Abstract
Background:
Multiple surgical techniques for fixation of Neer type IIB distal clavicle fractures have been described without consensus on optimal treatment. The purpose of this study is to compare functional and radiographic results with surgical management of Neer type IIB distal clavicle fractures at a single institution.
Methods:
Sixty-three patients with acute Neer type IIB fractures treated operatively were evaluated. Patients with a minimum of two year follow up were included. Functional scores included American Shoulder and Elbow Surgeons (ASES), Single Assessment Numeric Evaluation (SANE), Simple Shoulder Test (SST), and Likert patient satisfaction (1 to 5). Radiographs were assessed for osseous union and coracoclavicular (CC) distance.
Results:
Thirty-eight patients met inclusion with a mean follow-up of 5.3 years. Patients were divided into five groups based on fixation technique: suture-only CC fixation (n=6), CC screw fixation only (n=3), open reduction internal fixation (ORIF) without CC fixation (n=8), hook plate fixation (n=4), and ORIF with suture CC reconstruction (n=17). Outcome scores for the entire cohort were 91.8 for ASES, 90.2 for SANE, and 10.8 for STT. Patients with hook plates had significantly lower SANE score (p=0.016), but no other significant differences in functional, satisfaction, or radiographic outcomes were found between groups. Sixteen patients (42.1%) required reoperation.
Conclusion:
Treatment of Neer type IIB fractures via suture- only fixation, plate-only fixation, or a combination of both demonstrated satisfactory mid to long term outcomes. While implant removal was more common in the CC screw and ORIF groups, no fixation technique proved functionally superior.
Key Words: Clavicle fracture, Neer IIB distal clavicle fracture, Acromioclavicular separation, Hook plate, Locking plate, Bosworth screw, Suture repair
Introduction
Distal clavicle fractures account for approximately 15-25% of all clavicular fractures (1,2). Neer classified distal clavicle fractures into types I through III (3). Craig further modified Neer’s classification by subdividing type 2 clavicle fractures into type IIA and type IIB depending on the competence of the conoid ligament which helps to maintain coracoclavicular (CC) stability (4).
Even among Neer IIB fractures, two patterns may exist. The fracture line of the clavicle may occur between the coracoclavicular ligaments or lateral to both torn ligaments. Neer IIB fractures managed conservatively are at risk for developing nonunion due to deforming forces (5). Previous studies demonstrated that patients treated nonoperatively had higher incidences of nonunion and residual shoulder dysfunction than those treated by open reduction and internal fixation (1,5).
Despite the general agreement that displaced Neer IIB fractures should be treated operatively, no consensus on the optimal fixation technique exists (1,2). The technical challenges with repair include an often small and comminuted distal fracture fragment as well as the potential need for reconstruction of the coracoclavicular (CC) ligament disruption. Described techniques include suture fixation, plate and screw osteosynthesis alone, hook plating, plating with CC ligament reconstruction, and CC screw fixation (Bosworth screw) (6,7,16,17,8–15). The combination of plate osteosynthesis with CC ligament augmentation is thought to give superior stability and promote better fracture healing (17). However, studies have not shown a biomechanical advantage to using such CC ligament augmentation (18–20). Hook plates, alternatively, have good clinical results and non-union rates, but often require a second surgery and may cause subacromial impingement and acromial erosion (21,22).
Many studies have compared surgical techniques in the setting of Neer type IIB distal clavicle fractures but mostly in small cohorts comparing only two different techniques (23,24). The purpose of this study is to evaluate the radiographic and functional outcomes of patients with type IIB distal clavicle fractures and compare various fixation techniques and their complication rates. We hypothesize that fractures treated via any technique will result in good and similar outcomes.
