Abstract
Introduction: The position paper on critical care pharmacy services describes two tiers of responsibilities: essential and desirable activities. Activities are categorized into five domains: patient care, quality improvement, research and scholarship, training and education, and professional development. Documentation of these activities can be important for justifying pharmacist positions, comparing pharmacy practice models, conducting performance evaluations, and tracking individual workload; however, limited recommendations are provided for standardized productivity tracking, and national practices remain largely uncharacterized. Objectives: The purpose of this survey was to describe documentation practices of critical care pharmacist activities. Methods: A cross-sectional survey was distributed via email to 1694 members of the ACCP critical care practice research network. The survey asked respondents to describe the methods used to document productivity as it relates to the 5 domains. Results: Seventy-nine (4.7%) critical care pharmacists from 63 institutions completed the survey. Intervention documentation was used for position justification and annual reviews among 54.4% and 44.1% of pharmacists, respectively. Pharmacists were routinely expected to perform additional responsibilities beyond patient care that contribute to overall productivity, but the percentage of institutions that track these activities as a measure of pharmacist productivity was relatively low: quality improvement (46%), research/scholarship (29%), training/education (38%), and professional development (27%). Documentation of these additional responsibilities and activities was primarily used for annual evaluations, but the majority of respondents answered that no standardized method for tracking activities existed. In multivariate regression, dedicated ICU pharmacists was a significant predictor for increased satisfaction (Exp(ß) 4.498, 95% CI 1.054-19.187, P = .042). Conclusion: Practice variation exists in how and for what intent critical care pharmacists track productivity. Further evaluation and standardization of productivity tracking may aid in position justification and practice model evaluation for dedicated ICU pharmacists in today’s value-based era.
Keywords: pharmacy practice models, critical care, medication safety
Measurement is the first step that leads to control and eventually to improvement. If you can’t measure something, you can’t understand it. If you can’t understand it, you can’t control it. If you can’t control it, you can’t improve it.―H. James Harrington
Introduction
Critical care pharmacists (CCP) improve patient outcomes while reducing healthcare costs but must still justify their value. 1 Even though the 2020 position statement from American College of Clinical Pharmacy (ACCP), Society of Critical Care Medicine (SCCM), and American Society of Health-System Pharmacists (ASHP) states that critical care pharmacists are essential to the delivery of high quality patient care and recommends “appropriate documentation tools to demonstrate their impact on patient care and economic value,” no standardized recommendations for how to track productivity and justify positions are provided. 2 CCPs provide value through 2 primary avenues: direct patient care (eg, interprofessional rounding, clinical interventions, pharmacokinetic monitoring, code participation) and non-direct patient care activities (eg, quality improvement initiatives, formulary management, antimicrobial stewardship, research and scholarship, training, and education), but both direct and non-direct patient care activities are notoriously hard to track, and no standardized unit of productivity has been established.3-11 These limitations of productivity tracking, in addition to overall practice variation, have notable downstream effects regarding future position justification and pharmacy practice model advancement as it is difficult to measure incremental improvements of lower CPP-to-patient ratios.12-16 The purpose of this survey was to characterize current productivity tracking practices for CCPs (eg, what and how productivity is measured, intention of use for tracking).
Methods
A cross-sectional electronic survey was developed and determined to be exempt by the institutional review board at the primary investigator’s institution. The survey was distributed 3 times between June 16th 2020 and June 30th 2020 via email to the ACCP Critical Care Practice and Research Network (PRN), which consisted of 2006 members as of April 2020, of which 1694 were eligible (ie, practicing non-resident critical care pharmacists). The survey was developed and completed in the Qualtrics™ platform and is provided in Supplemental Appendix 1. Prior to distribution, the survey was sent to 3 critical care pharmacists for peer review and refined based on feedback. Based on these reviews, the survey underwent multiple rounds of revisions. Participation in the survey was voluntary, and responses remained anonymous. As compensation for their time, respondents were offered a $5 electronic gift card upon completion of the survey. The gift card was distributed via email after survey completion and funding came from an institutional seed grant. Respondent email addresses were collected for the purpose of distribution of reimbursement and were kept separate from survey responses.
