Introduction
Amelanotic and hypomelanotic melanomas (AHM) represent 2–8% of all melanomas. They are often diagnosed late due to the lack of a distinctive clinical appearance. As a result, AHM is associated with higher mortality compared with pigmented melanomas. It is, therefore, crucial to be aware of the dermoscopic features of such lesions to aid early diagnosis.
Case Presentation
During a 6-year period (2014–2019), a total of 165 melanoma cases were diagnosed via our teledermoscopy service, using Nikon D300S camera and Heine® Delta 20T dermatoscope. Of those, 49 cases (29.7%) were AHM, including 27 males and 22 females with a median age of 68 years (range 16–87 years). Most AMH were on the upper limbs (20 patients) and the trunk (13 patients). The rest were on the lower limbs (9 patients), and head and neck (7 patients).
Most lesions (n = 46, 83.8%) were invasive AHM (superficial spreading = 27; nodular = 14; desmoplastic melanoma = 3; lentigomaligna melanoma = 2). The remaining 3 lesions were in situ AHM. The median Breslow thickness of AHM was higher than pigmented MM (AHM = 1.7 mm interquartile range [IQR] = 3.50) versus 0.98 mm (IQR = 1.23) for pigmented MM).
Short white lines (Figure 1B) and milky-red areas (Figure 2B) were the most common dermoscopic findings in our cohort of AHM, observed in 39 lesions (79.6%) and 33 lesions (67.3%), respectively. Milky-red areas were present in similar frequencies in lesions ≤ 1 mm in thickness (70%) and lesions > 1 mm in thickness (63.9%) (Table 1).
Figure 1.
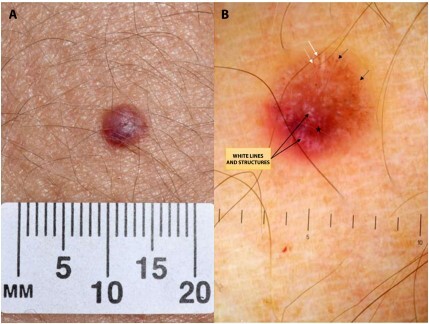
(A) Lesion on the forearm of a 46-year-old woman. A confirmed melanoma with Breslow thickness of 1.1 mm. (B) Dermoscopy shows dotted (black arrows) and looped (white arrows) vessels, milky red areas (stars), and white structures (long arrows).
Figure 2.
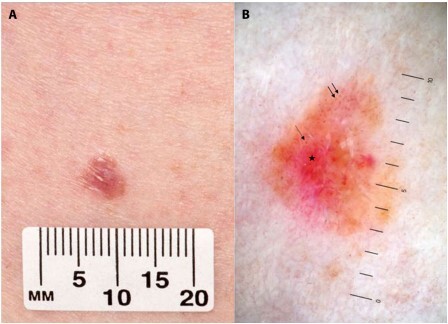
(A) Lesion on the lower leg of a 57-year-old woman. A confirmed melanoma with Breslow thickness of 3 mm. (B) Dermoscopy shows irregularly distributed dotted vessels (arrows), a milky red area (star), and a subtle remnant of pigment at the periphery.
Table 1.
Dermoscopic features of Amelanotic and hypomelanotic melanoma in our study
| Dermoscopic criteria | AHM ≤ 1mm in thickness (n = 10) | AHM > 1 mm in thickness (n = 36) | AHM in situ (n = 3) | Total AHM (n = 49) | ||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| Dotted vessels | 9 | 90.0 | 16 | 44.4 | 3 | 100 | 28 | 57.1 |
| Linear vessels | 5 | 50.0 | 23 | 63.9 | 3 | 100 | 31 | 63.2 |
| Looped vessels | 3 | 30.0 | 26 | 72.2 | 2 | 66.7 | 31 | 63.3 |
| Granular structures | 5 | 50.0 | 16 | 44.4 | 1 | 33.3 | 22 | 44.9 |
| Short white lines | 8 | 80.0 | 28 | 77.8 | 3 | 100 | 39 | 79.6 |
| Lacuna structures | 3 | 30.0 | 10 | 27.8 | 0 | 0 | 13 | 26.5 |
| Milky-red areas | 7 | 70.0 | 23 | 63.9 | 3 | 100 | 33 | 67.3 |
| Remnant pigment | 7 | 70.0 | 18 | 50.0 | 2 | 66.7 | 27 | 55.1 |
| Polymorphous vessels | 6 | 60.0 | 22 | 61.1 | 3 | 100 | 31 | 63.2 |
AHM = amelanotic and hypomelanotic melanomas.
In our study, 63.3% of AHM had more than one vascular pattern (Table 1). Dotted, linear, and looped vessels were present in 57.1%, 63.2%, and 63.3% of lesions, respectively. Dotted vessels were seen in 90% of AHM of < 1mm, compared with 44.4% of AHM of > 1mm.
Remnant pigment was present in 27 lesions (55.1%), and present in 70% of lesions ≤ 1mm in thickness and 50% of lesions > 1 mm in thickness. Gray granular structures and lacunae were less frequently seen, found in 44.9% and 26.5% of lesions, respectively.
Discussion
Short white lines were the most common finding in our cohort, seen in 79.6% of cases. This is higher than reported observations at 30.8% [1]. We assume reviewing magnified images on the monitor contributed to better visualization of these subtle features.
The incidence of milky-red areas in our study (67.3%) was close to the incidence reported in the literature at 54.5% [2,3]. Also, polymorphic vessels, an important distinguishing feature in AHM, were present in over 50% of our AHM cases.
Dotted vessels were present in nearly half of our cases. This was similar to the incident reported in the literature [1]). Zalaudeket al reported a strong association between dotted vessels and AHM with Breslow thickness less than 1 mm [4]. Our study supports this observation.
Conclusions
Our study reinforces the findings that polymorphic vessels and milky-red areas are common features of AHM. In addition, our study indicates that short white lines are also common and helpful predictive feature. Clinicians should be aware of these dermoscopic findings when non-specific lesions are encountered.
Acknowledgement
We thank the Medical Illustration Department at Aneurin Bevan University Health Board for providing the teledermatology service.
Footnotes
Funding: None.
Competing interests: None.
Authorship: All authors have contributed significantly to this publication.
References
- 1.Paolino G, Bearzi P, Pampena R, et al. Clinicopathological and dermoscopic features of amelanotic and hypomelanotic melanoma: a retrospective multicentric study. Int J Dermatol. 2020;59(11):1371–1380. doi: 10.1111/ijd.15064. [DOI] [PubMed] [Google Scholar]
- 2.Pizzichetta MA, Talamini R, Stanganelli I, et al. Amelanotic/hypomelanotic melanoma: clinical and dermoscopic features. Br J Dermatol. 2004;150(6):1117–1124. doi: 10.1111/j.1365-2133.2004.05928.x. [DOI] [PubMed] [Google Scholar]
- 3.Lin MJ, Xie C, Pan Y, Jalilian C, Kelly JW. Dermoscopy improves diagnostic accuracy for clinically amelanotic nodules. Australas J Dermatol. 2019;60(1):45–49. doi: 10.1111/ajd.12902. [DOI] [PubMed] [Google Scholar]
- 4.Zalaudek I, Kreusch J, Giacomel J, Ferrara G, Catricalà C, Argenziano G. How to diagnose nonpigmented skin tumors: a review of vascular structures seen with dermoscopy: part I. Melanocytic skin tumors. J Am Acad Dermatol. 2010;63(3):361–374. doi: 10.1016/j.jaad.2009.11.698. [DOI] [PubMed] [Google Scholar]


