Abstract
Objective
This article reassesses the gender differences in COVID‐19 attitudes and behavior found in previous studies by examining to what extent the gender gap in the adoption of COVID‐19 preventive behaviors is dependent on women's and men's perceptions of risk.
Methods
The data utilized in this study were obtained from the “Understanding America Study Coronavirus in America (‘COVID’) Survey,” conducted by the Center for Economic and Social Research (CESR), at the University of Southern California.
Result
This study shows that women are more risk averse than men, but that the gender gap in risk behavior depends on the level of risk that is associated with COVID‐19.
Conclusion
Risk perception is a stronger driver of risk behavior for men than for women, who generally tend to adopt safe measures to protect themselves and others. Different messages should be delivered to women and men to increase compliance with norms.
Keywords: COVID‐19, gender stereotypes, risk attitudes, risk behavior
Introduction
Governments throughout the world have reacted to COVID‐19 by implementing different types of measures aimed at decreasing the rate of infection transmission (Porcher, 2020; Ratto et al., 2021). Citizens’ levels of compliance with these restrictive measures has varied (Lin et al., 2021) and in some contexts were highly modulated by ideology and political sympathies (Becher et al., 2021; Gonzalez et al., 2021; Wu and Huber, 2021). One common finding cross‐nationally is that there is greater compliance with the restrictive measures established as a consequence of the COVID‐19 breakout among women than among men (Bronfman et al., 2021; Chuang and Liu, 2020; Clark et al., 2020; Galasso et al., 2020; Stockemer et al., 2021), even if men are more likely to suffer worse health consequences from COVID‐19 than women (Islam et al., 2020; Peckham et al., 2020). These gender differences seem to be partly related to gender differences in risk attitudes (Guenther et al., 2021; Lewis and Duch, 2021). This study expands upon previous evidence and shows that women are indeed more risk averse than men in a context of pandemic, but that the gender gap in risk behavior depends on the level of risk that is associated with COVID‐19.
Risk Attitudes and Gender
The common wisdom across disciplines is that women tend to be more risk averse than men. Women tend to have a broader notion of risk and to adopt less risky behaviors than men. Examples of this can be found in the economic sphere (Azmat and Petrongolo, 2014), the political sphere (Kanthak and Woon, 2015; Preece and Stoddard, 2015; Schneider et al., 2016), and the public sphere more generally (Larkin and Pines, 2003). No matter to which sphere of life they refer, most studies conclude that men are more risk‐taking than women (Byrnes et al., 1999; Harris et al., 2006; Weber et al., 2002) either because risk attitudes are attributes of masculine or feminine psychology (Wilson and Daly, 1985), or because they are culturally and stereotypically learnt (Fine, 2017; Morgenroth et al., 2018).
There is also evidence that women are more risk averse than men in the health domain, although differences in health risk behavior between women and men tend to be typically related to well‐established gender stereotypes. One of such gender‐stereotyped risks is alcohol consumption (Wickrama et al., 1999). Since alcohol consumption (a cause of major health problems according to the U.S. Centers for Disease Control and Prevention) is generally associated with masculinity, men are more likely than women to drink alcohol to comply with male stereotypes (Lebreton et al., 2017). On the contrary, women are more likely than men to take other health risks that go against health prescription, such as indoor tanning (linked to illnesses such as cancer according to the U.S. Surgeon General). Women's pressure to look good, under the stereotype that women's bodies are constantly observed and compared with the ideal body, lead them to take higher health risks than other groups of the population by doing indoor tanning or taking diet pills (Choukas‐Bradley et al., 2019; Hill and Durante, 2011). Risk‐taking in sexual behavior is also highly gender stereotyped. Risky sexual behavior is generally more frequent among men than women (Bell et al., 1999), whereas women's sexual relationships tend to search to avoid risk and shame (Setty, 2019), especially when contraception issues are involved (Pearson, 2006).
Health‐care habits that are apparently not related to specific roles of women and men in society also appear to be influenced by gender stereotypes. Whereas men are socialized to be strong and perceive themselves as invulnerable, women are taught to be weak (Prentice and Carranza, 2002). Caring for themselves and for others is seen as part of women's reproductive function (Eagly and Wood, 1999; Fenstermaker and West, 2002), and the health‐care sector itself is heavily feminized: 70 percent of the global health workforce are women (Lotta et al., 2021; Shannon et al., 2019). Conceivably related to gender socialization, there is evidence that men tend to care less about their health than women in relation to smoking, preventative health, and dietary habits (Courtenay, 2000b; Sánchez–López et al., 2012), which has a large influence on their well‐being and affects men's death rates (Courtenay, 2000a). Men are also less likely to take care of themselves and seek for help in case of illness than women (Juvrud and Rennels, 2017), whereas women are incentivized to seek for help (Nathanson, 1977). Generally, men are more likely to take risks that affect health than women (Courtenay, 1999).
Existing evidence in relation to COVID‐19 complies with the stereotype that women are more risk averse than men. Women are generally more informed about COVID‐19 than men (Sylvester, 2021), and more supportive of, and compliant with, the restrictive measures (Bronfman et al., 2021; Chuang and Liu, 2020; Clark et al., 2020; Fredén and Sikström, 2021; Galasso et al., 2020; Lin et al., 2021; Stockemer et al., 2021), independently of their ideology (Algara et al., 2021). A meta‐analysis of individuals’ risk perception of COVID also shows that most studies find a gender difference in risk perception, as women tend to perceive higher risks than men (Lewis and Duch, 2021). Building on the above, Hypothesis 1 predicts that in real‐time risks such as COVID‐19: (a) women will perceive COVID‐19 as riskier than men; (b) women will attribute less benefits to risky behaviors during COVID‐19 than men; and (c) women will take less risks related to COVID‐19 than men.
