Abstract
Background and Objectives:
While inadequate nutrition can weaken the immune system and lead to negative health sequelae for vulnerable populations, little is known about nutritional intake among people who inject drugs (PWID). We aimed to quantify nutritional intake among PWID and to explore associations between protein intake and drug use.
Methods:
A cross-sectional design was used to analyze self-reported participant data. PWID were recruited from community settings in California in 2016/17. Participants reported on food consumption per day for a 30-day period, from which a continuous protein intake variable was created.
Results:
Modal characteristics of participants (N=937) were: white (42.5%), male (75.3%), healthy BMI (56.6%), and unhoused (82.9%). Less than 1% of participants met or exceeded recommended guidelines for protein intake (0.80 grams per day per 1 kg body weight). The final multiple regression model found protein intake to be significantly positively associated with older age, high school or greater education, frequency of opiate and marijuana use, while Latinx ethnicity was inversely associated with protein intake, adjusting for gender.
Discussion and Conclusions:
Our study shows PWID are generally not underweight, yet they are grossly protein deficient, which can be harder to recognize. Poverty, homelessness, and other structural barriers likely contribute to this issue, which demonstrates the need for communities to provide more access to nutrient-rich food to PWID.
Scientific Significance:
Our findings demonstrate the novel findings that opiate and marijuana use frequency, but not stimulants (methamphetamine and cocaine) may increase preference for protein-rich foods among PWID.
Introduction
People who inject drugs (PWID) in the United States face barriers to basic human needs such as shelter, food, and healthcare. Research has shown that food insecurity, defined by Anderson1 as “limited or uncertain availability of nutritionally adequate and safe foods, or limited or uncertain ability to acquire acceptable foods in socially acceptable ways,” is highly prevalent among PWID.2,3,4 In 2019, the prevalence of being food insecure anytime in the past 12 months was 10.5% among the general population of U.S. adults.5 Among PWID living in Los Angeles and San Francisco, the prevalence of food insecurity is over four times the national average-- as high as 58%.3 Furthermore, over half of PWID in Ontario, Canada (60.4%) reported not being able to eat the quality or quantity of food that they wanted on a daily or weekly basis.4 While there is considerable research on food insecurity among under-served communities, there is a lack of studies reporting on intake of essential constituents of the human diet such as protein among PWID.
The total caloric energy intake of people who use drugs (PWUD) has been found to be lower than the general population’s by as much as 23%.6 Nutrient deficiencies are prevalent in this population,7 and protein may only account for 1/10 of total energy intake among PWUD.6 Inadequate protein intake (along with vitamin, mineral, and total caloric intake), can lead to muscle wasting,8 poor wound healing,9 and greater risk of infection due to impaired immunity.10 The U.S. Department of Agriculture (USDA) recommends an average consumption of 50 grams of protein or 0.8 grams per 1 kg of body weight per day.11 The majority of Americans meet or exceed protein guidelines as set forth by the USDA; in 2016, American men consumed an average of 97 grams/day and females 69 grams/day of protein.12
Only half of people who use drugs use (PWUD) in a small Norwegian study (N=195) had a protein intake that met the accepted maintenance requirements, although it was noted that the deficiencies were likely a result of overall low food intake.6 When people use opioids, they have been reported to consume high amounts of sugar and sweets,13,14 cheap and convenient food,13,15 and to have little interest in food during active heroin use.15 Similarly, when people use methamphetamine, they also have a higher consumption of sugary beverages and snacks.16 Use of stimulants (including methamphetamine and cocaine) often leads to decreased appetite,17 and crack cocaine use may be associated with reduced protein intake.18
Chronic malnutrition can lead to negative health effects that compound the dangers of injecting drug use and may exacerbate co-morbidities. PWID are at a greater risk of having lower body weight and intake of micronutrients such as zinc, calcium, iron, fiber, folate, and vitamins A, C, and E than people who do not use drugs.19,20 Intravenous drug use and alcohol consumption may interfere with the absorption of nutrients, alter appetite and metabolism, and impair immunity.15,17,21 Decreased immunity can lead to secondary infections in those who have chronic immune disorders (e.g. HIV), which can lead to weight loss, and can impair nutrient intake as these diseases progress.22,23 Thus, adequate nutrition is important for PWID, especially those with other health conditions such as HIV, hepatitis, or other infections. Malnutrition can lead to negative health sequelae in a population that is already at an increased risk of morbidity and mortality resulting from acute or chronic diseases.24
To date, there are few studies on diet among PWID, especially as it regards protein consumption, which is a vitally important macronutrient. This study aimed to quantify protein intake among PWID in Los Angeles and San Francisco and explore associations between protein intake and drug use.
