Abstract
Background
Asymptomatic and high-risk COVID-19 patients are advised to self-isolate at home. However, patients may not realize that the condition is deteriorating until too late.
Objective
This study aims to review various artificial intelligence-based telemedicine research during the COVID-19 outbreak and proposes a framework for developing telemedicine powered by artificial intelligence to monitor progression in COVID-19 patients during isolation at home. It also aims to map challenges using artificial intelligence-based telemedicine in the community.
Methods
A systematic review was performed for the related articles published in 2019–2021 and conducted in the PubMed and ScienceDirect database using the keywords “telemedicine,” “artificial intelligence,” and “COVID-19”. The inclusion criteria were full-text articles and original research written in the English language.
Results
Thirteen articles were included in this review to describe the current application of artificial intelligence-based telemedicine during the COVID-19 pandemic. Various current applications have been implemented, such as for early diagnosis and tracing of contact for the users, to monitor symptoms and decision-making treatment, clinical management, and virtual and remote treatment. We also proposed the framework of telemedicine powered by artificial intelligence for support the self-isolation of COVID-19 patients based on the recent update in technology. However, we identified some challenges for using digital health technologies because of the ethical and practical use, the policy and regulation, and device use both for healthcare workers and patients.
Conclusion
Artificial intelligence promises to improve the practice of medicine in various ways. However, practical applications still need to be explored, and medical professionals also need to adapt to these advances for better healthcare delivery to the public.
Keywords: Artificial intelligence, telemedicine, COVID-19, self-isolation patient
Introduction
It has been highlighted that the emergence of the coronavirus disease 2019 (COVID-19) pandemic in the world, including in Indonesia, posed a new challenge to the efforts to control infectious diseases. COVID-19 is characterized by a range of clinical signs of asymptomatic infection. 1 COVID-19 can also be particularly dangerous for certain high-risk patients, including elderly patients and those with specific pre-existing health conditions. 2 In practice, asymptomatic and high-risk patients self-isolate at home and are expected to call their doctor if their condition worsens.3,4 However, patients can begin to deteriorate without notice, and by the time they realize that something is mistaken, the chance for early life-saving treatment may have been missed. 4 Based on the issue, it is necessary to develop methods to communicate efficiently with asymptomatic and high-risk COVID-19 patients under self-isolation at home.
Telemedicine is a term that was invented back in the 1970s, which means “healing from afar” and refers to information communication technology used to improve society's health and well-being by enhancing access to healthcare information. 5 It allows clinicians to provide health services when social distancing is needed without direct contact with patients. 6 The most commonly used technologies are voice and video calls. 7 Telemedicine allows using technology without requiring healthcare professionals and patients to be in the same place. 8 Telemedicine combines convenience, comfortability, and low-cost access to information regarding health and communication technology to support health practice remotely through phone, video, email, and mobile health applications.8,9 However, data security problems, poor user education background, and lack of telemedicine features have been found as the problems faced today in the application of telemedicine in the community. 10
Although artificial intelligence (AI) was initially introduced > 60 years ago, the rapid evolution of AI-based technology and applications occurred after the improvement of graphic processing units in the 2010s. 11 AI is the term used to describe computers and technology to simulate intelligent behavior and critical thinking comparable to a human being. 12 John McCarthy first defined AI in 1956 as the science and engineering of making intelligent machines. 13 Recently, AI algorithms have been studied and established in various medical fields to facilitate exam interpretations, improve the accuracy of diagnoses, and reduce time and human resource consumption. 14
This review focuses on recent advances in AI technology and its current application in telemedicine during the COVID-19 era. The proposed framework for the development of telemedicine powered by AI to support self-isolation in COVID-19 patients is provided in the following description. It also identifies the challenges and acceptable use of AI in telemedicine during the COVID-19 era. The contributions of this article are summarized as follows:
Provide a clear insight into the current implementation of AI in telemedicine for various diseases during the COVID-19 outbreak.
Identify challenges and recommend solutions for researchers to develop an advanced AI-based telemedicine system for quarantining of COVID-19 patients based on the integration of recent studies.
Helps policymakers and clinicians identify the key points for implementing AI-based telemedicine in patients.
