Abstract
Background
Meniscal ramp lesions are injuries of the posterior horn of the medial meniscus at the meniscocapsular junction or the meniscotibial ligament and are frequently associated with concomitant anterior cruciate ligament (ACL) injury.
Objective
To review the current literature on meniscal ramp lesion management to better define the indications for and outcomes of repair.
Methods
A narrative literature review was performed using PubMed, Embase, and Scopus databases. Studies of all evidence levels (I-V) pertaining to meniscal ramp lesions were reviewed and included.
Results
The incidence of ramp lesions has been reported between 16% and 42%. Arthroscopy remains the diagnostic gold standard as magnetic resonance imaging has limited sensitivity. Biomechanically, ramp lesions are known to increase anterior tibial translation and rotational laxity. Clinical investigations regarding optimal management are largely limited to studies of low evidence levels. While case series have demonstrated that repair is safe and efficacious, comparative studies have failed to suggest that repair of stable lesions results in superior outcomes when compared to conservative treatment approaches. However, repair may be warranted in unstable ramp lesion injuries despite the increased risk for revision surgery.
Conclusion
While there is evidence to suggest that ramp lesion repair can restore joint kinematics, the current body of clinical literature fails to suggest that outcomes following repair are superior to injuries managed conservatively. The current body of clinical literature is limited, and further robust, long-term study is warranted to better guide injury diagnosis and management protocol.
Keywords: Ramp lesion, Meniscus, Meniscocapsular junction, Meniscotibial ligament
1. Introduction to meniscal ramp lesions
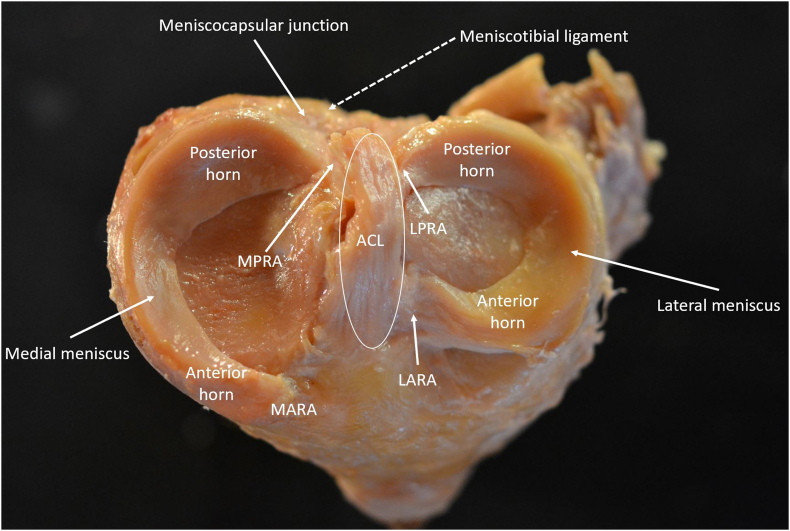
While the primary sites of meniscal attachment are via the anterior and posterior root attachments, connections between the meniscal body and its attachment with the surrounding joint capsule, termed the meniscocapsular junction, and the meniscotibial ligament provides additional stabilization.1 The posterior capsular junction spans nearly the majority of the posteroinferior aspect of the posterior horn of the medial meniscus, while the meniscotibial ligament arises from the articular cartilage margin of the posterior medial tibial plateau and inserts onto the meniscocapsular junction (Fig. 1).2 The meniscocapsular junction and meniscotibial ligament are important to normal knee kinematics as they permit the medial meniscus itself to serve as a secondary stabilizer against anterior tibial translation which can protect the ACL from excessive load-bearing. However, due to this mechanistic association, ramp lesions frequently occur at the time of anterior cruciate ligament (ACL) rupture as the loss of stability precipitates sudden anterior tibial translation that can increase forces on the meniscocapsular junction by more than 200%.3
Fig. 1.
Meniscal Anatomy. Superior view of the medial tibial plateau illustrating relevant meniscal anatomy, the anterior cruciate ligament (ACL), and the structures of the meniscocapsular junction. MARA, medial anterior root attachment; MPRA, medial posterior root attachment; LARA, lateral anterior root attachment; LPRA, lateral posterior root attachment.