Methods
Recruitment
Data was collected between 2016 and 2017 as part of a randomized controlled trial to evaluate the “Change the Cycle” intervention. Participants were recruited from community settings using target sampling methods in Los Angeles and San Francisco.25–27 Eligibility criteria include 18 years of age or older, and self-reported drug injection in the last 30 days, verified by visual inspection for signs of recent venipuncture or track marks.28 Eligible and consenting participants completed a baseline interview with questions on multiple domains including demographics, current and past drug use patterns, health status, injection-drug use risk behaviors, and food consumption. The University of Southern California Institutional Review Board (IRB) approved all protocols.
While the original trial is longitudinal, this paper only reports on the cross-sectional analysis of the baseline data, which consists of 984 participants. Of the 984 participants, 24 were missing all food consumption data. We also removed an additional 23 participants using case wise diagnostics (inspecting residuals and removing outliers outside 3 standard deviations) resulting in a final sample size of N= 937 (4.8% of total sample missing). Of the final sample, 892 participants had complete height and weight data (measured by research staff), which was used to create two BMI variables (numerical and categorical).
Measures
Items concerning food consumption were modeled on questions appearing in the 2015 National Health Interview Survey from the Centers for Disease Control and Prevention.29 Questions regarding nutrition were framed as: “In the last 30 days, how often did you eat at least an ounce of _____?” These sources included: chicken, beef, fish, eggs, nuts and seeds, tofu, beans, cheese, and yogurt. Drug use was measured by the question “In the last 30 days, how often did you use _____?” The protein intake variable was created by adding weights to each protein source according to its protein value (in grams) by ounce. The weights were assigned as follows (grams of protein per ounce consumed): tofu and yogurt: 2; nuts and seeds: 5; fish, eggs, and beans: 6; cheese and beef: 7; chicken 8.11 A continuous variable of past-30-day protein intake (grams) was created that added together all weighted sources of protein within the last 30 days. Upon examination of protein intake, and all past-30- day drug use variables, it was noted that the variables were highly skewed, and so were log transformed to normalize the distribution for analysis.
Prior research has indicated that drug use patterns can influence nutritional intake and food insecurity,3,13,14,15, 19,20 so we examined whether drug use pattern and frequency were associated with protein intake. We collected data on the following drugs by times used through injection and non-injection routes: heroin, cocaine, crack cocaine, methamphetamine, combinations of heroin with cocaine (i.e. speedball) and heroin with methamphetamine (i.e. goofball), prescription opioids, tranquilizers, sedatives, stimulants, marijuana, and alcohol in the last 30 days. Other relevant measures included demographics (i.e., race, gender, age, education), months of being homeless, HIV and HCV status, food insecurity in the last 30 days, drug treatment involvement (i.e., methadone detoxification, methadone maintenance, buprenorphine, inpatient, outpatient, and residential), and criminal legal involvement in the last 6 months (any police contact, any arrest, any jail stays).
Data Analysis
A one-sample t-test was conducted to determine if mean protein intake was similar to the USDA Nutrition Guidelines (50 grams/day *30 =1,500 grams/month). Bivariate linear regression was conducted with the log-transformed protein intake variable as the dependent variable to investigate the association between protein intake and covariates identified in the literature such as unstable housing,2 relationship status,3, income,4,30 gender4 age,4 education,30 drug use,30 drug treatment,15 race,31 and engagement with the criminal justice system.14 Covariates which were significant at p < 0.05 in the bivariate analysis were then included in a final multiple linear regression model, using a stepwise regression method to achieve optimal results for the final model. Data analysis was conducted using SPSS Version 25.32
Results
Descriptive statistics of our final sample of PWID are presented in Table 1. Modal characteristics of our sample were: White (42.5%), male (75.3%), healthy BMI (56.5%), possessing high school education or greater (72.4%) and unhoused (82.9%) with a median (IQR) age of 43 (31-52). Half (51.7%) of participants were recruited from one site in San Francisco, while the other half were spread among three different sites in Los Angeles (specifically Hollywood, Skid Row/Downtown LA, and East Los Angeles). Heroin/opiates was the most frequently used drug, with 91% of our sample endorsing use in the last 30 days with a median of 90 times used (roughly 3x per day), followed by methamphetamine (78% of sample used in the past 30 days, median 24 uses). Most of our sample (77.5%) had ever participated in substance use/alcohol treatment, and a quarter (27.4%) had participated in methadone maintenance treatment in the last 6 months. Although the majority of our sample reported less than $1,000 of income in the past month (54.0%), only 4% stated they had received no income. Common income sources endorsed by participants included welfare and food stamps (42%), illegal activities (40.3%), panhandling (26.9%), recycling (22.4%), and SSI or retirement benefits (12.9%).
