Abstract
Background
With increasing requirements for medical effects, and huge differences among individuals, traditional surgical instruments are difficult to meet the patients' growing medical demands. 3D printing is increasingly mature, which connects to medical services critically as well. The patient specific surgical guide plate provides the condition for precision medicine in orthopaedics.
Methods
In this paper, a systematic review of the orthopedic guide template is presented, where the history of 3D-printing-guided technology, the process of guides, and basic clinical applications of orthopedic guide templates are described. Finally, the limitations of the template and possible future directions are discussed.
Results
The technology of 3D printing surgical templates is increasingly mature, standard, and intelligent. With the help of guide templates, the surgeon can easily determine the direction and depth of the screw path, and choose the angle and range of osteotomy, increasing the precision, safety, and reliability of the procedure in various types of surgeries. It simplifies the difficult surgical steps and accelerates the growth of young and mid-career physicians. But some problems such as cost, materials, and equipment limit its development.
Conclusions
In different fields of orthopedics, the use of guide templates can significantly improve surgical accuracy, shorten the surgical time, and reduce intraoperative bleeding and radiation. With the development of 3D printing, the guide template will be standardized and simplified from design to production and use. 3D printing guides will be further sublimated in the application of orthopedics and better serve the patients.
The translational potential of this paper
Precision, intelligence, and individuation are the future development direction of orthopedics. It is more and more popular as the price of printers falls and materials are developed. In addition, the technology of meta-universe, digital twin, and artificial intelligence have made revolutionary effects on template guides. We aim to summarize recent developments and applications of 3D printing guide templates for engineers and surgeons to develop more accurate and efficient templates.
Keywords: 3D printing, Guide templates, Orthopedic applications
1. Introduction
With the increasingly close connection between digital technology and orthopedics, we have diagnosed and cured individual patients in patterns of precision, personalization, and digitalization instead of empirical, generalization, and contouring. As a form of digital technology, 3D printing is an effective method to achieve individualization and precision in various orthopedic procedures [[1], [2], [3]].
3D printing, also known as additive manufacturing (AM) or rapid prototyping, is an emerging technology that uses digital model files as the basis for producing objects [3,4]. The technology differs from the traditional methods of modeling, which changes the traditional removal process to an additional process [2,5,6]. It has advantages that are unmatched by traditional processes, such as rapid forming, better repeatability, and individualization to meet unique or special requirements.
In the medical field, it is increasingly used in a wide range of clinical applications, including guide templates, preoperative models, the implant, human tissue, organs, etc [5]. One of the significant applications is the design and fabrication of patient-specific guides to perform drilling and cutting operations. With the evolution of printing materials and advances in medical imaging, the materials that can satisfy 3D printing have evolved from single solid powders such as metals, plastics, and ceramics to mixed liquids, gels, and cells [3]. Radiological diagnosis of computed tomography (CT) and magnetic resonance imaging (MRI) has become less invasive and more informative [4].
The 3D surgical templates are instruments that are used to guide the placement of internal fixations such as screws, assist in bone repositioning, and aid in determining the extent of osteotomy [7]. During cadaver research as well as clinical studies, the template has attracted increasing attention from clinicians because of its position-independent character and the reduction of surgical procedures [[8], [9], [10]]. With the help of guide templates, the surgeon can easily determine the direction and depth of the screw path, choose the angle and range of osteotomy, increasing the precision, safety, and reliability of the procedure [5,7]. It simplifies the difficult surgical steps, shortens the learning curve for physicians, and accelerates the growth of young and mid-career physicians [11]. The reduction of radiations can reduce surgical complications and improve the quality of orthopedic surgery [12,13]. Compared to surgical navigation systems, surgical guides are more convenient and easier to use. In addition, surgical guides can be performed under minimally invasive conditions, reducing the time spent in the operating room, substantial cost savings for the hospital, reduced patient risk [1,2].
Currently, many hospitals have a positive attitude towards the use of 3D printing technology, and it is widely used in orthopedic surgery, but the attendant problems with data acquisition, guide design, manufacturing, and application have increased accordingly [3,14]. The aim of this article is to review the progress and basic application of surgical guides, analyze the limitations. We hope this review would provide useful information for the engineers and surgeons to design and apply more accurate and intelligent guides, especially for those new to this field and who would like to make contributions to this important multidisciplinary biomedical engineering and orthopedic field.
In this article, the history of 3D printing technology is first reviewed before introducing the progress and main applications of the guide templates. Finally, this article discusses the limitations of the guides and, and looks forward to the future, intending to guide clinical.
2. History of 3D printing
Over the past decades, many professors have conducted research into 3D printing. The concept of using 3D medical imaging, specifically CT data, to reconstruct a physical model was first suggested in 1979 [15]. In the mid-1980s, Professor Charles Hull invented and patented the stereolithography apparatus (SLA) for printing 3D models in the USA. Then he founded a company called 3D Systems to focus on the development of 3D printing technology. In 1988, they invented the first printer which is regarded as a pioneer in 3D printing technology [16].
Scott Crump proposed fused deposition modeling (FDM) in the same year and applied it to the first commercial printer in 1991, followed by the founding of Stratas company [2,17]. Carl Dechard invented selective laser sintering (SLS) at the University of Texas in 1986 and was awarded the first SLS patent for printing 3D models in 1989 [17]. In 1992, laminated object manufacturing (LOM) was invented, but it was not widely used due to its inferior performance [18]. 3D printing technology was first patented in 1989, this is also the first time that the term “3D printer” has been used and is licensed for printing plastic, metal, and ceramic parts.
In the medical field, Mankovich reproduced one of the first anatomical models of the skull by SLA based on CT scan data in 1990 [19]. Early on, a company in San Francisco, USA, made all the components of a prosthetic leg for a patient. The concept of computer-aided orthopedic surgical guides was first introduced in the 1990s by German professor Klaus Radermacher to guide implant placement, tumor removal, osteotomy, bone repositioning and to provide accurate placement of implants or prostheses. The use of surgical guides, which allow for the transfer of pre-operative planning to the actual surgical site, can improve the precision, safety, and reliability of surgery, but the limitations of the equipment, materials, and software at the time did not allow for the manufacture of surgical guides to meet the needs of patients.
Since the early 2000s, computer and 3D printing have developed significantly and have been carried out in the medicine, the aerospace industry, the automotive industry, kitchenware, and other manufacturing industries. Surgical guides were first used as a high-precision tool for oral dental implants and have since been used in maxillofacial surgery, abdominal tumor removal, urology, and cardiovascular surgery. The first application in orthopedics was reported to produce guides in the placement of pedicle screws. With the development of technology, it is gradually used in shoulder, hip, knee, ankle, and trauma surgery, greatly improving surgical efficiency [7,20]. Precision, intelligence, and minimal invasiveness are the future direction of orthopedics, and guide templates will play an important role in all aspects of orthopedic surgery.
3. The process of 3D printing
3D printing surgical guides have become a hot spot in the field of medical image computing. Although the steps to generate a digital 3D model vary from different applications, the following are the general steps required to print a 3D model [1,5,7]. We can use imaging equipment to obtain source datasets visualized in two dimensions. With post-processing tools and algorithms, it is possible to produce multiplanar reformations and 3D views of the anatomy.
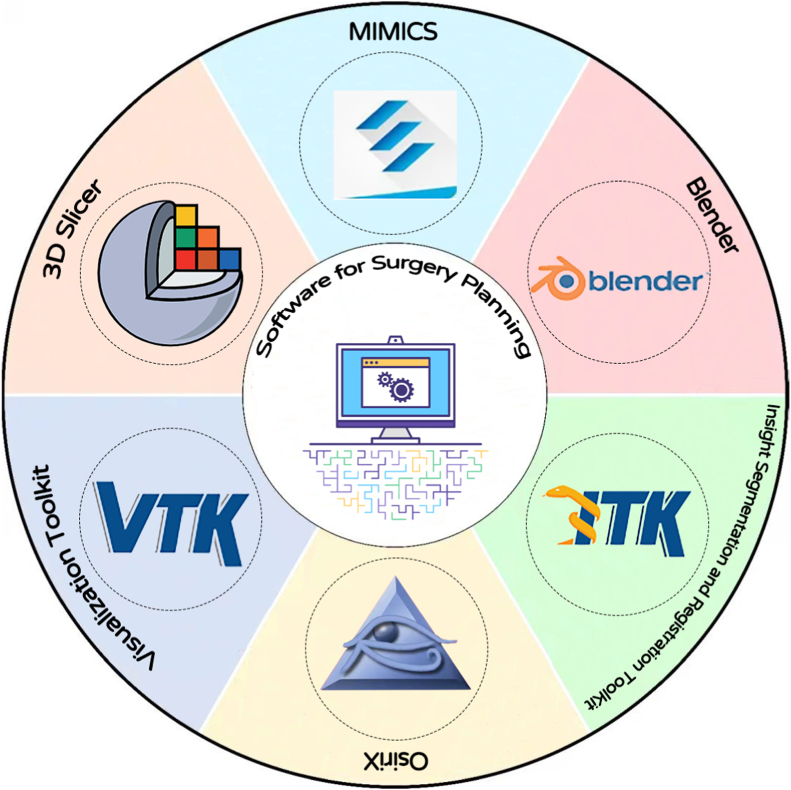
Currently, the medical designed software for surgery planning is mainly divided into three categories [21]. Firstly, the commercially available software, such as the MIMICS system developed by Materialise in Belgium was one of the most widely used and the most comprehensive software [22]. It can perform dedicated anatomical analysis, create accurate virtual 3D models, and plan a surgical procedure virtually [23]. Other software, for example, Analyze, 3D-DOCTOR, SimPlant, and SurgiCase can import image data and export 3D models for 3D analysis, finite element analysis meshing, design, or 3D printing [7].
Then, there are some open-source medical image processing softwares in open source, such as 3DSlicer, OsiriX, and Blender. These open source medical imaging frameworks are freely available to developers. 3DSlicer is the most developed and comprehensive open source image processing tool [2]. It can operate on iOS, Windows, and Linux, which carry out analysis and visualization of diffusion tensor imaging data and automatic image segmentation. However, it has many parameters and is very complicated to use. OsiriX can only operate on iOS system, which carries out medical image processing, 3D visualization, and partial PACS functions [24]. It is very useful but the functions mainly focus on image fusion, image rendering, and image annotation. Blender supports the entirety of the 3D pipeline: modeling, rigging, animation, simulation, rendering, and compositing [25].
Finally, some research organizations have developed Algorithms Toolkit, including Visualization Toolkit (VTK), insight segmentation and registration ToolKit (ITK), and so on [26]. They offer great benefits to researchers, but they have some drawbacks. ITK doesn't provide visualization capabilities and must be used with VTK, which makes it difficult for users to learn from two large and inconsistent development packages [27]. The above software for surgery planning are shown in Fig. 1.
Fig. 1.
The software for surgery planning.
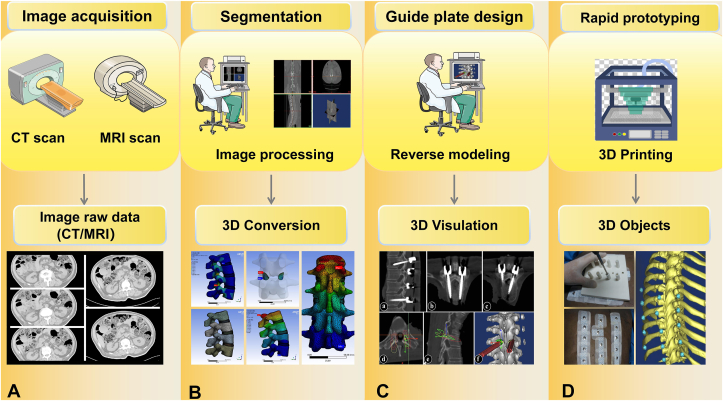
According to the demands of the clinic, we determine the surgical plans, reversely generate surgical guides, and perform 3D printing [4]. The key technologies involved in this method include image acquisition, segmentation/conversion of the medical image, template design, and 3D printing, which are discussed below (Fig. 2).
Fig. 2.
The process of 3D printing (A) The raw data were acquired by using CT or MRI scans of patients (B) Engineers and doctors used Softwares to segment the region of interest area (C) Engineers and doctors completed the 3D reconstruction of the data according to clinical needs (D) According to the data saved in the file, the powders were printed layer by layer to get the final 1:1 recovery of the 3D guide templates.
3.1. Image acquisition
Image acquisition is a very important step in generating a 3D model because the quality of the model depends on the clarity and accuracy of the data [7]. We usually choose CT or MRI data and store the data set in the form of Digital Imaging and Communication in Medicine (DICOM) files [1,28,29]. Although both CT and MRI can be done at ultra-high spatial resolution (400–600 microns) with good quality contrast, CT is widely used in 3D printing because the image post-processing of CT data is relatively simple [2,30]. In addition, several 3D imaging options such as positron emission tomography (PET), single-photon emission computed tomography (SPECT), ultrasound (US), and even images captured on an iPhone are other non-invasive imaging methods that can be used for data collection [1].
3.2. Segmentation/conversion of the medical image
At this stage, either open-source (Osiris® for Macintosh, 3D Slicer® for Windows and Linux, MeVisLab) or licensed (Mimics®, Magics®) can be used to segment the region of interest and complete the 3D reconstruction of the data according to clinical needs. The bone tissue on the image can be segmented manually, but the segmentation is usually not perfect. Part of it is because less bone tissue is selected, and part is because more non-bone tissue is selected. Although automatic segmentation can be done using gray thresholds, the output quality is lower than manual or semi-automatic segmentation. The accurate segmentation of bones requires doctors have good skills and experience in using software segmentation tools [2]. The digital model is still relatively rough and needs further processing. The area to be processed can be converted into a 3D triangular mesh using software, which further processes the mesh data using triangular faces to approximate the shape of the part [31]. Obviously, tiny triangular faces produce smoother surfaces but increase the size of the data. Additional surface refinements can be performed, such as checking and correcting any overlapping surfaces, simplifying image files for more efficient printing.
Nowadays, researchers are focusing on the development of automatic image segmentation algorithms including the region growing method [32], watershed algorithm [33], the deformable biomechanical model method [34], and so on. However, the accuracy of the segmented result may not be sufficient to meet the clinical requirements.
3.3. Guide template design
Afterward, it is processed according to specific clinical needs, surgical approach, and parameters related to the scope of exposure. On this basis, a guiding tube or groove is designed as an intraoperative navigation device. The 3D guides are established to fit, and the obtained guide template data is converted into a printable format. The file should be saved in Stereo Lithography (STL) format [17]. Finally, import the STL file into the 3D printer. Determine the appropriate 3D printing methods and materials based on the clinical requirements, and then build the corresponding physical guides after a certain amount of accumulation based on the collected cross-sectional information. It uses special materials such as metal or plastic powder with laser beams or hot melt nozzles to print the outline of the guide template on the cross-section on a two-dimensional (2D) plane, and then stacks in the z-coordinate layer to form a 3D structure [2]. In addition, in order to simplify the guide design process, some scholars use the C++ programming language (Visual Studio 2013, Microsoft, Redmond, WA) to optimize the operation interface, so that doctors can use the software more easily.
3.4. 3D printing
By reading the data saved in the file, 3D printers manufacture layer by layer to get the final 1:1 recovery of the 3D physical model. The choice of materials is more abundant, such as powder, metal, plastic, etc [2,5]. Table 1 summarizes the 3D Printing technology.
Table 1.
The detailed classification of 3D printing (rapid prototyping or additive manufacturing) technology.
| Types | Description | Materials | Systems for instance | Accuracy | Cost | Advantages | Disadvantages |
|---|---|---|---|---|---|---|---|
| SLA [2,35] | The laser illuminates the bottom of a tank filled with a photo-polymerizing resin. Starting from the bottom layer by layer in the same way to form a 3D model. | Photopolymers | 3D Systems, Rock Hill, SC, USA | +++ | $$ | Large part size, high precision, excellent surface quality, the ability to be waterproof | Moderate strength, photosensitive resin swells or crumples due to changes in physical or chemical conditions |
| FDM [2,17] | The material is heated above its melting temperature. Then extrude and deposit the material layer after layer in the desired shape. | Fused thermoplastic materials or eutectic metals | Stratas Inc., Eden Prairie, MN, USA | ++ | $ | Low cost, good strength, without gases during the printing process | With low speed, the process can lead to high temperatures, which may pose a safety risk |
| SLS [17,18] | The laser selectively scans and melts a layer of material powder at a set speed and energy density. | Small particles of thermoplastic, metal, ceramic, or glass powders | EOS GmbH, Munich, Germany | ++ | $$$ | Large part size, variety of materials, good strength, resistance to water and corrosion, no significant need for support structures | The powdery surface, produces an odor during the melting process |
| LOM [18] | The laser cutting system cuts the contours of the workpiece and hot-melt adhesive coated the workpiece layer by layer to make a three-dimensional workpiece. | Layers of paper or plastic films | Cubic Technologies, Torrance, CA, USA | + | $ | Low cost, large part size | Limited materials |
| SLM [36] | Uses a high power-density laser to melt and fuse metallic powders together; SLM is considered to be a subcategory of SLS. | Metal powders (such as titanium) | Arcam, Molndal, Sweden | ++ | $$ | Variety of materials, relatively low cost | Low speed, rough surfaces, limited materials |
| EBM [36] | The electron beams scan and melt the raw material causing the powders to fuse with each other and solidify. | Metal powders | EOS GmbH | + | $$$ | High forming efficiency, operation in a vacuum environment, avoiding oxidation, and being able to recycle the remaining powder | Less accurate |
SLA = stereo lithography apparatus; FDM = fused deposition modeling; SLS = selective laser sintering; LOM = laminated object manufacturing; SLM = selective laser melting; EBM = electron beam melting.
There are many printing technologies currently in clinical use, SLA [2,35] was the first technology to emerge and be commercialized. It is one of the most intensively researched and widely used 3D printing technologies. Due to its early appearance, the technology is very mature and achieves a high degree of automation to meet the needs of different product models. FDM [2,17] is currently one of the most popular 3D printing technologies. The main clinical applications are preoperative models, intraoperative navigation, and the printing of medical teaching aids. SLS [17] is known as one of the most practical 3D printing technologies due to its low material consumption and high material stability. Because the high temperatures cause the powders to aggregate with each other to form solids, subsequent layers are deposited on the sintered layers until the corresponding 3D model solids are formed. The main clinical applications are the printing of guides, fixation frame, and braces [18].
The EBM and SLM are similar [36]. It's important to note that we need to operate in a vacuum environment. The difference is that the heat source is a laser beam instead of an electron beam. Additionally, Inkjet printing technology, also known as 3D bioprinting technology, is an additive manufacturing technique that can be used for layer-by-layer fabrication of highly complex tissues such as bone and cartilage [2,6,17]. If bioprinting technology can be used to manufacture orthopedic surgical guide templates, it can reduce patient trauma and contribute to the recovery of patient trauma, showing a good application prospect [37].
Even non-professionals can produce impeccable constructions of complex structures with such an easy way in the computer center that has one of these smart printers. There is no need for a specific type of workshop or long-term training for basic access [38]. This encouraged the surgeon to grow up faster through the daily practice of these devices. After all the above work is completed, the surgeon can use the surgical template to perform the operation.
