Abstract
Objective
The purpose of this study was to examine the effectiveness and mechanism of clear aligner therapy for the correction of anterior open bite in adult nonextraction cases.
Methods
Sixty-nine adult patients with anterior open bite were enrolled and classified into Angle’s Class I, II, and III groups. Fifty patients presented with skeletal open bite (mandibular plane angle [MPA] ≥ 38°), whereas 19 presented with dental open bite. Fifteen cephalometric landmarks were identified before (T1) and after (T2) treatment. The magnitudes of planned and actual movements of the incisors and molars were calculated.
Results
Positive overbite was achieved in 94% patients, with a mean final overbite of 1.1 ± 0.8 mm. The mean change in overbite was 3.3 ± 1.4 mm. With clear aligners alone, 0.36 ± 0.58 mm of maxillary molar intrusion was achieved. Compared with the Class I group, the Class II group showed greater maxillary molar intrusion and MPA reduction. The Class III group showed greater mandibular incisor extrusion with no significant vertical skeletal changes.
Conclusions
Clear aligners can be effective in controlling the vertical dimension and correcting mild to moderate anterior open bite in adult nonextraction cases. The treatment mechanism for Class III patients significantly differed from that for Class I and Class II patients. Maxillary incisor extrusion in patients with dental open bite and MPA reduction with mandibular incisor extrusion in patients with skeletal open bite are the most significant contributing factors for open bite closure.
Keywords: Clear aligner, Orthodontic treatment, Tooth movement, Anterior open bite
INTRODUCTION
Open bite is one of the most challenging malocclusions to treat, because it is associated with skeletal, dental, functional, and habitual factors.1-3 Open bite is classified into dental open bite and skeletal open bite. The latter is characterized by an increased mandibular plane angle (MPA) and lower facial height (LFH). In contrast, dental open bite is characterized by proclined incisors, undererupted anterior teeth, and a normal or slightly excessive molar height, and patients often exhibit thumb or finger sucking habits.4
In adults, treatment options are limited.5-8 Orthognathic surgery is indicated for adult patients with severe skeletal open bite and unesthetic facial proportions.9,10 For patients with less severe skeletal open bite and those who do not wish to undergo surgery, nonsurgical fixed appliance therapy with intermaxillary vertical elastics and, occasionally, extraction has been a viable alternative. However, this treatment often results in a poor facial esthetics and significant side effects such as root resorption.11,12 Therefore, the search for more effective and efficient treatment modalities is ongoing. Over the past two decades, skeletal temporary anchorage devices (TADs) have significantly expanded the scope of orthodontic treatment beyond the traditional limits of tooth movement, facilitating the correction of anterior open bite with orthodontic treatment alone.13-15
Adult orthodontic patients frequently seek less invasive treatment alternatives for open bite correction in order to avoid extractions, temporary skeletal anchorage devices (TADs), or surgery. Clear aligners have become popular for the treatment of adult patients because of superior esthetics and comfort.16-18 Previous literature has indicated that clear aligners may be effective in the treatment of open bite because occlusal coverage provides a mechanical advantage over fixed appliances in terms of vertical dimension control.16-21 However, the mechanism by which clear aligners correct open bite remains controversial. Most evidence supporting the effectiveness of open bite treatment with clear aligners has come from case reports, case series, or manufacturer’s claims. While some previous studies have reported both intrusion of molars and extrusion of incisors as the mechanism for open bite correction by clear aligners,17,21 others have reported extrusion of incisors as the main mechanism.22
Accordingly, we designed this retrospective study to examine the effectiveness and mechanism of clear aligner therapy for the correction of anterior open bite in adult nonextraction cases. We also aimed to explore the mechanism by which clear aligners correct anterior open bite and determine differences in treatment mechanics among different vertical skeletal patterns and Angle’s classification method.
MATERIALS AND METHODS
Subjects
This retrospective study was approved by the institutional review board of University of the Pacific (#16-77). The sample was drawn from the database of patients treated at the practice of a single board-certified (American Board of Orthodontics) clinician (B.G.) who is also a Top 1% Invisalign provider. To minimize selection bias, the clinician was not involved in the sampling process. A list of all patients who started orthodontic treatment between 2011 and December of 2019 was generated. This period was chosen because algorithms for posterior teeth intrusion were introduced in 2011. The total number of adult patients eligible for screening was 1,799. The primary inclusion criteria were as follows: 1) age > 18 years, 2) receipt of Invisalign treatment, 3) complete pre- and post-treatment records (lateral cephalograms and study casts), and 4) presence of an anterior open bite of overbite < −0.5 mm on lateral cephalograms. Patients with craniofacial anomalies, fixed orthodontic treatment, limited treatment, extraction of teeth other than third molars, and surgeries were excluded. To identify patients with anterior open bite, two research dentists visually examined initial lateral cephalograms and photographs of all eligible adult patients using Dolphin ImagingTM (version 11.8; Dolphin Imaging and Management Solutions, Chatsworth, CA, USA). From 79 (4.5%) patients with a clinically detectable anterior open bite, 10 were further excluded because anterior open bite was less than 0.5 mm on the radiograph.
The final sample comprised 69 adult patients with anterior open bite (Table 1). Skeletal and dental open bites were differentiated on the basis of the initial MPA using SN-MPA. Patients with MPA ≥ 38° were classified into the skeletal open bite group, whereas patients with MPA < 38° were classified into the dental open bite group. Fifty of 69 patients (72%) had skeletal open bite; the remaining 19 had dental open bite (Table 1). Regarding the sagittal relationship, the patients were divided into three groups using Angle’s classification. The Class II group included patients with an equal or greater than end-on Class II molar relationship bilaterally. Patients who presented with a less than half cusp Class II to Class I molar relationship were classified into the Class I group. The Class III group included patients with an equal or greater than end-on Class III molar relationship bilaterally, with a negative or edge-to-edge overjet. Because severe skeletal Class III open bites were predominantly treated by orthognathic surgery, only nine patients with Class III malocclusion were included in the final sample. The total sample included 44 Class I, 16 Class II, and 9 Class III patients.
Table 1.
