Abstract
Introduction
There is little evidence regarding the treatment of stage IVB endometrial cancer. Therefore, chemotherapy is more likely to be chosen as the initial and first-line treatment. Pembrolizumab is a new treatment choice for unresectable endometrial cancer after first-line chemotherapy failure.
Presentation of case
Herein, we report the case of a 56-year-old patient diagnosed with stage IVB endometrial cancer. After eight cycles of first-line chemotherapy, computed tomography (CT) revealed relapse with re-enlargement of the para-aortic lymph nodes. Since the primary tumour had high microsatellite instability, we switched to pembrolizumab treatment. Pembrolizumab was effective but could not be continued due to adverse events after 10 cycles. Positron emission tomography-CT revealed active cancer in the uterus and para-aortic lymph nodes.
Discussion
Since pembrolizumab treatment had to be discontinued, we performed salvage surgery, which achieved complete tumour removal, and the patient has had no evidence of disease for 16 months.
Conclusion
This is the first case of complete surgical resection after administering pembrolizumab as a second-line treatment for advanced endometrial cancer.
Keywords: Endometrial cancer, Pembrolizumab, Salvage surgery, Case report
Highlights
-
•
This is the first report of complete resection of residual tumor after second-line treatment with pembrolizumab for stage IV endometrial cancer.
-
•
The present case is still showing no evidence of disease without additional treatment to date 16 months after this salvage surgery.
-
•
Pembrolizumab could be a neoadjuvant therapy for stage IV endometrial cancer with MSI-H.
1. Introduction
Chemotherapy is more likely to be chosen as initial treatment for inoperable advanced endometrial cancer [1]. Salvage surgery based on the response to neoadjuvant chemotherapy (NACT) is an effective treatment strategy. Tumours deficient in DNA mismatch repair (dMMR) have high microsatellite instability (MSI-H) and are likely to be immunogenic, triggering upregulation of immune checkpoint proteins. Pembrolizumab, an immune checkpoint inhibitor, has anti-tumour activity against MSI-H/dMMR cancer [2]. MSI-H is identified in approximately 30% of endometrial cancer tissues [3]. Pembrolizumab is a potential new treatment strategy for unresectable endometrial cancer after first-line chemotherapy failure for MSI-H endometrial cancer.
Herein, we present the first case of advanced endometrial cancer with MSI-H that could be completely resected by salvage surgery following administration of pembrolizumab as a second-line treatment. This report has been reported in line with the SCARE 2020 criteria [4].
2. Presentation of case
A 56-year-old non-gravida woman who became menopausal at 51 years reported some abnormal bleeding episodes with low back pain and lower abdominal pain after menopause. She was referred to us because of a solid tumour mass found on transvaginal ultrasonography. Her medical history included hypertension, hyperlipidaemia, and anaemia. She had a family history of hypertension (mother).
2.1. Investigations
Pelvic examination revealed a fist-sized, immobile uterus and a mass causing mild pain in the Douglas fossa. Transvaginal ultrasonography revealed a solid tumour in the uterine body that reached the serosal uterine surface. Histology of the tumour biopsy sample of the uterine cavity indicated endometrioid carcinoma (grade 2).
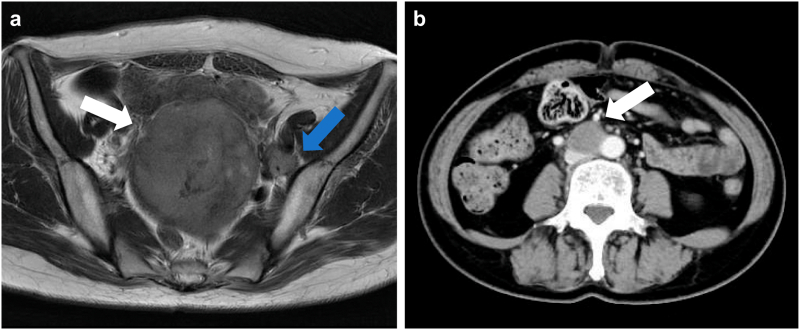
Magnetic resonance imaging revealed a 9-cm mass occupying almost the entire uterus. The mass was enhanced nonuniformly on contrast-enhanced imaging. It showed high intensity on T2-weighted imaging (Fig. 1a). Contrast-enhanced positron emission tomography-computed tomography (PET-CT) confirmed the presence of multiple para-aortic lymph node metastases (maximum size of minor diameter was 25 mm) (Fig. 1b), pelvic lymph node metastases, left supraclavicular lymph node metastasis, peritoneal dissemination, and lung metastasis. Tumour marker assessment indicated elevated serum CA125 (303.0 U/mL) and CA19–9 (117.2 U/mL) levels.
