Abstract
Background/Objectives
The COVID‐19 pandemic necessitated rapid implementation of telemedicine at medical centers across the United States. As telemedicine is expected to persist beyond the pandemic in subspecialties like pediatric dermatology, there is growing concern that socioeconomic factors may contribute to inequitable telemedicine access. This study aims to identify factors associated with disparities in telemedicine use among pediatric dermatology patients during the pandemic.
Methods
In this single‐center cross‐sectional study, patients less than 18 years old who completed a visit with a pediatric dermatologist via a video telemedicine call or in‐person office visit during the specified time periods were included. Univariate and multivariable analyses were performed to compare demographic factors for (1) patients who had a telemedicine visit versus office visit during June 1, 2020, to January 22, 2021, and (2) patients who had either visit type during June 1, 2020, to January 22, 2021, versus June 1, 2019, to January 2020.
Results
The independent factors associated with lower odds of telemedicine include identifying as Black/African American, having a non‐English preferred language, and having public insurance, whereas the independent factors reducing overall access to pediatric dermatology care during the pandemic include identifying as Hispanic/Latino and having public insurance.
Conclusions
Differential telemedicine use in vulnerable communities may be attributed to disparities in technology access and digital literacy and should be addressed at a structural level. If such disparities are identified and adequately remedied, telemedicine can serve as an important tool for expanding access in the field of pediatric dermatology.
Keywords: COVID‐19, cross‐sectional studies, disparities, health care delivery, telemedicine
1. INTRODUCTION
The COVID‐19 pandemic catalyzed the rapid implementation of telemedicine in many specialties and medical centers across the United States. Virtual modalities have the potential to make health care more accessible by reducing barriers such as transportation, childcare, and time off work. 1 , 2 However, there is growing concern that telemedicine may contribute to health disparities, evidenced by studies in multiple specialties showing that virtual visits were more likely to be utilized by patients who were White, English speaking, and commercially insured. 3 , 4 , 5 , 6
Dialog on this particular issue in dermatology and specifically pediatric dermatology has been scarce. The only other report in pediatric dermatology showed that Spanish‐speaking patients were significantly less likely to schedule telemedicine visits, which the authors attributed to those patients having lower rates of email connectedness and online patient portal access. 7 Given that telemedicine in pediatric dermatology will likely persist as a health care delivery modality beyond the pandemic, it is important to investigate socioeconomic factors contributing to inequitable access in this patient population. In this study, we identified factors associated with disparities in telemedicine use among pediatric dermatology patients, in addition to disparities to accessing care overall during the COVID‐19 pandemic at an urban outpatient clinic.
2. METHODS
2.1. Data source
This cross‐sectional study was approved by the institutional review board. De‐identified data of patients who had dermatology encounters at the University of Chicago between June 1, 2019, and January 22, 2021, were obtained from the Clinical Research Data Warehouse (CRDW) of the Center for Research Informatics (CRI). The analysis included clinical encounters with a fellowship‐trained pediatric dermatologist by a patient less than 18 years old that were completed via a video or in‐person visit.
2.2. Institutional telemedicine practices
Prior to the COVID‐19 pandemic, the study institution did not offer telemedicine due to a lack of infrastructure and reimbursement guidelines. At onset of the pandemic, the institution rapidly implemented a telemedicine platform and U.S. health insurance plans expanded coverage to reimburse for telemedicine at rates comparable to in‐person services.
During the study period, protocols for telemedicine were analogous to in‐person visits at our institution. Both visit types employed the same personnel, medical interpretation services, and post‐visit workflow (e.g., e‐prescriptions, after‐visit summaries, and follow‐up scheduling). No physician approval was required for patients to make a virtual appointment, and all visits were billed to insurance. For telemedicine, patients were asked to submit high‐resolution photographs of their problem via the patient portal but were permitted to use any video‐enabled device (e.g., computer, tablet, and phone) for the virtual encounter.