Table 1:
Demographic characteristics, drug use, and protein intake among people who inject drugs in Los Angeles and San Francisco (N=937)
| Frequency Variables | N(%) | Continuous Variables | Median (IQR) |
|---|---|---|---|
|
| |||
| Gender | Protein consumption, past 30 days (grams) | 428 (266-623.5) | |
| Male | 706 (75.3%) | ||
| Female | 226 (23.0%) | ||
| Transgender | 9 (0.9%) | ||
| Other | 5 (0.5%) | ||
|
| |||
| High school education or more | 678 (72.4%) | Daily protein consumption, grams per weight (kg) | 0.20 (0.12-0.28) |
|
| |||
| BMI category | BMI (kg/m2) | 23.7 (21.6-26.5) | |
| Underweight | 22 (2.2%) | ||
| Healthy | 557 (56.6%) | ||
| Overweight | 263 (26.7%) | ||
| Obese | 83 (8.4%) | ||
|
| |||
| Homeless / unstably housed | 777 (82.9%) | Months homeless / unstably housed | 36 (12-80) |
|
| |||
| Any alcohol or substance use disorder treatment, lifetime | 763 (77.5%) | Age | 43 (31-52) |
|
| |||
| Substance use treatment, last 6 months | Years since first injection | 19 (7-32) | |
| Methadone maintenance | 257 (27.4%) | ||
| Outpatient | 173 (18.5%) | ||
| Methadone detoxification | 136 (14.5%) | ||
| Residential | 112 (12.0%) | ||
| Inpatient | 111 (11.8%) | ||
| Buprenorphine | 76 (8.1%) | ||
|
| |||
| Race/ethnicity | Times used drug , past 30 days | ||
| White | 398 (42.5%) | ||
| Latinx | 221 (23.6%) | Total # of injections | 92 (43-167) |
| Black | 187 (20.0%) | Total # of non-injections | 36 (12-96) |
| Native American | 63 (6.7%) | Heroin/Opiates | 90 (30-150) |
| Asian/Pacific Islander | 10 (1.1%) | Cocaine | 2 (0-21) |
| Mixed Race/Other | 58 (6.3%) | Methamphetamine | 24 (1.25-75) |
| Marijuana | 20 (5-50) | ||
|
| |||
| Income | |||
| Less than $1,000 | 506 (54.0%) | ||
| $1,000 to $1,400 | 150 (16.0%) | ||
| $1,401 to $2,100 | 129 (13.8%) | ||
| $2,101 or more | 150 (16.0%) | ||
|
| |||
| Engagement with criminal justice | |||
| Currently on parole | 35 (3.7%) | ||
| Currently on probation | 232 (24.8%) | ||
|
| |||
| Relationship status | |||
| Single, no main partner | 677 (68.8%) | ||
| Casual sex partner in last 6 months | 334 (33.9%) | ||
| Steady sex partner in last 6 months | 460 (46.7%) | ||
|
| |||
| Area of recruitment | |||
| San Francisco | 484 (51.7%) | ||
| Los Angeles: Skid Row | 240 (25.6%) | ||
| East Los Angeles | 107 (11.4%) | ||
| Hollywood | 106 (11.3%) | ||
|
| |||
| Couldn’t eat balanced meals in the last 30 days | |||
| Never true | 154 (16.4%) | ||
| Sometimes true | 322 (34.4%) | ||
| Often true | 461 (49.2%) | ||
Among participants (N=937), only 1% met the recommended dietary allowance (RDA) of 1,500 grams/month of protein as defined by the USDA. The median (IQR) protein intake was 428 grams/month (266-623.5) among PWID in this sample. The monthly median protein intake was 1,072 grams below guidelines recommended by the USDA (p<0.0001; Figure 1). Of the slightly smaller sample of participants (N=892) that had complete height and weight data, only 22 participants (2.2%) had a BMI that was classified as underweight. For this sub-set of PWID, median daily protein intake (grams) per 1 kilogram of body weight was 0.20 (IQR = 0.12-0.28), which is well below the recommended 0.80 grams/kg a day (Figure 2). Additionally, 83.6% of our sample indicated that they couldn’t eat balanced meals ‘sometimes’ or ‘often’ in the past 30 days.