The survey focused on three areas of assessment: (1) individual demographics (7 questions); (2) institution demographics (26 questions); and (3) pharmacist productivity tracking (36 questions). Individual demographic information included type of institution, ICU practice site (eg, medical, surgical), leadership roles held, and participation in activities outside of direct patient care. Institution demographic information included type of institution, geographic region, level of ICU, institution bed count, ICU bed count, pharmacy practice model type, number, and type of ICU. The level of ICU was defined per the American College of Critical Care Medicine definitions. 17 The ICU levels range from level I to level III, with level I being the most comprehensive ICU care. 17 Survey participants provided information on the critical care pharmacy practice model at their respective institution. This information included type of pharmacy practice model, responsibilities of clinical pharmacists, number of critical care pharmacist personnel during day shift, evening shift, night shift, weekends, and holidays, types of clinical services provided by pharmacists during each shift, and presence of a pharmacist dedicated per ICU. Study participants were asked to report average patient count per pharmacist, coverage of non-ICU patients in addition to ICU patients, hours worked per week, other required activities (eg, precepting, research, quality improvement, supervisor activities, etc.), and time spent on documentation activities. Further questions about documentation include how clinical pharmacist positions in the ICU are supported, what activities are included in pharmacist productivity tracking, frequency and purpose of intervention tracking, logistics of intervention tracking including software and specific intervention types utilized (eg, pharmacokinetic dosing, antimicrobial stewardship, renal dose adjustments, etc.), and documentation of other activities (quality improvement, research/scholarship, training/education, and professional development). The perception of how satisfied respondents were with their institution’s current productivity tracking system and how supervisors monitor their productivity was assessed using a Likert Scale composed of the following options: strongly disagree, disagree, somewhat disagree, neither agree nor disagree, somewhat agree, agree, or strongly agree.
Data were found to fit a non-parametric distribution and, as such, were presented as number and percentage for categorical variables and as median and interquartile range (IQR) for continuous variables. In order to concisely present the data, combinations of Likert Scale responses of agree and disagree variations were done to express dichotomized positive/negative perceptions. Multiple linear regression models were constructed to determine if productivity documentation characteristics were associated with perceived satisfaction with the process and how it was used to justify positions and in annual evaluations. Likert scale responses were not dichotomized for these analyses but were assessed as continuous variables on the 7-point scale ranging from strongly disagree (1) to strongly agree (7). Covariates with a P-value less than .1 on univariate analysis were considered for inclusion in the model after they were determined to have a plausible effect on the outcome of interest by consensus of the investigators. Outcomes with a P-value less than .05 were considered to be significant.
Results
A total of 1694 eligible critical care pharmacists were contacted to participate in this study, and 79 pharmacists from 63 different institutions responded to the survey (response rate 4.7%). Eight pharmacists partially completed the survey, and their responses were excluded from the analysis. Demographic characteristics are summarized in Table 1. The number of total hospital beds varied among respondents, with 41% (n = 26) having between 301 and 600 beds and 27% (n = 17) having between 601 and 900 beds. Over half of the pharmacists surveyed (n = 48, 61%) care for more than 15 ICU patients at a time, and almost half (n = 36, 46%) also cover non-ICU patients in addition to ICU patients. Additionally, most pharmacists reported extra roles with 66% (n = 52) of pharmacists holding a supplementary title, including supervisor, residency program director, and faculty positions. Of respondents, 53% (n = 42) reported that they work more than 40 hours per week in the hospital setting. Sixty three percent of respondents (n = 48) also reported that they spend 5% to 20% of their time on documentation of the pharmacists surveyed (n = 48, 61%) care for more than 15 ICU patients at a time, and almost half (n = 36, 46%) also cover non-ICU patients in addition to ICU patients. Additionally, most pharmacists reported extra roles with 66% (n = 52) of pharmacists holding a supplementary title, including supervisor, residency program director, and faculty positions. Of respondents, 53% (n = 42) reported that they work more than 40 hours per week in the hospital setting. Sixty three percent of respondents (n = 48) also reported that they spend 5% to 20% of their time on documentation of activities, and 63% (n = 50) are expected to document clinical interventions on a daily basis (Table 2).
Table 1.
