Abstract
The aim of this study was to evaluate the effects on the adherence of drug prescription to the guideline recommendations of a chronic care model based on the close interaction between hospital and local healthcare district cardiologists through a shared web-based database. From 2018 to 2021, patients hospitalized for an episode of acute decompensated heart failure (HF) (de novo or worsening) in cardiology wards from the healthcare district of Bari, Italy, were enrolled. The follow-up programme was based on a first visit after discharge within 1 month; patients were therefore addressed to the local health district cardiologist outpatient clinics when not requiring further invasive investigations and haemodynamically stable and followed-up with at least one visit every 6 months. In order to share in-hospital patients’ data with outpatient clinics, at discharge, they were entered in a web-based database accessible for all cardiologists and centres participating in the Ponte Project. The group of patients affected by HF with reduced ejection fraction (HFrEF) were considered for the analyses. Drug prescription rates at 1-year follow-up were analysed as endpoint, as well as the re-admission for HF worsening. Out of 1200 HF patients enrolled in the project until December 2021, 56% were affected by HFrEF. At 1-year follow-up, 91% of patients were assuming beta-blockers, 86% mineralocorticoid receptor antagonists, 98% angiotensin-converting enzyme inhibitors/angiotensin receptor antagonists/neprilysin angiotensin receptor antagonists, and 13% ARNI. Compared to patients enrolled before 2020, ARNI prescription increased in 2021 (60% vs. 13%, respectively, P < 0.001). In 30% of patients, ARNI were prescribed before hospital discharge. Furthermore, in 10% of the population (most diabetics), sodium-glucose cotransporter 2 inhibitors were also prescribed. The implementation of the PONTE project was associated with an improved adherence to guidelines recommendations.
Keywords: Chronic heart failure, Web, Data sharing, Adherence, HF management programmes
Introduction
Over the last decades, several classes of drugs have been demonstrated to improve the prognosis of heart failure (HF) patients. In particular, in patients affected by HF with reduced ejection fraction (HFrEF), first, the role of angiotensin-converting enzyme inhibitors (ACEis), angiotensin receptor blockers (ARBs), betablockers (BBs), and mineralocorticoid receptor antagonists (MRAs) in improving prognosis has been well established in several clinical trials.1 Moreover, over the last few years, new classes of drugs, i.e. sacubitril/valsartan (ARNI)2 and sodium-glucose cotransporter 2 inhibitors (SGLT2i), empagliflozin,3 and dapagliflozin4 have been demonstrated to further decrease the risk of HF progression.
In HFrEF patients, the estimated effects of a comprehensive disease-modifying pharmacological therapy (ARNI, BBs, MRA, and SGLT2i) are 2.7–8.3 additional years free from cardiovascular death or first hospital admission for HF and 1.4–6.3 additional years of survival when compared with conventional therapy (ACE inhibitor or ARB and BB).5
Despite the great advance in pharmacological treatment, HF still remains a leading cause of mortality and hospitalization worldwide.6,7 This could be in part due to missed prescription of the disease modifier drugs.8 For this reason, HF programmes aimed to reach an optimal treatment of HF patients are strongly recommended by current guidelines.7
The aim of this study was therefore to evaluate the possible effects of an HF chronic care model on the adherence to guidelines recommendations. The HF programme was based on the strict interaction between hospital and local healthcare district cardiologists through a shared web-based database.
Methods
A chronic care model based on the strict integration between hospital and health district cardiologists through an integrated web-based clinical data sharing has been implemented in Apulia region, Italy, since 2018, in order to optimize the management of the HF patient after a hospitalization for HF: the PONTE (PDTA FOR INTEGRATED FOLLOW-UP TERRITORY HOSPITAL OF THE PATIENT WITH CARDIAC HEART FAILURE) (bridge) project. Patients hospitalized for an episode of acute HF (de novo or worsening) in cardiology wards throughout the healthcare district of Bari, Italy, and participating in the project were enrolled in the study. According to shared diagnostic-therapeutic pathways, the optimization of drug treatment was started before the discharge. Moreover, since 2020, on the basis of the results of PIONEER and TRANSITION studies, the onset of therapy with ARNI before discharge was strongly recommended in order to increase the rate of its prescription.
