Abstract
Background:
Several studies have investigated the distribution of hip-knee-ankle (HKA) angle in healthy populations; however, few have evaluated this metric in patients undergoing total knee arthroplasty (TKA). The purpose of this study was to compare HKA angle distribution in early and advanced knee osteoarthritis (OA) patients.
Methods:
Full limb radiographs were used to measure HKA angle for 983 subjects from the Osteoarthritis Initiative (OAI) cohort and 4901 pre-TKA patients from an institutional cohort. Measurements were made using a previously-validated deep learning algorithm. Linear regression models were used to determine the association of HKA alignment angle with patient characteristics.
Results:
The mean± standard deviation HKA angle was −1.3° ± 3.2° in the OAI cohort and −4.1° ± 6.1° in the pre-TKA cohort. In the OAI cohort, normal alignment (64%) was the most common knee alignment followed by varus (29%), and valgus (7%). In pre-TKA patients, the most common alignment was varus (62%), followed by normal (27%) and valgus (11%). In pre-TKA patients, mean HKA angle in primary knee OA, post-traumatic knee OA and rheumatoid arthritis patients were −4.3° ± 6.1°, −3.2° ± 6.4° and −2.9° ± 6.1°, respectively. HKA angle was strongly associated (p<0.001) with sex and BMI.
Conclusion:
TKA patients have a wider alignment distribution and more severe varus and valgus alignment than individuals “at risk” for knee OA from the OAI cohort. These epidemiologic findings improve our understanding of HKA angle distribution and its correlation with demographic characteristics in early and late-stage arthritis.
Keywords: knee coronal alignment, osteoarthritis epidemiology, artificial intelligence, deep learning, knee arthroplasty
Introduction
Hip-knee-ankle (HKA) angle is defined as the angle formed by the mechanical axis of the femur and tibia as measured on a full limb radiograph (1). In a neutrally aligned knee, this line passes from the center of the femoral head, through the midpoint between the tibia intercondylar eminences, and through the center of the talus. HKA angle has an important role in proportional load distribution between medial and lateral compartments of the knee joint. While in a neutrally aligned knee, 60–70% of knee force passes across the medial compartment during daily activity, in varus and valgus knees the force passes disproportionately through the medial and lateral compartments, respectively (2, 3).
HKA angle is an important measure of the lower limb due to its association with knee osteoarthritis (OA) and its application for preoperative planning in knee joint reconstruction surgeries such as osteotomies and knee arthroplasty (4, 5). Severity of lower limb malalignment is associated with progression of knee OA, magnitude of cartilage loss as assessed by magnetic resonance imaging (MRI) and quantitative joint loss on radiographs (6–8).
There are several studies that investigated the distribution of knee alignment in healthy individuals (9–12). Yet relatively little is known how knee alignment differs in early and advanced knee OA patients. This is in part due to the need for full length lower extremity radiographs for HKA angle measurement, which in turn makes large scale epidemiologic studies cumbersome and expensive. In a small study by Cooke et al (13), investigators showed that knee alignment in 167 patients with knee OA (−3.95 ± 7.75) differed significantly from 119 healthy adults (−0.97 ± 2.68) and overall alignment was more varus by approximately 3°. Furthermore, Brouwer et al (8) investigated the association between knee malalignment and the development and progression of knee OA in 1,501 participants, but the study was limited since it relied on anatomic axis in knee radiographs instead of the mechanical axis in full-limb radiographs.
We therefore aimed to compare HKA angle distribution in two large cohorts representing different stages of knee OA. One cohort included individuals from the Osteoarthritis Initiative (OAI) with either established knee OA or significant risk factors for development of knee OA. The other cohort included individuals with advanced symptomatic knee OA who underwent TKA (pre-TKA). We compared the distribution of HKA angles in these cohorts, and examined the association between HKA angle with age, sex, body mass index (BMI), and the etiology of arthritis. We hypothesized that HKA angle distribution would differ in these cohorts and by patient characteristics.