2.3. Variables of interest
The primary variables of interest were patient race, ethnicity, preferred language, and payor type. Other variables (e.g., patient type, gender, age, and ZIP (postal) code of residence) were included in the analyses to reduce possible confounding.
2.4. Payor type
In the United States, “private” health insurance refers to employer‐based and individually sponsored plans, whereas “public” health insurance refers to government‐run programs like Medicaid for which there is an income eligibility limit. In Illinois, children qualify for Medicaid if their family income level is up to 147% of the federal poverty level (e.g., maximum income for an eligible family of four with two children is $36,570). 8 Payor type was used as a proxy for income, as >99% of patients having public insurance included in this study were insured by Medicaid.
2.5. ZIP code
ZIP (postal) code of residence was used to approximate the geographic distance of patients from the clinic. Patients were grouped by proximity to the clinic: (1) within Chicago, (2) within Cook County outside of Chicago, and (3) outside of Cook County. The City of Chicago is approximately 228 mi2 and is situated in Cook County, Illinois, which spans approximately 1635 mi2.
2.6. Statistical analysis
Univariate logistic regressions were performed to compare characteristics of patients seen via telemedicine versus office visits during the 8‐month “pandemic period” (June 1, 2020, to January 22, 2021) (Figure 1). Reference groups were chosen based on previous literature on disparities in telemedicine. 4 , 9 , 10 Variables with p values <.05 were included in a multivariable logistic regression analysis to determine adjusted odds ratios. The same methods were used to compare the characteristics of patients accessing pediatric dermatology care overall, combining patient encounters conducted via telemedicine and office visits, during the pandemic period (June 1, 2020, to January 22, 2021) versus the same 8‐month “pre‐pandemic period” the prior year (June 1, 2019, to January 22, 2020). Patients who had Chicago ZIP (postal) codes were included in a subgroup analysis of median household income (determined at the zip code level), 11 , 12 patient portal activation status, and email record status. All analyses were performed using Stata 16/MP 16.1.
FIGURE 1.
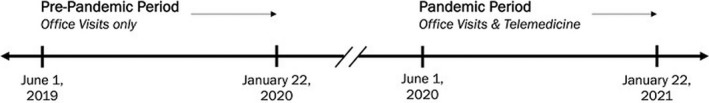
Study timeline
3. RESULTS
3.1. Telemedicine versus office visits
Between June 1, 2020, and January 22, 2021, 1237 in‐person office visits and 207 video telemedicine visits were completed in pediatric dermatology (Table 1). The demographic characteristics of new and return patients who accessed telemedicine were similar. A univariate analysis found that new patients were significantly less likely to have had a telemedicine visit than return patients (odds ratio [OR], 0.17; p < .0005). There was no difference in telemedicine use based on gender identity or age group. Black/African American patients were four times less likely to have used telemedicine compared with White patients (p < .0005). No association was found between telemedicine use and Hispanic/Latino ethnicity. Patients who had a non‐English preferred language were about four times less likely to have used telemedicine than patients who preferred English (p = .015). Patients with public insurance were three times less likely to utilize telemedicine compared to those with private insurance (p < .0005). Compared with Chicago residents, patients living in the broader Cook County outside of Chicago were 2.77 times as likely to utilize telemedicine over office visits (p < .0005), while residents outside of Cook County were 4.50 times as likely (p < .0005).
TABLE 1.
