Abstract
Modern advances in techniques and implants have allowed for a better operative fixation for distal femoral fractures. Both locked plating and retromedullary nail have allowed surgeons to stabilize these fractures with minimal soft tissue dissection and preserve blood supply. Although both the implants have been used extensively for such types of fractures, the superiority of one implant over the other is still doubtful. Therefore, we conducted this meta-analysis to compare locked plating and retrograde intramedullary nailing in distal femoral fractures. Based on prisma guidelines, electronic databases, including PubMed, Embase, Scopus, and Ovid Medline were searched using a well-defined search strategy. Outcome measures which were studied included blood loss, implant failure, infection, knee range of motion, malunion, non-union, pain, surgical duration and union time Surgical duration (95% CI 2.90 to 17.13, p <0.01) and blood loss (95% CI 69.60 to123.18, p <0.01) favoured plating group and the difference is significant. But while analysing parameters like implant failure, knee range of motion, non-union and union time, our analysis favoured nailing group, but the difference is not significant. Overall, both locked plating and retrograde intramedullary nailing are comparable with respect to union and complications in distal femur fractures, but we need further larger and high quality randomized studies to evaluate the difference.
Key Words: Distal femur, Fracture, Locked plating, Retrograde nailing, Metaanalysis
Introduction
Distal femoral fractures account for around 1/20th of all the fractures involving femur (1). Non-operative treatment of these fractures is no longer in favor due to the higher chance of complications like malunion, non-union, and joint stiffness (2). Modern advances in techniques and implants have allowed for a better operative fixation for distal femoral fractures. Still, there is a debate regarding the optimal choice of implant for such fractures.
The use of implants like condylar blade plate in distal femoral fractures have resulted in high complications, and development of locking plates have allowed for a better fixation with improved outcome (3). Placement of condylar blade plate is technically demanding and requires 3-dimensional correction simultaneously. Incorrect placement of chisel and plate will lead to condylar malalignment (4).
The locked plating has allowed surgeons to stabilize these fractures with minimal soft tissue dissection and preserve blood supply. In addition, the construct is not dependent on the screw-bone interface and is less likely to fail than an unlocked plate, especially in osteoporotic bone and comminuted fractures (5).
The retrograde intramedullary nail has been used in distal femur fractures, especially with extra-articular involvement, with decent results and fewer complications (6,7). The use of such a nail can allow fracture fixation with limited soft tissue damage and preservation of fracture hematoma (5).
Several articles suggest that retrograde nailing can be done in intra articular fractures. Hieholzer et al did a comparative study on nailing versus plating for distal femur fractures. They performed nailing in type C1 intra articular fractures and showed better results (8). Neubauer et al did nailing in type C1 intra articular fractures and showed reliable results (9). Saumya et al did a comparative study on nailing versus plating for distal femur fractures where nailing was performed in type C1-C3 intra articular fractures (10). Garnavos et al did a prospective study on treating intra articular distal femur fractures with retrograde nailing and compression screws, facilitated early weight bearing without complications (11). Warner et al did a cohort study on treatment of complete intra articular fractures with retrograde nailing augmented with articular screws, showed favourable radiological and clinical outcomes. Warner et al also mentioned about the difficulties in nailing in complete articular fractures. Potential problems, included iatrogenic comminution, inability to place sufficient fixation for the articular fractures, and insufficient fixation overall, which require plate augmentation (12)
Retrograde nailing can be used in femur peri-prosthetic fractures and studies mentioned that it is a better option. Major drawbacks include, not all prosthetic designs are suitable for nailing, and extension deformity of fracture can occur due to posterior entry point (13).
Although both the implants have been used extensively for such types of fractures, the superiority of one implant over the other is still doubtful. Few studies comparing the use of these implants in distal femoral fractures have been published, and these have not given a consistent conclusion regards the advantages of both implants. Therefore, we conducted this meta-analysis to compare locked plating and retrograde intramedullary nailing in distal femoral fractures.
Materials and Methods
Search strategy
This study was planned and conducted according to the PRISMA guidelines (14). Electronic databases, including PubMed, Embase, Scopus, and Ovid Medline were searched from the inception of database upto 14 July 2019 with the search restricted to publications in English. The key terms for searching were: "distal", "femur", "fracture", "intramedullary fixation or plate or plating" and "nail or nailing". Additionally, we manually searched the reference lists of the included studies for potentially eligible studies. Reference lists from published original articles and previous reviews were scanned for more relevant studies.
Inclusion and exclusion criteria
Studies were included if the following criteria were fulfilled:
(1) studies were either randomized controlled trials (RCTs) or comparative studies( Level 1,2,3,4).
(2) the participants in the study were adult patients with distal femoral fractures, either closed or open;
(3) Studies must have had two or more groups where one of them must have used a locked plate and another retrograde nail to fix the distal femoral fracture.
(4) the assessment indexes included one or more of anterior knee pain, malunion, non-union, surgical duration, implant failure and infection.
On the contrary, studies were excluded if they were:
(1) studies including only elderly patients or exclusively periprosthetic distal femur fractures.
(2) studies in which condylar blade plate or angle blade plate was used.
(3) studies with incomplete data for statistical analysis;
(4) reviews, letters or comments;
(5) duplicated literature
(6) Cadaveric studies, case reports
(7) any studies that included other femoral fractures.