Demographics.
| Practice site/intensive care unit characteristic | Individual institutions, n (%) |
|---|---|
| n = 63 | |
| Institution type | |
| Academic medical center | 23 (37) |
| Community teaching | 22 (35) |
| Community non-teaching | 17 (27) |
| Government | 1 (2) |
| Hospital bed size | |
| < 100 | 3 (5) |
| 101-300 | 11 (14) |
| 301-600 | 26 (41) |
| 601-900 | 17 (27) |
| >900 | 6 (10) |
| ICU beds | |
| <20 | 7 (11) |
| 21-40 | 19 (30) |
| 41-70 | 13 (21) |
| 71-100 | 8 (13) |
| >100 | 16 (25) |
| Number of ICUs, mean ± SD | 4 (2-7) |
| Types of ICUs | |
| Medical | 44 (70) |
| Cardiac | 39 (62) |
| Neurology | 37 (59) |
| Cardiothoracic surgery | 35 (56) |
| Surgical | 37 (59) |
| Trauma | 27 (43) |
| Emergency department | 26 (41) |
| Neonatal | 24 (38) |
| Mixed medical-surgical | 26 (41) |
| Pediatric | 16 (25) |
| Burn | 8 (13) |
| Other | 2 (3) |
| Presence of dedicated critical care pharmacist in each ICU | 46 (73) |
| Critical care pharmacist order verification responsibilities | |
| Entire shift | 16 (25) |
| Part of shift | 13 (21) |
| None | 17 (27) |
| Level of ICU | |
| Level I | 41 (65) |
| Level II | 22 (35) |
| Level III | 0 (0) |
| ICU pharmacist clinical services | |
| Pharmacokinetic dosing | 63 (100) |
| Expanded therapeutic drug monitoring (warfarin, digoxin, phenytoin, enoxaparin) | 60 (95) |
| Profile Review | 63 (100) |
| Participation in rounds with the ICU team | 62 (98) |
| Number of employed critical care pharmacists at institution, mean ± SD | Median (range) |
| Day shift | 4 (1-24) |
| Evening shift | 0 (0-6) |
| Number of employed critical care pharmacists at institution, mean ± SD | Median (range) |
| Night shift | 0 (0-2) |
| Number of critical care pharmacists on service, mean ± SD | |
| Day shift | |
| Weekday | 3 (1-7) |
| Weekend | 1 (0-6) |
| Holiday | 1 (0-6) |
| Evening shift | |
| Weekday | 0 (0-4) |
| Weekend | 0 (0-3) |
| Holiday | 0 (0-3) |
| Night shift | |
| Weekday | 0 (0-2) |
| Weekend | 0 (0-2) |
| Holiday | 0 (0-2) |
| Individual respondent characteristic | All respondents, n (%) (n = 79) |
| Primary area of practice | |
| Mixed medical-surgical | 27 (34) |
| Medical | 18 (23) |
| Emergency department | 5 (6) |
| Surgical | 5 (6) |
| Cardiac | 4 (5) |
| Cardiothoracic surgery | 4 (5) |
| Trauma | 4 (5) |
| Neurology | 4 (5) |
| Other | 6 (8) |
| Number of ICU patients assigned per pharmacist on a typical weekday | |
| <10 | 8 (10) |
| 10-15 | 25 (32) |
| 16-20 | 16 (20) |
| 21-25 | 16 (20) |
| 26-30 | 8 (10) |
| >30 | 4 (5) |
| Other titles held in addition to critical care pharmacist | |
| Supervisor/manager/clinical coordinator | 11 (14) |
| Residency program director/coordinator | 14 (18) |
| Adjunct faculty appointment | 25 (32) |
| Full time faculty appointment | 2 (3) |
| How critical care pharmacist positions are supported | |
| FTE/dose dispensed | 12 (15) |
| FTE/patient days | 5 (6) |
| FTE/patient census | 29 (37) |
| ICU staff request/preference | 28 (35) |
| Percentage of time spent documenting activities | |
| <5% | 10 (13) |
| 5-10% | 18 (23) |
| 11-20% | 20 (25) |
| 21-30% | 12 (15) |
| 31-40% | 10 (13) |
| 41-50% | 3 (4) |
| >50% | 3 (4) |
Table 2.