Materials and Methods
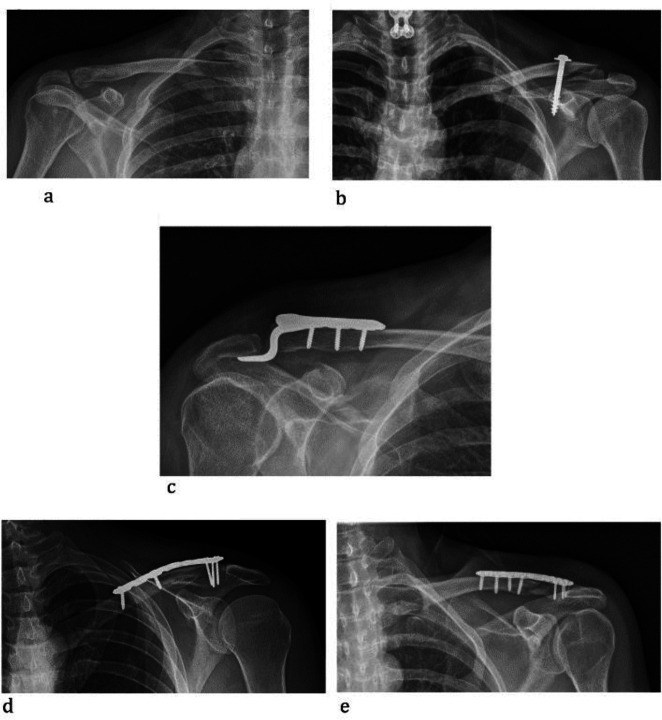
This retrospective study was performed at a single institution and included all patients treated surgically for Neer type IIB distal clavicle fractures between July 2006 and November 2017. Patients were treated by one of ten fellowship-trained shoulder and elbow or trauma surgeons. Institutional review board (IRB) approval was obtained. Patients with clavicle fractures and acromioclavicular disruptions were identified through querying Current Procedural Terminology (CPT codes 23515; 23550; 23552), yielding 905 patients. Inclusion criteria required patients to have acute Neer type IIB distal clavicle fractures (within 8 weeks of injury). Exclusion criteria included patients younger than 18 years of age, patients treated non-operatively, other distal clavicle fracture types, isolated acromioclavicular injuries, or other ipsilateral shoulder surgery. Diagnosis of acute Neer type IIB distal clavicle fractures was made via review of preoperative clinical note and radiographs. Operative reports and postoperative radiographs were reviewed to identify the surgical method performed by each surgeon. To assess outcomes, patients were divided into five groups based on surgical technique: only suture or TightRope (Arthrex, Naples, FL) fixation [suture-only, figure 1a], Bosworth screw fixation [CC screw, figure 1b], open reduction internal fixation with hook plate [hook plate, figure 1c], open reduction internal fixation with locking plate [ORIF-only, figure 1d], and plate ORIF with CC ligament reconstruction [ORIF+CC, figure 1e].
Figure 1.
a: Suture Fixation, b: Bosworth screw fixation, c: Open reduction internal fixation with hook plate, d: Open reduction internal fixation with locking plate, e: Open reduction internal fixation with locking plate in conjunction with CC ligament reconstruction
All patients were contacted for functional scores, complications, and revision surgeries via REDCap surveys (25). The survey was composed of American Shoulder and Elbow Surgeons (ASES), Single Assessment Numeric Evaluation (SANE), Simple Shoulder Test (SST) surveys, along with a Likert-scaled satisfaction survey ranging between 1-5 (1= very unsatisfied and 5= very satisfied).
Radiographic assessment was performed on all patients using preoperative, immediate postoperative, and most recent radiographs (at a minimum of 3 months postoperatively). The CC distance was measured on both preoperative and final postoperative radiographs. Radiographs were also assessed for any evidence of nonunion, loss of reduction, and implant complications. Reviewers were blinded to the patient’s current shoulder functional scores.
Non-parametric tests were performed to evaluate differences between groups due to the smaller sample size and non-normal distribution of our data. Kruskal-Wallis test was performed to assess the differences in demographics, functional scores, and CC measurements. Spearman’s correlational analysis was utilized to examine the relationship between functional scores and CC measurements. All statistical analysis was executed on Statistical Package for the Social Science (SPSS) version 26 (IBM Corp., Armonk, NY). Statistical significance was defined as p <0.05.
