Abstract
Aims
To estimate the prevalence of burnout risk among nurses during the peak of the first wave of the COVID‐19 pandemic in Belgium and to identify risk groups and protective and risk factors.
Background
Nurses are at high risk of burnout, and this can have negative consequences for them, patients and health care systems. The pandemic may have changed their working conditions and increased their risk of burnout.
Methods
The risk of burnout was assessed through the Maslach Burnout Inventory Scale. Information on socio‐demographic and working conditions during the pandemic was also collected. We obtained 4552 respondents through convenience sampling.
Results
A high risk of burnout was found in 70% of respondents. The main risk factors of burnout were the lack of personal protective equipment, changes in perceived workload and working with COVID‐19 patients.
Conclusions
An uneven workload for nurses is an underlying problem during the COVID‐19 pandemic and a significant risk factor for their burnout. The decreased workload is a risk factor for burnout as important as increased workload and repeated exposure to COVID‐19.
Implications for Nursing Management
Burnout prevention and treatment interventions must target the correct risk factors and identify nurses at risk to be cost‐effective.
Keywords: burnout, COVID‐19, nurses, protective factors, risk factors
What is already known
Nurses have a high prevalence of burnout around the world (11.2%) and more specifically in Belgium.
Belgium experienced nurse and hospital bed shortages before the outbreak of the COVID‐19 pandemic.
Different risk and protective factors for developing burnout among nurses exist.
What this paper adds
The current study found that 70% of nurses were at high risk of burnout during the first wave of the COVID‐19 in Belgium.
The main risk factors of burnout for nurses during the first wave of the COVID‐19 pandemic were a lack of personal protective equipment for COVID‐19 and changes in perceived workload.
In terms of working conditions during the pandemic, the following burnout risk factors have been identified: working above full‐time schedule over the past weeks, having more than 75% of patients with COVID‐19 in the ward, being exposed to the death of COVID‐19 patients and having more than half of the colleagues on sick leave.
1. BACKGROUND
In December 2019, the SARS‐COV‐2 virus originated in China, and in a matter of weeks, the COVID‐19 pandemic affected our lives on a worldwide scale (WHO, 2020b). Belgium was harshly affected by the virus in terms of hospitalizations and deaths (Sciensano, 2020). In pre‐COVID times, indicators on nurse workforce availability questioned Belgian capacity to handle demographic changes. Moreover, the number of nurses per patient in the hospital remained low compared with other countries (KCE, 2019a). Past reductions of hospital beds in Belgium have not eased COVID‐19 crisis management either (WHO, 2020). The rapid spread of the virus and the difficulties in anticipating the evolution of the pandemic reinforced the deficit of intensive care unit (ICU) beds and health care workers and material resources shortage (Cheung et al., 2020). Protective equipment and medical supplies including personal protective equipment (PPE), ventilators and diagnostic tests scarcity were of preeminent concern (Emanuel et al., 2020; Pecoraro et al., 2020). The circumstances also increased nurses' workload and exposure to death and suffering (Bruyneel et al., 2021; Guixia & Hui, 2020; Hu et al., 2020). These facts illustrate how the COVID‐19 pandemic has exposed nurses to working conditions, which could partly explain the increase in their risk of burnout.
Burnout is defined as a dangerous circumstance experienced by a professional in response to chronic work‐related stress (WHO, 2019). Maslach and Jackson highlighted three dimensions to the burnout syndrome: emotional exhaustion (EE), depersonalization (DP) and reduced personal accomplishment (PA) (Maslach et al., 1986). EE is a state of generalized fatigue that may be caused by time‐consuming interactions with patients and/or fellow workers. DP is the development of a detached attitude towards work and patient care. Finally, reduced PA can be revealed when nurses have an overall poor professional self‐esteem (American Thoracic Society, 2016). The interaction of these three dimensions distinguishes burnout from stress and other psychological issues with comparable symptoms like fatigue or depression (Awa et al., 2010). Approximately 1/10 of nurses worldwide suffered high burnout symptoms in pre‐COVID times (Woo et al., 2020). A Belgian study conducted before the outbreak of the pandemic found that 36% of nurses working in acute hospitals had a high risk of EE, 32% high risk of DP and 31% high risk of reduced PA (KCE, 2019b). Various personal factors (e.g., gender, age and having children) and/or external factors (e.g., poor working conditions, excessive workloads and frequent call duties) may be associated with burnout development in nurses (Molina‐Praena et al., 2018; Patel et al., 2018).
Although the burnout of nurses was significant pre‐COVID‐19 times, their living and working conditions during the pandemic such as daily exposure to death, increased workload, poor knowledge of the virus, lack of clear guidelines, shortage of PPE and professional devaluation can enhance their risk of burnout (Miranda et al., 2020). In addition, the increased number of infected patients and hospital admissions without an increased nursing staff induces a higher patient per nurse ratio and therefore an increased workload. Finally, some countries have been more severely hit by the pandemic than others.
In Belgium, the COVID‐19 Hospital Emergency Plan was launched on 13 March 2020, and the first peak of the pandemic took place in April and May 2020 with between 400 and 500 new hospitalizations per day (Sciensano, 2020). Between March and June 2020, 1696 COVID‐19 patients were admitted to ICUs in Belgium (Faes et al., 2021), and the number of intensive care beds was increased to 2000 with the opening of 800 new beds (Taccone et al., 2021). Belgium was strongly impacted by the first wave of COVID‐19 compared with other European countries. During the first peak of the pandemic, Belgium's hospitalization rate was nearly twelve times higher than that of France, and its crude death rate from COVID‐19 was almost twice as high (Etalab, 2020; Hardy et al., 2021; Sciensano, 2020).
Taken together, these different elements highlight that the COVID‐19 pandemic may have worsened the risk of burnout among nurses, with potentially negative consequences for professionals, for health systems and above all for patients. In addition, as we do not know for how long the pandemic will last, it is crucial to (1) assess the risk of burnout among nurses, (2) prevent risk factors of burnout while enhancing protective factors and (3) to set up adequate diagnostic and treatment programmes. To date, only a few studies have evaluated global nurses' burnout and associated risk factors during the COVID‐19 pandemic (Galanis et al., 2020). However, to the best of our knowledge, no such analysis has been conducted in Belgium. The objectives of this study were (1) to estimate the prevalence of burnout risk among nurses in Belgium during the peak of the first wave of the COVID‐19 pandemic and (2) to identify groups more at risk as well as protective and risk factors for burnout to focus on efficient prevention and treatment programmes.