Patient Care Productivity Tracking.
| Characteristic | Individual institutions, n (%) |
|---|---|
| (n = 63) | |
| Frequency of documenting clinical interventions | |
| On rounds | 7 |
| Daily | 44 |
| Never | 9 |
| “Spot check” on random audit | 3 |
| Purpose of Clinical Intervention Documentation | |
| Pharmacist hand-off communication | 43 |
| Interdisciplinary communication | 17 |
| Position justification | 30 |
| Annual review | 26 |
| Other | 3 |
| None | 1 |
| Systems used to track clinical pharmacist interventions | |
| Dashboards | 7 |
| Electronic tools integrated into electronic health record | 34 |
| Third-party downloadable software | 19 |
| Electronic medical record documentation | 27 |
| Spreadsheet | 5 |
| Paper | 2 |
| None | 1 |
| Utilization of clinical pharmacist interventions to evaluate critical care pharmacists | |
| Yes | 28 |
| No | 31 |
| Other | 4 |
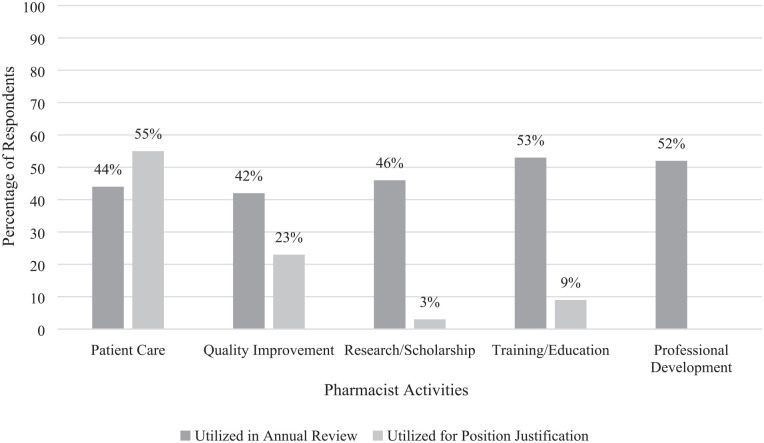
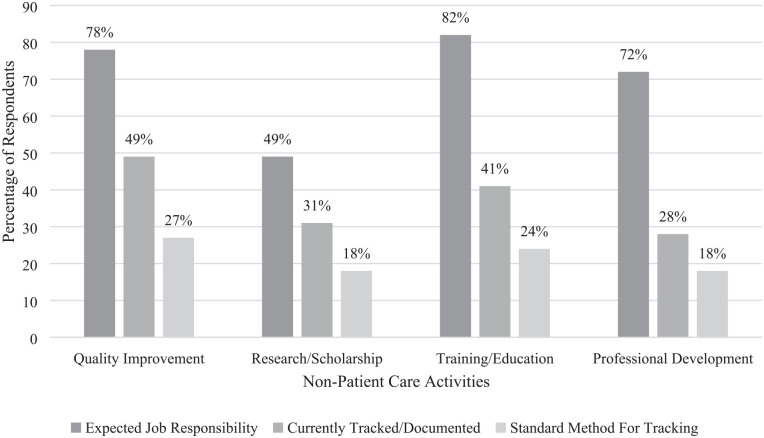
Patient care documentation is used for employee annual reviews and position justification for approximately 50% of respondents (Figure 1). Furthermore, many pharmacists engage in activities beyond direct patient care, including quality improvement, research/scholarship, training/education, and professional development. While expected of most pharmacists, standardized methods for documentation of non-patient care activities were lacking at many institutions (Figure 2); however, these non-direct patient care activities did contribute to both annual reviews for pharmacists and position justification (Figure 1). Figures 3 to 5 in the Supplemental Materials provide further information regarding specific activities that comprise quality improvement, research/scholarship, and training/education based on responses to the survey. While 68% of respondents (n = 50) report documenting clinical patient care interventions daily, fewer respondents documented additional activities including quality improvement (49%), research/scholarship (31%), training/education (41%), and professional development (29%) (Figure 2). A variety of systems were used to track interventions, including dashboards, electronic tools integrated into the electronic health record (EHR), third-party downloadable software, EHR documentation, spreadsheet, and paper (Table 3).
Figure 1.
Utilization of productivity tracking for annual review and position justification (n = 79).
Figure 2.
Pharmacist responsibilities and documentation practices (n = 79).