Results
Patient Selection
Sixty-three patients met initial criteria for inclusion. 38 patients completed surveys at a mean follow-up of 5.3 years (range 2-13 years); four patients were deceased, 15 could not be reached, and 6 refused to participate. The patients had an average age of 48.2 years (range: 27-73) and were composed of 26 (68.4%) males and 12 (31.6%) females. Patients received treatment via five different surgical techniques: suture-only (n=6), CC screw (n=3), hook plate (n=4), ORIF-only (n=8) and ORIF+CC (n=17).
Functional Assessment
There were no differences in postoperative functional outcomes or patient satisfaction based on the repair method. Neither age, body mass index (BMI), preoperative CC distance, postoperative CC distance, nor differences between preoperative and postoperative CC interval affected functional outcomes in any of the groups [Table 1 and 2].
Table 1.
Comparison of functional scores and coracoclavicular distance based on method of fracture fixation
| Suture-only (n=6) | CC screw (n=3) | Hook plate (n=4) | ORIF-only (n=8) | ORIF+CC (n=17) | p-value | |
|---|---|---|---|---|---|---|
| Gender | 4M, 2F | 2M, 1F | 2M, 2F | 7M, 1F | 11M, 6F | --- |
| Age (years) | 42.8 ± 12.0 | 56.0 ± 13.9 | 56.3 ± 7.2 | 47.0 ± 16.7 | 47.3 ± 12.8 | 0.531 |
| Body Mass Index | 23.4 ± 1.5 | 26.9 ± 2.5 | 24.0 ± 4.7 | 25.3 ± 4.7 | 24.2 ± 2.5 | 0.701 |
| Preoperative CC Interval | 31.6 ± 6.1 | 28.4 ± 6.9 | 21.1 ± 5.5 | 30.0 ± 16.5 | 26.6 ± 5.8 | 0.368 |
| Postoperative CC Interval | 13.6 ± 4.0 | 22.1 ± 12.2 | 10.5 ± 4.2 | 15.7 ± 5.1 | 13.1 ± 4.8 | 0.430 |
| Difference CC Interval | 16.7 ± 7.0 | 6.3 ± 5.4 | 10.7 ± 1.4 | 13.2 ± 18.8 | 14.8 ± 5.3 | 0.258 |
| Postoperative ASES | 93.0 ± 5.2 | 84.3 ± 15.8 | 89.9 ± 7.8 | 93.9 ± 8.8 | 92.2 ± 12.4 | 0.587 |
| Postoperative SANE | 96.0 ± 4.2 | 86.7 ± 10.4 | 80.5 ± 8.0 | 95.4 ± 7.2 | 89.0 ± 12.5 | 0.036 |
| Postoperative SST | 11.0 ± 1.1 | 10.0 ± 2.0 | 9.2 ± 1.5 | 11.4 ± 1.1 | 11.0 ± 1.8 | 0.111 |
| Postoperative VAS | 1.2 ± 1.2 | 1.7 ± 1.7 | 1.0 ± 1.2 | 0.8 ± 1.5 | 0.8 ± 1.4 | 0.629 |
| Satisfaction | 4.7 ± 0.5 | 3.3 ± 2.1 | 4.5 ± 0.6 | 5.0 ± 0.0 | 4.5 ± 0.8 | 0.228 |
| Hardware removal | 0 (0%) | 3 (100%) | 4 (100%) | 1 (12.5%) | 7 (41.2%) | --- |
* ORIF-only= Open reduction internal fixation with locking plate without CC fixation; ORIF+CC= Open Reduction Internal fixation with CC ligament reconstruction; CC interval= Coracoclavicular interval; ASES=American Shoulder and Elbow Score; SANE=Single Assessment Numeric Evaluation; SST=Simple Shoulder Test Score; VAS=Visual Analog Score for pain
Table 2.