Further, previous research has shown that there is a causal link between the risk perception related to COVID‐19 and the willingness to comply with restrictive measures imposed by governments (Bruine de Bruin and Bennett, 2020; Wise et al., 2020). A major assumption derived from this finding is that the observed gender gap in compliance during the pandemic is due to the fact that women perceive higher risks related to COVID than men. The scarce existing studies do point at mixed findings in this regard, however. In line with the assumption posed in the previous lines, Alsharawy et al. (2021) find that gender differences in COVID compliance disappear once perceptions of fear are controlled for, meaning that the gender gap in compliance with the norms is partly derived from women's higher risk perception associated with COVID‐19. To the contrary, Stockemer et al. (2021) found that there are only slight gender differences in health risk perceptions associated with COVID‐19, and yet women are significantly more supportive of strict restrictive measures than men (see also Galasso et al., 2020). In that case, the gender gap in compliance is not dependent on different assessments of risk by women and men. As shown above, most literature on risk‐taking in the health domain tends to endorse the second view, namely, that women are more likely to care for themselves and adopt healthy habits than men. Women's risk behavior might be less dependent on the context (that is, for example, on how big the effective risk of infection is) than men, as women typically behave more safely than men even in the absence of risks. Hypothesis 2 thus expects that men's risk behavior will be more influenced by risk perception and expected benefit than women's.
Method
Sample
The data utilized in this study were obtained from the “Understanding America Study Coronavirus in America (‘COVID’) Survey,” conducted by the Center for Economic and Social Research (CESR), at the University of South Carolina. The survey was launched on March 10 in all 50 of the U.S. states, and it is an ongoing tracking poll, which is re‐fielded every two weeks, with invitation sent to one fourteenth of the respondents. This article uses five waves of the study of the representative sample for the whole of the United States, starting March 10 and ending June 8, 2020. List‐wise deletion of observations with missing data on the independent variables was used (Allison, 2002). Before dropping missing variables, the sample size was 22,388. The final sample size is 21,932 observations, for 5,142 interviewees from the United States (2,170 men and 2,972 women) who have been interviewed 4.23 times on average (unbalanced data). Table A.1 in the Supplementary Information presents descriptive data about the sample. The survey measures U.S. citizens’ attitudes and behaviors toward the new COVID‐19 and it fits the objectives of this study particularly well, as it includes measurements of risk‐taking in relation to COVID‐19; measurements of risk perception of COVID‐19; and a set of measurements on the expected benefits of risk avoidance.
Dependent Variable: Risk Behavior
To operationalize risk behavior related to COVID‐19, a battery of items is used that asks respondents whether they have done any of the activities included on a list to avoid risks from COVID: “Which of the following have you done in the last seven days to keep yourself safe from coronavirus? Only consider actions that you took or decisions that you made personally.” The question includes 13 actions, including wearing a facemask or cancelling a doctor's appointment (see Table 1 for the whole list). The original variables have been recoded so that they take value 0 if the respondent has done the action in the last seven days (the safe option), and value 1 if the respondent has not done the action (the risky option). The resulting variable is the count of the risky actions each respondent has done in the COVID context, a variable that ranges from 0 (if the respondent has done all the actions to protect him/herself, and therefore assumes the safest behavior) to 13 (if the respondent has not done any of the actions to protect him/herself, and therefore assumes the riskiest behavior). Cronbach's alpha of the scale of risk behavior is 0.82.
TABLE 1.
Dependent variable: Gender differences in risk behavior
| Female (%) | Male (%) | Female–male diff | |
|---|---|---|---|
| Wash hands | 5.16 | 8.19 | −3.03*** |
| Avoided public spaces | 20.01 | 22.59 | −2.58*** |
| Avoided contact with high‐risk people | 20.18 | 23.11 | −2.93*** |
| Avoided restaurants | 26.26 | 28.85 | −2.59*** |
| Worn facemask | 40.96 | 44.67 | −3.71*** |
| Changed personal or social activities | 41.63 | 45.43 | −3.79*** |
| Changed pleasure travel | 54.12 | 57.40 | −3.28*** |
| Worked or studied from home | 54.12 | 56.74 | −2.62*** |
| Changed work or school activities | 67.15 | 73.69 | −6.54*** |
| Cancelled a doctor's appointment | 71.70 | 78.62 | −6.91*** |
| Avoided Chinese restaurant | 74.79 | 80.71 | −5.92*** |
| Stockpiled food or water | 75.64 | 78.59 | −2.95*** |
| Changed work travel | 78.51 | 77.72 | 0.80 |
| Female (mean) | Male (mean) | Female−male diff. | |
| Scale of risk behavior (0–13) | 5.66 | 6.08 | −0.41*** |
Differences statistically significant at p < 0.000. T test, two‐tailed.