Table 3.
Regression Analysis of Pharmacist Satisfaction Based on Patient Care Workload.
| Characteristic | Exp(B) (95% CI) | P-value |
|---|---|---|
| Presence of dedicated critical care pharmacist in each ICU | 4.498 (1.054-19.187) | .042 |
| Pharmacist coverage of non-ICU patients in addition to ICU patients | 1.418 (0.486-4.138) | .523 |
| Average census: | ||
| 15 or fewer patients | Reference | |
| 16-20 patients | 1.705 (0.441-6.598) | .439 |
| 21-25 patients | 1.735 (0.391-7.710) | .469 |
| >25 patients | 1.267 (0.265-6.056) | .767 |
| Hour per week worked: | ||
| <40 hours | Reference | |
| 40 hours | 0.761 (0.84-6.874) | .808 |
| 41-50 hours | 0.429 (0.046-3.987) | .456 |
| >50 hours | 6.108 (0.299-124.654) | .24 |
Additionally, respondents were asked about their level of satisfaction based on various job responsibilities. There was no relationship between average patient census or hours per week worked and level of satisfaction (Table 3). However, having a dedicated ICU pharmacist for each ICU at the institution was associated with job satisfaction (Exp(ß) 4.498; 95% CI 1.054-19.187).
Discussion
In this cross-sectional survey of critical care pharmacists throughout the United States, practice variation was present for what type of activities and how activities were documented. Despite lack of routine documentation, a majority of pharmacists participated in activities outside of patient care, and these activities were used in annual performance reviews and for justification of new positions. Higher rates of tracking patient-care interventions was present, but other essential and desirable activities as outlined by the ACCP/SCCM/ASHP position statement had less formalized tracking, even though these activities may represent a significant portion of respondent daily activities. 18 This survey provides unique perspective on the relationship between best practice of CCPs versus current management practices.
Practice variation in productivity tracking is unsurprising, as there are numerous challenges to which no ideal solutions have been identified. First, pharmacist productivity has traditionally utilized metrics such as number of doses dispensed and number of orders verified due to the distribution centered model of pharmacy.19,20 However, traditional productivity measures (eg, number of orders verified per shift) often do not represent intellectual workload or other clinical activities. For example, Rough et al notes that while one can track pharmacist productivity as full time employees (FTEs) per patient-adjusted day, some patients require more pharmacist interventions for optimal care, and strict numerical correlation does not appropriately track pharmacist workload (eg, relative expertise required to verify docusate vs daptomycin). 21 As the pharmacist’s role shifts to a more patient-focused model, productivity may be better measured using clinical interventions on the patient-level as well as non-direct patient care activities that pharmacists regularly engage in. Yet, these methods, often labeled “widget tracking,” have limitations as well. 22 First, the validity and usefulness of value tracking lies in the individual pharmacist’s consistent documentation of their own interventions.23-25 As such, the additional task of documentation, which often requires an external system, may be a barrier to consistent documentation as pharmacists may feel that they do not have the time to document interventions fully. 21 Further, the quality or impact of interventions has not been well established. Additionally, the distinction between cost-savings and cost-avoidance and how these are calculated can also limit value tracking.3,26-28 Direct cost-savings has traditionally been used as a measure of pharmacist productivity; however, this metric may underestimate the true monetary contribution from pharmacists that could be better classified through cost-avoidance.3,29 Yet, utilizing cost-avoidance as a measure of pharmacist productivity has been criticized as likely overestimating the financial contribution of pharmacists, given that the numbers used for estimates of cost-avoidance are based on low-quality evidence.26,30 Finally, the simple summation of activities, both patient-care and non-patient care, does not allow for an accurate depiction of time or value per activity as pure documentation is unlikely to fully demonstrate outcomes or value associated with that activity. 21