Fig. 1.
MRI and CT before first-line treatment
(a) MRI (high intensity on T2WI) revealed a 9-cm mass occupying almost the size of the entire uterus (white arrow) and 15-mm left obturator lymph node metastasis (blue arrow). (b) Contrast-enhanced CT confirmed the presence of multiple para-aortic lymph node metastases (white arrow).
MRI: magnetic resonance imaging; CT: computed tomography; T2W1: T2-weighted imaging. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
2.2. Differential diagnosis
The patient was diagnosed with stage IVB endometrial cancer based on tumour histology and distant metastases observed on CT.
2.3. Treatment
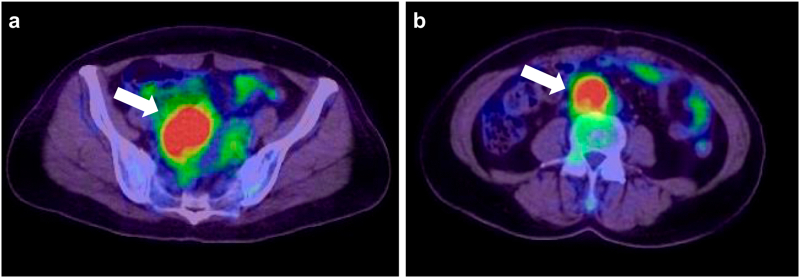
Systemic chemotherapy was initiated with paclitaxel (175 mg/m2) + carboplatin (AUC 6) as the first-line regimen. After three cycles, CT indicated partial response; the tumour in the uterus had shrunk to 4 cm in diameter, the para-aortic lymph nodes shrunk to 2 cm in diameter, and the lung metastases disappeared. Serum CA125 and CA19–9 levels decreased after six cycles but increased after the seventh cycle. After eight cycles, CT revealed re-enlargement of the para-aortic lymph nodes. Since the primary tumour was MSI-H, we decided to switch to pembrolizumab treatment (200 mg/kg body weight every 3 weeks). After 10 cycles of pembrolizumab administration, CT showed stable disease (SD), and serum CA125 (26.0 U/mL) and CA19–9 (15.5 U/mL) levels decreased to within normal ranges. Following a grade 3 immune-related adverse event (AE) of liver dysfunction, pembrolizumab was discontinued. The AE rapidly improved with steroid administration. Three months after pembrolizumab discontinuation, the tumour in the uterus had increased to 5 cm in diameter, and serum CA125 (30.4 U/mL) and CA19–9 (85.4 U/mL) levels increased again. Furthermore, the tumour in the uterus (Fig. 2a) and para-aortic lymph nodes (Fig. 2b) were fluorodeoxyglucose-avid on PET-CT. Therefore, we decided to perform salvage surgery (total abdominal hysterectomy + bilateral salpingo-oophorectomy + removal of the para-aortic lymph node metastasis).
Fig. 2.
PET-CT 3 months after discontinuation of pembrolizumab
(a) The uterus (white arrow) and (b) para-aortic lymph node metastases (white arrow) showed high FDG uptake.
PET-CT: positron emission tomography-computed tomography; FDG: fluorodeoxyglucose.
Macroscopically, there were small ascites, and the goose egg-sized uterus had white lesions and was suspected of infiltrating the left-sided serosal uterine surface. The ovaries and fallopian tubes appeared normal, and the pelvic peritoneum was generally thickened. Dissemination-suspected nodules were found on the left side of the vesico-uterine pouch peritoneum. Total abdominal hysterectomy and bilateral salpingo-oophorectomy, including removal of the dissemination-suspected peritoneum, were performed by a gynaecologic oncologist. The swollen para-aortic lymph node on PET-CT, measuring 3 cm by palpation, was visible on the right side of the aorta, cranial side of the common iliac artery bifurcation, and caudal side of the inferior mesenteric artery (Fig. 3). This node was also removed during the surgery; complete tumour resection was performed. Fig. 4 shows the resected specimens, including those of the uterine cavity, ovaries, fallopian tubes, and para-aortic lymph nodes.
Fig. 3.
