Abstract
Introduction
People bereaved by suicide are at high-risk for developing mental disorders and suicidal tendencies. Grief after suicide differs from grief after other types of death, and bereaved persons may require support tailored to their situation. In this study, we evaluate an online intervention for individuals bereaved by suicide and its effectiveness on mental health.
Methods
A total of 140 participants were included in the intervention and randomized to either the treatment or the waitlist control group. The intervention consisted of 12 weekly modules, based on cognitive-behavioral methods, and took place as a webinar in a group format. Primary outcomes were depression and suicidality; secondary outcomes were symptoms of prolonged grief, PTSD, posttraumatic cognitions, hopelessness, and grief-specific symptoms.
Results
Symptoms of posttraumatic avoidance improved significantly in the intention-to-treat analyses (dbetween = 0.43) and in treatment completers (dbetween = 0.56), posttraumatic intrusion improved in treatment completers (dbetween = 0.50) compared to the waitlist control group. In the intervention group, psychopathological symptoms decreased significantly from baseline to 6-month follow-up. Furthermore, factors such as higher scores of depression, grief, suicide ideation, and posttraumatic stress symptoms were identified at baseline, which impacted the effectiveness of the intervention.
Conclusions
The results of this study indicate that completing an online group intervention for the suicide bereaved could reduce trauma-related outcomes. However, the waiting control group also improved significantly from pre- to post-measurement in all other outcomes. Future studies with active control groups are needed to further examine the effectiveness.
Keywords: Suicide bereavement, Suicidality, Grief, Group intervention, Prolonged grief disorder
Highlights
-
•
The online group-intervention for suicide survivors was successful in reducing posttraumatic avoidance to a waitlist control group.
-
•
In the intervention group, psychopathological symptoms decreased significantly from baseline to 6-months follow-up.
-
•
No differences between the two groups in terms of primary outcomes were found.
-
•
Higher scores of depression, grief, suicide ideation, and posttraumatic stress symptoms at baseline impacted the effectiveness.
1. Background
The World health Organization (WHO, 2019) estimates that 800,000 people die by suicide each year, while suicide attempts are ten times more prevalent. Suicide is considered the second leading cause of death among adolescents and young adults, with numbers increasing over the past decade.
In many ways, suicide bereavement is similar to the grief experienced after other kinds of death (Kolves et al., 2019). However, certain grief reactions are related specifically to suicide bereavement. Individuals affected by suicide often feel stigmatized by their environment, which in turn leads to increased social isolation and a reduced willingness to seek help (Pitman et al., 2016). Other common suicide-related grief reactions are self-attributed responsibility for the death and feelings of guilt. Furthermore, the bereaved might experience strong anger towards the deceased person, feelings of abandonment, or the perpetual question of the reason for the suicide (Pitman et al., 2014; Ross et al., 2019). Previous studies have reported that the suicide bereaved are more prone to develop a mental illness, which, in turn, can lead to severe impairments in daily life as well as in social and occupational contexts. In a population-based prospective study, Wilcox et al. (2015) analyzed data of 1,051,515 suicide bereaved parents and found that this population had a tenfold higher risk to be absent from work for more than 30 days, due to mental health problems, than non-bereaved parents. In addition, fathers of children who died by suicide were found to have a 40% higher risk of absenteeism due to somatic health problems. Bolton et al. (2013) showed an increased likelihood of depression and anxiety disorders among parents who lost their child to suicide. Similarly, bereaved youth who have lost a parent to suicide are more likely to develop depression or posttraumatic stress disorder (PTSD) in the first 9 months after the loss, compared to bereaved youth who lost a parent through an accident or sudden natural death (Brent et al., 2009). This bereavement group also shows an increased prevalence for prolonged grief, compared to bereaved individuals following a nonviolent death. The prevalence for prolonged grief among the suicide bereaved has been estimated to be approximately 43–80% (Bellini et al., 2018; Mitchell et al., 2005). Furthermore, prolonged grief has been significantly associated with increased suicidality and thus noted to be an area of great concern among this bereavement group (Pitman et al., 2014). In their review, Molina et al. (2019) found that 14.1–49% of individuals bereaved by suicide expressed suicidal ideation— the highest rate compared to individuals who lost a person through other types of death. Therefore, the WHO (WHO, 2019) has described people bereaved through suicide as a high-risk group for own suicide, describing aftercare of the suicide bereaved as an essential part of national and international suicide prevention.
Providing support to the suicide bereaved has become increasingly relevant in recent years, with the specific needs of this bereaved population attracting more attention in the field of psychosocial healthcare. Few evidence-based psychotherapeutic interventions specifically aimed at this bereavement group exist, whether offered online or offline. In their systematic review, Linde et al. (2017) examined of a total of 7 interventions aimed at reducing grief in the suicide bereaved. While some of the interventions were shown to be effective in reducing grief reactions and suicidal ideation, only one intervention was shown to decrease prolonged grief disorder. The authors also noted the methodological limitations of the included interventions. Similarly, a recent systematic review, including 11 studies on the effectiveness of interventions for people bereaved through suicide, showed that few interventions led to a decrease of uncomplicated grief reactions in the bereaved (Andriessen et al., 2019).
Several studies have indicated that cognitive-behavioral therapy (CBT) leads to a reduction of symptoms of prolonged grief disorder in bereaved populations (Boelen et al., 2007; Wittouck et al., 2011). To date, only a few studies investigating CBT after suicide bereavement exist, but results in this area have shown promising effects (de Groot et al., 2007; Pfeffer et al., 2002; Kovac and Range, 2000). In recent years, research has shown that web-based bereavement interventions can be beneficial to the bereaved, with treatment effects comparable to those of face-to-face treatments. A meta-analysis and systematic review evaluated the efficacy of web-based bereavement interventions for bereaved people, based on seven included studies (Wagner et al., 2020). Most of the included internet-based interventions used structured writing assignments with and without therapist support, and all were based on cognitive-behavioral principles. The effects of the internet-based grief interventions on grief reduction were promising, showing moderate effect sizes.
The aim of the present study was to develop and evaluate an online group intervention for the suicide bereaved. The intervention was manualized and based on the principles of cognitive behavioral therapy. The main objective of the study was to reduce suicidality and depression in the suicide bereaved. Secondary outcomes were PTSD, prolonged grief (PG) and hopelessness.
2. Methods
2.1. Protocol
Ethical approval for the study was given by the Ethics Committee of XXX (03.03.2018, reference number XXX, information removed for blinded review process). Prior to the start of the intervention, participants received study information providing details on the procedure, inclusion and exclusion criteria, study objectives as well as confidentiality, data storage and data protection guidelines. Signed consent was given by all participants either by email or post. The detailed study protocol was published in January 2020 (XXX, information removed for blinded review process).
2.2. Design
The study was a randomized controlled trial with two conditions: a treatment group and a waitlist control group. The treatment group began the intervention immediately, while the waitlist control group took part in the intervention after a waiting period of 12 weeks. Individuals in both conditions received the same intervention. Assessment was conducted at baseline (pre-test), middle (after six sessions), post, and after 3 and 6 months (follow up: treatment group only). This RCT was conducted according to the standards of the CONSORT 2010 statement guidelines for randomized controlled trials (Schulz et al., 2010).