The Other Components of Risk: Risk Perception and Expected Benefit
Two alternative variables are used to operationalize the respondent's risk perceptions of COVID‐19. A first variable measures the respondent's perceived risk of being infected with COVID‐19: “On a scale of 0 to 100 percent, what is the chance that you will get the coronavirus in the next three months?” A second item captures the respondents’ perceived risk of dying from COVID‐19 if infected: “If you do get the coronavirus, what is the percent chance [on a scale of 0 to 100 percent] you will die from it?” The two original variables are used separately in the analyses, as they tap into different dimensions of risk. Pearson's correlation between the two is 0.31 (significant at p < 0.001).
The following set of questions is used for the expected benefit of risk‐taking: “How effective are the following actions for keeping you safe from coronavirus? Wearing a mask; Washing hands; Avoiding public events; Avoiding high‐risk people; Avoiding restaurants; and Avoiding travelling” (five response categories, from extremely ineffective—value 0—to extremely effective—value 4; midpoint is “unsure”). The six items have been added to create a scale that takes value 0 if the respondent assesses all actions as extremely ineffective in protecting against COVID, and value 25 if the respondent assesses all actions as extremely effective in protecting against COVID. The resulting scale, therefore, is not an indicator of the expected benefits of taking risks, but a scale of perceived effectiveness of risk avoidance (Cronbach's alpha for the scale is 0.87). It is therefore expected that there is a negative relationship between the scale of risk avoidance and the scale of risk behavior.
Other Independent Variables
Corresponding with the theoretical expectations, sex is the main independent variable, a dichotomous variable that takes value 0 for male and 1 for female. In addition, a set of controls are introduced in the statistical models that are expected to influence risk behavior. Age and life period are generally related to different propensity to risk: While the youth are generally more willing to take risks, the propensity to engage in risky actions diminishes as people become old. This holds true in the COVID‐19 context (Lin et al., 2021). Age is included as a continuous variable that ranges from 18 to 101 years old. Levels of education are related to the capacity to obtain information, which in turn is related to better decision making and higher compliance with norms (Hermans et al., 2021). A categorical variable accounts for education levels, distinguishing between respondents with less than a high school education (the reference category), a high school education, a college education, a bachelor's degree, or a master's or PhD. The family situation is also introduced, as a proxy for interpersonal relationships (Elder and Greene, 2021; Leiter et al., 2021). Indeed, people who live alone might feel less pressure to protect themselves from COVID than people who live with their partner (a dichotomous variable that indicates whether the respondent lives with his/her partner—1—or not—0) or their children (a dichotomous variable that distinguishes between childless respondents—0—and respondents with children—1).
Considering that COVID‐19 might have influenced respondents’ stress levels and that this is likely to affect their risk behavior (Obschonka et al., 2021), mental distress is also accounted for, as a composite measure of the frequency (from not at all to nearly every day) respondents have been bothered by the following problems: feeling anxious, feeling depressed, feeling little interest, and feeling worried. The scale of mental distress takes value 0 if the respondent has not been affected by any of these problems, and value 12 if she has been affected by all these problems nearly every day (Cronbach's alpha of the scale of distress is 0.89). Ethnoracial identity (distinguishing between white—the reference category—black, American Indian/Alaska native, Asian, Hawaiian/Pacific, and Mixed) and labor situation (distinguishing between employed—the reference category—unemployed, retired, disabled, and other) are also used as controls. Finally, to account for the fact that COVID‐19 has had a different impact both across the U.S. states and across time which is likely to affect citizens’ risk perceptions and behaviors, two additional variables are included: the state of residence (a categorical variable that identifies each of the 50 states and the District of Columbia; the reference category is Alabama) and the date of the interview (introduced as a continuous variable, from March 10, 2020, to June 8, 2021).
Analysis Plan
To test for the main hypotheses posed in this article, two empirical strategies are used. First, the article presents gender differences (percentages and means) and statistical significance tests (two‐tailed) for the three components of risk (risk behavior, risk perception, and expected benefit). Second, to test for the stability of gender differences in risk behavior after controlling for additional variables, a set of statistical models are estimated using Stata 17. In particular, due to the panel structure of the data, five random‐effects models (with robust standard errors) are estimated that include all variables described in the previous sections. Apart from the panel nature of the data, random‐effect modeling is especially suited for the purposes of this study, as it allows for time‐invariant variables such as sex to play a role as explanatory variables (the Hausman test also supports the appropriateness of using random‐effect modeling). The dependent variable is risk behavior, and the main independent variables are sex, risk perception, and the scale of expected effectiveness of risk avoidance. To test for Hypothesis 2 (the relationship between risk perception/benefit and risk behavior is stronger for men than for women), an interaction term has been introduced between risk perception (perceived risk of infection with COVID and perceived risk of death from COVID) and the scale of expected effectiveness of risk avoidance and sex. Main results are presented in the following section.
Results
Table 1 presents the percentage of respondents who avoided each of the 13 actions that compose the scale of risk behavior, and took risks. As can be seen in the table, except for one of the actions—“changed work travel”—males are significantly more likely to take risks than women (t test, two‐tailed). Gender differences range from 2.58 percent (avoided public spaces) to almost 7 percent (cancelled a doctor's appointment). On average, women are significantly more likely to take safe actions than men: The mean is 5.66 for women and 6.08 for men (differences statistically significant at p < 0.000). Data from Table 1 are therefore in line with Hypothesis 1, confirming the higher propensity of men to take risks than women in the COVID‐19 context.
