Abstract
Background
Subjective social status (SSS) has shown inverse relationships with cardiometabolic risk, but intersectionalities of race/ethnicity and sex may indicate more nuanced relationships.
Purpose
To investigate associations of SSS with cardiometabolic risk markers by race/ethnicity and sex.
Methods
Data were from Wave IV (2008) of the National Longitudinal Study of Adolescent to Adult Health (n = 4,847; 24–32 years), which collected biological cardiometabolic risk markers. A 10-step ladder captured SSS; respondents indicated on which step they perceived they stood in relation to other people in the U.S. higher values indicated higher SSS (range: 1–10). We tested the relationship between SSS and individual markers using generalized least square means linear regression models, testing three-way interactions between SSS, race/ethnicity, and sex (p < .10) before stratification.
Results
SSS–race/ethnicity–sex interactions were significantly associated with waist circumference (p ≤ .0001), body mass index (BMI; p ≤ .0001), systolic blood pressure (SBP; p ≤ .0001), diastolic blood pressure (DBP; p = .0004), and high-density lipoprotein cholesterol (HDL-C; p = .07). SSS was associated with waist circumference (β [SE]: −1.2 (0.4), p < .05) and BMI (−0.6 [0.2], p < .01) for non-Hispanic White females, compared with males; with HDL-C among non-Hispanic White (0.2 [0.1]; p < .05) and Hispanic (0.3 (0.1); p < .05) females, compared with males; with SBP for non-Hispanic Asian (1.7 [0.8]; p < .05) and Multiracial (1.8 [0.8]; p < .05), versus White, females; and with DBP for non-Hispanic Black (0.8 [0.3]; p < .01), versus White, males.
Conclusions
SSS was differentially related to cardiometabolic risk markers by race/ethnicity and sex, suggesting intersectional aspects. Clinical and research applications of SSS should consider race/ethnicity- and sex-specific pathways influencing cardiometabolic risk.
Keywords: Subjective social status, Cardiovascular risk, Metabolic risk, Sex, Race, Ethnicity
Young White women with higher levels of subjective social status had smaller waist circumference and lower systolic blood pressure, but higher subjective social status was not as protective for young White men, Asian women, or Multiracial women.
Introduction
Cardiovascular diseases affect 48.0% of U.S. adults over the age of 19 years, accounting for an estimated $351.2 billion in annual direct and indirect costs [1]. Non-Hispanic Black (NHB) females and Mexican American females evidence worse cardiovascular health, as defined by the American Heart Association’s Life’s Simple 7, compared with their non-Hispanic White (NHW) female counterparts [2]. Furthermore, disparities in cardiovascular health between NHW adults and NHB and Mexican American adults have continued over the past two decades [3]. Similarly, although 9.8% of U.S. adults aged ≥20 years old have diagnosed diabetes [1], prevalence differs by sex and race/ethnicity, with greater prevalence among Black males (14.7%) and females (13.4%), Hispanic males (15.1%) and females (14.1%), and Asian males (12.8%), compared with White males (9.4%) and females (7.3%) [1]. Racial and ethnic disparities in cardiometabolic diseases in the United States will cost the healthcare system $50 billion by 2050 if not addressed [4], warranting interdisciplinary approaches to elucidate the complex factors that influence the health of diverse U.S. populations.
Socioeconomic status (SES) is known to have an inverse, graded relationship with cardiometabolic diseases [5]. However, the nature of this relationship may vary by race/ethnicity and by sex [6–8]. For example, in a cohort of diverse U.S. adults (45–84 years), SES was inversely associated with diabetes, hypertension, and body mass index (BMI) for White and Black women and White men and with diabetes for Hispanic women and men, but these relationships were inconsistent for Black men and Chinese women and men [6]. Other research also demonstrates that even after adjusting for SES, racial/ethnic disparities in health persist [9]. Employing an assessment of one’s “perception of his/her own position in the social hierarchy” [10], or subjective social status (SSS), may provide more nuanced insights into cardiometabolic risk disparities. As often assessed in terms of subjective status in relation to “greater society” (e.g., United States) [11, 12], SSS is hypothesized to be a unique factor influencing physical health, above and beyond objective SES [13]. This additive influence of SSS could be linked to social processes, such as social conflicts [14], or to psychological processes, including negative affect [11], underscoring the potential utility of SSS as a tool for understanding health disparities [13]. SSS may also capture accumulated social status experiences over the life course [15], which is important to understanding social patterning in health [16].
SSS has shown a strong positive association with self-rated health; a moderate inverse relationship with biological, symptom-specific health; and a moderate positive relationship with self-reported physical health, independent of objective measures of SES [13]. Moreover, in a meta-analysis, cumulative effect sizes of SSS in relation to physical health were significantly larger for Blacks compared with Whites (0.071 vs. 0.031) and for women compared with men (0.047 vs. 0.023) [13]. Self-perception of social status may connect objective SES to biological risk, as low-SES individuals likely develop lower thresholds for social threat interpretations which can negatively affect the neuroendocrine system and eventually disrupt cardiometabolic biomarkers [17]. A recent systematic review and meta-analysis also documented that among adults (≥33 years), SSS was inversely associated with coronary artery disease, hypertension, diabetes, and dyslipidemia, although only SSS and dyslipidemia were robust to adjustment for objective SES. Yet, this review also found that associations between SSS and hypertension, diabetes, and obesity were strongest among mostly (≥75%) White samples compared with mostly non-White samples [18]. Furthermore, race/ethnicity of study participants partially explained heterogeneity between studies on SSS and cardiovascular disease risk [18], indicating potential racial/ethnic distinctions in the SSS–cardiometabolic risk relationship and in what contributes to SSS.
Race/Ethnicity Differences in Subjective Social Status and Its Correlates
Race and ethnicity are likely intertwined with SSS, as SES is typically correlated with race/ethnicity [19]. Several studies with diverse samples of participants indicate that White and Black adults have higher SSS compared with Hispanic and Asian adults [20–22] and that relationships between SSS and objective SES are stronger for White and Asian adults, weaker for Hispanic adults, and weakest for Black adults. These relationships have been shown in women-exclusive cohorts [20] and studies of all genders [21], with no reports in the literature exclusively for men. Traditional objective SES experiences may not qualitatively have the same meaning and value for racial/ethnic groups with unique or marginalized histories, compared with their White counterparts [20, 23, 24], which underscores the potential utility of SSS in elucidating nuances in social determinants of health [21]. Several studies, including a meta-analysis, documented higher SSS scores for Black compared with White adults and SSS appeared to be less closely aligned with objective resources for Blacks compared with Whites [13, 25]. Instead, research suggests non-SES factors, such as resilience [26], lower anxiety and negative affect [27], higher language acculturation [28, 29], and general social trust [29], may be stronger determinants of higher SSS among NHB and Hispanic adults. In contrast, objective SES constructs have been positively associated with SSS [30] among Asian adults in the United States. Franzini and Fernandez-Esquer concluded that while objective SES is likely still a salient factor determining SSS, the most marginalized groups rely least on objective SES to inform their SSS rankings. Thus, exploring how race/ethnicity influences the relationship between SSS and health is warranted [20].
Intersectional Race/Ethnicity and Sex Differences in Subjective Social Status and Its Correlates
Further obscuring the relationships between SSS and physical health outcomes within racial/ethnic groups is the potential intersectionality with sex. The term “intersectionality” was coined in 1989 by Kimberlé Crenshaw [31] and was adopted as an approach to better capture the complexities of interacting facets of a person’s identity on discriminatory experiences [32, 33]. Multiple group identities function in a synergistic way to shape health; for example, individuals having membership in more than one disadvantaged category (e.g., low social status, racial/ethnic minority, female, sexual minority, disabled person, immigrant) may experience an additive negative effect on health and disease risk [9, 34]. Additionally, they may be less likely to gain health benefits from attaining a more privileged SES position [17]. Health disparities scholars have used an intersectional approach to capture nuances in health risk [35], including cardiovascular disease risk, because the implications of identity intersections on health cannot be realized in isolation from each other [35]. The same argument could be made for SSS, as the salience of objective SES on rankings of SSS and the influence of SSS on health also appear to differ by sex. Some studies documenting sex differences in SSS have shown that men tend to rank themselves higher on the SSS ladder compared women and that traditional SES markers are more strongly related to SSS for men than women [36–38]. SSS has also been shown to be more strongly correlated with household financial situation and less strongly correlated with personal income [39] among women, compared with men. However, although SSS rankings do not appear to differ by sex among more racially/ethnically diverse U.S. samples [25, 27, 28, 40, 41], sex differences in SES and non-SES contributions to SSS have been studied less [25, 40]. Among Black and White adults (30–64 years) in Baltimore, SSS rankings did not differ by sex, yet being employed, compared with unemployed, was associated with higher SSS among men but not among women [25].
Intersectional Race/Ethnicity and Sex Differences in the Relationship of Subjective Social Status With Cardiometabolic Risk
The SSS–cardiometabolic risk relationship is likely to intersect differentially by race/ethnicity and sex because systems of social inequality shape how individuals perceive and experience the world [34, 35], ultimately affecting how individuals behave and their subsequent health outcomes. For example, a study of Black and White young- to middle-aged U.S. adults (33–48 years) documented an inverse relationship between SSS and hypertension only for White men [42], and a study among U.S. Black adults (21–95 years) showed an inverse association between SSS and insulin resistance among women, but not men [40]. Williams et al. argued that investigating the complex means by which social status, race/ethnicity, and sex impact health should be a research priority to progress our understanding of disease patterning [9] and may further help identify subgroups in which SSS may be an appropriate target for behavioral interventions aimed to equitably improve cardiometabolic health. In aggregate, these findings underscore the need for additional research that considers intersectional distinctions in SSS–cardiometabolic risk relationships by race/ethnicity and sex.
The Present Study
The National Longitudinal Study of Adolescent to Adult Health (Add Health) provides a unique opportunity to investigate race/ethnicity and sex intersectionality potentially differentiating SSS–cardiometabolic risk relationships, as the cohort comprises a diverse sample of U.S. young adults for whom cardiometabolic disease prevention is warranted. Previous work in the cohort showed that mean SSS in relation to U.S. society did not differ by sex [43]. SSS was inversely associated with BMI, and this association was partially explained (48.6%) by both respondent and parental objective SES indicators [44]. The authors concluded that SSS seems to encapsulate social and economic aspects of the lived experience that are not captured by traditional objective SES [44]. SSS was also inversely associated with hsCRP, independent of objective SES measures, but only among males [43]. Yet, these studies did not consider both sex and race/ethnicity differences, which may help elucidate nuances that can inform how to conceptualize and address health disparities. An investigation of life course SES and a cardiovascular risk score in Add Health found stark heterogeneity by race/ethnicity and sex [45], and Perreira et al. previously observed in Add Health that darker (interviewer-ascribed) skin color was associated with higher BMI and odds of obesity among women but not men [46]. These findings further justify the need for an intersectional approach, considering both race/ethnicity and sex. Thus, the objective of our study was to investigate the cross-sectional associations of SSS in relation to others in the United States with cardiometabolic risk markers (waist circumference, BMI, blood pressure, high-density lipoprotein cholesterol (LDL-C), triglycerides (TG), hsCRP, glycated hemoglobin, and glucose) by both race/ethnicity and sex in the Add Health cohort.