2. METHODS
2.1. Study setting and design
The Belgian health care system is a regulated‐market, social insurance‐based system characterized by a substantial level of corporatism in policy decision‐making. Although the provision, coordination and funding of care are the responsibility of the political authorities, these responsibilities tend to be delegated to semi‐public institutions in which stakeholders, such as sickness funds and representatives of professionals, have a high level of bargaining power and defend their particular interests (Gerkens & Merkur, 2010). At the end of January 2020, the Belgian authorities reported the identification of a new coronavirus in Wuhan, China, and in March 2020, the number of COVID‐19 cases in Belgium increased exponentially. As previously explained, Belgium was strongly impacted by the first wave of COVID‐19 compared with other European countries. The data for this study were collected between April 2 and 4 May 2020, during the first peak of the pandemic in Belgium (see Figure 1).
FIGURE 1.
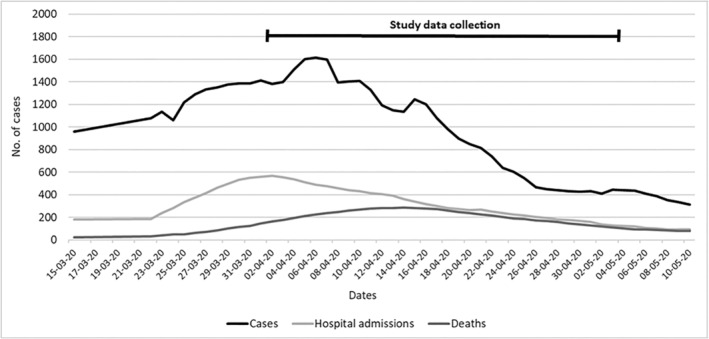
Number of COVID‐19 cases, hospital admissions and deaths in Belgium between 15 March and 10 May 2020 (data centralized by Sciensano, the Belgian federal public health institute)
The study was cross‐sectional. To be included in the study, nurses had to be over 18 years old, and they had to be working in the French‐speaking part of Belgium. Questions about these inclusion criteria were asked following informed consent and were required to access the questionnaire. In addition, participants who were professionally inactive during the pandemic were excluded. The survey contained a question to ensure that the respondent was working as a nurse during the pandemic. We established a web‐based survey through Qualtrics® XM platform, which is compliant with General Data Protection Regulation. The self‐administered online questionnaire was available from April 2 until 4 May 2020 and was disseminated among Belgian professional nursing associations, inpatient and outpatient health care services (e.g., hospitals, nursing homes and home care services) and social media. In 2016, there were 202,402 nurses licenced to practice in Belgium, and 124,196 of them were working in the health care sector (e.g., hospitals and nursing homes). The distribution of nurses among the three Belgian regions is proportionate to the size of the population in each region. Among the nurses working in the health care sector, 64% are in Flanders, 28% in Wallonia and 8% in Brussels. We targeted nurses working in and out of hospitals in the French‐speaking part of Belgium (i.e., Wallonia and Brussels) and got a total of 4552 respondents through convenience sampling, which represents around 11% of the nurses practising in Wallonia and Brussels.
2.2. Primary outcome
The primary outcome of interest was the risk of burnout. Because our study is cross‐sectional, we assessed the prevalence of burnout. We were looking at one moment in time, and we did not determine whether there were new cases of burnout (CDC, 2012). Burnout was assessed by the Maslach Burnout Inventory (MBI) scale, which can be considered as a gold standard instrument for the assessment of the risk of burnout among care professionals (Cañadas‐de la Fuente et al., 2015; Maslach et al., 1986; Pérez‐Fuentes et al., 2018; Ribeiro et al., 2014; Trockel et al., 2018). The MBI captures the following dimensions of burnout: EE, DP and reduced PA. We used the validated French version of the MBI, which is a 22‐item questionnaire (nine items for EE, five items for DP and eight items for reduced PA). The three dimensions have pre‐determined cut‐off points to identify, in each category, individuals at low, moderate and high risk of burnout as suggested in the scale user manual (Maslach et al., 1986).
The cut‐off points for low, moderate and high risk were, respectively:
For EE (from 0 to 54): 0–18, 19–26 and ≥27;
For DP (from 0 to 30): 0–5, 6–9 and ≥10;
For reduced PA (from 0 to 48): ≥40, 34–39 and 0–33.
Similarly to other studies, to estimate the overall risk of burnout, we considered that an individual with a high risk in at least one of the three dimensions can be considered to be at high risk of burnout (Rotenstein et al., 2018).
2.3. Independent variables
Based on the literature, socio‐demographic data as well as data on working conditions during the COVID‐19 pandemic were collected and included in the analysis (Miranda et al., 2020; Molina‐Praena et al., 2018; Patel et al., 2018). These potential explanatory factors for the risk of burnout included age, gender, the type of degree, seniority in the health care sector, the type of service in which the nurse works, the length of working time, the perceived workload during the COVID‐19 pandemic, the adequacy and availability of PPE, the perceived proportion of COVID‐19 patients in the ward over the past week, the perceived proportion of patients who died from COVID‐19 in the ward and the proportion of colleagues on sick leave due to COVID‐19.
2.4. Data analysis
Descriptive statistics were computed to describe socio‐demographic, work and COVID‐19‐related characteristics of the sample. In addition, Chi‐square tests were performed to assess whether the proportion of overall risk of burnout (i.e., having a high risk in at least one of the three dimensions of burnout) was significantly different depending on the characteristics of the nurses.
Afterwards, univariate and multivariate logistic regression models were performed to analyse the strength of the association between the potential determinants and the overall risk of burnout. Regarding the potential determinants, for categorical variables, a reference category was chosen for each variable. For example, for the variable ‘types of services’ comprising 11 categories, the reference category was ‘medical or surgical ward’ because this category represents general services in hospitals and had a satisfactory sample size. The risk of burnout in other services is therefore determined in comparison with nurses working in medical or surgical ward. Only the significant determinants in univariate regressions were included in the multivariate regression models to limit the number of variables and the risk of collinearity in the final models. Odds ratio (OR), 95% confidence intervals (95% CI) and p values were used to describe the results. All statistics were performed using IBM SPSS Statistics 27.0 and SAS 9.3. P values less than .05 were considered statistically significant.