Characteristics of adult patients with anterior open bite in the present study
| Category | n | % |
|---|---|---|
| Sex | ||
| Male | 15 | 23 |
| Female | 54 | 77 |
| Age (yr) | ||
| 18–25 | 6 | 9 |
| 25–35 | 44 | 64 |
| ≥ 35 | 19 | 27 |
| Initial overbite (mm) | ||
| < −5 | 3 | 4 |
| −5 to −4 | 7 | 10 |
| −4 to −3 | 9 | 13 |
| −3 to −2 | 10 | 14 |
| −2 to −1 | 30 | 44 |
| −1 to −0.5 | 10 | 14 |
| Vertical pattern (M:F) | ||
| Dental open bite | 19 (8:11) | 28 |
| Skeletal open bite | 50 (7:43) | 72 |
| Angle Classification (M:F; Dental open bite:Skeletal open bite) | ||
| Class I | 44 (9:35; 13:31) | 64 |
| Class II | 16 (2:14; 2:14) | 23 |
| Class III | 9 (4:5; 4:5) | 13 |
| Previous orthodontic treatment | ||
| Yes (Extraction vs. Non-extraction) | 13 (6 vs. 7) | 19 |
| None | 56 | 81 |
| Third molar present at T1 | 18 | |
| Extraction during treatment | 9 | 50 |
| Remained in arch | 9 | 50 |
Treatment modality
No TADs were utilized, and crowding was resolved by interproximal reduction and some arch expansion. Extraction of third molars before clear aligner therapy was recommended if they occluded with the opposing teeth. Before treatment, myofunctional therapy was discussed for patients who presented with anterior tongue thrust. The patients were instructed to change their aligners every 7 to 10 days. In general, clear aligner therapy exerts intrusive forces on the posterior teeth and extrusive forces on the anterior teeth by utilizing optimized attachments; they extrude the anterior teeth as a unit by leveraging the posterior teeth as anchorage to close the open bite (Invisalign’s G4 protocol).
Class I malocclusion with skeletal open bite is considered “masked Class III malocclusion.” When the molars are intruded, the mandible often autorotates, and a more severe Class III relationship develops and requires Class III elastics with additional incisor retraction. For Class II patients with open bite, greater molar intrusion was planned. The clinician planned to close the open bite through molar intrusion and autorotation of the mandible. For half cusp or less Class II molar relationships, Class II correction was achieved with the use of Class II elastics, whereas full-cusp Class II molar relationships were treated by sequential distalization. Class II elastics were applied from precision cuts in the maxillary canine and buttons on the mandibular first molar. For Class III patients with skeletal open bite, molar intrusion was planned to maintain the vertical dimension while Class III elastics were used. In contrast, Class III patients with dental open bite were treated by extrusion of the maxillary molars and mandibular incisors using Class III elastics.
Cephalometric analysis
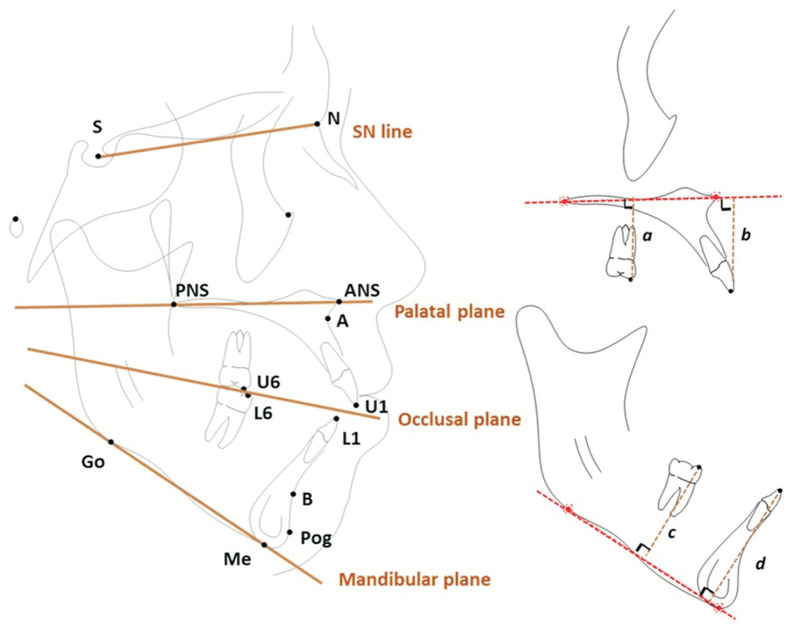
Pre (T1)- and post-treatment (T2) lateral cephalograms were imported into Dolphin ImagingTM. Cephalometric landmark location and superimpositions were independently performed using Dolphin ImagingTM by two orthodontic faculty members. Following anterior cranial base, maxillary, and mandibular structural superimpositions, three reference planes (S-N, ANS-PNS, and Go-Me) were transferred from the T1 tracing to the T2 tracing. Fifteen cephalometric measurements were generated by the computer operations in Dolphin ImagingTM (Figure 1). The average values of estimates derived by the two orthodontists were used.
Figure 1.
Cephalometric landmarks, reference planes, and dentoalveolar linear measurements used in this study. Measurements were measured using the same reference planes at T1 and T2 tracings. a (U6-PP), perpendicular distance between mesiobuccal cusp of maxillary 1st molar and palatal plane (ANS-PNS) (mm); b (U1-PP), perpendicular distance between incisal edge of maxillary central incisor and palatal plane (mm); c (L6-MP), perpendicular distance between mesiobuccal cusp of mandibular 1st molar and mandibular plane (Go-Me) (mm); d (L1-MP), perpendicular distance between incisal edge of mandibular central incisor and mandibular plane (mm).
T1, before treatment; T2, after treatment; S, sella; N, nasion; A, A point; B, B point; Pog, pogonion; Go, gonion; Me, menton; ANS, anterior nasal spine; PNS, posterior nasal spine.