3.5. Printing materials
There are many printing materials that can be used for 3D printing, including photosensitive resin, Polylactic Acid (PLA), Acrylonitrile Butadiene Copolymers (ABS), nylon, and metal [2,39,40]. Since the surgical guides require contact with human tissue directly, it has high requirements on materials [41]. The materials should have no cytotoxicity, no irritation, no skin allergy, and chemical composition in line with the requirements of national and industrial standards [1,42]. According to the physical and chemical properties of the material and various types of surgery, we divide the surgical guides into metal guides and nonmetal guides. Because nonmetal materials are not strong enough, they are often used to make guiding devices, such as round holes to guide Kirschner needles [3]. Metal guides are used to assist the operations of bone-knife and electronic tools in osteotomy or drilling. Because in the process of operation, if the strength is not enough, the surgical guides may create fine chips, and even deformed due to friction heat generation [25].
At present, photosensitive resin is the preferred guide material because of its stable properties and certain strength [43]. ABS and PLA are suitable for some large guides, such as percutaneous spinal guides [44]. The resin can be used for positioning guidance for lower limb osteotomy and deformity correction [45]. Nylon has high precision and high strength, so it is recommended to be used for guide plates with small volume and certain strength requirements like total knee arthroplasty [40,46]. Titanium, medical stainless steel, aluminum alloy, and other metal materials can be processed into guide plates [47]. It can assist the operations of bone-knife and electronic tools in osteotomy or drilling, which increase guide strength and reduce the generation of chips. However, its materials and equipment are expensive, and its costs are high.
4. Basic types and clinical applications of orthopedic 3D printing guide templates
In view of the clinical use of 3D printing orthopedic surgical guides, the guides can be divided into three types: screw placement guides, osteotomy guides, and other series of guides. Osteotomy guides are the main player of 3D printing guides. In orthopedic surgery, 3D printing surgical guides have been used as bone cutting guides and plate positioning guides to help with making corrective osteotomy cuts for malunion cases [23]. It is easier to perform the procedure using the guide because there was no confusion about the bone cutting. The application has resulted in shortened operating time and less intra-operative blood loss [1].
For the radius, a volar Henry approach was assisted by surgical guides, and additional soft tissue release was not required for correction of the deformity [48]. In Bauer's research, all ulnar osteotomies were performed through the subcutaneous approach to the ulna. The drill guides were used first, followed by the osteotomy guides. All cases went according to plan and we encountered no issues in using the guides [49]. To correct the pronated deformity after the first metatarsophalangeal joint arthrodesis accurately, it has been used to guide the bone saw in cutting the metatarsal and proximal phalanx perpendicular to the longitudinal axis [50]. For complicated tibial plateau fracture fixation, the role of the navigational template was to guide the insertion of screws that were locking to the plates. The placement of the locking plate was determined when the location and direction of the screwing were determined [51].
In various types of surgeries, such as the spine, joint, trauma, and bone tumor, the osteotomy guides are used widely. The 3D-printed guides technique makes the preoperative planning more straightforward to execute, without the need for excessive bone cortex removal or multiple fragments, and it increases the chances of success. We will discuss it in different anatomical regions in detail.
Some surgeons often use the freehand technique to select the trajectory of the screw. However, it often leads to postoperative complications, such as vertebral artery and spinal cord injuries, which have a negative impact on the patient's prognosis [52,53]. In order to prevent or minimize the incidence of these complications and determine the optimal trajectory, some operators now use multiple intraoperative X-ray images to guide the orthopedic operation. However, this increases the radiation exposure of both the patient and the surgeon and prolongs the duration of the procedure [54].
Therefore, in order to improve the accuracy and efficiency of the surgery, many doctors have started to investigate 3D printed surgical guides [55]. Adequate stability between the template and the bone is critical in determining whether this technology can be used. Pijpker et al. [56] designed a new 3D printing guide including metal inlays, caudally positioned hooks, and a crosslink support structure that can move more stably with the vertebrae and tested good screw placement accuracy in both the cervical and upper thoracic spine of a cadaver. With regard to the possibility of using the guide template technique for multi-segmental vertebrae, it is still controversial. The reason for this is that large areas of muscle exposure lead to deviations in template placement. In theory, the larger contact area will conduct a better positioning effect. When the surgical exposure site is small, it will block the surgeon's vision, resulting in positioning errors. Therefore, the surgical exposure site must be expanded to ensure that all support points without exception are in contact with the zone of interest [57]. However, excessive dissection of soft tissue may increase the risk of bleeding and infection. Instead, we can choose to use the design of percutaneous guides without the need for surgical exposure site, especially in the parts with thin soft tissues such as ankle joint and iliac crest. Takemoto et al. designed a new template for thoracic pedicle screw placement can reduce the contact area without sacrificing stability [58]. The following will introduce some of their applications in their respective fields. Table 2 shows the main basic research for various types of surgeries and results.
Table 2.
The main basic research of various surgeries.
| Year | Authors | Journal | Case number | Research type | Type of surgery | Results |
|---|---|---|---|---|---|---|
| 2021 | Rho YH et al. [127] | Vet Sci | 8 | dog | A cutting guide and reduction guide for corrective osteotomy | It is useful for novice surgeons to accurately perform corrective osteotomy in dogs without complications. |
| 2021 | Caiti G et al. [137] | Int J Comput Assist Radiol Surg | 5 | cadaver | A cutting and drill guide for fracture of the distal radius | For normal weight arm specimens, navigation of corrective osteotomy via a cast-based guide resulted in transfer errors comparable to those using invasive surgical guides. |
| 2021 | Toni C et al. [9] | Vet Comp Orthop Traumatol | 5 | dog | Lumbar pedicle screws fixation for degenerative lumbosacral stenosis and discospondylitis. | This technique enabled an accurate and safe placement of pedicle screws in the lumbosacral region of dogs with the lumbosacral disease. |
| 2021 | Zhao Y et al. [96] | BMC Musculoskelet Disord | 6 | cadaver | Simultaneously inserting traditional pedicle screws and cortical bone trajectory screws fixation | Using such templates is a safe, feasible, and accurate screw placement method. |
| 2020 | Li Z et al. [44] | J Clin Neurosci | 6 | cadaver | PPSF | It improved the accuracy of PPSF in cadaveric specimens. |
| 2020 | Chen X et al. [86] | Ann Transl Med | 15 | cadaver | Thoracic pedicle screw fixation | The optimal trajectory was obtained through the pedicle central axis, which significantly reduced the risk of cortex breach. |
| 2020 | Easter TG et al. [133] | Vet Surg | 11 | dog | Patient-specific drill guides for HIF | 3D printed guides should be considered as accurate and consistent for placing screws for the treatment of HIF in dogs. |
| 2020 | Liang J et al. [164] | BMC Surg | 17 | cadaver | Acetabular and femoral stem prostheses for THRA | The template of the femoral head can effectively assist surgeons in accurately implanting the femoral head components to the desired position in THRA. |
| 2019 | Pijpker PAJ et al. [56] | Oper Neurosurg | 5 | cadaver | Pedicle and lateral mass screw locus in cervical and upper thoracic vertebrae | The study ultimately resulted in an advanced guide design including caudally positioned hooks, crosslink support structure, and metal inlays. |
| 2019 | Chen XL et al. [66] | PLoS One | 12 | 3D models | Pedicle screw fixation in the upper cervical spine | To implant pedicle screw assisted with the template in the posterior cervical surgery can improve the accuracy of pedicle screw placement and safety of the surgery. |
| 2019 | Fujioka T et al. [82] | Vet Surg | 4 | cadaver | Thoracolumbar pedicle screw fixation | Drill guide templates were useful for accurate intraoperative screw navigation in thoracolumbar fixation in small dogs. |
| 2019 | Wang K et al. [85] | World Neurosurg | 10 | cadaver | Thoracic pedicle screw fixation | Insertion of the CBT screws in the middle-upper thoracic spine with the assistance of the navigation template was safe and convenient. |
| 2019 | Naddeo F et al. [89] | Int J Med Robot | 1 | 3D models | Thoracic pedicle screw fixation | Improvements in terms of precision, duration, and safety were achieved without changing the standard procedure. |
| 2019 | Guo Y et al. [141] | J Hand Surg Am | 12 | cadaver | A drill template for scaphoid fractures | Template to assist screw guidewire placement into an intact scaphoid, mimicking a nondisplaced scaphoid fracture, showed acceptable accuracy in cadaver wrists. |
| 2019 | Wan SX et al. [142] | Curr Med Sci | 10 | cadaver/clinic patients | Mini-invasive percutaneous internal screw fixation for fractured scaphoid | The guide used can assist in accurate placement of the screw, shorten operation time and reduce insertion and X-ray exposure times, reducing the radiation injury and damage to the substance and the blood circulation of carpal bone. |
| 2018 | Zhang G et al. [75] | Orthopade | 12 | cadaver | Cervical pedicle fixation. | This guiding tool may effectively prevent intraoperative drifting and accurately places cervical pedicle screws. |
| 2018 | Peng P et al. [76] | J Orthop Surg Res | 4 | cadaver | CBT screw fixation | Bio-safe drill templates can facilitate cervical anterior transpedicular insertion with good feasibility and accuracy. |
| 2018 | Krämer M et al. [161] | Int J Med Robot | 7 | cadaver | Acetabular cup for total hip arthroplasty | The acetabular cup positioning in total hip arthroplasty procedures can potentially increase the precision of cup placement. |
| 2018 | Wang H et al. [94] | Injury | 15 | bovines | Minimally invasive lumbar pedicle screw placement trajectory | It is promising and could prevent too much radiation exposure intraoperatively. |
| 2018 | Ge DW et al. [95] | Eur Rev Med Pharmacol Sci | 12 | cadaver | Multi-level drill guide template for lumbar pedicle screws | The multi-level drill guide template can be properly applied in pedicle screw placement and promises to be a potential option in clinical application. |
| 2017 | Guo F et al. [65] | PLoS One | 13 | 3D models | Pedicle screw fixation in the upper cervical spine. | The 3D printing navigation template for pedicle screw fixation is easy and safe, with a high success rate in upper cervical spine surgery. |
| 2017 | Yu Z et al. [78] | Eur Spine J | 12 | cadaver | Cervical pedicle placement. | The template combined with the screw tunnel design based on the 3D cutting technique can help facilitate accurate cervical pedicle screw insertion. |
| 2017 | Chen X et al. [144] | Injury | 14 | 3D models | Plates and screws for acetabular fractures | The 3D-printed guiding template helped achieve accurate placement of plates and screws in the pelvis of adult cadavers. |
| 2017 | Sallent A et al. [181] | Bone Joint Res | 5 | cadaver | A cutting guide for pelvic tumor resection | The template improved accuracy in pelvic tumor resections, bringing osteotomy results closer to the parameters set in pre-operative planning, as compared with standard manual techniques. |
| 2017 | Shao ZX et al. [103] | PeerJ | 30 | 3D models | TPTD screw fixation | All TPTD screws were successfully introduced into the 3D-printed model guided by the TPTD screw custom drill guide. |
| 2016 | Chen H et al. [84] | Med Sci Monit | 3 | cadaver | Thoracic pedicle screw fixation | With a high accuracy in placement and convenient operation, it provides a new method for accurate placement of thoracic pedicle screws. |
| 2016 | Zhou Y et al. [157] | Medicine (Baltimore) | 5 | cadaver | The bone-drilling template for Bernese PAO | The application of patient-specific 3D printed bone-drilling and rotation templates in PAO is feasible and may facilitate improved clinical outcomes. |
| 2016 | Huang AB et al. [170] | J Orthop Res | 6 | cadaver | A cutting guide for patellar resurfacing | Customized templates improved the accuracy of patellar resurfacing in terms of obliquity and thickness. |
| 2013 | Hu Y et al. [71] | Eur Spine J | 32 | cadaver | C2 translaminar screws | This technology improves the safety profile of this fixation technique and should be further studied in clinical applications. |
| 2013 | Fu M et al. [11] | PLoS One | 4 | 3D models | ATPS | The drill template is biocompatible, easy-to-apply, and accurate in assisting ATPS insertion. Its clinical applications should be further researched. |
| 2012 | Ma T et al. [83] | Arch Orthop Trauma Surg | 20 | cadaver | Thoracic pedicle screw fixation | We have developed the patient-specific template for thoracic pedicle screw placement with good applicability and high accuracy. |
| 2009 | Ryken TC et al. [73] | J Neurosurg Spine | 4 | cadaver | C3–C7 Pedicle screws | The authors' methods appear to provide an accurate technique and trajectory for pedicle screws placement in the cervical spine. |
| 2009 | Lu S et al. [92] | Int J Med Robot | 12 | cadaver/clinic patients | Lumbar pedicle screws fixation | This method has shown its ability to customize the placement and size of each screw, based on the unique morphology of the lumbar vertebra. |
| 2006 | Hafez MA et al. [166] | Clin Orthop Relat Res | 45 | cadaver/3D models | Cutting blocks for total knee arthroplasty | Patient-specific templates are a practical alternative to conventional instrumentations, but additional clinical validation is required before clinical use. |
| 2001 | Goffin J et al. [53] | Spine | 8 | cadaver/clinic patients | Transarticular C1–C2 fixation | A template with a drill guide might simplify and shorten the surgical act and at the same time enhance the accuracy of C1–C2 transarticular screw positioning. |
PPSF = percutaneous pedicle screw fixation; HIF = humeral intracondylar fissures; THRA = total hip resurfacing arthroplasty; CBT = cortical bone trajectorys; TPTD = transpedicular transdiscal; PAO = periacetabular osteotomy; ATPS = anterior transpedicular screw.
4.1. Spine
Spine surgeons need to deal with a variety of complex spinal problems, including deformity, infection, trauma, and degeneration diseases [59]. In traditional methods of screw fixation, osteotomy, and other operations, the surgeon usually judges whether the screw placement is accurate according to the results of the C-arm or O-arm monitors during the operation or uses computer-aided guidance systems to assist in the placement of the screws [60]. However, due to the varying degrees of proficiency and experience of the surgeon, it is difficult to ensure the accuracy of the operation after the patient's posture changes [61]. The navigation system is expensive, complicated to operate, and has a large amount of radiation exposure. It is difficult to meet the needs of patients and not conducive to universal promotion [12].
As a personalized technology, the patient-specific navigation template can be designed according to the actual situation of the patients [62]. 3D printing screw guides are used to guide precise intraoperative screw placement. The spinal and pelvic region anatomy is complex, adjacent to important blood vessels and nerves. If the screw track trajectory is not ideal, this can lead to a significant reduction in fixation strength and, in severe cases, injury to the vertebral artery, causing significant bleeding problems [61]. The use of pedicle screw guides was first reported in 2005 in a cadaveric study by Berry et al. He tested 3D printing drill templates in cadaveric specimens with varying degrees of success [63]. Subsequently, the professors conducted a large number of experiments for spine pedicle screw placement, vertebral screw placement, cortical bone trajectory (CBT) screw placement, etc [64]. During cadavers and animals study, it improves the surgical team's ability to achieve negative margins.
What is the impact of spinal screw guides on different segments? At present, the main studies and applications of the spine are in vitro simulated screw placement and preliminary clinical applications. We will discuss them in detail separately. Table 3 shows the main clinical application and results of different types of surgery in the spine.
Table 3.
The main clinical application of spinal surgeries.