As for the other two components of risk, Table 2 presents means and standard deviations of the scale of perceived effectiveness of risk avoidance (and its constituents) and risk perceptions of COVID of women and men (two‐tailed significance t test). As hypothesized, and even if there is a generalized belief that most measures are effective in protecting against COVID among respondents (the mean is above 3 for all measures, the “somewhat effective” response category), women's perceptions of effectiveness are significantly higher than men's (significant at p < 0.000). In other words, women tend to perceive the benefits of the safe option more than men do: The mean value for women on the scale of perceived efficacy of risk avoidance is 20.5 compared with men's 19.7 (difference is 0.78, statistically significant at p < 0.000). Table 2 also shows that there are differences between males and females in relation to risk perception. Women tend to perceive COVID as riskier than men, in relation to both risk of infection and risk of death. On average, women estimate they have around a 25 percent chance of being infected by COVID, while men estimate their chances at 22.6 percent. Similarly, females think they have greater chances of dying due to COVID (21.4 percent) than men (18.6 percent; differences statistically significant at p < 0.000). Confirming H1, in real‐time risks, women tend to perceive greater risks than men; they perceive that the safe options are more effective than men do; and they take less risks than men.
TABLE 2.
Other components of risk: Gender differences in perceived effectiveness of risk avoidance, and risk perceptions of infections with and death from COVID
| Female | Male | ||||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Female–male diff. | |
| Expected benefit of risk avoidance | |||||
| Effectiveness: Washing hands (0–4) | 3.69 | 0.81 | 3.57 | 0.9 | 0.12*** |
| Effectiveness: Avoiding high‐risk people (0–4) | 3.6 | 0.89 | 3.52 | 0.97 | 0.08*** |
| Effectiveness: Avoiding public (0–4) | 3.54 | 0.91 | 3.44 | 0.98 | 0.10*** |
| Effectiveness: Avoiding travel (0–4) | 3.41 | 0.95 | 3.21 | 1.06 | 0.20*** |
| Effectiveness: Avoiding restaurants (0–4) | 3.27 | 1.02 | 3.14 | 1.09 | 0.13*** |
| Effectiveness: Wearing facemasks (0–4) | 3.0 | 1.15 | 2.83 | 1.19 | 0.17*** |
| Scale of effectiveness of risk avoidance (0–25) | 20.46 | 4.51 | 19.68 | 4.87 | 0.78*** |
| Perceived risk | |||||
| Perceived risk of infection (0–100) | 25.06 | 22.64 | 22.63 | 21.12 | 2.43*** |
| Perceived risk of death (0–00) | 21.45 | 25.78 | 18.64 | 24.95 | 2.81*** |
Differences statistically significant at p < 0.000. T test, two‐tailed.
But are gender differences stable even after controlling for other potential contextual and individual characteristics that influence risk behavior? Table 3 presents the estimation results of five random‐effects models, predicting risk behavior. For the sake of clarity, only the main variables of interest are retained in Table 3, but complete results including all independent variables can be found in Table A.2 in the Supplementary Information. Models 1 and 2 in Table 3 show the effect of the components of risk (perceived risk and expected benefit) on the dependent variable (risk behavior), as well as the effect of sex and date of the interview. Models 3 to 5 in Table 3 introduce the interactive term between perceived risk or expected benefit and sex to test for potential gender differences in the relationship between the different components of risk.
TABLE 3.
Random‐effects models with the scale of risk behavior as the dependent variable
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |
|---|---|---|---|---|---|
| Variables | |||||
| Sex (female) | −0.165*** | −0.159*** | −0.252*** | −0.223*** | −0.172 |
| (0.0583) | (0.0584) | (0.0769) | (0.0679) | (0.267) | |
| Perceived risk of infection | −0.0155*** | −0.0178*** | −0.0155*** | ||
| (0.00105) | (0.00166) | (0.00105) | |||
| Perceived risk of death | −0.0166*** | −0.0186*** | |||
| (0.00104) | (0.00165) | ||||
| Risk avoidance effectiveness scale | −0.144*** | −0.144*** | −0.144*** | −0.144*** | −0.145*** |
| (0.00637) | (0.00638) | (0.00637) | (0.00637) | (0.00953) | |
| Date of interview | −0.0351*** | −0.0344*** | −0.0351*** | −0.0344*** | −0.0351*** |
| (0.000721) | (0.000721) | (0.000722) | (0.000721) | (0.000721) | |
| Perceived risk of infection#sex | 0.00373* | ||||
| (0.00211) | |||||
| Perceived risk of death#sex | 0.00330 | ||||
| (0.00204) | |||||
| Scale of effectiveness#sex | 0.000331 | ||||
| (0.0126) | |||||
| Constant | 11.92*** | 11.59*** | 11.97*** | 11.63*** | 11.92*** |
| (0.330) | (0.334) | (0.332) | (0.335) | (0.364) | |
| Observations | 21,932 | 21,927 | 21,932 | 21,927 | 21,932 |
| Number of numid | 5,142 | 5,140 | 5,142 | 5,140 | 5,142 |
Robust standard errors in parentheses. Tests of significance are two‐tailed.
p < 0.01.
**p < 0.05.
p < 0.1.