Evaluation of programmed tooth movements in ClinCheck®
The programmed vertical movements for each tooth were exported from the tooth movement table in the first ClinCheck® (Align Technology Inc., San Jose, CA, USA) plan approved by the clinician. The mean value for the right and left first molars was used for molar movement, while the average value for the four incisors was used for incisor movement. The following equation was used for estimation of the percentage accuracy: Percentage accuracy = 100% − ([|planned − achieved|/|planned|] × 100%).23,24
Statistical analysis
The inter-rater reliability of the cephalometric measurements was assessed by the intraclass coefficient (ICC). Chi-square tests were used to compare proportions between the groups. With regard to treatment-changes, stepwise multiple regression was performed to investigate relationships among variables. The paired t-test was used to assess cephalometric changes. Two-way analysis of variance (ANOVA) and Tukey’s post hoc test were used to evaluate the influences of Angle’s classification and the vertical pattern and their interaction with treatment changes. Pearson’s correlation analysis was performed to investigate the relationships among variables in the dental and skeletal groups. p-values < 0.05 were considered statistically significant. All statistical analyses were performed using SPSS (version 24.0; IBM Corp., Armonk, NY, USA) and language R (version 3.6.1; R Foundation for Statistical Computing, Vienna, Austria).
RESULTS
In total, 77% patients were female, and there was no statistically significant difference in sex distribution among the Class I, II, and III groups. However, the proportion of female patients was significantly higher in the skeletal open bite group than in the dental open bite group (86% vs. 58%, respectively; p = 0.005). Overall, the mean age at T1 was 33.0 ± 8.4 years, and the mean treatment duration was 1.4 ± 0.72 years. There were no statistically significant differences in the treatment duration and the number of refinements among the Class I, II, and III groups.
Cephalometric analysis
The inter-rater reliability was excellent, with an ICC > 0.9 for all cephalometric measurements. Table 1 shows the distribution of open bite severity. At T1, the mean overbite was −2.2 mm and MPA was 41.07° (Table 2). The initial skeletal characteristics except overjet were similar in the Class I and II groups (Table 3). Class II patients presented with significantly greater MPAs than did Class III patients. At T2, positive overbite was achieved in 94% patients. Only four of the 69 patients did not achieve a positive overbite. The mean change in overbite for the overall sample was 3.3 ± 1.4 mm (Table 2), with no significant differences in mean overbite changes and the mean final overbite among the Class I, II, and III groups (Table 3).
Table 2.
Mean, standard deviation, minimum, and maximum values and comparison of cephalometric measurements before (T1) and after (T2) clear aligner treatment for open bite correction in adult nonextraction cases (n = 69)
| Measurement | T1 | T2 | Changes (T2-T1) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Min | Max | Mean | SD | Min | Max | Mean | SD | Min | Max | p-value | |||
| ANB (°) | 4.21 | 2.65 | −1.60 | 9.90 | 4.10 | 2.66 | −1.95 | 9.40 | −0.11 | 0.46 | −2.00 | 0.80 | 0.05 | ||
| SNA (°) | 79.47 | 4.05 | 71.70 | 90.30 | 79.51 | 4.13 | 71.70 | 90.65 | 0.04 | 0.20 | −0.75 | 0.65 | 0.07 | ||
| SNB (°) | 75.26 | 4.67 | 65.70 | 88.65 | 75.42 | 4.63 | 66.90 | 88.50 | 0.16 | 0.44 | −1.00 | 1.40 | 0.004** | ||
| OPA (°) | 20.68 | 5.42 | 5.00 | 34.40 | 21.23 | 5.88 | 3.45 | 32.65 | 0.54 | 2.21 | −3.35 | 8.05 | 0.05 | ||
| MPA (°) | 41.07 | 7.41 | 22.75 | 57.75 | 40.64 | 7.41 | 23.20 | 57.65 | −0.42 | 0.95 | −2.35 | 3.40 | 0.004** | ||
| LFH (mm) | 72.64 | 5.41 | 59.30 | 87.15 | 72.04 | 5.64 | 59.30 | 86.50 | −0.60 | 1.10 | −3.05 | 3.40 | < 0.001*** | ||
| IIA (°) | 122.78 | 9.13 | 100.95 | 143.35 | 132.80 | 8.42 | 112.90 | 152.80 | 10.02 | 6.40 | −5.55 | 30.25 | < 0.001*** | ||
| U1SNA (°) | 102.04 | 6.81 | 89.30 | 120.40 | 96.35 | 7.30 | 83.00 | 116.95 | −5.69 | 4.38 | −21.75 | 3.95 | < 0.001*** | ||
| IMPA (°) | 94.11 | 7.11 | 75.60 | 109.10 | 90.22 | 7.67 | 67.40 | 104.20 | −3.89 | 4.55 | −16.00 | 13.55 | < 0.001*** | ||
| OB (mm) | −2.21 | 1.39 | −6.55 | −0.55 | 1.09 | 0.80 | −0.85 | 2.85 | 3.30 | 1.43 | 0.70 | 7.05 | < 0.001*** | ||
| OJ (mm) | 3.22 | 2.05 | −2.75 | 10.75 | 2.64 | 0.69 | 0.80 | 5.75 | −0.59 | 1.94 | −8.85 | 4.65 | 0.01* | ||
| U6-PP (mm) | 24.99 | 2.38 | 20.35 | 31.30 | 24.63 | 2.44 | 19.70 | 31.80 | −0.36 | 0.58 | −1.85 | 1.25 | < 0.001*** | ||
| U1-PP (mm) | 29.80 | 2.83 | 23.65 | 38.35 | 31.01 | 2.92 | 24.40 | 38.40 | 1.20 | 0.93 | −0.45 | 3.90 | < 0.001*** | ||
| L6-MP (mm) | 33.85 | 2.78 | 28.90 | 42.80 | 33.73 | 2.82 | 28.80 | 42.05 | −0.12 | 0.47 | −1.00 | 1.35 | 0.04* | ||
| L1-MP (mm) | 37.39 | 3.37 | 30.50 | 43.85 | 38.75 | 3.85 | 32.15 | 47.70 | 1.36 | 1.30 | −1.60 | 4.70 | < 0.001*** | ||
ANB, point A-nasion-poing B angle; SNA, sella-nasion-point A angle; SNB, sella-nasion-point B angle; OPA, occlusal plane angle; MPA, mandibular plane angle; LFH, lower facial height; IIA, interincisal angle; U1SNA, upper incisor to sella-nasion angle; IMPA, incisor mandibular plane angle; OB, overbite; OJ, overjet.
Paired sample t-tests were performed to compare T1 and T2 difference. *p < 0.05; **p < 0.01; ***p < 0.001.