2.5. Ethical considerations
Participation was voluntary, anonymous and did not involve any compensation. Inform consent was obtained from all participants. The Belgian Law does not require approval from an Ethical Board for an online survey with the general population. However, the study is covered by privacy regulations. Participants were provided with legal information relating to consent. All information related to respondents' consent and the General Data Protection Regulation is available on request. This is by the Law that is applicable, including the regulation 2016/679 of the European Parliament and of the Council of 27 April 2016 on the protection of natural persons about the processing of personal data and on the free movement of such data and repealing Directive 95/46/EC—General Data Protection Regulation. All methods were performed under the relevant Belgian guidelines and regulations.
3. RESULTS
Table 1 shows the descriptive analysis of sociodemographic, work and COVID‐19‐related characteristics of the sample as well as the distribution of the overall risk of burnout. The mean age in years of respondents was 39.7 (SD = 10.9), and most of them were female (84%). In terms of seniority in the health care sector, 25% of the respondents had between 0 and 5 years of seniority and 27% between 11 and 20 years. There was a higher proportion of respondents working in ICU (28%), medical or surgical wards in hospital (22%), home care (14%) and hospital emergency services (11%).
TABLE 1.
Descriptive analysis of socio‐demographic, work and COVID‐19‐related and risk of burnout variables of the sample (n = 4 552)
| Variables | Total n = 4552 | Overall risk of burnout a | χ 2 (p value) |
|---|---|---|---|
| Age, year, n (%) | |||
|
1224 (26.9) | 71.0% | 2.9 (.29) |
|
1356 (29.8) | 69.7% | |
|
1042 (22.9) | 67.8% | |
|
930 (20.4) | 67.1% | |
| Gender, n (%) | |||
|
3823 (84.0) | 68.3% | 9.7 (.007) |
|
729 (16.0) | 73.6% | |
| Nurses with child(ren), n (%) | |||
|
2730 (60.3) | 68.9% | 3.8 (.05) |
|
1822 (49.7) | 71.0% | |
| Seniority in the health care sector, year, n (%) | |||
|
1119 (24.6) | 71.1% | 11.6 (.02) |
|
720 (15.8) | 70.7% | |
|
1224 (26.9) | 66.3% | |
|
901 (19.8) | 65.2% | |
|
588 (12.9) | 63.6% | |
| Types of services, n (%) | |||
|
921 (22.6) | 67.6% | 31.6 (<.001) |
|
237 (5.8) | 73.1% | |
|
96 (2.3) | 71.9% | |
|
467 (11.5) | 71.5% | |
|
1149 (28.2) | 67.8% | |
|
566 (13.9) | 66.6% | |
|
112 (2.7) | 65.1% | |
|
135 (3.4) | 64.3% | |
|
81 (2.0) | 61.7% | |
|
148 (3.6) | 58.8% | |
|
162 (4.0) | 65.7% | |
| Working above full‐time schedule over the past weeks, n (%) | |||
|
740 (16.4) | 71.0% | 3.8 (.04) |
|
3812 (83.6) | 67.2% | |
| Having adequate and sufficient PPE for COVID‐19, n (%) | |||
|
1484 (39.6) | 60.1% | 47.6 (<.001) |
|
3068 (60.4) | 74.5% | |
| Proportion of COVID‐19 patients in the ward over the last week, n (%) | |||
|
958 (25.9) | 71.0% | 35.4 (<.001) |
|
480 (12.9) | 68.8% | |
|
700 (18.9) | 67.4% | |
|
1070 (28.9) | 60.4% | |
|
500 (13.4) | 57.5% | |
| Proportion of deaths related to COVID‐19 since COVID‐19 outbreak, n (%) | |||
|
135 (3.0) | 70.1% | 30.1 (<.001) |
|
313 (6.9) | 71.5% | |
|
1529 (33.8) | 68.0% | |
|
1687 (37.3) | 60.1% | |
| Proportion of colleagues on sick leave since COVID‐19 outbreak, n (%) | |||
|
99 (2.2) | 69.5% | 24.2 (<.001) |
|
236 (5.2) | 75.3% | |
|
2187 (48.3) | 65.9% | |
|
1198 (26.5) | 60.1% | |
| The perceived workload during the COVID‐19 pandemic was, n (%) | |||
|
513 (14.3) | 68.5% | 35.6 (<.001) |
|
561 (15.6) | 60.2% | |
|
2516 (70.1) | 71.2% | |
| Measures of burnout, n (%) | |||
|
1581 (34.9) | / | |
|
1062 (23.5) | ||
|
1704 (37.7) | ||
|
3205 (70.1) |
Note: Descriptive statistics were performed after the exclusion of missing data.
Abbreviations: ICU, intensive care unit; PPE, personal protective equipment; SD, standard deviation.
Having a high risk in at least one of the three dimensions of burnout.
Almost two‐thirds (60%) of the respondents declared having inadequate and insufficient PPE. Nearly 26% of respondents revealed treating more than 75% of COVID‐19 patients in their ward over the past week. Approximately 50% of the respondents stated that less than 25% of their colleagues were absent since the start of the pandemic. The majority of respondents also had a higher perceived workload since the outbreak of the pandemic (70%).
The analysis on the MBI revealed that 35% of respondents were at high risk of EE, 24% at high risk of DP and 38% at high risk of reduced PA. An overall risk of burnout (i.e., having a high risk in at least one of the three dimensions of burnout) was found in 70% of the respondents.