Correlation between coracoclavicular interval measurements and post-operative functional scores
| Preoperative CC Interval | Postoperative CC Interval | Delta CC Interval | ||||
|---|---|---|---|---|---|---|
| Mean: 27.6 + 8.9 | Mean: 14.0 + 5.3 | Mean: 13.5 + 9.6 | ||||
| Spearman's rho | p-value | Spearman's rho | p-value | Spearman's rho | p-value | |
| Postoperative ASES | 0.128 | 0.551 | 0.171 | 0.318 | 0.026 | 0.906 |
| Postoperative SANE | 0.265 | 0.233 | 0.110 | 0.543 | 0.130 | 0.564 |
| Postoperative SST | 0.060 | 0.728 | 0.098 | 0.568 | 0.134 | 0.532 |
| Postoperative VAS | -0.119 | 0.579 | -0.299 | 0.077 | -0.016 | 0.941 |
| Satisfaction | 0.070 | 0.745 | -0.141 | 0.421 | 0.179 | 0.403 |
| Complications | -0.073 | 0.735 | 0.293 | 0.083 | -0.355 | 0.089 |
* CC interval= Coracoclavicular interval; ASES=American Shoulder and Elbow Score; SANE=Single Assessment Numeric Evaluation; SST=Simple Shoulder Test Score; VAS=Visual Analog Score for pain
For the entire cohort, the mean ASES, SANE, and SST scores were 91.8, 90.2, and 10.8, respectively. Overall satisfaction was rated 4.5 out of 5. No observable differences were noted in shoulder pain or functional scores with VAS pain (p=0.629), ASES (p=0.587), SST(p=0.111) or shoulder satisfaction (p=0.228) between the different fixation techniques. ORIF-only patients had significantly higher SANE scores than hook plate patients (p=0.016). All patients reported a neutral to very satisfied rating for surgical satisfaction (70% were very satisfied). Only one patient who had a screw fixation had below neutral satisfaction.
Reoperation and Complications
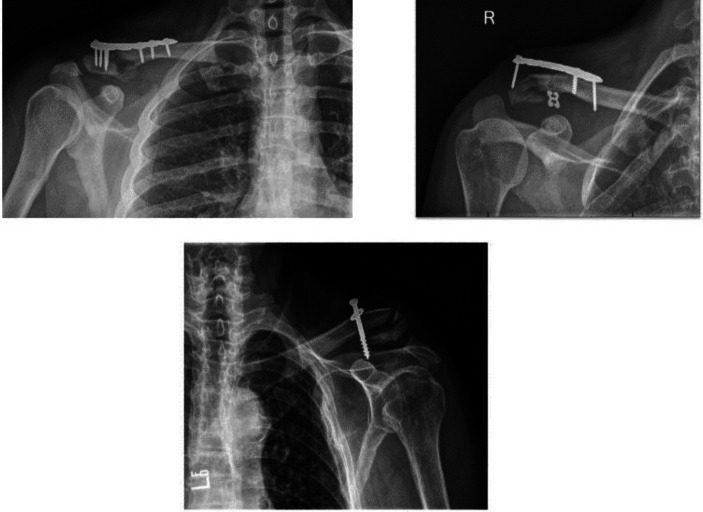
Three patients (7.9%) had overt fixation failure with two requiring revision surgery. The first patient was initially treated via ORIF-only, and developed implant failure secondary to screw loosening [Figure 2a]. The patient underwent revision surgery with ORIF with locking plate and CC suture reconstruction fixation and no further intervention was necessary. The second patient was initially treated with ORIF+CC and experienced fixation failure requiring revision surgery [Figure 2b]. Subsequently, the patient experienced a prominent implant with risk of skin protrusion following the revision surgery. The implant was removed and the patient remained with a nonunion. The third patient had failure of a Bosworth screw secondary to loosening from the coracoid. The screw was removed 2.5 months after surgery and the patient developed a nonunion [Figure 2c]. There were no fixation failures in suture-only patients.