Figure 1:
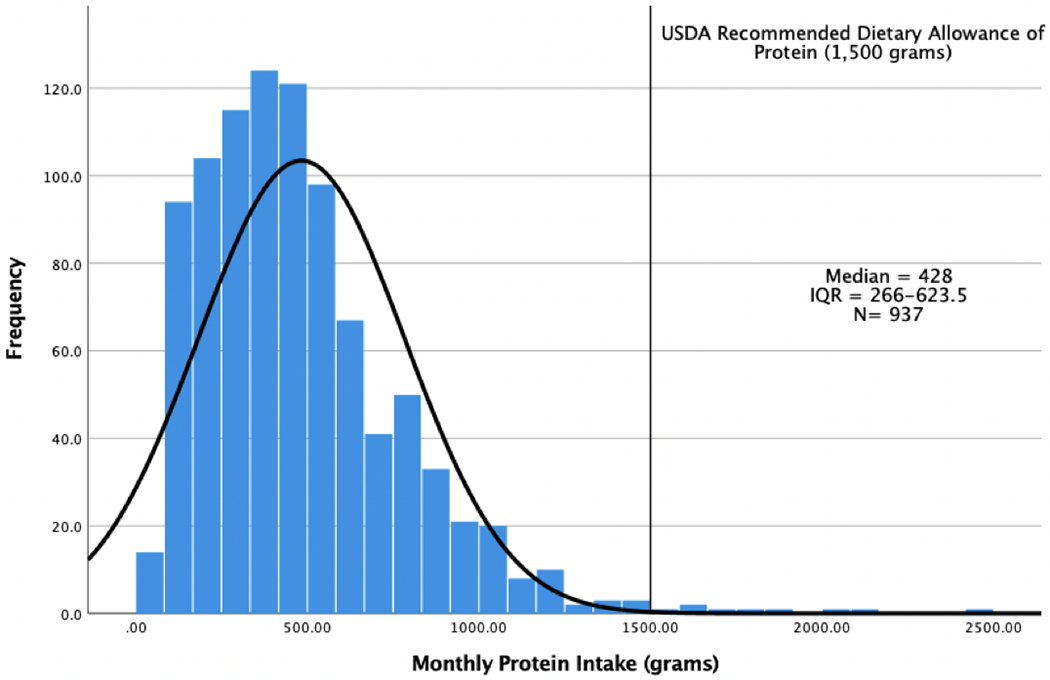
Distribution of Protein Intake among PWID
Figure 2:
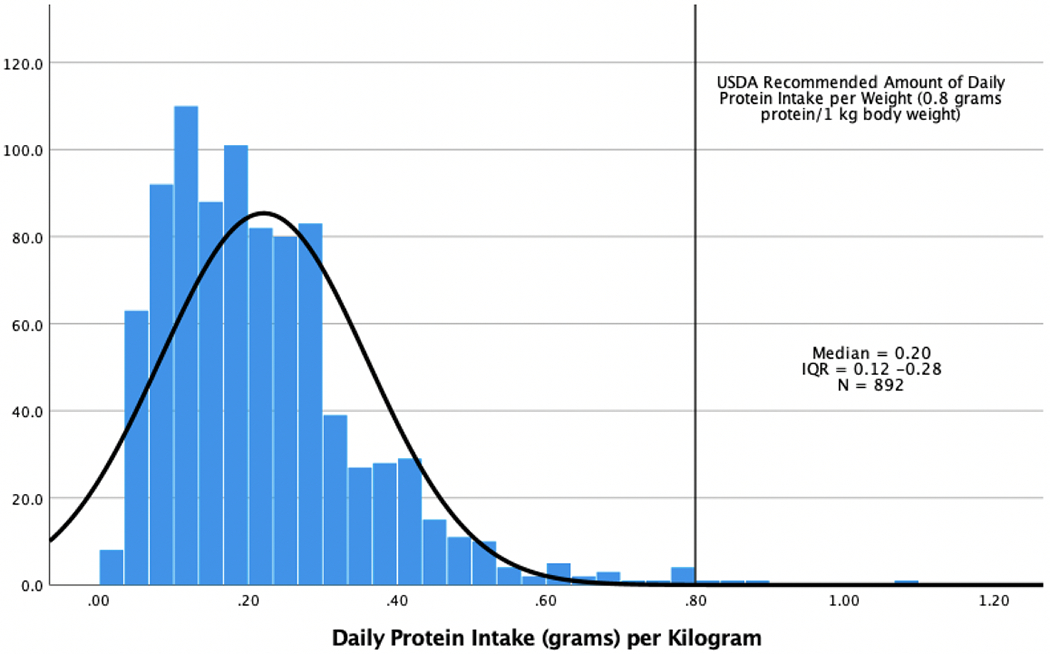
Distribution of Daily Protein Intake(grams) per Body Weight (kg) among PWID
Bivariate linear regression analysis showed that the following sociodemographic variables were significantly associated with past 30-day protein intake (Table 2): age (p=0.05), identifying as a female (p<0.001), Latinx ethnicity (p=0.017), high school education or greater (p=0.002), having a casual sex partner in the last 6 months (p=0.010), and currently being on parole (p=0.028). Past 30-day protein intake was also positively associated with the following drug patterns over the past 30 days: total number of drug injections (p=0.009), total number of drugs used without injecting (p=.001), heroin use frequency (p=0.013), and marijuana use frequency (p=0.005). All other variables were not significant in bivariate analysis.
Table 2:
Bivariate Associations of Log-Transformed Monthly Protein Intake among People who Inject Drugs in Los Angeles and San Francisco (N=937)
| Variable | Parameter Estimate (β)(95% CI)1 | P-Value |
|---|---|---|
| Age (years) | 0.003 (0, 0.007) | 0.050 |
| Female | −0.213 (−0.311, −0.115) | <0.001 |
| Latinx ethnicity | −0.119(−0.217, −0.021) | 0.017 |
| High school education or greater | 0.149 (0.057, 0.242) | 0.002 |
| Unstable housing or homeless | −0.027 (−0.138, 0.084) | 0.633 |
| Income of less than $1,400/month | 0.083 (−0.007, 0.174) | 0.072 |