A significantly higher proportion of men had an overall risk of burnout compared with women (74% vs. 68%, χ 2 = 9.7, p = .007). The proportion of overall risk of burnout was also significantly different according to seniority (χ 2 = 11.6, p = .02), with 71% of risk of burnout among respondents with 0–5 years of seniority and 64% among those with more than 30 years of seniority. The proportion of overall risk of burnout was significantly different between services (χ 2 = 31.6, p < .001), with a higher proportion in nursing homes (73%), in COVID‐19 hospital wards (72%) and in emergency services (71%). The lowest proportion was in hospital psychiatric wards (59%). A significantly higher proportion of overall risk of burnout was also found among respondents working above full time over the past weeks (71% vs. 67%, χ 2 = 3.8, p = .04) and not having adequate and sufficient PPE (74% vs. 60%, χ 2 = 47.6, p < .001). This proportion was also significantly different depending on the number of COVID‐19 patients in the ward over the last weeks (χ 2 = 35.4, p < .001), the number of COVID‐19‐related deaths (χ 2 = 30.1, p < .001) and the number of colleagues on sick leave since the COVID‐19 outbreak (χ 2 = 24.2, p < .001). The proportion of overall risk of burnout being higher among respondents exposed to more COVID‐19 patients in the ward over the last weeks, more COVID‐19‐related deaths and more colleagues on sick leave. Finally, this proportion was significantly higher among respondents with an increased workload (71%) and those with a decreased workload (68%) than among those with a stable workload (60%) during the pandemic (χ 2 = 35.6, p < .001). The proportion of overall risk of burnout was not significantly different depending on the age of the respondents and whether or not they had children.
Table 2 presents the associations between sociodemographic, work and COVID‐19‐related variables and the overall risk of burnout, using univariate and multivariate logistic regression models.
TABLE 2.
Factors associated with the overall risk of burnout using univariate and multivariate logistic regression models
| Variables | Risk of burnout (yes) | |
|---|---|---|
| Univariate OR (95% CI) | Multivariate OR (95% CI) | |
| Age (year) | ||
|
2.2 (1.8–2.8)** | 1.7 (1.2–2.5)** |
|
0.9 (0.6–1.3) | 0.9 (0.4–1.7) |
|
0.8 (0.6–1.1) | 0.8 (0.4–1.5) |
|
REF | REF |
| Gender, women (REF = men) | 1.0 (0.8–1.2) | |
| Children, yes (REF = no) | 0.9 (0.7–1.1) | |
| Seniority in health care (year) | ||
|
1.9 (1.4–2.6)** | 1.7 (0.7–2.1) |
|
1.7 (1.2–2.3)** | 1.3 (0.7–2.2) |
|
1.2 (0.8–1.7) | 0.9 (0.6–1.6) |
|
1.2 (0.8–1.6) | 1.1 (0.7–1.7) |
|
REF | REF |
| Types of services: | ||
|
REF | REF |
|
2.2 (1.2–4.1)** | 1.5 (1.1–1.9)** |
|
0.7 (0.3–1.4) | 0.9 (0.5–1.6) |
|
1.5 (1.1–2.3)* | 1.1 (0.7–1.8) |
|
1.1 (0.7–1.7) | 1.4 (0.9–2.2) |
|
2.3 (1.8–3.0)*** | 1.7 (1.6–1.9)** |
|
0.9 (0.4–1.7) | 0.8 (0.5–1.2) |
|
0.8 (0.4–1.5) | 1.2 (0.9–1.6) |
|
1.7 (1.2–2.3)*** | 1.4 (1.1–1.9)** |
|
0.9 (0.7–1.3) | 0.9 (0.6–1.6) |
|
1.3 (0.8–2.2) | 1.4 (0.7–2.8) |
| Working above full‐time schedule over the past weeks (REF = no) | 1.9 (1.4–2.6)** | 1.5 (1.2–1.8)** |
| Having adequate and sufficient PPE for COVID‐19 (REF = no) | 2.7 (1.9–4.2)*** | 2.3 (1.8–3.1)*** |
| Proportion of COVID‐19 patients in the ward over the last week | ||
|
1.8 (1.2–2.7)** | 1.5 (1.2–2.1)** |
|
1.2 (0.7–1.8) | 0.9 (0.8–1.4) |
|
1.1 (0.8–1.7) | 1.0 (0.9–1.1) |
|
1.2 (0.8–1.6) | 0.7 (0.4–1.2) |
|
REF | REF |
| Proportion of deaths related to COVID‐19 since COVID‐19 outbreak | ||
|
2.3 (1.8–3.1)** | 1.8 (1.2–2.7)** |
|
1.5 (1.1–1.9)** | 1.2 (0.9–1.6) |
|
1.1 (0.9–1.3) | 0.9 (0.8–1.4) |
|
REF | REF |
| Proportion of colleagues on sick leave since COVID‐19 outbreak | ||
|
2.1 (1.5–2.8)** | 1.7 (1.2–2.4)* |
|
1.0 (0.7–1.4) | 0.9 (0.7–1.2) |
|
1.0 (0.9–1.2) | 0.9 (0.7–1.3) |
|
REF | REF |
| The perceived workload during the COVID‐19 pandemic was | ||
|
1.5 (1.2–2.1)** | 1.2 (1.1–1.5)* |
|
REF | REF |
|
2.7 (2.1–3.6)*** | 2.1 (1.5–2.8)*** |
Abbreviations: 95% CI = 95% confidence intervals; ICU, intensive care unit; OR, odds ratio; PPE, personal protective equipment.
p value < .05.
p value < .01.
p value < .001.
The univariate logistic regression models on the overall risk of burnout highlighted several associated factors. Nurses aged 18–30 were more at risk of burnout (OR = 2.2, 95% CI = 1.8–2.8) compared with those over 50, and nurses with seniority in health care between 0 and 5 years (OR = 1.9, 95% CI = 1.4–2.6) and 6 and 10 years (OR = 1.7, 95% CI = 1.2–2.3) were also more at risk than those with more than 30 years of seniority. Nurses working in ICU (OR = 2.3, 95% CI = 1.8–3.0), in hospital emergency services (OR = 2.2, 95% CI = 1.2–4.1), in nursing homes (OR = 1.7, 95% CI = 1.2–2.3) and in COVID‐19 wards in hospital (OR = 1.5, 95% CI = 1.1–2.3) had a higher probability of being at risk of burnout in comparison with those working in hospital medical or surgical wards. Working above full‐time schedule over the past weeks (OR = 1.9, 95% CI = 1.4–2.6) and not having enough PPE for COVID‐19 (OR = 2.7, 95% CI = 1.9–4.2) were also associated with a higher probability of burnout risk. Nurses working in wards with more than 75% of patients with COVID‐19 (OR = 1.8, 95% CI = 1.2–2.7) and exposed to deaths in more than 25% of COVID‐19 patients (between 25%a nd 49%: OR = 1.5, 95% CI = 1.1–1.9; more than 50%: OR = 2.3, 95% CI = 1.8–3.1) had a higher probability of being at risk of burnout compared with nurses working in wards without COVID‐19 patient. Nurses with more than 50% of colleagues on sick leave (OR = 2.1, 95% CI = 1.5–2.8) had a higher probability of burnout risk compared with nurses without colleagues on sick leave. Finally, nurses reporting an increase (OR = 2.7, 95% CI = 2.1–3.6) or a decrease (OR = 1.5, 95% CI = 1.2–2.1) in their workload during the pandemic had a higher probability of burnout risk than those with a stable workload.
