Abstract
Human papilloma virus (HPV) vaccination for adolescents aged 11–12 years and cervical cancer screening for women aged 21–65 years are recommended to help prevent cervical cancer. The purpose of this study was to describe 2018 National Committee for Quality Assurance (NCQA) Healthcare Effectiveness Data and Information Set (HEDIS®) data for the United States on HPV vaccination and cervical cancer screening from 275 commercial preferred provider organizations (PPOs), 219 commercial health maintenance organizations (HMOs), and 204 Medicaid HMOs. The Centers for Disease Control and Prevention and NCQA analyzed the data in 2021. The HEDIS® measure for HPV vaccination was the percentage of male and female adolescents aged 13 years who completed HPV immunization (2– or 3–dose series) on or before their 13th birthday. The measure for cervical cancer screening was the percentage of women screened either with cervical cytology within the last 3 years for women aged 21–64 years or with cervical cytology/HPV co-testing within the last 5 years for women aged 30–64 years. Nationally, the mean rate for HPV vaccination in 2018 was 37.8% in Medicaid HMOs, 30.3% in commercial HMOs, and 24.9% in commercial PPOs. The mean rate for cervical cancer screening was 75.9% in commercial HMOs, 72.6% in commercial PPOs, and 60.3% among Medicaid HMOs. Medicaid HMOs reported higher HPV vaccination rates but lower cervical cancer screening rates than commercial plans. These differences raise questions about explanatory factors and how to improve prevention performance by plan category.
Keywords: Managed care plans, Quality measures, Human papilloma virus vaccination, Cervical cancer screening
1. Introduction
Almost all cervical cancers and cervical pre-cancers in the United States can be attributed to infection with human papilloma virus (HPV) (Centers for Disease Control and Prevention, 2020). Each year, HPV-attributable infections result in an estimated 196,000 cervical pre-cancers and 11,000 cervical cancers in the United States (Centers for Disease Control and Prevention, 2020). The annual cancer burden linked to HPV infections in the United States also includes cancers of the vagina (700 cases), vulva (2800 cases), penis (900 cases), anus (6500 cases total, with 4400 in female individuals and 2100 in male individuals), and oropharynx (14000 cases total, with 2200 in female individuals and 11800 in male individuals) (Centers for Disease Control and Prevention, 2020).
To prevent HPV-associated morbidity, the Advisory Committee on Immunization Practices (ACIP) first recommended the HPV vaccine as a 3-dose series in 2006 for adolescent females, in 2011 for adolescent males, and in 2016 recommended a 2-dose HPV vaccine series for male and female adolescents (Meites et al., 2016; Meites et al., 2019). Three-doses of HPV vaccine are recommended for persons who initiated vaccination at ages 15–26 years of age or persons who are immunocompromised.
Cervical cancer screening can help detect precancers before they turn into invasive cancer. For women aged 21–29 years, the United States Preventive Services Task Force (USPSTF) recommends screening for cervical cancer every 3 years with cervical cytology (Papanicolaou smear) (US Preventive Services Task Force, 2018). For women aged 30–65 years, the USPSTF recommends several screening options: cervical cytology every 3 years, cytology with HPV testing (co-testing) every 5 years, or HPV testing every 5 years (primary HPV testing) (US Preventive Services Task Force, 2018).
Health plans are positioned to influence both clinicians and members about preventive services. Health plans can identify which members have not had preventive services and feed this information to clinicians. Health plans can also reach out directly to members to provide reminders and educational material about preventive services.
The National Committee for Quality Assurance (NCQA) Healthcare Effectiveness Data and Information Set® (HEDIS®) uses measures based on information from administrative data sources (such as claims and enrollment files) and medical records to evaluate managed care plan effectiveness of care for HPV vaccination and cervical cancer screening (National Committee for Quality Assurance, 2021). With HEDIS® measures, individual health plans can assess how their HEDIS® performance rates compare with rates reported by other plans and measure the effects of strategies put into place to promote preventive services. An estimated 191 million people are enrolled in plans that annually report HEDIS® measures to the NCQA (National Committee for Quality Assurance, 2021). In the United States, the Centers for Medicare and Medicaid Services (CMS) (Centers for Medicare and Medicaid Services. Medicaid Quality of Care. Performance Measurement, 2021a; Centers for Medicare and Medicaid Services. Medicaid Quality of Care. Performance Measurement, 2021b; Centers for Medicare and Medicaid Services, 2021c; Centers for Medicare and Medicaid Services, 2021d) and the Health Resources and Services Administration (Health Resources and Services Administration, 2019) have incorporated HEDIS® measures as part of their clinical quality improvement programs.
To assess compliance with HPV vaccination and cervical cancer screening measures in managed care plans, the Centers for Disease Control and Prevention and the NCQA analyzed data in 2021 from the 2018 HEDIS® measurement year for the United States. The purpose of this study was to describe the national and regional results for the HEDIS® measures for HPV vaccination and cervical cancer screening measures, stratified by managed care plan category, type, and Health and Human Services (HHS) region.
2. Methods
The 2018 HEDIS® measure for HPV vaccination was the percentage of male and female adolescents aged 13 years who completed HPV immunization (2- or 3-dose series) on or before their 13th birthday. The HEDIS® measure for cervical cancer screening in 2018 reflected 2012 USPSTF recommendations for women aged 21–64 years (Moyer and U.S. Preventive Services Task Force, 2012). The measure included women aged 21–64 years who had cervical cytology performed within the last 3 years and women aged 30–64 years who had cervical cytology/HPV co-testing within the last 5 years. Women with absence of the cervix were excluded. The HEDIS® measures for HPV vaccination and cervical cancer screening did not include Medicare plans because Medicare primarily enrolls older adults who were not recommended to receive these services.
The 2018 HEDIS® measurement year included three categories of health plans: 275 commercial preferred provider organizations (PPOs), 219 commercial health maintenance organizations (HMOs), and 204 Medicaid HMOs. For HPV vaccination, 19.6% of commercial PPO plans were missing rates. However, out of the 54 commercial PPO plans with missing rates for HPV vaccination, 51 of the missing rates were associated with a single plan with offices in multiple states. For all other plan categories, the percent of plans with missing rates was less than 10%. For this report, plans with reportable rates were analyzed, with no imputation for missing rates.