Methods
To give a brief description of the current application of AI-based telemedicine during the COVID-19 pandemic in the medicinal field, we conducted a systematic review in accordance with the Preferred Reporting Item for Systematic reviews and Meta-Analyses. 15 It includes various processes: information source and eligibility criteria, study selection, and data extraction.
Information source and eligibility criteria
The selection for the related article published in 2019–2021 was conducted in the PubMed and ScienceDirect database using the keywords “telemedicine,” “artificial intelligence,” and “COVID-19.” The inclusion criteria were full-text articles written in the English language and original research studies. We excluded the articles that did not describe the use of AI-driven technology in telemedicine in COVID-19 cases or other diseases during the COVID-19 pandemic, protocol studies, conference abstracts, case reports, commentaries, editorials, and reviews.
Study selection
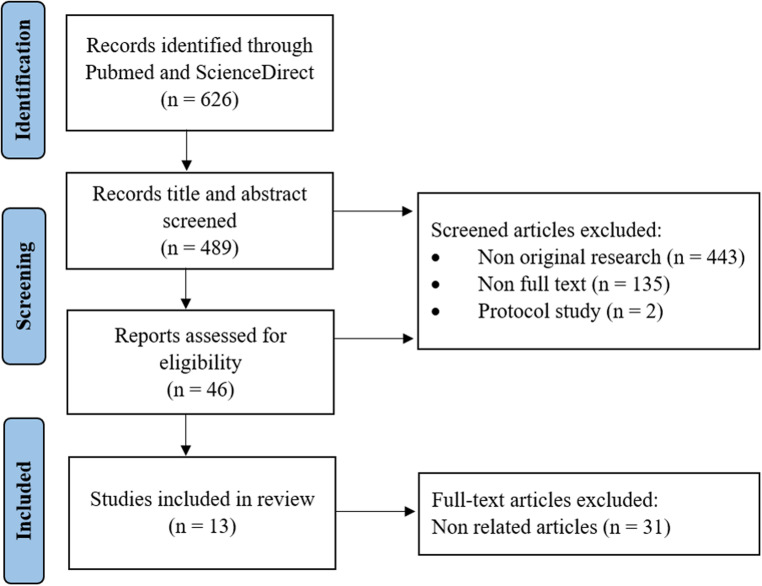
The search process of this study consisted of three sub-processes, they are a collection of articles, scanning of title and abstract, and reading of the full text. Each article was assessed by two reviewers to ensure the inclusion criteria and the extracted data. Any disagreement between the two reviewers was resolved by a senior reviewer. The senior reviewer also evaluated the quality of the included articles to ensure their significance to this review. A total of 626 publications were found, 13 of which met the inclusion criteria (Figure 1).
Figure 1.
Flow diagram of inclusion and exclusion of studies. Reasons for exclusion are conference abstract, case reports, commentaries, editorials, protocols, and reviews (narrative review, systematic review, and meta-analysis).
Data extraction
We extracted the required data and collected it for further analysis manually using an Excel spreadsheet. The numerous parameters such as title, year, type of articles, and the result were selected for achieving the key points of the systematic reviews.
Telemedicine and AI during COVID-19 era: Current application
AI is growing into the public health sector and will significantly impact every aspect of primary care. AI in medicine can be divided into two subtypes: virtual and physical. The virtual component is represented by Machine or Deep Learning, represented by mathematical algorithms that improve learning through experience. It enables “systems thinking” about healthcare; it not only focuses on the classical interactions between patients and providers but also considers larger-scale organizations and cycles. The virtual part ranges from electronic health record systems to neural network-based guidance in treatment decisions. 13
The second form of application of AI in medicine includes physical objects, medical devices, and increasingly sophisticated robots in care delivery. 16 The most promising approach is using robots as helpers; for example, a robot companion for the aging population with cognitive decline or limited mobility. Robots are used in surgery as assistant surgeons or even as solo performers. 17 The physical part deals with robots assisting in performing surgeries, intelligent prostheses for disabled people, and elderly care.
The current research focuses on utilizing AI developments to support various diseases, including COVID-19 during the Coronavirus outbreak. It is categorized under several uses: early diagnosis and tracing of contacts, monitoring symptoms and decision-making treatment, clinical management, and virtual and remote treatment (Table 1).