As a short summary, Table A.2 in the Supplementary Information suggests that the young, those with less education, white people, and respondents who have low levels of mental distress are more likely to take risks related to COVID than the old, the highly educated, non‐white people, and respondents who suffer from high levels of mental distress. Importantly, in line with previous studies (Bruine de Bruin and Bennett, 2020; Wise et al., 2020), risk behavior is affected by the two other components of risk: risk perception and expected benefits. The willingness to engage in risky actions decreases significantly the higher the perceived risk of infection with or death from COVID is, as shown by the negative and statistically significant coefficients in Table 3. Confirming the different nature of the two risks—infection versus death—the magnitude of the coefficients is different, and the effect of the perceived risk of death is the strongest of the two. Accordingly, time is also negatively correlated to risk behavior: as people become aware of the risks involved with COVID, they are more likely to protect themselves and avoid risky behavior. This notwithstanding, the correlation between time and risk perception is low (Pearson's correlation between time and perceived risk of infection is 0.004; between time and perceived risk of death is 0.05, significant at p < 0.01), which is an indication that risk perception is imperfectly related to the context but rather depends on individuals’ interpretations of the content and context of risk. The other component of risk—the scale of perceived effectiveness of risk avoidance—is also negatively and significantly related to risk behavior: The more one believes that cautious attitudes are effective against COVID, the more likely it is that she will avoid risky behaviors.
However, the main variable of interest in Table 3 is sex. Results confirm that even after controlling for other potential correlates of risk behavior, the coefficient of sex is negative and significant. Women are less likely to take risks than men are, including in real‐time risk situations such as COVID‐19. Tables 1 and 2 have shown that all components of risk are gender‐biased, but including the risk components in the model does not cancel the effect of sex on risk behavior, which is strongly in favor of a differentiated effect of sex on risk attitudes. Table 3 further confirms H1 that there are gender differences in risk perception and risk behavior in real situations.
H2 (men's risk behavior will be more strongly influenced by risk perception/expected benefit than women's) is partially confirmed in Table 3, Models 3 to 5. On the one hand, the interaction term between perceived risk and sex is positive and significant (the coefficient for perceived risk of death is at the limit of significance, p = 0.106), which means that the effect of perceived risk on the dependent variable is different for women and for men (models 3 and 4 in Table 3). As predicted by Hypothesis 2, while men tend to behave and adopt risks in accordance to their perception of risks, women's risk behavior is less affected by their perceptions of risk. Put differently, the relationship between risk perception and risk behavior is stronger for men than for women. There are, however, no sex differences in the effect of the scale of perceived effectiveness of risk avoidance on the dependent variable (model 5 in Table 3). Risk perception is the variable that most conditions risk behavior of women and men. For ease of interpretation of the interactive term, Figure 1 shows the marginal effects of sex on the scale of risk avoidance for different levels of perception of risk of infection (left quadrant in Figure 1, Model 3 in Table 3) and different levels of perception of risk of death (right quadrant in Figure 1, Model 4 in Table 3). As can be seen in the two figures, the relationship between perception of risk and risk behavior is steeper for men than for women. With low perception of risk (less than 25 percent chances of being infected or dying), women are less likely to adopt risks than men are. Yet once perceptions of risk increase (above 25 percent), differences in risk‐taking between women and men disappear. Risk perception is therefore a stronger driver of risk behavior for men than for women, who generally tend to adopt safe measures to protect themselves and others (as stereotyping would predict).
FIGURE 1.
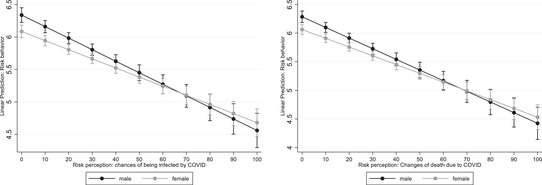
Marginal effects of sex on the scale of risk behavior for different levels of perception of risk of infection with COVID (left quadrant) and risk of death from COVID (right quadrant). The figure presents the marginal effects of a respondent's perceived risk of infection (left quadrant) and death (right quadrant), with 95 percent confidence intervals, dependent on their sex, on the scale of risk behavior, and based on the interaction model estimates (models 3 and 4 of Table 3)
Conclusions
This article provides further evidence of the gender gap in risk in context. Using evidence of Americans’ risk behavior during the first two months of the COVID‐19 pandemic, it shows that women are less likely than men to engage in risky behavior in real risk situations. Women's risk behavior, in addition, is less influenced than men's by the extent to which they perceive COVID‐19 as a risk. Thus, women have stronger preferences than men for the safe option, even when the risks associated with COVID‐19 are low. Findings from this article confirm, therefore, previous evidence in the COVID‐19 context (e.g., Galasso et al., 2020) and advance our knowledge about the differentiated relationship between risk perception and risk behavior for women and men.
An important implication of these findings is that different messages ought to be sent to foster women's and men's compliance in a context of risk such as COVID‐19, taking into account that risk behavior tends to conform to gender stereotypes. As such, information addressed to men ought to be aimed at raising their perception of risk, since men are more likely to adopt safe measures once they become aware of the risks associated with COVID‐19 (see also Lewis and Duch, 2021).