As shown in Figure 1, first follow-up was held within 1 month after discharge in hospital HF outpatient clinic. After this first follow-up visit, patients were addressed to:
Figure 1.

Possible follow-up pathway after hospital discharge for heart failure.
local health district cardiologists/clinics or spoke centres when not requiring further invasive investigations and haemodynamically stable (low risk);
cardiology wards when requiring coronary angiography/implantable electric cardiac devices or haemodynamically unstable (high risk); and
referral heart transplantation centre if indicated.
Further follow-up visits were scheduled every 6 months or earlier in case of signs or symptoms suggestive of HF worsening.
Clinical data of HF patients were entered in a shared web-based database accessible for all cardiologists and centres participating in the Ponte Project (Figure 2). Moreover, individual primary physicians were also notified with personal discharge letter for all patients enrolled in the study.
Figure 2.
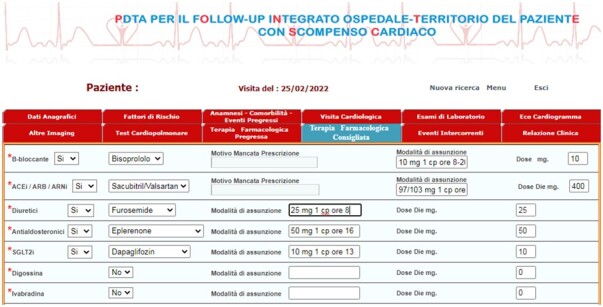
Data entry interface of the Ponte HF web-based registry.
Out of all patients, demographic, clinical, laboratory, and echocardiographic characteristics of those with HFrEF were analysed. The prescription rates of therapies recommended for the treatment of HFrEF, in particular, BB, MRA, ACEi/ARB/ARNI, and SGLT2i were evaluated.
ARNI prescription rates before and after 2020 were also compared. Re-admission rate for HF worsening was also analysed.
Results
Out of 1200 patients enrolled in the project, 690 (56%) were affected by HFrEF.
Clinical characteristics of this group are shown in Table 1. In brief, the mean age was 63 years, 71% were affected by essential hypertension, 27% diabetes, and 40% by ischaemic heart disease. Forty-two percent were previously treated with coronary angioplasty, 56% had an ICD/CRT, and 44% had atrial fibrillation. Mean New York Heart Association class was 2.2, mean left ventricular ejection fraction 30%, mean NT-proBNP values 4027 pg/mL, and mean serum creatinine 1 mg/dL.
Table 1.
Principal enrolled population features: Ponte Heart Failure before and after 2020 compared with ESC Heart Failure Long Term Registry
| Ponte heart failure (N = 690) | ESC Heart Failure Long Term Registry | |
|---|---|---|
| Mean/% | ||
| Age | 63 | 64 |
| Hypertension | 71 | 58 |
| Diabetes | 27 | 39 |
| Non-ischaemic | 60 | 35 |
| Ischaemic | 40 | 48 |
| ICD/CRT | 56 | 41 |
| AF | 44 | 44 |
| LVEF | 29 | 37 |
| NT-ProBNP (pg/ml) | 4027 | 1608 |
| Creatinine (mg/dL) | 1.01 | |
| BB | 91 | 90 |
| MRA | 86 | 63 |
| ACEi/ARB/ARNI | 98 | 90 |
| ARNI | 13 | 13 |
| 60 after 2020 P < 0.001 |
At 1-year follow-up, 91% of patients were taking BB, 86% MRA, and 98% ACEi/ARB/ARNI (13% ARNI).
Compared to patients enrolled before 2020, ARNI prescription increased in 2021 (60% vs. 13%, P < 0.001); in 30% ARNI were prescribed in hospital before discharge. Furthermore, in 10% of the population (most diabetics), SGLT2is have been prescribed as indicated by the latest European Society of Cardiology (ESC) 2021 guidelines.
Re-hospitalization rate was reduced from 10% before 2020 to 8% after.
Discussion
The main finding of this study is that the implementation of a chronic care model based on shared diagnostic and therapeutic pathways and facilitated by the use of web-based clinical data sharing may be associated with a higher adherence to the guidelines-recommended drug treatment.