Figure 2.
a: Failure of ORIF with locking plate, b: ORIF+CC fixation failure with nonunion, c: Fixation failure of Bosworth Screw with nonunion
The incidence of reoperation for any indication was highest in CC screw and hook plate (100%) patients and lowest in suture-only patients (0%) [Table 1]. The rate of plate removal in ORIF-only was 1/8 (12.5%) compared to 4/4 (100%) in hook plates. The rate of plate removal in patients with ORIF-only (1/8, 12.5%) and those with ORIF+CC (7/17, 41.2%) were not significantly different (p=0.205). Lastly, acromial erosion occurred in 2/4 (50%) hook plates. Both patients did not experience any clinical signs of acromial erosion.
Six patients noted residual functional limitations that persisted after surgery. Of the two patients with CC screws, one patient had continued weakness and limited range of motion (ROM); the other patient noted residual pain only. One patient with ORIF locking plate complained of weakness and an inability to carry heavy boxes. Of those patients who underwent ORIF+CC, one noted pain when wearing a seatbelt, one had weakness during pushups, and one complained of stiffness and limited ROM.
Bone Healing Assessment
Based on clinical and radiographic evidence, 33 patients (86.8%) achieved osseous union within 12 weeks. Three patients experienced delayed union, and two experienced non-union (5.3%). Nonunions occurred in one CC screw patient [Figure 2c] one ORIF+CC patient [Figure 2b]. No patients developed infections.
Discussion
Most orthopedic surgeons agree that Neer IIB distal clavicle fractures require surgical management; however, the preferred fixation technique is debated (2,24,26). Overall, we found that surgical fixation, regardless of technique, restored function well and resulted in high satisfaction rates. While only 6 of our patients were treated with suture fixation alone, this treatment method achieved the highest mean SANE score. While definitive conclusions are difficult to make based on this retrospective study, fixation of Neer IIB distal clavicle fractures with a CC suture reconstruction technique appears to produce similar functional results to other modes of fixation. Patients who received fracture management via suture fixation only were the only cohort to not require any subsequent operations. This may lessen the need for additional recovery and also minimize additional costs (6–8,26). Further studies are warranted to determine if there is a significant benefit to this surgical approach.
Previous studies have attempted to analyze outcomes comparing distal clavicle fracture management via suture fixation compared to plate osteosynthesis. Chen et al. compared suture fixation to hook plates and found that patients in both groups had comparable functional outcomes. The group treated via suture fixation, however, had significantly less intra-operative blood loss and operation time due to the smaller incision required for treatment (27). In addition, all patients with hook plates required reoperation for implant removal compared to none in the suture fixation group. The implications of a second operation cannot be overstated, as it puts patients at higher risk for complications in an area known for wound issues and adds substantial costs. Fox et al. performed a systematic review to compare the cost-effectiveness of suture button, locking plate, and hook plate for Neer Type II distal clavicle fractures (26). The results demonstrated comparable functional outcomes between the groups, though suture button was the most cost-effective due to the decreased need for subsequent surgery.
In our cohort, 3 patients underwent treatment via Bosworth screw between 2008 to 2010. This treatment method has fallen out of favor with surgeons at our institution due to the requirement for screw removal and the evolution of precontoured plates which provide improved fracture fixation (6–8). Similarly, although still used in certain situations, the use of hook plates has declined in our practice for similar concerns.
The most common treatment method amongst our surgeons was the combination of distal clavicle plate osteosynthesis with CC ligament reconstruction via suture fixation. The screws are able to provide direct fragment compression and fixation, while CC ligament augmentation reduces the vertical forces applied to the plate at the fracture interface (11,28). Furthermore, biomechanical studies have shown that the combination of a locking plate with CC ligament augmentation can provide better fracture stability than either treatment method alone (20). Many believe that the reduction of plate loading results in a decreased rate of fracture nonunion than using the locking plate alone (20). In situations when the plate is unable to achieve good fixation via screw fixation, CC ligament augmentation via suture or tightrope has been shown to provide stability preventing the potential for nonunion (18,29).