Patients and Methods
The study population included two cohorts: 983 subjects from the OAI cohort and 4901 TKA patients from the institutional joint replacement registry. Mean age of the 983 OAI subjects was 61.5 ± 9.1 years, mean BMI was 27.6 ± 4.3 kg/m2, mean KL (Kellgren and Lawrence) grade was 1.08 ± 1.14 and 53%were female. Briefly, the OAI is a publicly available, longitudinal, observational cohort study of individuals with either established knee OA or with significant risk factors for development of knee OA (14). The institutional TKA cohort comprised 4901 patients with advanced symptomatic knee OA who underwent TKA surgery between 2000 and 2017 and had full limb pre-surgery radiographs available. Mean age of the 4901 pre-TKA patients was 66 ± 10.4 years, mean BMI was 31.7 ± 6 kg/m2, and 55% were female. Age and BMI were similar between males and females (Table 1). The most common etiology for TKA was primary knee OA (83%), followed by post-traumatic arthritis (14%) and rheumatoid arthritis (RA) (1%).
Table 1.
Characteristics of 4901 institutional pre-TKA patients
| Characteristic | Male | Female | Total |
|---|---|---|---|
| Number of patients | 2203 | 2698 | 4901 |
| Age ± SD (years) | 66.5 ±10.4 (range, 17–96) | 65.5 ±10.4 (range, 22–96) | 66 ±10.4 (range, 17–96) |
| Height ± SD (cm) | 177.4 ± 36.8 (range, 153–200) | 162.3 ±13.7 (range, 109–89) | 169.1 ± 27.7 (range, 109–200) |
| Weight ± SD (kg) | 98 ± 18.5 (range, 58–174) | 84.3 ± 18.6 (range, 37–172) | 90.4 ± 19.7 (range, 37–174) |
| Body Mass Index ± SD (kg/m2) | 31.3 ± 5.3 (range, 18.1–56.8) | 31.9 ± 6.6 (range, 15.6–61.2) | 31.7 ± 6 (range, 15.6–61.2) |
| Arthritis etiology (% of total) | |||
| Primary osteoarthritis | 1747 (79.3%) | 2323(86.1%) | 4070 (83.0%) |
| Post-traumatic osteoarthritis | 380 (17.2%) | 288 (10.7%) | 668 (13.6%) |
| Rheumatoid arthritis | 16 (0.7%) | 29 (1.1%) | 45 (0.9%) |
| Other | 60 (2.7%) | 58 (2.1%) | 118 (2.4%) |
For measurement of the HKA angles, we used a previously developed and validated deep learning algorithm (15). Briefly, the deep learning algorithm was developed using radiographs from the OAI cohort and validated using institutional radiographs. The mean difference between human-level and machine-level HKA measurements was 0.44° ± 0.35°, and differences of 1.5° or more between human-level and machine-level measurements were observed in less than 0.6% of cases, indicating almost perfect performance. By convention, varus angles were indicated by negative numbers and valgus angles were indicated by positive numbers. Knees were considered as having varus malalignment if the HKA angle was −3° or less, as normal if the HKA angle was between −3° and +3°, and as having valgus malalignment if the HKA angle was 3° or more.
Statistical analysis:
Demographic data were presented using means and standard deviations for continuous data and counts and percentages for categorical data, as appropriate. To account for issues of multiple testing, we employed a multivariate analysis of variance (MANOVA) test to evaluate relationships between age, sex, BMI, and etiology of arthritis with HKA angles. We explored several alternative models that included transformations of the BMI variable (i.e., square root BMI, log BMI, cube root BMI, BMI squared, BMI cubed) to account for curvilinear relationships of BMI with HKA angles as well as interaction terms. The R-square values for different models were relatively low at 0.05 and 0.09 for both legs. Each BMI transformation resulted in changes to the R-square of only tenths or hundredths of a percent. Thus, none were deemed to be a significant improvement to the model’s ability to explain variation in HKA angles. The untransformed BMI was used for all analyses. Similarly, the R-square values in models with and without the sex*BMI interaction term were similar a R-square differences of about 0.1% in the left leg, and 0.3% in the right leg. All statistical analyses were performed using [SAS/STAT] software, Version [9.4] of the SAS System for [Unix], copyright 2016 SAS Institute Inc., Cary, NC, USA. P-values <0.05 were considered statistically significant.