See Figure 1 for definitions of the other measurement.
Table 3.
Comparison of cephalometric measurements among Angle’s Class I, II, and III groups of adult patients with anterior open bite treated by clear aligners without extraction
| Measure-ment | Class I (n = 44) | Class II (n = 16) | Class III (n = 9) | p-value‡ | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T1 | T2 | T2-T1 | p-value† | T1 | T2 | T2-T1 | p-value† | T1 | T2 | T2-T1 | p-value† | ||||
| ANB (°) | 4.30 ± 2.37 | 4.17 ± 2.47 | −0.14 ± 0.39 | 0.02* | 5.51 ± 2.75 | 5.32 ± 2.75 | −0.20 ± 0.65 | 0.25 | 1.43 ± 1.78 | 1.58 ± 1.74 | 0.15 ± 0.35 | 0.24 | 0.21 | ||
| SNA (°) | 79.20 ± 3.79 | 79.24 ± 3.85 | 0.04 ± 0.13 | 0.05 | 78.72 ± 4.06 | 78.75 ± 4.17 | 0.03 ± 0.33 | 0.74 | 82.08 ± 4.72 | 82.17 ± 4.8 | 0.09 ± 0.16 | 0.14 | 0.78 | ||
| SNB (°) | 74.90 ± 3.99 | 75.08 ± 4.02 | 0.18 ± 0.41 | 0.006** | 73.22 ± 4.04 | 73.44 ± 4.02 | 0.22 ± 0.57 | 0.15 | 80.64 ± 5.2 | 80.58 ± 5.14 | −0.06 ± 0.27 | 0.51 | 0.16 | ||
| OPA (°) | 20.96 ± 5.09 | 21.36 ± 4.86 | 0.40 ± 1.57a | 0.10* | 22.11 ± 4.94 | 24.50 ± 5.52 | 2.40 ± 2.51b | 0.002** | 16.83 ± 6.58 | 14.76 ± 6.41 | −2.07 ± 1.28c | 0.001** | < 0.001*** | ||
| MPA (°) | 40.82 ± 7.36 | 40.42 ± 7.53 | −0.45 ± 0.67ac | 0.001** | 44.63 ± 6.35 | 43.84 ± 6.60 | −0.80 ± 0.91a | 0.003** | 35.91 ± 6.61 | 36.07 ± 5.93 | 0.16 ± 1.46c | 0.76 | 0.04* | ||
| LFH (mm) | 72.52 ± 5.66 | 71.87 ± 5.80 | −0.65 ± 0.93ac | < 0.001*** | 71.90 ± 4.93 | 70.95 ± 5.10 | −0.95 ± 1.00a | 0.002** | 74.57 ± 5.09 | 74.8 ± 5.44 | 0.23 ± 1.67c | 0.69 | 0.02* | ||
| IIA (°) | 122.33 ± 8.25 | 130.70 ± 8.14 | 9.38 ± 4.88 | < 0.001*** | 121.19 ± 10.61 | 132.95 ± 8.73 | 11.77 ± 9.73 | < 0.001*** | 127.81 ± 9.87 | 137.84 ± 8.26 | 10.04 ± 5.85 | < 0.001*** | 0.61 | ||
| U1SNA (°) | 101.94 ± 6.20 | 96.70 ± 6.23 | −5.24 ± 3.36a | < 0.001*** | 100.79 ± 6.49 | 92.02 ± 6.91 | −8.76 ± 5.71b | < 0.001*** | 104.75 ± 9.88 | 102.31 ± 8.74 | −2.44 ± 2.99a | 0.04* | 0.003** | ||
| IMPA (°) | 94.91 ± 7.05 | 91.19 ± 7.80 | −3.72 ± 3.29a | < 0.001*** | 93.38 ± 7.55 | 91.20 ± 6.04 | −2.18 ± 6.39a | 0.19 | 91.53 ± 6.56 | 83.78 ± 7.09 | −7.75 ± 4.31c | < 0.001*** | 0.005** | ||
| OB (mm) | −2.20 ± 1.50 | 1.10 ± 0.71 | 3.30 ± 1.46 | < 0.001*** | −2.55 ± 1.36 | 1.08 ± 0.96 | 3.63 ± 1.43 | < 0.001*** | −1.66 ± 0.56 | 1.06 ± 0.98 | 2.72 ± 1.17 | < 0.001*** | 0.48 | ||
| OJ (mm) | 3.28 ± 1.46 | 2.71 ± 0.70 | −0.57 ± 1.41a | 0.01* | 4.63 ± 2.26 | 2.63 ± 0.64 | −2.00 ± 2.22b | 0.003** | 0.43 ± 1.34 | 2.26 ± 0.7 | 1.83 ± 1.29c | 0.003** | < 0.001*** | ||
| U6-PP (mm) | 24.88 ± 2.23 | 24.49 ± 2.23 | −0.39 ± 0.51a | < 0.001*** | 24.35 ± 2.50 | 23.79 ± 2.55 | −0.56 ± 0.51a | < 0.001*** | 26.66 ± 2.35 | 26.81 ± 2.22 | 0.14 ± 0.74c | 0.58 | 0.01* | ||
| U1-PP (mm) | 29.72 ± 2.84 | 30.89 ± 2.91 | 1.16 ± 0.86ac | < 0.001*** | 29.44 ± 2.65 | 31.20 ± 2.97 | 1.76 ± 1.00a | < 0.001*** | 30.85 ± 3.16 | 31.27 ± 3.2 | 0.42 ± 0.48c | 0.03* | 0.002** | ||
| L6-MP (mm) | 33.98 ± 2.94 | 33.82 ± 2.92 | −0.16 ± 0.47 | 0.03* | 33.12 ± 2.47 | 33.07 ± 2.58 | −0.05 ± 0.39 | 0.62 | 34.49 ± 2.47 | 34.47 ± 2.8 | −0.03 ± 0.62 | 0.90 | 0.59 | ||
| L1-MP (mm) | 37.46 ± 3.25 | 38.81 ± 3.43 | 1.35 ± 0.94a | < 0.001*** | 35.67 ± 3.15 | 36.28 ± 3.23 | 0.61 ± 1.53a | 0.13 | 40.07 ± 2.62 | 42.84 ± 3.47 | 2.77 ± 1.37c | < 0.001*** | < 0.001*** | ||
Values are presented as mean ± standard deviation.