Mean health plan performance rates (%) for each HEDIS® measure were calculated using SPSS Custom Tables at the national level by health care plan category, and at the regional level by health plan category and Health and Human Services (HHS) region. Differences in the mean health plan performance rates at the national level by health plan category were assessed with independent-sample t-tests. Correlations between the mean health plan performance rates for each HEDIS® measure by health plan category and by HHS region were evaluated with Spearman’s rank-order correlation coefficients. The Commercial HMO minus Commercial PPO differences in health plan performance rates (%) and the Commercial HMO minus Medicaid HMO differences in rates were calculated for the US overall and for each HHS region.
The project was reviewed by the CDC National Center for Chronic Disease Prevention and Health Promotion Human Subject Coordinator, who determined that the project was secondary analysis of data with no human subject identifiers, and additional review by a CDC Institutional Review Board was not required.
3. Results
Nationally, the overall US mean health plan performance rate for cervical cancer screening was 75.9% in commercial HMOs, 72.6% in commercial PPOs, and 60.3% among Medicaid HMOs (Table 1). t-tests for equality of means (2 tailed with 95% confidence intervals) were statistically different (p < 0.001) for cervical cancer screening for rates for commercial HMOs versus commercial PPOs, and for rates for commercial HMOs versus Medicaid HMOs.
Table 1.
Mean health plan performance rates for cervical cancer screening* among females, by plan category and type, for the United States overall and by Health and Human Services (HHS) regions, Healthcare Effectiveness Data and Information Set (HEDIS®), 2018 HEDIS® Measurement Year.
| HHS region (HQ city) | Plan category (type) | Plans analyzed | Mean rate (95% CI) | Row | Difference |
|---|---|---|---|---|---|
| US (overall) | Commercial (PPO) | 273 | 72.6 (71.9–73.3) | A | B-A = 3.3 |
| US (overall) | Commercial (HMO) | 218 | 75.9 (75.0–76.7) | B | – |
| US (overall) | Medicaid (HMO) | 197 | 60.3 (59.0–61.6) | C | B-C = 15.6 |
| 1 (Boston) | Commercial (PPO) | 29 | 76.3 (73.3–79.3) | A | B-A = 4.2 |
| 1 (Boston) | Commercial (HMO) | 25 | 80.5 (77.8–83.1) | B | – |
| 1 (Boston) | Medicaid (HMO) | 10 | 70.7 (65.8–75.5) | C | B-C = 9.8 |
| 2 (New York) | Commercial (PPO) | 15 | 76.6 (73.4–79.8) | A | B-A = 0.1 |
| 2 (New York) | Commercial (HMO) | 16 | 76.7 (74.0–79.4) | B | – |
| 2 (New York) | Medicaid (HMO) | 17 | 65.7 (60.8–70.6) | C | B-C = 11.0 |
| 3 (Philadelphia) | Commercial (PPO) | 36 | 74.7 (73.0–76.5) | A | B-A = 2.2 |
| 3 (Philadelphia) | Commercial (HMO) | 48 | 76.9 (75.4–78.3) | B | – |
| 3 (Philadelphia) | Medicaid (HMO) | 34 | 55.3 (50.6–60.0) | C | B-C = 21.6 |
| 4 (Atlanta) | Commercial (PPO) | 41 | 72.5 (70.8–74.2) | A | B-A = 5.9 |
| 4 (Atlanta) | Commercial (HMO) | 22 | 78.4 (76.2–80.6) | B | – |
| 4 (Atlanta) | Medicaid (HMO) | 28 | 60.8 (58.6–63.1) | C | B-C = 17.6 |
| 5 (Chicago) | Commercial (PPO) | 33 | 71.9 (70.4–73.5) | A | B-A = 3.1 |
| 5 (Chicago) | Commercial (HMO) | 40 | 75.0 (72.7–77.2) | B | – |
| 5 (Chicago) | Medicaid (HMO) | 41 | 62.4 (60.4–64.4) | C | B-C = 12.6 |
| 6 (Dallas) | Commercial (PPO) | 22 | 70.2 (67.5–72.9) | A | B-A = −0.8 |
| 6 (Dallas) | Commercial (HMO) | 14 | 69.4 (64.5–74.4) | B | – |
| 6 (Dallas) | Medicaid (HMO) | 19 | 57.6 (53.9–61.3) | C | B-C = 11.8 |
| 7 (Kansas City) | Commercial (PPO) | 22 | 70.4 (68.7–72.2) | A | B-A = 1.9 |
| 7 (Kansas City) | Commercial (HMO) | 15 | 72.3 (70.2–74.3) | B | – |
| 7 (Kansas City) | Medicaid (HMO) | 9 | 56.6 (51.6–61.5) | C | B-C = 15.7 |
| 8 (Denver) | Commercial (PPO) | 23 | 68.8 (66.7–71.0) | A | B-A = 2.9 |
| 8 (Denver) | Commercial (HMO) | 13 | 71.7 (68.8–74.5) | B | – |
| 8 (Denver) | Medicaid (HMO) | 5 | 53.9 (45.9–61.9) | C | B-C = 17.8 |
| 9 (San Francisco) | Commercial (PPO) | 20 | 71.9 (69.3–74.4) | A | B-A = 3.9 |
| 9 (San Francisco) | Commercial (HMO) | 21 | 75.8 (72.6–78.9) | B | – |
| 9 (San Francisco) | Medicaid (HMO) | 29 | 60.5 (57.5–63.5) | C | B-C = 15.3 |
| 10 (Seattle) | Commercial (PPO) | 32 | 71.9 (70.0–73.8) | A | B-A = 5.1 |
| 10 (Seattle) | Commercial (HMO) | 4 | 77.0 (63.8–90.2) | B | – |
| 10 (Seattle) | Medicaid (HMO) | 5 | 56.1 (50.0–62.1) | C | B-C = 20.9 |
Abbreviations: CI is confidence interval; HQ is the regional office headquarters for the HHS region; HMO is health maintenance organization; PPO is preferred provider organization.