Results
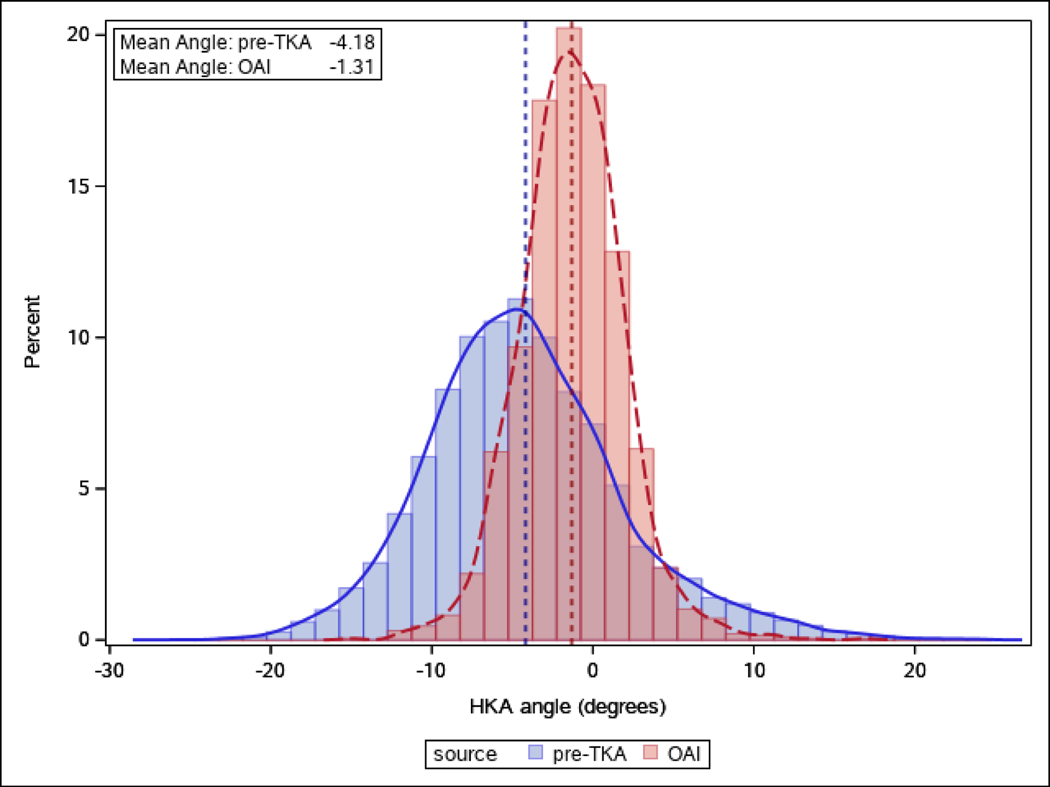
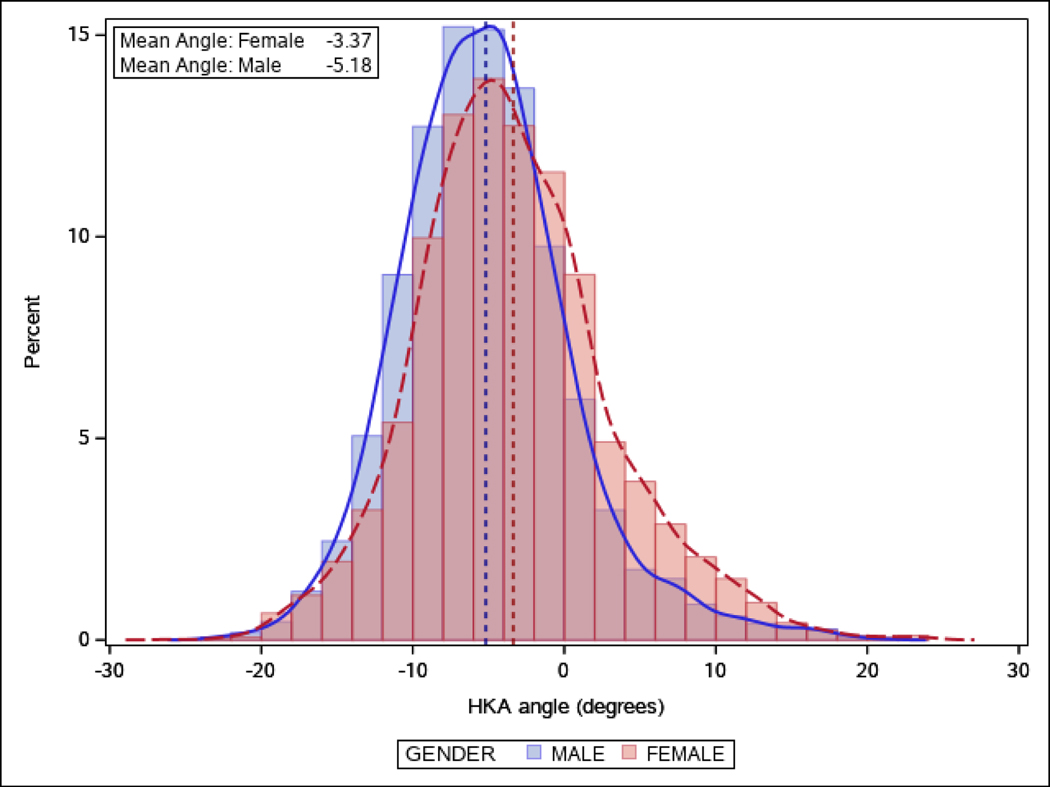
Mean HKA angle for the 983 OAI subjects was −1.3° ± 3.2° (Figure 1). Mean HKA angle in male and female subjects were −1.9° ± 3.2° and −0.8° ± 3.1°, respectively. The most common categorical knee alignment was normal (64%) followed by varus (29%), and valgus (7%). The distribution of the HKA angle among the 4901 pre-TKA patients in the institutional cohort was wider than the OAI cohort with a mean of −4.1° ± 6.1° and a median of −4.6° (Figure 1). The most common categorical knee alignment was varus (62%), followed by normal (27%) and valgus (11%). Mean HKA angle in male and female patients was −5.2° ± 5.6° and −3.3° ± 6.4°, respectively (Figure 2). While there was similar male to female ratio in varus malalignment knees (50%), valgus malaligned knees were more common among female compared to male