| Year | Authors | Journal | Case number | Type of surgery | Results |
|---|---|---|---|---|---|
| 2021 | Li Y et al. [67] | Eur Spine J | 60 | Pedicle screw fixation in the upper cervical spine for type II odontoid fractures | 3D printed navigation template leads to greater improvement in the screw safety, efficacy, and accuracy. |
| 2021 | Pijpker PAJ et al. [59] | Spine | 15 | Pedicle and lateral mass screw fixation in the cervical and cervico-thoracic spine | 3D-printed patient-specific drill guides appear to be safe and accurate for pedicle and lateral mass screw insertion in the cervical and upper-thoracic spine. |
| 2021 | Zhao Y et al. [10] | World Neurosurg | 27 | S2AI screw for degenerative scoliosis, revision surgery, spondylolisthesis, and lumbar stenosis | S2AI screw placement assisted by a 3D-printed surgical guide is safe and accurate. |
| 2021 | Liang W et al. [112] | Eur Spine J | 175 | Pedicle screws fixation | 3DP drill guide template was a promising tool for assisting the pedicle screw placement in spinal deformity surgery and deserved further promotion. |
| 2021 | Tu Q et al. [117] | World Neurosurg | 24 | Pedicle screw fixation for hemivertebrectomy and short-segment fixation | 3D-printed individualized templates allow surgery for the correction of congenital scoliosis to enter a new stage of personalized precision surgery. |
| 2021 | Hu PL et al. [120] | J Orthop Surg Res | 36 | PVP for acute painful single segment OVCF | 3D printing template-assisted PVP could minimize fluoroscopy shot operation times and fluoroscopy dosage and is a more precise and feasible operation method. |
| 2021 | He K et al. [100] | Clin Interv Aging | 18 | CBT screws for revision surgery of ASD | Revision surgery for ASD with CBT screws assisted by 3D-printed navigation templates has satisfactory clinical efficacy with the advantages of a short operation time, a small incision, and less blood loss. |
| 2020 | Matsukawa K et al. [102] | Neurosurgical review | 43 | CBT screws for posterior lumbar spinal fusion | A total of 193 screws (97.5%) were placed completely inside the pedicle and there was no incidence of neurovascular injuries. |
| 2020 | Thayaparan GK et al. [80] | J Clin Neurosci | 1 | Cervical pedicle placement for progressive neck pain due to a pathologic fracture of C1. | 3D-printing patient-specific tools and implants that are viable for occipitocervical fixation surgery. |
| 2020 | Zhou W et al. [93] | Arch Orthop Trauma Surg | 31 | Sacroiliac screws placement for sacroiliac complex injury | 3D-printed template technology-assisted surgery for sacroiliac screws placement in sacroiliac complex injury patients possesses advantages such as shortened operation time and reduced X-ray exposure times. |
| 2020 | Zhao Y et al. [104] | BMC Surg | 47 | S2AI screw fixation | The 3D-printed guide technique is superior to the free-hand technique in terms of safety and accuracy. |
| 2020 | Wu C et al. [105] | J Orthop Surg Res | 22 | TSS fixation for sacral fractures | The patient-specific locked navigation template-assisted in TSS placement with less operative time, less intraoperative fluoroscopy, and higher safety of screw placement. |
| 2020 | Wu C et al. [106] | Orthop Surg | 37 | IS fixation for sacral fracture and dislocation | Using the combined template to assist with the insertion of IS screws delivered good accuracy, less fluoroscopy, and shorter operation time, and avoided neurovascular injury as a result of screw malposition. |
| 2020 | Eltes PE et al. [107] | Front Surg | 1 | Pedicle screws fixation | Biomechanical parameters; is more affordable, and the intraoperative X-ray exposure can be reduced. |
| 2020 | Senkoylu A et al. [116] | World Neurosurg | 11 | Pedicle screw fixation for AIS | The use of these low-cost personalized 3D guides is completely safe and effective in both convex and concave sides of the curves. |
| 2020 | Petrone S et al. [101] | J Clin Neurosc | 238 | CBT screws for degenerative lumbosacral disease. | The CBT technique is a safe procedure, especially with accurate preoperative CT scan-based planning. |
| 2019 | Tian Y et al. [13] | Med Sci Monit | 64 | C2 pedicle screws or C2 pars screws fixation in the upper cervical spine. | 3D-printed navigation template technology achieved more accurate C2 pedicle screw placement than C-arm based navigation-assisted. |
| 2019 | Chen PC et al. [108] | Biomed Res Int | 10 | Pedicle screws fixation | 3D printing technology provides an effective alternative for spinal deformity surgery when expensive medical equipment. |
| 2019 | Cecchinato R et al. [109] | Eur Spine J | 29 | Pedicle screw fixation for spinal deformity | 3D-printed pedicle screw guides increase safety in a wide spectrum of deformity conditions. In addition, the total radiation dose is reduced, even considering the need for a low-dose preoperative CT for surgical planning. |
| 2019 | Tu Q et al. [119] | World Neurosurg | 9 | PSOs for severe kyphoscoliosis secondary to AS | 3D-printed templates can guide the performance of planned PSO to provide functional restoration of severe kyphoscoliosis secondary to AS. |
| 2019 | Marengo N et al. [97] | World Neurosurg | 49 | CBT screws for degenerative disease | These devices could also improve placement accuracy and decrease the risk of nerve damage. |
| 2019 | Kim J et al. [98] | World Neurosurg | 1 | CBT screw fixation combined with posterior lumbar interbody fusion | It improved screw placement accuracy while minimizing cortical breach, reduced the operative time, and lower cost compared with intraoperative computed tomography-based neuronavigation. |
| 2018 | Sugawara T et al. [46] | Spine | 103 | Pedicle screw fixation for cervical, thoracic, or cervicothoracic pathologies by the multistep template. | Postoperative CT scans confirmed that 801 screws (98.5%) were accurately placed without cortical violation. There were no injuries to the vessels or nerves. |
| 2018 | Pu X et al. [68] | Clinics | 17 | Pedicle screw fixation in the upper cervical spine for atlantoaxial dislocation and deformity | Atlantoaxial pedicle screw placement assisted by a modified 3D-printed navigation template is worth recommending due to the improved accuracy in screw placement, improved patient safety, and beneficial clinical effects. |
| 2018 | Thayaparan GK et al. [69] | J Clin Neurosci | 3 | Posterior atlantoaxial fixation surgery with C1–C2 transarticular and C1 posterior arch screws. | A safe, accurate, efficient, and relatively inexpensive process to stabilize the atlantoaxial spine using transarticular screws. |
| 2018 | Pijpker PAJ et al. [118] | World Neurosurg | 1 | PSOs for severe congenital kyphoscoliosis in a young girl with skeletal dysplasia | In addition to direct translation of the planned PSO for surgery, the 3D planning also facilitated a detailed preoperative evaluation, greater insight into the case-specific anatomy, and accurate planning of the required correction. |
| 2018 | Li J et al. [43] | J Clin Neurosci | 1 | PVP for fractures of L1 and L3 vertebrae | The perfect fitting between skin and guide template to ensure the puncture stability and accuracy, and increased puncture precision and decreased puncture-related complications, surgical time, and radiation exposure. |
| 2017 | Sugawara T et al. [70] | Spine | 12 | C1LMS-C2PS fixation for atlantoaxial dis-location | The multistep, patient-specific screw guide improves the accuracy of screw insertion and reduces operation time and radiation exposure of posterior C1–C2 fixation surgery. |
| 2017 | Azimifar F et al. [110] | Biomed Eng Online | 12 | Pedicle screws fixation | The proposed template significantly reduced screw misplacements, increased stability, and decreased the sliding and intervention invasiveness. |
| 2017 | Li X et al. [113] | Acta Ortop Bras | 8 | Pedicle screws fixation rigid scoliosis | The placement of pedicle screws shows high accuracy in scoliosis with shorter surgical time, less blood loss, and less radiation exposure. |
| 2017 | Liu K et al. [115] | Eur Spine J | 10 | Pedicle screw fixation for severe and rigid scoliosis (Cobb angle >70° and flexibility <30%) | The incidence of cortex perforation in severe and rigid scoliosis decreased and this technology is, therefore, potentially applicable in clinical practice. |
| 2017 | Zhang Y et al. [121] | Comput Assist Surg | 8 | Intervertebral endoscopy for lumbar disc herniation | This customized navigation board could promote accuracy and diminish the duration of intervertebral disc ablation. |
| 2016 | Deng T et al. [79] | Comput Assist Surg | 10 | Cervical pedicle placement. | This individualized 3D printing screw insertion template was user-friendly, at a moderate cost, and enabled a radiation-free cervical screw insertion. |
| 2016 | Takemoto M et al. [58] | Eur Spine J | 40 | Thoracic pedicle screw fixation for scoliosis and OPLL | This study provides a useful design concept for the development and introduction of patient-specific navigational templates for placing pedicle screws. |
| 2016 | Hu Y et al. [67] | Eur Spine J | 151 | Thoracic pedicle screw fixation for thoracic instrumentation and fusion | The use of template to assist in the placement of mid and upper thoracic pedicle screws may lead to increased accuracy. |
| 2015 | Kaneyama S et al. [55] | Spine | 20 | Midcervical pedicle screws for posterior cervical reconstruction surgery | The templates prevent screwing error along with the change of spinal alignment, guarantee the high accuracy in screw insertion, which allowed surgeons to insert cervical pedicle screws safely. |
| 2015 | Chen H et al. [99] | Med Sci Monit | 43 | Lumbar pedicle screw fixation | 3D printing guide plate can shorten the operation time and reduce the amount of hemorrhage. |
| 2013 | Sugawara T et al. [87] | J Neurosurg Spine | 10 | Thoracic pedicle screw for thoracic or cervicothoracic pathological entities | This simple and economical method can improve the accuracy of pedicle screw insertion and reduce the operating time and radiation exposure of spinal fixation surgery. |
| 2012 | Lu S et al. [111] | Med Biol Eng Comput | 16 | Pedicle screws fixation for scoliosis | The surgical navigation system reduced the perforation rate and insertion angle errors, demonstrating the clear advantage in safe and accurate pedicle screw placement of scoliosis surgery. |
| 2009 | Lu S et al. [72] | Eur Spine J | 9 | C2 laminar screws for basilar invagination | This method has shown its ability to customize the placement and size of each screw, based on the unique morphology of the lumbar vertebra. |
| 2009 | Lu S et al. [74] | Spine | 25 | Transpedicular screw placement for cervical spinal pathology included destabilizing cervical spine injuries, cervical spondylotic myelopathy, and basilar invagination | This method significantly reduces the operation time and radiation exposure for the members of the surgical team. |
S2AI=S2 alar-iliac; PVP = percutaneous vertebroplasty; OVCF = osteoporotic vertebral compression fracture; CBT = cortical bone trajectory; ASD = adjacent segment degeneration; TSS = Transverse sacroiliac screw; IS=Iliosacral screw; AIS = adolescent idiopathic scoliosis; PSOs = pedicle subtraction osteotomies; AS = ankylosing spondylitis; PVP = percutaneous vertebroplasty; C1LMS-C2PS C1 lateral mass screw-C2 pedicle screw; OPLL = ossification of the posterior longitudinal ligament.
4.1.1. Auxiliary screw placement of cervical vertebra
The pedicle screw fixation has become the strongest and most common method of internal fixation in posterior cervical surgery due to its excellent biomechanical properties [8,[65], [66], [67], [68], [69], [70], [71], [72], [73], [74], [75]]. However, it is difficult, inefficient, and risky to place pedicle screws. For the purposes of this study, we usually divide the cervical spine into the atlantoaxial and inferior cervical vertebra (C3–C7).
To solve the issue, Guo et al. [65] designed a navigation template for upper cervical pedicle screw fixation and placed 32 screws on a 3D printing model, with an acceptable rate of 94.60%. Compared to the free-hand screw placement group, the procedure time and frequency of fluoroscopy were reduced, which was beneficial for both the doctor and the patient. Chen et al. [66] modified the conventional 3D printing guide and was more accurate than before. It removed the original guiding channels and replaced them with an inward-moving navigation pole, retaining only the screw holes. In 12 cadavers, 48 screws were placed in cervical specimens, with a good screw placement rate of 97.9%.
In clinical practice, where patients with complex conditions are encountered, the surgical guide also demonstrates a high accuracy rate in screw placement, improving surgical precision and reducing post-operative complications. Compared to the free-hand group, Li et al. [67] have found that the use of templates significantly improves the success rate of pedicle screw placement. 96.7% safety rates were achieved for C1 pedicle screws and even 100% for C2 pedicle screws, showing good promise as an alternative to freehand screw placement in the treatment of odontoid fractures. Pu et al. [68] used a modified 3D printing template with channels on both sides of the guide template as well as a 30 mm long, 3 mm diameter guide pillar. In 17 patients, the modified guide showed a significant improvement in accuracy and safety in atlantoaxial pedicle screw placement, with a success rate of 97.06%.
In addition, some researches have been carried out in other screw placement methods, such as transarticular screw fixation [53], occipitocervical screw [69], C1 lateral mass screw-C2 pedicle screw (C1LMS-C2PS) fixation [70], and C2 translaminar screws (C2TLS) [71,72]. It concluded that a surgical guide could simplify the transarticular screw and C2TLS fixation, improve the accuracy of the screw [71]. In clinical practice, screw misalignment has not been observed. No neural or vascular injuries were observed in each patient [69,72]. Although C1LMS-C2PS fixation has the advantage of reducing the risk of vascular injury and achieving immediate rigid fixation, it is difficult to place screws in this way. Sugawara et al. [70] found template can be precisely fitted and locked to the vertebral template, and screw insertion was successfully completed without cortical invasion of the screw. The mean deviation from the planned trajectory was only 0.70 ± 0.42 mm.
The anatomical variation in the middle and lower cervical spine is large. Without identifiable anatomical landmarks, it is difficult to determine the correct insertion point and angle of insertion, even with fluoroscopic assistance. A number of cadaveric studies were finished to test the influence of guide templates and demonstrated that guides can significantly improve the accuracy of screw placement [11,73]. Through theoretical research, more experience has been gained with the placement of surgical guides, which are also used clinically to assist the surgeon. Lu et al. [74] placed 88 screws through guides in 25 patients with cervical spinal pathology at segments C2–C7. The postoperative placement of screwing guides was proven to be accurate and applicable, reducing the operative time and radiation exposure of the patient. Pijpker et al. [59] found that the point of entry and angular deviation of the 76 screw trajectories were 1.40 ± 0.81 mm and 6.70 ± 3.77°, respectively. A safe level is achieved with no neurovascular injury, facet joint violation, or violation of the pedicle wall.
Whether soft tissue should be considered is still controversial. Through the trial, academics have drawn some lessons on the placement of guides. 1) reduce soft tissue interference with guide placement 2) drill holes of sufficient length, 3) in vitro stimulation to determine trajectory safety 4) guide size not to exceed the spacing of individual vertebrae [13]. However, it has been suggested that attempts can be made to optimize the surface of the guide template by removing soft tissue from the bone surface. Zhang et al. [75] performed a cadaveric study and removed the soft tissue from the bone surface. A total of 158 screws were placed with 98.1% accuracy. On this basis, Peng et al. [76] developed a template for guiding cortical bone trajectory screws. It successfully improved the success rate of screw placement and reduced intraoperative complications. Kaneyama et al. [77] provided the guides for 20 consecutive patients. It was fit directly to the target vertebral template and prevented screw deviation from the expected trajectory even spinal alignment changed during the procedure.
Furthermore, some scholars have also conducted studies on the whole cervical spine [[78], [79], [80]]. They selected the ideal screw access according to a different segment. The navigation templates improved the accuracy and safety for patients with cervical spine fixation. Almost all screws were placed into the vertebral body without cortical invasion. There was no intraoperative vascular or neurological injury.
In summary, 3D printing guides for cervical screw placements are still at the stage of vitro research. Clinical experience exists but there is a lack of randomized controlled long-term observation trials. This may be due to the high requirements of the cervical template for the pedicle entry point, the general instability of the template placement, and the interference of the soft tissues. In addition, a resorbable surgical guide has recently been investigated [81]. The use of bioresorbable guides effectively eliminates the need for template removal after spinal fusion and does not present difficulties in imaging like metal implants. However, the question of whether bioresorbable templates provide sufficient stability for fusion is debatable and is still under investigation and deserves the attention of doctors.
4.1.2. Auxiliary screw placement of thoracic vertebra
The freehand screw placement remains the most dominant for thoracic pedicle screw placement. However, the size of the thoracic vertebra pedicle makes pedicle screw internal fixation difficult and risky. 3D printing templates are now an ideal solution to address these technical challenges [82].
Ma et al. [83] inserted a total of 240 thoracic screws in 20 thoracic cadaveric specimens. The navigational template showed a higher accuracy rate of about 93.4% and a lower incidence of risk than the free-hand method. To effectively assess the effectiveness in the human thoracic spine, Chen et al. [84] applied a surgical guide in the placement of 50 screws in 25 human cadaveric thoracic vertebrae. The high precision of the screw placement and the short operation time deserve promoting clinical trial. In minimally invasive surgery, Li et al. [44] further improved the 3D printing guide. They successfully placed 96 pedicle screws bilaterally in the T6-L1 segment of six adult cadavers, with a 98.6% accuracy rate on CT results. The guide template was not loosened or displaced when operated by a single hand. It shorted the learning curve of the guide template placement and made it worthy of more clinical trials.
Applying guide templates in CBT screws have been attempted in the thoracic spine [58,85]. It was an ideal screw placement for osteoporotic or other diseases that may lead to screw loosening. Further studies in vivo are anticipated. The concept of determining optimal screw trajectory was first proposed by Chen et al. [86]. For each vertebra, there can only be one optimal screw placement trajectory. They designed a 3D printing guide to assist in the placement of 358 thoracic pedicle screws in order to find the optimal trajectory through the central axis of the pedicle. Compared to the design trajectory, 98.6% of the screw entry points were accurate and 98.9% of the screw exit points were accurate.
Physicians have gradually built up confidence in applying guides to complete the surgery, gaining experience in the use of guides for the thoracic spine. Hu et al. [87] placed a total of 582 pedicle screws into the mid and upper thoracic spine in 151 patients. 559 of the 582 screws (96.1%) were located completely within the thoracic pedicle, demonstrating good placement accuracy. Furthermore, Sugawara et al. [88] describe a new fit-and-lock template and multistep screw insertion technique for more accurate screw placement. None of the screws were found to violate the cortex of the pedicles of the vertebra models. For the accurate guidance of the PS insertion, Sugawara et al. [46] produced three templates that could cover the 3D shape of the laminae and developed a unique multistep procedure. Postoperative CT scans confirmed that 801 screws (98.5%) into the cervical and thoracic spine were accurately placed without cortical violation. There were no injuries to the vessels or nerves. Naddeo et al. [89] proposed an innovative design disengaging of 3D printing guides. It accelerated standard surgical procedures, reducing operative time and achieving excellent results in terms of screw positioning accuracy and X-ray exposure time.
4.1.3. Auxiliary screw placement of lumbosacral vertebra
In animal and cadaveric trials, all surgeons gave positive feedback on the 3D printing surgical guide template, such as the ease of handling, the improved accuracy of screw placement, and the significant reduction in radiation exposure [9,[90], [91], [92], [93]]. Furthermore, they tested the feasibility of 3D printing surgical guides for minimally invasive lumbar pedicle screw placement. It demonstrated that the guides can significantly improve the accuracy of screw placement, reduce excessive radiation exposure [94,95]. Zhao et al. [96] simultaneously placed traditional pedicle trajectory (TPT) and CBT screws in cadavers, with 82.5% of the screws located entirely in the cortical bone. It was a safe and accurate method of pedicle screw placement. This template showed a potential option for clinical applications.
The first clinical study of surgical guides for posterior lumbar cortical bone trajectory screws was performed by Marengo et al. [97]. Subsequently, an increasing number of authors have reported the use of guides in lumbar screw placement [[98], [99], [100]]. It offers a similar effect in the cadaveric study. At the follow-up, patients showed a reduction in pain and claudication. Petrone et al. [101] evaluated 238 patients undergoing CBT fusion for degenerative lumbosacral disease. Through comparison, the use of surgical guides reduced operative time, radiation exposure, and complication, providing a higher screw placement success rate of 93.9% than other modalities of screw placement. More clinical studies about the long-term outcomes and accuracy are needed to directly compare the placement of traditional pedicle screws with CBT screws. Matsukawa et al. [102]evaluate the clinical accuracy of long CBT screw placement using a patient-specific template guide. A total of 193 screws (97.5%) were placed completely inside the pedicle and there was no incidence of neurovascular injuries. In recent years, a novel 3D printing guide template-assisted transpedicular transdiscal (TPTD) lumbar screw fixation has been designed and validated on a 3D printing spine model [103].
Sacral fractures are a common clinical disease. In the placement of S2 Alar-Iliac (S2AI) screws, many surgeons used a 3D printing surgical guide [10,104]. Compared to the freehand screw placement group, it showed a higher accuracy rate with the use of a guide template. In the placement of transverse sacroiliac screw (TSS), Wu et al. [105] used a guide to assist placement in 22 patients with sacral fractures. The use of the guides significantly reduced the patient's operative time and radiation exposure [106].
More importantly, Eltes et al. [107] proposed a 3D printing guide based on patient-specific biomechanical characteristics, which is cheaper and reduces intraoperative X-ray exposure. Such a guide could be used in revision spine surgery or in more challenging cases after further clinical validation. However, it is also important to consider that separate design of the navigation template requires software support, a complex guide design process, and a long learning curve to operate the software.
4.1.4. Spinal deformities
Currently, the pedicle screw has been the major surgical method for the correction of spinal deformities. Because the screws can pass through the anterior, middle, and posterior columns of the spine, pedicle screws are used for better correction and stabilization instead of other fixation devices [5]. However, variations in spinal deformities which are complicated with arch root deficiency, rotation and compression of the vertebral body, joint and disc hyperplasia, fusion, and ossification of the attached ligaments, resulted in difficult identification of traditional bony marks and insertion angles [108]. The use of conventional imaging data, such as X-rays, makes it difficult for the surgeon to obtain visual and accurate 3D anatomical information, resulting in a high failure rate of screw placement. In addition, because of the great variability between patients with different spinal deformities, patients often have secondary structural variations in the lung, spinal cord, great vessels, and nerve roots [109].
3D printing guides abandon the previously anatomical positioning of the vertebral body, overcome alterations in spatial vertebral structure, and eliminate the need for expensive equipment [58,108,110,111]. Liang et al. [112] compared 1384 pedicle screws placed by templates with 1392 pedicle screws placed by freehand, the accuracy of templates assisted placement was significantly higher than that of the freehand. The operation time and blood loss were all significantly reduced in the 3D printing template group. Li et al. [113] retrospectively analyzed sixteen patients and found that the position of the pedicle screws was more accurate if using the template. Cecchinato et al. [109] observed that the screw placement accuracy was significantly higher in the guide group at 96.1% than in the freehand group at 82.9%, with a spinal correction rate of 60%, demonstrating the feasibility of replacing the traditional freehand screw placement technique.