The cervical cancer screening HEDIS® measure evaluates the percentage of women 21–64 years of age screened for cervical cancer and includes: Women 21–64 years of age who had cervical cytology performed within the last 3 years; and women 30–64 years of age who had cervical cytology/HPV co-testing within the last 5 years. Women with absence of the cervix were excluded.
For cervical cancer screening, the range of rates by HHS region was 68.8–76.6% for commercial PPOs, 69.4–80.5% for commercial HMOs, and 53.9–70.7% for Medicaid HMOs (Table 1 and Figure 1). The three HHS regions with the highest mean health plan performance rates for cervical cancer screening were commercial HMOs, and included region 1 (Boston, 80.5%), region 4 (Atlanta, 78.4%), and region 10 (Seattle, 77.0%). For cervical cancer screening, the lowest mean health plan performance rates were in Medicaid HMOs.
Fig. 1.
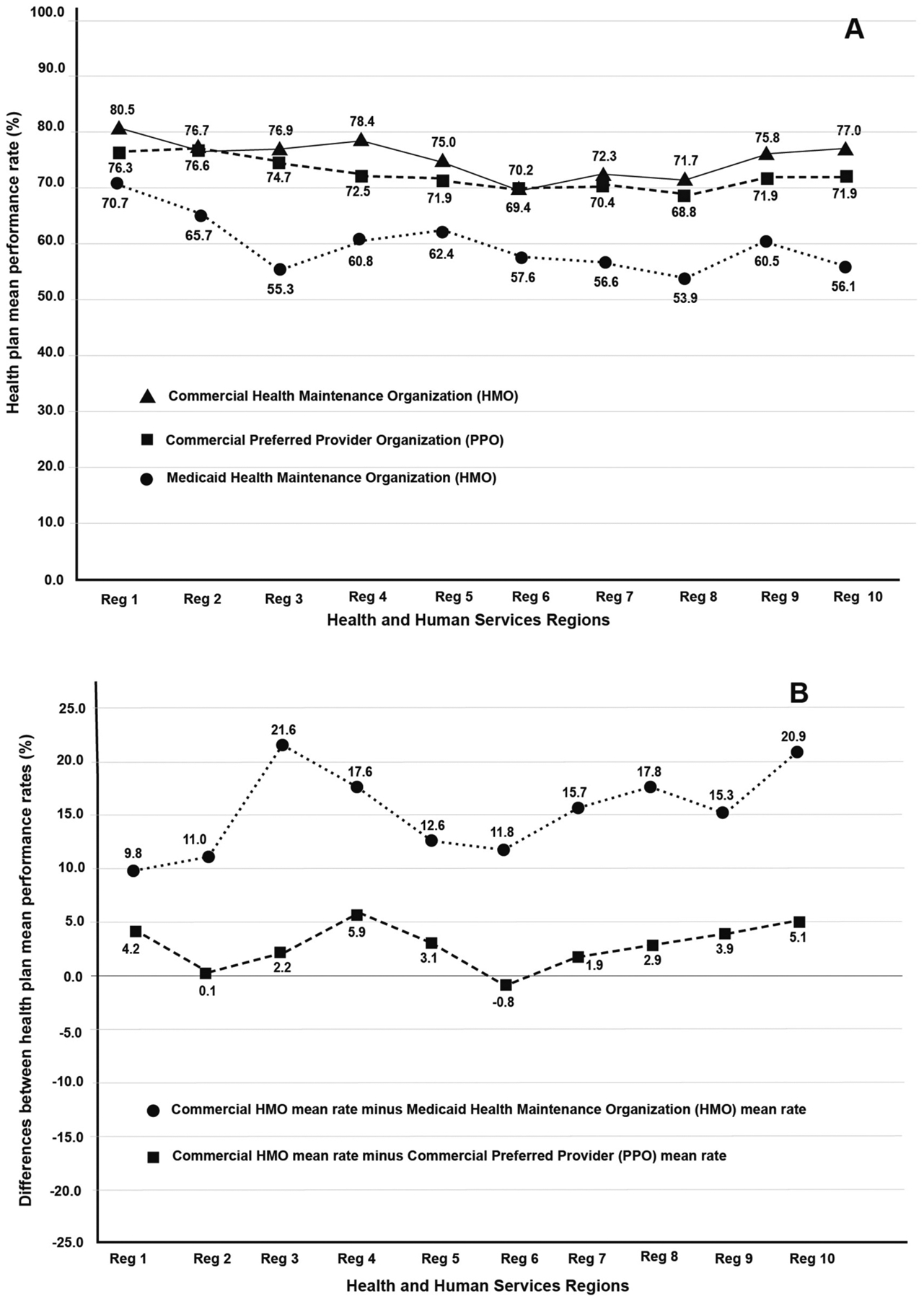
Cervical cancer screening performance rates (%), 2018 HEDIS® measurement year. Inset A shows health plan mean performance rates (%) by plan category and region. Inset B shows the B-A (Commercial HMO minus Commercial PPO) and B-C (Commercial HMO minus Medicaid HMO) rate differences (%) from Table 1.
The commercial HMO minus the commercial PPO difference in health plan performance rates (%) for cervical cancer screening was 3.3% for the US (overall) and ranged from −0.8% to 5.9% by HHS region (Table 1 and Figure 1). The commercial HMO minus the Medicaid HMO difference in rates was 15.6% for the US (overall) and ranged from 9.8% to 21.6% by HHS region.
The overall US mean health plan performance rate for HPV vaccination in 2018 was 37.8% in Medicaid HMOs, 30.3% in commercial HMOs, and 24.9% in commercial PPOs (Table 2). t-tests for equality of means (2 tailed with 95% confidence intervals) were statistically different (p < 0.001) for HPV vaccination rates for commercial HMOs versus commercial PPOs, and for rates for commercial HMOs versus Medicaid HMOs.
Table 2.