T1, before treatment; T2, after treatment.
*p < 0.05; **p < 0.01; ***p < 0.001.
†Intragroup comparison of T2-T1 difference (paired-sample t-test; significance at p < 0.05).
‡ANOVA for cephalometric changes across Class I, Class II, and Class III groups; values with different superscript letters are significantly different.
To determine the mechanism by which open bite correction was achieved with clear aligners, stepwise multiple regression analysis was performed (n = 69). A model including changes (ΔT2-T1) in U1-PP, L1-MP, and MPA was selected as follows: ΔOverbite (mm) = 0.57 + 1.01 [ΔU1-PP (mm)] + 0.83 [ΔL1-MP (mm)] − 0.92 [ΔMPA (°)] (R2 = 0.831, p < 0.0001) (Table 4). Another well-fitting model was built on the basis of vertical changes in the molars instead of the change in MPA: ΔOverbite (mm) = 0.42 + 1.08 [ΔU1-PP (mm)] + 0.78 [Δ L1-MP (mm)] − 1.20 [ΔU6-PP (mm)] − 0.74 [ΔL6-MP (mm)] (R2 = 0.836, p < 0.0001; Table 4).
Table 4.
Selected regression models presenting relationships between changes in overbite and predictor variables in adult patients with anterior open bite treated by clear aligners without extraction
| Predictors | ∆Overbite (mm) | |||
|---|---|---|---|---|
| Estimates | CI | p-value | ||
| Model 1 | Intercept | 0.57 | 0.22 to 0.91 | 0.002** |
| ∆U1-PP (mm) | 1.01 | 0.84 to 1.17 | < 0.001*** | |
| ∆L1-MP (mm) | 0.83 | 0.71 to 0.95 | < 0.001*** | |
| ∆MPA (°) | −0.92 | −1.08 to −0.75 | < 0.001*** | |
| R2 | 0.831 | |||
| Model 2 | Intercept | 0.42 | 0.05 to 0.79 | 0.028* |
| ∆U1-PP (mm) | 1.08 | 0.91 to 1.24 | < 0.001*** | |
| ∆L1-MP (mm) | 0.78 | 0.66 to 0.91 | < 0.001*** | |
| ∆U6-PP (mm) | −1.2 | −1.49 to −0.91 | < 0.001*** | |
| ∆L6-MP (mm) | −0.74 | −1.07 to −0.42 | < 0.001*** | |
| R2 | 0.836 | |||
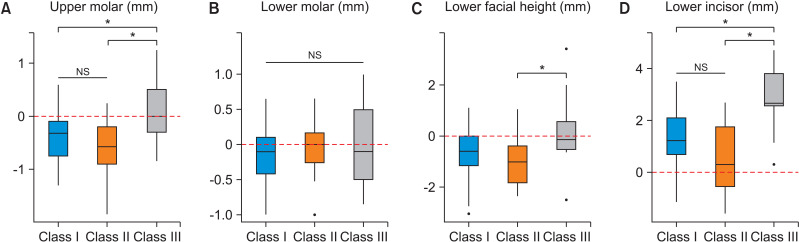
With regard to cephalometric changes (T2-T1), two-way ANOVA found no statistically significant interaction between Angle’s classification and the vertical pattern. Therefore, the results were separately interpreted. The treatment mechanism in the Class III group was significantly different from those in the Class I and Class II groups (Table 3, Figure 2). There were statistically significant differences in changes in the vertical dimension. The magnitudes of maxillary molar intrusion in the Class I and Class II groups were similar at 0.39 and 0.56 mm, respectively. Maxillary molar intrusion contributed to autorotation of the mandible and a decrease in the lower face height in both the Class I and Class II groups. In contrast, the vertical positions of the maxillary and mandibular molars were maintained in the Class III group, where a significantly greater amount of mandibular incisor extrusion and retroclination contributed to anterior open bite closure (Figure 2).
Figure 2.
Vertical changes by Angle class groups. A, U6-PP change; B, L6-MP change; C, lower facial height change; D, L1-MP change. Dental intrusion presented as negative value; dental extrusion presented as positive value.
NS, not significant.
* Represents significant difference between the groups. Statistical significance set at p < 0.05.
See Figure 1 for definitions of each measurement.
In the comparison of the dental and skeletal open bite groups, we found no statistically significant differences in changes in cephalometric measurements. Overbite correction was slightly greater in the skeletal (3.47 ± 1.38 mm) than in the dental (2.84 ± 1.48 mm) open bite group, although the difference was not statistically significant. Changes in MPA, LFH, and L1-MP were moderately correlated with changes in overbite in the skeletal open bite group, but not in the dental open bite group (Table 5).
Table 5.
Relationship between changes in overbite and changes in cephalometric variables during treatment (T2-T1) according to the vertical skeletal pattern
| Changes (T1-T2) | Dental open bite group (n = 19) | Skeletal open bite group (n = 50) | |||
|---|---|---|---|---|---|
| Correlation coefficient (r) | p-value | Correlation coefficient (r) | p-value | ||
| ANB | −0.49 | 0.03* | −0.32 | 0.01* | |
| SNA | −0.05 | 0.83 | 0.21 | 0.14 | |
| SNB | 0.51 | 0.03* | 0.44 | 0.001** | |
| OPA | −0.11 | 0.66 | −0.14 | 0.33 | |
| MPA | −0.29 | 0.23 | −0.53 | < 0.001*** | |
| LFH | −0.36 | 0.13 | −0.52 | < 0.001*** | |
| IIA | 0.15 | 0.53 | 0.35 | 0.01* | |
| U1SNA | −0.24 | 0.32 | −0.16 | 0.26 | |
| IMPA | 0.10 | 0.68 | −0.25 | 0.04* | |
| OJ | −0.31 | 0.20 | 0.01 | 0.92 | |
| U6-PP | 0.00 | 0.99 | −0.33 | 0.01* | |
| U1-PP | 0.76 | < 0.001*** | 0.32 | 0.01* | |
| L6-MP | −0.53* | 0.02 | −0.35 | 0.01* | |
| L1-MP | 0.37 | 0.12 | 0.45 | 0.001** | |
Comparison of planned and actual incisor and molar movements
With regard to programmed tooth movements in ClinCheck® (Table 6), the amount of programmed intrusion in the Class II group was almost twice the amount programmed for the Class I and Class III groups. Only about 55% and 38% of the programmed maxillary molar intrusion was achieved in the Class I and Class II groups, respectively. No maxillary molar intrusion was observed in the Class III group (Table 3). Moreover, no meaningful mandibular molar intrusion was achieved despite programmed intrusion of approximately 0.5–0.6 mm for all three groups.