patients (71% versus 29%). Normal knee alignment was more common among females compared to males (60% versus 40%). Mean HKA angle in primary knee OA, post-traumatic knee OA and rheumatoid arthritis patients were −4.3° ± 6.1°, −3.2° ± 6.4° and −2.9° ± 6.1°, respectively (Table 2).
Figure 1.
Distribution of hip-knee-ankle (HKA) angle and mean HKA in 983 of OAI participants and 4901 institutional pre-TKA patients.
Figure 2.
Distribution of hip-knee-ankle (HKA) angle and mean HKA of 2203 male and 2698 female institutional pre-TKA patients
Table 2.
HKA angle measurements by arthritis etiology in 4901 institutional pre-TKA patients
| Characteristic | Male (N=2203) | Female (N=2698) | All (N=4901) |
|---|---|---|---|
| HKA angle ± range | −5.2° ± 5.6° | −3.3° ± 6.4° | −4.1° ± 6.1° |
| Primary osteoarthritis | −5.4° ± 5.5° | −3.5° ± 6.4° | −4.3° ± 6.1° |
| Post-traumatic osteoarthritis | −4.1° ± 6.3° | −2.2° ± 6.4° | −3.2° ± 6.4° |
| Rheumatoid Arthritis | −4.8° ± 4.4° | −1.8° ± 6.7° | −2.9° ± 6.1° |
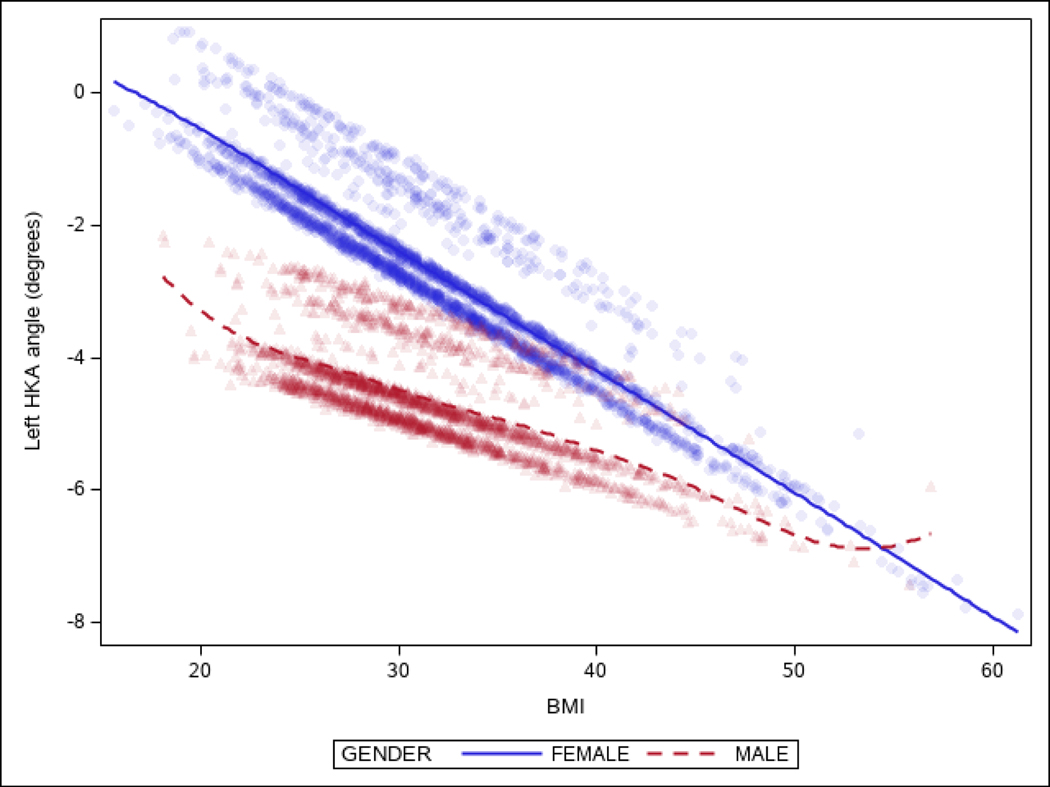
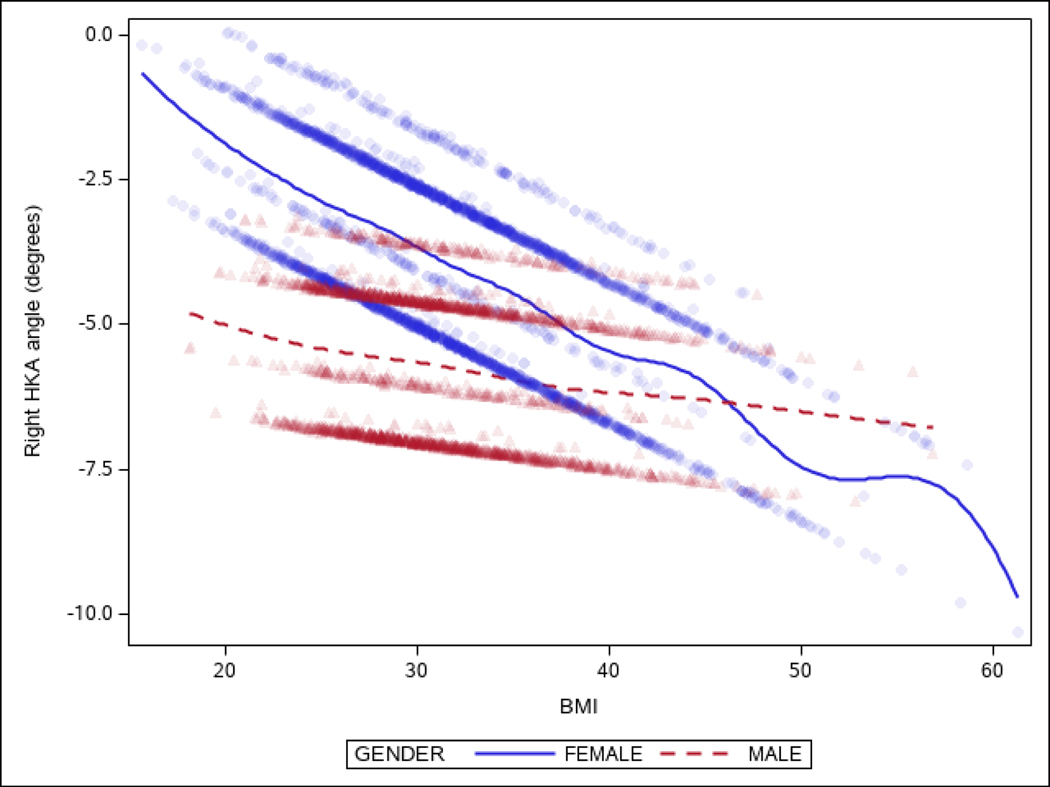
In MANOVA (Table 3), we observed strong associations (p<0.001) between HKA angle with sex and BMI and a significant quantitative interaction between sex and BMI (p<0.001). The association between BMI and HKA angles was different in females and in males (Figures 3A and 3B). At lower BMI, HKA angles were more varus in males than in females. However, at higher BMI, HKA angles were more varus in females than in males. For example, mean HKA angle was −1.3° in male patients with a normal BMI (18.5–25 kg/m2) and −3.8° in female patients with a normal BMI, corresponding to a difference of 2.5°. At a BMI of >40kg/m2, mean HKA angle was −5° in both females and males with a difference of only 0.5° (Figure 3A and 3B).