Particularly in the correction of severe (Cobb angle >70°) and rigid (flexibility <30%) scoliosis is still pretty high risk [112]. Luo et al. [114] designed a surgical guide for patients with severe scoliosis and used it to assist in the placement of pedicle screws in 15 patients. 244 pedicle screws were placed and the success rate of the assisted placement was 96%, shortening the operative time. Though there were limited clinical reports about the application of multi-level drill guide templates in scoliosis. Liu et al. [115] applied a multi-level template in 48 pedicle screws in severe and rigid scoliosis. 93.8% of the pedicle screws were accurately placed by template, and all screws were implanted one time without adjustment. This study demonstrates that the use of guides significantly reduces the incidence of cortical perforation in severe and rigid scoliosis and that this technique has clinical potential.
Congenital scoliosis is one of the more difficult problems in spinal deformity correction surgery. Drawbacks of these techniques consist of high radiation exposure to the young child, increased operative time, potential blood loss, and high cost. For adolescents who are still in the process of development, Senkoylu et al. [116] designed a 3D pedicle screw guide and achieved positioning accuracy in 92.5% of the screws with a total of 134 screws. Tu et al. [117] used 3D printing guides to assist screw placement in 24 patients with scoliosis, with an overall accuracy rate of 95.56% significantly higher than the 82.76% achieved in the conventional treatment group.
4.1.5. Spinal osteotomy
It is essential to plan and design the extent of the osteotomy accurately before surgery. Due to the complexity of spinal deformities, spinal osteotomy has been widely used in the orthopedic treatment of spinal deformities with good clinical results. But if the osteotomy is too large, the adjacent spinal nerves and blood vessels may be damaged, making it difficult to maintain spinal stability, while if the osteotomy is too small, it will not be effective in improving the appearance of the deformity, achieving adequate decompression and achieving spinal balance. Therefore, 3D printing spinal osteotomy guides based on individual patient design can provide precise guidance for osteotomy procedures, freeing spinal osteotomy from the constraints of experience to the digital stage and simplifying the procedure.
During the design of the guide template, factors such as the sagittal and coronal balance of the spine, the relaxation of the spinal nerves, the cardiopulmonary status, and the compliance of the prevertebral vessels should be taken into account, as well as the degree of muscle pull, so that the appropriate osteotomy area can be determined. Pijpker et al. [118] used 3D printing patient-specific osteotomy templates to guide the pedicle subtraction osteotomies. It is the first report describing this technique for complex spinal osteotomies. The patient was discharged without any neurological deficit after 8 days. Early postoperative radiographs showed good correction of the posterior convexity deformity with a reduction in the posterior convexity angle from 74° to 22° and normalization of the coronal plane. Tu et al. [119] report a new method to perform complicated asymmetric wedge pedicle subtraction osteotomy in patients with severe thoracolumbar kyphoscoliosis secondary to AS. Postoperative X-rays showed a mean correction of 65.9° at the osteotomy site. At the last follow-up, a CT scan showed bone fusion at the osteotomy site without screw loosening in all 9 patients.
4.1.6. Others
In recent years, there have been attempts to use a 3D printing guide applying puncture technology in Percutaneous vertebroplasty (PVP) [43,120] and intervertebral endoscopy surgery [121]. Through preoperative simulation in the software, we could establish optimal skin entry points, needle trajectories, insertion depths, and make the best puncture plan, reducing the operation duration of intervertebral disc ablation. Following the accurate puncture pathway, the incidence of cement leakage could be reduced. Although in theory, the guides are able to achieve accurate screw placement, the problem of accurate matching and the lack of a stable apposition surface due to soft tissue slippage of 3D printing guides remains to be solved. Because of the limitations of printing materials, we need to solve the problem of templates deformation after low-temperature steam disinfection.
4.2. Trauma
Due to the complexity and diversity of fracture types, traumatic surgery has a wide range of treatment options, resulting in widely varying outcomes. Some complex comminuted fractures require solid anatomical knowledge and extensive surgical experience, but even then it is difficult to achieve good alignment and precise fixation, often resulting in unsatisfactory fracture repositioning and misaligned template and screw fixation [122]. In addition, some patients with fracture malunion often suffer from varying degrees of pain or dysfunction, which seriously affects their quality of life [25]. It requires osteotomy surgery to alter the force lines of the limb in order to correct the deformity, ensure joint stability, and relieve pain. The osteotomy methods are divided into angular, rotational, and translational osteotomies. The selection of osteotomy area is based on the principles of facilitating osteotomy fixation, promoting fracture healing, and not interfering with joint function. Over the past decade, orthopedic surgeons have increasingly used 3D printing technology to create intraoperative aids including cutting guides, guidewires, and guides for screws. As shown in Table 4, this allows surgeons to perform complex fracture fixation and discontinuous reconstruction.
Table 4.
The main clinical application of traumatic surgeries.
| Year | Authors | Journal | Case number | Type of surgery | Results |
|---|---|---|---|---|---|
| 2021 | Casari FA et al. [139] | Arch Orthop Trauma Surg | 7 | A drill template for distal intraarticular radius fracture | The template navigated intraarticular radius fracture treatment is feasible, safe, and accurate. |
| 2021 | Duan D et al. [124] | Pain Res Manag | 1 | Opening wedge high tibial osteotomy | Patient-specific plates have the advantages of small trauma, few complications, simple operation, and fast recovery in treating knee osteoarthritis. |
| 2020 | Dong XP et al. [125] | Asian J Surg | 1 | Bone grafting and screws for tibial plateau fracture (Schatzker type V) | 3D printing assisted percutaneous guide plate in the reduction and internal fixation of tibial plateau fracture is safe and effective. |
| 2020 | Sun L et al. [126] | Injury | 54 | Indirect reduction and internal fixation with the minimally invasive percutaneous plate osteosynthesis (MIPPO) | MIPPO assisted by 3D printing navigation templates could practically improve surgical accuracy and eliminate postoperative rotational deformity in patients with distal femoral fractures. |
| 2020 | Zhang YW et al. [129] | Asian J Surg | 1 | A cutting guide for transverse tibial bone transport | The operations of TTBT guided by 3D printing guide plates can effectively protect the relative integrity of bone window and periosteum. |
| 2020 | Hu X et al. [134] | J Orthop Surg Res | 35 | A cutting guide for cubitus varus deformity | Individualized navigation templates simplify procedures, reduce operation time, and improve accuracy. |
| 2019 | Nie W et al. [123] | Injury | 11 | Screw fixation for bicondylar tibial plateau fractures | It provides a comprehensive understanding of fracture features, accurate patient-specific preoperative planning, and intraoperative guidance for real surgeries |
| 2019 | Oka K et al. [135] | J Orthop Sci | 1 | A cutting guide for cubitus varus deformity | The limb's appearance considerably improved and the range of elbow motion reverted to what it had been before surgery. |
| 2019 | Chen K et al. [143] | Biomed Res Int | 28 | “Blunt end” Kirschner wire (KW) insertion for unstable pelvic fractures | The “blunt end” KW technique with a 3D printed external template is a safe and effective method. |
| 2018 | Chen Y et al. [132] | J Bone Joint Surg Am | 131 | Plate and screw fixation for fractures of the proximal end of the humerus | The clinical outcomes in both the virtual surgical and 3D printing groups were better than those in the conventional group. |
| 2017 | Bauer AS et al. [149] | J Pediatr Orthop | 19 | A cutting and drill guide for deformity of the forearm | 3-dimensional computer modeling permits complex and multiple osteotomies to be done safely to achieve deformity correction in children. |
| 2015 | Huang H et al. [51] | Australas Phys Eng Sci Med | 6 | Plate and screw fixation for Schatzker classification V or VI tibial plateau fracture | This technology improves the accuracy and efficiency of personalized internal fixation surgery. |
| 2015 | Omori S et al. [136] | J Shoulder Elbow Surg | 17 | A cutting guide for cubitus varus deformity | The 3D correction of cubitus varus deformity was performed accurately within the allowable error limits. |
Kirschner wire = KW
Traumatic cases are mainly classified as the pelvis, lower limbs requiring weight-bearing, non-weight bearing humerus and ulna, radius, and navicular bone of the hand [23].
4.2.1. Femur and tibia
With regard to the lower limbs, almost all clinical measurements of the femur and tibia show inadequate postoperative correction [25]. In particular, the degree of correction of the tibial plateau osteotomy in the coronal and sagittal planes differs considerably from the preoperative plan. The basic requirement for the treatment of tibial plateau fracture is to restore the force line of the limb and the flatness of the joint surface. To evaluate the accuracy of personalized preoperative planning of plate and screw for the complex tibial plateau fracture surgery, Huang et al. [51] used 3D printing surgical guides to identify 33 screw entries and place six locking compression plates in six patients with tibial plateau fractures. Postoperative X-rays showed no significant differences in parameters such as screw length, entry point, and screw orientation from the preoperative plan, with well-matched plates and good application results. Other surgeons applied templates in patients with bicondylar tibial plateau fractures or wedge high tibial osteotomy [123,124]. The postoperative screw fixation and osteotomy was accurate and no perioperative complications such as infection, deep vein thrombosis (DVT), or neurovascular injury occurred within follow-up.
Minimally invasive surgery can reduce patient trauma, muscle scar formation, and recovery time, but the procedure is more difficult. Dong et al. [125] reported a case of percutaneous guide in minimally invasive internal fixation of a tibial plateau fracture. Postoperative imaging showed precise fracture repositioning, flat articular surface, and satisfactory screw fixation, which can be a clinical option to achieve minimally invasive treatment of tibial plateau fractures. Sun et al. [126] reviewed a total of 54 patients who underwent minimally invasive percutaneous plate osteotomy (MIPPO) of distal femur fractures. The template-guided MIPPO group was found to have greater surgical accuracy, with less variation in femoral length, anatomical lateral distal femoral angle (aLDFA), anatomical posterior distal femoral angle (aPDFA), and anteversion angle, with neater alignment and more significant advantages. In addition, the assistance of the guide can reduce the gap between novice and experienced surgeons [127].
Tibial plateau malunion (TPM) can be restored to the anatomical position of the knee surface using intra-articular corrective osteotomy, but precise restoration is not easy. Hsu et al. [128] used 3D printing surgical guides to provide precise positioning of the osteotomy and improve TMP outcomes, which is a viable alternative to conventional surgery. Zhang et al. [129] designed a guide to assist in transverse tibial bone transport (TTBT) surgery in order to promote the impact of vascular regeneration in treating patients with diabetic feet. The guide effectively protects the relative integrity of the bone window and periosteum.
However, these surgical guide templates also have their limitations. The precise positioning of the surgical guide is achieved by adequate exposure around the bone, blood flow to the periosteum may be compromised. The lack of soft tissue may lead to postoperative wound complications (e.g. infection). Furthermore, the use of a surgical guide is limited to certain anatomical boundaries to remove periosteal soft tissue [130].
4.2.2. Humerus
In humeral disease, the surgical guide is mainly used to assist in the correction of cubitus varus deformity. The key to osteotomy is the determination of the osteotomy region, the osteotomy angle, and the length of the bottom edge. Traditional osteotomy angles are based on radiographic measurements and have unsatisfactory osteotomy accuracy. 3D printing osteotomy guides can be used to greatly improve osteotomy accuracy, reduce postoperative complications and reduce operating room costs [131]. But compared with computer-assisted virtual surgical technology in fractures of the humerus, the templates exist controversial [132].
Easter et al. [133] applied the guide template in the dog elbow and found that it allowed accurate placement in the humeral condyle. In children with cubitus varus deformity, the osteotomy guide was fitted to the osteotomy area and guided Kirschner wires fixation [134]. Oka et al. [135] reported a child with cubitus varus deformity after healing of an elbow fracture. Twenty months after osteotomy surgery, the limb's appearance considerably improved and the range of elbow motion reverted to what it had been before surgery. Omori et al. [136] performed corrective osteotomy with 17 patients with cubitus varus deformity after a supracondylar fracture. The motion range of the elbow joint returned to normal after correction, offering a new solution for future patients with improved elbow deformity.
4.2.3. Radius and ulna
The forearm osteotomy can be divided into radial stem osteotomy, combined distal radius and ulnar osteotomy, or only a single osteotomy of the ulna or radius [28]. 3D printing templates can be used to correct deformities of the radial and ulnar trunks with limited rotation of the forearm. This has been used in adult and pediatric patients with congenital or post-traumatic deformities. In a study by Bauer et al. [49], 19 consecutive children who underwent forearm osteotomy were applied 3D printing surgical guides and found that all patients had excellent postoperative bone healing with no fixation through the epiphysis. The magnitude of the deformity was significantly reduced and there were no postoperative complications. For the correction of distal radius fracture deformity healing, we used surgical guides to assist in osteotomy and screw placement. The advantages of designing a 3D printing surgical guide for deformity correction based on the contralateral, uninjured distal radius are clear, but further study is needed to determine whether these aids affect functional outcomes, deformity correction, and complication rates and whether they are cost-effective.
Corrective osteotomy for distal radius fracture deformity healing is challenging to pass. On cadaver research, a novel minimally invasive osteotomy method achieves comparable accuracy to open surgery [137]. Honigmann et al. [138] used a guide template to guide the placement of screw and osteotomy of the distal radius, achieving rapid and reliable accurate anatomical. Casari et al. [139] used guides to treat intra-articular fractures of the radius. At 16 months follow-up, the patient recovered all ranges of motion and showed significant recovery in flexion, extension, and rotation.
4.2.4. Scaphoid
In scaphoid fractures with no or little displacement, 3D printing guides allow simple and accurate placement of the central guidewire for percutaneous scaphoid fixation [140]. It has been demonstrated on multiple cadaveric models that the use of 3D printing guides assisted in screw placement can reduce linear and angular deviations from the planned positions, shorten operative times, and reduce the need for fluoroscopy [141]. Wan et al. [142] conducted a cadaveric study and a preliminary clinical study about minimally invasive percutaneous internal screw fixation. The intraoperative guides fitted well to the skin surface and the guide wires and screws were accurately fitted in a single session. There was a clinically significant reduction in operative time and X-ray exposure time, with good functional recovery of the hand postoperatively.
4.2.5. Pelvis
The recent development of pelvic screw technology has reduced the trauma of traditional surgery while providing better biomechanical properties [143]. However, pelvic screw placement requires a precise trajectory and the experienced operator in this field, as well as repeated intraoperative fluoroscopy from multiple angles to determine the anatomical relationships. Chen et al. [144] placed 64 plates and 339 screws on the cadaver without cortical rupture. The guide template was attached to the bone surface in the appropriate pre-determined area during the procedure.
4.2.6. Others
In addition to the commonly used screw and osteotomy guides, there are also pelvic fracture and prosthesis placement guides. Some scholars have made use of 3D repositioning of pelvic fractures, 3D printing of the repositioned fracture form, pre-curved plates, and design for the intraoperative application. This reliance on 3D models of pre-curved plates to guide fracture repositioning provides a meaningful attempt to apply guide template technology to fracture repositioning [24,145]. Many other scholars have also made attempts to use adjunctive guides for different surgical procedures, such as personalized guided orthopedic guides and personalized bone defect repair guides [146], in order to allow more efficient and accurate solutions to difficult surgical problems [31,147].
4.3. Joint
In joint surgery, the restoration of force lines and soft-tissue balance in the affected limb after arthroplasty is an important factor in assessing the success of the operation. The accuracy of the intraoperative osteotomy is decisive. Statistics have shown that more than half of all primary arthroplasty and second-stage revision failures are due to inadequate intraoperative osteotomies [148,149].
The 3D printing osteotomy guide is a digital method to process the image data according to the prosthesis type and patient's osteotomy plane [150], which significantly reduces the difficulty of intraoperative osteotomy operations [151] and shortens the operation time [29]. As summarized in Table 5, the use of surgical guides has shown to be clinically important in terms of improving surgical outcomes, limb force line accuracy, soft tissue balance adjustment, and post-operative joint mobility [37,152]. In addition, the use of surgical guides reduces the variety of surgical instruments, thereby reducing set-up and handling time and sterilization costs. The reduced operative time may help to reduce infection rates and the lack of an intramedullary assist device also reduces the risk of fat embolism [153]. Surgical guides are used in the treatment of joint-related diseases including fractures, replacement of the shoulder, total hip, knee, ankle, and periacetabular osteotomies.
Table 5.
The main clinical application of joint surgeries.
| Year | Authors | Journal | Case number | Type of surgery | Results |
|---|---|---|---|---|---|
| 2020 | Shi Q et al. [155] | J Orthop Surg Res | 29 | Proximal femoral corrective osteotomy for DDH | The template is effective and safe, which could improve the femoral osteotomy accuracy, reduce radiation exposure, and shorten the operation time. |
| 2020 | Yan L et al. [162] | Indian J Orthop | 25 | Acetabular cup placement for DDH | 3D printing template for THA with DDH can facilitate the surgical procedure and create an ideal artificial acetabulum placement. |
| 2020 | Tu Q et al. [163] | Hip Int | 12 | Femoral osteotomy guiding template for DDH | It provided a new personalized surgical plan for the precise positioning and orientation of acetabular reconstruction and femoral osteotomy. |
| 2020 | Gu F et al. [169] | Biomed Res Int | 22 | Customized guiding template for UKA | The 3D-printed template decreased operation time, decreased blood loss, and improved short-term clinical outcomes in patients undergoing UKA surgery. |
| 2020 | Faldini C et al. [172] | J Orthop Traumatol | 1 | A cutting guide for total ankle arthroplasty | The complete customization process for total ankle arthroplasty provided accurate and reliable implant positioning, with satisfactory short-term clinical outcomes. |
| 2020 | Liu D et al. [174] | Ann Transl Med | 43 | A drill template for ACL rupture | The 3D-printed template showed good location accuracy and reduced intraoperative positioning time compared to the traditional method for ACL reconstruction. |
| 2020 | Wu Q et al. [175] | Med Sci Monit | 34 | A drill template for CLAI | Both the template technique and the conventional method provided satisfactory outcomes for CLAI patients. |
| 2019 | Wang X et al. [158] | J Orthop Surg Res | 20 | A novel customized cutting and rotating template for Bernese PAO | It is feasible and could realize the predicted results accurately during the actual PAO. |
| 2019 | Gemalmaz HC et al. [167] | Acta Orthop Traumatol Turc | 20 | Cutting blocks for total knee arthroplasty | The template may improve TKR alignment by improving the ratio of the outlier patients with marked malalignment. |
| 2018 | Schneider AK et al. [159] | Hip Int | 30 | Femoral neck osteotomies | The osteotomy guides provide an accurate method of performing femoral neck osteotomies in minimally invasive hip arthroplasty. |
| 2017 | Zheng P et al. [160] | Int J Comput Assist Radiol Surg | 11 | LCP-PHP for femoral neck fracture and DDH | This technology can reduce intraoperative damage to the femoral neck epiphysis, decrease operation time, reduce intraoperative hemorrhage, and decrease radiation exposure to patients and personnel during the surgery. |
| 2017 | Zheng P et al. [156] | Sci Rep | 12 | Proximal femoral varus rotation and shortening osteotomy template for DDH | Application of the template can reduce the operation time, radiation exposure, and epiphysis damage, which also simplifies surgery and improves precision. |
| 2016 | Gauci MO et al. [154] | Bone Joint J | 17 | PSGs for TSA | The use of PSGs provides accurate and reproducible positioning and orientation of the glenoid component in anatomical TSA. |
| 2016 | Köster G et al. [168] | Orthopade | 88 | Pin placement and cutting guides for uni- and bicompartmental knee replacement | The template using the applied technique proved to be practicable and reliable. Soft tissue balancing has only been included in the technique to a limited degree so far. |
| 2013 | Du H et al. [165] | Int Orthop | 16 | Valgus-oriented prosthesis for total hip resurfacing arthroplasty | It can provide the precise and dependable location for hip resurfacing femoral components and ensure the valgus stem placement necessary for optimal outcomes. |
DDH = developmental dysplasia of the hip; UKA = unicompartmental knee arthroplasty; ACL = anterior cruciate ligament; CLAI = chronic lateral ankle instability; PAO = periacetabular osteotomy; LCP-PHP = locking compression pediatric hip plate; PSGs = Patient-specific glenoid guides; TSA = total shoulder arthroplasty.