Methods
Participants
We used publicly available cross-sectional data from Wave IV of the National Longitudinal Study of Adolescent to Adult Health (Add Health), a nationally representative sample of U.S. adolescents beginning in grades 7–12 during the 1994–1995 school year (n = 20,745) and followed up through 2016–2018 (Wave V) [47]. The purpose of Add Health is to investigate multi-level influences on adolescent health, health behaviors, and well-being and how these relate to health and well-being during transition into adulthood. Wave IV, conducted in 2008, sought to investigate trajectories of development and health from adolescence to young adulthood (24–32 years), and was the first time that biological markers of health and disease were incorporated (n = 5,114) [47]. Data for the current analyses were secondary and had no personal identifiers; thus, the analyses were exempt from Institutional Review Board approval.
Race/Ethnicity
In Wave I, respondents self-reported Hispanic or Latino ethnicity and race (White, Black or African American, American Indian or Native American, Asian or Pacific Islander, or Other). If respondents reported Hispanic/Latino or Asian/Pacific Islander race/ethnicity, they were then asked about their specific heritage (e.g., Mexican/Mexican American, Cuban/Cuban American, Chinese, Filipino). We used this self-reported race/ethnicity data to categorize respondents into the following mutually exclusive categories: NHW, NHB, non-Hispanic Asian/Pacific Islander (NHA), non-Hispanic Multiracial (NHM), and Hispanic. Because there were few respondents reporting American Indian or Native American (n = 23) or Other (n = 55), they were excluded from the analyses to ensure adequate power to detect potential interactions with SSS, race/ethnicity, and sex.
Subjective Social Status
Computer-assisted interviews were used to administer the survey portion of data collection, including SSS. SSS was assessed using the original MacArthur Scale of SSS [11, 12]. Respondents were given a drawing of a ladder with 10 rungs, with the following instructions [11]: “Think of this ladder as representing where people stand in the United States. At the top of the ladder (step 10) are the people who have the most money and education, and the most respected jobs. At the bottom of the ladder (step 1) are the people who have the least money and education, and the least respected jobs or no job. Where would you place yourself on this ladder? Pick the number for the step that shows where you think you stand at this time in your life, relative to other people in the United States.” Thus, SSS was appraised within a range of 1–10, with higher steps (values) on the ladder indicating higher perceived social status and lower steps (values) on the ladder indicating lower perceived social status. For descriptive purposes, we created a categorical variable for SSS based on the median score (4.5) for the sample: <5, 5, >5.
Cardiometabolic Measures
Immediately after completing the survey, interviewers collected physical measurements and biological specimens, using standardized protocols, including height (cm), weight (kg), waist circumference (cm), and systolic and diastolic blood pressure (SBP and DBP; mmHg). Measured height and weight were used to calculate BMI as kg/m2. Blood pressure was measured three times with a validated automatic device, and the second and third measures were averaged [48]. Respondents provided dried blood spots for total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), LDL-C, TC-HDL-C ratio (TC-HDL), TG, hsCRP (mg/L), glycated hemoglobin (HbA1c; %), and glucose (mg/dL) [49]. All lipid values were rank ordered and categorized into deciles, with higher deciles representing higher values [50].
Covariates
Covariates we considered included sex, age, childhood household income, maternal educational attainment, household income, educational attainment, depression, and perceived discrimination. We used household income and the respondent’s maternal educational attainment, both reported at Wave 1, to account for life course SES. Respondents self-reported whether or not they had ever been diagnosed with depression. Perceived discrimination was captured with the general question, “In your day-to-day life, how often do you feel you have been treated with less respect or courtesy than other people,” with response options never, rarely, sometimes, or often.
Analyses
Our analytical sample included females and males at Wave IV of data collection. We excluded respondents (n = 267) who were missing race/ethnicity data, reported race/ethnicity as American Indian or Native American or Other, or reported being pregnant. Of the respondents in our analytical sample (n = 4847), the following proportion of analytical variables were missing completely at random or at random: 0.02% (age, depression, education), 0.2% (SSS), 1% (waist circumference, BMI), 3% (SBP, DBP), 7% (Wave IV income), 9% (maternal education, HbA1c), 11% (glucose, hsCRP), 12% (TC), 13% (HDL-C, TC-HDL-C ratio), 17% (LDL), and 23% (Wave I income). These missing data were imputed with multiple imputation for chained equations using classification and regression trees. We first tested unadjusted differences in participants’ characteristics by race/ethnicity and by SSS category using Rao-Scott chi-square tests for categorical variables and ANOVA for continuous variables. Next, we tested unweighted correlations between SSS and objective SES measures for the analytical sample and by sex and race/ethnicity of the analytical sample. We then used generalized least square means linear regression to test the intersectional relationships of objective SES with SSS by including a three-way interaction term between each objective SES indicator, sex, and race/ethnicity, adjusted for age and depression. The generalized least square means procedure is both robust in smaller sample sizes (e.g., 50) and provides control over Type-1 error, providing adequate power to detect main and interaction effects that were of interest [51]. Models with significant interactions were stratified by sex and race/ethnicity to estimate mean SSS by each level of the SES indicator. Next, we used generalized least square means linear regression to test relationships between SSS and individual cardiometabolic risk markers. HbA1c, glucose, and hsCRP values were log-transformed to restore normality. Because of potential distinctions of the SSS–cardiometabolic risk relationship by race/ethnicity and sex, we tested a three-way interaction between SSS, race/ethnicity, and sex. As some sample sizes by race/ethnicity were small, significance was set at p < .10 for three-way interactions. Linear regression models with significant interactions were stratified first by sex and then by race/ethnicity, to further explore the interactions. When models were stratified by race/ethnicity we included an interaction term between SSS and sex. When models were stratified by sex, we included an interaction term between SSS and race/ethnicity. This approach parallels previous analyses in Add Health that stratified models by race/ethnicity and included a SES–sex interaction to investigate race/ethnicity and sex differences in the relationship between life course SES and cardiovascular risk [45]. Model 1 was adjusted for age, sex, and race/ethnicity. Model 2 was adjusted for Model 1 covariates plus childhood household income (reported by parents at Wave 1), maternal educational attainment (reported at Wave 1), household income, and educational attainment. Childhood household income and maternal educational attainment captured SES in childhood, which has been found to contribute to SSS rankings later in life [15], including in the Add Health cohort [44]. Depression and perceived discrimination were tested in all models and retained if significant or if they appreciably changed the SSS–cardiometabolic risk relationship. Depression is often associated with both SSS and cardiometabolic risk markers, and previous work in Add Health demonstrated that depression is likely not on the pathway between SSS and hsCRP [43] or SSS and BMI [44], indicating it may instead be a confounder. All statistical tests accounted for complex survey design and sampling weights using SAS version 9.4. Significance was set at p < .05 for main effects.
Results
Participant Characteristics
Socioeconomic characteristics, lifestyle behaviors, and health outcomes differed by race/ethnicity for females (Table 1) and males (Table 2). Mean SSS among females differed by race/ethnicity, with NHM having the lowest and NHA having the highest SSS. NHA females tended to have higher household income, and NHW and NHA females tended to have higher educational attainment. All cardiometabolic markers varied significantly by race/ethnicity. NHA had the smallest mean waist circumference and smallest proportion classified with obesity, whereas NHB and NHM females had the highest mean waist circumference and highest proportion classified with obesity. NHB females had the highest mean SBP and DBP, HbA1c, and hsCRP, and the lowest mean TG decile and TC decile. NHA females had the lowest mean SBP, DBP, and hsCRP and the highest mean TC decile and LDL decile.
Table 1.
Weighted characteristics by race/ethnicity for females in Wave IV of the National Longitudinal Study of Adolescent to Adult Health Study (2008)
| Non-Hispanic White | Non-Hispanic Black | Non-Hispanic Asian/Pacific Islander | Hispanic | Non-Hispanic Multiracial | ||
|---|---|---|---|---|---|---|
| Characteristic | (n = 1,503) | (n = 604) | (n = 62) | (n = 263) | (n = 99) | p-value |
| Age | 28.2 (28.0–28.5) | 28.5 (28.1–28.9) | 28.9 (28.3–29.5) | 28.2 (27.8–28.7) | 28.2 (27.7–28.6) | .12 |
| Subjective social status scalea | 5.0 (4.9–5.2) | 4.8 (4.6–5.0) | 5.7 (5.3–6.2) | 4.8 (4.5–5.0) | 4.1 (3.7–4.5) | <.0001 |
| Household income at Wave I | <.0001 | |||||
