐109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Kecojevic A, Basch CH, Sullivan M, et al. The impact of the COVID‐19 epidemic on mental health of undergraduate students in New Jersey, cross‐sectional study. PLoS ONE. 2020;15(9):e0239696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Moriarty T, Bourbeau K, Fontana F, et al. The relationship between psychological stress and healthy lifestyle behaviors during COVID‐19 among students in a US Midwest University. Int J Environ Res Public Health. 2021;18(9):4752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Wang X, Hegde S, Son C, et al. Investigating mental health of US college students during the COVID‐19 pandemic: cross‐sectional survey study. J Med Internet Res. 2020;22(9):e22817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Alsan M, Stantcheva S, Yang D, et al. Disparities in coronavirus 2019 reported incidence, knowledge, and behavior among US adults. JAMA Netw Open. 2020;3(6):e2012403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Jones J, Sullivan PS, Sanchez TH, et al. Similarities and differences in COVID‐19 awareness, concern, and symptoms by race and ethnicity in the United States: cross‐sectional survey. J Med Internet Res. 2020;22(7):e20001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Geana MV. Kansans in the middle of the pandemic: risk perception, knowledge, compliance with preventive measures, and primary sources of information about COVID‐19. Kans J Med. 2020;13:160‐164. [PMC free article] [PubMed] [Google Scholar]
- 45. Thorpe A, Scherer AM, Han PKJ, et al. Exposure to common geographic COVID‐19 prevalence maps and public knowledge, risk perceptions, and behavioral intentions. JAMA Netw Open. 2021;4(1):e2033538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Bruine de Bruin W, Bennett D. Relationships between initial COVID‐19 risk perceptions and protective health behaviors: a national survey. Am J Prev Med. 2020;59(2):157‐167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Clements JM. Knowledge and behaviors toward COVID‐19 among US residents during the early days of the pandemic: cross‐sectional online questionnaire. JMIR Public Health Surveill. 2020;6(2):e19161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. French MT, Mortensen K, Timming AR. Psychological distress and coronavirus fears during the initial phase of the COVID‐19 pandemic in the United States. J Ment Health Policy Econ. 2020;23(3):93‐100. [PubMed] [Google Scholar]
- 49. Ali SH, Foreman J, Capasso A, et al. Social media as a recruitment platform for a nationwide online survey of COVID‐19 knowledge, beliefs, and practices in the United States: methodology and feasibility analysis. BMC Med Res Methodol. 2020;20(1):116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Fridman I, Lucas N, Henke D, et al. Association between public knowledge about COVID‐19, trust in information sources, and adherence to social distancing: cross‐sectional survey. JMIR Public Health Surveill. 2020;6(3):e22060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Nagler RH, Vogel RI, Gollust SE, et al. Public perceptions of conflicting information surrounding COVID‐19: results from a nationally representative survey of U.S. adults. PLoS ONE. 2020;15(10):e0240776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Riehm KE, Holingue C, Kalb LG, et al. Associations between media exposure and mental distress among U.S. adults at the beginning of the COVID‐19 pandemic. Am J Prev Med. 2020;59(5):630‐638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Zhong B, Jiang Z, Xie W, et al. Association of social media use with mental health conditions of nonpatients during the COVID‐19 outbreak: insights from a national survey study. J Med Internet Res. 2020;22(12):e23696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Boschuetz N, Cheng S, Mei L, Loy VM. Changes in alcohol use patterns in the United States during COVID‐19 pandemic. WMJ. 2020;119(3):171‐176. [PubMed] [Google Scholar]
- 55. Pollard MS, Tucker JS. Changes in adult alcohol use and consequences during the COVID‐19 pandemic in the US. JAMA Netw Open. 2020;3(9):e2022942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Duncan GE, Avery AR, Seto E, et al. Perceived change in physical activity levels and mental health during COVID‐19: findings among adult twin pairs. PLoS ONE. 2020;15(8):e0237695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Ettman CK, Abdalla SM, Cohen GH, et al. Prevalence of depression symptoms in US adults before and during the COVID‐19 pandemic. JAMA Netw Open. 2020;3(9):e2019686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Holingue C, Badillo‐Goicoechea E, Riehm KE, et al. Mental distress during the COVID‐19 pandemic among US adults without a pre‐existing mental health condition: findings from American trend panel survey. Prev Med. 2020;139:106231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Kantor BN, Kantor J. Mental health outcomes and associations during the COVID‐19 pandemic: a cross‐sectional population‐based study in the United States. Front Psychiatry. 2020;11:569083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Taylor S, Landry CA, Paluszek MM, et al. Worry, avoidance, and coping during the COVID‐19 pandemic: a comprehensive network analysis. J Anxiety Disord. 2020;76:102327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Beck AM, Gilbert AS, Duncan DD, et al. A cross‐sectional comparison of physical activity during COVID‐19 in a sample of rural and non‐rural participants in the US. Int J Environ Res Public Health. 2021;18(9):4991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Callaghan T, Lueck JA, Trujillo KL, et al. Rural and urban differences in COVID‐19 prevention behaviors. J Rural Health. 2021;37(2):287‐295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Probst JC, Crouch EL, Eberth JM. COVID‐19 risk mitigation behaviors among rural and urban community‐dwelling older adults in summer, 2020. J Rural Health. 2021;37(3):473‐478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Rural Health Information Hub (RHIHub) . Critical Access Hospitals (CAHs). Available at https://www.ruralhealthinfo.org/topics/critical‐access‐hospitals. Accessed October 5, 2021.