Mean health plan performance rates for human papilloma virus (HPV) vaccination* among male and female adolescents, by plan category and type, for the United States overall and by Health and Human Services (HHS) regions, Healthcare Effectiveness Data and Information Set (HEDIS®), 2018 HEDIS® Measurement Year.
| HHS region (HQ city) | Plan category (type) | Plans analyzed | Mean rate (95% CI) | Row | Difference |
|---|---|---|---|---|---|
| US (overall) | Commercial (PPO) | 221 | 24.9 (24.1–25.8) | A | B-A = 5.4 |
| US (overall) | Commercial (HMO) | 206 | 30.3 (28.9–31.7) | B | – |
| US (overall) | Medicaid (HMO) | 186 | 37.8 (36.4–39.1) | C | B-C = −7.5 |
| 1 (Boston) | Commercial (PPO) | 23 | 27.6 (23.1–32.1) | A | B-A = 0.7 |
| 1 (Boston) | Commercial (HMO) | 25 | 28.3 (26.4–30.2) | B | – |
| 1 (Boston) | Medicaid (HMO) | 10 | 41.0 (36.9–45.2) | C | B-C = −12.7 |
| 2 (New York) | Commercial (PPO) | 13 | 18.6 (15.4–21.7) | A | B-A = 7.9 |
| 2 (New York) | Commercial (HMO) | 12 | 26.5 (21.6–31.5) | B | – |
| 2 (New York) | Medicaid (HMO) | 16 | 39.3 (33.7–45.0) | C | B-C = −12.8 |
| 3 (Philadelphia) | Commercial (PPO) | 30 | 26.0 (24.3–27.7) | A | B-A = 5.0 |
| 3 (Philadelphia) | Commercial (HMO) | 48 | 31.0 (28.0–34.1) | B | – |
| 3 (Philadelphia) | Medicaid (HMO) | 32 | 39.8 (35.3–44.4) | C | B-C = −8.8 |
| 4 (Atlanta) | Commercial (PPO) | 32 | 21.6 (20.0–23.3) | A | B-A = 4.8 |
| 4 (Atlanta) | Commercial (HMO) | 21 | 26.4 (22.9–29.8) | B | – |
| 4 (Atlanta) | Medicaid (HMO) | 27 | 33.0 (30.5–35.5) | C | B-C = −6.6 |
| 5 (Chicago) | Commercial (PPO) | 27 | 25.7 (23.7–27.8) | A | B-A = 4.6 |
| 5 (Chicago) | Commercial (HMO) | 36 | 30.3 (27.2–33.4) | B | – |
| 5 (Chicago) | Medicaid (HMO) | 36 | 36.3 (33.9–38.8) | C | B-C = −6.0 |
| 6 (Dallas) | Commercial (PPO) | 17 | 24.0 (21.1–26.9) | A | B-A = 0.1 |
| 6 (Dallas) | Commercial (HMO) | 14 | 24.1 (19.2–28.9) | B | – |
| 6 (Dallas) | Medicaid (HMO) | 18 | 38.1 (35.3–40.8) | C | B-C = −14.0 |
| 7 (Kansas City) | Commercial (PPO) | 18 | 22.5 (20.3–24.7) | A | B-A = 6.1 |
| 7 (Kansas City) | Commercial (HMO) | 13 | 28.6 (22.9–34.4) | B | – |
| 7 (Kansas City) | Medicaid (HMO) | 9 | 29.6 (23.5–35.7) | C | B-C = −1.0 |
| 8 (Denver) | Commercial (PPO) | 17 | 26.5 (21.9–31.0) | A | B-A = 9.5 |
| 8 (Denver) | Commercial (HMO) | 13 | 36.0 (27.9–44.0) | B | – |
| 8 (Denver) | Medicaid (HMO) | 5 | 39.2 (27.2–51.2) | C | B-C = −3.2 |
| 9 (San Francisco) | Commercial (PPO) | 16 | 25.8 (22.6–29.0) | A | B-A = 11.1 |
| 9 (San Francisco) | Commercial (HMO) | 20 | 36.9 (31.2–42.7) | B | – |
| 9 (San Francisco) | Medicaid (HMO) | 28 | 41.6 (37.4–45.8) | C | B-C = −4.7 |
| 10 (Seattle) | Commercial (PPO) | 28 | 28.5 (26.4–30.5) | A | B-A = 12.9 |
| 10 (Seattle) | Commercial (HMO) | 4 | 41.4 (17.6–65.2) | B | – |
| 10 (Seattle) | Medicaid (HMO) | 5 | 39.2 (30.4–48.1) | C | B-C = 2.2 |
Abbreviations: CI is confidence interval; HQ is the regional office headquarters for the HHS region; HMO is health maintenance organization; PPO is preferred provider organization.
The human papilloma virus (HPV) vaccination HEDIS® measure evaluates the percentage of adolescents (male and female) 13 years of age who completed an HPV vaccination series (2 or 3 doses) on or before their 13th birthday.
For HPV vaccination in adolescents, the range of rates (%) by HHS region was from 18.6% to 28.5% for commercial PPOs, 24.1% to 41.4% for commercial HMOs, and 29.6% to 41.6% for Medicaid HMOs (Table 2 and Figure 2). The three HHS regions with the highest mean health plan performance rates for HPV vaccination were region 9 (Medicaid HMO, San Francisco, 41.6%), region 10 (commercial HMO, Seattle, 41.4%), and region 1 (Medicaid HMO, Boston, 41.0%). The commercial HMO minus the commercial PPO difference in health plan performance rates (%) for HPV vaccination was 5.4% for the US (overall) and ranged from 0.1% to 12.9% by HHS region (Table 2 and Figure 2). The commercial HMO minus the Medicaid HMO differences in rates was −7.5% for the US (overall) and ranged from −14.0% to 2.2% by HHS region.
Fig. 2.