Regarding the variables associated with a risk of burnout in the multivariate model, only seniority in the health sector was no longer significantly associated. The main predictors of burnout risk were not having enough PPE for COVID‐19 (AOR = 2.3, 95% CI = 1.8–3.1) and having an increased workload during the pandemic (AOR = 2.1, 95% CI = 1.5–2.8). The following predictors remained significantly associated with burnout: younger age (18–30 years old, AOR = 1.7, 95% CI = 1.2–2.5), working in hospital emergency services (AOR = 1.5, 95% CI = 1.1–1.9), in ICU (AOR = 1.7, 95% CI = 1.6–1.9) or in nursing homes (AOR = 1.4, 95% CI = 1.1–1.9), working above full‐time schedule over the past weeks (AOR = 1.5, 95% CI = 1.2–1.8), having more than 75% of patients with COVID‐19 in the ward (AOR = 1.5, 95% CI = 1.2–2.1), being exposed to deaths in more than 50% of COVID‐19 patients (AOR = 1.8, 95% CI = 1.2–2.7), having more than 50% of colleagues on sick leave (AOR = 1.7, 95% CI = 1.2–2.4) and having a decreased workload during the pandemic (AOR = 1.2, 95% CI = 1.1–1.5).
4. DISCUSSION
4.1. Main findings
The current study found that 70% of our sample of nurses was at high risk of burnout (overall risk, i.e., having a high risk in at least one of the three dimensions of burnout) during the first wave of the COVID‐19 in Belgium. Our findings showed that 34.9% of our sample was at high risk of EE, 37.7% at high risk of reduced PA and 23.5% at high risk of DP.
The two main risk factors of burnout were lacking adequate PPE for COVID‐19 and having an increased workload during the pandemic. Interestingly, having a decreased workload during the pandemic was also associated with a significant risk of burnout. Younger nurses (i.e., between 18 and 30 years old) were more at risk of burnout. Nurses working in certain services such as ICU, hospital emergency services and nursing homes were also at greater risk of burnout. In terms of working conditions during the pandemic, the following burnout risk factors have been identified: working above full‐time schedule over the past weeks, having more than 75% of patients with COVID‐19 in the ward, being exposed to the death of COVID‐19 patients and having more than half of colleagues on sick leave.
4.2. Interpretation of findings
Our results are consistent with a Belgian study on nurses in acute hospitals, which had been performed in 2019 before the outbreak of the COVID‐19 pandemic and which has found that 36% of the sample had a high risk of EE, 32% high risk of DP and 31% a high risk of reduced PA (KCE, 2019b). The higher prevalence of EE and reduced PA in our study can be explained by the outbreak of the pandemic and its consequences on the work environment of nurses. The lower prevalence of DP in our sample may also be explained by the uncommonness of the sanitary situation. Indeed, at the beginning of the pandemic, some nurses may have felt a peak of adrenaline due to the circumstances with a high level of commitment regarding the patients and their work (Permarupan et al., 2020). So far, few studies have assessed the impact of the COVID‐19 pandemic on the risk of burnout among nurses. A systematic review and meta‐analysis using the MBI to measure burnout among nurses found an overall prevalence for EE similar to ours (34.1%), a lower prevalence for DP (12.6%) and reduced PA (15.2%) (Galanis et al., 2020). Belgium's higher figures may be explained by the intensity at which its health care system has been hit. The figures shown in the meta‐analysis were based on the results of studies led in countries, which, compared with Belgium, have been affected less harshly by the pandemic (WHO, 2020a).
The main risk factors of burnout among nurses were the lack of adequate PPE for COVID‐19 and changes in perceived workload. Those factors create a high‐risk environment for nurses to work in. Studies conducted during pre‐COVID times have shown that inadequate staffing and resources had a negative impact on burnout risk among nurses (Nantsupawat et al., 2017; Toh et al., 2012). A systematic review and meta‐analysis have confirmed this trend in COVID times (Galanis et al., 2020). Therefore, strategies for optimizing the supply of PPE and staffing during shortages should be put in place. Sequential plans have to be organised where conventional strategies are implemented before contingency strategies, and contingency strategies are enforced before crisis strategies. Conventional strategies are part of general infection prevention and control plans; contingency strategies are used to anticipate PPE and staffing shortages (e.g., cancelling non‐urgent appointments, decreasing the length of stay for stable patients, adjusting staff schedules, hiring additional nurses and increasing the nurse‐to‐patient ratio for COVID‐19 patients), and crisis strategies are used when supplies are insufficient to meet nurses' needs (Brook et al., 2021; CDC, 2020; Jun et al., 2021).
Regarding the workload, this study highlighted an interesting result: Having an increased or decreased workload during the pandemic were both risk factors for burnout. In the first case, this study also highlighted that nurses working in ICU and in hospital emergency department were more at risk of burnout. The high risk of burnout among those nurses may be explained by increased workloads and by continuous and direct contact with COVID‐19 patients, long shifts, organisational changes in terms of units or teams, lack of adequate PPE or concerns regarding one's safety and the safety of the family (Tiete et al., 2021; Zerbini et al., 2020). In the second case, some nurses were also exposed to a reduced workload because ‘non‐urgent’ medical care was postponed or because patients fearing COVID‐19 infection cancelled their appointments (Danhieux et al., 2020; Frogner & Skillman, 2020). They may have developed a feeling of uselessness regarding their lack of contribution.