| Single relationship status | −0.020 (−0.110, 0.070) | 0.668 |
| Steady sex partner in the last 6 months | 0.052 (−0.031, 0.136) | 0.217 |
| Casual sex partner in the last 6 months | 0.115 (0.028, 0.203) | 0.010 |
| Currently on probation | 0.002 (−0.095, 0.099) | 0.968 |
| Currently on parole | 0.246 (0.026, 0.465) | 0.028 |
| Any alcohol or drug treatment | 0.046 (−0.055, 0.148) | 0.374 |
| Methadone maintenance treatment, last 6 months | −0.046 (−0.139, 0.048) | 0.335 |
| Total number of drug injections, past 30-days (log transformed) | 0.048 (0.012, 0.084) | 0.009 |
| Total number of drugs used without injecting, past 30 days (log transformed) | 0.050 (0.02, 0.08) | 0.001 |
| Times used heroin/opiates, past 30-days (log transformed) | 0.045 (0.010, 0.081) | 0.013 |
| Times used methamphetamine, past 30-days (log transformed) | 0.031 (−0.001, 0.064) | 0.061 |
| Times used marijuana, past 30-days (log transformed) | 0.048 (0.014, 0.081) | 0.005 |
| Times used cocaine, past 30-days (log transformed) | 0.014 (−0.017, 0.044) | 0.376 |
Bolded values are significant at the P < 0.05 level
The final multiple regression model (Table 3) found older age (β = 0.006, p=0.009), Latinx ethnicity (β = −0.139, p=0.032), high school or greater education (β = 0.120, p=0.043), frequency of heroin/opioid use (β = 0.066, p=0.002), and frequency of marijuana use in the past 30-days (β = 0.055, p= 0.002) to be significantly associated with protein intake while adjusting for gender.