| ≤$22,000 | 18.7 (15.8–21.6) | 46.2 (40.3–52.1) | 25.9 (14.5–37.2) | 40.0 (33.8–46.2) | 26.4 (12.7–40.0) | |
| $22,001–$40,000 | 28.5 (25.6–31.4) | 28.0 (24.0–32.0) | 20.0 (8.5–31.5) | 33.9 (28.2–39.6) | 27.0 (15.7–38.3) | |
| $40,001–$60,000 | 27.0 (24.2–29.7) | 14.3 (10.7–17.9) | 34.4 (21.3–47.6) | 14.7 (10.5–18.9) | 31.8 (20.0–43.5) | |
| ≤$60,000 | 25.8 (21.6–30.0) | 11.5 (7.4–15.5) | 19.7 (7.8–31.6) | 11.4 (7.8–31.6) | 14.9 (6.5–23.2) | |
| Household income | <.0001 | |||||
| ≤$39,999 | 33.7 (30.1–37.2) | 59.8 (53.7–65.8) | 24.8 (13.9–35.6) | 35.2 (28.3–42.1) | 51.7 (38.6–64.7) | |
| $40,000–$74,999 | 37.0 (33.9–40.0) | 27.8 (23.6–31.9) | 24.4 (11.5–37.4) | 36.4 (30.1–42.8) | 24.5 (14.0–35.1) | |
| ≥$75,000 | 29.4 (25.8–32.9) | 12.5 (7.7–17.2) | 50.8 (37.5–64.2) | 28.4 (22.0–34.8) | 23.8 (13.7–33.9) | |
| Maternal educational attainment | <.0001 | |||||
| Less than high school diploma/GED | 10.9 (8.6–13.1) | 16.0 (11.4–20.6) | 22.5 (9.2–35.9) | 43.7 (36.6–50.9) | 21.5 (11.3–31.7) | |
| High school diploma/GED | 46.7 (42.8–50.5) | 49.7 (43.5–55.9) | 17.7 (6.7–28.7) | 34.7 (28.4–41.0) | 42.9 (29.2–56.5) | |
| Some college | 13.0 (10.9–15.1) | 14.2 (10.2–18.3) | 9.9 (3.1–16.6) | 10.6 (6.4–14.8) | 15.2 (6.8–23.5) | |
| College graduate or higher | 29.5 (25.5–33.5) | 20.0 (15.3–24.7) | 49.9 (34.2–65.6) | 11.0 (6.3–15.7) | 20.5 (11.0–30.0) | |
| Educational attainment | <.0001 | |||||
| Vocational/technical training or less | 26.1 (22.7–29.5) | 39.1 (32.0–46.3) | 19.9 (8.1–31.6) | 43.4 (36.4–50.4) | 35.6 (25.1–46.0) | |
| Some college | 35.5 (32.1–38.9) | 35.7 (31.2–40.2) | 29.7 (17.4–42.1) | 34.1 (27.3–40.9) | 43.6 (32.8–54.4) | |
| College graduate or higher | 38.4 (33.8–42.9) | 25.2 (18.5–31.9) | 50.4 (31.9–69.0) | 22.5 (16.0–29.1) | 20.8 (10.0–31.6) | |
| Ever diagnosed with depression | 25.8 (22.9–28.8) | 13.4 (9.9–16.8) | 12.3 (1.9–22.8) | 18.2 (12.6–23.8) | 36.1 (24.7–47.5) | <.0001 |
| Perceived discriminationb | .01 | |||||
| Never | 31.5 (29.1–22.8) | 31.6 (26.1–37.2) | 21.7 (11.2–32.2) | 33.6 (26.9–40.2) | 18.5 (10.1–27.0) | |
| Rarely | 44.8 (42.1–47.5) | 36.8 (32.5–41.0) | 50.7 (34.7–66.6) | 38.1 (31.0–45.3) | 45.7 (34.2–57.1) | |
| Sometimes/Often | 23.7 (21.2–26.2) | 31.6 (26.7–36.5) | 27.6 (16.7–38.5) | 28.3 (21.1–35.5) | 35.8 (22.2–49.4) | |
| Waist circumference (cm) | 96.3 (94.9–97.7) | 102 (100–104) | 89.6 (84.2–95.1) | 95.8 (93.6–98.0) | 102 (97.8–106) | <.0001 |
| Body mass index category | <.0001 | |||||
| Underweight (<18.5 kg/m2) | 2.2 (1.4–3.0) | 1.3 (0.3–2.3) | 3.4 (0–10.2) | 1.8 (0.1–3.4) | 1.3 (0–3.7) | |
| Normal (18.5–24.9 kg/m2) | 38.9 (35.0–42.8) | 20.3 (16.7–23.8) | 46.3 (27.9–64.7) | 30.0 (23.7–36.3) | 27.9 (17.3–38.5) | |
| Overweight (25–29.9 kg/m2) | 23.6 (20.5–26.6) | 25.8 (21.8–29.9) | 31.8 (17.1–46.5) | 27.3 (21.5–33.1) | 21.8 (12.7–30.9) | |
| Obesity (≥30 kg/m2) | 35.3 (32.0–38.6) | 52.6 (48.9–56.4) | 18.5 (7.8–29.2) | 40.9 (33.6–48.1) | 49.1 (36.4–61.8) | |
| Systolic blood pressure (mmHg) | 120 (119–121) | 125 (123–126) | 117 (113–121) | 119 (117–121) | 119 (116–122) | <.0001 |
| Diastolic blood pressure (mmHg) | 77.0 (76.4–77.7) | 80.2 (78.9–81.6) | 76.3 (73.9–78.6) | 76.5 (74.7–78.3) | 77.4 (75.1–79.7) | .0002 |
| Triglyceride decilec | 5.1 (4.9–5.3) | 4.0 (3.8–4.3) | 4.9 (3.9–6.0) | 5.4 (5.0–5.7) | 5.2 (4.6–5.7) | <.0001 |
| Total cholesterol decilec | 5.5 (5.4–5.7) | 4.8 (4.5–5.1) | 5.7 (5.0–6.4) | 5.1 (4.6–5.5) | 5.1 (4.4–5.8) | .0004 |
| High-density lipoprotein cholesterol decilec | 6.0 (5.8–6.2) | 5.6 (5.4–5.9) | 5.9 (5.2–6.6) | 5.4 (5.0–5.8) | 5.9 (5.2–6.6) | .04 |
| Low-density lipoprotein cholesterol decilec | 5.5 (5.3–5.6) | 5.1 (4.9–5.4) | 5.7 (4.9–6.4) | 5.1 (4.7–5.5) | 5.0 (4.3–5.6) | .08 |
| Total cholesterol–HDL-C ratio decilec | 5.0 (4.9–5.2) | 4.8 (4.5–5.1) | 5.1 (4.3–5.9) | 5.3 (4.8–5.7) | 4.7 (4.1–5.3) | .28 |
| Glucose (mg/dL) | 104 (102–105) | 104 (100–109) | 107 (98.3–115) | 107 (103–111) | 110 (104–117) | .20 |
| Glycated hemoglobin (%) | 5.4 (5.4–5.5) | 5.9 (5.8–6.0) | 5.7 (5.4–5.9) | 5.6 (5.5–5.6) | 5.6 (5.4–5.7) | <.0001 |
| C-reactive protein (mg/L) | 5.6 (5.2–6.0) | 7.9 (6.8–9.0) | 4.0 (2.4–5.5) | 6.7 (5.2–8.3) | 6.5 (4.8–8.1) | .0001 |
Data shown as (mean [95% CI] or % [95% CI]). CI confidence interval; HDL-C high-density lipoprotein cholesterol.
aHigher steps on the subjective social status ladder indicate higher perceived social status. Lower steps on the ladder indicate lower perceived social status (range: 1–10).
bResponse to the question, “In your day-to-day life, how often do you feel you have been treated with less respect or courtesy than other people?”
cValues were rank ordered and categorized into deciles. Higher deciles represent higher values (range: 1–10).
Table 2.
Weighted characteristics by race/ethnicity for males in Wave IV of the National Longitudinal Study of Adolescent to Adult Health Study (2008)
| Non-Hispanic White | Non-Hispanic Black | Non-Hispanic Asian/ Pacific Islander | Hispanic | Non-Hispanic Multiracial | ||
|---|---|---|---|---|---|---|
| Characteristic | (n = 1425) | (n = 497) | (n = 67) | (n = 245) | (n = 82) | p-value |
| Age, years | 28.4 (28.2–28.7) | 28.7 (28.2–29.2) | 28.5 (27.7–29.2) | 28.4 (27.9–28.9) | 28.3 (27.8–28.8) | .75 |
| Subjective social status scalea | 5.1 (4.9–5.2) | 4.7 (4.4–4.9) | 5.6 (5.3–5.9) | 4.9 (4.6–5.2) | 4.5 (4.9–5.2) | <.0001 |
| Household income at Wave I | <.0001 | |||||
| ≤$22,000 | 18.8 (14.7–22.9) | 46.9 (37.7–56.2) | 18.0 (7.8–28.1) | 49.0 (40.6–57.5) | 33.1 (20.4–45.8) | |
| $22,001–$40,000 | 29.1 (25.8–32.4) | 25.1 (19.9–30.2) | 21.2 (9.7–32.7) | 25.4 (19.5–31.4) | 27.5 (16.2–38.8) | |
| $40,001–$60,000 | 28.0 (25.4–30.6) | 16.5 (11.7–21.3) | 40.5 (24.6–56.5) | 19.6 (13.9–25.3) | 19.4 (9.0–29.8) | |
| ≤$60,000 | 24.1 (19.9–28.4) | 11.5 (7.8–15.2) | 20.3 (12.8–27.8) | 5.9 (2.4–9.4) | 20.0 (10.3–29.7) | |
| Household income | <.0001 | |||||
| ≤$39,999 | 28.8 (25.5–32.1) | 50.0 (44.6–55.4) | 13.4 (3.3–23.6) | 31.4 (25.1–37.8) | 32.9 (21.8–43.9) | |
| $40,000–$74,999 | 38.5 (35.7–41.3) | 31.3 (26.9–35.7) | 25.2 (14.2–36.2) | 34.8 (28.5–41.2) | 34.0 (23.9–44.2) | |
| ≥$75,000 | 32.7 (29.4–36.0) | 18.7 (13.2–24.3) | 61.4 (48.3–74.5) | 33.8 (26.9–40.6) | 33.1 (21.5–44.7) | |
| Maternal educational attainment | <0.0001 | |||||
| Less than high school diploma/GED | 9.4 (7.4–11.4) | 10.1 (6.5–13.7) | 17.8 (6.5–29.1) | 41.4 (33.1–49.8) | 16.0 (6.1–25.8) | |
| High school diploma/GED | 46.0 (42.0–50.1) | 51.5 (43.1–60.0) | 19.5 (11.7–27.3) | 33.1 (25.6–40.6) | 42.9 (30.9–54.8) | |
| Some college | 13.2 (11.1–15.3) | 12.5 (8.7–16.3) | 14.3 (4.1–24.5) | 10.6 (6.6–14.5) | 19.3 (9.4–29.3) | |
| College graduate or higher | 31.4 (26.6–36.1) | 25.9 (17.5–34.2) | 48.4 (37.2–59.6) | 14.9 (10.7–19.1) | 21.8 (12.1–31.6) | |
| Educational attainment | <.0001 | |||||
| Vocational/technical training or less | 40.1 (35.0–45.2) | 55.8 (44.9–66.6) | 15.9 (2.8–29.1) | 49.5 (43.8–55.3) | 40.5 (26.4–54.6) | |
| Some college | 30.2 (27.2–33.1) | 26.8 (20.5–33.0) | 27.3 (16.0–38.7) | 35.6 (29.2–42.0) | 32.3 (21.0–43.5) | |
| College graduate or higher | 29.7 (24.1–35.3) | 17.5 (10.7–24.3) | 56.8 (45.5–68.1) | 14.9 (9.5–20.3) | 27.2 (16.0–38.5) | |
| Ever diagnosed with depression | 12.4 (10.4–14.3) | 5.9 (3.6–8.1) | 6.4 (0–13.5) | 9.3 (5.5–13.2) | 10.5 (2.7–18.3) | .01 |
| Perceived discriminationb | .07 | |||||
| Never | 29.2 (26.7–31.8) | 29.6 (24.3–35.0) | 37.8 (21.6–53.9) | 37.3 (29.6–44.9) | 26.9 (15.7–38.1) | |
| Rarely | 47.8 (44.7–50.9) | 41.4 (36.2–46.6) | 46.5 (30.5–62.5) | 39.1 (32.6–45.6) | 50.0 (37.4–62.5) | |
| Sometimes/often | 23.0 (20.4–25.6) | 29.0 (23.7–34.2) | 15.7 (4.7–26.8) | 23.6 (19.0–28.2) | 23.1 (13.0–33.3) | |
| Waist circumference (cm) | 99.9 (99.0–101) | 99.5 (97.4–102) | 92.4 (89.4–95.3) | 102 (99.9–105) | 97.9 (94.6–101) | <.0001 |
| Body Mass Index category | .04 | |||||
| Underweight or normal (<24.9 kg/m2) | 29.5 (26.6–32.5) | 31.2 (25.2–37.1) | 33.2 (22.4–44.0) | 18.9 (13.9–23.8) | 28.2 (16.8–39.5) | |
| Overweight (25–29.9 kg/m2) | 35.8 (32.8–38.9) | 33.3 (28.3–38.3) | 41.7 (27.3–56.1) | 37.8 (31.9–43.7) | 37.8 (25.3–50.3) | |
| Obesity (≥30 kg/m2) | 34.6 (31.8–37.5) | 35.5 (30.7–40.3) | 25.1 (13.9–36.3) | 43.3 (36.7–50.0) | 34.0 (23.2–44.8) | |
| Systolic blood pressure, mmHg | 130 (129–131) | 130 (129–132) | 131 (128–135) | 130 (128–132) | 130 (126–133) | .95 |
| Diastolic blood pressure, mmHg | 82.0 (81.4–82.6) | 81.6 (80.2–83.0) | 81.9 (80.5–83.5) | 82.0 (80.5–83.5) | 81.1 (78.1–84.1) | .97 |
| Triglyceride decilec | 6.3 (6.1–6.5) | 4.9 (4.6–5.1) | 6.4 (5.6–7.1) | 6.6 (6.3–7.0) | 5.9 (5.0–6.8) | <.0001 |
| Total cholesterol decilec | 5.7 (5.5–5.9) | 5.3 (5.0–5.6) | 5.7 (4.9–6.6) | 5.5 (5.1–5.9) | 5.2 (4.5–5.8) | .27 |
| High-density lipoprotein cholesterol decilec | 5.0 (4.8–5.2) | 5.1 (4.7–5.6) | 4.5 (3.6–5.4) | 4.5 (4.1–5.0) | 4.6 (3.9–5.3) | .25 |
| Low-density lipoprotein cholesterol decilec | 5.6 (5.4–5.8) | 5.4 (5.1–5.8) | 5.8 (5.1–6.5) | 5.3 (4.9–5.7) | 5.2 (4.5–5.8) | .55 |
| Total cholesterol–HDL-C ratio decilec | 6.1 (5.9–6.3) | 5.6 (5.2–6.0) | 6.6 (5.9–7.4) | 6.3 (5.9–6.7) | 5.9 (5.2–6.5) | .09 |
| Glucose, mg/dL | 110 (109–112) | 108 (103–113) | 108 (102–114) | 114 (107–122) | 109 (106–112) | .48 |
| Glycated hemoglobin, % | 5.5 (5.5–5.6) | 6.0 (5.8–6.1) | 5.6 (5.5–5.7) | 5.8 (5.6–6.0) | 5.7 (5.6–5.8) | <.0001 |
| C-reactive protein, mg/L | 3.1 (2.8–3.4) | 4.2 (3.2–5.2) | 1.8 (1.3–2.4) | 4.0 (3.2–4.9) | 3.0 (1.9–4.1) | .0002 |
Data shown as (mean [95% CI] or % [95% CI]). CI confidence interval; HDL-C high-density lipoprotein cholesterol.
aHigher steps on the subjective social status ladder indicate higher perceived social status. Lower steps on the ladder indicate lower perceived social status (range: 1–10).
bResponse to the question, “In your day-to-day life, how often do you feel you have been treated with less respect or courtesy than other people?”
cValues were rank ordered and categorized into deciles. Higher deciles represent higher values (range: 1–10).