Despite being the most popular contemporary option, plate osteosynthesis with CC ligament augmentation did not yield superior long-term outcomes in this study. Interestingly, the combination of plate osteosynthesis with CC ligament augmentation provides comparable functional outcomes to either suture or plate fixation alone [Table 1]. While not significant (p=0.205), patients who received the combination of ORIF and CC ligament trended towards higher implant removal rates than ORIF without CC ligament reconstruction (12.5% vs 41.2%). Additionally, the difference between preoperative CC interval and postoperative CC interval was nearly identical with or without CC ligament augmentation.
In the literature, locking plates are advantageous since the implant removal rate is only 19.8% compared to 92.5% in patients with hook plates (26). As mentioned, 100% of hook plates were removed while only 32% of locking plates with and without suture fixation were removed. Additionally, locking plates achieve nearly identical functional outcomes as hook plates with fewer potential complications (26,30). In our study, patients with locking plates had the highest average functional and satisfaction score with statistically significant higher SANE scores. This has unclear implications given the small sample size, but there is potential for long term effects from hook plating such as acromion osteolysis which was seen in 2 of the 4 patients with hook plate fixation [Figure 3]. In addition, the lower reoperation rates favor the use of locking plates over hook plates.
This study is not without its limitations. First, this study is retrospective and is prone to inherent selection bias. An example of this would be if a surgeon treated patients with better intraoperative bone quality with ORIF alone versus supplementing with a hook plate or CC reconstruction to improve stability. Furthermore, the individual cohorts within this study were small and there was not an equal number of patients treated within each group. With a larger sample size, more statistical significance may have been deduced. Our cohort also lacks preoperative functional scores, and no baseline level of function is known. Finally, a high number of patients were lost due to inadequate follow-up. However, despite the loss of follow up, this is the largest study to date analyzing outcomes in patients with type IIB distal clavicle fractures comparing more than two surgical methods. In the future, large prospective studies will be needed to properly assess the most advantageous treatment method.
Treatment of Neer Type IIB fractures via suture fixation, plate fixation, or the combination of plate osteosynthesis with suture fixation demonstrated excellent functional outcomes and satisfaction at least two years postoperatively. Equivalent functional outcomes and a low reoperation rate make the suture-only CC reconstruction a viable option compared to more traditional plate and screw constructs for Neer IIB distal clavicle fractures.Conflict of interests: The authors declare that there are no competing interests.
Conflicts of Interest and Source of Funding
The authors and any research foundation with which they are affiliated did not receive any financial payments or other benefits from any commercial entity related to the subject of this article. There are no relevant disclosures. All authors significantly contributed to the document and have reviewed the final manuscript.
References
- 1.Edwards DJ, Kavanagh TG, Flannery MC. Fractures of the distal clavicle: a case for fixation. Injury. 1992;23(1):44–46. doi: 10.1016/0020-1383(92)90125-c. [DOI] [PubMed] [Google Scholar]