Table 3.
Association of patient characteristics with HKA angles in 4901 institutional pre-TKA patients
| Characteristic | F-Value | p-value |
|---|---|---|
| Age | 0.64 | 0.5268 |
| Sex | 17.52 | <0.0001 |
| Body Mass Index | 38.77 | <0.0001 |
| Arthritis etiology | 6.38 | <0.0001 |
| Sex*Body Mass Index | 6.83 | 0.0011 |
Figure 3A.
Distribution of left HKA angles by body mass index (BMI)in males and females.
Figure 3B.
Distribution of right HKA angles by body mass index (BMI) in males and females.
Discussion
Lower limb malalignment as measured by the HKA angle is an established risk factor for knee OA. A better understanding of the distribution of HKA angle over time and how it relates to other knee OA risk factors is important to understand the etiology of knee OA, enhance preoperative planning, and potentially enable more patient-specific TKA alignment targets. However, measurement of the HKA angle is a cumbersome task in research settings for large patient cohorts. We used a previously-validated deep learning model to automatically measure HKA angle in two large cohorts of patients representing both early and advanced knee OA. Our findings indicate that the distribution of knee alignment differ significantly in early and advanced knee OA. In pre-TKA patients, knee alignment is strongly associated with both sex and BMI, and the association between BMI and knee alignment differs in females and males.
The first notable finding of our study is the significant difference in HKA angles in the OAI cohort and the institutional pre-TKA patients. While the OAI population is a selected group of participants (16) at high risk for knee OA (14), our institutional cohort was comprised of patients with advanced radiographic and symptomatic knee OA with plans for TKA. Therefore, the most common alignment in the OAI dataset was normal (between −3° to 3°), whereas the most common alignment among the pre-TKA patients was varus. This finding is consistent with previous studies reporting on HKA angle in healthy and low-grade knee OA populations (9, 11–13, 17).
In pre-TKA patients, we examined the cross-sectional association of HKA angles with four patient characteristics: age, sex, BMI, and arthritis etiology. Male patients had more varus knee malalignment compared to female patients overall, but this difference was highly variable between BMI categories. Another important finding is that about 40% of the pre-TKA cohort had either normal or valgus knee alignment. Female to male ratio was 3:2 in the normal knee alignment group and was even higher (about 2.5:1) in the valgus knee malalignment group. High BMI is a well-known risk factor for knee OA and most patients in our preoperative cohort were obese. We found that every 5 kg/m2 increase in BMI was associated with −0.60° change in HKA angle. Furthermore, we found that HKA angles were more varus in males than in females at lower BMI and the opposite at higher BMI. This finding is in agreement with a previous study of 300 subjects with OA (18) which showed BMI and malalignment were correlated in varus knees but not in those with valgus knees. In terms of etiology, all three arthritis etiologic groups (OA, RA, post-traumatic) had mean varus malalignment with primary OA being the most pronounced.