In the clinical setting, ramp lesions are difficult to identify. While magnetic resonance imaging (MRI) is often highly reliable for diagnosing meniscal pathology, ramp lesions are notoriously difficult to diagnose on imaging.4 Arthroscopic diagnosis is also challenging and often requires the need for an accessory posteromedial portal because of the posterior location of the injury.4 Indications and optimal treatment strategies of ramp lesions also remain controversial because clinical outcome data is limited, heterogeneous, and of low evidence level. The purpose of this study is to review the existing literature investigating the management of meniscal ramp lesions in order to better define the indications for meniscal repair and outcomes of treatment. We hypothesized that the outstanding literature would indicate that clinical outcomes following non-operative management would not differ when compared to clinical outcomes following surgical repair.
2. Classification
There is currently no consensus on the exact definition of a meniscal ramp lesion in the orthopaedic literature (Table 1). Meniscus ramp lesions were originally defined as longitudinal tears that occur in the posterior periphery of the medial meniscus at the meniscocapsular junction.5,6 However, the literature remains convoluted as more recent investigation suggests that ramp lesions are injuries at the common insertion site of the posteromedial capsule and the meniscotibial ligament.2,7 In 2016, Thaunat and colleagues classified meniscus ramp lesions into 5 categories.8 Type I lesions included injuries to the periphery of the meniscocapsular junction and synovial sheath. Type II lesions were defined as stable, partial lesions of the superior meniscocapsular junction. Partial “hidden” inferior junction lesions that cannot be directly visualized with a trans-intercondylar notch approach but display instability with mechanical probing suggesting meniscotibial ligament injury were defined as type III lesions. Type IV lesions were defined as complete tears in the peripheral, red-red zone of the meniscus. The type V classification was reserved for visible, complete double tears of both the peripheral meniscus and the meniscotibial attachment.8 The proposed classification system by Thaunat was further revised in 2020 by Grief and colleagues who suggested that type III lesions involving the inferior meniscocapsular junction and full-thickness type IV lesions be further stratified into subtypes based on whether the injury involved only meniscal body tissue versus peripheral meniscocapsular or meniscotibial ligament tissue.9
Table 1.
Classification of meniscal ramp lesions based on combined methodology proposed by Thaunat et al.8 and Greif et al.9
| Classification | Description | Stability |
|---|---|---|
| Type I | Peripheral meniscocapsular tear | Stable |
| Type II | Partial superior meniscocapsular tear | Stable |
| Type III | Partial inferior tear | Stable |
| Type IIIa | Partial inferior posterior meniscal horn tear | Stable |
| Type IIIb | Partial meniscotibial ligament tear | Stable |
| Type IV | Complete tear | Unstable |
| Type IVa | Complete peripheral posterior meniscal horn tear | Unstable |
| Type IVb | Complete meniscocapsular junction tear | Unstable |
| Type V | Complete, double tear of the peripheral posterior meniscal horn and the meniscocapsular junction | Unstable |
3. Epidemiology
While the true prevalence of ramp lesions is not reported in the literature, the natural history of meniscus tears in the presence of ACL injury is well documented.10, 11, 12 Previous studies have estimated the incidence of the ramp lesions in ACL-deficient populations to be between 16% and 42%,5,12, 13, 14, 15 and that ramp lesions comprise between 16% and 24% of all meniscal injuries sustained at the time of ACL rupture.16, 17, 18 In reviewing the records of 2156 primary or revision ACL reconstruction cases, Thaunat et al. identified that ramp lesions in 334 (16%) patients. The authors noted that type I lesions of the peripheral meniscocapsular junction or synovial sheath were the most common type of tear (47.9% of cases), while the second most type of injury were double, type IV tears of the meniscal red-red zone.13 In a similar retrospective study, Sonnery-Cottet and colleagues identified 769 (24%) ramp lesions in 3,214 patients who underwent ACL reconstruction. Male gender, younger age, concomitant lateral sided meniscal tears, primary ACL reconstruction failure, varus or valgus laxity