- 2.Van der Meijden OA, Gaskill TR, Millett PJ. Treatment of clavicle fractures: Current concepts review. J Shoulder Elbow Surg. 2012;21(3):423–429. doi: 10.1016/j.jse.2011.08.053. [DOI] [PubMed] [Google Scholar]
- 3.Neer CS. Fractures of the distal third of the clavicle. Clin Orthop Relat Res. 1968;58:43–50. [PubMed] [Google Scholar]
- 4.Craig EV. Fractures of the clavicle. In: Rockwood CA Jr, Matsen FA 3rd., editors. The Shoulder. Philadelphia: WB Saunders; 1990. pp. 367–412. [Google Scholar]
- 5.Oh JH, Kim SH, Lee JH, Shin SH, Gong HS. Treatment of distal clavicle fracture: a systematic review of treatment. Arch Orthop Trauma Surg. 2011;131(4):525–533. doi: 10.1007/s00402-010-1196-y. [DOI] [PubMed] [Google Scholar]
- 6.Macheras G, Kateros KT, Savvidou OD, Sofianos J, Fawzy EA, Papagelopoulos PJ. Coracoclavicular screw fixation for unstable distal clavicle fractures. Orthopedics. 2005;28(7):693–696. doi: 10.3928/0147-7447-20050701-18. [DOI] [PubMed] [Google Scholar]
- 7.Jin CZ, Kim HK, Min BH. Surgical treatment for distal clavicle fracture associated with coracoclavicular ligament rupture using a cannulated screw fixation technique. J Trauma. 2006;60(6):1358–1361. doi: 10.1097/01.ta.0000220385.34197.f9. [DOI] [PubMed] [Google Scholar]
- 8.Tiefenboeck TM, Popp D, Boesmueller S, Payr S, Joestl J, Komjati M, et al. Acromioclavicular joint dislocation treated with Bosworth screw and additional K-wiring: Results after 7 8 years - Still an adequate procedure? BMC Musculoskelet Disord . 2017;18:339. doi: 10.1186/s12891-017-1692-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cisneros LN, Reiriz JS. Management of unstable distal third clavicle fractures: clinical and radiological outcomes of the arthroscopy-assisted conoid ligament reconstruction and fracture cerclage with sutures. Eur J Orthop Surg Traumatol. 2017;27(3):373–380. doi: 10.1007/s00590-017-1925-9. [DOI] [PubMed] [Google Scholar]
- 10.Daglar B, Delialioglu OM, Minareci E, Tasbas BA, Bayrakci K, Gunel U. An alternative fixation method for the treatment of unstable distal clavicle fractures: Locked distal radius plate. Acta Orthop Traumatol Turc. 2009;43(4):324–330. doi: 10.3944/AOTT.2009.324. [DOI] [PubMed] [Google Scholar]
- 11.Lee SK, Lee JW, Song DG, Choy WS. Precontoured locking plate fixation for displaced lateral clavicle fractures. Orthopedics. 2013;36(6):801–807. doi: 10.3928/01477447-20130523-28. [DOI] [PubMed] [Google Scholar]
- 12.Renger RJ, Roukema GR, Reurings JC, Raams PM, Font J, Verleisdonk EJMM. The clavicle hook plate for Neer type II lateral clavicle fractures. J Orthop Trauma. 2009;23(8):570–574. doi: 10.1097/BOT.0b013e318193d878. [DOI] [PubMed] [Google Scholar]
- 13.Kirsch JM, Blum L, Hake ME. Distal Clavicle Fractures: Open Reduction and Internal Fixation With a Hook Plate. J Orthop Trauma. 2018;32 Suppl 1:S2–S3. doi: 10.1097/BOT.0000000000001214. [DOI] [PubMed] [Google Scholar]
- 14.Muramatsu K, Shigetomi M, Matsunaga T, Murata Y, Taguchi T. Use of the AO hook-plate for treatment of unstable fractures of the distal clavicle. Arch Orthop Trauma Surg. 2007;127(3):191–194. doi: 10.1007/s00402-006-0284-5. [DOI] [PubMed] [Google Scholar]
- 15.Han L, Hu Y, Quan R, Fang W, Jin B, Huang L. Treatment of Neer IIb Distal Clavicle Fractures Using Anatomical Locked Plate Fixation With Coracoclavicular Ligament Augmentation. J Hand Surg Am. 2017;42(12):1036.e1–1036. doi: 10.1016/j.jhsa.2017.08.005. [DOI] [PubMed] [Google Scholar]
- 16.Herrmann S, Schmidmaier G, Greiner S. Stabilisation of vertical unstable distal clavicular fractures (Neer 2b) using locking T-plates and suture anchors. Injury. 2009;40(3):236–239. doi: 10.1016/j.injury.2008.07.021. [DOI] [PubMed] [Google Scholar]