Among males, NHA males had the highest and NHM males had the lowest mean SSS. NHA males also tended to report higher household income and educational attainment compared with all other racial/ethnic groups. Some cardiometabolic markers also differed by race/ethnicity for males. NHA males had the lowest mean waist circumference and the lowest proportion classified with obesity, whereas Hispanic males had the highest mean waist circumference and the highest proportion classified with obesity. NHA males also had the lowest mean hsCRP and highest mean TG decile, whereas NHB males had the highest mean hsCRP and the lowest mean TG decile. NHB males also had the highest mean HbA1c.
Socioeconomic characteristics and health outcomes also differed by SSS score (Table 3). Individuals reporting low (<5) SSS scores tended to report lower household income and lower educational attainment, and to be NHB or NHM. Individuals with low SSS also had a higher proportion of having been diagnosed with depression and to having sometimes or often experienced perceived discrimination. Those reporting low SSS also tended to be classified with obesity and had higher mean waist circumference, SBP, DBP, TG decile, HbA1c, and hsCRP.
Table 3.
Weighted characteristics by subjective social status score for adults in Wave IV of the National Longitudinal Study of Adolescent to Adult Health Study (2008)
| Subjective Social Status Scorea | ||||
|---|---|---|---|---|
| <5 | 5 | >5 | ||
| Characteristic | n = 1,796 | n = 1,313 | n = 1,738 | p-value |
| Age, years | 28.4 (28.1–28.6) | 28.3 (28.0–28.5) | 28.5 (28.2–28.7) | .11 |
| Female | 47.2 (44.6–49.8) | 51.3 (48.5–54.1) | 45.5 (42.2–48.8) | .02 |
| Household income at Wave I | <.0001 | |||
| ≤$22,000 | 47.2 (43.7–50.7) | 27.1 (24.9–29.4) | 25.7 (22.6–28.7) | |
| $22,001–$40,000 | 40.8 (37.5–44.1) | 29.4 (26.4–32.3) | 29.8 (26.9–32.8) | |
| $40,001–$60,000 | 34.1 (30.9–37.2) | 26.6 (23.8–29.3) | 39.4 (35.9–42.8) | |
| ≤$60,000 | 25.1 (21.4–28.8) | 24.1 (20.7–27.5) | 50.8 (46.0–55.5) | |
| Household income | <.0001 | |||
| ≤$39,999 | 50.7 (48.0–53.5) | 31.9 (28.7–35.2) | 20.7 (17.4–24.1) | |
| $40,000–$74,999 | 35.2 (33.0–37.3) | 40.3 (36.8–43.8) | 32.8 (29.8–35.8) | |
| ≥$75,000 | 14.1 (12.1–16.1) | 27.8 (24.7–30.8) | 46.5 (43.2–49.8) | |
| Maternal educational attainment | <.0001 | |||
| Less than high school diploma/GED | 19.1 (16.4–21.7) | 15.8 (12.5–19.2) | 9.1 (6.9–11.2) | |
| High school diploma/GED | 48.6 (45.7–51.5) | 46.6 (43.2–50.0) | 39.5 (35.3–43.7) | |
| Some college | 12.0 (10.4–13.6) | 12.3 (10.1–14.5) | 14.5 (12.7–16.4) | |
| College graduate or higher | 20.3 (17.7–22.9) | 25.3 (21.6–28.9) | 36.9 (32.3–41.5) | |
| Educational attainment | <.0001 | |||
| Vocational/technical training or less | 49.2 (45.6–52.7) | 37.3 (33.5–41.2) | 23.5 (19.7–27.4) | |
| Some college | 36.1 (33.3–38.8) | 36.2 (33.3–39.0) | 26.6 (23.8–29.5) | |
| College graduate or higher | 14.8 (12.3–17.3) | 26.5 (23.2–29.8) | 49.8 (44.7–55.0) | |
| Race/ethnicity | <.0001 | |||
| Non-Hispanic White | 65.4 (59.4–71.5) | 66.4 (59.6–73.1) | 72.2 (66.1–78.2) | |
| Non-Hispanic Black | 17.8 13.0–22.7) | 15.6 (10.9–20.4) | 12.6 (8.2–17.0) | |
| Non-Hispanic Asian/Pacific Islander | 1.5 (0.7–2.3) | 1.9 (0.8–2.9) | 3.5 (1.8–5.1) | |
| Hispanic | 11.0 (7.5–14.5) | 13.3 (8.7–18.0) | 9.6 (6.3–13.0) | |
| Non-Hispanic Multiracial | 4.2 (3.1–5.3) | 2.8 (1.8–3.8) | 2.1 (1.4–2.8) | |
| Ever diagnosed with depression | 49.0 (45.4–52.6) | 25.9 (22.7–29.0) | 25.2 (21.5–28.9) | <.0001 |
| Perceived discriminationb | <.0001 | |||
| Never | 23.8 (21.7–26.0) | 29.8 (26.8–32.8) | 38.6 (35.8–41.5) | |
| Rarely | 42.6 (40.0–45.2) | 47.2 (44.1–50.3) | 44.5 (41.3–47.6) | |
| Sometimes/often | 33.6 (31.0–36.2) | 23.0 (20.4–25.6) | 16.9 (14.7–19.1) | |
| Waist circumference, cm | 101 (99.7–102) | 98.6 (97.5–99.7) | 96.2 (95.2–97.2) | <.0001 |
| Body mass index category | <.0001 | |||
| Underweight (<18.5 9 kg/m2) | 1.6 (0.9–2.3) | 1.9 (0.8–3.0) | 1.2 (0.6–1.8) | |
| Normal (18.5–24.9 kg/m2) | 29.2 (26.6–31.7) | 27.9 (25.1–30.7) | 35.4 (31.7–39.1) | |
| Overweight (25–29.9 kg/m2) | 27.9 (25.7–30.0) | 32.1 (29.2–35.0) | 31.9 (28.5–35.3) | |
| Obesity (≥30 kg/m2) | 41.4 (38.6–44.1) | 38.1 (34.8–41.4) | 31.5 (28.7–34.6) | |
| Systolic blood pressure, mmHg | 127 (126–128) | 125 (124–126) | 124 (124–125) | .04 |
| Diastolic blood pressure, mmHg | 80.5 (79.9–81.2) | 79.8 (79.1–80.4) | 79.0 (78.5–79.6) | .0004 |
| Triglyceride decilec | 5.7 (5.5–5.9) | 5.5 (5.3–5.7) | 5.4 (5.2–5.5) | .01 |
| Total cholesterol decilec | 5.5 (5.3–5.7) | 5.5 (5.3–5.7) | 5.4 (5.3–5.6) | .79 |
| High-density lipoprotein cholesterol decilec | 5.3 (5.2–5.5) | 5.5 (5.3–5.7) | 5.4 (5.2–5.6) | .52 |
| Low-density lipoprotein cholesterol decilec | 5.4 (5.3–5.6) | 5.5 (5.3–5.6) | 5.5 (5.3–5.6) | .94 |
| Total cholesterol–HDL-C ratio decilec | 5.7 (5.5–5.8) | 5.5 (5.3–5.7) | 5.5 (5.3–5.7) | .22 |
| Glucose, mg/dL | 109 (107–111) | 107 (106–109) | 107 (105–108) | .15 |
| Glycated hemoglobin, % | 5.6 (5.6–5.7) | 5.6 (5.5–5.6) | 5.5 (5.5–5.6) | .0002 |
| C-reactive protein, mg/L | 5.4 (4.9–5.9) | 4.5 (4.0–5.0) | 3.9 (3.5–4.3) | <.0001 |
Data shown as (mean [95% CI] or % [95% CI]). CI confidence interval; HDL-C high-density lipoprotein cholesterol.
aSubjective social status scores were categorized based on the weighted median score (4.5) for the sample.
bResponse to the question, “In your day-to-day life, how often do you feel you have been treated with less respect or courtesy than other people?”
cValues were rank ordered and categorized into deciles. Higher deciles represent higher values (range: 1–10).
Intersectional Associations Between Objective Socioeconomic Status and Subjective Social Status
In unweighted correlation analyses, all measures of subjective and objective social status were significantly intercorrelated for the total analytical sample, for females, for males, for NHW, and for NHB (Supplementary Material 1). Correlations were less consistent for NHA, Hispanics, and NHM. In regression models, all three-way interactions between individual objective SES indicators, sex, and race/ethnicity were statistically significant: household income at Wave 1 (p = .03), current household income (p = .02), maternal educational attainment (p < .0001), and current educational attainment (p = .09). When models were stratified by sex and race/ethnicity, each objective SES measures demonstrated a strong graded relationship with SSS for NHW females and males (Supplementary Material 2). For NHB females, higher household income and educational attainment were associated with higher mean SSS. Only higher educational attainment was associated with higher mean SSS for NHB males. For NHA females, Wave I and current household income and educational attainment appeared to have a graded relationship with SSS, although these did not always reach statistical significance. The relationships were less consistent for NHA males. For Hispanic females and males, higher household income and educational attainment were associated with higher mean SSS. Higher household income at Wave I was also related to higher mean SSS among Hispanic males. For NHM females, higher educational attainment was associated with higher mean SSS, and higher household income appeared to have a graded relationship with mean SSS, though the association was not significant. All objective SES indicators appeared to have a graded relationship with mean SSS for NHM males, though only household income and educational attainment reached statistical significance in relation to SSS.
Three-Way Interactions of Subjective Social Status, Sex, and Race/Ethnicity on Cardiometabolic Risk Factors
Five of the three-way interactions (SSS–race/ethnicity–sex) tested in minimally adjusted models were statistically significant: waist circumference (p ≤ 0.0001), BMI (p ≤ 0.0001), SBP (p ≤ 0.0001), DBP (p = .0004), and HDL-C (p = .07) (Supplementary Material 3). We explored these significant three-way interactions by stratifying models, as reported below.