2.3. Participants and recruitment
Recruitment took place primarily through the intervention website and through the cooperation partners: the Federal Association of Bereaved Parents and Bereaved Siblings in Germany (VEID e.V.) and the Association for the Suicide Bereaved (AGUS e.V.). Furthermore, participants were recruited via social media (e.g., Instagram, Facebook), specific forums and websites for bereaved individuals and via advertisements on social media platforms and flyers.
Participants meeting the following criteria were included in the study: (1) loss of a close person through suicide, (2) aged between 18 and 75 years, (3) sufficient German language skills, (4) internet access, and (5) providing a signed consent form. Participants could not participate in the study if they met one or more of the following exclusion criteria: (1) severe depression (BDI-II > 35), (2) acute suicidality, (3) current psychosis, (4) substance abuse, (5) bipolar disorder, (6) borderline personality disorder, or (7) self-harm.
For the study protocol, a power analysis was conducted (see study protocol, information removed for blinded review process). We aimed to include a total of 104 participants.
2.4. Procedure and randomization
Individuals interested in taking part in the study were invited to register on the intervention website. Participants subsequently received an e-mail with detailed information about the study and the intervention, as well as a consent form. As soon as the consent form was signed, participants were invited to take part in an online questionnaire, which was then followed by a telephone interview. Participants who met the inclusion criteria were assigned to the next group by the study coordinators. Once 12 participants were included, individuals were randomly assigned to either the treatment or the waitlist control group using block randomization without extra stratification. The randomization ratio was 1:1, with both groups being equally allocated.
2.5. Intervention
The online group intervention consisted of 12 weekly sessions, each with a duration of 90 min. Study participation was free of charge. The entire intervention was manualized based on cognitive behavioral methods (see table A.1 in the Supplementary Material) and consisted of topics relevant to suicide survivors (e.g., guilt, stigma). Between sessions, participants could voluntarily work on additional homework assignments (e.g., describing the relationship to the deceased person). Each session followed a similar structure. First, participants briefly shared how they were currently feeling, then psychoeducational content was used to introduce the topic, after which a testimonial video was shown, in which bereaved relatives shared their experiences with grief. This was followed by a group discussion and interaction. At the end of each session, the group leader presented the homework and there was time for questions.
The entire intervention took place via the software program Adobe Connect. Participants received a link to the webinar room as well as technical instructions before the group started. Each intervention session was conducted by two group leaders: (1) a psychotherapist or a psychotherapist in training and (2) a person who had lost someone through suicide and had experience in conducting self-help groups. The group leaders were given special training and received regular supervision at a 1-month interval.
2.6. Instruments
2.6.1. Screening for eligibility criteria
The study coordinators conducted a telephone interview with each participant, which served as an eligibility screening. The respective sections of the German version of the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I) (Wittchen et al., 1997) were used. The following exclusion criteria were set: bipolar disorder, major depression, manic episode, borderline personality disorder, post-traumatic stress disorder, as well as alcohol and substance abuse. The German version (Knaevelsrud, 2005) of the Suicide Risk Assessment Interview (Lange et al., 2000) and the German version of the Dutch Screening Device for Psychotic Disorder (Arnoldi et al., 2000) were used to record acute suicidal tendencies and psychotic symptoms. Furthermore, the interview included questions about the loss (e.g., “Who found the person?”) and about the current state of health of the participants (e.g., “Do you currently have physical complaints?”).
2.7. Outcome measures
2.7.1. Beck depression inventory (BDI-II)
The BDI-II (Hautzinger et al., 2006) is a self-assessment tool for assessing the severity of depression. Participants choose the statement that most accurately reflects their condition within the last 2 weeks. A total score is then calculated from all 21 items, which provides information on the severity of the depressive episode. The BDI-II reports an internal consistency of α = 0.93 in a clinical sample and of α = 0.85 in the current sample.
2.7.2. Beck scale for suicide ideation (BSSI)
The BSSI (Beck et al., 1988) is a self-assessment tool for assessing the severity of suicidal ideation. The questionnaire consists of 19 items, with three groups of statements within each item (coded 0–2). Two additional items assess past attempts of suicide but are not included in the total score. The overall BSSI score can vary between 0 and 38, with higher scores indicating a higher risk of suicide. The internal consistency is reported as excellent, with α = 0.94 in a German sample (Kliem et al., 2017) and α = 0.85 in the present sample.
2.7.3. The acquired capability for suicide scale (ACSS-FAD)
The ACSS-FAD (Spangenberg et al., 2014) assesses the fearlessness of death, which is seen as a sub-dimension of the ability to commit suicide. The questionnaire consists of seven items on a 4-point Likert scale (0 = “does not apply to me at all” to 4 = “applies completely to me”). The internal consistency in a German sample was reported as good with α = 0.79 and α = 0.76 in the present sample.
2.7.4. Revised impact of event scale (IES-R)
The German version of the IES-R (Maercker and Schützwohl, 1998) assesses posttraumatic stress reactions within seven days after a traumatic event. The questionnaire consists of 22 items on a 4-point Likert scale (0 = “not at all” to 5 = “often”). The IES-R is divided into three subscales: avoidance (eight items), intrusion (seven items) and hyperarousal (seven items). The internal consistency for the subscales varies between α = 0.71 and α = 0.90 in a clinical sample, and varied between α = 0.71 and α = 0.82 in the present sample.
2.7.5. Inventory of complicated grief (ICG—D)
The German version (Lumbeck et al., 2012) of the ICG-D (Prigerson et al., 1995) is used to assess symptoms of prolonged grief. The questionnaire consists of 19 items rated on a 5-point Likert scale (0 = “never” to 4 = “always”). A sum score is calculated for all 19 items, and a higher score indicates a higher symptom severity. With α = 0.87 in a German clinical sample and with α = 0.84 in the present sample, the internal consistency was deemed good.
2.7.6. Grief experience questionnaire (GEQ)
The GEQ (Bailley et al., 2000) assesses grief reactions after the loss of a close person and includes, among others, grief reactions often experienced after a loss through suicide. In this study, the subscales stigmatization (10 items), guilt (six items), responsibility (five items) and shame (seven items) were used. The items are rated on a 5-point Likert scale (1 = “never” to 5 = “almost always”). A total score can be calculated for each subscale; all subscales can be added up to a total score. The internal consistency of the subscales was good and varied between α = 0.70 and α = 0.86 in a sample of bereaved students. The internal consistency in our sample varied between α = 0.78 and α = 0.89.
2.7.7. Short version of the patient health questionnaire (PHQ-9)
The German version of the PHQ-9 (Löwe et al., 2002) is a screening tool for assessing depressive disorders consisting of nine items, each rated on a 4-point rating scale (1 = “not at all” to 4 = “almost every day”), anxiety and panic disorders (five items with a yes/no answer format) and psychosocial impairment (one item, 4-point rating scale from “not at all impaired” to “strongly impaired”). The internal consistency was good, with Cronbach's Alpha of α = 0.89 in a clinical sample (Gräfe et al., 2004) and α = 0.82 in the current sample.