Study selection and characteristics
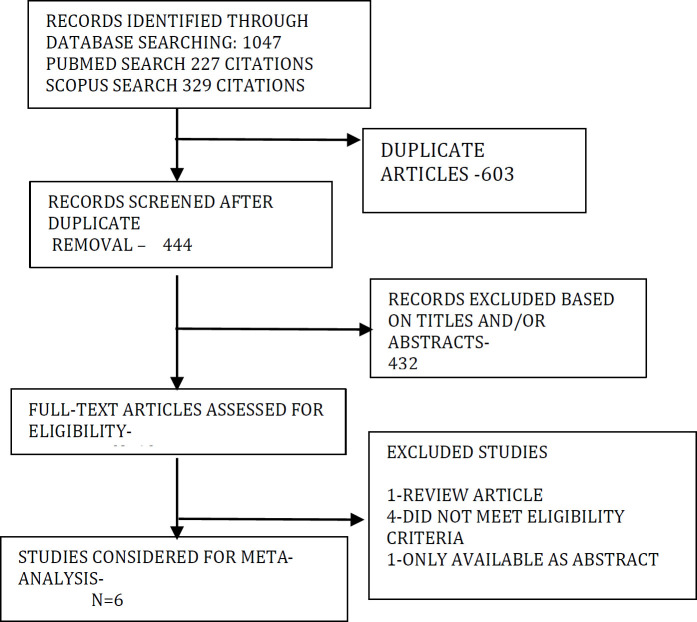
The initial search retrieved 1047 studies, out of which 603 duplicates were removed. 444 articles were screened, and 427 studies were excluded based on title and abstract. 3 studies were excluded as they did not exclusively use locked plates or have not mentioned it (15,16,17). One study included exclusively osteoporotic elderly patients and one study was a feasibility trial which were excluded (18,19). After examining the titles, abstracts, and full text of the short-listed papers, 6 were identified as suitable studies (8,10,20-23) [Tables 1 and 2].
Table 1.
Search Methodology
| DATABASE | DATE: 14 July 2019 | RESULTS |
|---|---|---|
| PUBMED | ((distal[All Fields] AND ("femur"[MeSH Terms] OR "femur"[All Fields]) AND ("fractures, bone"[MeSH Terms] OR ("fractures"[All Fields] AND "bone"[All Fields]) OR "bone fractures"[All Fields] OR "fracture"[All Fields])) AND English[lang]) AND English[lang] | 2720 |
| (distal[All Fields] AND ("femur"[MeSH Terms] OR "femur"[All Fields]) AND ("fractures, bone"[MeSH Terms] OR ("fractures"[All Fields] AND "bone"[All Fields]) OR "bone fractures"[All Fields] OR "fracture"[All Fields])) AND ("intramedullary fixation"[All Fields] OR ("nails"[MeSH Terms] OR "nails"[All Fields] OR "nail"[All Fields]) OR ("fracture fixation, intramedullary"[MeSH Terms] OR ("fracture"[All Fields] AND "fixation"[All Fields] AND "intramedullary"[All Fields]) OR "intramedullary fracture fixation"[All Fields] OR "nailing"[All Fields])) AND English[lang] | 743 | |
| (((distal[All Fields] AND ("femur"[MeSH Terms] OR "femur"[All Fields])) AND ("fractures, bone"[MeSH Terms] OR ("fractures"[All Fields] AND "bone"[All Fields]) OR "bone fractures"[All Fields] OR "fracture"[All Fields])) AND ("intramedullary fixation"[All Fields] OR ("nails"[MeSH Terms] OR "nails"[All Fields] OR "nail"[All Fields]) OR ("fracture fixation, intramedullary"[MeSH Terms] OR ("fracture"[All Fields] AND "fixation"[All Fields] AND "intramedullary"[All Fields]) OR "intramedullary fracture fixation"[All Fields] OR "nailing"[All Fields]))) AND (("bone plates"[MeSH Terms] OR ("bone"[All Fields] AND "plates"[All Fields]) OR "bone plates"[All Fields] OR "plate"[All Fields]) OR plating[All Fields]) AND English[lang] | 227 | |
| SCOPUS | TITLE-ABS-KEY ( ( distal AND femur AND fracture ) AND ( intramedullary AND fixation OR nail OR nailing ) AND ( plate OR plating ) ) AND ( LIMIT-TO ( LANGUAGE , "English" ) ) | 329 |
| EMBASE | distal AND femur AND fracture AND ('intramedullary fixation' OR nail OR 'intramedullary nailing') AND (plate OR plating) AND [english]/lim | 330 |
| OVID MEDLINE | (distal and femur and fracture and ("intramedullary fixation" or nail or nailing) and (plate or plating)).af. (After English filter) | 161 |
Table 2.
Prisma flow chart
Data collection and analysis
Two reviewers (D.N. and P.S) independently screened the studies. The title of the present study was utilized to assess the articles that appeared to be fit for inclusion, and their abstracts were read. In case of any doubt that aroused during abstract screening, full texts were retrieved and assessed. The articles that pertained to the study question were identified and finally these short-listed articles were included in the review for the analysis. Any selection conflicts between the two authors were resolved by discussion involving the other co-authors to arrive at a final consensus. Data extracted were collected and registered on a structured form under two groups (Group 1—Retrograde medullary nail/RLN and Group 2—distal locked plating/DLP). This included names of the authors, year of publishing, demographic parameters like age, sex and number of patients, complications like infection, malunion, anterior knee pain etc. Where there was missing information for studies, we contacted authors of articles. This was summarized in tabular form [Tables 3 and 4].
Table 3.