4.3.1. Shoulder
Appropriate positioning of the glenoid component in total shoulder arthroplasty (TSA) is crucial to avoid early loosening. In 17 patients undergoing total shoulder arthroplasty (TSA), Gauci et al. [154] used CT data of the shoulder to create surgical guides in TSA, and the mean error of the articular glenoid component compared with the planned preoperative position was 0.9 mm, reducing the difficulty of the surgical operation.
4.3.2. Hip
Developmental dysplasia of the hip (DDH) is the incomplete coverage of the acetabulum to the femoral head and it is the main cause of osteoarthritis (OA) of the hip. In hip preservation surgery, periacetabular osteotomy (PAO) and proximal femur osteotomy can effective relieve pain and improve joint function. 3D printing guides making it an effective and safe to improve the accuracy of femoral osteotomy, reduce radiation exposure and shorten the operative time [155,156]. In cadaver's research, the templates greatly facilitated intraoperative rotation and fixation of the osteotomized segment and allowed accurate final placement of the acetabulum based on pre-planned data [157]. Wang et al. [158] designed a customized cutting template and applied it in the actual periacetabular osteotomy (PAO) of all 20 patients. It could not only shorten the duration of the operation but also reduce the number of irradiations used, which benefits both the surgeon and the patient. Schneider et al. [159] used templates for patients undergoing minimally invasive hip arthroplasty and found that most osteotomies could be accurate to within 3 mm deviation. The Locking compression pediatric hip plate (LCP-PHP) surgical guide was innovatively proposed by Zheng et al. [160] to reduce intraoperative damage to the femoral neck epiphysis and increase the accuracy of screw placement. It significantly reduces operative time, intraoperative bleeding, and patient exposure to radiation during surgery.
Total hip arthroplasty is recognized as an effective surgical method for the treatment of end-stage hip disease. The cadaveric study demonstrated that the template improved the accuracy of cup placement and provided a theoretical basis for clinical practice [161]. Yan et al. [162] conducted a study of 25 patients who underwent total hip. The 12 patients who used 3D printing guides had better operative time, intraoperative and postoperative bleeding, and Harris Hip Score (HHS) scores at 6 months postoperatively, with no incidence of infection or joint loosening, which accelerated the patients' recovery and quality of life. Tu et al. [163] evaluated 12 patients with 3D-printing individualized guiding templates in total hip arthroplasty (THA) for the treatment of DDH. The 3D printing personalized guidance template met the surgeon's specific requirements for the treatment of Crowe IV DDH, and the patient recovered well after surgery with no loosening of the hip joint, providing a new personalized surgical plan for the precise positioning and orientation of acetabular reconstruction and femoral osteotomy.
The distinct advantages of total hip resurfacing arthroplasty (THRA) over conventional total hip replacement include preservation of the proximal femur bone, increased range of motion, and reduced dislocation rates. However, the procedure is technically demanding and has a high probability of postoperative complications. Liang et al. [164] used a guide to assist the surgeon in placing acetabular and femoral stem prostheses in 17 cadavers. The postoperative assessment showed that the Kirschner wires accurately passed through the center of the femoral head and femoral neck and the femoral prosthesis orientation was able to achieve reasonable valgus. In clinical practice, Du et al. [165] used 3D printing templates in 16 patients with hip resurfacing arthroplasty. The benefits of this method include accurate placement of the component, decreasing operative time, easy intraoperative handling, reduced instrumentation, and a relatively decreased learning curve for beginners, which has been a factor in the rate of a femoral neck fracture.
4.3.3. Knee
In 2006, it was the first time to use knee CT data creating individualized osteotomy templates for use in total knee arthroplasty (TKA) by Hafez et al. [166]. It showed that the templates were simple to manipulate, less invasive, and time-saving compared to previous approaches. In clinical practice, Gemalmaz et al. [167] used 3D printing guides to assist in osteotomies and postoperatively found that the guides provided better osteotomy accuracy and better mechanical alignment compared to conventional TKA for abnormal cases with more than 3° of malalignment. Köster et al. [168] operated on 87 patients requiring knee arthroplasty with conventional and 3D printing surgical guides and found that the use of 3D printing guides allowed for better osteotomy and soft tissue balance, and X-rays showed better joint alignment in patients using 3D printing guides.
Routine radiography analysis CT, and MRI images of the knee joint is difficult to accurately obtain the 3D structure of the lower extremities, and it is also difficult to quantitatively show the cartilage wear of the medial compartment. Gu et al. [169] designed a 3D printing guide for patients undergoing unicompartmental knee arthroplasty with reference to both MRI data and CT data. Postoperatively, it was found that the guide template helped to shorten the operative time, reduce blood loss and improve short-term clinical prognosis in patients undergoing unicompartmental knee arthroplasty. When performing patellar resurfacing in knee arthroplasty, it can be difficult to accurately and symmetrically resect irregular patellae. Huang et al. [170] develop a customized template design for patellar resurfacing. The customized cutting template provided a symmetric resection with ML and SI angles of 1.21° and 1.95°, respectively, in the patellar models, and 0.62° and 2.03°, respectively, in cadaveric specimens.
Compared to semi-automated robot-assisted knee replacements, Jaffry et al. [171] found that the clinical correction results for unicompartmental knee arthroplasty (UKA) using 3D printing guides were essentially the same, but took half the time of the robot using 3D printing personalized guides. With further development, 3D printing personalized guides may even surpass the accuracy of robots and complete planned procedures in less time.
4.3.4. Ankle
Compared to hip and knee arthroplasty, the outcome of ankle arthroplasty is always less satisfactory. Faldini et al. [172] reported on a 57-year-old patient who underwent total ankle arthroplasty and used a 3D printing osteotomy guide to assist in the osteotomy. Postoperative X-rays showed good prosthesis positioning. After 4 months, the patient recovered well from motor function, with normal function, ankle joint torque, and muscle activation time normalized, establishing the feasibility of 3D printing guides for use in ankle arthroplasty.
4.3.5. Others
In addition, the use of guides in ligament reconstruction has also been described. The location of the ACL on the femur exhibits great variability and it is not easy to accurately determine the anatomical insertion point of the ACL during reconstruction [173]. Liu et al. [174] used 3D printing personalized navigation templates to assist in anterior cruciate ligament (ACL) reconstruction and found that the 3D printing guides were more accurately positioned compared to the conventional procedure, with no difference to the preoperatively designed bone access location and reduced intraoperative Positioning time was reduced. In patients with chronic lateral ankle instability (CLAI), Wu et al. [175] used 3D printing guides to assist with lateral ankle ligament reconstruction and found that the accurate bone access created using the guides significantly reduced the duration of surgery and radiation exposure, suggesting that it is a better option for the treatment of CLAI.
4.4. Bone tumors
Although tumors such as bone metastases, osteosarcomas, benign and malignant bone tumors are less common, accounting for less than 1% of all newly diagnosed cancers, their 5-year survival rate is only 50%, presenting greater challenges [176]. In recent years, with the development of neoadjuvant chemotherapy, limb salvage surgery has become the preferred surgical method for most patients. Most of the bone tumors are irregular in shape and the preoperative image positioning is fuzzy, so the surgeon can only perform tumor resection under the naked eye. Accurate resection of tumor tissue has always been a challenge for orthopedic oncologists. The selection of surgical plan, the repair of bone defect after resection of large tumor tissue and functional reconstruction are also the difficulties of limb salvage surgery. 3D printing technology was used to design surgical guide rails, and rapid prototyping technology was used to make solid guide rails for intraoperative guidance to achieve accurate tumor resection, bringing a new vision for bone tumor resection. Table 6 shows the main clinical applications and outcomes of different types of surgery for bone tumors.
Table 6.
The main clinical application of bone tumors surgeries.
| Year | Authors | Journal | Case number | Type of surgery | Results |
|---|---|---|---|---|---|
| 2021 | Wong KC et al. [45] | Journal of orthopaedic translation | 3 | Using both Computer Navigation and Patient-Specific Guide for bone sarcoma patients who underwent joint-preserving bone tumor resections and reconstruction | The mean maximum deviation errors of the nine achieved bone resections were 1.64 ± 0.35 mm. The histological examination of the tumor specimens showed negative resection margin. |
| 2019 | Evrard R et al. [182] | Orthop Traumatol Surg Res | 9 | A cutting guide for limb salvage surgery for pelvic bone sarcoma | The improved resection accuracy directly influences the risk of local recurrence. It is effective in improving resection accuracy. |
| 2019 | Liu X et al. [183] | J Arthroplasty | 38 | Customized Cutting Blocks for pelvic reconstruction after pelvic tumor resection | It can increase surgical safety and reduce recurrence after tumor resection. The innovative therapy reconstructs the pelvis of zone III to improve the quality of patient life. |
| 2016 | Lin CL et al. [179] | Eur Spine J | 1 | A cutting guide for giant invasive sacral schwannoma | This technology can be applied to complex surgical procedures easily and reliably. |
| 2016 | Ma L et al. [178] | Sci Rep | 8 | A cutting guide for osteosarcoma resection | The templates were leading to more precise resection of the tumorous bone and the implantation of the bone implants, less blood loss, shorter operation time, and reduced radiation exposure during the operation. |
In bone tumor surgery, reducing operative time while making more precise osteotomy and shaping the graft or prosthesis at the defect site may improve the prognosis of patients with tumors [177]. Ma et al. [178] used 3D printing guides to assist in osteosarcoma resection surgery in a total of eight patients from 2011 to 2013. The implant is stable and able to hold enough weight to allow the patient to eventually return to normal physical activity with less intraoperative bleeding, shorter surgery time, and reduced radiation exposure. Post-operative X-ray scans showed that using the individual templates resulted in the surgery with a high degree of precision. In 2016, Lin et al. [179] reported a case of resection of giant invasive sacral schwannoma using a 3D printing osteotomy tool. With this novel customized osteotomy guiding block, combined with the intraoperative frozen section, we get a more accurate intraoperative localization of the resection margin of the tumor. Postoperatively, clinical symptoms improved significantly with the nerve and dura being preserved. When the resection is geometric with multiple osteotomy planes, the current 3D printing surgical guides may be superior to the computer navigation in bone tumor resections. With the combined techniques in complex joint-preserving bone tumor resection, more conservative bone resections that preserve native joints and ligaments may be achieved for reconstruction with a better limb function [45].
In pelvic tumors, surgery is more difficult and recurrence rates are higher due to the complex anatomy and dense neurovascular of the pelvis [180]. To address this difficulty, attempts have been made to use 3D printing guides to assist in tumor resection. Sallent et al. [181] used guides for osteotomy in the left half of the pelvis and freehand osteotomy in the right half of the pelvis in five female cadavers and found that computer-assisted planning and guide guided osteotomy had higher accuracy compared to freehand osteotomy.
Evrard et al. [182] performed surgical guide-assisted resection of primary pelvic sarcomas including chondrosarcoma, Ewing sarcoma, osteosarcoma, and fibrosarcoma. The R0 bone margin could be achieved in 8 patients (88.9%) in the group using the template, compared with only 13 patients (68.4%) in the group not using the template, demonstrating that the use of the guide was effective in improving resection accuracy. None of the patients managed with PSI-guided resection subsequently had local tumor recurrences within the bone, suggesting that the better resection accuracy offered by PSI can directly influence whether local recurrence occurs. In addition, Liu et al. [183] invented a modified anatomic template (MAT) that was used for pelvic reconstruction after tumor resection. It allowed for less bleeding and easier manipulation during pelvic tumor resection. The tumor recurrence rate was lower and the accuracy of tumor resection was higher using the modified 3D printing guide. It should be noted, however, that patients using the modified guide had a significantly higher rate of postoperative implant loosening compared to the conventional method.
5. Limitations
According to clinical needs, a 3D printer can be used to customize surgical guide templates by selecting appropriate 3D printing technology. Compared with existing manufacturing technology, 3D printing guide template production does not require a large company to produce [7]. In different fields of orthopedics, the use of guide templates can significantly improve surgical accuracy, shorten the surgical time, reduce intraoperative bleeding and radiation [62]. But there are still some problems that limit its development.
5.1. Printing materials and equipment
There are not enough kinds of materials available for 3D printing. The printing accuracy error of resin is large and it is easy to damage deformation. Titanium alloy template with a 3 d application can provide better strength and accuracy, however, high price and requirements for printing equipment restrict its wide application. Other printing technologies of metal materials and polymer materials are still in the experimental stage [184]. Additionally, we also need to pay attention to the orthopedic surgery guide used in the human body has many restrictions, such as disinfection, strength, oxygen content, liquidity, etc [1,185]. The accuracy requirements of image data, the selection of printing materials and processing methods, the disinfection and sterilization methods of guide templates still need to be solved.
5.2. Cost
Pre-design and manufacturing of guide templates can increase the workload of orthopedic surgeons and hospital. The cost of 3D printers can range from hundreds to thousands of dollars, not including the cost of plastic and resin-based materials [64]. And because of the unique and complex software applications used in the design of the surgical guide, it can take hours to days to get the final guide. Depending on the complexity of the machine and product used, it may not be suitable for more common scenarios or emergency surgery [1,4].
5.3. Long-term clinic trials
In order to achieve more ideal intraoperative stability of the guide, more soft tissues are often removed, which increases iatrogenic trauma of patients and may lead to postoperative complications. In 2017, the 3D printing guide of bone osteotomy in children has been allowed by the United States food and drug administration (FDA). Hope in the near future, long-term case studies with a large sample size of 3D guides compared with traditional surgical methods will emerge.
5.4. Laws and standards
The final template quality varies greatly. The difference ranges from aspects such as internal processes and clinical practice guidelines to the availability of post-processing equipment, which in some cases is critical to safety. At present, it is difficult to establish a unified quality evaluation mechanism. If we cannot form relevant industry standards and laws for 3D printed medical products, so as to provide a reasonable and reliable reference system for the industry, the quality of the products cannot be guaranteed. The practical application scope of the guide templates needs to be solved and standardized.
6. Prospect and summary
Since the introduction of 3D printing technology over the past decades, the method of using medical imaging, specifically CT data, to reconstruct a physical model has been increasingly mature. According to the state of the material, surgical site, and type of surgical guide, we can choose the different printing techniques, such as SLA, FDM, SLS, LOM, and so on. Although the steps to generate a digital 3D model vary from different applications, image acquisition, segmentation/conversion of the medical image, guide template design and 3D printing are the general steps required to print a 3D model. With the development of machine learning, the steps will be easier for anatomical segmentation, which is more suitable for doctors.
The interest of patient-specific surgical templates is to ensure strict application of the preoperative plan. Good implant positioning and exact bone correction are the expected benefits. In the aspects of the spine, trauma, joint, and bone tumor, the 3D surgical guide allows digitally surgical plans to be accurately implemented onto surgical sites. As well as improving exactness, it allows a lower radiation dose and shorter operating time. They also enable junior surgeons to train in techniques otherwise reserved for hyperspecialists. With the emergence of 4D printing, we hope 3D printing surgical guides can change their shape, performance, and function over time according to the needs of patients, reducing the need for secondary surgery.
With the growing knowledge and technology advances in biomaterials and the boost of the market, 3D printing guide templates have become an important complementary technology in orthopedic surgery. The production process of the guide template produces less waste and saves a lot of medical resources, which is in line with the development of the new era. Many hospitals are equipped with digital studios for more accurate image segmentation and surface processing, as well as preoperative planning, which facilitates doctors' participation in guide template design, improves doctors' 3D understanding of anatomical morphology, shorts the learning curve of young doctors. Surgeon constantly optimizes the surgical plan in the design of a surgical guide, which is beneficial to both doctors and patients.
With the rapid development of technology today, the development of orthopedic guides has ushered in a huge opportunity. Professionals in bioengineering, biomaterials, imaging processing, and other fields continue to cooperate deeply, and the combination of medical and industrial talents gradually emerge. Computer engineers constantly optimize software interfaces and develop automated algorithms (such as region growth, watershed, level set, and Markov random field models) for anatomical segmentation, which are more suitable for physicians. With the emergence of 4D printing, 3D printing forms can change their shape, performance, and function over time according to the needs of patients, reducing the need for secondary surgery. With the support of analysis of 5G, cloud computing, and big data, more accurate, fast, and reliable orthopedic guide templates will be presented to meet the needs of different groups.
In the future, the meta-universe, digital twin, and artificial intelligence will be applied to clinical work, which will greatly improve work efficiency and save medical resources. With the introduction of 3D printing industry guidelines and regulations, the guide template will be standardized from design to production and use. 3D printing guides will be further sublimated in the application of orthopedics and better serve the patients.
Declaration of competing interest
The authors declare that they have no competing interests.