2.7.8. H-scale
The H-Scale is the German version (Krampen, 1994) of the Beck Hopelessness Scale (Beck et al., 1974). The scales assess three dimensions: negative expectations of one's self, negative expectations of the environment and negative expectations of the future. In this study, the short version with 10 items rated on a 6-point rating scale (1 = “completely wrong” to 6 = “completely correct”) is used. The internal consistency was good to excellent with α = 0.74 and α = 0.92 in a clinical and a non-clinical sample. In the present sample, Cronbach's Alpha was α = 0.89.
2.7.9. Posttraumatic cognitions inventory (PTCI)
The German version (Müller et al., 2010) of the PTCI (Foa et al., 1999) consists of 33 items on a 7-point rating scale (1 = “totally disagree” to 7 = “totally agree”), which measure dysfunctional cognitions following a traumatic event. Consisting of three subscales (negative cognitions about the self, negative cognitions about the world, self-blame), the questionnaire showed a good internal consistency in this sample with α = 0.97, α = 0.88, and α = 0.86, respectively.
2.8. Statistical analysis
Data were analyzed using SPSS Version 27. Demographic data were analyzed using frequencies and descriptive statistics while presenting frequencies for categorical variables and means and standard deviations for continuous variables. t-tests were used to compare baseline between-group differences in the pre-measures as well as in demographics. Differences between the treatment and the waitlist control group were analyzed using repeated measures ANCOVAs, with group as the between-subject factor and time as the within-subject factor, while following the principles of intention-to-treat analyses for all analyses. Additionally, we controlled for current professional support by including this variable as a covariate in the ANCOVAs. Effect sizes were calculated for within- and between-subject analyses. Cohens d (Cohen, 1988) was used for within-subject effect sizes, and dbetween (dppc2) was calculated for between-subject effect sizes (Morris, 2008) by subtracting the mean pre-post change in the control group from the mean pre-post change in the treatment group, and dividing by the pooled pre-test standard deviation. A completer analysis was also performed in order to analyze the results without any replaced values. Completers were defined as participants who attended eight or more sessions and completed the post questionnaire. Furthermore, missing values were imputed using the expectation maximization algorithm to preserve trial power and to control for confounding factors. The analyses were presented once with imputed values and once as a complete analysis.
To evaluate the effectiveness and long-term effects of the intervention in the treatment group, repeated-measures ANCOVAs were conducted for the primary outcomes and additionally for prolonged grief (ICG) and posttraumatic stress symptoms (IES-R). These values were obtained from baseline, post, and follow-up after 3 and 6 months, while also controlling for the variable current professional support. The Greenhouse-Geisser adjustment was used to correct for violations of sphericity.
The clinically significant change was additionally calculated to evaluate improvements in the outcomes of depression, grief, and suicide ideation. The clinically significant change indicates whether participants' scores change from the “dysfunctional population” before participating in the intervention to the “healthy population” after participating (Jacobson and Truax, 1991). For this, a cut-off is determined by using the sum of the products of the means and standard deviations of our clinical sample and a non-clinical sample divided by the sum of their standard deviations (Evans et al., 1998).
3. Results
3.1. Sample
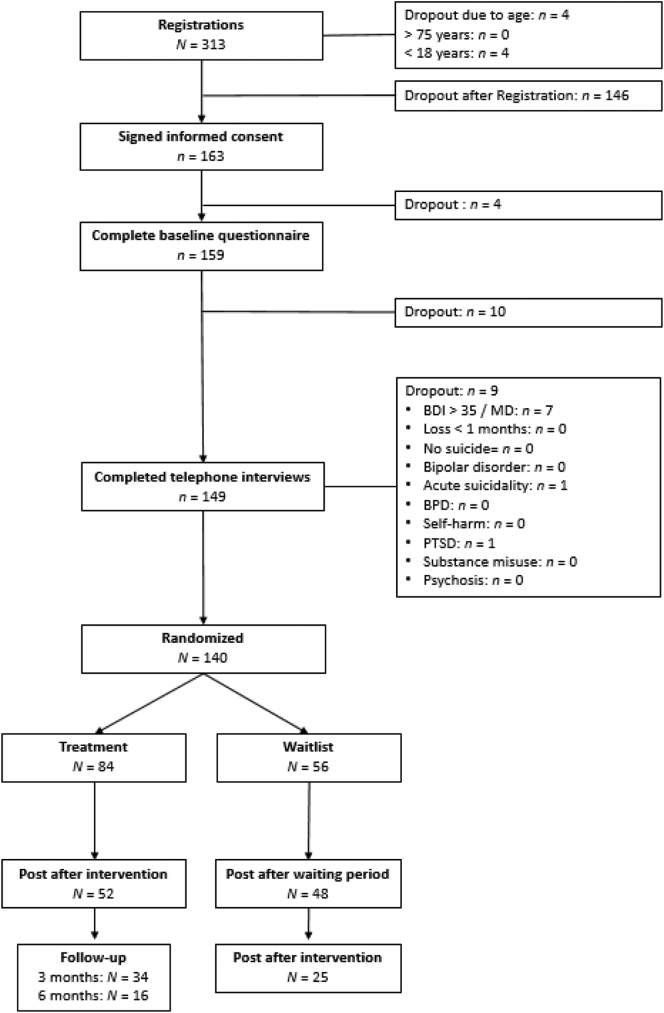
A total of N = 313 participants registered for the study. The detailed flow of participants can be seen in Fig. 1. A total of N = 140 participants could be enrolled and randomized to either the treatment group (n = 84) or the waitlist control group (n = 56).
Fig. 1.
Flowchart of participants.
Sociodemographic information and loss-related characteristics can be seen in Table 1. No significant differences between the two groups regarding sociodemographic or loss-related data at baseline level were found. In the treatment group, n = 24 (28.6%) participants dropped out during treatment, and n = 8 (9.5%) additional individuals did not complete the post-questionnaire, despite completing the program. In the waitlist condition, n = 8 (14.3%) participants dropped out after randomization, and a total of n = 23 (41.1%) participants dropped out during the intervention. Overall, participants in the treatment condition attended 8.67 (SD = 4.21) sessions.
Table 1.