pre operative data in the studies
| Serial No. | Authors | Year | Type Of Study |
Groups
(1=RMN , 2=DLP) |
No. Of Patients | Percentage of high energy trauma (%) | Fracture Types(AO classification) | Percentage of Males (%) | Mean Age (years) | Mean Follow up (months) |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Markmiller et al (Germany) | 2004 | Pro- spective |
RMN | 16 | 69 | AO: 33A-11 33C-8 |
87.5 | 43.7 | > 12 months overall |
| DLP | 16 | 56 | AO: 33A-10 33C-10 |
37.5 | 57.2 | |||||
| 2 | Hierholzer et al (Germany) | 2011 | Retro-spective | RMN | 59 | 53 | AO: 33A-31 33C-28 |
64.3 overall | 54 overall | 13 |
| DLP | 56 | 67 | AO: 33A-21 33C-35 |
15 | ||||||
| 3 | Gao et al (China) | 2013 | Retro-spective | RMN | 17 | 76.5 | AO: 33A1-6,A2-8,A3-3 | 76.5 | 50.6 | 26.3 |
| DLP | 19 | 63.2 | AO: 33A1-8,A2-7,A3-4 | 70.5 | 54.7 | 23.4 | ||||
| 4 | Demirtas et al (Turkey) | 2014 | Retro-spective | RMN | 13 | 84.6 | AO: 33A1-4,A2-5,A3-4 | 84.6 | 31.1 | 26.7 |
| DLP | 15 | 86.7 | AO: 33A1-3,A2-5,A3-7 | 86.7 | 36 | 31.3 | ||||
| 5 | Gill et al (India) | 2017 | RCT | RMN | 20 | 70 | AO: 33A1-7,A2-10,A3-3 | 65 | 36 | 27.8 |
| DLP | 22 | 63.6 | AO: 33A1-9,A2-8,A3-5 | 72.7 | 38.7 | 29.2 | ||||
| 6 | Saumya et al (India) | 2018 | RCT | RMN | 20 | 85 | AO:33A1-2,A2-4,A3-10 C1-3,C2-14,C3-7 (Overall) |
75 | 39.6 | 10.4 overall |
| DLP | 20 | 95 | 80 | 37.4 |
Table 4.
Postoperative data in the studies
| Study | Study | Groups (1=RMN , 2=DLP) | Operative time (mins) |
Post operative data
(Ambulation time/ Time o surgery) |
Radiological union rates and weeks | Delayed unions and non unions | Malalignment (Coronal / Saggital) ( in degrees) | Infection | Knee ROM/ Anterior knee pain | Authors Conclusion |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Markmiller et al | RMN | 142 | Full wt bearing at radiological union / 3.4 days overall |
94.7% ; 14.6 | 1/19 NU | 2 (1-Varus malalignment > 5°,1-Outer rotational malalignment > 15°) | 1 (5.3%) | 103°/ N/A |
The author concludes that there was no significant difference between the plate and nail group with respect to malalignment, non-union, infection and functional outcome in our patients. The LISS offers good stabilization in periprosthetic fractures |
| DLP | 155 | 90%; 13.8 | 2/20 NU | 3 (2-Varus malalignment > 5°,1-Outer rotational malalignment > 15°) | 0 | 110°/ N/A |
||||
| 2 | Hierholzer et al | RMN | N/A | Full wt bearing at radiological union / N/A |
91.5%, N/A | 5/59 NU 4/59 Delayed Union |
N/A | 1(1.7%-superficial infection) | N/A | No differences were seen in outcome between implants regarding fracture healing, nonunion, and infection. Locked plating may be utilized for all distal femur fractures including complex type C fractures, periprosthetic fractures, as well as osteoporotic fractures. IM nailing may be successfully implanted in bilateral, multisegmental fractures as well as in extra-articular and type C1 fractures. |
| DLP | 89.3%, N/A | 6/56 NU 6/56 Delayed Union |
5(3 superfici3al & 2 deep infection-8.9 %) | |||||||
| 3 | Gao et al | RMN | 87.4 | Full wt at radiological union/2.1 days | 94.1%, N/A | 1/17 NU 0/17 Delayed Union |
2 Malunion | 0 | 103.5, N/A | The overall union disturbance rate in the LP group was higher than in the RN group. No significant difference between the groups in infection, malalignment and knee pain |
| DLP | 79.7 | Full wt at radiological union/1.7 days | 84.2%, N/A | 3/19 NU 4/19 Delayed Union |
1 Malunion | 1 (5.3%) | 98.2 , N/A | |||
| 4 | Demirtas et al | RMN | N/A | Full wt at radiological union/3.2 days | 92.3%, 22.3 | 1/13 NU 2/13 Delayed Union |
3 (1-Malalignment >10°, 2 -Malalignment 5-10°) |
N/A | N/A, 3(23.1%) |
The author concludes that the outcomes of the plating and nailing methods for the treatment of extra-articular distal femur fractures were similar and both methods can be applied in all fractures, with the exception of Gustilo- Anderson Type 3B and C open fractures |
| DLP | Full wt at radiological union/2.8 days | 86.7 %, 25.7 | 2/15 NU 3/15 Delayed Union |
4 (2-Malalignment >10°, 2 -Malalignment 5-10°) |
N/A, 3(20%) |
|||||
| 5 | Gill et al | RMN | 102.3 | Full wt bearing at radiological union / 5.2 days | 90% , 22.6 | 2/20 NU 1/20 Delayed Union . |
6 (2-Malalignment >10°, 4 -Malalignment 5-10°) |
3(1.7%-superficial infection) | 107 , 4(20%) |
The author stated that nailing had the disadvantages of increased operating time and blood loss and successive anterior knee pain but had the advantage of earlier union. On the other hand, technical errors are more common with minimally invasive plating |
| DLP | 88.4 | Full wt bearing at radiological union / 6.2 days | 90.9%, 26.5 | 2/22 NU 5/22 Delayed Union |