This survey observed that non-direct patient care activities were formally documented to a lesser extent (29%-49% for non-direct patient care activities vs 68% for clinical interventions); however, more emphasis on this pharmacist activity may be warranted as many protocols that have been incepted, created, and implemented by clinical pharmacists have shown substantial improvement in patient outcomes.31-33 Additionally, these non-direct patient care activities may prevent the need for direct patient care interventions (eg, policy for safe use of neuromuscular blocking agents may prevent need for pharmacist interventions in this complex and vulnerable population), but this quality improvement based optimization may require more labor intensive evaluation to document and assign value (eg, manual chart review for a medication use evaluation). Further, while each individual initiative may be evaluated for efficacy, holistic summaries of departmental initiatives may or may not be tracked. These non-direct patient care activities may support cost-savings initiatives, medication safety improvements, etc. that all serve the institutions in achievement of strategic planning goals. Such, quality improvement initiatives may support compliance with legal and accreditation requirements. Indeed, in the ACCP Standards of Practice for Clinical Pharmacists, while much delineation is present for the process of direct patient care, just a short paragraph supporting these other roles is provided. 34
This study also observed further patterns including that respondents frequently work more than forty hours per week, care for more than 15 patients on a regular basis (a ratio touted as ideal by expert opinion), and participate in a wide variety of activities and roles. 35 Interestingly, this study observed an association between dedicated ICU pharmacists and satisfaction. Although beyond the scope of this study, a possibility exists that a link exists between an inability to reliably quantify and predict the value of care provided, high patient care workloads, and clinical burnout. A recent literature review of ICU clinician workload for intensivists and advanced practice providers found that increased workload and conflict among professional colleagues, among others, were common independent risk factors for burnout, which is supported by similar studies in critical care pharmacists.36-38 Indeed, now more than ever, the conversation of the workload of ICU professionals has come to the forefront, and deliberate evaluation of how this scarce resource is both justified and deployed is warranted. 36
This study has several limitations. This was a cross-sectional study thus limiting the ability to examine causal relationships between pharmacist perceptions and pharmacy practice. Overall, the response rate was lower than anticipated (<5%), potentially due to the timing during the COVID-19 pandemic. Additionally, there were multiple responses from the same institution, which could potentially introduce bias in the responses. The distribution platform of the survey being those pharmacists that pay annual dues to be part of a critical care pharmacist community may also select for more involved pharmacists who participate in an above average amount of non-patient care activities, as potentially evidenced by the high rate of leadership positions and academic medical centers, which may introduce bias; however, even among this more homogenous group, lack of standardization was present and may indicate areas for future evaluation.
Conclusion
Pharmacists regularly partake in activities that include both direct and indirect patient care activities; however, documentation practices do not always appear to capture these activities. Standardized methods for documenting and assigning value to critical care pharmacists’ activities may support incremental improvement of critical care pharmacist practice models and optimizing the care of critically ill patients and warrants further investigation.
Supplemental Material
Supplemental material, sj-docx-1-hpx-10.1177_00185787211024209 for Productivity Tracking: A Survey of Critical Care Pharmacist Practices and Satisfaction by Christy Cecil Forehand, Kathryn Fitton, Kelli Keats, Aaron Chase, Susan E. Smith and Andrea Sikora Newsome in Hospital Pharmacy
Acknowledgments
Sarah Payne Maddox, PharmD; Ah Hyun Jun, PharmD, BCCCP.