Table 3:
Final Linear Regression Model of Log-Transformed Monthly Protein Intake among People who Inject Drugs in Los Angeles and San Francisco (N=937)1
| Variable | Parameter Estimate (β)(95% CI)2 |
|---|---|
| Intercept | 5.33 (4.96, 5.71) |
| Female | −0.77 (−0.201, 0.047) |
| Age (years) | 0.006 (0.001, 0.01) |
| Latinx ethnicity | −0.139 (−0.266, −0.012) |
| Times used heroin/opiates, past 30-days (log transformed) | 0.066 (0.024, 0.107) |
| Times used marijuana, past 30-days (log transformed) | 0.055 (0.02, 0.09) |
| High school education or greater | 0.120 (0.004, 0.236) |
Adjusted R2 = 0.037
Bolded values are significant at the P < 0.05 level
Discussion
Results from this analysis demonstrate that the vast majority of PWID in this sample did not consume adequate levels of protein, which could potentially lead to malnourishment and negative health sequalae. Compared to a similar population in Norway in which half of PWID met the minimum recommended protein intake requirement,6 nearly all participants in our study (99%) fell below the recommended amount. Similar to the Norway study, our sample was predominantly (97.8%) at a healthy BMI or overweight/obese. This paradoxical finding illustrates that PWID may not be under-fed, but rather, they suffer the consequences of an unbalanced diet consisting primarily of sugar and carbohydrates.6,7 This underscores the necessity to examine basic needs for PWID in the US and to include social determinants of health in routine assessments of the well-being of PWID in future studies.
Age, education, ethnicity, and use of heroin and marijuana were all significantly associated with protein intake of PWID. Although women tend to have less body weight than men, burning less calories, and thus requiring less protein on average, identifying as female was not significant in the final model after inclusion of other sociodemographic and drug use variables. Previous research found that protein intake decreases with age for Americans as a result of lower overall energy intake,12 however, this study found that increased age of PWID led to increased protein intake, even after adjusting for other covariates in the final model. The positive association between having a high school education or greater and increased protein intake corroborates previous research,30 and may be due to a general exposure to the importance of proper nutrition in US schools.34
California has the largest Latinx population (15.4 million) in the United States.32 Almost a quarter (23.6%) of our sample identified as Latinx, which was inversely associated with protein intake. Prevalence of food insecurity is much greater among the Latinx population compared to non-Hispanic White Americans.5 Latinos made up over two-thirds (67.4%) of the proportion of all food-insecure households in Los Angeles County, and over half (58.3%) of low-income Latinx families surveyed in the San Francisco Bay Area had high food insecurity.33, In particular, one of our recruitment sites was based in East Los Angeles, which is a predominantly Latinx area, and has been found to be inequitably lacking in access to affordable, healthy foods.32, These data show that Latinx PWID consume less protein than non-Latinx PWID, and supports the need for more affordable grocery stores and access to free food in Latinx communities.
Total amount of both injection and non-injection drug use was associated with increased protein intake, indicating that route of administration of drugs may not have a role in nutritional intake. Higher frequency of heroin and marijuana use was associated with increased protein intake, but not methamphetamine or cocaine. Use of stimulants can decrease appetite,17,18 while extensive marijuana use has been linked to higher caloric intake and increased appetite35 which could theoretically lead to increased protein intake. However, the finding that frequency of opiate use increases protein intake is novel and worth further investigation. A qualitative study revealed dysfunctional eating patterns among persons who use heroin, with participants endorsing little interest in food while actively using heroin,15 which does not seem to be the case in our sample. Opioid users have been found to consume high amounts of sugar compared to overall nutrient intake,6 and perhaps this is the first study that demonstrates a link between frequency of heroin use and preference for protein-rich foods.
Limitations to consider for this study include the following. All data was based on self-reports. Studies often measure nutrition recall over a 30-day period, however, we do not know the reliability and validity of reports for largely unhoused PWID. Recall bias may have influenced our results. Protein intake was estimated by using weights after a single question assessing intake of each food item by ounce rather than using a 24-hour recall. In addition, we did not use models or visual aids to assist participants in discerning ounces for a typical serving. Further, when calculating the food weight we did not use a nutrition software to conduct analyses. In addition, a stepwise method was used in the final multivariate regression analysis which can cause bias in parameter estimations. Data analyzed for this report are cross-sectional so we cannot establish causality between nutrition and our independent variables. Finally, results are from only 2 California cities and are not generalizable to PWID in other places, so further studies need to be conducted to determine if these findings are common among PWID in other areas.