Table 1.
Implementations of recent technologies in medicine during the COVID-19 era.
| References | Subject | Study design | Highlight | Function |
|---|---|---|---|---|
| Miyake et al. 18 | Ten clinicians from the COVID team who used a CT-first triage protocol and telemedicine for 165 individuals inpatients and outpatients | Participants were evaluated the serum-specific antibodies for SARS-CoV-2 at the initial and end of the study, PCR at the end of the study, and 36-item short-form of the Medical Outcome Study Questionnaire | Combination of telemedicine and CT protocol was found to help the medical staff protect from the risk of infection who dealt with COVID-19 patients | Contact tracing |
| Alodat 19 | Eleven participants were randomly chosen from different areas who had respiratory symptoms | Eligible participants have made chest X-ray images to analyze and predict COVID-19. Four robust models in real-time telemedicine were developed and used to assist those X-ray images | Deep learning-based real-time medicine using Convolutional Neural Networks using Tensorflow (CNN-TF) model was able to discriminate between positive and negative COVID-19 cases | Diagnosis |
| Bassam et al. 20 | The study did not directly simulate humans. The AI model was trained using a recording signal for both cough and noise for 10 s | The proposed system is implemented with three-layered functionalities as wearable IoT sensor layer, cloud layer with API and Android web layer for mobile phones. These integrated systems were trained to predict signs of COVID-19 patients | IoT-based wearable monitoring device was designed to measure various vital signs related to COVID-19, such as body temperature, oxygen saturation in the blood, heartbeat monitoring, respiratory system | Monitoring signs and symptoms |
| Sharma et al. 21 | The study did not directly simulate humans. Simulations were done using the R software and cooza simulator | Proposed diagnostic model was based on electrocardiogram, photoplethysmography, temperature, and accelerometer and was validated using 10-fold cross-validation. Accuracy of the model was trained to classify the patients into an infected and non-infected | Bio wearable sensor system based on ontology method used sensory 1D biomedical signals to monitor remote patients and provide medical help to distant locations | Decision-making treatment |
| Faris et al. 22 | A total of 246,814 consultations and 1206 diagnoses were collected from Altibbi company | The system was built from a fusion of ML models trained based on two modalities: the symptoms and the medical questions of the patients | Combination of telemedicine and computer-aided intelligence was reported to help doctors and clinicians in making correct treatment decisions based on the given symptoms and patients’ questions | Decision-making treatment |
| Dawoodbohy et al. 23 | 9 mental health healthcare practitioners (HCPs) and 11 artificial intelligence (AI) experts | Combination of a narrative literature review and pilot interview was conducted with AI and mental health experts | AI integrated with telemedicine is utilized to improve the delivery of preventive and personalized care for mental health condition patients | Preventive and clinical management |
| Miyake et al. 18 | Ten doctors of the COVID team, who used a CT-first triage protocol and telemedicine for 165 individuals inpatients and outpatients | Evaluation of serum-specific antibodies for SARS-CoV-2 at the initial and end of the study, PCR result at the end of the study, and 36-item short-form of the Medical Outcome Study Questionnaire | Deep learning-based real-time medicine using the Random Forest classification model could predict patients with a risk of death and provide appropriate healthcare | Clinical management |
| Adly et al. 24 | In total, 60 participants with stage 1 pneumonia caused by SARS-CoV-2 infection | Group A received oxygen therapy with bilevel positive airway pressure ventilation, and group B received osteopathic manipulative respiratory and physical therapy techniques. Arterial blood gases, pH, vital signs, and chest CT scans were used for follow-up and assessment | A newly developed Telemanagement with home-based oxygen therapy with bilevel positive airway pressure was found to be more effective for prophylactic treatment in early-stage COVID-19 pneumonia | Clinical management |
| Keenan et al. 25 | Four individuals (mean age, 73.8 years) with neovascular age-related macular degeneration (one or both eyes) undergoing anti-vascular endothelial growth factor therapy | Eligible participants performed daily self-imaging with the NVHO coherence tomography for 1 month. The macular cube scans were uploaded automatically to the Notal Health Cloud. They underwent evaluation separately by the Notal OCT Analyzer and human expert graders for fluid presence, segmentation, and volume | Telemedicine powered by NVHO-based deep learning is used to evaluate neovascular age-related macular degeneration patients who do a home treatment. It may allow highly personalized retreatment decisions, with fewer unnecessary injections and clinic visits | Virtual and remote treatment |
| Chae et al. 26 | In total, two groups of stroke survivors contain 17 and 6 participants were enrolled for statistical analysis | An HBR system involves an off-the-shelf smartwatch, a smartphone, and custom-developed apps. A convolutional neural network was used to train the ML algorithm for detecting home exercises | A smartphone app equipped with an ML created with accelerometer and gyroscope data performed effectively and improved the wolf motor function in HBR chronic stroke patients | Virtual and remote treatment |
Note: CT: computed tomography; API: application peripheral interface; NVHO coherence tomography: Notal Vision Home Optical coherence tomography; HBR: home-based rehabilitation; ML: machine learning.