Table 6.
Comparison of programmed vertical tooth movements in ClinCheck®† among Angle’s Class I, II, and III groups of adult patients with anterior open bite treated by clear aligners without extraction
| Vertical movements | Planned movement | Actual movement | ||||||
|---|---|---|---|---|---|---|---|---|
| Class I (n = 44) | Class II (n = 16) | Class III (n = 9) | p-value‡ | Dental open bite group (n = 19) | Skeletal open bite group (n = 50) | p-value‡ | ||
| U6 (mm) | −0.71 ± 0.52a | −1.45 ± 0.78bc | −0.79 ± 0.66ac | < 0.001 | −0.77 ± 0.53 | −0.93 ± 0.72 | 0.34 | |
| L6 (mm) | −0.63 ± 0.56 | −0.48 ± 0.63 | −0.60 ± 0.54 | 0.54 | −0.42 ± 0.45 | −0.66 ± 0.60 | 0.13 | |
| U1 (mm)* | 0.69 ± 1.00 | 0.49 ± 1.05 | 0.31 ± 0.37 | 0.48 | 0.80 ± 1.16 | 0.52 ± 0.86 | 0.29 | |
| L1 (mm)* | 0.11 ± 0.86 | 0.13 ± 0.58 | −0.42 ± 0.99 | 0.19 | 0.08 ± 1.15 | 0.02 ± 0.69 | 0.79 | |
Values are presented as mean ± standard deviation.
The minus sign indicates intrusion while the plus sign indicates extrusion.
U6, maxillary 1st molar; L6, mandibular 1st molar; U1, maxillary central incisor; L1, mandibular central incisor.
*Vertical movements of the incisors included only absolute extrusion/intrusion movements.
†Data collected from the first ClinCheck® (Align Technology Inc., San Jose, CA, USA).
‡Two-way ANOVA and Tukey post hoc test. Values with different superscript letters are significantly different (p < 0.05).
DISCUSSION
Clear aligner therapy is a relatively new approach, and studies regarding its biomechanics and effectiveness are limited. In the present study, we demonstrated that correction of mild to moderate anterior open bite using clear aligners was effective in adult nonextraction cases. The mean change in overbite was 3.3 ± 1.4 mm (range: 0.7 mm to 7.1 mm). A positive overbite was achieved in over 94% patients overall, and the average treatment duration was approximately 1.5 years.
A complicated feature of research involving clear aligner treatment is that there are three tooth positions involved in the treatment: desired tooth position, planned (programmed) tooth position in ClinCheck®, and actual tooth position. The programmed tooth movement and actual tooth movement may differ25 as a result of anchorage loss or interarch elastic use. Therefore, in certain cases, overcorrection or undercorrection might be programmed to achieve the desired tooth position.23 In this study, we mainly focused on the actual vertical tooth movement achieved by clear aligners.
According to the stepwise regression model, approximately 0.4 mm of maxillary molar intrusion results in an increase of 0.5 mm in overbite. Therefore, for a change of 3.3 mm in overbite (mean overbite change, n = 69), 0.4 mm of maxillary molar intrusion (mean maxillary molar intrusion, n = 69) made a 15% contribution to the total open bite correction. The increase in overbite of 1.2 mm per 1 mm of maxillary molar intrusion in the present study was smaller than that in previous studies, which reported a 2–3 mm increase in overbite.26-29 This discrepancy may be attributed to the data interpretation methods, as simple ratios and linear regressions can be differently interpreted. The coefficient for maxillary molar intrusion in the present study was close to that in previous studies that showed an overbite increase of 1.5 mm26 and 1.2 mm28 per 1 mm of additional maxillary molar intrusion. Although its generalizability is limited, the model could adequately assess the contribution of molar intrusion to open bite correction.
The present study also showed that cephalometric changes differed according to the characteristics of open bite in the Class I, II, and III groups. In Class II patients, the greatest changes were observed in terms of maxillary incisor retroclination, MPA reduction, and maxillary molar intrusion (Table 3). Even with Class II elastics and distalization mechanics, good vertical control was achieved with slight MPA reduction. Mild to moderate Class III patients with less severe skeletal open bite achieved bite closure through good vertical control and retroclination and extrusion of the mandibular incisors. The clinician programmed intrusive movements for the maxillary molars and mandibular incisors in order to negate significant extrusive movements due to the Class III elastics (Table 6).
We found no statistically significant differences in treatment changes between the dental and skeletal open bite groups in the present study, probably because most of the included patients showed hyperdivergent patterns, although 19 patients were classified into the dental open bite group (MPA < 38°). The results of the correlation analysis (Table 5) indicated that maxillary incisor extrusion (U1-PP) was strongly correlated with changes in overbite in the dental open bite group, whereas MPA reduction and the consequent LFH reduction, along with mandibular incisor extrusion (L1-MP), were moderately correlated with open bite closure in the skeletal open bite group.
There was a significant difference between programmed and actual extrusive movements of incisors in the present study (Tables 6 and 3, respectively). The actual vertical position change (U1- PP) in the maxillary incisors has three components: programmed absolute extrusion of U1, relative extrusion from U1 retroclination, and the reciprocal extrusive force on the incisor from molar intrusion-related anchorage loss. Celebi and Bicakci30 reported that 0.4–0.5 mm of relative extrusion/intrusion occurred with each 5° change in inclination when U1-SNA ranged from 93°–115°.