3 (1-Malalignment >10°, 2 -Malalignment 5-10°) |
5(3 superficial & 2 deep infection-8.9 %) | 112 , 1(4.5%) |
|||
| 6 | Saumya et al | RMN | 105 | Full wt bearing at radiological union / 2.3 days | 100%, 14.6 | 0/20 NU 0/20 Delayed Union |
3 malunion | N/A | 113.4 , N/A |
The author concludes that retrograde nailing was found to be a better fixation system for both extra as well as intra-articular fractures of distal femur with better outcome in terms of range of movements, early mobilisation and less operative time and blood loss. |
| DLP | 110 | Full wt bearing at radiological union / 3 days | 100%, 16.2 | 0/20 NU 1/20 Delayed Union |
2 malunion | N/A | 106.3 , N/A |
Quality assessment
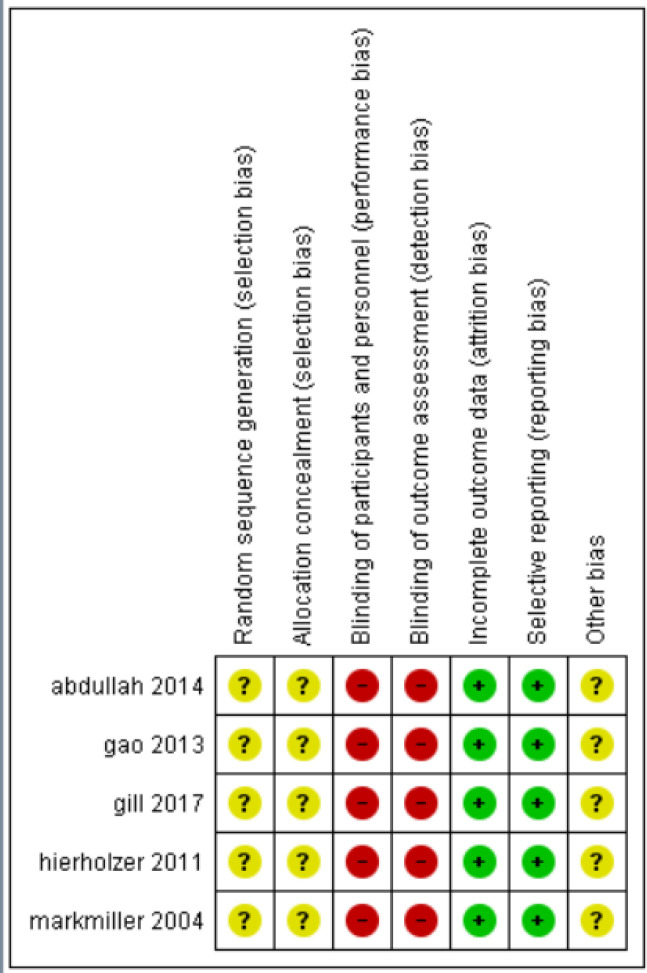
All studies were assessed by two independent reviewers (KJ and VK) to check the methodological quality of clinical trials using Cochrane Collaboration recommendations. Aspects like random sequence generation, allocation concealment, blinding of outcome assessments, incomplete outcome data, selective reporting and other biases were assessed using revman software.
Statistical analysis
We analyzed our data with Review Manager Software (Rev-Man 5.3). For dichotomous data, odds ratio (OR) and 95% confidence intervals (CI) were calculated. For continuous data, weighted mean difference (WMD) and 95% CI were calculated. We used fixed effects model to estimate overall effect sizes. I2 value and chi-square test were used to assess statistical heterogeneity. p value > 0.1 and I2 value of > 50% were considered as statistical heterogeneity. Sensitivity analysis was carried out to check whether a particular study has larger impact on outcome.
Risk of bias
Risk of bias of the studies we included were assessed using rev man software. Parameters like randomization techniques like computer-generation and allocation concealment, blinding were assessed [Figure 1]. Red color indicate high risk studies, yellow color indicate intermediate risk studies and green color indicates high risk studies.
Figure 1.
risk of bias summary: risk of bias item for each included study
Results
Study characteristics
All studies included in the analysis directly compared intramedullary nailing with plating for distal femoral fractures, both intraarticular and extraarticular. Out of the six studies included, 2 were retrospective, 2 were prospective and 2 were randomized controlled trials. All of them were published in last 20 years. The least number of patients included is 13 in nailing group and 15 in plating group (20). The maximum number of patients in a study is 115 (8). The studies have mentioned comparability of individual groups in terms of preoperative parameters like age, sex and type of fracture.
Demographic variables
Age, sex, fracture type & implant
All the included studies have patients of age ranging from 17 years to 89 years. All the studies included only skeletally mature patients in the analysis. The studies were not exclusive to elderly osteoporotic patients. One retrospective study which included only osteoporotic elderly distal femoral fractures which can cause bias was excluded (18). All the studies have shown that distal femoral fractures are more commonly seen in males compared to their female counterparts. Most of the patients have high energy trauma due to road traffic accidents as the cause, hence resulting in a male majority who are more involved in accidents compared to females. Both the groups in most of the studies (except 1) were comparable without any gender bias with a proportional male-to-female ratio between the groups, with males being in the majority. One study has a female dominant plating group and male-dominant nailing group (23).
3 studies included only extra-articular supracondylar femur fractures (20-22). 3 studies included both intra-articular and extra-articular fractures, with similar distribution among nailing and plating groups (8,10,23). These studies have used nailing even in intra-articular distal femur fractures with comparable distribution of AO Type C fractures among both the nailing and plating groups and hence amenable to comparision. Retrograde intramedullary nailing (RMN) consisted of an intramedullary nail with an expanded distal end with at least two distal interlocking bolts. Internal fixation with plating was achieved with a lateral distal femur locked plate (DLP). The studies included here used only locking plates and did not include studies with use of condylar blade plate and angular blade plate. Also, studies analyzing distal femur fractures exclusively in periprosthetic fractures were excluded.