The strengths of our study rely upon our large and diversified sample, which counts nurses working outside hospital structures (e.g., home care, nursing homes and ambulatory services). Indeed, literature on the determinants of burnout among nurses more often include samples of hospital nurses (Kim, 2020; Nantsupawat et al., 2016; Ribeiro et al., 2014). Furthermore, we launched the study at an optimal time, which enabled us to capture the determinants of risk of burnout among nurses during the first wave of the COVID‐19 pandemic in Belgium. Another asset of our study is the use of the MBI, which is a validated tool used to assess burnout among health care professionals.
4.3. Limitations
This study presents limitations that should be considered when interpreting the results. We used convenience sampling, which is a method highly vulnerable to selection bias because only individuals who want to take part in the study are included. This potential selection bias can have two consequences on our estimates. On the one hand, nurses who responded to the survey may be the ones who felt psychologically fragile and wanted to share their feelings. On the other hand, the ones who already had burnout or another illness and were on sick leave may not have had access to the questionnaire. Therefore, our overall burnout prevalence may be over‐ or underestimated. Nonetheless, in our multivariate models, we partially consider the effect of several independent variables such as age, gender, seniority and more, which can partially overcome the implications of selection bias.
5. CONCLUSION
This study found a high prevalence of burnout risk among nurses (70%) during the first wave of the COVID‐19 in Belgium. More than one‐third of our sample was at high risk of EE (34.9%) and reduced PA (37.7%), and nearly one‐fourth was at high risk of DP (23.5%). The main risk factors of burnout among nurses were the lack of adequate PPE for COVID‐19 and changes in perceived workload. Regarding the workload, this study highlighted an interesting result: Having an increased or decreased workload during the pandemic were both risk factors for burnout. In the context of a pandemic, a workload decrease (due to cancellation or postponement of ‘non‐urgent’ care) seems to be a risk factor for burnout as important as a workload increase. This highlights the importance of targeting correct risk factors for burnout prevention and treatment interventions to be cost‐effective. Finally, this study found that the main risk factors for burnout among nurses during the first wave of the pandemic were the lack of PPE and the greater perceived workload. This highlights the importance of sequential planning to implement adequate strategies aimed at optimizing PPE supplies and preventing nurse shortages.
6. IMPLICATIONS FOR NURSING MANAGEMENT
A burnout workforce may negatively impact patients and organisational outcomes; therefore, health care system policymakers and managers must provide adequate evidence‐based interventions to support workers' well‐being (Hofmeyer et al., 2020). Several studies encourage nurse managers to focus on organisation and communication (Duncan, 2020; Franck, Goossens, et al., 2021; Franck, Haegdorens, et al., 2021; Nelson & Lee‐Winn, 2020). Individual or group debriefing is an information‐sharing and event‐processing session conducted as a conversation and that is considered good practice after a disaster or after an adverse event (Debra & Romana, 2007). Nurse managers may have to determine whether a worker would benefit from further individual counselling. After a stressful or traumatic event such as the death of COVID‐19 patients, a personal review debrief could be beneficial to nurses within 24 h of the event to reduce compassion fatigue (Schmidt & Haglund, 2017). Debriefing appears as a low‐cost method to improve nurses' well‐being and healing. Nonetheless, training nurse managers to conduct those sessions may be expensive. Therefore, it is essential to target the correct risk factors and to identify nurses who may be at high risk of burnout for those strategies to be cost‐effective.
CONFLICT OF INTEREST
The authors declare that they have no conflict of interest.
ETHICAL APPROVAL
The Belgian Law does not require an approval from an Ethical Board for an online survey with the general population.
ACKNOWLEDGEMENT
The authors would like to gratefully acknowledge the nurses that took part in the study.
Khan, Y. , Bruyneel, A. , & Smith, P. (2022). Determinants of the risk of burnout among nurses during the first wave of the COVID‐19 pandemic in Belgium: A cross‐sectional study. Journal of Nursing Management, 30(5), 1125–1135. 10.1111/jonm.13624
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
REFERENCES
- American Thoracic Society . (2016). What is Burnout Syndrome (BOS)? https://www.thoracic.org/patients/patient-resources/resources/burnout-syndrome.pdf
- Awa, W. L. , Plaumann, M. , & Walter, U. (2010). Burnout prevention: A review of intervention programs. Patient Education and Counseling, 78(2), 184–190. 10.1016/j.pec.2009.04.008 [DOI] [PubMed] [Google Scholar]
- Brook, J. , Aitken, L. M. , MacLaren, J.‐A. , & Salmon, D. (2021). An intervention to decrease burnout and increase retention of early career nurses: A mixed methods study of acceptability and feasibility. BMC Nursing, 20(1), 19. 10.1186/s12912-020-00524-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruyneel, A. , Lucchini, A. , & Hoogendoorn, M. (2021). Impact of COVID‐19 on nursing workload as measured with the Nursing Activities Score in intensive care: Summary of findings. Intensive & Critical Care Nursing, 69, 103170. 10.1016/j.iccn.2021.103170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cañadas‐de la Fuente, G. A. , Vargas, C. , San Luis, C. , García, I. , Cañadas, G. R. , & de la Fuente, E. I. (2015). Risk factors and prevalence of burnout syndrome in the nursing profession. International Journal of Nursing Studies, 52(1), 240–249. 10.1016/j.ijnurstu.2014.07.001 [DOI] [PubMed] [Google Scholar]