Vertical control tends to be challenging in adult patients. Molar extrusion resulting in clockwise rotation of the mandible is generally observed with fixed appliance therapy.14,31 On the other hand, maxillary molar intrusion due to skeletal anchorage has been reported in the range of 1.45–4 mm, with a mean intrusion of approximately 2 mm.11,14,32,33 The present study showed that clear aligners alone achieved a relatively small amount of molar intrusion yet reliable vertical control. Consistent maxillary molar intrusion, although in small amounts, was achieved in 55 of the 69 cases. For the Class I and II groups in the present study, approximately 1 mm of maxillary molar intrusion was planned, and less than 1 mm was achieved (0.4 and 0.6 mm in the Class I and Class II groups, respectively) with clear aligners alone. Maxillary molar intrusion of 0.4 mm with clear aligners was reported in a previous study.17 While the present study showed a statistically significant but clinically small amount of intrusion, the possibility of more intrusion with an increase in programmed remains questionable. Currently, some clinicians consider > 1 mm of intrusion to be less predictable.34 In addition, molar intrusion anchorage loss could result in greater maxillary incisor extrusion.34 It is also important to consider the fact that patients with skeletal open bite, who comprised the majority of the sample in the present study, tend to have a weak musculature and low occlusal bite forces.35,36 While mandibular molar intrusion of 0.8 mm was reported in the prior study,17 we found that mandibular molar intrusion was achieved in half of the total cases, while the vertical position of the mandibular molars were maintained in the other half, in the present study.
The present study has some limitations other than its retrospective design. First, the study would have benefitted from a larger sample size, particularly for the Class III group. According to the results, however, the treatment mechanism for open bite correction with clear aligners in Class III patients is significantly different from that in Class I and Class II patients. Accordingly, future studies should consider the Class III group as a separate group. Second, to compare differences between the programmed and actual tooth movements and quantify the predictability of tooth movement using clear aligners, actual tooth movements were measured from lateral cephalograms so that global references could be used, given that no teeth or structures in the dental arch could be used for superimposition. Thus, only a general pattern for each tooth movement could be evaluated. Digital scans integrated with a cone beam computed tomography study in the future should resolve this issue. Finally, the generalizability of the results of this study is limited because the sample was derived from a single clinician’s practice. However, this reduced heterogeneity and eliminated the effects of variability in clinical skills.
CONCLUSION
Using nonextraction Clear aligner therapy, open bite correction (positive overbite) was achieved in 94% adult patients with anterior open bite.
Clear aligners alone can provide limited but consistent maxillary molar intrusion with maintenance of the vertical position of the mandibular molars. This, in turn, offered reasonable vertical control.
The mechanism of open bite correction using clear aligners in Class III patients was significantly different from that in Class I and Class II patients.
Maxillary incisor extrusion in dental open bite group and MPA reduction with mandibular incisor extrusion in skeletal open bite group are the most significant contributing factors for open bite closure.
Footnotes
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
REFERENCES
- 1.Remmers D, Van't Hullenaar RW, Bronkhorst EM, Bergé SJ, Katsaros C. Treatment results and long-term stability of anterior open bite malocclusion. Orthod Craniofac Res. 2008;11:32–42. doi: 10.1111/j.1601-6343.2008.00411.x. [DOI] [PubMed] [Google Scholar]
- 2.Todoki LS, Finkleman SA, Funkhouser E, Greenlee GM, Choi KW, Ko HC, et al. The National Dental Practice-Based Research Network adult anterior open bite study: treatment success. Am J Orthod Dentofacial Orthop. 2020;158:e137–50. doi: 10.1016/j.ajodo.2020.07.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ngan P, Fields HW. Open bite: a review of etiology and management. Pediatr Dent. 1997;19:91–8. [PubMed] [Google Scholar]
- 4.Beane RA., Jr Nonsurgical management of the anterior open bite: a review of the options. Semin Orthod. 1999;5:275–83. doi: 10.1016/S1073-8746(99)80021-8. [DOI] [PubMed] [Google Scholar]
- 5.Subtelny JD, Sakuda M. Open-bite: diagnosis and treatment. Am J Orthod. 1964;50:337–58. doi: 10.1016/0002-9416(64)90175-7. [DOI] [Google Scholar]
- 6.Dung DJ, Smith RJ. Cephalometric and clinical diagnoses of open bite tendency. Am J Orthod Dentofacial Orthop. 1988;94:484–90. doi: 10.1016/0889-5406(88)90006-6. [DOI] [PubMed] [Google Scholar]
- 7.Nielsen IL. Vertical malocclusions: etiology, development, diagnosis and some aspects of treatment. Angle Orthod. 1991;61:247–60. doi: 10.1043/0003-3219(1991)061<0247:VMEDDA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 8.Greenlee GM, Huang GJ, Chen SS, Chen J, Koepsell T, Hujoel P. Stability of treatment for anterior open-bite malocclusion: a meta-analysis. Am J Orthod Dentofacial Orthop. 2011;139:154–69. doi: 10.1016/j.ajodo.2010.10.019. [DOI] [PubMed] [Google Scholar]
- 9.Conley RS, Legan HL. Correction of severe vertical maxillary excess with anterior open bite and transverse maxillary deficiency. Angle Orthod. 2002;72:265–74. doi: 10.1043/0003-3219(2002)072<0265:COSVME>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 10.Quintão APA, Nunes LKF, Rédua RB, Brunharo IHP, Quintão CCA. Nonsurgical treatment for a severe anterior and lateral open bite and multiple congenitally missing teeth: a case report with 4-year follow-up. Dental Press J Orthod. 2017;22:74–85. doi: 10.1590/2177-6709.22.6.074-085.oar. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sherwood KH, Burch JG, Thompson WJ. Closing anterior open bites by intruding molars with titanium miniplate anchorage. Am J Orthod Dentofacial Orthop. 2002;122:593–600. doi: 10.1067/mod.2002.128641. [DOI] [PubMed] [Google Scholar]