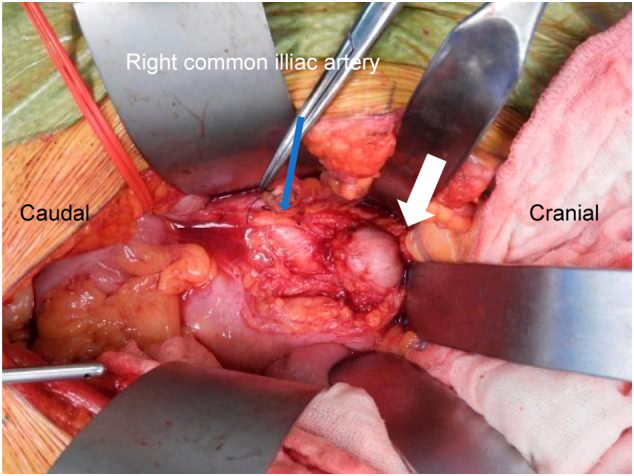
Macroscopic image of the metastatic para-aortic lymph node intraoperatively (white arrow). Metastatic para-aortic lymph was located caudally below the right renal vein.
Fig. 4.
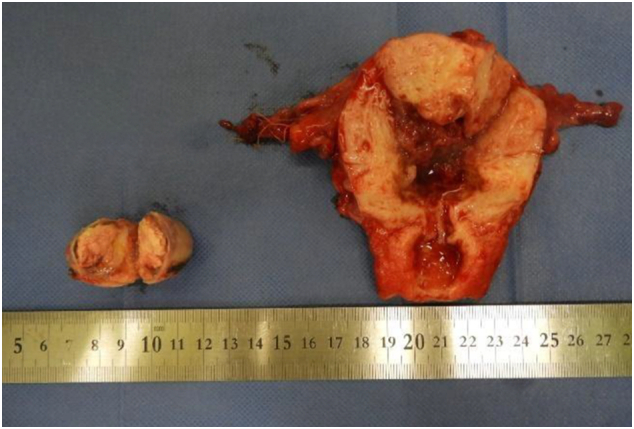
Macroscopic findings of the specimen
(Left) Almost all of the uterine corpus was replaced by the tumour. The cervix, ovaries, and fallopian tubes were normal.
(Right) The cut surface of the para-aortic lymph node was solid with central necrosis.
Pathological evaluation was suggestive of endometrial carcinoma (G2), ypT1bpN2Mx, ly (+), v (−) (Fig. 5). Regarding pathological and cytological findings, the ascites was benign, and viable tumour cells were observed in most of the residual tumour mass. More than half the myometrium was invaded. The tumour cells partially invaded the serosal surface of the uterus, but the lesion did not spread along the serosal surfaces or the uterine cervix. Tumour cells were not found in the nodules on the left side of the vesico-uterine pouch peritoneum. These tumour cells were oestrogen receptor-positive and focally progesterone receptor-positive. The resected para-aortic lymph node was pathologically invaded by endometrial carcinoma (G2), similar to the uterus. However, this para-aortic lymph node metastasis did not show extra-nodal invasion.
Fig. 5.
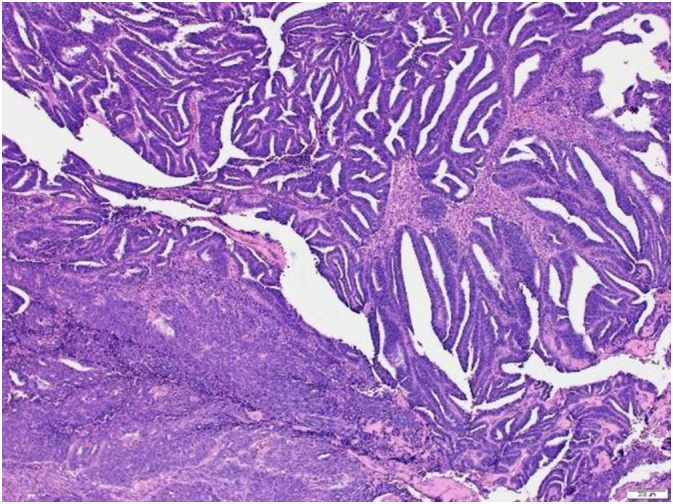
Pathological findings of the uterus (haematoxylin and eosin staining. Original magnification ×40)
Cancer cells forming a distorted ductal structure proliferated densely and solid growth were also partially observed. These viable tumour cells were observed in the corpus. Similar findings were observed in the para-aortic lymph node.
2.4. Outcome and follow-up
The postoperative course was uneventful. Adjuvant therapy was not administered due to complete resection; instead, we continued routine follow-up (medical examination, tumour marker and CT). The patient has been healthy and has had no evidence of disease for 16 months after the salvage surgery.