Sociodemographic and loss-related characteristics of participants in treatment (n = 84) and waitlist (n = 56) condition and for the total sample (n = 140) at baseline (t0).
| Treatment | Waitlist | Total | |
|---|---|---|---|
| Sociodemographic characteristics | |||
| Gender (female) | 89.3% | 89.3% | 89.3% |
| Age in years | 40.96 (13.02) | 41.55 (12.41) | 41.20 (12.74) |
| Marital status | |||
| Single | 33.3% | 28.6% | 31.4% |
| In a relationship | 17.9% | 23.2% | 20.0% |
| Married | 32.1% | 25.0% | 29.3% |
| Widowed | 10.7% | 16.1% | 12.9% |
| Divorced | 6.0% | 7.1% | 6.4% |
| Education level | |||
| Primary | 4.8% | 3.6% | 4.3% |
| Secondary | 23.8% | 21.4% | 22.9% |
| Higher | 71.4% | 75.0% | 72.9% |
| Current professional support | 54.8% | 55.4% | 55.0% |
| Current psychotropic medication | 19.0% | 12.5% | 16.4% |
| Loss-related characteristics | |||
| Age of deceased in years | 42.80 (17.37) | 39.36 (16.94) | 41.42 (17.22) |
| Time since the loss in months | 27.76 (57.78) | 30.93 (49.88) | 29.03 (54.60) |
| Kinship to the deceased | |||
| Child | 15.5% | 23.2% | 18.6% |
| Parent | 27.4% | 23.2% | 25.7% |
| Sibling | 26.2% | 17.9% | 22.9% |
| Partner | 21.4% | 19.6% | 20.7% |
| Friend | 1.2% | 3.6% | 2.1% |
| Colleague | 3.6% | 3.6% | 3.6% |
| Other | 4.8% | 8.9% | 6.4% |
| Farewell letter received | 31.0% | 42.9% | 35.7% |
| Number of completed homework (M, SD)⁎ | 4.95 (3.39) | ||
| Number of sessions attended (M, SD)⁎ | 8.67 (4.21) | ||
only for treatment group reported.
Table 2 presents means, standard deviations and effect sizes at baseline and post-treatment for the treatment group as well as those at baseline and post after the waiting period for the waitlist control group, after intention-to-treat analyses were conducted.
Table 2.
Primary and secondary outcomes measured per condition (treatment, waitlist) at baseline (t0), post-assessment (t2), and (within and between) group differences for intention-to-treat data with “additional support” as a covariate, n = 140 (TG = 84, WCG = 56).
| Outcome |
Group |
Pre |
Post |
Interaction effect |
Effect sizes |
Main effect |
|||
|---|---|---|---|---|---|---|---|---|---|
| M (SD) | M (SD) | Time ∗ group | p | dbetween | dwithin | Time | p | ||
| Primary outcomes | |||||||||
| BDI-II | TG | 18.90 (7.59) | 13.07 (7.73) | F(1, 137) = 0.95 | 0.333 | 0.19 | 0.76 | F (1,137) = 22.25 | <0.001 |
| WCG | 18.57 (8.83) | 14.28 (8.87) | 0.49 | ||||||
| BSSI | TG | 2.10 (3.86) | 2.11 (4.04) | F(1, 137) = 0.05 | 0.823 | 0.05 | −0.03 | F (1,137) =0.13 | 0.715 |
| WCG | 1.75 (2.92) | 1.60 (2.73) | 0.05 | ||||||
| ACSS-FAD | TG | 1.96 (0.85) | 1.80 (0.70) | F(1, 137) = 0.52 | 0.474 | 0.10 | 0.21 | F (1,137) = 0.06 | 0.807 |
| WCG | 2.03 (0.91) | 1.96 (0.79) | 0.08 | ||||||
| Secondary outcomes | |||||||||
| ICG-D | TG | 33.68 (11.55) | 27.48 (10.11) | F(1, 137) = 0.96 | 0.329 | 0.15 | 0.57 | F (1,137) = 23.07 | <0.001 |
| WCG | 31.98 (10.74) | 27.46 (12.09) | 0.22 | ||||||
| IES-R avoidance | TG | 15.33 (10.49) | 11.03 (6.66) | F(1, 137) = 8.36 | 0.004 | 0.43 | 0.49 | F (1,137) = 13.95 | <0.001 |
| WCG | 11.54 (7.34) | 11.33 (7.97) | 0.03 | ||||||
| IES-R hyperarousal | TG | 12.80 (6.74) | 9.66 (5.39) | F(1, 137) = 1.91 | 0.169 | 0.21 | 0.52 | F (1,137) = 41.44 | <0.001 |
| WCG | 14.41 (8.36) | 9.70 (7.00) | 0.61 | ||||||
| IES-R intrusion | TG | 19.54 (7.28) | 12.97 (6.27) | F(1, 137) = 3.49 | 0.064 | 0.31 | 0.97 | F (1,137) = 53.26 | <0.001 |
| WCG | 17.86 (7.52) | 13.62 (7.36) | 0.57 | ||||||
| GEQ total | TG | 76.29 (16.94) | 70.78 (13.45) | F(1, 137) = 1.33 | 0.252 | 0.15 | 0.36 | F (1,137) = 6.16 | 0.014 |
| WCG | 72.89 (17.89) | 70.01 (17.82) | 0.16 | ||||||
| GEQ stigma | TG | 28.43 (8.96) | 26.99 (6.87) | F(1, 137) = 0.11 | 0.741 | 0.05 | 0.18 | F (1,137) = 1.19 | 0.278 |
| WCG | 27.93 (8.29) | 26.89 (6.90) | 0.14 | ||||||
| GEQ guilt | TG | 19.55 (5.11) | 17.33 (4.01) | F(1, 137) = 1.62 | 0.205 | 0.18 | 0.48 | F (1,137) = 15.62 | <0.001 |
| WCG | 18.88 (5.43) | 17.60 (5.53) | 0.23 | ||||||
| GEQ responsibility | TG | 10.49 (4.38) | 9.60 (3.34) | F(1, 137) = 0.32 | 0.570 | 0.08 | 0.05 | F (1,137) = 2.14 | 0.146 |
| WCG | 10.21 (4.04) | 9.66 (4.05) | 0.14 | ||||||
| GEQ shame | TG | 17.82 (5.66) | 16.86 (4.23) | F(1, 137) = 1.53 | 0.218 | 0.17 | 0.19 | F (1,137) = 0.57 | 0.453 |
| WCG | 15.88 (5.30) | 15.87 (5.79) | 0.002 | ||||||
| PHQ-9 depression | TG | 9.70 (4.71) | 6.56 (3.49) | F(1, 137) = 1.34 | 0.250 | 0.22 | 0.76 | F (1,137) = 27.13 | <0.001 |
| WCG | 9.55 (4.68) | 7.43 (4.38) | 0.47 | ||||||
| PHQ-9 impairment | TG | 1.15 (0.69) | 0.93 (0.49) | F(1, 137) = 1.63 | 0.205 | 0.24 | 0.37 | F (1,137) = 28.21 | <0.001 |
| WCG | 1.21 (0.73) | 0.82 (0.65) | 0.56 | ||||||
| PTCI total | TG | 9.09 (2.89) | 7.49 (2.56) | F(1, 137) = 2.60 | 0.110 | 0.27 | 0.59 | F (1,137) = 6.48 | 0.012 |
| WCG | 8.81 (3.10) | 8.01 (3.85) | 0.23 | ||||||
| H-scales | TG | 21.12 (8.91) | 18.73 (6.96) | F(1, 137) = 0.10 | 0.754 | 0.05 | 0.30 | F (1,137) = 3.59 | 0.060 |
| WCG | 19.75 (8.84) | 17.82 (9.11) | 0.22 | ||||||
Note. BDI-II = Beck Depression Inventory; BSSI = Beck Scale for Suicide Ideation; ACSS-FAD = The Acquired Capability for Suicide Scale; ICG-D = Inventory of Complicated Grief; IES-R: Revised Impact of Event Scale; GEQ: Grief Experience Questionnaire; PHQ-9 = Short Version of the Patient Health Questionnaire; PTCI=Posttraumatic Cognitions Inventory.