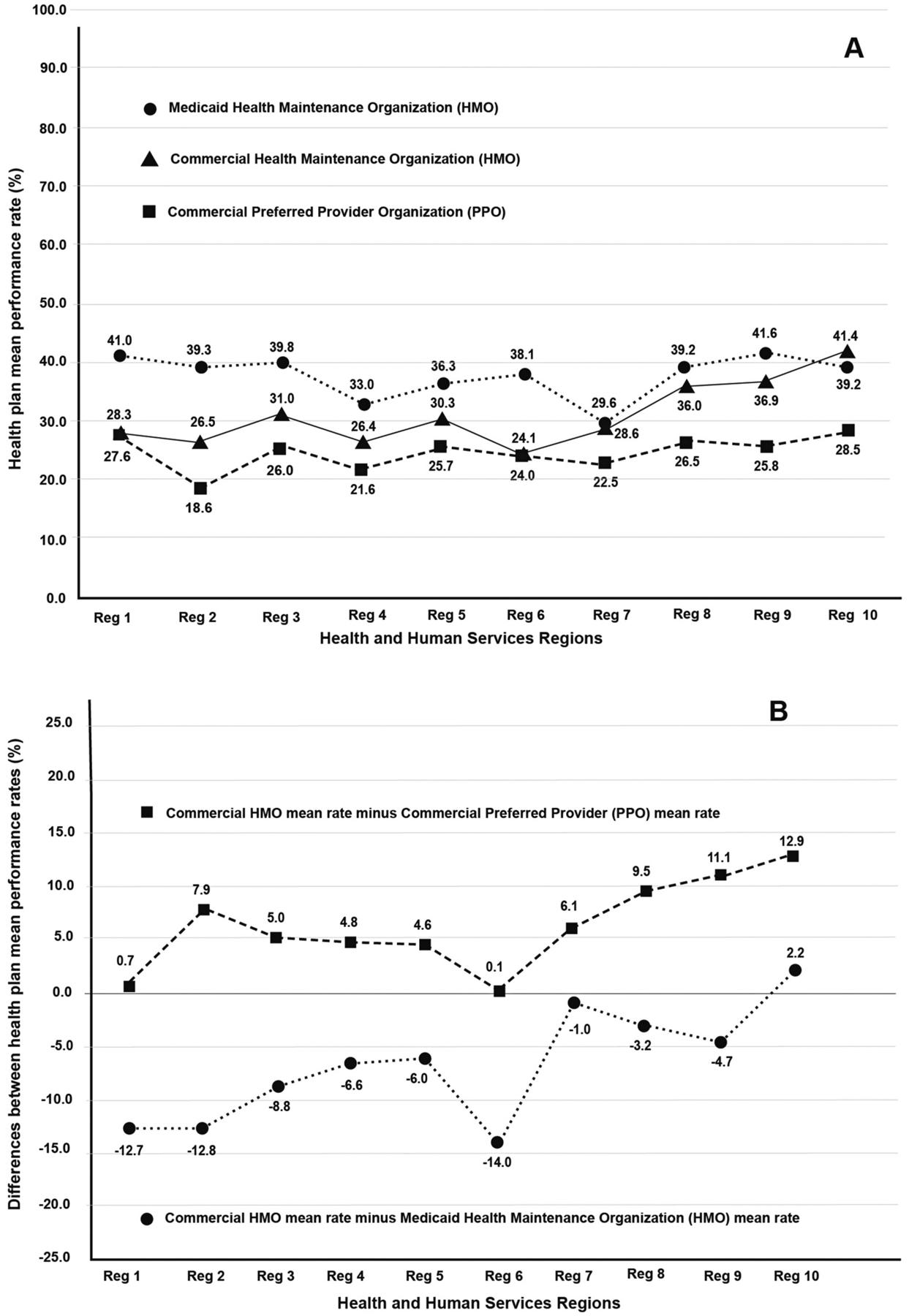
Human papilloma virus (HPV) vaccination rates (%), 2018 HEDIS® measurement year. Inset A shows health plan mean performance rates (%) by plan category and region. Inset B shows the B-A (Commercial HMO minus Commercial PPO) and B-C (Commercial HMO minus Medicaid HMO) rate differences (%) from Table 2.
Commercial PPO HPV vaccination health plan performance rates were positively correlated with commercial HMO HPV vaccination health plan performance rates by HHS region (correlation coefficient 0.685; significant at the 0.05 level, 2-tailed) (Appendix A). Similarly, commercial PPO cervical cancer screening health plan performance rates were positively correlated with commercial HMO cervical cancer screening health plan performance rates by HHS region (correlation coefficient 0.791; significant at 0.01 level, 2 tailed). For both HPV vaccination and cervical cancer screening health plan performance rates, no significant correlations were present between the rates for commercial plans and the rates for Medicaid HMOs by HHS region. Also, for each plan category, no correlations were present between health plan performance rates for HPV vaccination by HHS region and health plan performance rates for cervical cancer screening by HHS region.
4. Discussion
Cervical cancer is largely a disease of health inequity with higher rates among lower socio-economic groups, immigrant populations, and women in rural settings (Fuzzell et al., 2021). An estimated 50–60% of the women who develop cervical cancer in the United States have not been adequately screened or followed (Benard et al., 2021). In the 2018 HEDIS® measurement year, commercial PPOs and commercial HMOs reported that more than 70% of women aged 21–64 years received cervical cancer screening. Cervical cancer screening health plan performance rates were significantly lower in Medicaid HMOs (60%) than in commercial plans. The lower cervical cancer screening health plan performance rates in Medicaid HMOs are of potential concern because cervical cancer is largely preventable through screening and follow-up, and Medicaid HMOs serve populations that often are rarely or never screened.
While 2018 HEDIS® rates for commercial plans were higher than rates for Medicaid plans, rates for cervical cancer screening across all plans were lower than national objectives (US Department of Health and Human Services, n.d.). Healthy People 2030 Objective C-09 is to increase the proportion of females who get screened for cervical cancer, with a target of 84.3% (US Department of Health and Human Services, n. d.). The National Health Interview Survey (NHIS) is the data source to monitor progress towards meeting this objective. The 2018 NHIS results were selected as the 2030 Objective baseline (80.5% of females aged 21 to 65 years) (US Department of Health and Human Services, n.d.).
NHIS trends on utilization of cervical cancer screening indicate that cervical cancer rates are now lower than they were 10–20 years ago (National Cancer Institute, 2021; Suk et al., 2022). Cervical cancer screening reported in the 2018 NHIS was 80.5%, while the prevalence of cervical cancer screening reported in the 2000 NHIS was 86.5% (National Cancer Institute, 2021). The reported prevalence for the 2019 NHIS (73.5%) is even lower than in 2018 (National Cancer Institute, 2021). Historical HEDIS® data suggest a decrease in cervical cancer screening since 2003 (Appendix B). Commercial HMOs reported lower cervical cancer screening in 2018 (75.2%) than in 2003 (81.8%).