Outcomes
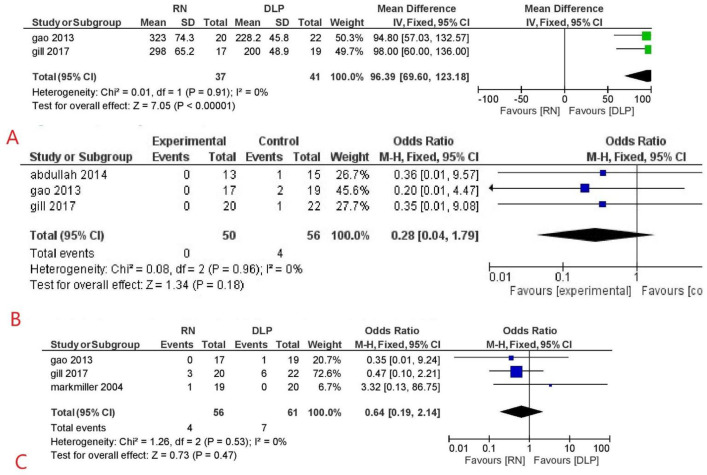
Blood loss
Only 2 out of 6 included studies mentioned about bloodloss (21,22). The mean blood loss was higher in patients of nailing group in comparison to the plating group with a mean difference of 96.39 in favor of the plating group and was statistically significant (95% CI 69.60 to123.18, p <0.01). Both the studies in this subset included only extra-articular supracondylar fractures and closed reduction with minimal invasive submuscular plating was done in the plating group, which could be the reason for lesser blood loss (Figure 2A).
Figure 2.
forest plot for (a) blood loss, (b) implant failure, and (c) infection
Implant failure
Only 3 out 6 included studies mentioned about implant failure (20-22). It was exclusively seen in the plating group with an Odds ratio of 0.28 favouring the nailing group but was statistically not significant (95% CI 0.04 to 1.79, p=0.18). The retrograde intramedullary nail is a load sharing device that allows early weight-bearing while locking plate is a load-bearing fixation that assumes 100% of the functional load. Hence nailing can be favourable in long bone fixation compared to plating with regards to implant failure (24, 25) [Figure 2B].
Infection
3 out of 6 studies mentioned about infection. It was more commonly seen in the plating group when compared to the nailing group. 4 out of 56 patients had an infection in the nailing group, and 7 out of 61 patients had an infection in the plating group. Although the results were not significant, the odds ratio was 0.64 (95% CI 0.19–2.14, p = 0.47), favoring the nailing group. IV antibiotics were used in such cases, and implant removal and debridement were done whenever necessary [Figure 2C]. Gao et al, mentioned that 1 patient in plating group had deep infection which lead to implant removal. Gill et al, mentioned superficial infection 4 in plating group and 2 in nailing group, 1 patient in each group had deep infection which lead to implant removal. Markmiller et al, didn’t mention about deep or superficial infection (21-23).
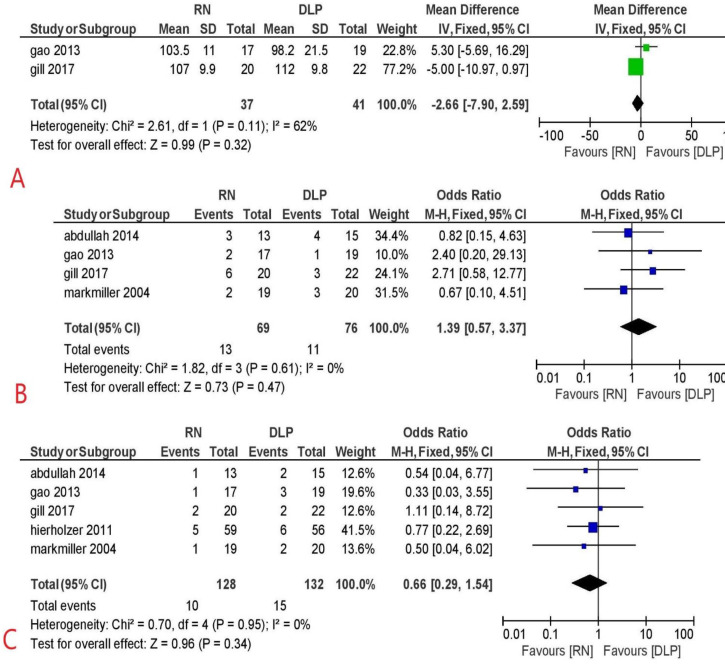
Knee rom
Only 2 out of 6 studies mentioned about knee ROM (21,22).
It was found to be comparable in both nailing and plating groups with a mean difference of -2.66 (95% CI -7.90 to 2.59, p= 0.11). Both the authors advocated a range of motion exercises for knee after surgery from the first postoperative day. An early active range of motion exercises for the knee can avoid stiffness and improve the final outcome [Figure 3A]. Full weight bearing was allowed only after radiological signs of union in any group.
Figure 3.
forest plot for (a) knee range of motion, (b) malunion, and (c) nonunion
Malunion
4 out of 6 studies mentioned about malunion (20-23). Malalignment was seen in 13 patients out of 69 patients with nailing and 11 patients out of 76 patients with plating with an odds ratio of 1.39, slightly favoring the plating group but not statistically significant (95% CI -0.57 to 3.37, p=0.47). malalignment of more than 5-10 degrees is considered as malunion. Although angular malunion is a known complication of retrograde medullary nailing, the use of longer and broader nails and the use of poller screws whenever necessary can reduce its occurrence (26,27) [Figure 3B].
Non union
5 out of 6 studies mentioned about non-union8 (8,20-23) Overall, 10 out of 128 patients in the nailing group and 15 out of 132 patients in the plating group had the complication of non-union with an odds ratio of 0.66, slightly favoring retrograde medullary nailing (95% CI 0.29 to 1.54, p=0.34). Non-union has been treated by exchange implants and autologous bone grafting in most patients. The addition of bone morphogenic protein (BMP-7) in atrophic non-union was done in a few patients in a study (8) [Figure 3C].