3.2. Outcome measures across time by condition
The following analyses are based on the principles of intention-to-treat analyses. The results of the completer analyses can be seen in Table B.1 in the Supplementary Material. Due to the fact that the results differ only minimally, only the intention-to-treat analyses will here be reported.
3.3. Primary outcome measures
Three repeated-measures ANCOVAs were run to determine the differences between both groups regarding depression (BDI-II) and suicidality (BSSI, ACSS) with time (baseline vs. post) as within-subject factor (see Table 2).
For the ITT analyses, no statistically significant interaction between group and time for depressive symptoms was found, F(1, 137) = 0.95, p = .333, dbetween = 0.19. For the scores of the BSSI and the ACSS, respectively, no statistically significant interaction between group and time for suicidality was found, F(1, 137) = 0.05, p = .823, dbetween = 0.05, and F(1, 137) = 0.52, p = .474, dbetween = 0.10. Similar results could be observed in the completer analysis.
3.4. Secondary outcome measures
Repeated-measures ANOVAs were run for the secondary outcomes to evaluate the differences between the two groups in terms of prolonged grief (ICG), grief reactions (GEQ), posttraumatic stress symptoms (IES), depressive symptoms, functional impairment (PHQ-9), dysfunctional cognitions (PTCI), and hopelessness (H-Scales) (Table 2).
The ITT analysis revealed no statistically significant interaction between group and time for symptoms of prolonged grief, F(1, 137) = 0.96, p = .329, dbetween = 0.15. There was also no significant interaction for grief reactions, F(1, 137) = 1.33, p = .252, dbetween = 0.15.
Similarly, no statistically significant interactions between group and time for posttraumatic intrusion and hyperarousal were found, F(1, 137) = 3.49, p = .064, dbetween = 0.31 and F(1, 137) = 1.91, p = .169, dbetween = 0.21, respectively. However, a statistically significant interaction could be observed for posttraumatic avoidance, F(1, 137) = 8.36, p = .004, dbetween = 0.43, with a substantial improvement in symptoms of posttraumatic avoidance in the treatment condition. The completer analyses also showed a significant interaction for posttraumatic intrusion, F(1, 97) = 11.78, p < .001, dbetween = 0.50, with a significant decrease in symptoms in the treatment condition.
There was no significant interaction for dysfunctional posttraumatic cognitions, F(1, 137) = 2.60, p = .110, dbetween = 0.27, and no significant differences for hopelessness, F(1, 137) = 0.10, p = .754, dbetween = 0.05.
Regarding the PHQ-9 (depressive symptoms, functional impairment), no significant interactions could be found, with F(1, 138) = 1.34, p = .249, dbetween = 0.22, and F(1, 138) = 1.494, p = .225, dbetween = 0.24, respectively.
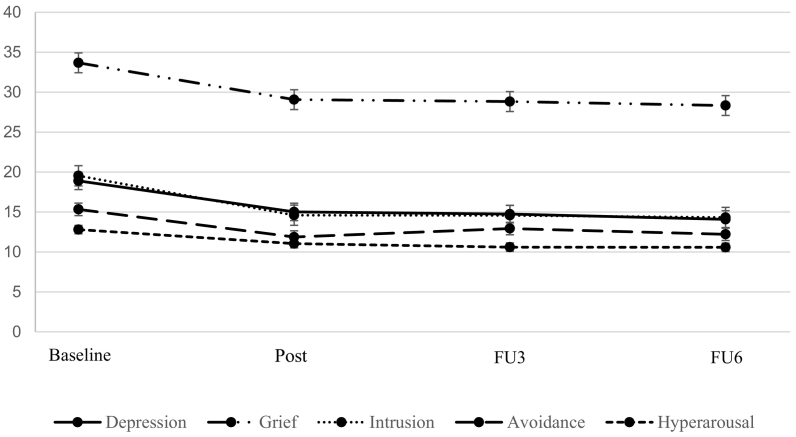
3.5. Effectiveness for the treatment group from baseline to follow-up
The intervention elicited statistically significant changes in depressive symptoms from baseline to the 6-month follow-up, F(2.23, 180.79) = 23.84, p < .001, dwithin = 1.51; findings indicated that symptoms decreased over time. There were no significant changes in suicidality measured with the BSSI and the ACSS-FAD, with F(2.12, 173.56) = 0.74, p = .530, dwithin = 0.27, and F(2.55, 208.92) = 7.30, p < .001, dwithin = 0.14, respectively. However, suicidality increased significantly after completing the intervention, but subsequently decreased significantly over time.
A statistically significant reduction in symptoms of prolonged grief from baseline to 6-month follow-up was found, F(2.31, 189.55) = 15.51, p < .001, dwithin = 1.13. Furthermore, the intervention led to a statistically significant decrease in the posttraumatic stress symptoms avoidance, intrusion, and hyperarousal, with F(2.22, 181.61) = 11.20, p < .001, dwithin = 0.81, F(2.41, 197.52) = 38.95, p < .001, dwithin = 1.75, and F(2.35, 192.75) = 22.98, p < .001, dwithin = 1.04, respectively.
For the subscales of the GEQ, statistically significant changes could be found for stigmatization as well as for guilt and shame from baseline to 6-month follow-up, with F(2.27, 186.21) = 3.34, p = .032, dwithin = 0.42, F(2.28, 186,98) = 8.62, p < .001, dwithin = 0.84, and F(2.04, 166.89) = 3.08, p = .028, dwithin = 0.05, respectively; indicating a decrease in the respective outcomes. There were no significant changes in the subscale feelings of responsibility (F(2.15, 176.65) = 1.05, p = .371, dwithin = 0.15) and no significant reduction over time regarding hopelessness, with F(2.02, 165.52) = 2.92, p = .056, dwithin = 0.55.
The same results are valid for the completer analyses, except for the GEQ subscales stigmatization and shame, where no improvement in symptoms from baseline to 6-month follow-up was observed.
Means and standard deviations for all time points are presented in Table B.2 (intention-to-treat) and B.3 (completer analyses) in the Supplementary Material. Fig. 2 shows the effects for the treatment group.
Fig. 2.
Effectiveness of the intervention for the treatment group.
Note. Depression (BDI-II), PG (ICG—D) and posttraumatic stress symptoms (IES-R) measured for intervention condition at baseline (t0), mid-assessment (t1), post-treatment (t2), 3-month follow-up (t3), and 6-month follow up (t4).
3.6. Clinically significant change
A clinically significant change could be found both for depression and grief. However, no significant differences between the treatment and the waitlist condition were observed (see table B.4 in the Supplementary Material).