greater than 6 mm at time of primary ACL reconstruction were all associated with concomitant ramp lesion injuries at the time of ACL reconstruction.14 Liu et al. reported similar risk factors in their retrospective review of 868 patients undergoing an ACL reconstruction.5 In total, 144 ramp lesions (17%) were identified, with males (P = 0.017) and those under the age of 30 (P < 0.01) at a higher risk of injury. In a smaller review of 372 patients with ACL injuries treated at a single institution, the presence of ramp lesions was associated with posteromedial tibia bone marrow edema (odds ratio (OR), 3.0; P < 0.001), a contact injury mechanism (OR, 1.8; P = 0.02), and a concomitant tear of the lateral meniscus (OR, 1.7; P = 0.02). The study did not find any factors predictive of injury leading to an unstable ramp lesion versus a stable ramp lesion.15 A cross-section study of 275 ACL reconstruction patients also identified the presence of bone edema of the posteromedial tibia to be associated with ramp lesion injury (OR = 4.201, P < 0.01).19 The report also found that varus alignment greater than 3° (OR = 2.339, P = 0.038), increased medial meniscus slope (OR, 1.464; P = 0.03), increased medial tibial slope (OR, 1.289, P = 0.049), and more gradual slope of the lateral tibia (OR = 0.775, P = 0.002) may also precipitate meniscal ramp lesion injury at time of ACL rupture.19
4. Diagnosis
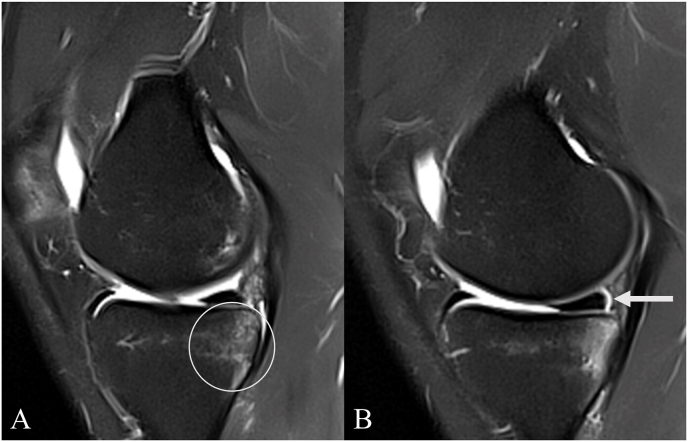
Though MRI is typically highly sensitive to most meniscal pathology, it is not nearly as reliable of a diagnostic modality for ramp lesions. A recent meta-analysis by Koo et al. found that MRI had a sensitivity of 71% and a specificity of 94% for diagnosing ramp lesions.4 However, Koo et al. noted through meta-regression analysis that obtaining MRI with the knee positioned in a neutral 30° of flexion rather than full extension, using a high resolution (3.0 T) magnet, and interpretation by a musculoskeletal radiologist increased pooled sensitivity values to 84%.4 MRI findings such as focal or step-like contour deformity or fluid signal intensity between the posterior horn and meniscocapsular attachment, perimeniscal fluid signal intensity within the posteromedial corner, soft tissue edema between the medial meniscus and medial collateral ligament, and edema of the posterior medial tibial plateau are all representative of potential ramp lesions (Fig. 2).4,9,20,21
Fig. 2.
MRI evidence of a meniscal ramp lesion. Sagittal plane MRI slices in an ACL-deficient patient demonstrating A) posterior medial tibial plateau edema and B) perimeniscal fluid signal intensity within the posteromedial corner of the medial meniscus.
It was first theorized by Bollen that MRI fails to identify ramp lesions because the knee is typically placed in full extension at the moment of the study which reduces the degree of meniscocapsular separation.22 This assertion has been supported by Thaunat et al., who reported that across 2156 patients undergoing ACL reconstruction, 106 of the 332 (32%) identified ramp lesions were missed on preoperative imaging, and that “hidden” type III lesions involving the inferior meniscocapsular margin were missed on MRI in nearly 50% of cases, while type IV lesions were the most readily diagnosed(75.8%).13
Results of the study by Thaunat et al. and others with similar conclusions about the utility of MRI suggest that arthroscopic evaluation is the gold standard of diagnosis of ramp lesions.1,4,5,13
After establishing standard anterior arthroscopic portal access, the knee should be comprehensively evaluated to assess for any concomitant joint pathology, most notably ACL rupture. To properly evaluate the meniscus for presence of a ramp lesion, medial meniscus tissue should be probed through the anterolateral portal to assess its stability. Any obvious forward displacement that occurs during direct probing manipulation should raise suspicion for the presence of a ramp lesion. A transnotch view can be utilized to better visualized the posteromedial compartment of the knee. Once a transnotch view has been established direct view of the posterior knee, a spinal needle can be introduced to directly probe the meniscus and aid with posteromedial portal placement. If a positive spinal needle manipulation test is elicited, a formal posteromedial portal can be established to provide direct arthroscopic access to the injury. However, the portal should be established carefully so as to protect the saphenous neurovascular bundle from injury.