- CDC . (2012). Principles of Epidemiology in Public Health Practice: An Introduction to Applied Epidemiology and Biostatistics (Third Edition). https://www.cdc.gov/csels/dsepd/ss1978/lesson1/section7.html
- CDC . (2020). Healthcare Workers. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/hcp/ppe-strategy/strategies-optimize-ppe-shortages.html [Google Scholar]
- Cheung, T. , Fong, T. K. H. , & Bressington, D. (2020). COVID‐19 under the SARS Cloud: Mental Health Nursing during the Pandemic in Hong Kong. Journal of Psychiatric and Mental Health Nursing, 12639. 10.1111/jpm.12639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danhieux, K. , Buffel, V. , Pairon, A. , Benkheil, A. , Remmen, R. , Wouters, E. , & van Olmen, J. (2020). The impact of COVID‐19 on chronic care according to providers: A qualitative study among primary care practices in Belgium. BMC Family Practice, 21(1), 255. 10.1186/s12875-020-01326-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Debra, H. , & Romana, M. (2007). Debriefing after a crisis. //www.nursingcenter.com/journalarticle?? Article_ID=735650&Journal_ID=54013&Issue_ID=735629
- Duncan, D. (2020). What the COVID‐19 pandemic tells us about the need to develop resilience in the nursing workforce. Nursing Management, 27. 10.7748/nm.2020.e1933 [DOI] [PubMed] [Google Scholar]
- Emanuel, E. J. , Persad, G. , Upshur, R. , Thome, B. , Parker, M. , Glickman, A. , Zhang, C. , Boyle, C. , Smith, M. , & Phillips, J. P. (2020). Fair allocation of scarce medical resources in the time of COVID‐19. New England Journal of Medicine, 382(21), 2049–2055. 10.1056/NEJMsb2005114 [DOI] [PubMed] [Google Scholar]
- Etalab ‐ Ministère des Solidarités et de la Santé et Santé Publique France . (2020). Tableau de bord COVID‐19. https://dashboard.covid19.data.gouv.fr/vue-d-ensemble?location=FRA
- Faes, C. , Hens, N. , & Gilbert, M. (2021). On the timing of interventions to preserve hospital capacity: Lessons to be learned from the Belgian SARS‐CoV‐2 pandemic in 2020. Archives of Public Health, 79(1), 164. 10.1186/s13690-021-00685-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franck, E. , Goossens, E. , Haegdorens, F. , Geuens, N. , Portzky, M. , Tytens, T. , Dilles, T. , Beeckman, K. , Timmermans, O. , Slootmans, S. , van Rompaey, B. , & van Bogaert, P. (2021). Role of resilience in healthcare workers' distress and somatization during the COVID‐19 pandemic: A cross‐sectional study across Flanders, Belgium. Nursing Open. 10.1002/nop2.1159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franck, E. , Haegdorens, F. , Goossens, E. , van Gils, Y. , Portzky, M. , Somville, F. , Abuawad, M. , Slootmans, S. , & van Bogaert, P. (2021). The role of coping behavior in healthcare workers' distress and somatization during the COVID‐19 pandemic. Frontiers in Psychology, 12, 2654. 10.3389/fpsyg.2021.684618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frogner, B. K. , & Skillman, S. M. (2020). The challenge in tracking unemployment among health care workers and why it matters. JAMA Health Forum, 1(11), e201358. 10.1001/jamahealthforum.2020.1358 [DOI] [PubMed] [Google Scholar]
- Galanis, P. , Vraka, I. , Fragkou, D. , Bilali, A. , & Kaitelidou, D. (2020). Nurses’ burnout and associated risk factors during the COVID‐19 pandemic: A systematic review and meta‐analysis. MedRxiv. 10.1101/2020.11.24.20237750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerkens, S. , & Merkur, S. (2010). Belgium: Health system review. Health Systems in Transition, 12(5), 1–266. https://www.ncbi.nlm.nih.gov/pubmed/21224177 [PubMed] [Google Scholar]
- Guixia, L. , & Hui, Z. (2020). A study on burnout of nurses in the period of COVID‐19. Psychology and Behavioral Sciences, 9(3), 31. 10.11648/j.pbs.20200903.12 [DOI] [Google Scholar]
- Hardy, O. J. , Dubourg, D. , Bourguignon, M. , Dellicour, S. , Eggerickx, T. , Gilbert, M. , Sanderson, J.‐P. , Scohy, A. , Vandael, E. , & Decroly, J.‐M. (2021). A world apart: Levels and determinants of excess mortality due to COVID‐19 in care homes: The case of the Belgian region of Wallonia during the spring 2020 wave. Demographic Research, 45(33), 1011–1040. 10.4054/DemRes.2021.45.33 [DOI] [Google Scholar]
- Hofmeyer, A. , Taylor, R. , & Kennedy, K. (2020). Fostering compassion and reducing burnout: How can health system leaders respond in the COVID‐19 pandemic and beyond? Nurse Education Today, 94, 104502. 10.1016/j.nedt.2020.104502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu, D. , Kong, Y. , Li, W. , Han, Q. , Zhang, X. , Zhu, L. X. , Wan, S. W. , Liu, Z. , Shen, Q. , Yang, J. , He, H.‐G. , & Zhu, J. (2020). Frontline nurses' burnout, anxiety, depression, and fear statuses and their associated factors during the COVID‐19 outbreak in Wuhan, China: A large‐scale cross‐sectional study. EClinicalMedicine, 24, 100424. 10.1016/j.eclinm.2020.100424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jun, J. , Ojemeni, M. M. , Kalamani, R. , Tong, J. , & Crecelius, M. L. (2021). Relationship between nurse burnout, patient and organizational outcomes: Systematic review. International Journal of Nursing Studies, 119, 103933. 10.1016/j.ijnurstu.2021.103933 [DOI] [PubMed] [Google Scholar]
- KCE . (2019a). Performance of the Belgian health system—Practising nurses on the health sector per 1000 inhabitants. https://www.healthybelgium.be/metadata/hspa/a6.pdf
- KCE . (2019b). Safe nurse staffing levels in acute hospitals. https://kce.fgov.be/en/safe-nurse-staffing-levels-in-acute-hospitals
- Kim, J.‐S. (2020). Emotional labor strategies, stress, and burnout among hospital nurses: A path analysis. Journal of Nursing Scholarship, 52(1), 105–112. 10.1111/jnu.12532 [DOI] [PubMed] [Google Scholar]
- Maslach, C. , Jackson, S. , Leiter, M. , Schaufeli, W. , & Schwab, R. (1986). Maslach Burnout Inventory manual, general survey, human services survey, educators survey ad scoring guides (Mind Garden).