Early diagnosis and tracing of contact for the users
Miyake et al. 18 conducted a study of the active telemedicine method and computed tomography (CT) protocol to reduce the risk of infection in a medical and non-medical team dealing with COVID-19 patients. It showed no positive serum-specific antibody testing and polymerase chain reaction testing results for SARS-CoV-2 in a group of COVID doctors. Furthermore, the 36-item short-form of the Medical Outcome Study Questionnaire showed no deterioration in physical and mental quality of life status. No in-hospital infection occurred during the study period. The combination strategy seems acceptable for both the protection and stress relief among the medical staff.
Alodat et al. 19 created real-time telemedicine powered by various deep learning-based real-time telemedicine for adapting and managing the COVID-19 pandemic crisis. It was reported that Convolutional Neural Networks using Tensorflow (CNN-TF) model were capable of discriminating between those with positive cases of COVID-19 and those with negative cases. Another model, the Random Forest classification, was found to predict COVID-19 patients at risk of death and provided appropriate healthcare assistance. 19 Chest X-ray image analysis was also performed to provide a differential diagnosis of respiratory diseases related to COVID-19.
Monitor symptoms and decision-making treatment
Bassam et al. 20 designed the Internet of Things (IoT) based wearable monitoring device to measure various vital signs related to COVID-19. The system will automatically alert the concerned clinical authorities about quarantine violations for potentially infected patients by monitoring their real-time GPS data. The proposed approach is implemented with three-layered functionalities: wearable IoT sensor layer, cloud layer with Application Peripheral Interface, and android web layer for mobile phones. This design may serve as an essential part of COVID-19 patients and can be used as a monitoring device to track the health and recovery of a COVID-19 patient.
Another IoT-based remote access was also developed by Sharma et al. 21 They combined it with an alarm-enabled bio wearable sensor system for the early detection of COVID-19. The design was based on the ontology method using sensory 1D biomedical signals such as electrocardiogram, photoplethysmography, temperature, and accelerometer to monitor remote patients and provide medical help to distant locations. It was reported that the efficiency of the proposed model was 96.33% to distinguish between COVID-19 patients and suspected COVID-19 patients.
A recent study proposes a computer-aided intelligent diagnosis decision support system as part of telemedicine to help clinicians make a correct decision. The design encompasses a fusion of machine learning (ML) models trained based on two modalities: the patients’ symptoms and the medical questions. The output of the combination showed promising predictive ability with a classification accuracy of 84.9%, indicating the potential of the model in predicting the diagnosis of possible patient conditions based on the given symptoms and patients’ questions that consequently could aid clinicians in making the right decisions. 22
Clinical management
Semi-structured interviews were conducted with AI and mental health experts. The data were then used to analyze and synthesize gathered data to construct an enhanced model with potential AI solutions integrated with telemedicine. The result showed that AI tools could enable improved delivery of preventive and personalized care by opening up new data collection and analysis avenues to enhance understanding of mental health conditions. For example, “active data” will be collected with active involvement from the patient, such as completing surveys or contributing audio samples using digital apps. They are then analyzed with AI to tailor services to the individual by further engaging patients in their recovery process. However, “passive data” can also be collected from digital devices via mobile applications. The smartphone application will collect data from mobile sensors and phone usage, such as location and SMS logs, to monitor the state of a patient's disease. 23
Adly et al. 24 compared the nonpharmacological respiratory treatment methods for home-isolated COVID-19 patients using a new Telemanagement healthcare system. It was found that home-based oxygen therapy with bilevel positive airway pressure can be a more effective prophylactic treatment than osteopathic manipulative respiratory and physical therapy techniques because it can impede exacerbation of early-stage COVID-19 pneumonia.