Characteristics and univariate analysis of pediatric dermatology encounters of patients seen via office visits versus telemedicine during the pandemic period (June 1, 2020, and January 22, 2021)
| Characteristic a | Office Visit b | Telemedicine b | OR | 95% CI for OR | p Value | |
|---|---|---|---|---|---|---|
| n = 1237 | n = 207 | Lower | Upper | |||
| Patient Type, n (%) | ||||||
| Return patient | 651 (52.6) | 179 (86.5) | Reference | |||
| New patient | 586 (47.4) | 28 (14) | 0.17 | 0.11 | 0.26 | <.0005*** |
| Gender, n (%) | ||||||
| Female | 704 (56.9) | 124 (59.9) | Reference | |||
| Male | 533 (43.1) | 83 (40) | 0.88 | 0.66 | 1.19 | .421 |
| Age, n (%) | ||||||
| 0–10 years | 623 (50.4) | 99 (47.8) | Reference | |||
| 11–17 years | 614 (49.6) | 108 (52.2) | 1.11 | 0.82 | 1.49 | .499 |
| Race, n (%) | ||||||
| White | 351 (28.4) | 109 (52.7) | Reference | |||
| Black/African American | 617 (49.9) | 47 (23) | 0.25 | 0.17 | 0.35 | <.0005*** |
| Asian/Mideast Indian | 52 (4) | 14 (7) | 0.87 | 0.46 | 1.62 | .656 |
| Other race/mixed/unknown | 217 (17.5) | 37 (18) | 0.55 | 0.36 | 0.83 | .004** |
| Ethnicity, n (%) | ||||||
| Non‐Hispanic/Latino | 969 (78.3) | 168 (81.2) | Reference | |||
| Hispanic/Latino | 171 (13.8) | 20 (10) | 0.67 | 0.41 | 1.10 | .116 |
| Unknown | 97 (8) | 19 (9) | 1.13 | 0.67 | 1.90 | .644 |
| Preferred Language, n (%) | ||||||
| English | 1,164 (94.1) | 204 (98.6) | Reference | |||
| Non‐English | 73 (6) | 3 (1) | 0.23 | 0.07 | 0.75 | .015* |
| Payor Type, n (%) | ||||||
| Private insurance | 671 (54.2) | 164 (79.2) | Reference | |||
| Public insurance | 535 (43.2) | 41 (20) | 0.31 | 0.22 | 0.45 | <.0005*** |
| Self‐pay/unknown | 31 (3) | 2 (1) | 0.26 | 0.06 | 1.11 | .070 |
| Zip Code, c n (%) | ||||||
| Chicago, IL (606###) | 884 (71.5) | 87 (42) | Reference | |||
| Cook County, IL (non−606###) | 213 (17.2) | 58 (28) | 2.77 | 1.92 | 3.98 | <.0005*** |
| Other Zip Code | 140 (11.3) | 62 (30) | 4.50 | 3.10 | 6.52 | <.0005*** |
p Value: <.05*, <.01**, <.001***.
Abbreviation: OR, odds ratio; CI, confidence interval; IL, Illinois.
Data provided by Clinical Research Data Warehouse at the University of Chicago and includes patient self‐reported classifications from electronic medical records.
Only successfully completed visits during the pandemic period (June 1, 2020, to January 22, 2021) are included. All office visits occurred in‐person, and all telemedicine visits occurred over synchronous video call.
Zip codes beginning with prefix 606‐ are of the City of Chicago in Cook County, IL.
A multivariable analysis (Table 2) showed that the independent factors reducing the odds of using telemedicine visits over office visits include being a new patient (aOR, 0.18; p < .0005), identifying as Black/African American (aOR, 0.40; p < .0005), having a non‐English preferred language (aOR, 0.28; 95% CI, 0.08–0.95; p = .041), and having public insurance (aOR, 0.51; p = .002). The factors that increased the odds of having telemedicine over office visits were living outside of Chicago in the broader Cook County (aOR, 2.67; p < .0005) and beyond Cook County (aOR, 2.81; p < .0005).
TABLE 2.