3.7. Additional analyses
A hierarchical multiple regression was run to determine if the stepwise addition of loss-related characteristics (time since loss, degree of relationship, age at suicide, age of the deceased), number of completed additional homework tasks, number of sessions attended, and primary outcomes at baseline had an influence on depressive symptoms and suicidality, as well as on posttraumatic stress symptoms and prolonged grief in the treatment group after completing the intervention.
First, we analyzed the change in depressive symptoms, which served as our dependent variable. The full model was statistically significant, R2 = 0.42, F(8, 74) = 8.90, p < .001, adjusted R2 = 0.37. Only the addition of the BDI-II-score at baseline led to a statistically significant increase in R2 of 0.21, F(1, 49) = 15.12, p < .001, indicating that higher BDI-II scores at baseline led to larger improvement in depressive symptoms at post level.
The same model was then computed for suicidality (BSSI). The full model was statistically significant, R2 = 0.28, F(9, 49) = 2.09, p = .048, adjusted R2 = 0.14. The addition of the age of the deceased led to a statistically significant increase in R2 of 0.10, F(1, 50) = 5.83, p = .019, indicating the older the deceased person, the more suicidality recedes. Also, the addition of the BSSI-score at baseline led to a significant increase in R2 of 0.09, F(1, 49) = 6.34, p = .015. The results also indicate that participants with higher BSSI scores at baseline showed a larger improvement in suicidality at post level.
Similar results could be observed for symptoms of prolonged grief and posttraumatic stress symptoms. When looking at the ICG, the full model was significant; R2 = 0.42, F(9, 49) = 3.86, p = .001, adjusted R2 = 0.31, and again, the addition of the age of the deceased as well as the addition of the ICG-score at baseline led to an increase in R2 of 0.12, F(1, 50) = 7.24, p = .010), and R2 of 0.21, F(1, 49) = 17.46, p < .001, respectively. Including the subscales avoidance, hyperarousal, and intrusion of the IES in the regression model, the full models were significant, with R2 = 0.62, F(9, 49) = 9.03, p < .001, adjusted R2 = 0.56, R2 = 0.44, F(9, 49) = 4.23, p < .001, adjusted R2 = 0.33, and R2 = 0.45, F(9, 49) = 4.45, p < .001, adjusted R2 = 0.35, respectively. Here, too, the addition of the respective subscale at baseline led to a significant increase in R2 of 0.53, F(1, 49) = 69.37, p < .001 for avoidance, R2 of 0.27, F(1, 49) = 23.34, p < .001 for hyperarousal, and R2 of 0.32, F(1, 49) = 28.54, p < .001 for intrusion, again, indicating that higher scores at baseline result in greater improvement at post level.
4. Discussion
The first aim of this study was to reduce suicidality and depression in suicide bereaved participants through a 12-week online intervention. Moreover, we aimed to reduce additional secondary outcomes such as prolonged grief, posttraumatic stress symptoms, anxiety, and hopelessness. We expected that symptomatology would improve significantly more in the treatment group after the intervention than in the waiting group after the 3-month waiting period. Furthermore, we wanted to find out which other factors influenced the outcome parameters.
The results of the present study are in line with existing grief literature (for a review, see (Andriessen et al., 2019). It appears that the intervention is effective in trauma-related avoidance in both treatment completers and intention-to-treat analyses and for intrusion in treatment completers. Almost all other outcomes, except suicidality and hopelessness, decreased equally in both groups.
We found no differences between the two groups in terms of primary outcomes. Both suicidality and depression were reduced in the intervention and the control condition. Our results indicate that although the program had an effect on those who completed it, the waiting period appeared to have a similarly positive effect on symptom reduction. These findings are partially consistent with those of previous studies. Van Spijker et al. (2018) developed a web-based self-help program for suicidal thinking and found overall positive effects; however, no differences were shown between the treatment group and the waitlist control group. Similarly, in a study examining the effectiveness of cognitive behavioral therapy on prolonged grief in suicide survivors, no differences were found between a treatment and a waiting group (de Groot et al., 2007). The reasons for this can be manifold. Previous studies have noted that time is a strong factor, especially with regard to grieving (Newsom et al., 2017). It can be assumed that many people process their own grief in a healthy way, even without therapeutic support. However, studies also suggest that while symptoms, especially symptoms of grief, might decrease over time, these might not completely vanish without any form of intervention (Kersting et al., 2011).
Furthermore, by simply participating in the study, filling out the questionnaires, participating in the clinical interview and the instillation of hope, as participants perceived that they would soon be able to take part in an intervention, symptoms could have been influenced— thus leading to a placebo effect (van Spijker et al., 2018). Through the questionnaires and the clinical interview, participants began processing aspects of the loss and reflecting on their own. The preoccupation with this alone could have possibly led to a reduction in symptoms. Even simply the perspective of an imminent intervention could perhaps increase hopefulness in individuals, as well as offer a purpose for the future.
The only significant between-group difference observed at post-assessment was regarding posttraumatic avoidance and intrusion. Here, the treatment group indicated a significant improvement after participation in the intervention.
Moreover, our analyses revealed a significant decrease in symptoms across the measurement points, including a further decline at 3- and 6-month follow-up, after completion of the intervention.
Additional factors that could possibly have an influence on symptomatology at post level in the treatment group were also extracted. Interestingly, neither the relationship to the deceased person, nor time since the loss, nor the number of sessions had an influence on symptomatology.
4.1. Strengths and limitations
To date, only a small number of studies have examined the effectiveness of interventions for individuals bereaved by suicide. However, most of these studies revealed methodological limitations, such as a lack of randomization and small sample sizes, resulting in no sufficient results to determine the actual effectiveness of interventions for the suicide bereaved.
One strength of our study is the randomized controlled design. This is one of the first studies to examine the effectiveness of an intervention specifically developed for the suicide bereaved in accordance with the standards of the CONSORT 2010 statement guidelines for randomized controlled trials (Schulz et al., 2010).
Furthermore, the intervention itself offers flexible and easy-to-implement support for the bereaved, which can be used in a professional context as well as in self-help groups. The materials can be used flexibly, and no additional materials that are difficult to obtain are used. The ease of implementation and online format make the program low-threshold and thus accessible to individuals with limited access to support.
4.2. Limitations
As commonly observed in group interventions, the present study had a high dropout rate, due to our assignment to groups. The results must therefore be considered against the background of the high dropout rate. Furthermore, as in many studies, we depended on participants to answer honestly and truthfully. Despite the telephone interview before inclusion in the study, we could not fully verify whether some psychopathological symptoms were more pronounced than participants reported. In particular, as interested participants were aware of the exclusion criteria, there might have been a moderation of the reported symptomatology. In interpreting the results, it should further be noted that just over half (55%) of the participants were receiving professional help at the time of the intervention. Due to our goal of providing the lowest possible threshold service for survivors after suicide, it did not seem ethically correct to exclude these individuals from the intervention. In other studies evaluating interventions for the suicide bereaved, the use of additional support was not reported as an exclusion criteria (de Groot et al., 2010; Wittouck et al., 2011).