Although we could not find any studies reporting on HKA angle measurements in preoperative full-limb radiographs of patients who underwent TKA, there are a few studies that investigated HKA angle distribution in full-limb radiographs of individuals with knee OA. Cooke et al (13) measured HKA angles in 167 participants with symptomatic knee OA with a mean age of 66 years. Overall alignment in this group was 3° varus, and HKA angle in male and female patients were −5.9° and −2.3°, respectively and categorically male patients were more likely to have varus whereas female patients were more likely to have valgus knee OA. In a study by Kraus et al (17), HKA angle was measured in 57 participants (40 female and 17 male) with symptomatic knee OA with a mean age of 67 years. They graded severity of knee OA based on the standard Kellgren and Lawrence radiographic system and reported HKA angle for each group. HKA angle in their population ranged from 16° varus to 13° valgus alignment. They did not observe any association between age and HKA angle, but the severity of knee OA and BMI were associated with HKA angle. It is important to note that a few studies reported on knee alignment angle based on knee anteroposterior (AP) radiographs instead of full limb radiographs (8, 19, 20). Although there is a correlation between mechanical and anatomical alignment (17, 21), this method is not optimal since the anatomical axis has approximately 4–6 degrees of femoral valgus compared to mechanical axis, and cannot account for extraarticular deformities (17).
There are several potential limitations of this study. First, although our model had high precision in measuring HKA angles and we randomly annotated and checked images in different alignment ranges which showed acceptable precision (mean error of 1.7°), there is still a chance that errors in our model prediction could affect the distribution of the alignment angle in our cohort. Second, the study reports knee alignment results in only a subset of subjects from the OAI and pre-TKA patients from an academic institution. Selection bias is a concern when only a subset of subjects is included from both cohorts. Importantly, we did not have data on Kellgren and Lawrence grades in pre-TKA patients and therefore, are unable to examine alignment distribution by OA grade. However, the large cohort size, inclusion of subjects with discrepant knee OA severity and association with other patient characteristics are the unique strengths of the study. Finally, we did not have computer tomography (CT) data for our cohort to use as a ground truth for HKA angle measurement. Therefore, we could not study the effect of the limb rotation on HKA angle measurements. Despite these limitations, this study demonstrates the potential of deep learning tools to measure hard-to-ascertain radiographic features in large scale research projects with relative ease and speed. It takes one second for the algorithm to measure HKA angle in each image. For the future direction of this study, we will use the same approach and a validated algorithm to measure HKA angles in post-TKA images which would make it feasible to correlate post-TKA angle with patient outcome and longevity of the prosthesis.
In conclusion, patients presenting for TKA have a wider alignment distribution and more severe varus and valgus alignment than individuals “at risk” for knee OA from the OAI cohort. Males tend to have more varus alignment than females and females have a higher likelihood to be in categorical valgus. BMI has a strong association with knee alignment and more prominently in females with a trend toward varus alignment as BMI increases. These epidemiologic data can serve as a benchmark for future studies and potentially improve understanding of preoperative to postoperative alignment change in TKA patients and how this influences survivorship, function, and patient satisfaction.
Supplementary Material
Acknowledgments
Funding: This work was supported by the National Institutes of Health (NIH) [grant numbers R01AR73147 and P30AR76312] and Mayo Benefactor Funded Career Development Grant.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.WM M. Arthroplasty of the Knee. Campbell’s Operative Orthopaedics. 13th ed. Philadelphia, PA: Elsevier, Inc; 2017. p. 405–7. [Google Scholar]
- 2.Andriacchi TP. Dynamics of knee malalignment. The Orthopedic clinics of North America. 1994;25(3):395. [PubMed] [Google Scholar]