Multivariable analysis of pediatric dermatology encounters characteristics completed by office visits versus telemedicine during the pandemic period (June 1, 2020, to January 22, 2021)
| Adjusted OR | 95% CI for aOR | Coefficient (β) | Standard Error (SE) | p Value | ||
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Patient type | ||||||
| Return patient | Reference | |||||
| New patient | 0.18 | 0.12 | 0.27 | −1.72 | 0.22 | <.0005*** |
| Race a | ||||||
| White | Reference | |||||
| Black/African American | 0.40 | 0.26 | 0.61 | −0.92 | 0.21 | <.0005*** |
| Asian/Mideast Indian | 0.96 | 0.48 | 1.89 | −0.05 | 0.35 | .897 |
| Other race/mixed/unknown | 0.76 | 0.49 | 1.19 | −0.27 | 0.23 | .235 |
| Preferred Language a | ||||||
| English | Reference | |||||
| Non‐English | 0.28 | 0.08 | 0.95 | −1.26 | 0.62 | .041* |
| Payor type | ||||||
| Private insurance | Reference | |||||
| Public insurance | 0.51 | 0.34 | 0.78 | −0.67 | 0.22 | .002** |
| Self‐pay/unknown | 0.27 | 0.06 | 1.21 | −1.30 | 0.76 | .088 |
| Zip code a | ||||||
| Chicago, IL (606###)b | Reference | |||||
| Cook County, IL (non−606###) | 2.67 | 1.80 | 3.98 | 0.98 | 0.20 | <.0005*** |
| Non‐Cook County | 2.81 | 1.87 | 4.23 | 1.03 | 0.21 | <.0005*** |
p Value: <.05*, <.01**, <.001***.
Abbreviation: OR, odds ratio; CI, confidence interval; aOR, adjusted odds ratio; IL, Illinois.
Self‐reported by patient at the time of the encounter.
Zip codes beginning with prefix 606‐ are of the City of Chicago in Cook County, IL.
3.2. Pandemic period versus pre‐pandemic period
A univariate analysis (Table 3) of pediatric dermatology visits during the pre‐pandemic period (n = 1631) compared with pandemic period (n = 1444) showed no difference between groups based on gender identity, age group, or zip code. There were more new patient visits prior to the pandemic to the pandemic period (OR, 0.80; p < .002). Race was not associated with significantly different odds of accessing care during the pandemic. Hispanic/Latino ethnicity (OR, 0.73; p = .002) and non‐English preferred language (OR, 0.71; p = .022) were both associated with decreased odds of having a visit during the pandemic. Finally, patients with public insurance (OR, 0.79; p = .001) and self‐pay or unknown payment method (OR, 0.63; p = .040) were negatively associated with accessing care during the pandemic period.
TABLE 3.
Characteristics and univariate analysis of pediatric dermatology encounters combining telemedicine and office visits during the pre‐pandemic period (June 1, 2019, to January 22, 2020) versus the pandemic period (June 1, 2020, to January 22, 2021)
| Characteristic a | Pre‐Pandemic b | Pandemic b | Unadjusted OR | 95% CI for OR | p Value | |
|---|---|---|---|---|---|---|
| n = 1631 | n = 1444 | Lower | Upper | |||
| Patient type, n (%) | ||||||
| Return patient | 847 (51.9) | 830 (57.5) | Reference | |||
| New patient | 784 (48.1) | 614 (42.5) | 0.80 | 0.69 | 0.92 | .002** |
| Gender, n (%) | ||||||
| Female | 897 (55.0) | 828 (57.3) | Reference | |||
| Male | 734 (45.0) | 616 (42.7) | 0.91 | 0.79 | 1.05 | .191 |
| Age, n (%) | ||||||
| 0–10 years | 870 (53.3) | 722 (50.0) | Reference | |||
| 11–17 years | 761 (46.7) | 722 (50.0) | 1.14 | 0.99 | 1.32 | .064 |
| Race, n (%) | ||||||
| White | 567 (34.8) | 460 (31.9) | Reference | |||
| Black/African American | 790 (48.4) | 664 (46.0) | 1.04 | 0.88 | 1.21 | .666 |