- 12.Motokawa M, Terao A, Kaku M, Kawata T, Gonzales C, Darendeliler MA, et al. Open bite as a risk factor for orthodontic root resorption. Eur J Orthod. 2013;35:790–5. doi: 10.1093/ejo/cjs100. [DOI] [PubMed] [Google Scholar]
- 13.Kuroda S, Sakai Y, Tamamura N, Deguchi T, Takano-Yamamoto T. Treatment of severe anterior open bite with skeletal anchorage in adults: comparison with orthognathic surgery outcomes. Am J Orthod Dentofacial Orthop. 2007;132:599–605. doi: 10.1016/j.ajodo.2005.11.046. [DOI] [PubMed] [Google Scholar]
- 14.Deguchi T, Kurosaka H, Oikawa H, Kuroda S, Takahashi I, Yamashiro T, et al. Comparison of orthodontic treatment outcomes in adults with skeletal open bite between conventional edgewise treatment and implant-anchored orthodontics. Am J Orthod Dentofacial Orthop. 2011;139(4 Suppl):S60–8. doi: 10.1016/j.ajodo.2009.04.029. [DOI] [PubMed] [Google Scholar]
- 15.Graber W, Vanarsdall R, Vig KWL, Huang G. Orthodontics: current principles and techniques. Elsevier; Louis: 2017. p. 212. [DOI] [Google Scholar]
- 16.Boyd RL, Waskalic V. Three-dimensional diagnosis andorthodontic treatment of complex malocclusions with the invisalign appliance. Semin Orthod. 2001;7:274–93. doi: 10.1053/sodo.2001.25414. [DOI] [Google Scholar]
- 17.Moshiri S, Araújo EA, McCray JF, Thiesen G, Kim KB. Cephalometric evaluation of adult anterior open bite non-extraction treatment with Invisalign. Dental Press J Orthod. 2017;22:30–8. doi: 10.1590/2177-6709.22.5.030-038.oar. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Garnett BS, Mahood K, Nguyen M, Al-Khateeb A, Liu S, Boyd R, et al. Cephalometric comparison of adult anterior open bite treatment using clear aligners and fixed appliances. Angle Orthod. 2019;89:3–9. doi: 10.2319/010418-4.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dayan W, Aliaga-Del Castillo A, Janson G. Open-bite treatment with aligners and selective posterior intrusion. J Clin Orthod. 2019;53:53–4. [PubMed] [Google Scholar]
- 20.Guarneri MP, Oliverio T, Silvestre I, Lombardo L, Siciliani G. Open bite treatment using clear aligners. Angle Orthod. 2013;83:913–9. doi: 10.2319/080212-627.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Harris K, Ojima K, Dan C, Upadhyay M, Alshehri A, Kuo CL, et al. Evaluation of open bite closure using clear aligners: a retrospective study. Prog Orthod. 2020;21:23. doi: 10.1186/s40510-020-00325-5.1b2c3ec4276d462e823544f101da2f1e [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Khosravi R, Cohanim B, Hujoel P, Daher S, Neal M, Liu W, et al. Management of overbite with the Invisalign appliance. Am J Orthod Dentofacial Orthop. 2017;151:691–9.e2. doi: 10.1016/j.ajodo.2016.09.022. [DOI] [PubMed] [Google Scholar]
- 23.Haouili N, Kravitz ND, Vaid NR, Ferguson DJ, Makki L. Has Invisalign improved? A prospective follow-up study on the efficacy of tooth movement with Invisalign. Am J Orthod Dentofacial Orthop. 2020;158:420–5. doi: 10.1016/j.ajodo.2019.12.015. [DOI] [PubMed] [Google Scholar]
- 24.Kravitz ND, Kusnoto B, BeGole E, Obrez A, Agran B. How well does Invisalign work? A prospective clinical study evaluating the efficacy of tooth movement with Invisalign. Am J Orthod Dentofacial Orthop. 2009;135:27–35. doi: 10.1016/j.ajodo.2007.05.018. [DOI] [PubMed] [Google Scholar]
- 25.Galan-Lopez L, Barcia-Gonzalez J, Plasencia E. A systematic review of the accuracy and efficiency of dental movements with Invisalign®. Korean J Orthod. 2019;49:140–9. doi: 10.4041/kjod.2019.49.3.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kim K, Choy K, Park YC, Han SY, Jung H, Choi YJ. Prediction of mandibular movement and its center of rotation for nonsurgical correction of anterior open bite via maxillary molar intrusion. Angle Orthod. 2018;88:538–44. doi: 10.2319/102317-714.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kuhn RJ. Control of anterior vertical dimension and proper selection of extraoral anchorage. Angle Orthod. 1968;38:340–9. doi: 10.1043/0003-3219(1968)038<0340:COAVDA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 28.Kassem HE, Marzouk ES. Prediction of changes due to mandibular autorotation following miniplate-anchored intrusion of maxillary posterior teeth in open bite cases. Prog Orthod. 2018;19:13. doi: 10.1186/s40510-018-0213-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schudy FF. The control of vertical overbite in clinical orthodontics. Angle Orthod. 1968;38:19–39. doi: 10.1043/0003-3219(1968)038<0019:TCOVOI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 30.Celebi F, Bicakci AA. Relative intrusion as a result of protrusion: a mathematical perspective. Int J Appl Dent Sci. 2017;3:218–23. [Google Scholar]
- 31.Arat M, Iseri H. Orthodontic and orthopaedic approach in the treatment of skeletal open bite. Eur J Orthod. 1992;14:207–15. doi: 10.1093/ejo/14.3.207. [DOI] [PubMed] [Google Scholar]
- 32.Scheffler NR, Proffit WR, Phillips C. Outcomes and stability in patients with anterior open bite and long anterior face height treated with temporary anchorage devices and a maxillary intrusion splint. Am J Orthod Dentofacial Orthop. 2014;146:594–602. doi: 10.1016/j.ajodo.2014.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lee HA, Park YC. Treatment and posttreatment changes following intrusion of maxillary posterior teeth with miniscrew implants for open bite correction. Korean J Orthod. 2008;38:31–40. doi: 10.4041/kjod.2008.38.1.31. [DOI] [Google Scholar]
- 34.Tai S. Clear aligner technique. International Quintessence Publishing Group; Berlin: 2018. [DOI] [Google Scholar]
- 35.Ingervall B, Helkimo E. Masticatory muscle force and facial morphology in man. Arch Oral Biol. 1978;23:203–6. doi: 10.1016/0003-9969(78)90217-0. [DOI] [PubMed] [Google Scholar]
- 36.Proffit WR, Fields HW, Nixon WL. Occlusal forces in normal- and long-face adults. J Dent Res. 1983;62:566–70. doi: 10.1177/00220345830620051201. [DOI] [PubMed] [Google Scholar]