Data from leading European registries show that the implementation of guidelines-recommended therapies is still far from being satisfactory, even in Europe. In the ESC-EORP HF registry, over 90% received ACEi or ARBs, about 90% received BBs, 63% received MRA, 88% were prescribed ACEi/ARB + BB, 64% ACEi/ARB + BB + MRA but only 12% of patients received ARNI.9 In the US CHAMP registry, 81% were prescribed ACEi/ARB, 83% BB, 33% MRA, and only 13% ARNI10 (Table 1).
Interventional HF programmes were designed to bridge the gap between evidence and practice: education, audit and feedback, organization levels (changes in medical records systems), clinical multidisciplinary teams, continuity of care after discharge, and financial incentives/penalties.11
In order to reduce hospitalizations and mortality, also guidelines recommend the use of multidisciplinary HF management programmes (HF-MPs), which enable patients to have the correct investigations, an accurate diagnosis, appropriate evidence-based therapy, education, and suitable follow-up along the whole HF trajectory (from onset, through critical events, periods of apparent stability, and its terminal stages).
Heart failure management programmes vary in their components and can apply different service models, such as clinic-based approaches (in primary, secondary, or tertiary care), home-based programmes, case management, hybrids of these and telemonitoring. No service model has been shown to be consistently superior to others.12
The PONTE (i.e. bridge in English) project may represent an after discharge care model for HF based on hospital-health district cardiologists integration to optimize the clinical management of the HF patient after hospitalization. The results of the APULIA HF project, a registry also based on hospital-territory integration and published in 2017, showed an overall reduction in hospitalizations of 6%, a significant increase in the percentage of ACEi/ARB prescription, BBs, diuretics, MRAs, ivabradine, antiplatelet agents, anticoagulants, and lipid-lowering agents, an adherence of 79% to post-discharge control, 78% at 3 months, and 67% at 6 months, a significant increase in costs related to drug therapy (+660%) and outpatient assessments (+136%), conversely associated with a significant reduction in costs related to total hospitalizations (−56%) and hospitalizations with DRG 127 (−65%), resulting in overall reduction in total costs.13
After this preliminary experience, the PONTE-HF project was implemented; based on web-based hospital-territory integration to manage patients after hospitalization for HF. The project was characterized by the opportunity for all cardiologists involved, both in and out of the hospital, to share clinical data (demographic, clinical, laboratory, and instrumental data) in order to facilitate clinical follow-up after hospital discharge and adherence to guidelines recommendations.
The first relevant finding of this study was to demonstrate that the integration between hospital and out of hospital health care district clinics may improve adherence to HF guidelines and the prescription of recommended drugs for HFrEF even early at hospital discharge.
The demographic, clinical, and instrumental data of PONTE HF population are in line with the ESC Long Heart Failure registry population and showed same rates of prescription of ACEi/ARB and BB but more prescriptions of MRA therapy. The ARNI prescription was the same of the ESC Long Heart Failure registry and CHAMP registry (13%) since 2020 but in the last year, there was a significantly improvement of ARNI prescription. Increased rates of ARNI prescriptions may be partly explained also as a consequence of the PIONEER HF and TRANSITION HF publications,14,15 with results supporting the early initiation of ARNI therapy in the pre-discharge phase of hospitalization. In the Ponte HF, 30% of ARNI prescriptions were done before discharge.
In the last year, according to ESC guidelines published in 2021, a considerable rate of SGLT2i prescription was also observed (about 10% of the HFrEF population).
The second finding is the reduction of re-hospitalization from 10% before 2020 to 8% after. Also, re-hospitalization data are in line with the ESC Long Heart Failure registry where 1-year events are 12%.
Further randomized studies are surely warranted to confirm such preliminary data coming from an observational registry, but the opportunity to share clinical data of hospitalized HF patients, both in and out of the hospital, may facilitate the implementation and the adherence to guidelines recommendations.
Conclusions
The implementation of the PONTE project is associated with an improved adherence to guideline recommendations.
Conflict of interest: none declared.