In some reports, posteromedial portal access has been shown to diagnostic accuracy.23 During a systematic exploration of 302 diagnostic arthroscopies prior to ACL reconstruction, Sonnery-Cottet et al. reported that 21 ramp lesions (17% of all meniscus injuries) were only identified after establishing direct posteromedial arthroscopic evaluation.7 However, these findings were contested by data reported by Malatray and colleagues who, using a similar methodology, found no additional ramp lesions when utilizing posteromedial access.24 Due to the overall lack of consensus in the current literature in conjunction with risks of saphenous neurovascular bundle injury and increased operative time, the senior author does not typically utilize posteromedial access during diagnostic arthroscopic evaluation unless there is a high index of suspicion.
5. Biomechanical consequences
The association between ramp lesions and ACL injury is well-reported in the literature.5,10,13,14,19 Biomechanical study indicates that at the time of ACL rupture, excessive valgus strain, internal tibial rotation, and compressive axial forces are transmitted posteromedially within the knee to the meniscocapsular junction, which acts as a secondary stabilizer against anterior translation. This sudden increase in load in an ACL-deficient knee has been shown to increase the risk of meniscocapsular injury.25,26 Other investigations have theorized that sudden contraction of the semimembranosus tendon causes posterior translation of the posterior horn which can precipitate peripheral meniscus tears and ramp lesions while the meniscus is under axial load.27 However, the literature does not suggest a clear correlation between ramp lesions and their impact on joint kinematics or whether surgical intervention fully restores function in vivo.
Peltier and colleagues reported on the biomechanical consequences of ramp and meniscotibial ligament lesions on knee stability. Knees with ramp lesions demonstrated significant increases in anterior tibial translation (P < 0.001) and internal rotation (P < 0.001) when compared to knees with fully in-tact knee anatomy.28 DePhillipo et al. evaluated the biomechanical effects of meniscocapsular and meniscotibial lesions in both ACL-deficient and ACL-reconstructed knees and determined that ACL reconstruction without meniscotibial or meniscocapsular repair restored anterior tibial translation (P > 0.05) but did not resolve internal (P < 0.002) or external (P < 0.002) rotational laxity.29 Potentially the greatest consequence of leaving meniscocapsular lesions untreated has been identified in studies investigating their influence on ACL failure. In a cadaveric study of 10 human knees, Papageorgiou et al. reported that medial meniscus deficiency was a risk factor for ACL failure and that the forces on the reconstructed ACL graft increased between 33% and 50% in the presence of the medial meniscal injury.3 However, isolated meniscocapsular lesions should not be assumed to be biomechanically and anatomically analogous to a knee that is with complete medial meniscal deficiency.
6. Treatment outcomes
Despite results from biomechanical studies which indicate that repair of meniscus ramp lesions may restore joint kinematics, the body of clinical literature is limited, heterogenous, and largely inconclusive. Indications for treatment largely rely on expert opinion than on robust clinical evidence.30 In 2020, a systematic review of all extant literature pertaining to the management of ramp lesion was conducted by Bumberger et al.31 Eight studies were included, five of which were case series8,16,32, 33, 34 and only one of which was a prospective randomized trial.35 All five case studies supported the notion that repair of meniscal ramp lesions is safe and effective. However, these studies were limited by lack of long-term follow-up and were without cohort comparison to other patients who were managed without repair.
The only prospective randomized trial to date comparing outcomes following ACL reconstruction with (N = 50) or without (N = 41) concomitant ramp lesion repair was published in 2017 by Liu et al.35 The authors reported that while two-year postoperative Lysholm and subjective International Knee Documentation Committee (IKDC) measures were significantly improved (P < 0.05 for both) compared to baseline for both treatment cohorts, both patient-reported outcome measures (PROMs) did not differ between groups at final follow-up. Additionally, there were no differences between groups detected in either post-operative physical stability examinations.35 Other retrospective case-control reports have published findings similar to Liu et al. Yang and colleagues analyzed outcomes of 68 patients who underwent ACL reconstruction with meniscal ramp lesions treated with either meniscal margin refreshing plus ramp lesions repair or with refreshing alone. The study found that while postoperative Lysholm, subjective IKDC scores, and knee range of motion (P < 0.05 for all) were significantly improved compared to baseline score, no difference between treatment cohorts at final follow-up.36 More recently, Balazs et al. evaluated 162 patients who underwent ACL reconstruction that were stratified into four groups based on the type of concomitant meniscus pathology present: no pathology, non-ramp lesion meniscus tears, stable ramp lesions managed conservatively, and unstable ramp lesions managed with all-inside repair.37 The findings illustrated no statistically significant difference in PROMs, odds of achieving a minimal clinically important difference (MCID), or revision ACL reconstruction rates. However, patients diagnosed with unstable ramp lesions prior who were treated with repair during the index surgery were significantly more likely to require subsequent reoperation for medial meniscal injury than those who had no meniscal pathology (P < 0.01) and to those who had stable ramp lesions treated without repair (P < 0.03) at time of ACL reconstruction.37 The authors concluded that ramp lesions should be managed on a case-by-case basis and that the repair may in some cases be unnecessary.