Interaction of Subjective Social Status and Sex on Cardiometabolic Risk Markers, Stratified by Race/Ethnicity
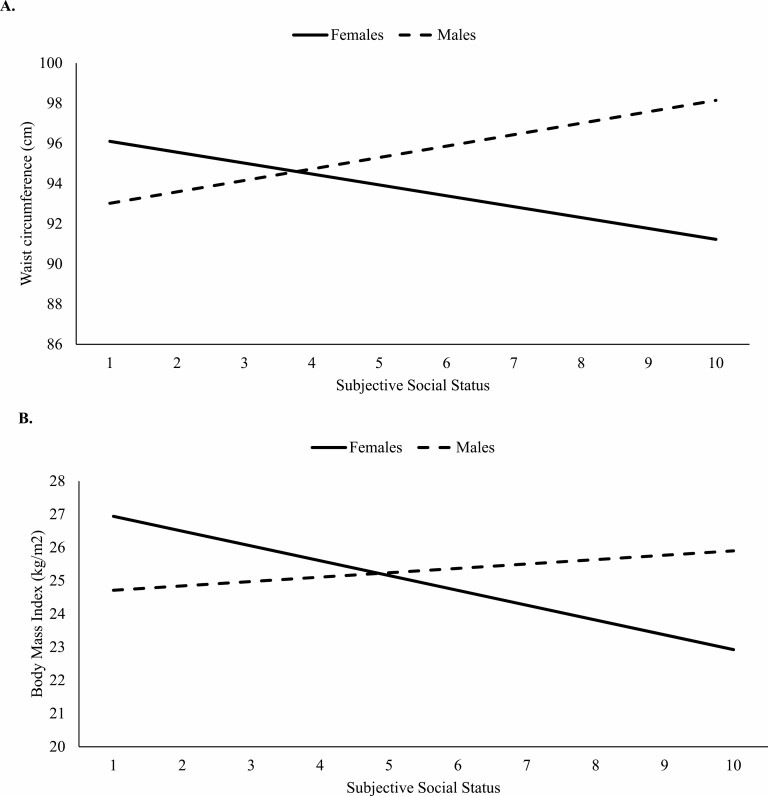
In models stratified by race/ethnicity with an interaction term between SSS and sex, SSS had a stronger inverse relationship with waist circumference (p = .005) and BMI (p = .003) for NHW females, compared with NHW males, before and after adjustment for objective SES (Table 4). Figure 1 displays the adjusted mean waist circumference and BMI for NHW females and males at each step on the SSS.
Table 4.
Estimates (β [SE]) for the association between subjective social status and cardiometabolic risk factors for females, stratified by race/ethnicity, in Wave IV of the National Longitudinal Study of Adolescent to Adult Health Study (2008)a
| Non-Hispanic White | Non-Hispanic Black | Non-Hispanic Asian/Pacific Islander | Hispanic | Non-Hispanic Multiracial | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Cardiometabolic outcomes | Model 1b | Model 2c | Model 1b | Model 2c | Model 1b | Model 2c | Model 1b | Model 2c | Model 1b | Model 2c |
| Waist circumference (cm) | −1.2 (0.4)** | −1.1 (0.4)* | 0.4 (0.7) | 0.3 (0.7) | 0.2 (1.7) | 0.3 (1.5) | 0.2 (1.1) | 0.4 (1.0) | 0.8 (1.3) | 1.0 (1.2) |
| Body mass index (kg/m2) | −0.6 (0.2)** | −0.6 (0.2)** | 0.3 (0.3) | 0.3 (0.3) | −0.2 (0.7) | −0.1 (0.6) | −0.4 (0.4) | −0.3 (0.4) | 0.4 (0.7) | 0.4 (0.6) |
| Systolic blood pressure (mmHg)d | −0.1 (0.3) | −0.1 (0.3) | 0.1 (0.5) | −0.1 (0.5) | 2.0 (1.3) | 2.2 (1.4) | 0.4 (0.7) | 0.5 (0.6) | 1.3 (1.3) | 0.8 (1.3) |
| Diastolic blood pressure (mmHg)d | −0.1 (0.2) | −0.1 (0.2) | −0.2 (0.4) | −0.3 (0.4) | 0.9 (1.1) | 1.2 (1.0) | −0.04 (0.6) | 0.03 (0.5) | 0.02 (1.1) | −0.3 (1.0) |
| High-density lipoprotein cholesterol decilee | 0.2 (0.1)* | 0.2 (0.1)* | −0.01 (0.1) | −0.04 (0.1) | −0.03 (0.3) | 0.01 (0.3) | 0.3 (0.1)* | 0.3 (0.1)* | −0.1 (0.3) | −0.2 (0.3) |
aEstimates are for females, compared with males.
bAdjusted for age and sex, with an interaction term between subjective social status and sex.
cAdjusted for covariates in Model 1 plus childhood household income, maternal education, adulthood household income, educational attainment, with an interaction term between subjective social status and sex. Significant interactions among non-Hispanic White (waist circumference: p = .01; body mass index: p = .004; high-density lipoprotein cholesterol: p = .03) and Hispanic (high-density lipoprotein cholesterol: p = .03).
dAdditionally adjusted for depression.
eValues were rank ordered and categorized into deciles. Higher deciles represent higher values (range: 1–10).
*p < .05, **p < .01.
Fig. 1.
Adjusted mean waist circumference and body mass index for each step of subjective social status among non-Hispanic White females and males in Wave IV of the National Longitudinal Study of Adolescent to Adult Health Study (2008). Adjusted for age, sex, childhood household income, maternal education, adulthood household income, and educational attainment, with an interaction term between subjective social status and sex.
For SBP, the interaction between SSS and sex was not statistically significant within each race/ethnicity, although SSS tended to have a stronger positive relationship with SBP for NHA females, compared with NHA males, before (p = .13) and after (p = .11) adjustment for objective SES. For DBP, the interaction between SSS and sex was not statistically significant within any race/ethnicity group.
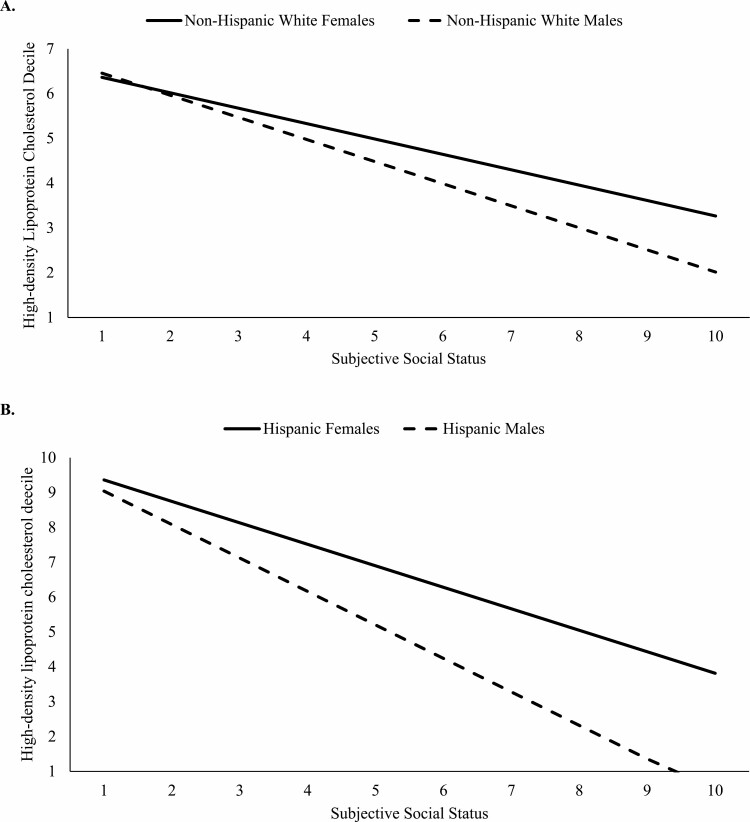
When modeling HDL-C, the interaction between SSS and sex was significant among NHW and among Hispanics before and after adjustment for objective SES. Before adjustment, SSS had a stronger positive relationship for NHW females, compared with NHW males (p = .01), and for Hispanic females, compared with Hispanic males (p = .02). These sex differences remained after adjustment for objective SES (NHW: p = .03; Hispanic: p = .03). Figure 2 displays the adjusted mean HDL-C for NHW and Hispanic females and males at each step on the SSS.
Fig. 2.
Adjusted mean high-density lipoprotein cholesterol decile for each step of subjective social status among Hispanic and non-Hispanic White females and males in Wave IV of the National Longitudinal Study of Adolescent to Adult Health Study (2008). Adjusted for age, sex, childhood household income, maternal education, adulthood household income, and educational attainment, with an interaction term between subjective social status and sex.
Interaction of Subjective Social Status and Race/Ethnicity on Cardiometabolic Risk Markers, Stratified by Sex
When modeling waist circumference in models stratified by sex, the interaction between SSS and race/ethnicity was marginally significant for females (p = .09), but not for males (p = .74), before adjustment for objective SES. Compared with NHW females, SSS was positively associated with waist circumference for NHB females (p = .02). After adjustment for objective SES, the interactions were not significant (females: p = .51; males: p = .57) (Table 5).
Table 5.
Estimates (β [SE]) for the association of subjective social status with cardiometabolic risk factors for Non-Hispanic Black, Asian/Pacific Islander, Multiracial, and Hispanic adults, stratified by sex, in Wave IV of the National Longitudinal Study of Adolescent to Adult Health Study (2008)
| Non-Hispanic White | Non-Hispanic Black | Non-Hispanic Asian/Pacific Islander | Hispanic | Non-Hispanic Multiracial | |||||
|---|---|---|---|---|---|---|---|---|---|
| Cardiometabolic outcomes | Referent | Model 1a | Model 2b | Model 1a | Model 2b | Model 1a | Model 2b | Model 1a | Model 2b |
| Females | |||||||||
| Waist circumference (cm) | — | 1.7 (0.7)* | 0.9 (0.7) | 2.1 (1.6) | 1.9 (1.7) | 0.8 (0.9) | 0.5 (0.9) | 1.8 (1.1) | 1.2 (1.1) |
| Body mass index (kg/m2) | — | 0.9 (0.3)** | 0.6 (0.3)* | 0.7 (0.7) | 0.7 (0.7) | 0.2 (0.3) | 0.1 (0.3) | 1.1 (0.6) | 0.9 (0.6) |
| Systolic blood pressure (mmHg) | — | 0.8 (0.5) | 0.6 (0.5) | 1.8 (0.7)* | 1.7 (0.8)* | 0.1 (0.5) | 0.02 (0.5) | 1.9 (0.8)* | 1.8 (0.8)* |
| Diastolic blood pressure (mmHg) | — | 0.6 (0.1)**** | 0.7 (0.4) | −0.1 (0.2) | 0.6 (0.8) | −0.1 (0.2) | 0.2 (0.4) | 0.1 (0.2) | 0.7 (0.6) |
| High-density lipoprotein cholesterol deciled | — | 0.1 (0.2) | 0.1 (0.2) | 0.2 (0.1) | 0.1 (0.1) | 0.2 (0.2) | 0.1 (0.2) | 0.2 (0.1) | 0.1 (0.1) |
| Males | |||||||||
| Waist circumference (cm) | — | 0.1 (0.6) | −0.02 (0.5) | 0.8 (0.6) | 0.6 (0.9) | −0.5 (0.6) | −0.8 (0.6) | −0.3 (1.0) | −0.6 (0.9) |
| Body mass index (kg/m2) | — | 0.04 (0.2) | −0.004 (0.2) | 0.3 (0.3) | 0.2 (0.3) | −0.01 (0.3) | −0.1 (0.3) | 0.1 (0.5) | −0.002 (0.5) |
| Systolic blood pressure (mmHg)c | — | 0.6 (0.4) | 0.6 (0.4) | −0.1 (1.2) | −0.3 (1.2) | −0.4 (0.6) | −0.4 (0.6) | 0.6 (1.1) | 0.5 (1.0) |
| Diastolic blood pressure (mmHg)c | — | −0.03 (0.1) | 0.8 (0.3)** | −0.003 (0.2) | −0.5 (0.9) | 0.02 (0.1) | 0.03 (0.5) | −0.1 (0.3) | 0.7 (0.8) |
| High-density lipoprotein cholesterol deciled | — | 0.1 (0.2) | 0.1 (0.2) | −0.l (0.1) | −0.2 (0.1) | 0.3 (0.2) | 0.3 (0.2) | −0.01 (0.1) | −0.03 (0.1) |
aAdjusted for age and race/ethnicity, with an interaction term between subjective social status and race/ethnicity.
bAdjusted for covariates in Model 1 plus childhood household income, maternal education, adulthood household income, educational attainment, with an interaction term between subjective social status and race/ethnicity. Significant interactions among females (systolic blood pressure: p = .04) and males (diastolic blood pressure: p = .07).
cAdditionally adjusted for depression.
dValues were rank ordered and categorized into deciles. Higher deciles represent higher values (range: 1–10).