Virtual and remote treatment
The system's performance of Notal Vision Home Optical (NVHO) coherence tomography, telemedicine infrastructure for automated data upload, and deep learning algorithm for automated optical coherence tomography of self-imaging at home were evaluated in longitudinally neovascular age-related macular degeneration patients. It was found that 87.9% of patients initiated self-imaging and 97.6% of these had satisfactory image quality. Thus, it may allow highly personalized retreatment decisions with fewer clinic visits and alternative disease monitoring during the COVID-19 pandemic. 25
A previous study developed a home-based rehabilitation (HBR) system that could recognize and record the type and frequency of rehabilitation exercises conducted by the user using a smartwatch and smartphone app equipped with an ML algorithm in chronic stroke survivors during the COVID-19 pandemic. It was found that the ML model created with accelerometer and gyroscope data was the most accurate (99.80%). It also performed a significant improvement (17/22) in the Wolf Motor Function Test for HBR patients. 26
Designing telemedicine powered by AI to support self-isolation of COVID-19 patients
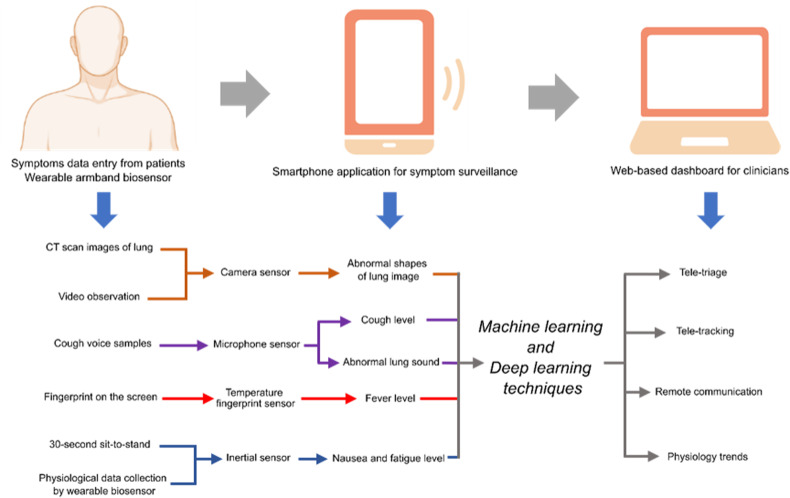
A built-in smartphone sensor can be implemented to test the capturing functions of COVID-19 symptoms in the diagnosing process. The parameters input are CT scan images of the lung, 30-s sit-to-stand, cough voice samples, and fingerprint on the screen. The smartphone's camera, microphone, and temperature fingerprint sensor can detect all these parameters to calculate abnormal sub-image lung shapes, nausea or fatigue level, cough level, and fever level. Based on a developed algorithm, symptom prediction will be analyzed by ML techniques for positive or negative COVID-19 initial results. 27 Inception Residual Recurrent Convolutional Neural Network with Transfer Learning (TL) can also be integrated into telemedicine to evaluate X-ray and CT scan images to detect COVID-19 cases (Figure 2). 28
Figure 2.
The framework of a smartphone application for supporting self-isolation COVID-19 patients.