- Miranda, F. M. D. , Santana, L. D. L. , Pizzolato, A. C. , & Sarquis, L. M. M. (2020). Condições de trabalho e o impacto na saúde dos profissionais de enfermagem frente a COVID‐19. Cogitare Enfermagem, 25. 10.5380/ce.v25i0.72702 [DOI] [Google Scholar]
- Molina‐Praena, J. , Ramirez‐Baena, L. , Gómez‐Urquiza, J. , Cañadas, G. , de la Fuente, E. , & Cañadas‐de la Fuente, G. (2018). Levels of burnout and risk factors in medical area nurses: A meta‐analytic study. International Journal of Environmental Research and Public Health, 15(12), 2800. 10.3390/ijerph15122800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nantsupawat, A. , Kunaviktikul, W. , Nantsupawat, R. , Wichaikhum, O.‐A. , Thienthong, H. , & Poghosyan, L. (2017). Effects of nurse work environment on job dissatisfaction, burnout, intention to leave. International Nursing Review, 64(1), 91–98. 10.1111/inr.12342 [DOI] [PubMed] [Google Scholar]
- Nantsupawat, A. , Nantsupawat, R. , Kunaviktikul, W. , Turale, S. , & Poghosyan, L. (2016). Nurse burnout, nurse‐reported quality of care, and patient outcomes in thai hospitals. Journal of Nursing Scholarship, 48(1), 83–90. 10.1111/jnu.12187 [DOI] [PubMed] [Google Scholar]
- Nelson, S. M. , & Lee‐Winn, A. E. (2020). The mental turmoil of hospital nurses in the COVID‐19 pandemic. Psychological Trauma Theory Research Practice and Policy, 12(S1, S126–S127. 10.1037/tra0000810 [DOI] [PubMed] [Google Scholar]
- Patel, R. S. , Bachu, R. , Adikey, A. , Malik, M. , & Shah, M. (2018). Factors related to physician burnout and its consequences: A review. Behavioral Science, 8(11). 10.3390/bs8110098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pecoraro, F. , Clemente, F. , & Luzi, D. (2020). The efficiency in the ordinary hospital bed management in Italy: An in‐depth analysis of intensive care unit in the areas affected by COVID‐19 before the outbreak. PLoS ONE, 15(9). 10.1371/journal.pone.0239249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pérez‐Fuentes, M. , Molero Jurado, M. , Martos Martínez, Á. , & Gázquez Linares, J. (2018). New burnout evaluation model based on the brief burnout questionnaire: Psychometric properties for nursing. International Journal of Environmental Research and Public Health, 12. 10.3390/ijerph15122718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Permarupan, P. Y. , Al Mamun, A. , Hayat, N. , Saufi, R. A. , & Samy, N. K. (2020). Nursing management challenges: Effect of quality of work life on depersonalization. International Journal of Healthcare Management, 1–10. 10.1080/20479700.2020.1728924 [DOI] [Google Scholar]
- Ribeiro, V. F. , Filho, C. , Valenti, V. E. , Ferreira, M. , de Abreu, L. , de Carvalho, T. , Xavier, V. , de Oliveira Filho, J. , Gregory, P. , Leão, E. , Francisco, N. G. , & Ferreira, C. (2014). Prevalence of burnout syndrome in clinical nurses at a hospital of excellence. International Archives of Medicine, 7(1), 22. 10.1186/1755-7682-7-22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotenstein, L. S. , Torre, M. , Ramos, M. A. , Rosales, R. C. , Guille, C. , Sen, S. , & Mata, D. A. (2018). Prevalence of burnout among physicians: A systematic review. JAMA, 320(11), 1131. 10.1001/jama.2018.12777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt, M. , & Haglund, K. (2017). Debrief in emergency departments to improve compassion fatigue and promote resiliency. Journal of Trauma Nursing, 24(5), 317–322. 10.1097/JTN.0000000000000315 [DOI] [PubMed] [Google Scholar]
- Sciensano . (2020). Belgium COVID‐19 Epidemiological Situation—Summary. https://datastudio.google.com/embed/reporting/c14a5cfc-cab7-4812-848c-0369173148ab/page/ZwmOB (April 10, 2021).
- Taccone, F. S. , van Goethem, N. , De Pauw, R. , Wittebole, X. , Blot, K. , van Oyen, H. , Lernout, T. , Montourcy, M. , Meyfroidt, G. , & van Beckhoven, D. (2021). The role of organizational characteristics on the outcome of COVID‐19 patients admitted to the ICU in Belgium. The Lancet Regional Health ‐ Europe, 2, 100019. 10.1016/j.lanepe.2020.100019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiete, J. , Lachaux, A. , Matossian, A. , Hougardy, J.‐M. , Loas, G. , & Rotsaert, M. (2021). Mental health outcomes in healthcare workers in COVID‐19 and non‐COVID‐19 care units: A cross‐sectional survey in Belgium. Frontiers in Psychology, 11. 10.3389/fpsyg.2020.612241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toh, S. G. , Ang, E. , & Devi, M. K. (2012). Systematic review on the relationship between the nursing shortage and job satisfaction, stress and burnout levels among nurses in oncology/haematology settings. International Journal of Evidence‐Based Healthcare, 10(2), 126–141. 10.1111/j.1744-1609.2012.00271.x [DOI] [PubMed] [Google Scholar]
- Trockel, M. , Bohman, B. , Lesure, E. , Hamidi, M. S. , Welle, D. , Roberts, L. , & Shanafelt, T. (2018). A brief instrument to assess both burnout and professional fulfillment in physicians: Reliability and validity, including correlation with self‐reported medical errors, in a sample of resident and practicing physicians. Academic Psychiatry, 42(1), 11–24. 10.1007/s40596-017-0849-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . (2019). Burn‐out an “occupational phenomenon”: International Classification of Diseases. https://www.who.int/news/item/28-05-2019-burn-out-an-occupational-phenomenon-international-classification-of-diseases
- WHO . (2020a). Coronavirus Disease (COVID‐19) Situation Reports. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports
- WHO . (2020b). Coronavirus Disease (COVID‐19)—Events as they happen. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen
- WHO European Health Information at Your Fingertips . (2020). Total number of hospital beds. https://gateway.euro.who.int/en/indicators/hfa_477-5051-total-number-of-hospital-beds/
- Woo, T. , Ho, R. , Tang, A. , & Tam, W. (2020). Global prevalence of burnout symptoms among nurses: A systematic review and meta‐analysis. Journal of Psychiatric Research, 123, 9–20. 10.1016/j.jpsychires.2019.12.015 [DOI] [PubMed] [Google Scholar]
- Zerbini, G. , Ebigbo, A. , Reicherts, P. , Kunz, M. , & Messman, H. (2020). Psychosocial burden of healthcare professionals in times of COVID‐19—A survey conducted at the University Hospital Augsburg. German Medical Science: GMS e‐Journal, 18, Doc05. 10.3205/000281 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, upon reasonable request.