| Asian/Mideast Indian | 77 (5) | 66 (5) | 1.06 | 0.74 | 1.50 | .759 |
| Other race/mixed/unknown | 197 (12.1) | 254 (17.6) | 1.59 | 1.27 | 1.99 | <.0005*** |
| Ethnicity, n (%) | ||||||
| Non‐Hispanic or Latino | 1,295 (79.4) | 1,137 (78.7) | Reference | |||
| Hispanic or Latino | 297 (18.2) | 191 (13.2) | 0.73 | 0.60 | 0.89 | .002** |
| Unknown | 39 (2) | 116 (8.0) | 3.39 | 2.34 | 4.91 | <.0005*** |
| Preferred Language, n (%) | ||||||
| English | 1,512 (92.7) | 1,368 (94.7) | Reference | |||
| Non‐English | 119 (7.3) | 76 (5) | 0.71 | 0.52 | 0.95 | .022* |
| Payer Type, n (%) | ||||||
| Private insurance | 842 (51.6) | 835 (57.8) | Reference | |||
| Public insurance | 736 (45.1) | 576 (39.9) | 0.79 | 0.68 | 0.91 | .001** |
| Self‐pay/unknown | 53 (3) | 33 (2) | 0.63 | 0.40 | 0.98 | .040* |
| Zip Code, c n (%) | ||||||
| Chicago, IL (606###) | 1,080 (66.2) | 971 (67.2) | Reference | |||
| Cook County, IL (non−606###) | 309 (18.9) | 271 (18.8) | 0.98 | 0.81 | 1.17 | .792 |
| Other Zip Code | 242 (14.8) | 202 (14.0) | 0.93 | 0.76 | 1.14 | .480 |
p Value: <.05*, <.01**, <.001***.
Abbreviation: OR, odds ratio; CI, confidence interval; IL, Illinois.
Data provided by Clinical Research Data Warehouse at the University of Chicago and includes patient self‐reported classifications from electronic medical records.
The 8‐month time periods are defined as pre‐pandemic period (June 1, 2019, to January 22, 2020) and pandemic period (June 1, 2020, to January 22, 2021). Only successfully completed visits are included.
Zip codes beginning with prefix 606‐ are of the City of Chicago in Cook County, IL.
Multivariable analysis (Table 4) found that the independent factors predicting decreased access to pediatric dermatology care during the pandemic period were being a new patient (aOR, 0.78; p = .001), identifying as Hispanic/Latino (aOR, 0.64; p = .002), and having public insurance (aOR, 0.82; p = .028). The factors that increased the odds of having a pandemic visit were identifying as an unspecified race (aOR, 1.53; p = .003) or unknown ethnicity (aOR, 2.43; p < .0005). After adjustment, non‐English language preference was no longer statistically significant.
TABLE 4.
Multivariable analysis of pediatric dermatology encounters characteristics during the pre‐pandemic period (June 1, 2019, to January 22, 2020) versus the pandemic period (June 1, 2020, to January 22, 2021)
| Adjusted OR | 95% CI for aOR | Coefficient (β) | Standard Error (SE) | p Value | ||
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Patient type | ||||||
| Return patient | Reference | |||||
| New patient | 0.78 | 0.67 | 0.90 | −0.25 | 0.07 | .001** |
| Race a | ||||||
| White | Reference | |||||
| Black/African American | 1.03 | 0.85 | 1.25 | 0.03 | 0.10 | .729 |
| Asian/Mideast Indian | 0.95 | 0.66 | 1.35 | −0.05 | 0.18 | .782 |
| Other race/mixed/unknown | 1.53 | 1.15 | 2.03 | 0.42 | 0.15 | .003** |
| Ethnicity a | ||||||
| Non‐Hispanic or Latino | Reference | |||||
| Hispanic or Latino | 0.64 | 0.49 | 0.84 | −0.44 | 0.14 | .002** |
| Unknown | 2.43 | 1.55 | 3.80 | 0.89 | 0.23 | <.0005*** |
| Preferred Language a | ||||||
| English | Reference | |||||
| Non‐English | 0.96 | 0.68 | 1.36 | −0.04 | 0.18 | 0.823 |
| Payer type | ||||||
| Private insurance | Reference | |||||
| Public insurance | 0.82 | 0.69 | 0.98 | −0.19 | 0.09 | .028* |
| Self‐pay/unknown | 0.68 | 0.44 | 1.07 | −0.38 | 0.23 | .098 |
p Value: <.05*, <.01**, <.001***.