Maintaining a healthy diet is important for all people, and especially PWID. PWID have high prevalence of HIV and HCV, which can be worsened by nutrition deficiencies. A healthy diet can help offset some of the negative health consequences of drug use by increasing energy and immune system, which are of vital importance when living on the streets, as much of our sample was. Communities should advocate for increased access to food for homeless populations and PWID and prioritize protein and nutrient-rich foods at existing food distribution centers.
Acknowledgements:
This work was supported by NIDA (grant numbers RO1046049, RO1DA038965). We thank study participants for their time and effort devoted to this project. We also thank the research assistants who helped collect data for this project.
Footnotes
Declaration of Interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this paper.
Reference List
- 1.Anderson SA. Core indicators of nutritional state for difficult-to-sample populations. The Journal of nutrition. 1990;120 Suppl 11:1559–1600. [DOI] [PubMed] [Google Scholar]
- 2.Anema A, Wood E, Weiser SD, Qi J, Montaner JSG, Kerr T. Hunger and associated harms among injection drug users in an urban Canadian setting. Substance Abuse Treatment, Prevention, and Policy. 2010;5(1):20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schmitz J, Kral AH, Chu D, Wenger LD, Bluthenthal RN. Food insecurity among people who inject drugs in Los Angeles and San Francisco. Public Health Nutr 2016;19(12):2204–2212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Strike C, Rudzinski K, Patterson J, Millson M. Frequent food insecurity among injection drug users: correlates and concerns. BMC Public Health. 2012;12(1):1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Coleman-Jensen A, Gregory C, & Singh A Household food security in the United States in 2019. 2020; USDA-ERS Economic Research Report, (173). [Google Scholar]
- 6.Saeland M, Haugen M, Eriksen FL, et al. High sugar consumption and poor nutrient intake among drug addicts in Oslo, Norway. British Journal of Nutrition. 2011;105(4):618–624. [DOI] [PubMed] [Google Scholar]
- 7.Jeynes KD, & Gibson EL (2017). The importance of nutrition in aiding recovery from substance use disorders: A review. Drug and alcohol dependence, 179, 229–239. [DOI] [PubMed] [Google Scholar]
- 8.Cohen S, Nathan JA, Goldberg AL. Muscle wasting in disease: molecular mechanisms and promising therapies. Nat Rev Drug Discov. 2015;14(1):58–74. [DOI] [PubMed] [Google Scholar]
- 9.Russell L The importance of patients’ nutritional status in wound healing. British Journal of Nursing. 2001;10(Sup1):S42–S49. [DOI] [PubMed] [Google Scholar]
- 10.Muller O, Krawinkel M. Malnutrition and health in developing countries. CMAJ. 2005;173(3):279–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.USDA. All about the Protein Foods Group. ChooseMyPlate. https://www.choosemyplate.gov/eathealthy/protein-foods. Accessed April 30, 2020.