A deep-learning algorithm can be used to diagnose and stratify the risk of COVID-19 from lung sounds. It is based on the fact that abnormal lung sounds have characteristic frequencies and duration, differentiating them from normal lung sounds. 29 Several data augmentation techniques will be explored, such as amplitude scaling, pitch shift, and random time shift. This data set will then be fed into a convolutional neural network with max-pooling and dropout before binary classification by a support vector machine into positive versus negative COVID-19 test results (diagnostic model) or hospitalization versus outpatient. 30
Wearable biosensors can be developed to continuously monitor multidimensional physiological parameters for the early detection of COVID-19 clinical progression. The physiological parameters monitored include skin temperature, respiratory rate, blood pressure, pulse rate, blood oxygen saturation, and daily activities rather than relying solely on temperature measurement. The wearable biosensor will be integrated with a specially designed smartphone application, and the patient can report their symptoms and record their cough sound using the smartphone. The analytics engine will process these multidimensional physiology parameters to detect subtle physiological changes preceding critical events, thereby enabling clinicians to review and intervene promptly. 31
Challenges and acceptable use of telemedicine and AI
The COVID-19 pandemic has become an additional accelerator of changes in terms of the healthcare system digitization. It brings healthcare workers closer to the patient, supporting the exchange of medical data between the doctor and the patient and improving the circulation of information. However, digital healthcare such as telemedicine has been debatable because of privacy and security, data format and management, synchronization, over-tracking, and lack of proper development and implementation guidelines that impact their efficacy and adoption. 32 This is exacerbated by hasty, poor user engagement, ill-prepared, or poorly communicated implementation of telemedicine that ultimately influences public trust 33
Trust in the age of digital healthcare
It is confirmed that the challenges of digital technology systems in the healthcare sector are not only technical since they are rooted and linked to the need to create a high level of trust in such scenarios. It is the foundation for the ethical and practical use of new digital tools in increased awareness and the more active role of patients in the treatment process. Even though a number of studies concerning trust in technology have been undertaken so far, the problem of trust in such systems is still up-to-date and requires further exploration. 34
Mbunge et al. 35 identified transparency, regular engagement, and possible user parameters to boost public trust However, poor communication and hasty implementation of digital healthcare will undermine public confidence and further risk efficacy. Despite the beneficial impact of digital healthcare, its integration into clinical practice should be carefully observed to avoid the potential violation of ethical practices and regulatory policies.
The policy and regulation of digital healthcare
The future of digital healthcare will be significantly influenced by a complex set of policy, legal, and regulatory frameworks. An understanding of these frameworks will help clinicians more effectively adopt and implement telemedicine platforms. Chen et al. 36 analyzed the impact of policy instruments to promote telemedicine interventions for COVID-19. It was reported that around 62% of policies aimed to strengthen clinical service, and more telemedicine technology interventions were implemented in clinical services (38.7%). However, emergency planning and preparedness had the least self-reported telemedicine intervention (27.1%). The adoption of telemedicine has been limited by licensure requirements, which impose compliance burdens on clinicians. Policymakers could reduce this burden by providing a telemedicine practitioner licensing pathway that would enable clinicians to practice telemedicine more easily. 37
Challenges in device use
Many digital health technologies for various diseases are currently available. However, adaptation into clinical practice by healthcare workers as well as patients is unclear. A recent electronic survey found that patients are likely to use digital healthcare recommended by healthcare practitioners (HCPs), as reported by Ding et al. 38 for digital health devices for atrial fibrillation (AF). A total of 53.4% of patients wanted guidelines from their HCP for optimal use. Around 64% of patients wanted more data comparing the accuracy of digital devices to conventional devices for AF monitoring. It can be observed that expanding familiarity with digital technology to general practitioners is needed. Device accuracy and improvement are also barriers identified by patients who want to use a digital device. Another study shows that many digital health technologies frequently did not provide a patient with the choice of a clinician or transparent clinician credentials and offered diagnoses without adequate medical history-taking. 39
Limitation
However, our study has limitations. Although the selected articles in our study supported the study approach, we only focused on two databases, PubMed and ScienceDirect, to identify the articles that met our article selection criteria. Thus, other related articles may not have been identified because they are not in those two databases. Despite the limitation, our study has described the current implementation of AI in telemedicine in various diseases during the COVID-19 outbreak. It also gives clear insights into the policymakers and clinicians to identify the key point for implementing AI-based telemedicine in patients.
Conclusion
AI promises to change the practice of medicine so far in various ways. However, many practical applications are still in their infancy and need to be explored and developed better. Medical professionals also need to understand and adapt to these advances for better healthcare delivery to the public. Moreover, support from a set of policies, regulatory frameworks, and data transparency are important keys leading to the more accessible use of telemedicine.