*p < .05, **p < .01, ***p < .001, ****p < .0001.
We observed a similar relationship when modeling BMI; before adjustment for objective SES, the interaction between SSS and race/ethnicity was significant among females (p = .03), but not among males (p = .84). Compared with NHW females, SSS was positively associated with BMI for NHB females (p = .003) and tended to be positively associated with BMI for NHM females (p = .07). The interaction was no longer significant after adjustment for objective SES (females: p = .22; males: p = .90), though the significant difference between NHB and NHW persisted (p = .046).
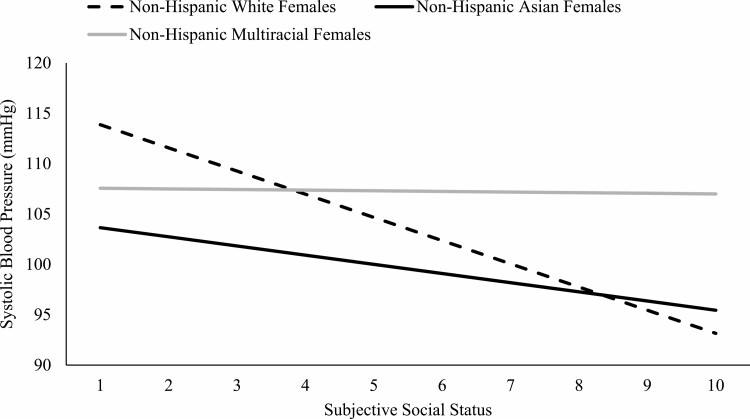
For SBP, the interaction of SSS and race/ethnicity was significant among females (p = .01), but not among males (p = .49), before adjustment for objective SES. Compared with NHW females, SSS was positively associated with SBP for NHA (p = .02) and NHM (p = .02) females, and tended to be positively associated with SBP for NHB females (p = .096). After adjustment for objective SES, the interaction remained significant for females (p = .04; males: p = .43). Compared with NHW females, SSS had a weaker inverse association with SBP among NHA (p = .04) and NHM (p = .03) females (Fig. 3).
Fig. 3.
Adjusted mean systolic blood pressure for each step of subjective social status among non-Hispanic Asian, Multiracial, and White females in Wave IV of the National Longitudinal Study of Adolescent to Adult Health Study (2008). Adjusted for age, sex, depression, childhood household income, maternal education, adulthood household income, and educational attainment, with an interaction term between subjective social status and race/ethnicity.
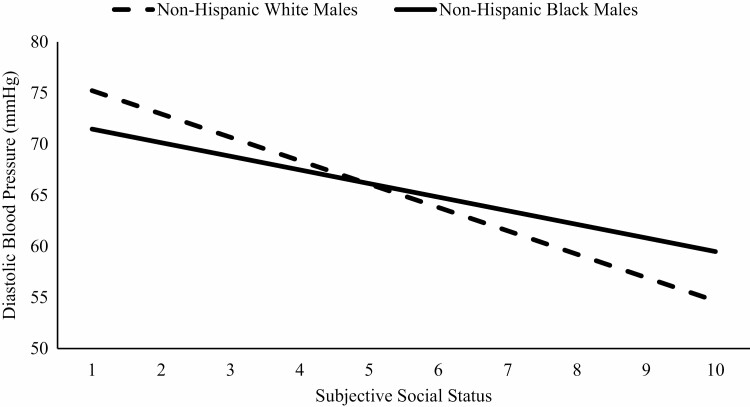
When modeling DBP in the sex-stratified model, the SSS–race/ethnicity interactions were significant for females (p = .0001), but not males (p = 1.0) before adjusting for objective SSS. Compared with NHW females, SSS was positively associated with DBP for NHB females (p < .0001). After adjustment for objective SES, the interaction was no longer significant for females (p = .42), although SSS tended to have a positive relationship with DBP for NHB compared with NHW females (p = .10). Notably, after adjustment for objective SES, the SSS–race/ethnicity interaction was marginally significant for males (p = .07). Compared with NHW males, SSS was positively associated with DBP among NHB males (p = .01) (Fig. 4).
Fig. 4.
Adjusted mean diastolic blood pressure for each step of subjective social status among non-Hispanic Black and White males in Wave IV of the National Longitudinal Study of Adolescent to Adult Health Study (2008). Adjusted for age, sex, depression, childhood household income, maternal education, adulthood household income, and educational attainment, with an interaction term between subjective social status and race/ethnicity.
For HDL-C in sex-stratified models, the interaction of SSS and race/ethnicity was not statistically significant for either sex before (females: p = .44, males: p = .34) or after (females: p = .76, males: p = .35) adjustment for objective SES.
Discussion
In a sample of diverse young adults, objective SES indicators were more strongly related to SSS among NHW females and males, with less consistent relationships among NHB, NHA, Hispanic, and NHM females and males. This aligns with other studies showing that the information used to evaluate SSS may vary by race and ethnicity [21, 25, 42]. Some differences in associations of SSS with cardiometabolic risk markers were observed by sex within NHW and Hispanic adults, but not within other ethnic/racial groups. Specifically, SSS had a stronger inverse relationship with waist circumference and BMI for NHW females, compared with NHW males, independent of objective SES. SSS had a weaker inverse association with HDL-C for NHW and Hispanic females, compared with their male counterparts, independent of objective SES. SSS also tended to have a stronger positive relationship with SBP for NHA females, compared with NHA males, although the interaction did not reach statistical significance. Some differences in associations of SSS with cardiometabolic risk markers were observed by race/ethnicity within females for SBP, and within males for DBP. SSS had a weaker inverse association with SBP for NHA and NHM females, compared with NHW females. Similarly, SSS had a weaker inverse association with DBP for NHB compared with NHW males. Notably, SES indicators appeared to explain some of the relationship of SSS to waist circumference and BMI among NHB females, compared with NHW females, and the relationship of SSS with DBP among NHB males, compared with NHW males.
These findings contribute to limited evidence on the relationship between SSS and cardiometabolic risk markers in racially/ethnically diverse adults. Previous findings on SSS and cardiometabolic risk factors by race/ethnicity are limited and mixed, though there appears to be stronger relationships among Whites than among ethnic/racial minorities [18, 42, 52], which supports some of our findings in a nationally representative sample of young adults. Across the few studies with diverse samples, SSS has been shown to be inversely associated with BMI [38, 44], hsCRP [43], and odds of metabolic syndrome, hypertension, and high waist circumference [53]. SSS has been shown to be associated with physical and mental health, independent of objective SES, in nationally representative and community-based samples of Black, Asian, and Hispanic/Latino adults [40, 54, 55]. SSS was previously found to have a stronger association with self-reported health compared with biologically based assessments of health in diverse samples [13], which may explain some of the differences across studies.
Yet, differences in SSS–cardiometabolic risk marker relationships may also stem from race/ethnicity as a proxy for the psychosocial context [56], including unique contributors to SSS within racial/ethnic groups and distinctions in the SSS comparison group used within racial/ethnic groups. In our study, traditional SES markers were more strongly associated with SSS among NHW adults compared with NHB, NHA, Hispanic, and NHM adults. Objective measures of SES may be a less salient factor for non-Whites in determining SSS [28, 29, 42, 57–60]. Higher SSS has been shown to be associated with higher levels of resilience among Black women [26] and higher likelihood of speaking English among Mexican-heritage adults [28, 29], potential protective factors worth exploring in future studies on SSS and cardiometabolic risk. Shaked et al. argued that, because of stigmatization, Blacks may be making in-group and not out-group comparisons [25], which could improve SSS ratings. Similarly, among Mexican-heritage adults in low-income neighborhoods in Texas, those more likely to speak English and be U.S. born tended to compare themselves to people in the United States, while their counterparts tended to compare themselves to Mexicans in the United States or to Mexicans in Mexico [29]. Future work necessitates exploring these additional intersectionalities in SSS correlates and comparison groups, as well as comparing the utility of the societal (U.S.) SSS versus the community SSS in explaining cardiometabolic risk markers. Some research indicates that community, versus societal, SSS may have a stronger association with access to health care [61], psychosocial health [22], and sympathetic nervous system receptor signaling [62], which can affect cardiometabolic risk.
Our findings advance the understanding of SSS–cardiometabolic risk marker relationships by considering intersectional differences by both race/ethnicity and sex in a diverse sample, of which limited evidence exists [40, 42]. Furthermore, our sample of young adults (24–32 years) allows for early indication of the role of SSS in shaping cardiometabolic risk before clinical chronic disease manifests. Most intersectional research on social status and cardiometabolic risk to date has been conducted in samples inclusive of middle-aged and older adults, which may help explain our limited findings, as cardiometabolic risk factors are more likely to be present with increasing age. For example, SSS was inversely associated with insulin resistance among Black women, but not Black men, in a community sample of U.S. adults (21–95 years) [40], a relationship we did not observe in our younger sample. Adiposity, blood pressure, and HDL-C may be cardiometabolic risk factors that present earlier, as we noted intersectional differences. Similar to our study, in a U.S. community sample of Black and White adults (33–48 years), lower SSS was associated with hypertension for White men and women and Black women, but not Black men, and the relationship only persisted for White men after adjusting for all objective SES markers [42]. Furthermore, our documented associations between SSS and cardiometabolic risk were not in the expected direction for several relationships, including SBP for NHA females versus males, HDL-C for NHW and Hispanic males versus females, and to some extent for waist circumference among NHW males versus females. Some evidence suggests that social status may have a stronger inverse relationship with body weight over time for NHW females, compared with NHW males [63]. Increases in objective SES among racial/ethnic minority adults do not appear to have a clear graded relationship with physical health as it does among White adults, suggesting “diminishing returns” [6, 7, 64]. Nationally representative data have shown that increases in household income are associated with increased odds of smoking, a behavioral risk factor of hypertension, among Chinese American, compared with White American adults [65]. One possible explanation is that discrimination may be a more salient factor among racial/ethnic minority adults of higher, versus lower, SES [66], which subsequently may promote poor health behaviors [67, 68] and poor physical health [7, 69]. We tested perceived discrimination in all of our models, but only retained it in one (model for TG decile). Although a previous study did not find that perceived racial discrimination confounded or moderated the relationship between SSS and insulin resistance among Black adults [40], additional research testing how intersectionalities of objective SES, race/ethnicity, and sex shape the relationship between SSS and cardiometabolic risk marker relationships are needed.