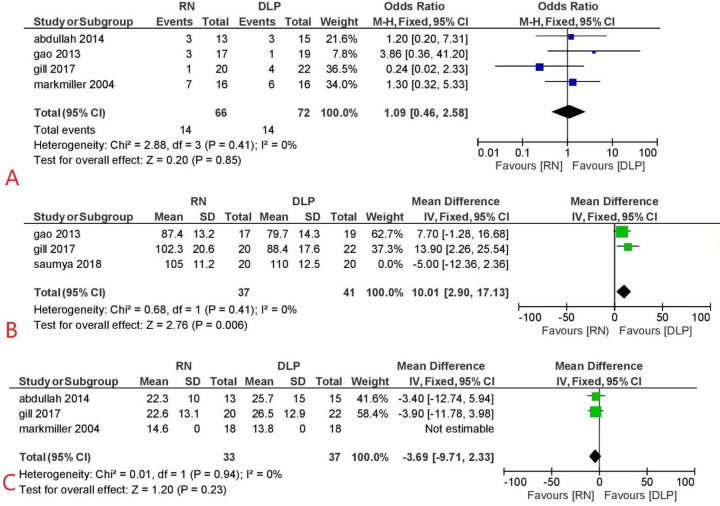
Pain
4 out of 6 included studies mentioned about anterior knee pain (20-23). It was a complaint seen similarly in both the nailing and plating groups with an odds ratio of 1.09 (95% CI 0.46 to 2.58, p=0.85). Although theoretically, anterior knee pain is more commonly associated with retrograde medullary nailing due to joint damage during the nail insertion, there was no significant difference between plating and nailing groups (28,29) [Figure 4A].
Figure 4.
forest plot for (a) pain, (b) surgical duration, And (c) union time
Surgical duration
3 out of 6 included studies mentioned about surgical duration (10,21,22). The overall mean surgical duration was seen to be higher in retrograde medullary nailing when compared to the plating group with a mean difference of 10.1, which was statistically significant (95% CI 2.90 to 17.13, p <0.01). Use of submuscular plating with percutaneous screw insertion with the help of aiming device can reduce the time required for plating while reaming of medullary canal to achieve a snugly fitting broader nail, the use of poller screws to avoid malalignment and use of freehand technique for the insertion of proximal screws can account for a higher operating time in the nailing group [Figure 4B].
Union time
3 out of 6 included studies mentioned about time to union (20,22,23). Although the union time was slightly favoring the nailing group, there was no significant difference in the union time between the plating and nailing group among all the three studies that have been analyzed for this parameter (mean difference of -3.69, 95% CI -9.71 to 2.33, p=0.23). Henderson et al. reported a higher amount of callus formation in the nailing group compared to the plating group at similar follow up time (30) [Figure 4C].
Discussion
Treatment for the fractures of the distal femur has evolved from the use of condylar screw and angled blade plate to the use of Less Invasive stabilization system and retrograde intramedullary nailing (7, 31). Several studies have been conducted for comparison of biomechanical analysis between locked plating and intramedullary implant for distal femur fractures, but comparative studies between these implants in the patients have been very few. (32-37). Both locked plating and distal femoral nailing allow the fixation with minimal soft tissue dissection and can adhere to the principle of biological osteosynthesis.
Both Gao et al and Gill et al have found similar findings in extra articular distal femur fractures (21,22). They have found significant difference between nailing group and plating in terms of blood loss and surgical time favouring the plating group. As the nailing patients required extra procedure of sequential reaming, increased blood loss as well as surgical time was seen in nailing. However, these findings did not translate into any long term effects as there was no significant difference between the two groups with respect to deep infection, implant failure, knee pain or knee range of motion. However, Gao et al reported more union disurbances, namely both non-union and delayed union combined in the plating group, when compared to the nailing group. Demirtas et al. also did not find an significant difference with respect to implant failure,,malunion , non-union, knee pain, or union time in extra articular distal femur fractures (20). Hierholzer et al, who compared the fixation methods in both extra and intraarticular fractures, have found no difference between the groups with respect to non-union and infection (8). Markmiller et al. also did not find any significant between the two groups with respect to infection, malunion or non-union (23).
On performing the analysis combining all the data, patients in the plating group are associated with lesser blood loss and lesser duration of surgery compared to the nailing group, which was statistically significant. Malunion was comparatively less in the plating group, although the finding was statistically not significant.
On the other hand, patients in the nailing group have a slightly lesser chance of implant failure, infection, and non-union, but the difference was insignificant; this could be attributed to a lesser number of studies. Other parameters such as knee ROM, anterior knee pain, and time to the union were equivocal in both plating and nailing group. Sub group analysis cannot be done based on fracture type to say whether a particular implant is better for particular type of fracture, as the data on results in various age groups and fracture types is not available. El-kawy et al did a study on retrograde nailing in elderly patients for distal femur fractures without intra articular extension and showed that it is a surgically limited and reliable procedure in elderly patients (38).
Hence, distal femur fractures can be managed with both locked plating and retrograde intramedullary nailing with both showing similar outcomes with respect to malunion, non-union, implant failure, infection, knee ROM, anterior knee pain and time to union with plating having the advantage of lesser blood loss and lesser duration of surgery which was significant. These results can also be applied to patients with intraarticular fractures of the distal femur as the patient distribution with respect to AO type C fractures was similar in both nailing and plating groups, albeit with reservations. On the other hand, retrograde nailing is a feasible alternative, even in fractures with comminution, and allows early weight-bearing and mobilization.
The limitation of this study is that the certainty of the evidence is very low as per our grading scores because there are very few randomized controlled trials in the literature. Also, the individual studies do not have all the parameters of outcomes that are being analyzed here and the inclusion of retrospective studies in our analysis can affect the strength of the evidence. Hence conducting larger prospective randomized controlled trials could further increase the strength of our results.
Limitations
Most of the included studies were observational studies, with both retrospective and prospective studies included in the analysis. Since the available RCTs were limited, these observational studies had to be included to compare both the implants in distal femur fracutres. In addition, another limitation of our analysis is less number of studies and less number of patients
Conclusions
In the present meta analysis, we came to a conclusion that surgical duration and blood loss favoured plating group and the difference is significant. But while analysing parameters like implant failure, infection and non-union, our analysis favoured nailing group, but the difference is not significant. This may be because of less number of studies and lesser sample size. Overall, both locked plating and retrograde intramedullary nailing are comparable with respect to complications in distal femur fractures, but we need further larger and high quality randomized studies to evaluate the difference.