- 65. Hoddinott SN, Bass MJ. The Dillman total design survey method. Can Fam Physician. 1986;32:2366‐2368. [PMC free article] [PubMed] [Google Scholar]
- 66. Centers for Disease Control and Prevention (CDC) . Behavioral Risk Factor Surveillance System Survey Questionnaire . Atlanta, GO: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention. Available at https://www.cdc.gov/brfss/index.html. Accessed October 5, 2021.
- 67. Centers for Disease Control and Prevention . Health Information National Trends Survey (HINTS) . National Center for Health Statistics, Hyattsville, MD, Centers for Disease Control and Prevention, U.S. Department of Health and Human Services. Available at https://hints.cancer.gov/docs/Instruments/HINTS_2003_Instrument‐English.pdf. Accessed January 31, 2022.
- 68. Centers for Disease Control and Prevention . National Health Interview Survey (NHIS) Public Use Data Release, NHIS Survey Description. Division of Health Interview Statistics, National Center for Health Statistics, Hyattsville, MD, Centers for Disease Control and Prevention, U.S. Department of Health and Human Services. Available at http://www.cdc.gov/nchs/nhis.htm. Accessed October 5, 2021.
- 69. Penedo FJ, Cohen L, Bower J, et al. Impact of the COVID‐19 Pandemic in Cancer Survivors. Unpublished Questionnaire. 2010.
- 70. Rural‐Urban Continuum Codes USDA ERS ‐ Rural‐Urban Continuum Codes. Available at https://www.ers.usda.gov/data‐products/rural‐urban‐continuum‐codes.aspx 2020. Accessed Mar 3, 2022.
- 71. Huang Q, Jackson S, & Derakhshan, S , et al. Urban‐rural differences in COVID‐19 exposures and outcomes in the South: a preliminary analysis of South Carolina. PLoS ONE. 2021;16(2):e0246548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Cuadros DF, Branscum AJ, & Mukandavire, Z , et al. Dynamics of the COVID‐19 epidemic in urban and rural areas in the United States. Ann Epidemiol. 2021;59:16‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Warbinton E. Mental Health in Rural Areas: To What Extent Do Stoicism, Stigma, and Community Affiliation Predict Mental Health Help‐Seeking Behaviors? Student dissertation. SHAREOK; 2021. [Google Scholar]
- 74. Swannell C. “Rural stoicism”: an excuse for poor health care access. InSight+. 2020;48(7). Available at https://insightplus.mja.com.au/2020/48/rural‐stoicism‐an‐excuse‐for‐poor‐health‐care‐access/. Accessed Mar 3, 2022. [Google Scholar]
- 75. Moore A, Grime J, & Campbell, P , et al. Troubling stoicism: sociocultural influences and applications to health and illness behaviour. SAGE Health. 2012;17(2):159‐173. [DOI] [PubMed] [Google Scholar]
- 76. Neelon B, Mutiso F, Mueller NT, Pearce JL, Benjamin‐Neelon SE. Associations between governor political affiliation and COVID‐19 cases, deaths, and testing in the U.S. Am J Prev Med. 2021;61(1):115‐119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. United States Census Bureau QuickFacts Iowa. Available at https://www.census.gov/quickfacts/IA. 2020. Accessed Mar 3, 2022.
- 78. Iowa State Data Center Iowa Quick Facts. Available at https://www.iowadatacenter.org/quickfacts. 2020. Accessed Mar 3, 2022.