SSS may also influence cardiometabolic risk through other pathways in diverse young adults, including psychological traits [11, 44], biological mechanisms [70, 71], and lifestyle behaviors [44, 72, 73]. For this reason, we did not adjust for these factors in our analyses. Life course experiences may also shape the SSS–health relationship [74, 75]. For example, a high-to-low SSS trajectory, but not baseline SSS, was associated with lower BMI among Black, but not White, adolescents over a 10-year follow-up period transitioning to young adulthood upon adjusting for baseline adiposity. However, lower baseline SSS or having a high-to-low SSS trajectory were associated with higher depressive symptoms among Whites, a relationship that did not persist for Blacks [74]. Together, these findings emphasize that health disparities research will benefit from future work that thoroughly investigates the longitudinal role of the psychosocial context in shaping SSS and health outcomes [56].
Our study had several limitations. First, the cross-sectional design of our study precludes determining the direction of the SSS–cardiometabolic risk marker relationships. These relationships may not be causal, but instead reciprocal [76]. Additionally, these analyses employed the U.S. SSS, which uses the nationwide population as the referent group, and may not be appropriate for all racial/ethnic groups. Community SSS may be more related to self-perceptions and psychosocial factors in women, though SSS scores do not appear to differ by race/ethnicity when using more distal referents, like broader U.S. society [59]. Tang et al. also argued that objective measures of SES may be on the pathway linking SSS and cardiometabolic risk, rather than objective measures being a confounder [18]. Thus, including objective measures in our models may have been an overadjustment. Given that our research objective focused on race/ethnicity and sex differences and there are clear disparities in objective SES by race/ethnicity and sex, we deemed it appropriate to adjust for these in our final models. Race/ethnicity may also be a proxy for other contextual factors for which we did not adjust, including cohort effects, acculturation, and racial/ethnic discrimination. The available measure of depression was also a limitation, as it was a single-item self-report of ever experiencing depression, which may have not adequately captured current depressive symptoms that would be correlated with SSS ratings. Similarly, the perceived discrimination measure was a broad single item that may capture experiences that are not discriminatory, rather experiences that are perceived as mean or dishonorable [77]. Last, samples sizes were small for NHA and NHM, potentially limiting generalizability, although analyses were weighted to represent the population. Sample sizes were also not large enough to investigate differences by self-reported heritage, which may be more meaningful than heterogenous groupings by race/ethnicity, or by Native Americans and Alaskan Natives, minority groups with evidenced cardiometabolic health disparities.
Our analyses also had several notable strengths that meaningfully contribute to the literature. First, the Add Health cohort is a large U.S. sample of young adults from diverse backgrounds. Most other studies have used local or non-U.S. samples or have not been inclusive of different races/ethnicities. Exploring the role of SSS in health necessitates more diverse samples to understand health disparities and promote health equity. Furthermore, we were able to account for objective measures of SES across the life course through adjustments for maternal educational attainment and household income at baseline (childhood), in addition to young adults’ current educational attainment and household income. Our analyses also employed objectively measured cardiometabolic risk factors, instead of self-reported cardiometabolic conditions. Objective measures are also important in this context as cardiometabolic conditions may have not yet manifested in young adulthood.
Our findings provide evidence that SSS is related to cardiometabolic risk differently depending on race/ethnicity and intersectionality of race/ethnicity and sex, with the most consistent relationships for NHW females. A prior intersectional study in the Add Health cohort suggests that SES, including various life course SES frameworks, may be more influential to the health of young adult White women born between 1976 and 1984, compared with their White male and racial/ethnic-minority counterparts [45]. The differences we documented may indicate distinct pathways of SSS in cardiometabolic health by intersections of race/ethnicity and sex, independent of objective measures of SES. Opportunities exist in diverse cohorts to elucidate longitudinal pathways linking SSS to cardiometabolic risk, which can serve to inform novel approaches to reducing health inequities. Future research should investigate these pathways and the determinants of SSS using an intersectional approach, not only for race/ethnicity and sex, but also for other intersections of identity that can affect cardiometabolic health. An intersectional lens is also warranted for future studies testing the utility of SSS in clinical and intervention settings [78], including strengthening SSS as a means to improve behaviors [79] and tailoring intervention approaches to level of SSS [80].
Supplementary Material
Acknowledgments
We thank Dr. Susan Levy for her consultation on analytical power for these analyses.
Funding
A.C.M. received support for this study from a National Institutes of Health (NIH) –National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) Ruth L. Kirschstein Institutional Training Grant Postdoctoral Fellowship (5 T32 DK 7703-23) and from a NIH–National Heart, Lung, and Blood Institute (NHLBI) K01 Mentored Career Development Award (K01-HL150406). L.C.G. received support during manuscript preparation from an NIH-NIDDK center grant (5 P30 DK111022-03) and an NIH-National Center for Advancing Translational Sciences ; HDL-C high-density lipoprotein cholestero lnstitutional grant (5 UL1 TR002550-02). J.M. received support for this study from an NIH–NHLBI Mentored Career Development Award to Promote Faculty Diversity (K01-HL120951).
Compliance With Ethical Standards
Authors’ Statement of Conflict of Interest and Adherence to Ethical Standards The authors have no other conflicts of interest to report. Data for the current analyses were secondary and had no personal identifiers; thus, the analyses were exempt from Institutional Review Board approval.
Author Contributions A.C.M designed the research question, analyzed the data, interpreted the results, wrote the manuscript, and has primary responsibility for final content. L.C.G. and J.M contributed to the analytical design and to interpretation and presentation of results. All authors read and approved the final manuscript.
Ethical Approval The University of North Carolina at Chapel Hill Public Health-Nursing Institutional Review Board approved the Add Health Study.
Informed Consent Written informed consent was obtained from all Add Health study participants.
References
- 1. Benjamin EJ, Muntner P, Alonso A, et al. ; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee . Heart disease and stroke statistics – 2019 Update: A report from the American Heart Association. Circulation. 2019;139:e56–e528. [DOI] [PubMed] [Google Scholar]
- 2. Pool L, Ning H, Lloyd‐Jones D, Allen N. Trends in Racial/ethnic disparities in cardiovascular health among US adults from 1999–2012. J Am Heart Assoc. 2017;6(9):e006027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Brown AF, Liang L-J, Vassar SD, et al. . Trends in racial/ethnic and nativity disparities in cardiovascular health among adults without prevalent cardiovascular disease in the United States, 1988 to 2014 disparities in cardiovascular health. Ann Intern Med. 2018;168(8):541–549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Waidmann T. Estimating the Cost of Racial and Ethnic Health Disparities. Washington, DC: The Urban Institute; 2009. Available at https://www.urban.org/sites/default/files/publication/30666/411962-Estimating-the-Cost-of-Racial-and-Ethnic-Health-Disparities.PDF. [Google Scholar]
- 5. de Mestral C, Stringhini S. Socioeconomic status and cardiovascular disease: An update. Curr Cardiol Rep. 2017;19:115. [DOI] [PubMed] [Google Scholar]
- 6. Boykin S, Diez-Roux AV, Carnethon M, Shrager S, Ni H, Whitt-Glover M. Racial/ethnic heterogeneity in the socioeconomic patterning of CVD risk factors: in the United States: The multi-ethnic study of atherosclerosis. J Health Care Poor Underserved. 2011;22:111–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Colen CG, Krueger PM, Boettner BL. Do rising tides lift all boats? Racial disparities in health across the lifecourse among middle-class African-Americans and Whites. SSM Popul Health. 2018;6:125–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. López-Cevallos DF, Molina KM, Bekteshi V, et al. . Is there a link between wealth and cardiovascular disease risk factors among Hispanic/Latinos? Results from the HCHS/SOL sociocultural ancillary study. Ethn Health. 2018;23(8):902–913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Williams DR, Mohammed SA, Leavell J, Collins C. Race, socioeconomic status, and health: Complexities, ongoing challenges, and research opportunities. Ann N Y Acad Sci. 2010;1186:69–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Jackman MR, Jackman RW. An interpretation of the relation between objective and subjective social status. Am Sociol Rev. 1973;38:569–582. [PubMed] [Google Scholar]
- 11. Adler NE, Epel ES, Castellazzo G, Ickovics JR. Relationship of subjective and objective social status with psychological and physiological functioning: Preliminary data in healthy white women. Health Psychol. 2000;19:586–592. [DOI] [PubMed] [Google Scholar]
- 12. Hu P, Adler NE, Goldman N, Weinstein M, Seeman TE. Relationship between subjective social status and measures of health in older Taiwanese persons. J Am Geriatr Soc. 2005;53:483–488. [DOI] [PubMed] [Google Scholar]
- 13. Cundiff JM, Matthews KA. Is subjective social status a unique correlate of physical health? A meta-analysis. Health Psychol. 2017;36:1109–1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Cundiff JM, Kamarck TW, Manuck SB. Daily interpersonal experience partially explains the association between social rank and physical health. Ann Behav Med. 2016;50:854–861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ferreira WA, Camelo L, Viana MC, Giatti L, Barreto SM. Is subjective social status a summary of life-course socioeconomic position? Cad Saude Publ. 2018;34:e00024317. [DOI] [PubMed] [Google Scholar]
- 16. Williams DR, Priest N, Anderson NB. Understanding associations among race, socioeconomic status, and health: Patterns and prospects. Health Psychol. 2016;35:407–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Miller G, Chen E, Cole SW. Health psychology: Developing biologically plausible models linking the social world and physical health. Annu Rev Psychol. 2009;60:501–524. [DOI] [PubMed] [Google Scholar]
- 18. Tang KL, Rashid R, Godley J, Ghali WA. Association between subjective social status and cardiovascular disease and cardiovascular risk factors: A systematic review and meta-analysis. BMJ Open. 2016;6:e010137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Cundiff JM, Smith TW, Baron CE, Uchino BN. Hierarchy and health: Physiological effects of interpersonal experiences associated with socioeconomic position. Health Psychol. 2016;35:356–365. [DOI] [PubMed] [Google Scholar]
- 20. Ostrove JM, Adler NE, Kuppermann M, Washington AE. Objective and subjective assessments of socioeconomic status and their relationship to self-rated health in an ethnically diverse sample of pregnant women. Health Psychol. 2000;19:613–618. [DOI] [PubMed] [Google Scholar]
- 21. Wolff LS, Acevedo-Garcia D, Subramanian SV, Weber D, Kawachi I. Subjective social status, a new measure in health disparities research: Do race/ethnicity and choice of referent group matter? J Health Psychol. 2010;15:560–574. [DOI] [PubMed] [Google Scholar]
- 22. Chen R, Kessler RC, Sadikova E, et al. . Racial and ethnic differences in individual-level and area-based socioeconomic status and 12-month DSM-IV mental disorders. J Psychiatr Res. 2019;119:48–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Howard JT, Sparks PJ. The role of education in explaining racial/ethnic allostatic load differentials in the United States. Biodemogr Soc Biol. 2015;61:18–39. [DOI] [PubMed] [Google Scholar]
