Abstract
Stump appendicitis is a rare and late complication following appendectomy and can often be overlooked. Our case details a 42-year-old male who presented to the Emergency Department with right-sided lower abdominal pain, nausea, and vomiting. A computed tomography scan of his abdomen and pelvis demonstrated a tubular, fluid-filled structure with surrounding inflammatory changes at the level of the patient's appendectomy clips with a 2.3-cm calcified intraluminal stone. Findings were concerning for stump appendicitis with appendicolith. He was admitted and taken to the operating room for a laparoscopic stump appendectomy. Stump appendicitis should always be considered in the differential diagnosis to prevent potentially serious complications.
Keywords: Stump appendicitis, Appendectomy, Abdominal pain
Introduction
Stump appendicitis is a rare and late complication following appendectomy and can often be overlooked in a patient presenting with right lower quadrant pain who previously had an appendectomy [1]. Stump appendicitis was first defined in 1945 as the condition when any appendiceal tissue retained following an appendectomy becomes re-inflamed [2]. The most common presenting symptom is right lower quadrant abdominal pain [1,3]. Similar to appendicitis, delayed recognition and treatment of stump appendicitis can lead to complications like perforation [3]. Laparoscopic appendectomy has also been suggested to contribute to more residual tissue, increasing the risk for stump appendicitis [4]. A longer stump has been thought to present a risk for fecolith obstruction, which was seen in our patient [3,4]. We detail the case of a 42-year-old male who presented to the Emergency Department (ED) complaining of right sided lower abdominal pain, nausea, and vomiting who was subsequently diagnosed with stump appendicitis.
Case report
A 42-year-old male presented to the ED with diffuse abdominal pain which was worse on his right side and awoke him from sleep. He described the abdominal pain as cramping and sharp and had associated nausea, nonbilious vomiting, and decreased appetite. The patient's past medical history was unremarkable other than he had appendicitis 1 year prior which was treated with an uncomplicated laparoscopic appendectomy. He denied recent illness, travel, sick contacts, or recent antibiotic use and stated that the pain felt similar to his previous appendicitis. On physical exam, his vital signs were as follows: blood pressure 146/89 mm Hg, heart rate 69 BPM, respiratory rate 18, and temperature 96.1°F (35.6°C). The patient did not appear to be in any acute distress and his abdomen was soft, and tender in the right lower quadrant without any rebound tenderness.
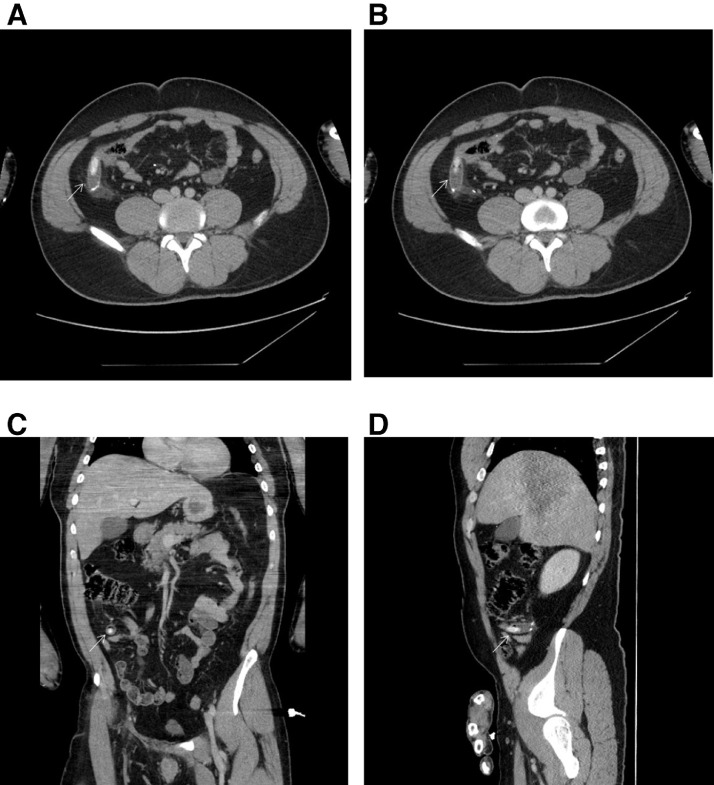
Further work-up showed a leukocytosis of 18.5 thousand/cm2. A computed tomography (CT) scan with intravenous contrast of his abdomen and pelvis showed a tubular, fluid-filled structure measuring 1.7 cm in diameter at the level of the patient's appendectomy clips with a 2.3 cm calcified intraluminal stone and mild free fluid in the right lower quadrant (Figs. 1A-1D).