- 3.Tetsworth K, Paley D. Malalignment and degenerative arthropathy. Orthopedic Clinics of North America. 1994;25(3):367–78. [PubMed] [Google Scholar]
- 4.Coventry MB, Ilstrup DM, Wallrichs SL. Proximal tibial osteotomy. A critical long-term study of eighty-seven cases. The Journal of Bone and Joint surgery American Volume. 1993;75(2):196–201. [DOI] [PubMed] [Google Scholar]
- 5.Hernigou P, Deschamps G. Alignment influences wear in the knee after medial unicompartmental arthroplasty. Clinical Orthopaedics and Related Research®. 2004;423:161–5. [DOI] [PubMed] [Google Scholar]
- 6.Cicuttini F, Wluka A, Hankin J, Wang Y. Longitudinal study of the relationship between knee angle and tibiofemoral cartilage volume in subjects with knee osteoarthritis. Rheumatology. 2004;43(3):321–4. [DOI] [PubMed] [Google Scholar]
- 7.Sharma L, Song J, Felson DT, Cahue S, Shamiyeh E, Dunlop DD. The role of knee alignment in disease progression and functional decline in knee osteoarthritis. Jama. 2001;286(2):188–95. [DOI] [PubMed] [Google Scholar]
- 8.Brouwer G, Tol AV, Bergink A, Belo J, Bernsen R, Reijman M, et al. Association between valgus and varus alignment and the development and progression of radiographic osteoarthritis of the knee. Arthritis & rheumatism. 2007;56(4):1204–11. [DOI] [PubMed] [Google Scholar]
- 9.Bellemans J, Colyn W, Vandenneucker H, Victor J. The Chitranjan Ranawat Award: is neutral mechanical alignment normal for all patients?: the concept of constitutional varus. Clinical Orthopaedics and Related Research®. 2012;470(1):45–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fahlman L, Sangeorzan E, Chheda N, Lambright D. Older adults without radiographic knee osteoarthritis: knee alignment and knee range of motion. Clinical Medicine Insights: Arthritis and Musculoskeletal Disorders. 2014;7:CMAMD. S13009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.HSU RW, HIMENO S, COVENTRY MB, CHAO EY. Normal axial alignment of the lower extremity and load-bearing distribution at the knee. Clinical Orthopaedics and Related Research®. 1990;255:215–27. [PubMed] [Google Scholar]
- 12.Moreland JR, Bassett L, Hanker G. Radiographic analysis of the axial alignment of the lower extremity. The Journal of bone and joint surgery American volume. 1987;69(5):745–9. [PubMed] [Google Scholar]
- 13.Cooke D, Scudamore A, Li J, Wyss U, Bryant T, Costigan P. Axial lower-limb alignment: comparison of knee geometry in normal volunteers and osteoarthritis patients. Osteoarthritis and cartilage. 1997;5(1):39–47. [DOI] [PubMed] [Google Scholar]
- 14.Nevitt M, Felson DT, Lester G. The Osteoarthritis Initiative: protocol for the cohort study [accessed February 8, 2022]. Available from: http://oai.epi-ucsf.org/datarelease/docs/StudyDesignProtocol.pdf
- 15.Yan S, Ramazanian T, Maradit Kremers H, & Chaudhary V. (2022). HKAA-prediction-on-preoperate-images (Version 1.0.0) [Computer software]. 10.5281/zenodo.1234 [DOI]
- 16.Fawaz-Estrup F. The osteoarthritis initiative: an overview. Rhode Island Medical Journal. 2004;87(6):169. [PubMed] [Google Scholar]
- 17.Kraus VB, Vail TP, Worrell T, McDaniel G. A comparative assessment of alignment angle of the knee by radiographic and physical examination methods. Arthritis & Rheumatism. 2005;52(6):1730–5. [DOI] [PubMed] [Google Scholar]
- 18.Sharma L, Lou C, Cahue S, Dunlop DD. The mechanism of the effect of obesity in knee osteoarthritis: the mediating role of malalignment. Arthritis & Rheumatism: Official Journal of the American College of Rheumatology. 2000;43(3):568–75. [DOI] [PubMed] [Google Scholar]
- 19.Goulston LM, Sanchez-Santos MT, D’Angelo S, Leyland KM, Hart DJ, Spector TD, et al. A comparison of radiographic anatomic axis knee alignment measurements and cross-sectional associations with knee osteoarthritis. Osteoarthritis and cartilage. 2016;24(4):61222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Harvey WF, Niu J, Zhang Y, McCree PI, Felson DT, Nevitt M, et al. Knee alignment differences between Chinese and Caucasian subjects without osteoarthritis. Annals of the rheumatic diseases. 2008;67(11):1524–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hinman RS, May RL, Crossley KM. Is there an alternative to the full-leg radiograph for determining knee joint alignment in osteoarthritis? Arthritis Care & Research: Official Journal of the American College of Rheumatology. 2006;55(2):306–13. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.