- 24. Matthews KA, Gallo LC. Psychological perspectives on pathways linking socioeconomic status and physical health. Annu Rev Psychol. 2011;62:501–530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Shaked D, Williams M, Evans MK, Zonderman AB. Indicators of subjective social status: Differential associations across race and sex. SSM Popul Health. 2016;2:700–707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Saban KL, Tell D, Janusek L. Resilience in African American women at risk for cardiovascular disease: An exploratory study. J Urban Health. 2019;96:44–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Reitzel LR, Childress SD, Obasi EM, et al. . Interactive effects of anxiety sensitivity and subjective social status on psychological symptomatology in Black adults. Behav Med. 2017;43:268–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Reitzel LR, Mazas CA, Cofta-Woerpel L, et al. . Acculturative and neighborhood influences on subjective social status among Spanish-speaking Latino immigrant smokers. Soc Sci Med. 2010;70:677–683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Franzini L, Fernandez-Esquer ME. The association of subjective social status and health in low-income Mexican-origin individuals in Texas. Soc Sci Med. 2006;63:788–804. [DOI] [PubMed] [Google Scholar]
- 30. de Castro AB, Gee GC, Takeuchi DT. Examining alternative measures of social disadvantage among Asian Americans: The relevance of economic opportunity, subjective social status, and financial strain for health. J Immigr Minor Health. 2010;12:659–671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Crenshaw K. Demarginalizing the intersection of race and sex: A Black feminist critique of antidiscrimination doctrine, feminist theory and antiracist politics. U Chi Legal F. 1989;1989(1):139–167. [Google Scholar]
- 32. Crenshaw K. Mapping the margins: Intersectionality, identity politics, and violence against women of color. Stan L Rev 1991;43(6):1241–1299. [Google Scholar]
- 33. Nash JC. Re-thinking intersectionality. Fem Rev. 2008;89(1):1–15. [Google Scholar]
- 34. Cole ER. Intersectionality and research in psychology. Am Psychol. 2009;64:170–180. [DOI] [PubMed] [Google Scholar]
- 35. Weber L, Zambrana RE, Fore ME, Parra-Medina D. Racial and ethnic health inequities: An intersectional approach. In: Batur P, Feagin J, eds. Handbook of the Sociology of Racial and Ethnic Relations. Handbooks of Sociology and Social Research. 2nd ed. Germany: Springer; 2018:133–160. [Google Scholar]
- 36. Singh-Manoux A, Marmot MG, Adler NE. Does subjective social status predict health and change in health status better than objective status? Psychosom Med. 2005;67:855–861. [DOI] [PubMed] [Google Scholar]
- 37. Demakakos P, Nazroo J, Breeze E, Marmot M. Socioeconomic status and health: the role of subjective social status. Soc Sci Med. 2008;67:330–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Dhurandhar EJ, Pavela G, Kaiser KA, et al. . Body mass index and subjective social status: The coronary artery risk development in young adults study. Obesity (Silver Spring). 2018;26:426–431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Miyakawa M, Magnusson Hanson LL, Theorell T, Westerlund H. Subjective social status: its determinants and association with health in the Swedish working population (the SLOSH study). Eur J Public Health. 2012;22:593–597. [DOI] [PubMed] [Google Scholar]
- 40. Subramanyam MA, Diez-Roux AV, Hickson DA, et al. . Subjective social status and psychosocial and metabolic risk factors for cardiovascular disease among African Americans in the Jackson Heart Study. Soc Sci Med. 2012;74:1146–1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Thompson LM, Murray KA, Jarvis S, Scarr E. Exploring the relationship between health insurance, social connectedness, and subjective social status among residents of O’ahu. Hawaii J Med Public Health. 2016;75:323–331. [PMC free article] [PubMed] [Google Scholar]
- 42. Adler N, Singh-Manoux A, Schwartz J, Stewart J, Matthews K, Marmot MG. Social status and health: A comparison of British civil servants in Whitehall-II with European- and African-Americans in CARDIA. Soc Sci Med. 2008;66:1034–1045. [DOI] [PubMed] [Google Scholar]
- 43. Freeman JA, Bauldry S, Volpe VV, Shanahan MJ, Shanahan L. Sex differences in associations between subjective social status and C-reactive protein in young adults. Psychosom Med. 2016;78:542–551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Bradshaw M, Kent BV, Henderson WM, Setar AC. Subjective social status, life course SES, and BMI in young adulthood. Health Psychol. 2017;36:682–694. [DOI] [PubMed] [Google Scholar]
- 45. Walsemann KM, Goosby BJ, Farr D. Life course SES and cardiovascular risk: Heterogeneity across race/ethnicity and gender. Soc Sci Med. 2016;152:147–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Perreira KM, Wassink J, Harris KM. Beyond race/ethnicity: Skin color, gender, and the health of young adults in the United States. Popul Res Policy Rev. 2019;38:271–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Harris KM, Halpern CT, Whitsel EA, et al. . Cohort profile: The National Longitudinal Study of Adolescent to Adult Health (Add Health). Int J Epidemiol. 2019;48(5):1415–1415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Nguyen QC, Tabor JW, Entzel PP, et al. . Discordance in national estimates of hypertension among young adults. Epidemiology. 2011;22:532–541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Harris K. The Add Health Study: Design and Accomplishments.2013. https://www.cpc.unc.edu/projects/addhealth/documentation/guides/DesignPaperWave_IIV.pdf. Accessed August 14, 2019.
- 50. Whitsel E, Cuthbertson C, Tabor J, et al. . Add Health Wave IV Documentation: Lipids. 2013. https://www.cpc.unc.edu/projects/addhealth/documentation/guides/Wave_IV_Lipids_documentation.pdf. Accessed August 14, 2019.
- 51. O’Brien P. Procedures for comparing samples with multiple endpoints. Biometrics. 1984;40(4):1079–1087. [PubMed] [Google Scholar]
- 52. Beresford S, Bowen D, Liittman A, et al. . Relationship of socioeconomic status indicators to obesity in Hispanic and non-Hispanic White middle-aged women: A population study. Int J Womens Health Wellness. 2019;5(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Manuck SB, Phillips JE, Gianaros PJ, Flory JD, Muldoon MF. Subjective socioeconomic status and presence of the metabolic syndrome in midlife community volunteers. Psychosom Med. 2010;72:35–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Garza JR, Glenn BA, Mistry RS, Ponce NA, Zimmerman FJ. Subjective social status and self-reported health among US-born and immigrant Latinos. J Immigr Minor Health. 2017;19:108–119. [DOI] [PubMed] [Google Scholar]
- 55. Gong F, Xu J, Takeuchi DT. Beyond conventional socioeconomic status: Examining subjective and objective social status with self-reported health among Asian immigrants. J Behav Med. 2012;35:407–419. [DOI] [PubMed] [Google Scholar]
- 56. Brondolo E. Racial and Ethnic Disparities in health: Examining the contexts that shape resilience and risk. Psychosom Med. 2014;77:2–5. [DOI] [PubMed] [Google Scholar]
- 57. Fleuriet J, Sunil T. The Latina birth weight paradox: The role of subjective social status. J Racial Ethn Health Disparities. 2018;5:747–757. [DOI] [PubMed] [Google Scholar]
- 58. Zvolensky MJ, Paulus DJ, Bakhshaie J, et al. . Anxiety sensitivity and age: Roles in understanding subjective social status among low income adult Latinos in primary care. J Immigr Minor Health. 2018;20:632–640. [DOI] [PubMed] [Google Scholar]
- 59. Wolff LS, Subramanian SV, Acevedo-Garcia D, Weber D, Kawachi I. Compared to whom? Subjective social status, self-rated health, and referent group sensitivity in a diverse US sample. Soc Sci Med. 2010;70:2019–2028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Brown RA, Adler NE, Worthman CM, Copeland WE, Costello EJ, Angold A. Cultural and community determinants of subjective social status among Cherokee and White youth. Ethn Health. 2008;13:289–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Tang KL, Pilote L, Behlouli H, Godley J, Ghali WA; GENESIS-PRAXY investigators . An exploration of the subjective social status construct in patients with acute coronary syndrome. BMC Cardiovasc Disord. 2018;18:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Euteneuer F, Mills PJ, Rief W, Ziegler MG, Dimsdale JE. Subjective social status predicts in vivo responsiveness of β-adrenergic receptors. Health Psychol. 2012;31:525–529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Insaf TZ, Shaw BA, Yucel RM, Chasan-Taber L, Strogatz DS. Lifecourse socioeconomic position and 16 year body mass index trajectories: differences by race and sex. Prev Med. 2014;67:17–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Farmer MM, Ferraro KF. Are racial disparities in health conditional on socioeconomic status? Soc Sci Med. 2005;60:191–204. [DOI] [PubMed] [Google Scholar]
- 65. Assari S. Diminished returns of income against cigarette smoking among Chinese Americans. J Health Econ Dev. 2019;1:1–8. [PubMed] [Google Scholar]
- 66. Everson-Rose SA, Lutsey PL, Roetker NS, et al. . Perceived discrimination and incident cardiovascular events: The multi-ethnic study of atherosclerosis. Am J Epidemiol. 2015;182:225–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Nadimpalli S, Keita A, Wang J, et al. . Are experiences of discrimination related to poorer dietary intakes among South Asians in the MASALA Study? J Nutr Educ Behav. 2017;49:872–876.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Van Dyke ME, Vaccarino V, Quyyumi AA, Lewis TT. Socioeconomic status discrimination is associated with poor sleep in African-Americans, but not Whites. Soc Sci Med. 2016;153:141–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Colen CG, Ramey DM, Cooksey EC, Williams DR. Racial disparities in health among nonpoor African Americans and Hispanics: The role of acute and chronic discrimination. Soc Sci Med. 2018;199:167–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Cooper DC, Milic MS, Mills PJ, Bardwell WA, Ziegler MG, Dimsdale JE. Endothelial function: the impact of objective and subjective socioeconomic status on flow-mediated dilation. Ann Behav Med. 2010;39:222–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Sim AY, Lim EX, Leow MK, Cheon BK. Low subjective socioeconomic status stimulates orexigenic hormone ghrelin – A randomised trial. Psychoneuroendocrinology. 2018;89:103–112. [DOI] [PubMed] [Google Scholar]
- 72. Cheon BK, Hong YY. Mere experience of low subjective socioeconomic status stimulates appetite and food intake. Proc Natl Acad Sci U S A. 2017;114:72–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Ghaed SG, Gallo LC. Subjective social status, objective socioeconomic status, and cardiovascular risk in women. Health Psychol. 2007;26:668–674. [DOI] [PubMed] [Google Scholar]
- 74. Goodman E, Maxwell S, Malspeis S, Adler N. Developmental trajectories of subjective social status. Pediatrics. 2015;136(3):e633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Alcántara C, Chen CN, Alegría M. Do post-migration perceptions of social mobility matter for Latino immigrant health? Soc Sci Med. 2014;101:94–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Garbarski D. Perceived social position and health: Is there a reciprocal relationship? Soc Sci Med. 2010;70:692–699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Boutwell BB, Nedelec JL, Winegard B, et al. . The prevalence of discrimination across racial groups in contemporary America: Results from a nationally representative sample of adults. PLoS One. 2017;12(8):e0183356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Whembolua GL, Davis JT, Reitzel LR, et al. . Subjective social status predicts smoking abstinence among light smokers. Am J Health Behav. 2012;36:639–646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Wilkinson AV, Miller EE, Koehly LM, Daniel CR, Forman MR. Correlates of physical activity differ by sex and country of birth among Mexican-heritage Youth. J Immigr Minor Health. 2017;19:246–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Wilkinson AV, Shete S, Vasudevan V, Prokhorov AV, Bondy ML, Spitz MR. Influence of subjective social status on the relationship between positive outcome expectations and experimentation with cigarettes. J Adolesc Health. 2009;44:342–348. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.