Abbreviation: OR, odds ratio; CI, confidence interval; aOR, adjusted odds ratio; IL, Illinois.
Self‐reported by patient at the time of the encounter.
3.3. Subgroup analysis
A univariate subgroup analysis of Chicago residents (Table 5) found that Black/African American patients were significantly more likely to reside in ZIP (postal) codes with median household incomes below Chicago's city‐wide median (OR, 3.70; p < .0005), less likely to have an activated patient portal (OR, 0.28; p < .0005), and less likely to have a recorded email address (OR, 0.48; p = .012) relative to White patients.
TABLE 5.
Univariate analysis of household income, patient portal status, and email record status among Black/African American pediatric dermatology patients residing in Chicago, IL, during an 8‐month period of the COVID‐19 pandemic
| Variable | OR | 95% CI for OR | p value | |||
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Median household income a | ||||||
| >City Median | <City Median | |||||
| White, n (%) | 55 (29) | 134 (70.9) | Reference | |||
| Black/African American, n (%) | 40 (10) | 361 (90.0) | 3.70 | 2.35 | 5.83 | <.0005*** |
| Patient portal status | ||||||
|---|---|---|---|---|---|---|
| Not activated | Activated | |||||
| White, n (%) | 43 (23) | 146 (77.2) | Reference | |||
| Black/African American, n (%) | 204 (50.9) | 197 (49.1) | 0.28 | 0.19 | 0.42 | <.0005*** |
| Email address on record | ||||||
|---|---|---|---|---|---|---|
| No | Yes | |||||
| White, n (%) | 16 (9) | 173 (91.5) | Reference | |||
| Black/African American, n (%) | 65 (16) | 336 (83.8) | 0.48 | 0.27 | 0.85 | .012* |
p Value: <.05*, <.01**, <.001***.
Abbreviation: OR, odds ratio; CI, confidence interval.
Determined at the zip code level according to 2015–2019 data from the Chicago Health Atlas. Median household income of the City of Chicago was $58,247 in 2015–2019 according to United States Census Bureau.
4. DISCUSSION
Our work reveals the existence of disparities in telemedicine access during the COVID‐19 pandemic among pediatric dermatology patients at our medical center. Specifically, we found that the independent factors associated with lower rates of telemedicine use include identifying as Black/African American, having a non‐English preferred language, and having public insurance. These findings corroborate studies in other medical fields, demonstrating the prevalence of inequitable telemedicine access across specialties and patient populations. 3 , 4 , 5 , 6
Disparities in telemedicine use among patients of color could be attributed to the intersection of individual and systemic factors. Particularly, structural racism may contribute to lower technology access and digital literacy in Black communities. 13 , 14 We found that, although the odds of Black/African American patients seeking care during the pandemic was similar to pre‐pandemic, the odds of using telemedicine was significantly less relative to White patients. This suggests that barriers to telemedicine access disproportionately affected Black patients seeking care during the pandemic, leading to a greater reliance on in‐person visits than other groups. We hypothesize that technology‐associated disparities including access to video‐enabled devices and digital literacy may drive lower telemedicine use, 15 supported by our results that Black patients were significantly less likely to have an activated patient portal and email addresses on record relative to White patients. Finally, possible mistrust of the health care system and technology in Black communities may contribute to lower rates of telemedicine use 3 , 14 and may influence patients of color to prefer in‐person medical visits, especially if meeting with a new provider.