Supporting information
Table A.1 Descriptive data
Table A.2 Full results of the random effect estimations
Ferrín, Mónica. 2022. “Reassessing Gender Differences in COVID‐19 Risk Perception and Behavior.” Social Science Quarterly. 103: 31–41. 10.1111/ssqu.13116
REFERENCES
- Algara, Carlos , Fuller Sam, Hare Christopher, and Kazemian Sara. 2021. “The Interactive Effects of Scientific Knowledge and Gender on COVID‐19 Social Distancing Compliance.” Social Science Quarterly 102(1): 7–16. 10.1111/ssqu.12894. [DOI] [Google Scholar]
- Allison, Paul. 2002. Missing Data. Thousand Oaks: SAGE Publications. [Google Scholar]
- Alsharawy, Abdelaziz , Spoon Ross, Smith Alec, and Ball Sheryl. 2021. “Gender Differences in Fear and Risk Perception During the COVID‐19 Pandemic.” Frontiers in Psychology 12(August): 689467. 10.3389/fpsyg.2021.689467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azmat, Ghazala , and Petrongolo Barbara. 2014. “Gender and the Labor Market: What Have We Learned from Field and Lab Experiments?” Labour Economics, Special Section articles on "What determined the dynamics of labour economics research in the past 25 years? edited by Joop Hartog and European Association of Labour Economists 25th Annual Conference, Turin, Italy, 19–21 September 2013 Edited by Michele Pellizzari, 30(October): 32–40. 10.1016/j.labeco.2014.06.005. [DOI] [Google Scholar]
- Becher, Michael , Stegmueller Daniel, Brouard Sylvain, and Kerrouche Eric. 2021. “Ideology and Compliance with Health Guidelines during the COVID‐19 Pandemic: A Comparative Perspective.” Social Science Quarterly 102(5): 2106–23. 10.1111/ssqu.13035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell, Nancy J. , O'Neal Keri K., Feng Du, and Schoenrock Carol J.. 1999. “Gender and Sexual Risk.” Sex Roles 41(5): 313–32. 10.1023/A:1018866515084. [DOI] [Google Scholar]
- Bronfman, Nicolas , Repetto Paula, Cordon Paola, Castaneda Javiera, and Cisternas Pamela. 2021. “Gender Differences on Psychosocial Factors Affecting COVID‐19 Preventive Behaviors.” Sustainability 13(11): 6148. 10.3390/su13116148. [DOI] [Google Scholar]
- Bruine de Bruin, Wändi , and Bennett Daniel. 2020. “Relationships Between Initial COVID‐19 Risk Perceptions and Protective Health Behaviors: A National Survey.” American Journal of Preventive Medicine 59(2): 157–67. 10.1016/j.amepre.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byrnes, James P. , Miller David C., and Schafer William D.. 1999. “Gender Differences in Risk Taking: A Meta‐Analysis.” Psychological Bulletin 125(3): 367–83. 10.1037/0033-2909.125.3.367. [DOI] [Google Scholar]
- Choukas‐Bradley, Sophia , Nesi Jacqueline, Widman Laura, and Noar Seth M.. 2019. “Examining the Roles of Self‐Objectification and Appearance Expectations in Young Women's Indoor Tanning Behavior.” Sex Roles 80(1): 52–62. 10.1007/s11199-018-0913-9. [DOI] [Google Scholar]
- Chuang, Yating , and Liu John Chung‐En. 2020. “Who Wears a Mask? Gender Differences in Risk Behaviors in the COVID‐19 Early Days in Taiwan.” Economics Bulletin 40(4): 2619–27. [Google Scholar]
- Clark, Cory , Davila Andrés, Regis Maxime, and Kraus Sascha. 2020. “Predictors of COVID‐19 Voluntary Compliance Behaviors: An International Investigation.” Global Transitions 2(January): 76–82. 10.1016/j.glt.2020.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Courtenay, W. H. 1999. “Better to Die than Cry? A Longitudinal and Constructionist Study of Masculinity and the Health Risk Behavior of Young American Men.” US: ProQuest Information & Learning.
- Courtenay, W. H. 2000a. “Constructions of Masculinity and Their Influence on Men's Well‐Being: A Theory of Gender and Health.” Social Science & Medicine 50(10): 1385–401. 10.1016/S0277-9536(99)00390-1. [DOI] [PubMed] [Google Scholar]
- Courtenay, W. H. 2000b. “Behavioral Factors Associated with Disease, Injury, and Death among Men: Evidence and Implications for Prevention.” The Journal of Men's Studies 9(1): 81–142. 10.3149/jms.0901.81. [DOI] [Google Scholar]
- Eagly, Alice H. , and Wood Wendy. 1999. “The Origins of Sex Differences in Human Behavior: Evolved Dispositions versus Social Roles.” American Psychologist 54(6): 408–23. [Google Scholar]
- Elder, Laurel , and Greene Steven. 2021. “A Recipe for Madness: Parenthood in the Era of Covid‐19.” Social Science Quarterly 102(5): 2296–311. 10.1111/ssqu.12959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fenstermaker, Sarah , and West Candace. 2002. Doing Gender, Doing Difference: Inequality, Power, and Institutional Change. East Sussex, UK: Psychology Press. [Google Scholar]
- Fine, Cordelia. 2017. Testosterone Rex: Myths of Sex, Science, and Society. New York: W. W. Norton & Company. [Google Scholar]