7. Technique considerations
It remains the view of the senior author that conservative management of meniscal ramp lesions is generally preferred to surgical repair given the lack of supporting clinical evidence in favor of routine repair. However, all patients with identified meniscal ramp lesions should be evaluated on a case-by-case basis which incorporates findings on MRI and arthroscopy as well as clinical information dictated by patient symptoms, lesion size and stability, ability to complete postoperative rehabilitation, and goals following treatment. Decisions for or against intervention should also incorporate the additional variables of increased surgical case time and potential additional posteromedial incision to improve access to the injury site into the decision-making process.
When it is determined that the lesion type is amenable to repair (i.e., meniscocapsular disruption rather than meniscotibial ligament disruption), an all-inside repair using standard arthroscopic access without additional posteromedial access is the preferred technique of the senior author. If necessary, medial collateral ligament “pie-crusting” release can be performed to increase the posteromedial gap and improve access to the injury site. However other surgical techniques such as all-inside repairs with the use of additional posteromedial portal access38 and inside-out39 repairs are also commonly utilized. To our knowledge, there are no studies that evaluate outcomes based on surgical repair technique especially as it relates to utilizing the specific classification system as a decision-making factor.
8. Conclusions
There is some evidence to suggest that ramp lesion repair at the time of ACL reconstruction restores joint kinematics and that ramp lesion repair is safe and efficacious. Patients with unstable lesions may also benefit from surgical repair compared to a more minimalist approach, primarily in situations where the lesions is found to be unstable during arthroscopic manipulation. However, the overall body of clinical literature remains heterogeneous, primarily of a low level of evidence, and limited by short-term follow-up, which makes recommendations for optimal management difficult. Further long-term study of robust methodologic quality is warranted to better guide the diagnosis and treatment of these injuries. While it is the general preference of the senior author to forego surgical repair of ramp lesions, especially in cases of stable injury, patients should be evaluated on a case-by-case basis with treatment dictated on lesion size and stability, symptom profile, and goals following treatment. When it is determined that the lesion type is amenable to treatment, the senior author prefers to utilize and all-inside repair technique utilizing standard arthroscopic portal access.
Funding/sponsorship
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Informed consent (patient/guardian), mandatory only for case reports/clinical images
Patient consent was obtained for the use of clinical images.
Institutional ethical committee approval (for all human studies)
Not applicable.
CRediT authorship contribution statement
Joshua T. Kaiser: Conceptualization, Methodology, Validation, Formal analysis, Investigation, Resources, Data curation, writing – original, Writing – review & editing, Visualization, Project administration. Zachary D. Meeker: Conceptualization, Methodology, Validation, Formal analysis, Investigation, Data curation, writing – original, Writing – review & editing, Visualization. Nolan S. Horner: Conceptualization, Methodology, Validation, Formal analysis, Investigation, Data curation, writing – original, Writing – review & editing, Visualization. Lakshmanan Sivasundaram: Conceptualization, Methodology, Validation, writing – original, Writing – review & editing. Kyle R. Wagner: Conceptualization, Methodology, Data curation, writing – original, Writing – review & editing. Armaan F. Mazra: Formal analysis, Investigation, Data curation, writing – original, Writing – review & editing. Brian J. Cole: Conceptualization, Methodology, writing – original, Writing – review & editing, Visualization, Project administration.
Declaration of competing interest
B.J.C:
Aesculap/B.Braun: Research support
American Journal of Orthopedics: Editorial or governing board.
American Journal of Sports Medicine: Editorial or governing board.
Arthrex, Inc: IP royalties; Paid consultant; Research support
Arthroscopy Association of North America: Board or committee member.
Athletico: Other financial or material support
Bandgrip Inc: Stock or stock Options.
Cartilage: Editorial or governing board.
Elsevier Publishing: IP royalties.
International Cartilage Repair Society: Board or committee member.