Footnotes
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Dr. Newsome has received research funding through the National Center for Advancing Translational Sciences (NCATS) of the National Institutes of Health (NIH) under Award Numbers UL1TR002378 and KL2TR002381; she consults for Ayma Therapeutics Inc. All other authors have no conflict of interest to disclose.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Christy Cecil Forehand  https://orcid.org/0000-0001-7523-0490
https://orcid.org/0000-0001-7523-0490
Kathryn Fitton  https://orcid.org/0000-0003-2759-8869
https://orcid.org/0000-0003-2759-8869
Kelli Keats  https://orcid.org/0000-0002-6686-1079
https://orcid.org/0000-0002-6686-1079
Aaron Chase  https://orcid.org/0000-0002-5891-4492
https://orcid.org/0000-0002-5891-4492
Susan E. Smith  https://orcid.org/0000-0002-5171-8405
https://orcid.org/0000-0002-5171-8405
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Erstad BL. Justification of the value of critical care pharmacists: still a work in progress? Am J Health Syst Pharm. 2020;22:1906-1909. [DOI] [PubMed] [Google Scholar]
- 2. Rudis MI, Brandl KM. Position paper on critical care pharmacy services. Society of Critical Care Medicine and American College of Clinical Pharmacy Task Force on Critical Care Pharmacy Services. Crit Care Med. 2000;11:3746-3750. [DOI] [PubMed] [Google Scholar]
- 3. Hammond DA, Flowers HJC, Meena N, Painter JT, Rech MA. Cost avoidance associated with clinical pharmacist presence in a medical intensive care unit. J Am Coll Clin Pharm. 2019;6:610-615. [Google Scholar]
- 4. Jones TW, Newsome AS, Smith SE, Forehand C. Interprofessional shared decision-making: who is at the table? Crit Care Med. 2020;2:e158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kane SL, Weber RJ, Dasta JF. The impact of critical care pharmacists on enhancing patient outcomes. Intensive Care Med. 2003;5:691-698. [DOI] [PubMed] [Google Scholar]
- 6. Leape LL, Cullen DJ, Clapp MD, et al. Pharmacist participation on physician rounds and adverse drug events in the intensive care unit. JAMA. 1999;3:267-270. [DOI] [PubMed] [Google Scholar]
- 7. Leguelinel-Blache G, Nguyen T-L, Louart B, et al. Impact of quality bundle enforcement by a critical care pharmacist on patient outcome and costs. Crit Care Med. 2018;2:199-207. [DOI] [PubMed] [Google Scholar]
- 8. MacLaren R, Bond CA, Martin SJ, Fike D. Clinical and economic outcomes of involving pharmacists in the direct care of critically ill patients with infections. Crit Care Med. 2008;12:3184-3189. [DOI] [PubMed] [Google Scholar]
- 9. Marshall J, Finn CA, Theodore AC. Impact of a clinical pharmacist-enforced intensive care unit sedation protocol on duration of mechanical ventilation and hospital stay. Crit Care Med. 2008;2:427-433. [DOI] [PubMed] [Google Scholar]
- 10. Preslaski CR, Lat I, MacLaren R, Poston J. Pharmacist contributions as members of the multidisciplinary ICU team. Chest. 2013;5:1687-1695. [DOI] [PubMed] [Google Scholar]
- 11. Stollings JL, Foss JJ, Ely EW, et al. Pharmacist leadership in ICU quality improvement: coordinating spontaneous awakening and breathing trials. Ann Pharmacother. 2015;8:883-891. [DOI] [PubMed] [Google Scholar]
- 12. Ball AM, Schultheis J, Lee H-J, Bush PW. Evidence of burnout in critical care pharmacists. Am J Health Syst Pharm. 2020; 10:790-796. [DOI] [PubMed] [Google Scholar]
- 13. Jones GM, Roe NA, Louden L, Tubbs CR. Factors associated with burnout among US hospital clinical pharmacy practitioners: results of a Nationwide Pilot Survey. Hosp Pharm. 2017;11:742-751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Navin TR, Miller KD, Satriale RF, Lobel HO. Adverse reactions associated with pyrimethamine-sulfadoxine prophylaxis for Pneumocystis carinii infections in AIDS. Lancet. 1985; 8441:1332. [DOI] [PubMed] [Google Scholar]
- 15. El-Ibiary SY, Yam L, Lee KC. Assessment of burnout and associated risk factors among pharmacy practice faculty in the United States. Am J Pharm Educ. 2017;4:75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Durham ME, Bush PW, Ball AM. Evidence of burnout in health-system pharmacists. Am J Health Syst Pharm. 2018; 23(Suppl 4):S93-S100. [DOI] [PubMed] [Google Scholar]