- Fredén, Annika , and Sikström Sverker. 2021. “Voters’ View of Leaders during the Covid‐19 Crisis: Quantitative Analysis of Keyword Descriptions Provides Strength and Direction of Evaluations.” Social Science Quarterly 102(5): 2170–83. 10.1111/ssqu.13036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galasso, Vincenzo , Pons Vincent, Profeta Paola, Becher Michael, Brouard Sylvain, and Foucault Martial. 2020. “Gender Differences in COVID‐19 Attitudes and Behavior: Panel Evidence from Eight Countries.” Proceedings of the National Academy of Sciences 117(44): 27285–91. 10.1073/pnas.2012520117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez, Kelsey E. , James Rina, Bjorklund Eric T., and Hill Terrence D.. 2021. “Conservatism and Infrequent Mask Usage: A Study of US Counties during the Novel Coronavirus (COVID‐19) Pandemic.” Social Science Quarterly 102(5): 2368–82. 10.1111/ssqu.13025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guenther, Benno , Galizzi Matteo M., and Sanders Jet G.. 2021. “Heterogeneity in Risk‐Taking During the COVID‐19 Pandemic: Evidence from the UK Lockdown.” Frontiers in Psychology 12: 852. 10.3389/fpsyg.2021.643653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris, Christine R. , Jenkins Michael, and Glaser Dale. 2006. “Gender Differences in Risk Assessment: Why Do Women Take Fewer Risks than Men?” Judgment and Decision Making 1(1): 48–63. [Google Scholar]
- Hermans, Lize , Van den Broucke Stephan, Gisle Lydia, Demarest Stefaan, and Charafeddine Rana. 2021. “Mental Health, Compliance with Measures and Health Prospects during the COVID‐19 Epidemic: The Role of Health Literacy.” BMC Public Health [Electronic Resource] 21(1):1365. 10.1186/s12889-021-11437-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill, Sarah E. , and Durante Kristina M.. 2011. “Courtship, Competition, and the Pursuit of Attractiveness: Mating Goals Facilitate Health‐Related Risk Taking and Strategic Risk Suppression in Women.” Personality and Social Psychology Bulletin 37(3): 383–94. 10.1177/0146167210395603. [DOI] [PubMed] [Google Scholar]
- Islam, Nazrul , Khunti Kamlesh, Dambha‐Miller Hajira, Kawachi Ichiro, and Marmot Michael. 2020. “COVID‐19 Mortality: A Complex Interplay of Sex, Gender and Ethnicity.” European Journal of Public Health 30(5): 847–48. 10.1093/eurpub/ckaa150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juvrud, Joshua , and Rennels Jennifer L.. 2017. “‘I Don't Need Help’: Gender Differences in How Gender Stereotypes Predict Help‐Seeking.” Sex Roles 76(1): 27–39. 10.1007/s11199-016-0653-7. [DOI] [Google Scholar]
- Kanthak, Kristin , and Woon Jonathan. 2015. “Women Don't Run? Election Aversion and Candidate Entry.” American Journal of Political Science 59(3): 595–612. 10.1111/ajps.12158. [DOI] [Google Scholar]
- Larkin, Judith E. , and Pines Harvey A.. 2003. “Gender and Risk in Public Performance.” Sex Roles 49(5): 197–210. 10.1023/A:1024689605569. [DOI] [Google Scholar]
- Lebreton, Florian , Peralta Robert L., Allen‐Collinson Jacquelyn, Wiley Lia Chervenak, and Routier Guillaume. 2017. “Contextualizing Students’ Alcohol Use Perceptions and Practices within French Culture: An Analysis of Gender and Drinking among Sport Science College Students.” Sex Roles 76(3): 218–35. 10.1007/s11199-016-0652-8. [DOI] [Google Scholar]
- Leiter, Debra , Reilly Jack, and Vonnahme Beth. 2021. “The Crowding of Social Distancing: How Social Context and Interpersonal Connections Affect Individual Responses to the Coronavirus.” Social Science Quarterly 102(5): 2435–51. 10.1111/ssqu.13060. [DOI] [Google Scholar]
- Lewis, Andrew , and Duch Raymond. 2021. “Gender Differences in Perceived Risk of COVID‐19.” Social Science Quarterly 102(5): 2124–33. 10.1111/ssqu.13079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin, Tian , Harris Elizabeth A., Heemskerk Amber, Bavel Jay J. Van, and Ebner Natalie C.. 2021. “A Multi‐National Test on Self‐Reported Compliance with COVID‐19 Public Health Measures: The Role of Individual Age and Gender Demographics and Countries’ Developmental Status.” Social Science & Medicine 286(October): 114335. 10.1016/j.socscimed.2021.114335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lotta, Gabriela , Fernandez Michelle, Pimenta Denise, and Wenham Clare. 2021. “Gender, Race, and Health Workers in the COVID‐19 Pandemic.” The Lancet 397(10281): 1264. 10.1016/S0140-6736(21)00530-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgenroth, Thekla , Fine Cordelia, Ryan Michelle K., and Genat Anna E.. 2018. “Sex, Drugs, and Reckless Driving: Are Measures Biased toward Identifying Risk‐Taking in Men?” Social Psychological and Personality Science 9(6): 744–53. 10.1177/1948550617722833. [DOI] [Google Scholar]
- Nathanson, Constance A. 1977. “Sex Roles as Variables in Preventive Health Behavior.” Journal of Community Health 3(2): 142–55. 10.1007/BF01674236. [DOI] [PubMed] [Google Scholar]