Acknowledgements
This study was supported by the Science and Technology Innovation Foundation of Dalian (2020JJ27SN070) and the open project of Key Laboratory for Micro/Nano Technology and System of Liaoning Province, Dalian University of Technology (20210101). The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Hoang D., Perrault D., Stevanovic M., Ghiassi A. Surgical applications of three-dimensional printing: a review of the current literature & how to get started. Ann Transl Med. 2016;4(23):456. doi: 10.21037/atm.2016.12.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Skelley N.W., Smith M.J., Ma R., Cook J.L. Three-dimensional printing technology in orthopaedics. J Am Acad Orthop Surg. 2019;27(24):918–925. doi: 10.5435/JAAOS-D-18-00746. [DOI] [PubMed] [Google Scholar]
- 3.Auricchio F., Marconi S. 3D printing: clinical applications in orthopaedics and traumatology. EFORT Open Rev. 2016;1(5):121–127. doi: 10.1302/2058-5241.1.000012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rengier F., Mehndiratta A., von Tengg-Kobligk H., Zechmann C.M., Unterhinninghofen R., Kauczor H.U., et al. 3D printing based on imaging data: review of medical applications. Int J Comput Assist Radiol Surg. 2010;5(4):335–341. doi: 10.1007/s11548-010-0476-x. [DOI] [PubMed] [Google Scholar]
- 5.Papagelopoulos P.J., Savvidou O.D., Koutsouradis P., Chloros G.D., Bolia I.K., Sakellariou V.I., et al. Three-dimensional technologies in orthopedics. Orthopedics. 2018;41(1):12–20. doi: 10.3928/01477447-20180109-04. [DOI] [PubMed] [Google Scholar]
- 6.Dhawan A., Kennedy P.M., Rizk E.B., Ozbolat I.T. Three-dimensional bioprinting for bone and cartilage restoration in orthopaedic surgery. J Am Acad Orthop Surg. 2019;27(5):e215–e226. doi: 10.5435/JAAOS-D-17-00632. [DOI] [PubMed] [Google Scholar]
- 7.Chen X., Xu L., Wang W., Li X., Sun Y., Politis C. Computer-aided design and manufacturing of surgical templates and their clinical applications: a review. Expet Rev Med Dev. 2016;13(9):853–864. doi: 10.1080/17434440.2016.1218758. [DOI] [PubMed] [Google Scholar]
- 8.Wang L., Zhao L., Gu Y., Yu L., Ma W., Xu R. Effectiveness of 2 types of drill templates for cervical anterior transpedicular screw placements: a comparative study. World Neurosurg. 2021;147:e343–e350. doi: 10.1016/j.wneu.2020.12.055. [DOI] [PubMed] [Google Scholar]
- 9.Toni C., Oxley B., Clarke S., Behr S. Accuracy of placement of pedicle screws in the lumbosacral region of dogs using 3D-printed patient-specific drill guides. Vet Comp Orthop Traumatol : Vet Comp Orthop Traumatol. 2021;34(1):53–58. doi: 10.1055/s-0040-1716840. [DOI] [PubMed] [Google Scholar]
- 10.Zhao Y., Luo H., Ma Y., Liang J., Han G., Xu Y., et al. Accuracy of S2 alar-iliac screw placement under the guidance of a 3D-printed surgical guide template. World Neurosurg. 2021;146:e161–e167. doi: 10.1016/j.wneu.2020.10.063. [DOI] [PubMed] [Google Scholar]
- 11.Fu M., Lin L., Kong X., Zhao W., Tang L., Li J., et al. Construction and accuracy assessment of patient-specific biocompatible drill template for cervical anterior transpedicular screw (ATPS) insertion: an in vitro study. PLoS One. 2013;8(1) doi: 10.1371/journal.pone.0053580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Azimifar F., Hassani K., Hossein Saveh A., Izadi F. A new template and teleoperation system for human-guided spine surgery. Artif Organs. 2019;43(4):424–434. doi: 10.1111/aor.13358. [DOI] [PubMed] [Google Scholar]
- 13.Tian Y., Zhang J., Liu T., Tang S., Chen H., Ding K., et al. A comparative study of C2 pedicle or pars screw placement with assistance from a 3-dimensional (3D)-printed navigation template versus C-arm based navigation. Med Sci Mon Int Med J Exp Clin Res : Int Med J Exp Clin Res. 2019;25:9981–9990. doi: 10.12659/MSM.918440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Éltes P.E., Kiss L., Bartos M., Eösze Z., Szövérfi Z., Varga P.P., et al. Attitude of spine surgeons towards the application of 3D technologies - a survey of AOSpine members. Ideggyogyaszati Szle. 2019;72(7–8):227–235. doi: 10.18071/isz.72.0227. [DOI] [PubMed] [Google Scholar]
- 15.Alberti C. Three-dimensional CT and structure models. Br J Radiol. 1980;53(627):261–262. doi: 10.1259/0007-1285-53-627-261-b. [DOI] [PubMed] [Google Scholar]
- 16.Gross B.C., Erkal J.L., Lockwood S.Y., Chen C., Spence D.M. Evaluation of 3D printing and its potential impact on biotechnology and the chemical sciences. Anal Chem. 2014;86(7):3240–3253. doi: 10.1021/ac403397r. [DOI] [PubMed] [Google Scholar]
- 17.Matter-Parrat V., Liverneaux P. 3D printing in hand surgery. Hand Surg Rehabil. 2019;38(6):338–347. doi: 10.1016/j.hansur.2019.09.006. [DOI] [PubMed] [Google Scholar]
- 18.Tao Y., Yin Q., Li P. An additive manufacturing method using large-scale wood inspired by laminated object manufacturing and plywood technology. Polymers. 2020;13(1) doi: 10.3390/polym13010144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mankovich N.J., Cheeseman A.M., Stoker N.G. The display of three-dimensional anatomy with stereolithographic models. J Digit Imag. 1990;3(3):200–203. doi: 10.1007/BF03167610. [DOI] [PubMed] [Google Scholar]
- 20.Radermacher K., Portheine F., Anton M., Zimolong A., Kaspers G., Rau G., et al. Computer assisted orthopaedic surgery with image based individual templates. Clin Orthop Relat Res. 1998;(354):28–38. doi: 10.1097/00003086-199809000-00005. [DOI] [PubMed] [Google Scholar]
- 21.Haleem A., Javaid M. Role of CT and MRI in the design and development of orthopaedic model using additive manufacturing. J Clin Orthopaed Trauma. 2018;9(3):213–217. doi: 10.1016/j.jcot.2018.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Farshad M., Selman F., Burkhard M.D., Müller D., Spirig J.M. Partial sacrectomy with patient-specific osteotomy guides. North Am Spine Soc J. 2021;8:100090. doi: 10.1016/j.xnsj.2021.100090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rosseels W., Herteleer M., Sermon A., Nijs S., Hoekstra H. Corrective osteotomies using patient-specific 3D-printed guides: a critical appraisal. Eur J Trauma Emerg Surg : Off Publ Eur Trauma Soc. 2019;45(2):299–307. doi: 10.1007/s00068-018-0903-1. [DOI] [PubMed] [Google Scholar]
- 24.Upex P., Jouffroy P., Riouallon G. Application of 3D printing for treating fractures of both columns of the acetabulum: benefit of pre-contouring plates on the mirrored healthy pelvis. Orthopaed Traumatol Surg Res : OTSR. 2017;103(3):331–334. doi: 10.1016/j.otsr.2016.11.021. [DOI] [PubMed] [Google Scholar]
- 25.Bruns N., Krettek C. [3D-printing in trauma surgery : planning, printing and processing] Unfallchirurg. 2019;122(4):270–277. doi: 10.1007/s00113-019-0625-9. [DOI] [PubMed] [Google Scholar]
- 26.Wheeler G., Deng S., Toussaint N., Pushparajah K., Schnabel J.A., Simpson J.M., et al. Virtual interaction and visualisation of 3D medical imaging data with VTK and Unity. Healthcare Technol Lett. 2018;5(5):148–153. doi: 10.1049/htl.2018.5064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lo Giudice A., Ronsivalle V., Grippaudo C., Lucchese A., Muraglie S., Lagravère M.O., et al. One step before 3D printing-evaluation of imaging software accuracy for 3-dimensional analysis of the mandible: a comparative study using a surface-to-surface matching technique. Materials. 2020;13(12) doi: 10.3390/ma13122798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhang D., Bauer A.S., Blazar P., Earp B.E. Three-dimensional printing in hand surgery. J Hand Surg. 2021;46(11):1016–1022. doi: 10.1016/j.jhsa.2021.05.028. [DOI] [PubMed] [Google Scholar]
- 29.Henckel J., Holme T.J., Radford W., Skinner J.A., Hart A.J. 3D-printed patient-specific guides for hip arthroplasty. J Am Acad Orthop Surg. 2018;26(16):e342–e348. doi: 10.5435/JAAOS-D-16-00719. [DOI] [PubMed] [Google Scholar]
- 30.Mahesh M. Search for isotropic resolution in CT from conventional through multiple-row detector. Radiographics : Rev Publ Radiol Soc North Am Inc. 2002;22(4):949–962. doi: 10.1148/radiographics.22.4.g02jl14949. [DOI] [PubMed] [Google Scholar]
- 31.De Armond C.C., Kim S.E., Lewis D.D., Biedryzcki A.H., Banks S.A., Cook J.L., et al. Three-dimensional-printed custom guides for bipolar coxofemoral osteochondral allograft in dogs. PLoS One. 2021;16(2) doi: 10.1371/journal.pone.0244208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lázár I., Hajdu A. Segmentation of retinal vessels by means of directional response vector similarity and region growing. Comput Biol Med. 2015;66:209–221. doi: 10.1016/j.compbiomed.2015.09.008. [DOI] [PubMed] [Google Scholar]
- 33.Sivakumar V., Janakiraman N. A novel method for segmenting brain tumor using modified watershed algorithm in MRI image with FPGA. Biosystems. 2020;198:104226. doi: 10.1016/j.biosystems.2020.104226. [DOI] [PubMed] [Google Scholar]
- 34.Samavati N., Velec M., Brock K. A hybrid biomechanical intensity based deformable image registration of lung 4DCT. Phys Med Biol. 2015;60(8):3359–3373. doi: 10.1088/0031-9155/60/8/3359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lin D., Jin S., Zhang F., Wang C., Wang Y., Zhou C., et al. 3D stereolithography printing of graphene oxide reinforced complex architectures. Nanotechnology. 2015;26(43):434003. doi: 10.1088/0957-4484/26/43/434003. [DOI] [PubMed] [Google Scholar]
- 36.Gokuldoss P.K., Kolla S., Eckert J. Additive manufacturing processes: selective laser melting, electron beam melting and binder jetting-selection guidelines. Materials. 2017;10(6) doi: 10.3390/ma10060672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Xia R.Z., Zhai Z.J., Chang Y.Y., Li H.W. Clinical applications of 3-dimensional printing technology in hip joint. Orthop Surg. 2019;11(4):533–544. doi: 10.1111/os.12468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Senkoylu A., Daldal I., Cetinkaya M. 3D printing and spine surgery. J Orthop Surg. 2020;28(2) doi: 10.1177/2309499020927081. 2309499020927081. [DOI] [PubMed] [Google Scholar]
- 39.Seon J.K., Park H.W., Yoo S.H., Song E.K. Assessing the accuracy of patient-specific guides for total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc : Off J ESSKA. 2016;24(11):3678–3683. doi: 10.1007/s00167-014-3429-z. [DOI] [PubMed] [Google Scholar]
- 40.Hafez M.A., Hamza H., Nabeel A. Hospital-based patient-specific templates for total knee arthroplasty: a proof of concept clinical study. Tech Orthop. 2018;33(4):258–263. doi: 10.1097/BTO.0000000000000253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sharma N., Cao S., Msallem B., Kunz C., Brantner P., Honigmann P., et al. Effects of steam sterilization on 3D printed biocompatible resin materials for surgical guides-an accuracy assessment study. J Clin Med. 2020;9(5) doi: 10.3390/jcm9051506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lachiewicz P.F., Watters T.S., Jacobs J.J. Metal hypersensitivity and total knee arthroplasty. J Am Acad Orthop Surg. 2016;24(2):106–112. doi: 10.5435/JAAOS-D-14-00290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Li J., Lin J., Yang Y., Xu J., Fei Q. 3-Dimensional printing guide template assisted percutaneous vertebroplasty: technical note. J Clin Neurosci : Off J Neurosurg Soc Australas. 2018;52:159–164. doi: 10.1016/j.jocn.2018.03.012. [DOI] [PubMed] [Google Scholar]
- 44.Li Z., Xu D., Li F., Liu M., Xu G., Yang M. Design and application of a novel patient-specific 3D printed drill navigational guiding template in percutaneous thoracolumbar pedicle screw fixation: a cadaveric study. J Clin Neurosci : Off J Neurosurg Soc Australas. 2020;73:294–298. doi: 10.1016/j.jocn.2020.01.083. [DOI] [PubMed] [Google Scholar]
- 45.Wong K.C., Sze L.K.Y., Kumta S.M. Complex joint-preserving bone tumor resection and reconstruction using computer navigation and 3D-printed patient-specific guides: a technical note of three cases. J Orthopaed Transl. 2021;29:152–162. doi: 10.1016/j.jot.2021.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sugawara T., Kaneyama S., Higashiyama N., Tamura S., Endo T., Takabatake M., et al. Prospective multicenter study of a multistep screw insertion technique using patient-specific screw guide templates for the cervical and thoracic spine. Spine. 2018;43(23):1685–1694. doi: 10.1097/BRS.0000000000002810. [DOI] [PubMed] [Google Scholar]
- 47.Cai H., Liu Z., Wei F., Yu M., Xu N., Li Z. 3D printing in spine surgery. Adv Exp Med Biol. 2018;1093:345–359. doi: 10.1007/978-981-13-1396-7_27. [DOI] [PubMed] [Google Scholar]
- 48.Byrne A.M., Impelmans B., Bertrand V., Van Haver A., Verstreken F. Corrective osteotomy for malunited diaphyseal forearm fractures using preoperative 3-dimensional planning and patient-specific surgical guides and implants. J Hand Surg. 2017;42(10) doi: 10.1016/j.jhsa.2017.06.003. 836.e1-36.e12. [DOI] [PubMed] [Google Scholar]
- 49.Bauer A.S., Storelli D.A.R., Sibbel S.E., McCarroll H.R., Lattanza L.L. Preoperative computer simulation and patient-specific guides are safe and effective to correct forearm deformity in children. J Pediatr Orthoped. 2017;37(7):504–510. doi: 10.1097/BPO.0000000000000673. [DOI] [PubMed] [Google Scholar]
- 50.Hirao M., Ikemoto S., Tsuboi H., Akita S., Ohshima S., Saeki Y., et al. Computer assisted planning and custom-made surgical guide for malunited pronation deformity after first metatarsophalangeal joint arthrodesis in rheumatoid arthritis: a case report. Comput Aided Surg : Off J Int Soc Comput Aided Surg. 2014;19(1–3):13–19. doi: 10.3109/10929088.2014.885992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Huang H., Hsieh M.F., Zhang G., Ouyang H., Zeng C., Yan B., et al. Improved accuracy of 3D-printed navigational template during complicated tibial plateau fracture surgery. Australas Phys Eng Sci Med. 2015;38(1):109–117. doi: 10.1007/s13246-015-0330-0. [DOI] [PubMed] [Google Scholar]
- 52.Berry E., Cuppone M., Porada S., Millner P.A., Rao A., Chiverton N., et al. Personalised image-based templates for intra-operative guidance. Proc IME H J Eng Med. 2005;219(2):111–118. doi: 10.1243/095441105X9273. [DOI] [PubMed] [Google Scholar]
- 53.Goffin J., Van Brussel K., Martens K., Vander Sloten J., Van Audekercke R., Smet M.H. Three-dimensional computed tomography-based, personalized drill guide for posterior cervical stabilization at C1-C2. Spine. 2001;26(12):1343–1347. doi: 10.1097/00007632-200106150-00017. [DOI] [PubMed] [Google Scholar]
- 54.Kahler D.M. Image guidance: fluoroscopic navigation. Clin Orthop Relat Res. 2004;(421):70–76. [PubMed] [Google Scholar]
- 55.Azimi P., Yazdanian T., Benzel E.C., Azimi A., Montazeri A. 3D-printed navigation template in cervical spine fusion: a systematic review and meta-analysis. Eur Spine J : Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sec Cerv Spine Res Soc. 2021;30(2):389–401. doi: 10.1007/s00586-020-06601-6. [DOI] [PubMed] [Google Scholar]
- 56.Pijpker P.A.J., Kraeima J., Witjes M.J.H., Oterdoom D.L.M., Coppes M.H., Groen R.J.M., et al. Accuracy assessment of pedicle and lateral mass screw insertion assisted by customized 3D-printed drill guides: a human cadaver study. Oper Neurosurg (Hagerstown, Md) 2019;16(1):94–102. doi: 10.1093/ons/opy060. [DOI] [PubMed] [Google Scholar]
- 57.Gauci M.O. Patient-specific guides in orthopedic surgery. Orthopaed Traumatol Surg Res : OTSR. 2022;108(1s):103154. doi: 10.1016/j.otsr.2021.103154. [DOI] [PubMed] [Google Scholar]
- 58.Takemoto M., Fujibayashi S., Ota E., Otsuki B., Kimura H., Sakamoto T., et al. Additive-manufactured patient-specific titanium templates for thoracic pedicle screw placement: novel design with reduced contact area. Eur Spine J : Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sec Cerv Spine Res Soc. 2016;25(6):1698–1705. doi: 10.1007/s00586-015-3908-z. [DOI] [PubMed] [Google Scholar]
- 59.Pijpker P.A.J., Kraeima J., Witjes M.J.H., Oterdoom D.L.M., Vergeer R.A., Coppes M.H., et al. Accuracy of patient-specific 3D-printed drill guides for pedicle and lateral mass screw insertion: an analysis of 76 cervical and thoracic screw trajectories. Spine. 2021;46(3):160–168. doi: 10.1097/BRS.0000000000003747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Adamczak S.E., Bova F.J., Hoh D.J. Intraoperative 3D computed tomography: spine surgery. Neurosurg Clin. 2017;28(4):585–594. doi: 10.1016/j.nec.2017.06.002. [DOI] [PubMed] [Google Scholar]
- 61.Provaggi E., Leong J.J.H., Kalaskar D.M. Applications of 3D printing in the management of severe spinal conditions. Proc IME H J Eng Med. 2017;231(6):471–486. doi: 10.1177/0954411916667761. [DOI] [PubMed] [Google Scholar]
- 62.Yu C., Ou Y., Xie C., Zhang Y., Wei J., Mu X. Pedicle screw placement in spinal neurosurgery using a 3D-printed drill guide template: a systematic review and meta-analysis. J Orthop Surg Res. 2020;15(1):1. doi: 10.1186/s13018-019-1510-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Garg B., Gupta M., Singh M., Kalyanasundaram D. Outcome and safety analysis of 3D-printed patient-specific pedicle screw jigs for complex spinal deformities: a comparative study. Spine J : Off J North Am Spine Soc. 2019;19(1):56–64. doi: 10.1016/j.spinee.2018.05.001. [DOI] [PubMed] [Google Scholar]
- 64.Sheha E.D., Gandhi S.D., Colman M.W. 3D printing in spine surgery. Ann Transl Med. 2019;7(Suppl 5):S164. doi: 10.21037/atm.2019.08.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Guo F., Dai J., Zhang J., Ma Y., Zhu G., Shen J., et al. Individualized 3D printing navigation template for pedicle screw fixation in upper cervical spine. PLoS One. 2017;12(2) doi: 10.1371/journal.pone.0171509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Chen X.L., Xie Y.F., Li J.X., Wu W., Li G.N., Hu H.J., et al. Design and basic research on accuracy of a novel individualized three-dimensional printed navigation template in atlantoaxial pedicle screw placement. PLoS One. 2019;14(4) doi: 10.1371/journal.pone.0214460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Li Y., Lin J., Wang Y., Luo H., Wang J., Lu S., et al. Comparative study of 3D printed navigation template-assisted atlantoaxial pedicle screws versus free-hand screws for type II odontoid fractures. Eur Spine J : Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sec Cerv Spine Res Soc. 2021;30(2):498–506. doi: 10.1007/s00586-020-06644-9. [DOI] [PubMed] [Google Scholar]