- 17. Haupt MT, Bekes CE, Brilli RJ, et al. Guidelines on critical care services and personnel: recommendations based on a system of categorization of three levels of care. Crit Care Med. 2003;11:2677-2683. [DOI] [PubMed] [Google Scholar]
- 18. Lat I, Paciullo C, Daley M, et al. Position paper on critical care pharmacy services: 2020 update. Crit Care Med. 2020; 48(9):e813-e834. [DOI] [PubMed] [Google Scholar]
- 19. Louden L, Lopez BR, Naseman RW, Weber RJ. Evolving pharmacist productivity models. Hosp Pharm. 2016;1:89-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Rough SS, McDaniel M, Rinehart JR. Effective use of workload and productivity monitoring tools in health-system pharmacy, part 2. Am J Health Syst Pharm. 2010;5: 380-388. [DOI] [PubMed] [Google Scholar]
- 21. Rough SS, McDaniel M, Rinehart JR. Effective use of workload and productivity monitoring tools in health-system pharmacy, part 1. Am J Health Syst Pharm. 2010;4:300-311. [DOI] [PubMed] [Google Scholar]
- 22. Abramowitz PW. The evolution and metamorphosis of the pharmacy practice model. Am J Health Syst Pharm. 2009;16: 1437-1446. [DOI] [PubMed] [Google Scholar]
- 23. Kim DY, Schepers G. Pharmacist intervention documentation in US health care Systems. Hosp Pharm 2017;38(12). [Google Scholar]
- 24. Pandya D. Capturing Pharmacy Interventions Without the Use of External Documentation. American Society of Health-System Pharamcists Practice Advancement Inititiave. [Google Scholar]
- 25. Sayles TJ. Documentation of pharmacists’ interventions and associated cost savings. Am J Health Syst Pharm. 2004;8:838-840. [DOI] [PubMed] [Google Scholar]
- 26. Haas CE, Vermeulen LC. Caution warranted when torturing data until they confess. J Am Coll Clin Pharm. 2019;6:606-607. [Google Scholar]
- 27. Sikora Newsome A, Murray B, Smith SE, et al. Optimization of critical care pharmacy clinical services: a gap analysis approach. Am J Health Syst Pharm. 2021;1;zxab237. doi: 10.1093/ajhp/zxab237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Murray B, Sikora Newsome A. Avoiding cost avoidance. Am J Health Syst Pharm. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hammond DA, Rech MA. Cautions heeded: a call to action for evaluating pharmacists’ direct and indirect patient care activities. J Am Coll Clin Pharm. 2020;546-547. [Google Scholar]
- 30. Vermeulen LC, Haas CE. Drs. Haas and Vermeulen reply to Drs. Hammond and Rech. J Am Coll Clin Pharm. 2020;2:548-549. [Google Scholar]
- 31. Stollings JL, Foss JJ, Ely EW, et al. Pharmacist leadership in ICU quality improvement: coordinating spontaneous awakening and breathing trials. Ann Pharmacother. 2015;8:883-891. [DOI] [PubMed] [Google Scholar]
- 32. Leguelinel-Blache G, Nguyen TL, Louart B, et al. Impact of quality bundle enforcement by a critical care pharmacist on patient outcome and costs. Crit Care Med. 2018;2:199-207. [DOI] [PubMed] [Google Scholar]
- 33. Bissell BD, Laine ME, Thompson Bastin ML, et al. Impact of protocolized diuresis for de-resuscitation in the intensive care unit. Crit Care. 2020;1:70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. American College of Clinical Pharmacy. Standards of practice for clinical pharmacists. Pharmacotherapy. 2014;8:794-797. [DOI] [PubMed] [Google Scholar]
- 35. Newsome AS, Smith SE, Jones TW, Taylor A, Berkel MAV, Rabinovich M. A survey of critical care pharmacists to patient ratios and practice characteristics in intensive care units. J Am Coll Clin Pharm. 2020;1:68-74. [Google Scholar]
- 36. Pastores SM, Kvetan V, Coopersmith CM, et al. Workforce, workload, and burnout among intensivists and advanced practice providers: a narrative review. Crit Care Med. 2019;4:550-557. [DOI] [PubMed] [Google Scholar]
- 37. McQuade BM, Reed BN, DiDomenico RJ, Baker WL, Shipper AG, Jarrett JB. Feeling the burn? A systematic review of burnout in pharmacists. J Am Coll Clin Pharm. 2020;3(3):663-675. [Google Scholar]
- 38. Smith SE, Slaughter AA, Finder SA, Buckley MS, MacLaren R, Sikora Newsome A. Examination of critical care pharmacist work activities and burnout. J Am Coll Clin Pharm. 2020;4:554-569. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-hpx-10.1177_00185787211024209 for Productivity Tracking: A Survey of Critical Care Pharmacist Practices and Satisfaction by Christy Cecil Forehand, Kathryn Fitton, Kelli Keats, Aaron Chase, Susan E. Smith and Andrea Sikora Newsome in Hospital Pharmacy