Acknowledgements
Conflict of interests:
The authors declare that they have no conflict of interest.
Funding:
No funding sources for this study
ETHICAL APPROVAL:
Our study is a review article and does not include any human or animal participation. So, we didn’t require ethical approval.
INFORMED CONSENT:
Our study doesn’t include human participation hence we didn’t require informed consent.
References
- 1.Court-Brown CM, Caesar B. Epidemiology of adult fractures: a review. Injury. 2006;37(8):691–7. doi: 10.1016/j.injury.2006.04.130. [DOI] [PubMed] [Google Scholar]
- 2.Jahangir AA, Cross WW, Schmidt AH. Current management of distal femoral fractures. Current Orthopaedic Practice. 2010;21(2):193–7. [Google Scholar]
- 3.Merchan EC, Maestu PR, Blanco RP. Blade-plating of closed displaced supracondylar fractures of the distal femur with the AO system. J Trauma. 1992;32(2):174–8. doi: 10.1097/00005373-199202000-00010. [DOI] [PubMed] [Google Scholar]
- 4.Albert MJ. Supracondylar Fractures of the Femur. J Am Acad Orthop Surg. 1997;5(3):163–171. doi: 10.5435/00124635-199705000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Kregor PJ, Stannard JA, Zlowodzki M, Cole PA. Treatment of distal femoral fractures using the less invasive stabilization system: Surgical experience and early clinical results in 103 fractures. J Orthop Trauma. 2004;18(8):509. doi: 10.1097/00005131-200409000-00006. [DOI] [PubMed] [Google Scholar]
- 6.Gurkan V, Orhun H, Doganay M, Salioğlu F, Ercan T, Dursun M, et al. Retrograde intramedullary interlocking nailing in fractures of the distal femur. Acta Orthop Traumatol Turc. 2009;43(3):199–205. doi: 10.3944/AOTT.2009.199. [DOI] [PubMed] [Google Scholar]
- 7.Handolin L, Pajarinen J, Lindahl J, Hirvensalo E. Retrograde intramedullary nailing in distal femoral fractures--results in a series of 46 consecutive operations. Injury. 2004;35(5):517–22. doi: 10.1016/S0020-1383(03)00191-8. [DOI] [PubMed] [Google Scholar]
- 8.Hierholzer C, von Rüden C, Pötzel T, Woltmann A, Bühren V. Outcome analysis of retrograde nailing and less invasive stabilization system in distal femoral fractures: A retrospective analysis. Indian J Orthop. 2011;45(3):243–50. doi: 10.4103/0019-5413.80043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Neubauer T, Ritter E, Potschka T, Karlbauer A, Wagner M. Retrograde nailing of femoral fractures. Acta Chir Orthop Traumatol Cech. 2008;75(3):158–166. [PubMed] [Google Scholar]
- 10.Agarwal S, Udapudi S, Gupta S. To Assess Functional Outcome for Intra-Articular and Extra-Articular Distal Femur Fracture in Patients using Retrograde Nailing or Locked Compression Plating. Journal of Clinical and Diagnostic Research. 2018;12(3):21–4. [Google Scholar]
- 11.Garnavos C, Lygdas P, Lasanianos NG. Retrograde nailing and compression bolts in the treatment of type C distal femoral fractures. Injury. 2012;43(7):1170–5. doi: 10.1016/j.injury.2012.03.023. [DOI] [PubMed] [Google Scholar]
- 12.Warner SJ, Achor TS. Intramedullary Nailing of Complete Articular Distal Femur Fractures. Operative techniques in orthopaedics. 2018;28(3):112–7. [Google Scholar]
- 13.Shin YS, Kim HJ, Lee DH. Similar outcomes of locking compression plating and retrograde intramedullary nailing for periprosthetic supracondylar femoral fractures following total knee arthroplasty: a meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2017;25(9):2921–2928. doi: 10.1007/s00167-016-4050-0. [DOI] [PubMed] [Google Scholar]
- 14.Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hoskins W, Sheehy R, Edwards ER, Hau RC, Bucknill A, Parsons N, et al. Nails or plates for fracture of the distal femur? data from the Victoria Orthopaedic Trauma Outcomes Registry. The bone & joint journal. 2016;98(6):846–50. doi: 10.1302/0301-620X.98B6.36826. [DOI] [PubMed] [Google Scholar]
- 16.Rossas C, Nikolopoulos D, Liarokapis S, Platanitis I, Karatzas G, Aggelidis C, et al. Retrograde intramedullary nailing vs plating in treatment of extrarticular distal femoral fractures: A comparative study. Injury. 2011;42(3):S20–S1. [Google Scholar]
- 17.Pean CA, Konda SR, Fields AC, Christiano A, Egol KA. Perioperative adverse events in distal femur fractures treated with intramedullary nail versus plate and screw fixation. Journal of orthopaedics. 2015;12(2):S195–S9. doi: 10.1016/j.jor.2015.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mukherjee P, Bovell C, Davis J. Less invasive stabilising system plate versus retrograde intramedullary nail for osteoporotic distal femoral fracture. European Journal of Orthopaedic Surgery and Traumatology. 2010;20(4):281–4. [Google Scholar]
- 19.Griffin XL, Costa ML, Achten J, Dritsaki M, Baird J, Parsons N. Trial of Acute Femoral Fracture Fixation (TrAFFix): study protocol for a randomised controlled feasibility trial. Trials. 2017;18(1):538. doi: 10.1186/s13063-017-2265-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Demirtaş A, Azboy I, Özkul E, Gem M, Alemdar C. Comparison of retrograde intramedullary nailing and bridge plating in the treatment of extra-articular fractures of the distal femur. Acta Orthop Traumatol Turc. 2014;48(5):521–6. doi: 10.3944/AOTT.2014.14.0004. [DOI] [PubMed] [Google Scholar]