Journal of Shoulder and Elbow Surgery: Editor only: Editorial or governing board.
Journal of the American Academy of Orthopaedic Surgeons: Editor only: Editorial or governing board.
JRF Ortho: Other financial or material support
National Institutes of Health (NIAMS & NICHD): Research support
Operative Techniques in Sports Medicine: Publishing royalties, financial or material support
Ossio: Stock or stock Options.
Regentis: Paid consultant; Research support; Stock or stock Options.
Samumed: Paid consultant.
Smith & Nephew: Other financial or material support
No declarations of interest for any other authors.
Acknowledgement (if any)
None.
Contributor Information
Joshua T. Kaiser, Email: joshkaiser28@gmail.com.
Zachary D. Meeker, Email: zmeeker8@gmail.com.
Nolan S. Horner, Email: nolan.horner@rushortho.com.
Lakshmanan Sivasundaram, Email: luckysivaster@gmail.com.
Kyle R. Wagner, Email: kylewagner85@gmail.com.
Armaan F. Mazra, Email: armaan_f_mazra@rush.edu.
Brian J. Cole, Email: bcole@rushortho.com.
References
- 1.Chahla J., Dean C.S., Moatshe G., et al. Meniscal ramp lesions. Orthop J Sports Med. 2016;4(7) doi: 10.1177/2325967116657815. 2325967116657815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.DePhillipo N.N., Moatshe G., Chahla J., et al. Quantitative and qualitative assessment of the posterior medial meniscus anatomy: defining meniscal ramp lesions. Am J Sports Med. 2019;47(2):372–378. doi: 10.1177/0363546518814258. [DOI] [PubMed] [Google Scholar]
- 3.Papageorgiou C.D., Gil J.E., Kanamori A., Fenwick J.A., Woo S.L., Fu F.H. The biomechanical interdependence between the anterior cruciate ligament replacement graft and the medial meniscus. Am J Sports Med. 2001;29(2):226–231. doi: 10.1177/03635465010290021801. [DOI] [PubMed] [Google Scholar]
- 4.Koo B., Lee S.H., Yun S.J., Song J.G. Diagnostic performance of magnetic resonance imaging for detecting meniscal ramp lesions in patients with anterior cruciate ligament tears: a systematic review and meta-analysis. Am J Sports Med. 2020;48(8):2051–2059. doi: 10.1177/0363546519880528. [DOI] [PubMed] [Google Scholar]
- 5.Liu X., Feng H., Zhang H., Hong L., Wang X.S., Zhang J. Arthroscopic prevalence of ramp lesion in 868 patients with anterior cruciate ligament injury. Am J Sports Med. 2011;39(4):832–837. doi: 10.1177/0363546510388933. [DOI] [PubMed] [Google Scholar]
- 6.Strobel M.J. In: Manual of Arthroscopic Surgery. Strobel M.J., editor. Springer; 2002. Knee joint — special part; pp. 97–669. [DOI] [Google Scholar]
- 7.Sonnery-Cottet B., Conteduca J., Thaunat M., Gunepin F.X., Seil R. Hidden lesions of the posterior horn of the medial meniscus: a systematic arthroscopic exploration of the concealed portion of the knee. Am J Sports Med. 2014;42(4):921–926. doi: 10.1177/0363546514522394. [DOI] [PubMed] [Google Scholar]
- 8.Thaunat M., Fayard J.M., Guimaraes T.M., Jan N., Murphy C.G., Sonnery-Cottet B. Classification and surgical repair of ramp lesions of the medial meniscus. Arthrosc Tech. 2016;5(4):e871–e875. doi: 10.1016/j.eats.2016.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Greif D.N., Baraga M.G., Rizzo M.G., et al. MRI appearance of the different meniscal ramp lesion types, with clinical and arthroscopic correlation. Skeletal Radiol. 2020;49(5):677–689. doi: 10.1007/s00256-020-03381-4. [DOI] [PubMed] [Google Scholar]
- 10.Keene G.C., Bickerstaff D., Rae P.J., Paterson R.S. The natural history of meniscal tears in anterior cruciate ligament insufficiency. Am J Sports Med. 1993;21(5):672–679. doi: 10.1177/036354659302100506. [DOI] [PubMed] [Google Scholar]
- 11.Smith J.P., Barrett G.R. Medial and lateral meniscal tear patterns in anterior cruciate ligament-deficient knees: a prospective analysis of 575 tears. Am J Sports Med. 2001;29(4):415–419. doi: 10.1177/03635465010290040501. [DOI] [PubMed] [Google Scholar]