The explanation for the decreased compliance with up-to-date cervical cancer screening since 2000 is unknown, but likely has resulted from multiple contributing factors (Suk et al., 2022). Potential solutions to increase cervical cancer screening rates might include health education campaigns culturally tailored for populations that rarely or never undergo screening; organized or structured approaches to remind health professionals to perform screening, such as reminders from electronic medical record systems; and improved methods of surveillance to obtain accurate and reliable information on whether a woman was screened and whether the test was cytology, HPV test, or both (Suk et al., 2022). In addition, health plans can share reports with clinicians about clinicians’ performance rates, which can serve as a useful feedback tool (Ng et al., 2017).
In our study of the 2018 HEDIS® measurement year, in contrast to cervical cancer screening, rates of HPV vaccination were much lower, with less than 50% of the adolescents in managed care plans receiving the recommended doses of HPV vaccine by the age of 13 years. HPV vaccination coverage among adolescents was the highest in Medicaid HMOs and lowest in commercial PPOs. There is a prior report that describes national HEDIS® HPV vaccination rates in 2013 by plan category (Ng et al., 2015). The HEDIS® measure for HPV vaccination in 2013 was for female adolescents, while the HEDIS® measure in this report was for male and female adolescents. Both the 2013 report and this report found that HPV vaccination health plan performance rates were highest in Medicaid HMOs and lowest in commercial PPOs.
Based on the historical HEDIS® data published by the NCQA (Appendix B), HPV vaccination rates have been improving since 2016, even though rates remained low in 2018. HPV vaccinations in adolescents almost doubled from 2016 to 2018 in all three categories of plans (National Committee for Quality Assurance, 2021). Additional studies examining methods to increase HPV vaccination health plan performance rates across all categories of plans, together with studies to better understand why Medicaid HMOs appear to be more successful in HPV vaccination delivery than commercial plans, would be helpful. HPV vaccination starting at age 9 is known to be associated with increased rates of completion by age 13 and may be a potential tactic to further increase HPV vaccination rates (St Sauver et al., 2016; Goleman et al., 2018; Casey et al., 2022).
HHS region was the most granular level of geographic information supported by the available data for this report. State-level analysis was not possible because some plans were licensed in a particular state but operated across several states. Nevertheless, regional benchmarks are potentially useful to health plans interested in how their individual plan performance compares with other plans in the same region.
The findings in the current study are subject to at least four limitations. First, the available information did not include details on potential factors that might help explain higher or lower performance rates. Second, the HEDIS® measure for HPV vaccination was for the overall proportion of adolescents (males and females combined). This measure is consistent with ACIP recommendations but prevented evaluation of vaccination rates by gender in this report. Third, this report is limited to the 2018 HEDIS® measurement year. The results do not account for disruptions and delays in routine cervical cancer screening and HPV vaccination resulting from the COVID-19 pandemic (Miller et al., 2021; Patel Murthy et al., 2021). Health plans may need to make specific efforts in order to return levels of routine cervical cancer screening and HPV vaccination prior to the pandemic. Fourth, although this study provides useful insights about HEDIS® measures among the insured population based on claims and medical record reviews, multiple data sources are helpful to provide a more complete picture of HPV vaccination and cervical cancer screening coverage in the United States, especially for groups that are not insured or not covered by managed care plans reporting HEDIS® measures (Fuzzell et al., 2021).
5. Conclusions
In summary, this study found that US health care plan performance rates in the 2018 HEDIS® measurement year for cervical cancer screening for women aged 21 to 64 years were lower than the Healthy People 2030 objective target and have decreased over the last 10–20 years. HEDIS® rates for HPV vaccination in adolescents have been improving but remain low. Rates vary among different categories of health care plans and across HHS regions. Medicaid HMOs reported higher HPV vaccination rates but lower cervical cancer screening rates than commercial plans. The differences observed by type of plan raise questions about explanatory factors and whether interventions might be possible to improve prevention performance by plan category. For potential next steps, studies of individual regions or state-wide cohorts might enable improved information about geographic patterns of plan coverage (Panozzo et al., 2019; Risley et al., 2021). Key informant interviews of a sample of managed care plans might provide additional insight into factors associated with higher or lower prevention performance (Ng et al., 2017).
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Abbreviations:
- ACIP
Advisory Committee on Immunization Practices
- HEDIS®
Healthcare Effectiveness Data and Information Set
- HHS
Health and Human Services
- NCQA
National Committee for Quality Assurance
- USPSTF
U.S. Preventive Services Task Force
Appendix A. Spearman’s rank order correlations between the Healthcare Effectiveness Data and Information Set (HEDIS®) health plan performance rates (%) for human papillomavirus (HPV) vaccination and for cervical cancer screening (CCS) in the ten Health and Human Services (HHS) regions, for Commercial (PPO), Commercial (HMO), and Medicaid (HMO) plans, United States, 2018
| HPV commercial (PPO) | HPV commercial (HMO) | HPV Medicaid (HMO) | CCS commercial (PPO) | CCS commercial (HMO) | CCS Medicaid (HMO) | ||
|---|---|---|---|---|---|---|---|
| HPV commercial (PPO) | Correlation coefficient | 1 | 0.685* | 0.468 | −0.141 | 0.236 | −0.358 |
| Sig. (2-tailed) | . | 0.029 | 0.172 | 0.697 | 0.511 | 0.31 | |
| N | 10 | 10 | 10 | 10 | 10 | 10 | |
| HPV commercial (HMO) | Correlation coefficient | 0.685* | 1 | 0.371 | −0.202 | 0.042 | −0.515 |
| Sig. (2-tailed) | 0.029 | . | 0.291 | 0.575 | 0.907 | 0.128 | |
| N | 10 | 10 | 10 | 10 | 10 | 10 | |
| HPV Medicaid (HMO) | Correlation coefficient | 0.468 | 0.371 | 1 | 0.437 | 0.334 | 0.128 |
| Sig. (2-tailed) | 0.172 | 0.291 | . | 0.207 | 0.345 | 0.725 | |
| N | 10 | 10 | 10 | 10 | 10 | 10 | |
| CCS commercial (PPO) | Correlation coefficient | − 0.141 | − 0.202 | 0.437 | 1 | 0.791** | 0.620 |
| Sig. (2-tailed) | 0.697 | 0.575 | 0.207 | . | 0.006 | 0.056 | |
| N | 10 | 10 | 10 | 10 | 10 | 10 | |
| CCS commercial (HMO) | Correlation coefficient | 0.236 | 0.042 | 0.334 | 0.791** | 1 | 0.406 |
| Sig. (2-tailed) | 0.511 | 0.907 | 0.345 | 0.006 | . | 0.244 | |
| N | 10 | 10 | 10 | 10 | 10 | 10 | |
| CCS Medicaid (HMO) | Correlation coefficient | −0.358 | −0.515 | 0.128 | 0.620 | 0.406 | 1 |
| Sig. (2-tailed) | 0.310 | 0.128 | 0.725 | 0.056 | 0.244 | . | |
| N | 10 | 10 | 10 | 10 | 10 | 10 |
N = number of Health and Human Services (HHS) regions.