Fig. 1.
(A-D) Arrows point to a tubular fluid-filled structure with surrounding inflammatory changes in the right lower quadrant at the level of patient's appendectomy clips with 2.3-cm calcified intraluminal stone. These findings are concerning for stump appendicitis with an appendicolith/enterolith (A and B are axial view, C is a coronal view, and D is a sagittal view).
Given the findings on the CT scan, the Surgery service was consulted, and the patient was taken for a laparoscopic stump appendectomy. The inflamed remnant of the appendix was visualized and excised intraoperatively. Surgical pathology confirmed that the excised tissue was acutely gangrenous appendicitis. The following day, the patient had stable vital signs, was able to tolerate a normal diet, ambulate, had regular bowel and bladder function, and was discharged home.
Discussion
Stump appendicitis has been reported in the literature and while rare, is a known entity [5]. The advantage to ongoing reporting on this relatively rare diagnosis is to continue to raise awareness so it is part of the provider's differential. The CT on our patient's scan revealed inflammatory changes at the level of the patient's appendectomy clips which were concerning for stump appendicitis with quite impressively, an appendicolith. A narrow field of vision and lack of physical feedback in laparoscopic appendectomies, which our patient had, can lead to the misidentification of the base of the appendix which can increase the risk for stump appendicitis [3]. A recommended stump length of less than 0.5 cm can decrease the risk as long as the surgeon can accurately locate the base of the appendix before the procedure begins which can be challenging in cases with severe local inflammation [3]. While some cases have been managed with non-operative treatment, due to the calcified deposit within the appendix, surgery was the preferred approach in this case [6]. Stump appendicitis, a rare complication occurring in 1/50,000 [1] cases following appendectomy anywhere from 9 weeks to 50 years [3], can be easily overlooked as a cause of abdominal pain. If missed, it can lead to significant morbidity and mortality with complications including perforation and peritonitis [1,2].
Conclusion
Considering stump appendicitis in the differential diagnosis of right lower abdominal pain of those with prior appendectomy can assist in preventing potentially serious complications.
Author contributions
All authors provided substantial contributions to manuscript content. All authors gave final approval of the version of the article to be published.
Patient consent statement
Patient consent was obtained for this case report.
Footnotes
Declarations of Interest: The authors have no outside support information, conflicts or financial interest to disclose.
Acknowledgments: The authors would like to acknowledge Joanna Schwab, BA for editing and submission assistance.
References
- 1.Casas MA, Dreifuss NH, Schlottmann F. High-volume center analysis and systematic review of stump appendicitis: solving the pending issue. Eur J Trauma Emerg Surg. 2021 doi: 10.1007/s00068-021-01707-y. Epub ahead of print. PMID: 34085112. [DOI] [PubMed] [Google Scholar]
- 2.Rose T. Recurrent appendiceal abscess. Med J Aust. 1945;32:659e62. https://onlinelibrary.wiley.com/doi/abs/10.5694/j.1326-5377.1945.tb55065.x Accessed: March 16, 2022. [Google Scholar]
- 3.Kanona H, Al Samaraee A, Nice C, Bhattacharya V. Stump appendicitis: a review. Int J Surg. 2012;10(9):425–428. doi: 10.1016/j.ijsu.2012.07.007. Epub 2012 Jul 27. PMID: 22846617. [DOI] [PubMed] [Google Scholar]
- 4.Hendahewa R, Shekhar A, Ratnayake S. The dilemma of stump appendicitis - a case report and literature review. Int J Surg Case Rep. 2015;14:101–103. doi: 10.1016/j.ijscr.2015.07.017. Epub 2015 Jul 26. PMID: 26255005; PMCID: PMC4573603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Subramanian A, Liang MK. A 60-year literature review of stump appendicitis: the need for a critical view. Am J Surg. 2012;203(4):503–507. doi: 10.1016/j.amjsurg.2011.04.009. Epub 2011 Dec 6. PMID: 22153086.6. [DOI] [PubMed] [Google Scholar]
- 6.Rios RE, Villanueva KM, Stirparo JJ, Kane KE. Recurrent (stump) appendicitis: a case series. Am J Emerg Med. 2015;33(3):480. doi: 10.1016/j.ajem.2014.08.050. e1-2Epub 2014 Aug 27. PMID: 25227975. [DOI] [PubMed] [Google Scholar]