Next, we found that patients who were Hispanic/Latino and non‐English speaking were disproportionately affected by the COVID‐19 pandemic. While having a non‐English preferred language factors into likelihood of telemedicine use, identifying as Hispanic/Latino played a larger role in accessing care during the pandemic overall regardless of visit type, even after adjusting for covariates. We hypothesize that factors other than language barriers influenced the ability of Hispanic/Latino patients to seek care during the pandemic, while language barriers specifically made telemedicine challenging for this group despite the availability of medical interpretation during virtual visits. 7
Finally, patients with public insurance had significantly lower odds of using telemedicine despite widely expanded coverage for telehealth services by U.S. health insurance plans. 16 Thus, we propose that public insurance as a proxy for income rather than insurance type alone predicts decreased telemedicine use. Telemedicine disparities among low‐income households are likely attributable to gaps in access to the technology and internet connectivity necessary to complete virtual visits.
This study has several limitations. First, the cross‐sectional design allows only for broad analysis of the defined time periods and does not show how changes may have gradually occurred. The retrospective data availability made some results difficult to interpret, such as how patients of unspecified race and ethnicity appear to have significantly higher odds of accessing care during the pandemic. One explanation could be that there were logistical challenges that reduced the completeness of documenting patients' race and ethnicity data during the pandemic. Finally, the single‐institution setting may challenge the generalizability of the findings, though an advantage to this design is the elimination of interinstitutional variability with respect to telemedicine protocols and implementation timelines.
5. CONCLUSION
Telemedicine may be an important tool to overcome challenges in equitable access to pediatric dermatology given several features unique to the specialty. First, there is a need for expanded access. Though skin complaints are common among pediatric patients, 17 there were only 400 practicing board‐certified pediatric dermatologists in the United States in 2020. 2 We found that telemedicine use was higher among patients living farther away from the clinic, suggesting that telemedicine may potentially reduce transportation barriers, resulting in improved access in wider geographical areas and decreased wait times in regions lacking pediatric dermatologists. Second, dermatology is uniquely positioned to implement virtual care due to its visually oriented nature. Telemedicine shows high diagnostic concordance with in‐person consultations for pediatric skin conditions 2 and yields high patient satisfaction. 18 Finally, contemporary youth are well‐versed in navigating technology, making telemedicine a potentially effective way to provide care for this group if provided access to video‐enabled devices and internet connection. 18 , 19
These features suggest that telemedicine may be a promising tool for increasing access to pediatric dermatology, but barriers to telemedicine may currently undermine its potential utility in some communities. Our work serves to promote further dialog on the issues of health equity and telemedicine access in pediatric dermatology.
CONFLICT OF INTEREST
None declared.
AUTHOR CONTRIBUTIONS
All authors had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Rosenblatt, Duan, Ruiz de Luzuriaga, and Schroedl contributed to study concept and design and critical revision of the manuscript for important intellectual content. Duan and Ruiz de Luzuriaga contributed to acquisition of data. Duan and Rosenblatt involved in analysis and interpretation of data and drafting of the manuscript. Duan contributed to statistical analysis. Duan, Rosenblatt, and Ruiz de Luzuriaga involved in administrative, technical, and material support. Rosenblatt contributed to study supervision.
CONSENT STATEMENT
Consent was not required since all data were de‐identified. Protocol was approved by the University of Chicago Biological Sciences Division Institutional Review Board (IRB20‐0848).
ACKNOWLEDGMENTS
This project was supported by the National Center for Advancing Translational Sciences (NCATS) of the National Institutes of Health (NIH) through Grant Number 5UL1TR002389‐04 that funds the Institute for Translational Medicine (ITM). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. We are also grateful for the funding support given by The David E. Rogers Fellowship Program of The New York Academy of Medicine and the University of Chicago Pritzker School of Medicine.