Acknowledgment
This study was supported by the Center of Excellence in Higher Education for Pharmaceutical Care Innovation, Universitas Padjadjaran.
Footnotes
Conflict of interest: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Contributorship: All authors make authorship contributions including conceptualization, expertise, technicalities, preparation of the initial draft, review, and revision of the final version of this study.
Ethical approval: Not applicable; no human subjects involvement.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Intan R Hartanti https://orcid.org/0000-0003-0538-5352
Dian AE Pitaloka https://orcid.org/0000-0002-8187-8864
References
- 1.Kronbichler A, Kresse D, Yoon S, et al. Asymptomatic patients as a source of COVID-19 infections: a systematic review and meta-analysis. Int J Infect Dis 2020; 98: 180–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020; 382: 1708–1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.CDC. Healthcare workers. Centers for Disease Control and Prevention, https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-guidance-management patients.html (2020, accessed 30 October 2021).
- 4.You Y, Yang X, Hung D, et al. Asymptomatic COVID-19 infection: diagnosis, transmission, population characteristics. BMJ Support Palliat Care 2021; 0: 002813. [DOI] [PubMed] [Google Scholar]
- 5.WHO. Telemedicine: Opportunities and Developments in Member State | Regional Office for Africa, https://www.afro.who.int/publications/telemedicine-opportunities-and-developments-member-state (2009, accessed 6 November 2021).
- 6.CDC. Telemedicine, https://www.cdc.gov/coronavirus/2019-ncov/global-covid-19/telemedicine.html (2020, accessed 30 October 2021).
- 7.Tozour JN, Bandremer S, Patberg E, et al. Application of telemedicine video visits in a maternal-fetal medicine practice at the epicenter of the COVID-19 pandemic. Am J Obstet Gynecol MFM 2021; 3: 100469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Banks J, Corrigan D, Grogan R, et al. LoVE in a time of COVID: clinician and patient experience using telemedicine for chronic epilepsy management. Epilepsy Behav EB 2021; 115: 107675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vidal-Alaball J, Acosta-Roja R, Pastor Hernández N, et al. Telemedicine in the face of the COVID-19 pandemic. Aten Primaria 2020; 52: 418–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Medical Clinic Express. 24 Hr TeleHealth Care, https://livetelemdcare.com (2020, accessed 30 October 2021).
- 11.LeCun Y, Bengio Y, Hinton G. Deep learning. Nature 2015; 521: 436–444. [DOI] [PubMed] [Google Scholar]
- 12.Amisha MP, Pathania M, et al. Overview of artificial intelligence in medicine. J Fam Med Prim Care 2019; 8: 2328–2331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mintz Y, Brodie R. Introduction to artificial intelligence in medicine. Minim Invasive Ther Allied Technol 2019; 28: 73–81. [DOI] [PubMed] [Google Scholar]
- 14.Jheng YC, Kao CL, Yarmishyn AA, et al. The era of artificial intelligence-based individualized telemedicine is coming. J Chin Med Assoc 2020; 83: 981–983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Br Med J 2021; 372: 71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cornet G. Chapter 4. Robot companions and ethics: a pragmatic approach of ethical design. J Int Bioethique 2013; 24: 49–58. [DOI] [PubMed] [Google Scholar]
- 17.Larson JA, Johnson MH, Bhayani SB. Application of surgical safety standards to robotic surgery: five principles of ethics for nonmaleficence. J Am Coll Surg 2014; 218: 290–293. [DOI] [PubMed] [Google Scholar]
- 18.Miyake S, Higurashi T, Kato H, et al. Evaluation of a combination protocol of CT-first triage and active telemedicine methods by a selected team tackling COVID-19: an experimental research study. J Infect Public Health 2021; 14: 1212–1217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Alodat M. Using deep learning model for adapting and managing COVID-19 pandemic crisis. Procedia Comput Sci 2021; 184: 558–564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Assam NA, Hussain SA, Qaraghuli AA, et al. IoT based wearable device to monitor the signs of quarantined remote patients of COVID-19. Inform Med Unlocked 2021; 24: 100588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sharma N, Mangla M, Mohanty SN, et al. A smart ontology-based IoT framework for remote patient monitoring. Biomed Signal Process Control 2021; 68: 102717. [Google Scholar]