- 12.Hoy MK, Clemens JC, Moshfegh AJ. Protein Intake of Adults in the U.S.: What We Eat in America, NHANES 2015–2016. Food Surveys Research Group Dietary Data Brief No. 29. January 2021, revised slightly from July 2020. [Google Scholar]
- 13.Baptiste F, Hamelin AM, Côté F. Drugs and diet among women street sex workers and injection drug users in Quebec City. Can J Urban Res. 2009;18:78–95. [Google Scholar]
- 14.Testa A, Jackson DB. Food Insecurity Among Formerly Incarcerated Adults. Criminal Justice and Behavior. 2019;46(10):1493–1511. [Google Scholar]
- 15.Neale J, Nettleton S, Pickering L, Fischer J. Eating patterns among heroin users: a qualitative study with implications for nutritional interventions. Addiction. 2012;107(3):635–641. [DOI] [PubMed] [Google Scholar]
- 16.Clague J, Belin TR, Shetty V. Mechanisms underlying methamphetamine-related dental disease. The Journal of the American Dental Association. 2017;148(6):377–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bello NT. Chapter 1 - Central Nervous System Stimulants and Drugs That Suppress Appetite. In: Ray SD. Side Effects of Drugs Annual. Vol 37. Elsevier; 2015:1–13. [Google Scholar]
- 18.Escobar M, Scherer JN, Soares CM, et al. Active Brazilian crack cocaine users: nutritional, anthropometric, and drug use profiles. Braz J Psychiatry. 2018;40(4):354–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hendricks KM, Erzen HD, Wanke CA, Tang AM. Nutrition issues in the HIV-infected injection drug user: findings from the nutrition for healthy living cohort. J Am Coll Nutr. 2010;29(2):136–143. [DOI] [PubMed] [Google Scholar]
- 20.Smit E, Graham NMH, Tang A, Flynn C, Solomon L, Vlahov D. Dietary intake of community-based HIV-1 seropositive and seronegative injecting drug users. Nutrition. 1996;12(7):496–501. [DOI] [PubMed] [Google Scholar]
- 21.Lieber CS. Relationships between nutrition, alcohol use, and liver disease. Alcohol Res Health. 2003;27(3):220–231. [PMC free article] [PubMed] [Google Scholar]
- 22.Mangili A, Murman DH, Zampini AM, Wanke CA, Mayer KH. Nutrition and HIV Infection: Review of Weight Loss and Wasting in the Era of Highly Active Antiretroviral Therapy from the Nutrition for Healthy Living Cohort. Clinical Infectious Diseases. 2006;42(6):836–842. [DOI] [PubMed] [Google Scholar]
- 23.Piroth L, Duong M, Quantin C, et al. Does hepatitis C virus co-infection accelerate clinical and immunological evolution of HIV-infected patients? AIDS. 1998;12(4):381–388. [DOI] [PubMed] [Google Scholar]
- 24.Mathers BM, Degenhardt L, Bucello C, Lemon J, Wiessing L, Hickman M. Mortality among people who inject drugs: a systematic review and meta-analysis. Bull World Health Organ. 2013;91(2):102–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bluthenthal RN, & Watters JK.Multimethod research from targeted sampling to HIV risk environments. NIDA research monograph. 1995;157, 212–230. [PubMed] [Google Scholar]
- 26.Kral AH, Malekinejad M, Vaudrey J, et al. Comparing respondent-driven sampling and targeted sampling methods of recruiting injection drug users in San Francisco. J Urban Health. 2010;87(5):839–850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Watters JK, Biernacki P. Targeted Sampling: Options for the Study of Hidden Populations*. Social Problems. 2014;36(4):416–430. [Google Scholar]
- 28.Cagle HH, Fisher DG, Senter TP, Thurmond RD, & Kastar AJ. Classifying skin lesions of injection drug users: a method for corroborating disease risk. US Department of Health and Human Services. 2002. Vol. DHHS Publication No.(SMA), 02–3753. [Google Scholar]
- 29.National Center for Health Statistics. National Health Interview Survey, 2015. Public-use data file and documentation. http://www.cdc.gov/nchs/nhis/quest_data_related_1997_forward.htm. 2016.
- 30.Nazrul Islam SK, Hossain KJ, Ahmed A, Ahsan M. Nutritional status of drug addicts undergoing detoxification: prevalence of malnutrition and influence of illicit drugs and lifestyle. British Journal of Nutrition. 2002;88(5):507–513. [DOI] [PubMed] [Google Scholar]
- 31.Myers AM, Painter MA. Food insecurity in the United States of America: an examination of race/ethnicity and nativity. Food Security. 2017;9(6):1419–1432. [Google Scholar]
- 32.United States Census Bureau. Annual Estimates of the Resident Population by Sex, Race, and Hispanic Origin for the United States, States, and Counties: April 1, 2010 to July 1, 2019. [Google Scholar]
- 33.Los Angeles County Department of Public Health, Office of Health Assessment and Epidemiology, Food Insecurity in Los Angeles County, September 2017 [Google Scholar]
- 34.Centers for Disease Control and Prevention. School health guidelines to promote healthy eating and physical activity. MMWR Morb Mortal Wkly Rep. 2011;60(RR-5):1–76. [PubMed] [Google Scholar]
- 35.Rodondi N, Pletcher MJ, Liu K, Hulley SB, Sidney S, Coronary Artery Risk Development in Young Adults S. Marijuana use, diet, body mass index, and cardiovascular risk factors (from the CARDIA study). Am J Cardiol. 2006;98(4):478–484. [DOI] [PubMed] [Google Scholar]