- 12.Butler D.L., Noyes F.R., Grood E.S. Ligamentous restraints to anterior-posterior drawer in the human knee. A biomechanical study. J Bone Joint Surg Am. 1980;62(2):259–270. [PubMed] [Google Scholar]
- 13.Thaunat M., Ingale P., Penet A., et al. Ramp lesion subtypes: prevalence, imaging, and arthroscopic findings in 2156 anterior cruciate ligament reconstructions. Am J Sports Med. 2021;49(7):1813–1821. doi: 10.1177/03635465211006103. [DOI] [PubMed] [Google Scholar]
- 14.Sonnery-Cottet B., Praz C., Rosenstiel N., et al. Epidemiological evaluation of meniscal ramp lesions in 3214 anterior cruciate ligament–injured knees from the SANTI study group database: a risk factor Analysis and study of secondary meniscectomy rates following 769 ramp repairs. Am J Sports Med. 2018;46(13):3189–3197. doi: 10.1177/0363546518800717. [DOI] [PubMed] [Google Scholar]
- 15.Balazs G.C., Greditzer H.G., Wang D., et al. Ramp lesions of the medial meniscus in patients undergoing primary and revision ACL reconstruction: prevalence and risk factors. Orthop J Sports Med. 2019;7(5) doi: 10.1177/2325967119843509. 2325967119843509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.ping Li W., Chen Z., Song B., Yang R., Tan W. The FasT-fix repair technique for ramp lesion of the medial meniscus. Knee Surg Relat Res. 2015;27(1):56–60. doi: 10.5792/ksrr.2015.27.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Seil R., Mouton C., Coquay J., et al. Ramp lesions associated with ACL injuries are more likely to be present in contact injuries and complete ACL tears. Knee Surg Sports Traumatol Arthrosc. 2018;26(4):1080–1085. doi: 10.1007/s00167-017-4598-3. [DOI] [PubMed] [Google Scholar]
- 18.DePhillipo N.N., Cinque M.E., Chahla J., Geeslin A.G., Engebretsen L., LaPrade R.F. Incidence and detection of meniscal ramp lesions on magnetic resonance imaging in patients with anterior cruciate ligament reconstruction. Am J Sports Med. 2017;45(10):2233–2237. doi: 10.1177/0363546517704426. [DOI] [PubMed] [Google Scholar]
- 19.Kim S.H., Seo H.J., Seo D.W., Kim K.I., Lee S.H. Analysis of risk factors for ramp lesions associated with anterior cruciate ligament injury. Am J Sports Med. 2020;48(7):1673–1681. doi: 10.1177/0363546520918207. [DOI] [PubMed] [Google Scholar]
- 20.Hash T.W. Magnetic resonance imaging of the knee. Sport Health. 2013;5(1):78–107. doi: 10.1177/1941738112468416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kumar N.S., Spencer T., Cote M.P., Arciero R.A., Edgar C. Is edema at the posterior medial tibial plateau indicative of a ramp lesion? An examination of 307 patients with anterior cruciate ligament reconstruction and medial meniscal tears. Orthop J Sports Med. 2018;6(6) doi: 10.1177/2325967118780089. 2325967118780089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bollen S.R. Posteromedial meniscocapsular injury associated with rupture of the anterior cruciate ligament: a previously unrecognised association. J Bone Joint Surg Br. 2010;92(2):222–223. doi: 10.1302/0301-620X.92B2.22974. [DOI] [PubMed] [Google Scholar]
- 23.Escoda Menéndez S., García González P., Meana Morís A.R., del Valle Soto M., Maestro Fernández A. Meniscal ramp lesions: what the radiologist needs to know. Acad Radiol. 2022;29(4):619–626. doi: 10.1016/j.acra.2021.02.005. [DOI] [PubMed] [Google Scholar]
- 24.Malatray M., Raux S., Peltier A., Pfirrmann C., Seil R., Chotel F. Ramp lesions in ACL deficient knees in children and adolescent population: a high prevalence confirmed in intercondylar and posteromedial exploration. Knee Surg Sports Traumatol Arthrosc. 2018;26(4):1074–1079. doi: 10.1007/s00167-017-4471-4. [DOI] [PubMed] [Google Scholar]
- 25.LaPrade R.F., Arendt E.A., Getgood A., Faucett S. Springer Berlin Heidelberg; 2017. The Menisci: A Comprehensive Review of Their Anatomy, Biomechanical Function and Surgical Treatment. [DOI] [Google Scholar]