- 22.Faris H, Habib M, Faris Met al. et al. An intelligent multimodal medical diagnosis system based on patients’ medical questions and structured symptoms for telemedicine. Inform Med Unlocked 2021; 23: 100513. [Google Scholar]
- 23.Dawoodbhoy FM, Delaney J, Cecula P, et al. AI in patient flow: applications of artificial intelligence to improve patient flow in NHS acute mental health inpatient units. Heliyon 2021; 7: e06993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Adly AS, Adly MS, Adly AS. Telemanagement of home-isolated COVID-19 patients using oxygen therapy with noninvasive positive pressure ventilation and physical therapy techniques: randomized clinical trial. J Med Internet Res 2021; 23: e23446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Keenan TDL, Goldstein M, Goldenberg Det al. et al. Prospective, longitudinal pilot study: daily self-imaging with patient-operated home OCT in neovascular age-related macular degeneration. Ophthalmol Sci 2021; 1: 100034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chae SH, Kim Y, Lee KSet al. et al. Development and clinical evaluation of a web-based upper limb home rehabilitation system using a smartwatch and machine learning model for chronic stroke survivors: prospective comparative study. JMIR MHealth UHealth 2020; 8: e17216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Maghdid HS, Ghafoor KZ, Sadiq ASet al. et al. A novel AI-enabled framework to diagnose coronavirus COVID 19 using smartphone embedded sensors: design study. ArXiv200307434 Cs Q-Bio 2020; 0: 180–187. [Google Scholar]
- 28.Alom MZ, Rahman MMS, Nasrin MSet al. et al. COVID_MTNet: COVID-19 detection with multi-task deep learning approaches. ArXiv200403747 Cs Eess 2020; 3: 1–10. [Google Scholar]
- 29.Bohadana A, Izbicki G, Kraman SS. Fundamentals of lung auscultation. N Engl J Med 2014; 370: 744–751. [DOI] [PubMed] [Google Scholar]
- 30.Glangetas A, Hartley MA, Cantais A, et al. Deep learning diagnostic and risk-stratification pattern detection for COVID-19 in digital lung auscultations: clinical protocol for a case-control and prospective cohort study. BMC Pulm Med 2021; 21: 03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wong CK, Ho DTY, Tam AR, et al. Artificial intelligence mobile health platform for early detection of COVID-19 in quarantine subjects using a wearable biosensor: protocol for a randomised controlled trial. BMJ Open 2020; 10: e038555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Min-Allah N, Alahmed BA, Albreek EM, et al. A survey of COVID-19 contact-tracing apps. Comput Biol Med 2021; 137: 104787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ranisch R, Nijsingh N, Ballantyne A, et al. Digital contact tracing and exposure notification: ethical guidance for trustworthy pandemic management. Ethics Inf Technol 2020; 23: 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wiśniewska J, Różycka M. The problem of trust in innovative ICT technologies used in e-health systems. The case study of private health care units located in Szczecin. Procedia Comput Sci 2021; 192: 3647–3656. [Google Scholar]
- 35.Mbunge E, Millham RC, Sibiya MN, et al. Framework for ethical and acceptable use of social distancing tools and smart devices during COVID-19 pandemic in Zimbabwe. Sustain Oper Comput 2021; 2: 190–199. [Google Scholar]
- 36.Chen M, Xu S, Husain Let al. et al. Digital health interventions for COVID-19 in China: a retrospective analysis. Intell Med 2021; 1: 29–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shachar C, Engel J, Elwyn G. Implications for telehealth in a postpandemic future: regulatory and privacy issues. JAMA 2020; 323: 2375–2376. [DOI] [PubMed] [Google Scholar]
- 38.Ding EY, Svennberg E, Wurster C, et al. Survey of current perspectives on consumer-available digital health devices for detecting atrial fibrillation. Cardiovasc Digit Health J 2020; 1: 21–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Resneck JS, Abrouk M, Steuer M, et al. Choice, transparency, coordination, and quality among direct-to-consumer telemedicine websites and apps treating skin disease. JAMA Dermatol 2016; 152: 768–775. [DOI] [PubMed] [Google Scholar]