3. Discussion
In the reported case, we performed complete surgical resection after second-line pembrolizumab treatment following initial chemotherapy for advanced endometrial cancer. Treatment strategy for stage IV endometrial cancer typically involves using multiple modalities, such as surgical therapy, chemotherapy, radiation therapy, and hormone therapy. There is little evidence regarding the treatment of stage IVB endometrial cancer because of the lack of available data. de Lange et al. examined patients with advanced endometrial cancer who were not suitable for primary debulking and determined that NACT followed by interval debulking surgery (IDS) was the most appropriate treatment. IDS can be considered suitable regardless of the histologic subtype [1]. Eto et al. reported that hysterectomy and chemotherapy are independent prognostic factors for survival and that combined hysterectomy and chemotherapy may benefit patients with stage IVB endometrial cancer. The subgroup analysis showed that the overall survival was similar between patients who underwent primary chemotherapy followed by surgery and those who underwent primary surgery alone [5]. In the present case, we suggested that complete resection would be difficult according to imaging examinations. Therefore, we initially treated the patient with chemotherapy.
Although the tumour temporarily responded to chemotherapy, PET-CT indicated re-expansion of the para-aortic lymph node metastasis. Approximately 30% of endometrial cancers are MSI-H [3]. KEYNOTE-158 included 49 patients with endometrial cancer (21% of the participants in the trial) and reported an objective response rate of 57% [2]. Pembrolizumab has become a new treatment strategy for these patients. In the present case, because the tumour was MSI-H, the patient was administered pembrolizumab. After 10 cycles, CT showed SD, and serum CA125 and CA19–9 levels decreased to within the normal range. Although pembrolizumab treatment had to be discontinued due to AE, we switched to salvage surgery and achieved complete tumour removal.
To the best of our knowledge, this is the first report of salvage surgery after pembrolizumab treatment in endometrial cancer. In cases where residual lesions are localised after pembrolizumab treatment, salvage surgery should be considered. Accumulating similar experiences may promote the administration of NACT with pembrolizumab as a new strategy.
4. Conclusion
We report the first case of complete surgical resection after using pembrolizumab as a second-line treatment method after chemotherapy for advanced endometrial cancer.
Patient's perspective
When I first heard about stage IV endometrial cancer, I was very surprised. Chemotherapy was a challenging experience because of hair loss, numbness in the limbs, and light-headedness. In contrast, the side effects while taking pembrolizumab were few. I thank the doctors and medical staff. The course is also uneventful, and I am grateful that I remain healthy now.
Funding sources
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approval
This case report has been approved by the ethics committee of our hospital.
The approval number is 2102005.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Research registration
None.
Guarantor
Kimihiko Ito.
Provenance and peer review
Not commissioned, externally peer-reviewed.
CRediT authorship contribution statement
Tomomi Taguchi (corresponding author): Patient treatment and writing the original draft.
Kimihiko Ito: Patient treatment, reviewing and editing the manuscript, and supervision.
Michiko Yamashita and Tomomi Egawa-Takata: Patient's treatment and review and editing the manuscript.
Declaration of competing interest
All authors have no conflict of interest.
Acknowledgements
We would like to thank Editage (www.editage.com) for English language editing.
References
- 1.de Lange N.M., Ezendam N.P.M., Kwon J.S., Vandenput I., Mirchandani D., Amant F., et al. Neoadjuvant chemotherapy followed by surgery for advanced-stage endometrial cancer. Curr. Oncol. 2019;26:e226–e232. doi: 10.3747/co.26.4655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Marabelle A., Le D.T., Ascierto P.A., Di Giacomo A.M., De Jesus-Acosta A., Delord J.P., et al. Efficacy of pembrolizumab in patients with noncolorectal high microsatellite instability/mismatch repair–deficient cancer: results from the phase II KEYNOTE-158 study. J. Clin. Oncol. 2020;38:1–10. doi: 10.1200/JCO.19.02105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bonneville R., Krook M.A., Kautto E.A., Miya J., Wing M.R., Chen H.Z., et al. Landscape of microsatellite instability across 39 cancer types. JCO Precis. Oncol. 2017:1–15. doi: 10.1200/PO.17.00073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Agha R.A., Franchi T., Sohrabi C., Mathew G., Kerwan A., SCARE Group The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 5.Eto T., Saito T., Shimokawa M., Hatae M., Takeshima N., Kobayashi H., et al. Status of treatment for the overall population of patients with stage IVb endometrial cancer, and evaluation of the role of preoperative chemotherapy: a retrospective multi-institutional study of 426 patients in Japan. Gynecol. Oncol. 2013;131:574–580. doi: 10.1016/j.ygyno.2013.08.036. [DOI] [PubMed] [Google Scholar]