Duan GY, Ruiz De Luzuriaga AM, Schroedl LM, Rosenblatt AE. Disparities in telemedicine use during the COVID‐19 pandemic among pediatric dermatology patients. Pediatr Dermatol. 2022;00:1–8. doi: 10.1111/pde.14982
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
REFERENCES
- 1. Katzow MW, Steinway C, Jan S. Telemedicine and health disparities during COVID‐19. Pediatrics. 2020;146(2):e20201586. doi: 10.1542/peds.2020-1586 [DOI] [PubMed] [Google Scholar]
- 2. Cartron AM, Aldana PC, Khachemoune A. Pediatric teledermatology: a review of the literature. Pediatr Dermatol. 2021;38(1):39‐44. [DOI] [PubMed] [Google Scholar]
- 3. Nouri S, Khoong EC, Lyles CR, Karliner L. Addressing equity in telemedicine for chronic disease management during the Covid‐19 pandemic. NEJM Catalyst. 2020;1(3):1–13. https://catalyst.nejm.org/doi/full/10.1056/CAT.20.0123 [Google Scholar]
- 4. Wood SM, White K, Peebles R, et al. Outcomes of a rapid adolescent telehealth scale‐up during the COVID‐19 pandemic. J Adolesc Health. 2020;67(2):172‐178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gmunder KN, Ruiz JW, Franceschi D, Suarez MM. Demographics associated with US healthcare disparities are exacerbated by the telemedicine surge during the COVID‐19 pandemic. J Telemed Telecare. 2021;9(8):e27977. [DOI] [PubMed] [Google Scholar]
- 6. Franciosi EB, Tan AJ, Kassamali B, et al. The impact of telehealth implementation on underserved populations and no‐show rates by medical specialty during the COVID‐19 pandemic. Telemed J E Health. 2021;27(8):874‐880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Blundell AR, Kroshinsky D, Hawryluk EB, Das S. Disparities in telemedicine access for Spanish‐speaking patients during the COVID‐19 crisis. Pediatr Dermatol. 2021;38(4):947‐949. [DOI] [PubMed] [Google Scholar]
- 8. Illinois Department of Healthcare and Family Services: medical programs. https://www2.illinois.gov/hfs/MedicalClients/Pages/medicalprograms.aspx Accessed December 31, 2021
- 9. Drake C, Lian T, Cameron B, Medynskaya K, Bosworth HB, Shah K. Understanding telemedicine's “new normal": variations in telemedicine use by specialty line and patient demographics. Telemed J E Health. 2022;28(1):51‐59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Gilson SF, Umscheid CA, Laiteerapong N, Ossey G, Nunes KJ, Shah SD. Growth of ambulatory virtual visits and differential use by patient sociodemographics at one urban academic medical center during the COVID‐19 pandemic: retrospective analysis. JMIR Med Inform. 2020;8(12):e24544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Chicago health atlas. https://chicagohealthatlas.org Accessed June 7, 2021
- 12. U.S. Census Bureau QuickFacts: Chicago city, Illinois; United States. https://www.census.gov/quickfacts/fact/table/chicagocityillinois,US/PST045219 Accessed June 7, 2021
- 13. Chunara R, Zhao Y, Chen J, et al. Telemedicine and healthcare disparities: a cohort study in a large healthcare system in New York City during COVID‐19. J Am Med Inform Assoc. 2021;28(1):33‐41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ortega G, Rodriguez JA, Maurer LR, et al. Telemedicine, COVID‐19, and disparities: policy implications. Health Policy Technol. 2020;9(3):368‐371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ukoha EP, Davis K, Yinger M, et al. Ensuring equitable implementation of telemedicine in perinatal care. Obstet Gynecol. 2021;137(3):487‐492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ye S, Kronish I, Fleck E, et al. Telemedicine expansion during the COVID‐19 pandemic and the potential for technology‐driven disparities. J Gen Intern Med. 2021;36(1):256‐258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Prindaville B, Antaya RJ, Siegfried EC. Pediatric dermatology: past, present, and future. Pediatr Dermatol. 2015;32(1):1‐12. [DOI] [PubMed] [Google Scholar]
- 18. Ruggiero A, Megna M, Annunziata MC, et al. Teledermatology for acne during COVID‐19: high patients’ satisfaction in spite of the emergency. J Eur Acad Dermatol Venereol. 2020;34(11):e662‐e663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gehris RP, Herman EIX. Pediatric teledermatology: a review. Curr Dermatol Rep. 2020;9(2):114‐122. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.