Data availability
Data would be available on reasonable request.
References
- 1. McMurray JJ, Adamopoulos S, Anker SD, Auricchio A, Böhm M, Dickstein K, Falk V, Filippatos G, Fonseca C, Gomez-Sanchez MA, Jaarsma T, Køber L, Lip GY, Maggioni AP, Parkhomenko A, Pieske BM, Popescu BA, Rønnevik PK, Rutten FH, Schwitter J, Seferovic P, Stepinska J, Trindade PT, Voors AA, Zannad F, Zeiher A; ESC Committee for Practice Guidelines. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: the Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail 2012;14:803–869. [DOI] [PubMed] [Google Scholar]
- 2. McMurray JJ, Packer M, Desai AS, Gong J, Lefkowitz MP, Rizkala AR, Rouleau JL, Shi VC, Solomon SD, Swedberg K, Zile MR; PARADIGM-HF Investigators and Committees. Angiotensin-neprilysin inhibition versus enalapril in heart failure. N Engl J Med 2014;371:993–1004. [DOI] [PubMed] [Google Scholar]
- 3. Packer M, Anker SD, Butler J, Filippatos G, Pocock SJ, Carson P, Januzzi J, Verma S, Tsutsui H, Brueckmann M, Jamal W, Kimura K, Schnee J, Zeller C, Cotton D, Bocchi E, Bohm M, Choi DJ, Chopra V, Chuquiure E, Giannetti N, Janssens S, Zhang J, Gonzalez Juanatey JR, Kaul S, Brunner-La Rocca HP, Merkely B, Nicholls SJ, Perrone S, Pina I, Ponikowski P, Sattar N, Senni M, Seronde MF, Spinar J, Squire I, Taddei S, Wanner C, Zannad F; EMPEROR Reduced Trial Investigators. Cardiovascular and renal outcomes with empagliflozin in heart failure. N Engl J Med 2020;383:1413–1424. [DOI] [PubMed] [Google Scholar]
- 4. McMurray JJV, Solomon SD, Inzucchi SE, Køber L, Kosiborod MN, Martinez FA, Ponikowski P, Sabatine MS, Anand IS, Belohlávek J, Böhm M, Chiang CE, Chopra VK, de Boer RA, Desai AS, Diez M, Drozdz J, Dukát A, Ge J, Howlett JG, Katova T, Kitakaze M, Ljungman CEA, Merkely B, Nicolau JC, O’Meara E, Petrie MC, Vinh PN, Schou M, Tereshchenko S, Verma S, Held C, DeMets DL, Docherty KF, Jhund PS, Bengtsson O, Sjöstrand M, Langkilde AM; DAPA-HF Trial Committees and Investigators. Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med 2019;381:1995–2008. [DOI] [PubMed] [Google Scholar]
- 5. Vaduganathan M, Claggett BL, Jhund PS, Cunningham JW, Pedro Ferreira J, Zannad F, Packer M, Fonarow GC, McMurray JJV, Solomon SD.. Estimating lifetime benefits of comprehensive disease-modifying pharmacological therapies in patients with heart failure with reduced ejection fraction: a comparative analysis of three randomised controlled trials. Lancet 2020;396:121–128. [DOI] [PubMed] [Google Scholar]
- 6. Komajda M, Böhm M, Borer JS, Ford I, Tavazzi L, Pannaux M, Swedberg K.. Incremental benefit of drug therapies for chronic heart failure with reduced ejection fraction: a network meta-analysis. Eur J Heart Fail 2018;20:1315–1322. [DOI] [PubMed] [Google Scholar]
- 7.Authors/Task Force Members; McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, Burri H, Butler J, Čelutkienė J, Chioncel O, Cleland JGF, Coats AJS, Crespo-Leiro MG, Farmakis D, Gilard M, Heymans S, Hoes AW, Jaarsma T, Jankowska EA, Lainscak M, Lam CSP, Lyon AR, McMurray JJV, Mebazaa A, Mindham R, Muneretto C, Francesco Piepoli M, Price S, Rosano GMC, Ruschitzka F, Kathrine Skibelund A; ESC Scientific Document Group. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). With the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 2021;42:3599–3726. [DOI] [PubMed] [Google Scholar]