- 68.Pu X., Luo C., Lu T., Yao S., Chen Q. Clinical application of atlantoaxial pedicle screw placement assisted by a modified 3D-printed navigation template. Clinics. 2018;73:e259. doi: 10.6061/clinics/2018/e259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Thayaparan G.K., Owbridge M.G., Thompson R.G., D'Urso P.S. Designing patient-specific 3D printed devices for posterior atlantoaxial transarticular fixation surgery. J Clin Neurosci : Off J Neurosurg Soc Australas. 2018;56:192–198. doi: 10.1016/j.jocn.2018.06.038. [DOI] [PubMed] [Google Scholar]
- 70.Sugawara T., Higashiyama N., Kaneyama S., Sumi M. Accurate and simple screw insertion procedure with patient-specific screw guide templates for posterior C1-C2 fixation. Spine. 2017;42(6) doi: 10.1097/BRS.0000000000001807. E340-e46. [DOI] [PubMed] [Google Scholar]
- 71.Hu Y., Yuan Z.S., Spiker W.R., Albert T.J., Dong W.X., Xie H., et al. Deviation analysis of C2 translaminar screw placement assisted by a novel rapid prototyping drill template: a cadaveric study. Eur Spine J : Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sec Cerv Spine Res Soc. 2013;22(12):2770–2776. doi: 10.1007/s00586-013-2993-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lu S., Xu Y.Q., Zhang Y.Z., Xie L., Guo H., Li D.P. A novel computer-assisted drill guide template for placement of C2 laminar screws. Eur Spine J : Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sec Cerv Spine Res Soc. 2009;18(9):1379–1385. doi: 10.1007/s00586-009-1051-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ryken T.C., Owen B.D., Christensen G.E., Reinhardt J.M. Image-based drill templates for cervical pedicle screw placement. J Neurosurg Spine. 2009;10(1):21–26. doi: 10.3171/2008.9.SPI08229. [DOI] [PubMed] [Google Scholar]
- 74.Lu S., Xu Y.Q., Lu W.W., Ni G.X., Li Y.B., Shi J.H., et al. A novel patient-specific navigational template for cervical pedicle screw placement. Spine. 2009;34(26):E959–E966. doi: 10.1097/BRS.0b013e3181c09985. [DOI] [PubMed] [Google Scholar]
- 75.Zhang G., Yu Z., Chen X., Chen X., Wu C., Lin Y., et al. Accurate placement of cervical pedicle screws using 3D-printed navigational templates : an improved technique with continuous image registration. Orthopä. 2018;47(5):428–436. doi: 10.1007/s00132-017-3515-2. [DOI] [PubMed] [Google Scholar]
- 76.Peng P., Xu Y., Zhang X., Zhu M., Du B., Li W., et al. Is a patient-specific drill template via a cortical bone trajectory safe in cervical anterior transpedicular insertion? J Orthop Surg Res. 2018;13(1):91. doi: 10.1186/s13018-018-0810-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kaneyama S., Sugawara T., Sumi M. Safe and accurate midcervical pedicle screw insertion procedure with the patient-specific screw guide template system. Spine. 2015;40(6):E341–E348. doi: 10.1097/BRS.0000000000000772. [DOI] [PubMed] [Google Scholar]
- 78.Yu Z., Zhang G., Chen X., Chen X., Wu C., Lin Y., et al. Application of a novel 3D drill template for cervical pedicle screw tunnel design: a cadaveric study. Eur Spine J : Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sec Cerv Spine Res Soc. 2017;26(9):2348–2356. doi: 10.1007/s00586-017-5118-3. [DOI] [PubMed] [Google Scholar]
- 79.Deng T., Jiang M., Lei Q., Cai L., Chen L. The accuracy and the safety of individualized 3D printing screws insertion templates for cervical screw insertion. Comput Assist Surg (Abingdon, England) 2016;21(1):143–149. doi: 10.1080/24699322.2016.1236146. [DOI] [PubMed] [Google Scholar]
- 80.Thayaparan G.K., Owbridge M.G., Thompson R.G., D'Urso P.S. Patient-specific processes for occipitocervical fixation using biomodelling and additive manufacturing. J Clin Neurosci : Off J Neurosurg Soc Australas. 2020;71:251–256. doi: 10.1016/j.jocn.2019.10.005. [DOI] [PubMed] [Google Scholar]
- 81.Ryken T.C., Kim J., Owen B.D., Christensen G.E., Reinhardt J.M. Engineering patient-specific drill templates and bioabsorbable posterior cervical plates: a feasibility study. J Neurosurg Spine. 2009;10(2):129–132. doi: 10.3171/2008.11.SPI0817677. [DOI] [PubMed] [Google Scholar]
- 82.Fujioka T., Nakata K., Nishida H., Sugawara T., Konno N., Maeda S., et al. A novel patient-specific drill guide template for stabilization of thoracolumbar vertebrae of dogs: cadaveric study and clinical cases. Vet Surg : Vysokomol Soedin. 2019;48(3):336–342. doi: 10.1111/vsu.13140. [DOI] [PubMed] [Google Scholar]
- 83.Ma T., Xu Y.Q., Cheng Y.B., Jiang M.Y., Xu X.M., Xie L., et al. A novel computer-assisted drill guide template for thoracic pedicle screw placement: a cadaveric study. Arch Orthop Trauma Surg. 2012;132(1):65–72. doi: 10.1007/s00402-011-1383-5. [DOI] [PubMed] [Google Scholar]
- 84.Chen H., Guo K., Yang H., Wu D., Yuan F. Thoracic pedicle screw placement guide plate produced by three-dimensional (3-D) laser printing. Med Sci Mon Int Med J Exp Clin Res : Int Med J Exp Clin Res. 2016;22:1682–1686. doi: 10.12659/MSM.896148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Wang K., Zhang Z.J., Chen J.X., Wu A.M., Wang X.Y., Sheng S.R. Design and application of individualized, 3-dimensional-printed navigation template for placing cortical bone trajectory screws in middle-upper thoracic spine: cadaver research study. World Neurosurg. 2019;125:e348–e352. doi: 10.1016/j.wneu.2019.01.076. [DOI] [PubMed] [Google Scholar]
- 86.Chen X., Gao X., Zhang G., Zheng F., Wang Y., Huang W., et al. Design, application, and evaluation of a novel method for determining optimal trajectory of thoracic pedicle screws. Ann Transl Med. 2020;8(16):1012. doi: 10.21037/atm-20-5426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Hu Y., Yuan Z.S., Spiker W.R., Dong W.X., Sun X.Y., Yuan J.B., et al. A comparative study on the accuracy of pedicle screw placement assisted by personalized rapid prototyping template between pre- and post-operation in patients with relatively normal mid-upper thoracic spine. Eur Spine J : Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sec Cerv Spine Res Soc. 2016;25(6):1706–1715. doi: 10.1007/s00586-016-4540-2. [DOI] [PubMed] [Google Scholar]
- 88.Sugawara T., Higashiyama N., Kaneyama S., Takabatake M., Watanabe N., Uchida F., et al. Multistep pedicle screw insertion procedure with patient-specific lamina fit-and-lock templates for the thoracic spine: clinical article. J Neurosurg Spine. 2013;19(2):185–190. doi: 10.3171/2013.4.SPINE121059. [DOI] [PubMed] [Google Scholar]
- 89.Naddeo F., Fontana C., Naddeo A., Cataldo E., Cappetti N., Narciso N. Novel design for a customized, 3D-printed surgical template for thoracic spinal arthrodesis. Int J Med Robot + Comput Assist Surg : MRCAS. 2019;15(4) doi: 10.1002/rcs.2005. [DOI] [PubMed] [Google Scholar]
- 90.Merc M., Drstvensek I., Vogrin M., Brajlih T., Recnik G. A multi-level rapid prototyping drill guide template reduces the perforation risk of pedicle screw placement in the lumbar and sacral spine. Arch Orthop Trauma Surg. 2013;133(7):893–899. doi: 10.1007/s00402-013-1755-0. [DOI] [PubMed] [Google Scholar]
- 91.Ferrari V., Parchi P., Condino S., Carbone M., Baluganti A., Ferrari M., et al. An optimal design for patient-specific templates for pedicle spine screws placement. Int J Med Robot + Comput Assist Surg : MRCAS. 2013;9(3):298–304. doi: 10.1002/rcs.1439. [DOI] [PubMed] [Google Scholar]
- 92.Lu S., Xu Y.Q., Zhang Y.Z., Li Y.B., Xie L., Shi J.H., et al. A novel computer-assisted drill guide template for lumbar pedicle screw placement: a cadaveric and clinical study. Int J Med Robot + Comput Assist Surg : MRCAS. 2009;5(2):184–191. doi: 10.1002/rcs.249. [DOI] [PubMed] [Google Scholar]
- 93.Zhou W., Xia T., Liu Y., Cao F., Liu M., Liu J., et al. Comparative study of sacroiliac screw placement guided by 3D-printed template technology and X-ray fluoroscopy. Arch Orthop Trauma Surg. 2020;140(1):11–17. doi: 10.1007/s00402-019-03207-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Wang H., Liu Y., Zhao Y., Song G., Liu J., Han J., et al. Feasibility and accuracy of computer-assisted individual drill guide template for minimally invasive lumbar pedicle screw placement trajectory. Injury. 2018;49(3):644–648. doi: 10.1016/j.injury.2018.02.011. [DOI] [PubMed] [Google Scholar]
- 95.Ge D.W., Yang L., Chen X., Tang J., Chen H.T., Li H.J., et al. A multi-level drill guide template improves the accuracy of pedicle screw placement in lumbar spine. Eur Rev Med Pharmacol Sci. 2018;22(12):3643–3648. doi: 10.26355/eurrev_201806_15241. [DOI] [PubMed] [Google Scholar]
- 96.Zhao Y., Liang J., Luo H., Xu Y., Lu S. Double-trajectory lumbar screw placement guided by a set of 3D-printed surgical guide templates: a cadaver study. BMC Muscoskel Disord. 2021;22(1):296. doi: 10.1186/s12891-021-04149-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Marengo N., Matsukawa K., Monticelli M., Ajello M., Pacca P., Cofano F., et al. Cortical bone trajectory screw placement accuracy with a patient-matched 3-dimensional printed guide in lumbar spinal surgery: a clinical study. World Neurosurg. 2019;130:e98–e104. doi: 10.1016/j.wneu.2019.05.241. [DOI] [PubMed] [Google Scholar]
- 98.Kim J., Rajadurai J., Choy W.J., Cassar L., Phan K., Harris L., et al. Three-dimensional patient-specific guides for intraoperative navigation for cortical screw trajectory pedicle fixation. World Neurosurg. 2019;122:674–679. doi: 10.1016/j.wneu.2018.11.159. [DOI] [PubMed] [Google Scholar]
- 99.Chen H., Wu D., Yang H., Guo K. Clinical use of 3D printing guide plate in posterior lumbar pedicle screw fixation. Med Sci Mon Int Med J Exp Clin Res : Int Med J Exp Clin Res. 2015;21:3948–3954. doi: 10.12659/MSM.895597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.He K., Dong C., Wei H., Yang F., Ma H., Tang X., et al. A minimally invasive technique using cortical bone trajectory screws assisted by 3D-printed navigation templates in lumbar adjacent segment degeneration. Clin Interv Aging. 2021;16:1403–1413. doi: 10.2147/CIA.S318525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Petrone S., Marengo N., Ajello M., Lavorato A., Penner F., Cofano F., et al. Cortical bone trajectory technique's outcomes and procedures for posterior lumbar fusion: a retrospective study. J Clin Neurosci : Off J Neurosurg Soc Australas. 2020;76:25–30. doi: 10.1016/j.jocn.2020.04.070. [DOI] [PubMed] [Google Scholar]
- 102.Matsukawa K., Kaito T., Abe Y. Accuracy of cortical bone trajectory screw placement using patient-specific template guide system. Neurosurg Rev. 2020;43(4):1135–1142. doi: 10.1007/s10143-019-01140-1. [DOI] [PubMed] [Google Scholar]
- 103.Shao Z.X., Wang J.S., Lin Z.K., Ni W.F., Wang X.Y., Wu A.M. Improving the trajectory of transpedicular transdiscal lumbar screw fixation with a computer-assisted 3D-printed custom drill guide. PeerJ. 2017;5 doi: 10.7717/peerj.3564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Zhao Y., Ma Y., Liang J., Luo H., Cai X., Xu Y., et al. Comparison of the 3D-printed operation guide template technique and the free-hand technique for S2-alar-iliac screw placement. BMC Surg. 2020;20(1):258. doi: 10.1186/s12893-020-00930-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Wu C., Deng J., Pan J., Li T., Tan L., Yuan D. Anatomical conditions and patient-specific locked navigation templates for transverse sacroiliac screw placement: a retrospective study. J Orthop Surg Res. 2020;15(1):260. doi: 10.1186/s13018-020-01752-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Wu C., Deng J.Y., Li T., Tan L., Yuan D.C. Combined 3D printed template to guide iliosacral screw insertion for sacral fracture and dislocation: a retrospective analysis. Orthop Surg. 2020;12(1):241–247. doi: 10.1111/os.12620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Eltes P.E., Bartos M., Hajnal B., Pokorni A.J., Kiss L., Lacroix D., et al. Development of a computer-aided design and finite element analysis combined method for affordable spine surgical navigation with 3D-printed customized template. Front Surg. 2020;7:583386. doi: 10.3389/fsurg.2020.583386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Chen P.C., Chang C.C., Chen H.T., Lin C.Y., Ho T.Y., Chen Y.J., et al. The accuracy of 3D printing assistance in the spinal deformity surgery. BioMed Res Int. 2019;2019:7196528. doi: 10.1155/2019/7196528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Cecchinato R., Berjano P., Zerbi A., Damilano M., Redaelli A., Lamartina C. Pedicle screw insertion with patient-specific 3D-printed guides based on low-dose CT scan is more accurate than free-hand technique in spine deformity patients: a prospective, randomized clinical trial. Eur Spine J : Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sec Cerv Spine Res Soc. 2019;28(7):1712–1723. doi: 10.1007/s00586-019-05978-3. [DOI] [PubMed] [Google Scholar]
- 110.Azimifar F., Hassani K., Saveh A.H., Ghomsheh F.T. A medium invasiveness multi-level patient's specific template for pedicle screw placement in the scoliosis surgery. Biomed Eng Online. 2017;16(1):130. doi: 10.1186/s12938-017-0421-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Lu S., Zhang Y.Z., Wang Z., Shi J.H., Chen Y.B., Xu X.M., et al. Accuracy and efficacy of thoracic pedicle screws in scoliosis with patient-specific drill template. Med Biol Eng Comput. 2012;50(7):751–758. doi: 10.1007/s11517-012-0900-1. [DOI] [PubMed] [Google Scholar]
- 112.Liang W., Han B., Hai J.J., Hai Y., Chen L., Kang N., et al. 3D-printed drill guide template, a promising tool to improve pedicle screw placement accuracy in spinal deformity surgery: a systematic review and meta-analysis. Eur Spine J : Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sec Cerv Spine Res Soc. 2021;30(5):1173–1183. doi: 10.1007/s00586-021-06739-x. [DOI] [PubMed] [Google Scholar]
- 113.Li X., Zhang Y., Zhang Q., Zhao C., Liu K. Clinical application OF a drill guide template for pedicle screw placement IN severe scoliosis. Acta Ortopédica Bras. 2017;25(2):67–70. doi: 10.1590/1413-785220172502138828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Luo M., Wang W., Yang N., Xia L. Does three-dimensional printing plus pedicle guider technology in severe congenital scoliosis facilitate accurate and efficient pedicle screw placement? Clin Orthop Relat Res. 2019;477(8):1904–1912. doi: 10.1097/CORR.0000000000000739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Liu K., Zhang Q., Li X., Zhao C., Quan X., Zhao R., et al. Preliminary application of a multi-level 3D printing drill guide template for pedicle screw placement in severe and rigid scoliosis. Eur Spine J : Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sec Cerv Spine Res Soc. 2017;26(6):1684–1689. doi: 10.1007/s00586-016-4926-1. [DOI] [PubMed] [Google Scholar]
- 116.Senkoylu A., Cetinkaya M., Daldal I., Necefov E., Eren A., Samartzis D. Personalized three-dimensional printing pedicle screw guide innovation for the surgical management of patients with adolescent idiopathic scoliosis. World Neurosurg. 2020;144:e513–e522. doi: 10.1016/j.wneu.2020.08.212. [DOI] [PubMed] [Google Scholar]
- 117.Tu Q., Chen H., Ding H.W., Yu G.W., Miao Q.J., Shen J.J., et al. Three-dimensional printing technology for surgical correction of congenital scoliosis caused by hemivertebrae. World Neurosurg. 2021;149:e969–e981. doi: 10.1016/j.wneu.2021.01.063. [DOI] [PubMed] [Google Scholar]
- 118.Pijpker P.A.J., Kuijlen J.M.A., Kraeima J., Faber C. Three-dimensional planning and use of individualized osteotomy-guiding templates for surgical correction of kyphoscoliosis: a technical case report. World Neurosurg. 2018;119:113–117. doi: 10.1016/j.wneu.2018.07.219. [DOI] [PubMed] [Google Scholar]
- 119.Tu Q., Ding H.W., Chen H., Miao Q.J., Yang X., Li K., et al. Three-dimensional-printed individualized guiding templates for surgical correction of severe kyphoscoliosis secondary to ankylosing spondylitis: outcomes of 9 cases. World Neurosurg. 2019;130:e961–e970. doi: 10.1016/j.wneu.2019.07.047. [DOI] [PubMed] [Google Scholar]
- 120.Hu P.L., Lin J.S., Meng H., Su N., Yang Y., Fei Q. A novel "three-dimensional-printed individual guide template-assisted percutaneous vertebroplasty" for osteoporotic vertebral compression fracture: a prospective, controlled study. J Orthop Surg Res. 2021;16(1):326. doi: 10.1186/s13018-021-02471-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Zhang Y., Gu D., Ji D. The design and application of a customized navigation board for lumbar disc ablation. Comput Assist Surg (Abingdon, England) 2017;22(sup1):305–311. doi: 10.1080/24699322.2017.1389409. [DOI] [PubMed] [Google Scholar]
- 122.Hall E.L., Baines S., Bilmont A., Oxley B. Accuracy of patient-specific three-dimensional-printed osteotomy and reduction guides for distal femoral osteotomy in dogs with medial patella luxation. Vet Surg : Vysokomol Soedin. 2019;48(4):584–591. doi: 10.1111/vsu.13126. [DOI] [PubMed] [Google Scholar]
- 123.Nie W., Gu F., Wang Z., Wu R., Yue Y., Shao A. Preliminary application of three-dimension printing technology in surgical management of bicondylar tibial plateau fractures. Injury. 2019;50(2):476–483. doi: 10.1016/j.injury.2018.12.019. [DOI] [PubMed] [Google Scholar]