correlation is significant at the 0.05 level (2-tailed).
correlation is significant at the 0.01 level (2-tailed).
Appendix B. Health plan performance rates (%) for National Committee on Quality Assurance (NCQA) Healthcare Effectiveness Data and Information Set (HEDIS®) measures for cervical cancer screening1 in women 21–64 years of age* and for human papillomavirus vaccinations in adolescents2
| Cervical cancer screening rates (%) | HPV vaccination rates (%) | |||||
|---|---|---|---|---|---|---|
| Year | Commercial PPOs | Commercial HMOs | Medicaid HMOs | Commercial PPOs | Commercial HMOs | Medicaid HMOs |
| 1999 | – | 71.8 | – | – | – | – |
| 2000 | – | 78.1 | – | – | – | – |
| 2001 | – | 80.0 | 61.1 | – | – | – |
| 2002 | – | 80.5 | 62.2 | – | – | – |
| 2003 | – | 81.8 | 64.0 | – | – | – |
| 2004 | – | 80.9 | 64.7 | – | – | – |
| 2005 | 74.6 | 81.8 | 65.2 | – | – | – |
| 2006 | 72.6 | 81.0 | 65.7 | – | – | – |
| 2007 | 73.5 | 81.7 | 64.8 | – | – | – |
| 2008 | 74.0 | 80.7 | 66.0 | – | – | – |
| 2009 | 74.6 | 77.3 | 65.8 | – | – | – |
| 2010 | 74.5 | 77.0 | 67.2 | – | – | – |
| 2011 | 74.4 | 76.5 | 66.7 | – | – | – |
| 2012 | 73.6 | 75.5 | 64.5 | – | – | – |
| 2014 | 73.8 | 76.3 | 60.2 | – | – | – |
| 2015 | 71.7 | 74.7 | 55.8 | – | – | – |
| 2016 | 73.0 | 74.3 | 58.0 | 13.9 | 16.7 | 22.7 |
| 2017 | 73.2 | 74.3 | 59.4 | 22.0 | 25.7 | 35.3 |
| 2018 | 73.5 | 75.2 | 59.3 | 24.8 | 29.8 | 37.8 |
| 2019 | 74.2 | 76.2 | 60.1 | 27.2 | 31.9 | 40.1 |
| 2020 | 72.4 | 73.8 | 56.8 | 29.2 | 33.4 | 39.9 |
The HEDIS® cervical cancer screening measure was updated in 2013 to reflect new guidelines from the US Preventive Services Task Force. Prior to 2013, the cervical cancer screening measure assessed women 21–64 years of ages who had cervical cytology performed within the last 3 years. Since 2013, the measure assesses women who were screened for cervical cancer using any of the following criteria: women 21–64 years of age who had cervical cytology performed within the last 3 years; women 30–64 years of age who had cervical high-risk human papillomavirus (hrHPV) testing performed within the last 5 years; and women 30–64 years of age who had cervical cytology/high-risk human papillomavirus (hrHPV) cotesting within the last 5 years.
Source:
National Committee for Quality Assurance. Healthcare Effectiveness Data and Information Set (HEDIS®) measures. Cervical cancer screening. https://www.ncqa.org/hedis/measures/cervical-cancer-screening/
National Committee for Quality Assurance. Healthcare Effectiveness Data and Information Set (HEDIS®) measures. Immunizations for Adolescents (IMA). Human Papillomavirus for Adolescents. https://www.ncqa.org/hedis/measures/immunizations-for-adolescents/
Footnotes
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
CRediT authorship contribution statement
Thomas B. Richards: Software, Data curation, Methodology, Writing – original draft, Writing – review & editing. Megan C. Lindley: Resources, Conceptualization, Methodology, Writing – original draft, Writing –– review & editing. Sepheen C. Byron: Conceptualization, Methodology, Writing – original draft, Writing –– review & editing. Mona Saraiya: Supervision, Conceptualization, Methodology, Writing – original draft, Writing –– review & editing.
Declaration of Competing Interest
Sepheen Byron is an employee of the National Committee for Quality Assurance (NCQA), which owns and stewards HEDIS®. However, HEDIS® measures and their use in NCQA programs are overseen by an independent, multistakeholder voting panel. The other authors declare no competing interests.
References
- Benard VB, Jackson JE, Greek A, Senkomago V, Huh WK, Thomas CC, et al. , 2021. A population study of screening history and diagnostic outcomes of women with invasive cervical cancer. Cancer Med 10 (12), 4127–4137. 10.1002/cam4.3951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casey SM, Jansen E, Drainoni ML, Schuch TJ, Leschly KS, Perkins RB, 2022. Long-term multilevel intervention impact on human papilloma virus vaccination rates spanning the COVID-19 pandemic. J Low Genit Tract Dis 26 (1), 13–19. 10.1097/LGT.0000000000000648. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention, 2020. How Many Cancers Are Linked with HPV each Year? Atlanta. Division of Cancer Prevention and Control, CDC, GA. https://www.cdc.gov/cancer/hpv/statistics/cases.htm. [Google Scholar]
- Centers for Medicare & Medicaid Services, 2021a. Health Insurance Exchange 2022 Quality Rating System Measure Technical Specifications https://www.cms.gov/files/document/2022-qrs-measure-tech-specs.pdf.