Overall, participants in the treatment condition attended an average of 8.67 sessions, which is not surprising for a 12-week program, but should be considered in the interpretation. Ideally, participants would have attended all sessions, but due to the length of the intervention, this became difficult for participants, due to various reasons (illness, childcare, work commitments).
5. Conclusion
The results of this study indicate that completing an online group intervention developed for the suicide bereaved could reduce psychopathological outcomes over the time. However, only for few symptoms could we find significant differences between the treatment and the waitlist control group, indicating that time itself, or other factors related to treatment expectancy, may be a strong factor in reducing specific psychopathological symptoms.
Although we did not find a significant difference in the respective outcomes, the program may still serve to support suicide bereaved individuals and may accompany them in their grief. Thus, the intervention may have preventive benefits and be used as an addition to ongoing therapy or as a bridge until other professional help can be sought.
The study highlighted that online therapy programs are well and gratefully received by participants and that their low-threshold nature makes them suitable for a large population. Nevertheless, it is important to further investigate online-group interventions in order to maximize their effectiveness and examine which type of intervention is most helpful for individuals bereaved by suicide.
Funding statement
The project was funded by the German Federal Ministry of Health (Bundesministerium für Gesundheit; Project Identifier: ZMVI1-517FSB126)
Ethics approval statement
The trial was approved by the Medical School Hamburg Ethical Committee (reference number MSB-2018-11).
Trial registration
German Clinical Trials Register, DRKS00014426. Registered on 12 April 2018.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.invent.2022.100542.
Appendix A. Supplementary data
Supplementary Material
References
- Andriessen K., Krysinska K., Hill N.T., Reifels L., Robinson J., Reavley N., Pirkis J. Effectiveness of interventions for people bereaved through suicide: a systematic review of controlled studies of grief, psychosocial and suicide-related outcomes. BMC Psychiatry. 2019;19(1):49. doi: 10.1186/s12888-019-2020-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnoldi J., Van de Ven J., Schrieken B., Lange A. University of Amsterdam; 2000. De Risico Taxatielijst eigenschappen van een kort screeningsintrument [Suicide Risk Assessment - A Short Screening Tool] [Google Scholar]
- Bailley S.E., Dunham K., Kral M.J. Factor structure of the Grief Experience Questionnaire (GEQ) Death Stud. 2000;24(8):721–738. doi: 10.1080/074811800750036596. [DOI] [PubMed] [Google Scholar]
- Beck A.T., Weissman A., Lester D., Trexler L. The measurement of pessimism: the hopelessness scale. J. Consult. Clin. Psychol. 1974;42(6):861. doi: 10.1037/h0037562. [DOI] [PubMed] [Google Scholar]
- Beck A.T., Steer R.A., Ranieri W.F. Scale for suicide ideation: psychometric properties of a self-report version. J. Clin. Psychol. 1988;44(4):499–505. doi: 10.1002/1097-4679(198807)44:4<499::aid-jclp2270440404>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- Bellini S., Erbuto D., Andriessen K., Milelli M., Innamorati M., Lester D., Sampogna G., Fiorillo A., Pompili M. Depression, hopelessness, and complicated grief in survivors of suicide. Front. Psychol. 2018;9:198. doi: 10.3389/fpsyg.2018.00198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boelen P.A., de Keijser J., van den Hout M.A., van den Bout J. Treatment of complicated grief: a comparison between cognitive-behavioral therapy and supportive counseling. J. Consult. Clin. Psychol. 2007;75(2):277–284. doi: 10.1037/0022-006x.75.2.277. [DOI] [PubMed] [Google Scholar]
- Bolton J.M., Au W., Leslie W.D., Martens P.J., Enns M.W., Roos L.L., Katz L.Y., Wilcox H.C., Erlangsen A., Chateau D., Walld R., Spiwak R., Seguin M., Shear K., Sareen J. Parents bereaved by offspring suicide: a population-based longitudinal case-control study. JAMA Psychiatry. 2013;70(2):158–167. doi: 10.1001/jamapsychiatry.2013.275. [DOI] [PubMed] [Google Scholar]
- Brent D., Melhem N., Donohoe M.B., Walker M. The incidence and course of depression in bereaved youth 21 months after the loss of a parent to suicide, accident, or sudden natural death. Am. J. Psychiatry. 2009;166(7):786–794. doi: 10.1176/appi.ajp.2009.08081244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen . vol. 2. Lawrence Erlbaum Associates, Publishers; 1988. Statistical Power Analysis for the Behavioral Sciences. [Google Scholar]
- Evans C., Margison F., Barkham M. The contribution of reliable and clinically significant change methods to evidence-based mental health. Evid. Based Ment. Health. 1998;1(3):70–72. doi: 10.1136/ebmh.1.3.70. [DOI] [Google Scholar]
- Foa E.B., Ehlers A., Clark D.M., Tolin D.F., Orsillo S.M. The Posttraumatic Cognitions Inventory (PTCI): development and validation. Psychol. Assess. 1999;11(3):303–314. doi: 10.1037/1040-3590.11.3.303. [DOI] [Google Scholar]
- Gräfe K., Zipfel S., Herzog W., Löwe B. Screening psychischer Störungen mit dem “Gesundheitsfragebogen für Patienten (PHQ-D) Diagnostica. 2004;50(4):171–181. [Google Scholar]
- de Groot M., de Keijser J., Neeleman J., Kerkhof A.J., Nolen W., Burger H. Cognitive behaviour therapy to prevent complicated grief among relatives and spouses bereaved by suicide: cluster randomised controlled trial. BMJ. 2007;334(994) doi: 10.1136/bmj.39161.457431.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Groot M., Neeleman J., van der Meer K., Burger H. The effectiveness of family-based cognitive-behavior grief therapy to prevent complicated grief in relatives of suicide victims: the mediating role of suicide ideation. Suicide Life Threat. Behav. 2010;40(5):425–437. doi: 10.1521/suli.2010.40.5.425. [DOI] [PubMed] [Google Scholar]
- Hautzinger M., Keller F., Kühner C. 2006. Beck Depressions-Inventar (BDI-II) [DOI] [PubMed] [Google Scholar]
- Jacobson N.S., Truax P. Clinical significance: a statistical approach to defining meaningful change in psychotherapy research. J. Consult. Clin. Psychol. 1991;59(1):12–19. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- Kersting A., Kroker K., Schlicht S., Baust K., Wagner B. Efficacy of cognitive behavioral internet-based therapy in parents after the loss of a child during pregnancy: pilot data from a randomized controlled trial. Arch. Womens Ment. Health. 2011;14(6):465–477. doi: 10.1007/s00737-011-0240-4. [DOI] [PubMed] [Google Scholar]