- 8. Tavazzi L, Senni M, Metra M, Gorini M, Cacciatore G, Chinaglia A, Di Lenarda A, Mortara A, Oliva F, Maggioni A; IN-HF (Italian Network on Heart Failure) Outcome Investigators. Multicenter prospective observational study on acute and chronic heart failure: one-year follow-up results of IN-HF (Italian Network on Heart Failure) outcome registry. Circ Heart Fail 2013;6:473–481. [DOI] [PubMed] [Google Scholar]
- 9. Kapelios CJ, Lainscak M, Savarese G, Laroche C, Seferovic P, Ruschitzka F, Coats A, Anker SD, Crespo-Leiro MG, Filippatos G, Piepoli MF, Rosano G, Zanolla L, Aguiar C, Murin J, Leszek P, McDonagh T, Maggioni AP, Lund LH; on behalf of the Heart Failure Long-Term Registry. Sacubitril/valsartan eligibility and outcomes in the ESC-EORP-HFA Heart Failure Long-Term Registry: bridging between European Medicines Agency/Food and Drug Administration label, the PARADIGM-HF trial, ESC guidelines, and real world. Eur J Heart Fail 2019;21:1383–1397. [DOI] [PubMed] [Google Scholar]
- 10. DeVore AD, Mi X, Thomas L, Sharma PP, Albert NM, Butler J, Hernandez AF, Patterson JH, Spertus JA, Williams FB, Duffy CI, McCague K, Fonarow GC.. Characteristics and treatments of patients enrolled in the CHAMP-HF registry compared with patients enrolled in the PARADIGM-HF trial. Am Heart Assoc 2018;7:e009237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Shanbhag D, Graham ID, Harlos K, Brian Haynes R, Gabizon I, Connolly SJ, Van Spall HGC.. Effectiveness of implementation interventions in improving physician adherence to guideline recommendations in heart failure: a systematic review BMJ Open 2018;8:e017765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Van Spall HGC, Rahman T, Mytton O, Ramasundarahettige C, Ibrahim Q, Kabali C, Coppens M, Brian Haynes R, Connolly S.. Comparative effectiveness of transitional care services in patients discharged from the hospital with heart failure: a systematic review and network meta-analysis. Eur J Heart Fail 2017;19:1427–1443. [DOI] [PubMed] [Google Scholar]
- 13. Iacoviello M, Pede S, Aspromonte N, Bux F, Panunzio M, Donadeo V, De Castro A, Antoncecchi E, D’Amato N, Squiccimarro E, Silvestri B, Malerba L, De Gennaro L, Modugno G, Serafini E, Curci B, Grande D, Colivicchi F, De Luca G, Ignone G, D’Agostino C, Caldarola P.. Studio multicentrico APULIA HF: efficacia di un protocollo di gestione condiviso fra ospedale e territorio dei pazienti ospedalizzati per scompenso cardiaco acuto. G Ital Cardiol 2017;18:150–158. [DOI] [PubMed] [Google Scholar]
- 14. Velazquez EJ, Morrow DA, DeVore AD, Duffy CI, Ambrosy AP, McCague K, Rocha R, Braunwald E; PIONEER-HF Investigators. Angiotensin-neprilysin inhibition in acute decompensated heart failure. N Engl J Med 2019;380:539–548. [DOI] [PubMed] [Google Scholar]
- 15. Wachter R, Senni M, Belohlavek J, Straburzynska-Migaj E, Witte KK, Kobalava Z, Fonseca C, Goncalvesova E, Cavusoglu Y, Fernandez A, Chaaban S, Bohmer E, Pouleur AC, Mueller C, Tribouilloy C, Lonn E, Buraiki ALJ, Gniot J, Mozheiko M, Lelonek M, Noè A, Schwende H, Bao W, Butylin D, Pascual-Figal D; TRANSITION Investigators. Initiation of sacubitril/valsartan in haemodynamically stabilised heart failure patients in hospital or early after discharge: primary results of the randomised TRANSITION study. Eur J Heart Fail 2019;21:998–1007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data would be available on reasonable request.