- 17.Johnston PS, Sears BW, Lazarus MR, Frieman BG. Fixation of unstable type II clavicle fractures with distal clavicle plate and suture button. 2014;28(11):e269–272. doi: 10.1097/BOT.0000000000000081. [DOI] [PubMed] [Google Scholar]
- 18.Madsen W, Yaseen Z, Lafrance R, Chen T, Awad H, Maloney M, et al. Addition of a suture anchor for coracoclavicular fixation to a superior locking plate improves stability of type IIB distal clavicle fractures. Arthroscopy. 2013;29(6):998–1004. doi: 10.1016/j.arthro.2013.02.024. [DOI] [PubMed] [Google Scholar]
- 19.Bishop JY, Roesch M, Lewis B, Jones GL, Litsky AS. A biomechanical comparison of distal clavicle fracture reconstructive techniques. Am J Orthop (Belle Mead NJ). 2013;42(3):114–118. [PubMed] [Google Scholar]
- 20.Rieser GR, Edwards K, Gould GC, Markert RJ, Goswami T, Rubino LJ. Distal-third clavicle fracture fixation: A biomechanical evaluation of fixation. J Shoulder Elbow Surg. 2013;22(6):848–855. doi: 10.1016/j.jse.2012.08.022. [DOI] [PubMed] [Google Scholar]
- 21.Charity RM, Haidar SG, Ghosh S, Tillu AB. Fixation failure of the clavicular hook plate: a report of three cases. J Orthop Surg (Hong Kong). 2006;14(3):333–335. doi: 10.1177/230949900601400320. [DOI] [PubMed] [Google Scholar]
- 22.Klein SM, Badman BL, Keating CJ, Devinney DS, Frankle MA, Mighell MA. Results of surgical treatment for unstable distal clavicular fractures. J Shoulder Elbow Surg. 2010;19(7):1049–1055. doi: 10.1016/j.jse.2009.11.056. [DOI] [PubMed] [Google Scholar]
- 23.Shin SJ, Ko YW, Lee J, Park MG. Use of plate fixation without coracoclavicular ligament augmentation for unstable distal clavicle fractures. J Shoulder Elbow Surg. 2016;25(6):942–948. doi: 10.1016/j.jse.2015.10.016. [DOI] [PubMed] [Google Scholar]
- 24.Zhang C, Huang J, Luo Y, Sun H. Comparison of the efficacy of a distal clavicular locking plate versus a clavicular hook plate in the treatment of unstable distal clavicle fractures and a systematic literature review. Int Orthop. 2014;38(7):1461–1468. doi: 10.1007/s00264-014-2340-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)-A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fox HM, Ramsey DC, Thompson AR, Hoekstra CJ, Mirarchi AJ, Nazir OF. Neer Type-II Distal Clavicle Fractures: A Cost-Effectiveness Analysis of Fixation Techniques. J Bone Joint Surg Am. 2020;102(3):254–261. doi: 10.2106/JBJS.19.00590. [DOI] [PubMed] [Google Scholar]
- 27.Chen CY, Yang SW, Lin KY, Lin KC, Tarng YW, Renn JH, et al. Comparison of single coracoclavicular suture fixation and hook plate for the treatment of acute unstable distal clavicle fractures. J Orthop Surg Res. 2014;9:42. doi: 10.1186/1749-799X-9-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fleming MA, Dachs R, Maqungo S, du Plessis JP, Vrettos BC, Roche SJL. Angular stable fixation of displaced distal-third clavicle fractures with superior precontoured locking plates. J Shoulder Elbow Surg. 2015;24(5):700–704. doi: 10.1016/j.jse.2014.09.024. [DOI] [PubMed] [Google Scholar]
- 29.Boonard M, Sumanont S, Arirachakaran A, Sikarinkul E, Ratanapongpean P, Kanchanatawan W, et al. Fixation method for treatment of unstable distal clavicle fracture: systematic review and network meta-analysis. 2018;28(6):1065–1078. doi: 10.1007/s00590-018-2187-x. [DOI] [PubMed] [Google Scholar]
- 30.Singh A, Schultzel M, Fleming JF, Navarro RA. Complications after surgical treatment of distal clavicle fractures. Orthop Traumatol Surg Res. 2019;105(5):853–859. doi: 10.1016/j.otsr.2019.03.012. [DOI] [PubMed] [Google Scholar]