- Centers for Medicare & Medicaid Services, 2021b. Electronic Clinical Quality Measures (eCQMs) for Cervical Cancer Screening https://ecqi.healthit.gov/ecqm/ep/2021/cms124v9.
- Centers for Medicare & Medicaid Services. Medicaid Quality of Care. Performance Measurement, 2021a. Core Set of Adult Health Care Quality Measures for Medicaid https://www.medicaid.gov/medicaid/quality-of-care/downloads/2021-adult-core-set.pdf.
- Centers for Medicare & Medicaid Services. Medicaid Quality of Care. Performance Measurement, 2021b. Core Set of Children’s Health Care Quality Measures for Medicaid and Children’s Health Insurance Program (CHIP) https://www.medicaid.gov/medicaid/quality-of-care/downloads/2021-child-core-set.pdf.
- Fuzzell LN, Perkins RB, Christy SM, Lake PW, Vadaparampil ST, 2021. Cervical cancer screening in the United States: challenges and potential solutions for under-screened groups. Prev. Med 144, 106400. 10.1016/j.ypmed.2020.106400. [DOI] [PubMed] [Google Scholar]
- Goleman MJ, Dolce M, Morack J, 2018. Quality improvement initiative to improve human papillomavirus vaccine initiation at 9 years of age. Acad. Pediatr 18 (7), 769–775. 10.1016/j.acap.2018.05.005. [DOI] [PubMed] [Google Scholar]
- Health Resources and Services Administration, 2019. Bureau of Primary Health Care. Uniform Data System. 2019 Table 6B Clinical Quality Measures. https://bphcdata.net/docs/table_6b.pdf. [Google Scholar]
- Meites E, Kempe A, Markowitz LE, 2016. Use of a 2-dose schedule for human papillomavirus vaccination - updated recommendations of the Advisory Committee on Immunization Practices. MMWR Morb. Mortal. Wkly Rep 65 (49), 1405–1408. 10.15585/mmwr.mm6549a5. [DOI] [PubMed] [Google Scholar]
- Meites E, Szilagyi PG, Chesson HW, Unger ER, Romero JR, Markowitz LE, 2019. Human papillomavirus vaccination for adults: updated recommendations of the Advisory Committee on Immunization Practices. MMWR Morb. Mortal. Wkly Rep 68 (32), 698–702. 10.15585/mmwr.mm6832a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller MJ, Xu L, Qin J, Hahn EE, Ngo-Metzger Q, Mittman B, et al. , 2021. Impact of COVID-19 on cervical cancer screening rates among women aged 21–65 years in a large integrated health care system - Southern California, January 1–September 30, 2019, and January 1–September 30, 2020. MMWR Morb Mortal Wkly Rep 70 (4), 109–113. 10.15585/mmwr.mm7004a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moyer VA, U.S. Preventive Services Task Force, 2012. Screening for cervical cancer: U. S. Preventive Services Task Force recommendation statement. Ann. Intern. Med 156 (12), 880–891. W312. https://www.acpjournals.org/doi/10.7326/0003-4819-156-12-201206190-00424. [DOI] [PubMed] [Google Scholar]
- National Cancer Institute, 2021. Cancer Trends Progress Report. Early Detection Cervical Cancer Screening. https://progressreport.cancer.gov/detection/cervical_cancer. [Google Scholar]
- National Committee for Quality Assurance, 2021. HEDIS® and performance measurement https://www.ncqa.org/hedis/.
- Ng J, Ye F, Roth L, Sobel K, Byron S, Barton M, et al. , 2015. Human papillomavirus vaccination coverage among female adolescents in managed care plans - United States, 2013. MMWR Morb Mortal Wkly Rep 64 (42), 1185–1189. 10.15585/mmwr.mm6442a1. [DOI] [PubMed] [Google Scholar]
- Ng JH, Sobel K, Roth L, Byron SC, Lindley MC, Stokley S, 2017. Supporting human papillomavirus vaccination in adolescents: perspectives from commercial and Medicaid health plans. J Public Health Manag Pract 23 (3), 283–290. 10.1097/PHH.0000000000000440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panozzo CA, Gilkey MB, Kornides ML, Wharam JF, 2019. Provider-level rates of HEDIS-consistent HPV vaccination in a regional health plan. Hum Vaccin Immunother 15 (7–8), 1708–1714. 10.1080/21645515.2019.1574150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel Murthy B, Zell E, Kirtland K, Jones-Jack N, Harris L, Sprague C, et al. , 2021. Impact of the COVID-19 pandemic on administration of selected routine childhood and adolescent vaccinations - 10 U.S. Jurisdictions, March–September 2020. MMWR Morb Mortal Wkly Rep 70 (23), 840–845. 10.15585/mmwr.mm7023a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Risley C, Stewart MW, Geisinger KR, Hiser LM, Morgan JC, Owens KJ, et al. , 2021. STRIDES - studying risk to improve disparities in cervical cancer in Mississippi - design and baseline results of a statewide cohort study. Prev. Med 153, 106740. 10.1016/j.ypmed.2021.106740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- St Sauver JL, Rutten LJF, Ebbert JO, Jacobson DJ, McGree ME, Jacobson RM, 2016. Younger age at initiation of the human papillomavirus (HPV) vaccination series is associated with higher rates of on-time completion. Prev. Med 89, 327–333. 10.1016/j.ypmed.2016.02.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suk R, Hong YR, Rajan SS, Xie Z, Zhu Y, Spencer JC, 2022. Assessment of US Preventive Services Task Force guideline-concordant cervical cancer screening rates and reasons for underscreening by age, race and ethnicity, sexual orientation, rurality, and insurance, 2005 to 2019. JAMA Netw. Open 5 (1), e2143582. 10.1001/jamanetworkopen.2021.43582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- US Department of Health and Human Services. Healthy People 2030 Objective C-09 https://health.gov/healthypeople/objectives-and-data/browse-objectives/cancer/increase-proportion-females-who-get-screened-cervical-cancer-c-09.
- US Preventive Services Task Force, 2018. Cervical cancer: screening. https://uspreventiveservicestaskforce.org/uspstf/recommendation/cervical-cancer-screening.