- Kliem S., Lohmann A., Mossle T., Brahler E. German Beck Scale for Suicide Ideation (BSS): psychometric properties from a representative population survey. BMC Psychiatry. 2017;17(1) doi: 10.1186/s12888-017-1559-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knaevelsrud C. Universtität Zürich; 2005. Efficacy of an Internet-driven Therapy (Interapy) for Posttraumatic Stress and the Online Therapeutic Alliance. [Google Scholar]
- Kolves K., Zhao J., Hawgood J., Spence S.H., De Leo D. Suicide and other sudden death bereavement of immediate family members: an analysis of grief reactions six-months after death. J. Affect. Disord. 2019;15(243):96–102. doi: 10.1016/j.jad.2018.09.018. [DOI] [PubMed] [Google Scholar]
- Kovac S.H., Range L.M. Writing projects: lessening undergraduates' unique suicidal bereavement. Suicide Life Threat. Behav. 2000;30(1):50–60. [PubMed] [Google Scholar]
- Krampen G. Hogrefe; Göttingen: 1994. H-Skalen—Skalen zur Erfassung von Hoffnungslosigkeit (Beck Hopelessness Scale; BHS) [Google Scholar]
- Lange A., Schrieken B., Blankers M., Van de Ven J., Slot M. Constructie en validatie van de Gewaarwordingenlijst (GL) een hulpmiddel bij het signaleren van een verhoogde kans op psychosen. Dir Ther. 2000;20(2):162–173. [Google Scholar]
- Linde K., Treml J., Steinig J., Nagl M., Kersting A. Grief interventions for people bereaved by suicide: a systematic review. PLoS One. 2017;12(6) doi: 10.1371/journal.pone.0179496. doi:10.1371/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Löwe B., Zipfel S., Herzog W. Pfizer; 2002. Deutsche Übersetzung und Validierung des “Brief Patient Health Questionnaire (Brief PHQ. [Google Scholar]
- Lumbeck G., Brandstätter M., Geissner E. Erstvalidierung der deutschen version des „Inventory of Complicated Grief” (ICG-D) Z. Klin. Psychol. Psychother. 2012;41(4):243–248. doi: 10.1026/1616-3443/a000172. [DOI] [Google Scholar]
- Maercker A., Schützwohl M. Diagnostica; 1998. Erfassung von psychischen Belastungsfolgen: Die Impact of Event Skala-revidierte Version (IES-R) [Google Scholar]
- Mitchell A.M., Kim Y., Prigerson H.G., Mortimer M.K. Complicated grief and suicidal ideation in adult survivors of suicide. Suicide Life Threat. Behav. 2005;35(5):498–506. doi: 10.1521/suli.2005.35.5.498. [DOI] [PubMed] [Google Scholar]
- Molina N., Viola M., Rogers M., Ouyang D., Gang J., Derry H., Prigerson H.G. Suicidal ideation in bereavement: a systematic review. Behav. Sci. 2019;9(5):53. doi: 10.3390/bs9050053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris S.B. Estimating effect sizes from pretest-posttest-control group designs. Organ. Res. Methods. 2008;11(2):364–386. doi: 10.1177/1094428106291059. [DOI] [Google Scholar]
- Müller J., Wessa M., Rabe S., Dörfel D., Knaevelsrud C., Flor H., Maercker A., Anke K. Psychometric properties of the Posttraumatic Cognitions Inventory (PTCI) in a German sample of individuals with a history of trauma. Psychol. Trauma Theory Res. Pract. Policy. 2010;2(12):116–125. doi: 10.1037/a0018603. [DOI] [Google Scholar]
- Newsom C., Schut H., Stroebe M., Wilson S., Birrell J., Moerbeek M.E., M.C. Effectiveness of bereavement counselling through a community-based organization: a naturalistic, controlled trial. Clin. Psychol. Psychother. 2017;24(6) doi: 10.1002/cpp.2113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfeffer C.R., Jiang H., Kakuma T., Hwang J., Metsch M. Group intervention for children bereaved by the suicide of a relative. J. Am. Acad. Child Adolesc. Psychiatry. 2002;41(5):505–513. doi: 10.1097/00004583-200205000-00007. [DOI] [PubMed] [Google Scholar]
- Pitman A., Osborn D., King M., Erlangsen A. Effects of suicide bereavement on mental health and suicide risk. Lancet Psychiatry. 2014;1(1):86–94. doi: 10.1016/S2215-0366(14)70224-X. [DOI] [PubMed] [Google Scholar]
- Pitman A.L., Osborn D.P., Rantell K., King M.B. The stigma perceived by people bereaved by suicide and other sudden deaths: a cross-sectional UK study of 3432 bereaved adults. J. Psychosom. Res. 2016;87:22–29. doi: 10.1016/j.jpsychores.2016.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prigerson H.G., Maciejewski P.K., Reynolds C., Bierhals A.J., Newsom J.T., Fasiczka A., Frank E., Doman J., Miller M. Inventory of complicated grief: a scale to measure maladaptive symptoms of loss. Psychiatry Res. 1995;59(1):65–79. doi: 10.1016/0165-1781(95)02757-2. [DOI] [PubMed] [Google Scholar]
- Ross V., Kolves K., De Leo D. Exploring the support needs of people bereaved by suicide: a qualitative study. Omega (Westport) 2019 doi: 10.1177/0030222819825775. 30222819825775. [DOI] [PubMed] [Google Scholar]
- Schulz K.F., Altmann D.G., Moher D. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. BMJ. 2010;340 doi: 10.1136/bmj.c332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spangenberg L., Glaesmer H., Scherer A., Gecht J., Barke A., Mainz V., Forkmann T. 2014. Furchtlosigkeit vor dem Tod: die Deutsche version der revidierten Acquired Capability for Suicide Scale. Testmanual. Psychometrikon: psychologisch-medizinisches Testportal. [Google Scholar]
- van Spijker B.A., Werner-Seidler A., Batterham P.J., Mackinnon A., Calear A.L., Gosling J.A., Reynolds J., Kerkhof A.J., Solomon D., Shand F., Christensen H. Effectiveness of a web-based self-help program for suicidal thinking in an Australian community sample: randomized controlled trial. J. Med. Internet Res. 2018;20(2) doi: 10.2196/jmir.8595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner B., Rosenberg N., Hofmann L., Maass U. Web-based bereavement care: a systematic review and meta-analysis. Front. Psychiatry. 2020;11(525) doi: 10.3389/fpsyt.2020.00525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . 2019. Suicide in the World - Global Health Estimates.https://apps.who.int/iris/bitstream/handle/10665/326948/WHO-MSD-MER-19.3-eng.pdf Retrieved 02.04.2022 from. [Google Scholar]
- Wilcox H.C., Mittendorfer-Rutz E., Kjeldgard L., Alexanderson K., Runeson B. Functional impairment due to bereavement after the death of adolescent or young adult offspring in a national population study of 1,051,515 parents. Soc. Psychiatry Psychiatr. Epidemiol. 2015;50(8):1249–1256. doi: 10.1007/s00127-014-0997-7. [DOI] [PubMed] [Google Scholar]
- Wittchen H.-U., Zaudig M., Fydrich T. vol. 28. Hogrefe; 1997. SKID Strukturiertes Klinisches Interview für DSM-IV. Achse I und II. [Google Scholar]
- Wittouck C., Van Autreve S., De Jaegere E., Portzky G., Van Heeringen K. The prevention and treatment of complicated grief: a meta-analysis. Clin. Psychol. Rev. 2011;31(1):69–78. doi: 10.1016/j.cpr.2010.09.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material