- 26.Brophy RH, Steinmetz RG, Smith MV, Matava MJ. Meniscal ramp lesions: anatomy, epidemiology, diagnosis, and treatment. JAAOS.J Am Acad Orthop Surg. Published online February 15, 2022:10.5435/JAAOS. doi:10.5435/JAAOS-D-21-00091. [DOI] [PubMed]
- 27.Hughston J.C., Eilers A.F. The role of the posterior oblique ligament in repairs of acute medial (collateral) ligament tears of the knee. J Bone Joint Surg Am. 1973;55(5):923–940. [PubMed] [Google Scholar]
- 28.Peltier A., Lording T., Maubisson L., Ballis R., Neyret P., Lustig S. The role of the meniscotibial ligament in posteromedial rotational knee stability. Knee Surg Sports Traumatol Arthrosc. 2015;23(10):2967–2973. doi: 10.1007/s00167-015-3751-0. [DOI] [PubMed] [Google Scholar]
- 29.DePhillipo N.N., Moatshe G., Brady A., et al. Effect of meniscocapsular and meniscotibial lesions in ACL-deficient and ACL-reconstructed knees: a biomechanical study. Am J Sports Med. 2018;46(10):2422–2431. doi: 10.1177/0363546518774315. [DOI] [PubMed] [Google Scholar]
- 30.DePhillipo N.N., Engebretsen L., LaPrade R.F. Current trends among US Surgeons in the identification, treatment, and time of repair for medial meniscal ramp lesions at the time of ACL surgery. Orthop J Sports Med. 2019;7(2) doi: 10.1177/2325967119827267. 2325967119827267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bumberger A., Koller U., Hofbauer M., et al. Ramp lesions are frequently missed in ACL-deficient knees and should be repaired in case of instability. Knee Surg Sports Traumatol Arthrosc. 2020;28(3):840–854. doi: 10.1007/s00167-019-05521-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Furumatsu T., Miyazawa S., Tanaka T., Okada Y., Fujii M., Ozaki T. Postoperative change in medial meniscal length in concurrent all-inside meniscus repair with anterior cruciate ligament reconstruction. Int Orthop. 2014;38(7):1393–1399. doi: 10.1007/s00264-013-2238-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Keyhani S., Ahn J.H., Verdonk R., Soleymanha M., Abbasian M. Arthroscopic all-inside ramp lesion repair using the posterolateral transseptal portal view. Knee Surg Sports Traumatol Arthrosc. 2017;25(2):454–458. doi: 10.1007/s00167-016-4410-9. [DOI] [PubMed] [Google Scholar]
- 34.Chen Z., Li W.P., Yang R., et al. Meniscal ramp lesion repair using the FasT-fix technique: evaluating healing and patient outcomes with second-look arthroscopy. J Knee Surg. 2018;31(8):710–715. doi: 10.1055/s-0037-1606378. [DOI] [PubMed] [Google Scholar]
- 35.Liu X., Zhang H., Feng H., Hong L., song Wang X., yang Song G. Is it necessary to repair stable ramp lesions of the medial meniscus during anterior cruciate ligament reconstruction? A prospective randomized controlled trial. Am J Sports Med. 2017;45(5):1004–1011. doi: 10.1177/0363546516682493. [DOI] [PubMed] [Google Scholar]
- 36.Yang J., Guan K., Wang J.Z. Clinical study on the arthroscopic refreshing treatment of anterior cruciate ligament injury combined with stable medial meniscus ramp injury. J Musculoskelet Neuronal Interact. 2017;17(2):108–113. [PMC free article] [PubMed] [Google Scholar]
- 37.Balazs G.C., Greditzer H.G., Wang D., et al. Non-treatment of stable ramp lesions does not degrade clinical outcomes in the setting of primary ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2020;28(11):3576–3586. doi: 10.1007/s00167-020-06017-1. [DOI] [PubMed] [Google Scholar]
- 38.Negrín R., Reyes N.O., Iñiguez M., Pellegrini J.J., Wainer M., Duboy J. Meniscal ramp lesion repair using an all-inside technique. Arthrosc Tech. 2018;7(3):e265–e270. doi: 10.1016/j.eats.2017.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.DePhillipo N.N., Cinque M.E., Kennedy N.I., et al. Inside-out repair of meniscal ramp lesions. Arthrosc Tech. 2017;6(4):e1315–e1320. doi: 10.1016/j.eats.2017.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]