- 124.Duan D., Cao Y., Li R., Wang G., Zhang Y., Xiang K., et al. Opening wedge high tibial osteotomy with combined use of patient-specific 3D-printed plates and taylor spatial frame for the treatment of knee osteoarthritis. Pain Res Manag. 2021;2021:8609921. doi: 10.1155/2021/8609921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Dong X.P., Zhang Y.W., Wang Z., Deng L. Clinical application of three-dimensional printing assisted percutaneous guide plate in minimally invasive reduction and internal fixation of tibial plateau fracture. Asian J Surg. 2020;43(9):921–923. doi: 10.1016/j.asjsur.2020.04.020. [DOI] [PubMed] [Google Scholar]
- 126.Sun L., Liu H., Xu C., Yan B., Yue H., Wang P. 3D printed navigation template-guided minimally invasive percutaneous plate osteosynthesis for distal femoral fracture: a retrospective cohort study. Injury. 2020;51(2):436–442. doi: 10.1016/j.injury.2019.10.086. [DOI] [PubMed] [Google Scholar]
- 127.Rho Y.H., Cho C.W., Ryu C.H., Lee J.H., Jeong S.M., Lee H.B. Comparison between novice and experienced surgeons performing corrective osteotomy with patient-specific guides in dogs based on resulting position accuracy. Vet Sci. 2021;8(3) doi: 10.3390/vetsci8030040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Hsu C.P., Lin S.C., Nazir A., Wu C.T., Chang S.S., Chan Y.S. Design and application of personalized surgical guides to treat complex tibial plateau malunion. Comput Methods Biomech Biomed Eng. 2021;24(4):419–428. doi: 10.1080/10255842.2020.1833193. [DOI] [PubMed] [Google Scholar]
- 129.Zhang Y.W., Xiong L.Y., Gao W.C., Deng L. Treatment of diabetic foot with the transverse tibial bone transport guided by three-dimensional printing guide plates. Asian J Surg. 2020;43(8):832–834. doi: 10.1016/j.asjsur.2020.03.009. [DOI] [PubMed] [Google Scholar]
- 130.Hoekstra H., Rosseels W., Sermon A., Nijs S. Corrective limb osteotomy using patient specific 3D-printed guides: a technical note. Injury. 2016;47(10):2375–2380. doi: 10.1016/j.injury.2016.07.021. [DOI] [PubMed] [Google Scholar]
- 131.Sys G., Eykens H., Lenaerts G., Shumelinsky F., Robbrecht C., Poffyn B. Accuracy assessment of surgical planning and three-dimensional-printed patient-specific guides for orthopaedic osteotomies. Proc IME H J Eng Med. 2017;231(6):499–508. doi: 10.1177/0954411917702177. [DOI] [PubMed] [Google Scholar]
- 132.Chen Y., Jia X., Qiang M., Zhang K., Chen S. Computer-assisted virtual surgical technology versus three-dimensional printing technology in preoperative planning for displaced three and four-Part Fractures of the proximal end of the humerus. J Bone Joint Surg Am. 2018;100(22):1960–1968. doi: 10.2106/JBJS.18.00477. [DOI] [PubMed] [Google Scholar]
- 133.Easter T.G., Bilmont A., Pink J., Oxley B. Accuracy of three-dimensional printed patient-specific drill guides for treatment of canine humeral intracondylar fissure. Vet Surg : Vysokomol Soedin. 2020;49(2):363–372. doi: 10.1111/vsu.13346. [DOI] [PubMed] [Google Scholar]
- 134.Hu X., Zhong M., Lou Y., Xu P., Jiang B., Mao F., et al. Clinical application of individualized 3D-printed navigation template to children with cubitus varus deformity. J Orthop Surg Res. 2020;15(1):111. doi: 10.1186/s13018-020-01615-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Oka K., Murase T., Okada K., Tanaka H., Yoshikawa H. Single-plane rotational osteotomy for cubitus varus deformity based on preoperative computer simulation. J Orthop Sci : Off J Jpn Orthopaed Assoc. 2019;24(5):945–951. doi: 10.1016/j.jos.2017.04.012. [DOI] [PubMed] [Google Scholar]
- 136.Omori S., Murase T., Oka K., Kawanishi Y., Oura K., Tanaka H., et al. Postoperative accuracy analysis of three-dimensional corrective osteotomy for cubitus varus deformity with a custom-made surgical guide based on computer simulation. J Shoulder Elbow Surg. 2015;24(2):242–249. doi: 10.1016/j.jse.2014.08.020. [DOI] [PubMed] [Google Scholar]
- 137.Caiti G., Dobbe J.G.G., Strackee S.D., van Doesburg M.H.M., Strijkers G.J., Streekstra G.J. A 3D printed cast for minimally invasive transfer of distal radius osteotomy: a cadaver study. Int J Comput Assist Radiol Surg. 2021;16(3):505–513. doi: 10.1007/s11548-021-02310-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Honigmann P., Thieringer F., Steiger R., Haefeli M., Schumacher R., Henning J. A simple 3-dimensional printed aid for a corrective palmar opening wedge osteotomy of the distal radius. J Hand Surg. 2016;41(3):464–469. doi: 10.1016/j.jhsa.2015.12.022. [DOI] [PubMed] [Google Scholar]
- 139.Casari F.A., Roner S., Fürnstahl P., Nagy L., Schweizer A. Computer-assisted open reduction internal fixation of intraarticular radius fractures navigated with patient-specific instrumentation, a prospective case series. Arch Orthop Trauma Surg. 2021;141(8):1425–1432. doi: 10.1007/s00402-021-03856-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Yin H.W., Xu J., Xu W.D. 3-Dimensional printing-assisted percutaneous fixation for acute scaphoid fracture: 1-shot procedure. J Hand Surg. 2017;42(4) doi: 10.1016/j.jhsa.2017.01.017. 301.e1-01.e5. [DOI] [PubMed] [Google Scholar]
- 141.Guo Y., Tian G., Zlotolow D.A., Tian W., Zhong W., Sun L. A cadaveric study on the accuracy of an individualized guiding template to assist scaphoid fixation using computed tomography and 3-dimensional printing. J Hand Surg. 2019;44(3) doi: 10.1016/j.jhsa.2018.06.017. 251.e1-51.e6. [DOI] [PubMed] [Google Scholar]
- 142.Wan S.X., Meng F.B., Zhang J., Chen Z., Yu L.B., Wen J.J. Experimental study and preliminary clinical application of mini-invasive percutaneous internal screw fixation for scaphoid fracture under the guidance of a 3D-printed guide plate. Curr Med Sci. 2019;39(6):990–996. doi: 10.1007/s11596-019-2133-0. [DOI] [PubMed] [Google Scholar]
- 143.Chen K., Yao S., Yang F., Drepaul D., Telemacque D., Zhu F., et al. Minimally invasive screw fixation of unstable pelvic fractures using the "blunt end" kirschner wire technique assisted by 3D printed external template. BioMed Res Int. 2019;2019:1524908. doi: 10.1155/2019/1524908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Chen X., Chen X., Zhang G., Lin H., Yu Z., Wu C., et al. Accurate fixation of plates and screws for the treatment of acetabular fractures using 3D-printed guiding templates: an experimental study. Injury. 2017;48(6):1147–1154. doi: 10.1016/j.injury.2017.03.009. [DOI] [PubMed] [Google Scholar]
- 145.Maini L., Verma T., Sharma A., Sharma A., Mishra A., Jha S. Evaluation of accuracy of virtual surgical planning for patient-specific pre-contoured plate in acetabular fracture fixation. Arch Orthop Trauma Surg. 2018;138(4):495–504. doi: 10.1007/s00402-018-2868-2. [DOI] [PubMed] [Google Scholar]
- 146.Peng W., Zheng R., Wang H., Huang X. Reconstruction of bony defects after tumor resection with 3D-printed anatomically conforming pelvic prostheses through a novel treatment strategy. BioMed Res Int. 2020;2020:8513070. doi: 10.1155/2020/8513070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Huotilainen E., Salmi M., Lindahl J. Three-dimensional printed surgical templates for fresh cadaveric osteochondral allograft surgery with dimension verification by multivariate computed tomography analysis. Knee. 2019;26(4):923–932. doi: 10.1016/j.knee.2019.05.007. [DOI] [PubMed] [Google Scholar]
- 148.Srivastava A., Lee G.Y., Steklov N., Colwell C.W., Jr., Ezzet K.A., D'Lima D.D. Effect of tibial component varus on wear in total knee arthroplasty. Knee. 2012;19(5):560–563. doi: 10.1016/j.knee.2011.11.003. [DOI] [PubMed] [Google Scholar]
- 149.Porter M.L., Gambhir A.K., Pradhan N. Image-guided surgery for total knee replacement. J Bone Joint Surg Am. 2004;86(5):1096. doi: 10.2106/00004623-200405000-00033. ; author reply 96-7. [DOI] [PubMed] [Google Scholar]
- 150.Sakai T. Patient-specific surgical guide for total hip arthroplasty. Adv Exp Med Biol. 2018;1093:307–314. doi: 10.1007/978-981-13-1396-7_23. [DOI] [PubMed] [Google Scholar]
- 151.Ng C.T.J., Newman S., Harris S., Clarke S., Cobb J. Patient-specific instrumentation improves alignment of lateral unicompartmental knee replacements by novice surgeons. Int Orthop. 2017;41(7):1379–1385. doi: 10.1007/s00264-017-3468-4. [DOI] [PubMed] [Google Scholar]
- 152.Qiu B., Liu F., Tang B., Deng B., Liu F., Zhu W., et al. Clinical study of 3D imaging and 3D printing technique for patient-specific instrumentation in total knee arthroplasty. J Knee Surg. 2017;30(8):822–828. doi: 10.1055/s-0036-1597980. [DOI] [PubMed] [Google Scholar]
- 153.Tibesku C.O. [Total knee arthroplasty with the use of patient specific instruments. The VISIONAIRE system] Orthopä. 2016;45(4):286–293. doi: 10.1007/s00132-016-3239-8. [DOI] [PubMed] [Google Scholar]
- 154.Gauci M.O., Boileau P., Baba M., Chaoui J., Walch G. Patient-specific glenoid guides provide accuracy and reproducibility in total shoulder arthroplasty. Bone Joint J. 2016;98-b(8):1080–1085. doi: 10.1302/0301-620X.98B8.37257. [DOI] [PubMed] [Google Scholar]
- 155.Shi Q., Sun D. Efficacy and safety of a novel personalized navigation template in proximal femoral corrective osteotomy for the treatment of DDH. J Orthop Surg Res. 2020;15(1):317. doi: 10.1186/s13018-020-01843-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Zheng P., Xu P., Yao Q., Tang K., Lou Y. 3D-printed navigation template in proximal femoral osteotomy for older children with developmental dysplasia of the hip. Sci Rep. 2017;7:44993. doi: 10.1038/srep44993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Zhou Y., Kang X., Li C., Xu X., Li R., Wang J., et al. Application of a 3-dimensional printed navigation template in Bernese periacetabular osteotomies: a cadaveric study. Medicine. 2016;95(50) doi: 10.1097/MD.0000000000005557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Wang X., Liu S., Peng J., Zhu Z., Zhang L., Guan J., et al. Development of a novel customized cutting and rotating template for Bernese periacetabular osteotomy. J Orthop Surg Res. 2019;14(1):217. doi: 10.1186/s13018-019-1267-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Schneider A.K., Pierrepont J.W., Hawdon G., McMahon S. Clinical accuracy of a patient-specific femoral osteotomy guide in minimally-invasive posterior hip arthroplasty. Hip Int : J Clin Exp Res hip Pathol Ther. 2018;28(6):636–641. doi: 10.1177/1120700018755691. [DOI] [PubMed] [Google Scholar]
- 160.Zheng P., Yao Q., Xu P., Wang L. Application of computer-aided design and 3D-printed navigation template in Locking Compression Pediatric Hip Plate(ΤΜ) placement for pediatric hip disease. Int J Comput Assist Radiol Surg. 2017;12(5):865–871. doi: 10.1007/s11548-017-1535-3. [DOI] [PubMed] [Google Scholar]
- 161.Krämer M., Kahrs L.A., Friese K.I., von Falck C., Hurschler C. Inter- and intra-operator reliability in patient-specific template positioning for total hip arthroplasty. A cadaver study. Int J Med Robot + Comput Assist Surg : MRCAS. 2018;14(2) doi: 10.1002/rcs.1887. [DOI] [PubMed] [Google Scholar]
- 162.Yan L., Wang P., Zhou H. 3D printing navigation template used in total hip arthroplasty for developmental dysplasia of the hip. Indian J Orthop. 2020;54(6):856–862. doi: 10.1007/s43465-020-00093-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Tu Q., Ding H.W., Chen H., Shen J.J., Miao Q.J., Liu B., et al. Preliminary application of 3D-printed individualised guiding templates for total hip arthroplasty in Crowe type IV developmental dysplasia of the hip. Hip Int : J Clin Exp Res hip Pathol Ther. 2020 doi: 10.1177/1120700020948006. 1120700020948006. [DOI] [PubMed] [Google Scholar]
- 164.Liang J., Zhao Y., Gao X., Fang X., Xu Y., Lu S. Design of custom-made navigational template of femoral head and pilot research in total hip resurfacing arthroplasty. BMC Surg. 2020;20(1):144. doi: 10.1186/s12893-020-00807-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Du H., Tian X.X., Li T.S., Yang J.S., Li K.H., Pei G.X., et al. Use of patient-specific templates in hip resurfacing arthroplasty: experience from sixteen cases. Int Orthop. 2013;37(5):777–782. doi: 10.1007/s00264-013-1842-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Hafez M.A., Chelule K.L., Seedhom B.B., Sherman K.P. Computer-assisted total knee arthroplasty using patient-specific templating. Clin Orthop Relat Res. 2006;444:184–192. doi: 10.1097/01.blo.0000201148.06454.ef. [DOI] [PubMed] [Google Scholar]
- 167.Gemalmaz H.C., Sarıyılmaz K., Ozkunt O., Sungur M., Kaya I., Dikici F. Postoperative mechanical alignment analysis of total knee replacement patients operated with 3D printed patient specific instruments: a Prospective Cohort Study. Acta Orthop Traumatol Turcica. 2019;53(5):323–328. doi: 10.1016/j.aott.2019.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Köster G., Biró C. [Total and unicompartmental knee replacement. Patient-specific Instrumentation] Orthopä. 2016;45(4):302–313. doi: 10.1007/s00132-016-3245-x. [DOI] [PubMed] [Google Scholar]
- 169.Gu F., Li L., Zhang H., Li X., Ling C., Wang L., et al. Three-dimensional-printed guiding template for unicompartmental knee arthroplasty. BioMed Res Int. 2020;2020:7019794. doi: 10.1155/2020/7019794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Huang A.B., Qi Y.S., Song C.H., Zhang J.Y., Yang Y.Q., Yu J.K. Novel customized template designing for patellar resurfacing in total knee arthroplasty. J Orthop Res : Off Publ Orthopaed Res Soc. 2016;34(10):1798–1803. doi: 10.1002/jor.23200. [DOI] [PubMed] [Google Scholar]
- 171.Jaffry Z., Masjedi M., Clarke S., Harris S., Karia M., Andrews B., et al. Unicompartmental knee arthroplasties: robot vs. patient specific instrumentation. Knee. 2014;21(2):428–434. doi: 10.1016/j.knee.2013.11.017. [DOI] [PubMed] [Google Scholar]
- 172.Faldini C., Mazzotti A., Belvedere C., Durastanti G., Panciera A., Geraci G., et al. A new ligament-compatible patient-specific 3D-printed implant and instrumentation for total ankle arthroplasty: from biomechanical studies to clinical cases. J Orthop Traumatol : Off J Ital Soc Orthopaed Traumatol. 2020;21(1):16. doi: 10.1186/s10195-020-00555-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Dimitriou D., Cheng R., Yang Y., Baumgaertner B., Helmy N., Tsai T.Y. High variability in anterior cruciate ligament femoral footprint: implications for anatomical anterior cruciate ligament reconstruction. Knee. 2021;30:141–147. doi: 10.1016/j.knee.2021.01.015. [DOI] [PubMed] [Google Scholar]
- 174.Liu D., Li Y., Li T., Yu Y., Cai G., Yang G., et al. The use of a 3D-printed individualized navigation template to assist in the anatomical reconstruction surgery of the anterior cruciate ligament. Ann Transl Med. 2020;8(24):1656. doi: 10.21037/atm-20-7515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Wu Q., Yu T., Lei B., Huang W., Huang R. A new individualized three-dimensional printed template for lateral ankle ligament reconstruction. Med Sci Mon Int Med J Exp Clin Res : Int Med J Exp Clin Res. 2020;26 doi: 10.12659/MSM.922925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Moreta-Martinez R., Pose-Díez-de-la-Lastra A., Calvo-Haro J.A., Mediavilla-Santos L., Pérez-Mañanes R., Pascau J. Combining augmented reality and 3D printing to improve surgical workflows in orthopedic oncology: smartphone application and clinical evaluation. Sensors. 2021;21(4) doi: 10.3390/s21041370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Schulze M., Gosheger G., Bockholt S., De Vaal M., Budny T., Tönnemann M., et al. Complex bone tumors of the trunk-the role of 3D printing and navigation in tumor orthopedics: a case series and review of the literature. J Personalized Med. 2021;11(6) doi: 10.3390/jpm11060517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Ma L., Zhou Y., Zhu Y., Lin Z., Wang Y., Zhang Y., et al. 3D-printed guiding templates for improved osteosarcoma resection. Sci Rep. 2016;6:23335. doi: 10.1038/srep23335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Lin C.L., Fang J.J., Lin R.M. Resection of giant invasive sacral schwannoma using image-based customized osteotomy tools. Eur Spine J : Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sec Cerv Spine Res Soc. 2016;25(12):4103–4107. doi: 10.1007/s00586-016-4782-z. [DOI] [PubMed] [Google Scholar]
- 180.McCulloch R.A., Frisoni T., Kurunskal V., Maria Donati D., Jeys L. Computer navigation and 3D printing in the surgical management of bone sarcoma. Cells. 2021;10(2) doi: 10.3390/cells10020195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Sallent A., Vicente M., Reverté M.M., Lopez A., Rodríguez-Baeza A., Pérez-Domínguez M., et al. How 3D patient-specific instruments improve accuracy of pelvic bone tumour resection in a cadaveric study. Bone Joint Res. 2017;6(10):577–583. doi: 10.1302/2046-3758.610.BJR-2017-0094.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Evrard R., Schubert T., Paul L., Docquier P.L. Resection margins obtained with patient-specific instruments for resecting primary pelvic bone sarcomas: a case-control study. Orthopaed Traumatol Surg Res : OTSR. 2019;105(4):781–787. doi: 10.1016/j.otsr.2018.12.016. [DOI] [PubMed] [Google Scholar]
- 183.Liu X., Liu Y., Lu W., Liao S., Du Q., Deng Z., et al. Combined application of modified three-dimensional printed anatomic templates and customized cutting blocks in pelvic reconstruction after pelvic tumor resection. J Arthroplasty. 2019;34(2):338–345. doi: 10.1016/j.arth.2018.10.001. e1. [DOI] [PubMed] [Google Scholar]
- 184.Wang H., Su K., Su L., Liang P., Ji P., Wang C. Comparison of 3D-printed porous tantalum and titanium scaffolds on osteointegration and osteogenesis. Mater Sci Eng C, Mater Biol Appl. 2019;104:109908. doi: 10.1016/j.msec.2019.109908. [DOI] [PubMed] [Google Scholar]
- 185.Marei H.F., Alshaia A., Alarifi S., Almasoud N., Abdelhady A. Effect of steam heat sterilization on the accuracy of 3D printed surgical guides. Implant Dent. 2019;28(4):372–377. doi: 10.1097/ID.0000000000000908. [DOI] [PubMed] [Google Scholar]