- Obschonka, Martin , Gewirtz Abigail H., and Zhu Liqi. 2021. “Psychological Implications of the COVID‐19 Pandemic around the World: Introduction to the Special Issue.” International Journal of Psychology 56(4): 493–97. 10.1002/ijop.12793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson, Jennifer. 2006. “Personal Control, Self‐Efficacy in Sexual Negotiation, and Contraceptive Risk among Adolescents: The Role of Gender.” Sex Roles 54(9): 615–25. 10.1007/s11199-006-9028-9. [DOI] [Google Scholar]
- Peckham, Hannah , Gruijter Nina M. de, Raine Charles, Radziszewska Anna, Ciurtin Coziana, Wedderburn Lucy R., Rosser Elizabeth C., Webb Kate, and Deakin Claire T.. 2020. “Male Sex Identified by Global COVID‐19 Meta‐Analysis as a Risk Factor for Death and ITU Admission.” Nature Communications 11(1): 6317. 10.1038/s41467-020-19741-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porcher, Simon. 2020. “Response2covid19, a Dataset of Governments’ Responses to COVID‐19 All around the World.” Scientific Data 7(1): 423. 10.1038/s41597-020-00757-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preece, Jessica , and Stoddard Olga. 2015. “Why Women Don't Run: Experimental Evidence on Gender Differences in Political Competition Aversion.” Journal of Economic Behavior & Organization 117(September): 296–308. 10.1016/j.jebo.2015.04.019. [DOI] [Google Scholar]
- Prentice, Deborah A. , and Carranza Erica. 2002. “What Women and Men Should Be, Shouldn't Be, Are Allowed to Be, and Don't Have to Be: The Contents of Prescriptive Gender Stereotypes.” Psychology of Women Quarterly 26(4): 269–81. 10.1111/1471-6402.t01-1-00066. [DOI] [Google Scholar]
- Ratto, María Celeste , Cabrera Juan Manuel, Zacharías Daniela, and Azerrat Juan Martín. 2021. “The Effectiveness of Government Measures during the First Wave of the Outbreak.” Social Science Quarterly 102(5): 2088–105. 10.1111/ssqu.13043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sánchez‐López, María del Pilar , Cuellar–Flores Isabel, and Dresch Virginia. 2012. “The Impact of Gender Roles on Health.” Women & Health 52(2): 182–96. 10.1080/03630242.2011.652352. [DOI] [PubMed] [Google Scholar]
- Schneider, Monica C. , Holman Mirya R., Diekman Amanda B., and McAndrew Thomas. 2016. “Power, Conflict, and Community: How Gendered Views of Political Power Influence Women's Political Ambition.” Political Psychology 37(4): 515–31. 10.1111/pops.12268. [DOI] [Google Scholar]
- Setty, Emily. 2019. “Meanings of Bodily and Sexual Expression in Youth Sexting Culture: Young Women's Negotiation of Gendered Risks and Harms.” Sex Roles 80(9): 586–606. 10.1007/s11199-018-0957-x. [DOI] [Google Scholar]
- Shannon, Geordan , Minckas Nicole, Des Tan Hassan Haghparast‐Bidgoli, Batura Neha, and Mannell Jenevieve. 2019. “Feminisation of the Health Workforce and Wage Conditions of Health Professions: An Exploratory Analysis.” Human Resources for Health 17(1): 72. 10.1186/s12960-019-0406-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stockemer, Daniel , Plank Friedrich, and Niemann Arne. 2021. “The COVID‐19 Pandemic and Government Responses: A Gender Perspective on Differences in Public Opinion.” Social Science Quarterly 102(5): 2383–93. 10.1111/ssqu.13028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sylvester, Steven M. 2021. “COVID‐19 and Motivated Reasoning: The Influence of Knowledge on COVID‐Related Policy and Health Behavior.” Social Science Quarterly 102(5): 2341–59. 10.1111/ssqu.12989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weber, Elke U. , Blais Ann‐Renée, and Betz Nancy E.. 2002. “A Domain‐Specific Risk‐Attitude Scale: Measuring Risk Perceptions and Risk Behaviors.” Journal of Behavioral Decision Making 15(4): 263–90. 10.1002/bdm.414. [DOI] [Google Scholar]
- Wickrama, K. A. S. , Conger Rand D., Wallace Lora Ebert, and Elder Glen H.. 1999. “The Intergenerational Transmission of Health‐Risk Behaviors: Adolescent Lifestyles and Gender Moderating Effects.” Journal of Health and Social Behavior 40(3): 258–72. 10.2307/2676351. [DOI] [PubMed] [Google Scholar]
- Wilson, Margo , and Daly Martin. 1985. “Competitiveness, Risk Taking, and Violence: The Young Male Syndrome.” Ethology and Sociobiology 6(1): 59–73. 10.1016/0162-3095(85)90041-X. [DOI] [Google Scholar]
- Wise, Toby , Zbozinek Tomislav D., Michelini Giorgia, Hagan Cindy C., and Mobbs Dean. 2020. “Changes in Risk Perception and Self‐Reported Protective Behaviour during the First Week of the COVID‐19 Pandemic in the United States.” Royal Society Open Science 7(9): 200742. 10.1098/rsos.200742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu, Jennifer D. , and Huber Gregory A.. 2021. “Partisan Differences in Social Distancing May Originate in Norms and Beliefs: Results from Novel Data.” Social Science Quarterly 102(5): 2251–65. 10.1111/ssqu.12947. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table A.1 Descriptive data
Table A.2 Full results of the random effect estimations