- 21.Gao K, Gao W, Huang J, Li H, Li F, Tao J, et al. Retrograde nailing versus locked plating of extra-articular distal femoral fractures: comparison of 36 cases. Med Princ Pract. 2013;22(2):161–6. doi: 10.1159/000342664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gill S, Mittal A, Raj M, Singh P, Singh J, Kumar S. Extra Articular Supracondylar Femur Fractures Managed with Locked Distal Femoral Plate or Supracondylar Nailing: A Comparative Outcome Study. J Clin Diagn Res. 2017;11(5):19–23. doi: 10.7860/JCDR/2017/25062.9936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Markmiller M, Konrad G, Südkamp N. Femur–LISS and Distal Femoral Nail for Fixation of Distal Femoral Fractures: Are There Differences in Outcome and Complications? Clinical Orthopaedics and Related Research. 2004;42(6):252–7. doi: 10.1097/01.blo.0000141935.86481.ba. [DOI] [PubMed] [Google Scholar]
- 24.Ricci WM, Streubel PN, Morshed S, Collinge CA, Nork SE, Gardner MJ. Risk factors for failure of locked plate fixation of distal femur fractures: an analysis of 335 cases. J Orthop Trauma. 2014;28(2):83–9. doi: 10.1097/BOT.0b013e31829e6dd0. [DOI] [PubMed] [Google Scholar]
- 25.Henderson CE, Kuhl LL, Fitzpatrick DC, Marsh JL. Locking plates for distal femur fractures: is there a problem with fracture healing? J Orthop Trauma. 2011;25(1):8–14. doi: 10.1097/BOT.0b013e3182070127. [DOI] [PubMed] [Google Scholar]
- 26.Acharya KN, Rao MR. Retrograde nailing for distal third femoral shaft fractures: a prospective study. J Orthop Surg. 2006;14(3):253–8. doi: 10.1177/230949900601400305. [DOI] [PubMed] [Google Scholar]
- 27.Ostrum RF, Maurer JP. Distal third femur fractures treated with retrograde femoral nailing and blocking screws. J Orthop Trauma. 2009;23(9):681–4. doi: 10.1097/BOT.0b013e3181ad61f2. [DOI] [PubMed] [Google Scholar]
- 28.Wenda K, Runkel M. Systemic complications in intramedullary nailing. [Article in German] Orthopade. 1996;25(3):292–9. [PubMed] [Google Scholar]
- 29.Leggon RE, Feldmann DD. Retrograde femoral nailing: a focus on the knee. Am J Knee Surg. 2001;14(2):109–18. [PubMed] [Google Scholar]
- 30.Henderson CE, Lujan TJ, Kuhl LL, Bottlang M, Fitzpatrick DC, Marsh JL. Mid-America orthopaedic association physician in training award: healing complications are common after locked plating for distal femur fractures. Clin Orthop Relat Res. 2011;469(6):1757–65. doi: 10.1007/s11999-011-1870-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kregor PJ, Stannard J, Zlowodzki M, Cole PA, Alonso J. Distal femoral fracture fixation utilizing the Less Invasive Stabilization System (L. I.S.S.): The technique and early results. Injury. 2001;32(3):32–47. doi: 10.1016/s0020-1383(01)00182-6. [DOI] [PubMed] [Google Scholar]
- 32.Bliemel C, Buecking B, Mueller T, et al. Distal femoral fractures in the elderly: biomechanical analysis of a polyaxial angle-stable locking plate versus a retrograde intramedullary nail in a human cadaveric bone model. Arch Orthop Trauma Surg. 2015;135(1):49–58. doi: 10.1007/s00402-014-2111-8. [DOI] [PubMed] [Google Scholar]
- 33.Cegoñino J, Aznar JMG, Doblaré M, Palanca D, Seral B, Seral F. A Comparative Analysis of Different Treatments for Distal Femur Fractures using the Finite Element Method. . Comput Methods Biomech Biomed Engin. 2004;7(5):245–6. doi: 10.1080/10255840412331307182. [DOI] [PubMed] [Google Scholar]
- 34.Heiney JP, Barnett MD, Vrabec GA, Schoenfeld AJ, Baji A, Njus GO. Distal Femoral Fixation: A Biomechanical Comparison of Trigen Retrograde Intramedullary Dynamic Condylar Screw (DCS), and Locking Compression Plate (LCP) Condylar Plate. J Trauma. 2009;66(2):443–9. doi: 10.1097/TA.0b013e31815edeb8. [DOI] [PubMed] [Google Scholar]
- 35.Putineanu D, Com S, Ciobota N-D. Comparative study of mechanical fixation of extreme distal femur fractures with plates and condylar intramedullary nails. UPB Scientific Bulletin, Series D: Mechanical Engineering. 2011;73(2):59–70. [Google Scholar]
- 36.Wähnert D, Hoffmeier K, Fröber R, Hofmann GO, Mückley T. Distal femur fractures of the elderly—Different treatment options in a biomechanical comparison. Injury. 2011;42(7):655–9. doi: 10.1016/j.injury.2010.09.009. [DOI] [PubMed] [Google Scholar]
- 37.Zlowodzki M, Williamson S, Cole P, Zardiackas L, Kregor P. Biomechanical Evaluation of the Less Invasive Stabilization System, Angled Blade Plate, and Retrograde Intramedullary Nail for the Internal Fixation of Distal Femur Fractures. Journal of Orthopaedic Trauma. 2004;18(8):494–502. doi: 10.1097/00005131-200409000-00004. [DOI] [PubMed] [Google Scholar]
- 38.El-Kawy S, Ansara S, Moftah A, Shalaby H, Varughese V. Retrograde femoral nailing in elderly patients with supracondylar fracture femur; is it the answer for a clinical problem? International orthopaedics. 2007;31(1):83–6. doi: 10.1007/s00264-006-0137-4. [DOI] [PMC free article] [PubMed] [Google Scholar]