Abstract
Objective:
Cervical cancer is the fourth most common gynaecological cancer in the world. Its incidence and burden are high in developing regions, especially in sub-Saharan Africa. The World Health Organization plans to increase vaccination, screening, and treatment of cases to 90%, 70%, and 90%, respectively, in developing countries by 2030. Therefore, the aim of this study was to assess knowledge, attitudes, and practices of cervical cancer screening and predictors among female healthcare providers.
Methods:
Institution-based cross-sectional survey was done from 4 March to 20 April 2019. The data were collected using a structured questionnaire. The data were entered into EpiData version 3.1 and analysed with SPSS version 25. Logistic regression analysis was used to identify associations. After controlling for confounders, an independent association was declared at a p-value of 0.05 with a 95% confidence interval.
Results:
Of a total of 404 participants, half were nurses. One hundred seventy-seven (43.8%) had adequate knowledge, 124 (30.7%) had a favourable attitude, and 35 (8.7%) had regular screening practice. The availability of trained personnel in the health facility and regular screening were variables associated with knowledge. Participants’ attitude was shown association with profession, level of education, and knowledge. Moreover, knowledge of the causes of cervical cancer and knowledge of screening were variables significantly associated with screening practice.
Conclusion and recommendations:
Unfortunately, there is low adequate knowledge, low favourable attitude, and irregular screening practice of cervical cancer in the study area. Despite their own effects, their knowledge and attitude may affect the vast majority of their clients. Therefore, this finding calls for prompt action, such as training for participants to increase awareness, to shape their attitudes, and to increase the uptake of screening services.
Keywords: Knowledge, attitude, cervical cancer screening, female healthcare provider
Introduction
Cervical cancer is an important public health problem and is the fourth most common gynaecological cancer in the world. In 2018 alone, around 570,000 cases and 311,000 deaths from cervical cancer occurred globally. 1
Cervical cancer is not far different from neglected tropical diseases (NTDs) because it highly affects the poor segment of the population; it can be feasibly prevented with available solutions, and they are prevalent in countries with weak health policies. 2
The incidence and mortality from cervical cancer are significantly higher in low- and middle-income countries where access to vaccines, screening, and treatment is limited. 3 Sub-Saharan Africa is a badly affected region by cervical cancer. Of the world’s top 20 countries with the highest cervical cancer cases in 2018, 19 were sub-Saharan countries. 4 Zambia and Ethiopia ranked first and thirteenth in Africa, respectively, in terms of cervical cancer incidence. 5
In Ethiopia, cervical cancer is the second most common cancer type among all cancer cases. It estimated 7445 new cases and caused 5338 cancer deaths nationally. 6
Human papillomavirus (HPV) vaccination and screening have a high potential to eradicate cervical cancer in low- and middle-income countries. 7 The HPV vaccination is a primary prevention strategy to reduce risk of infection with HPV. Services given during vaccination programme are as follows: vaccination of early adolescent girls, healthy sexual education, and provision of condom for sexually active adolescents. 8 Ethiopia introduced the HPV vaccination programme in 2018. 5
Screening is a secondary prevention strategy that helps in early detection and treatment of cases of pre-cancer before they progress to cancer. In the absence of linkage for treatment, screening could not be merely solution for prevention of cervical cancer.8,9 Screening methods include Pap test, HPV DNA test, and visual inspection with acetic acid. The Pap test is used to detect abnormal (cancerous) cells, and the HPV test identifies the specific strains of the virus. 10 In HPV DNA test, the sample can be collected easily, but it is resource-consuming method. Visual inspection with acetic acid is one of the most cheap methods of screening that can detect early cellular changes and more advanced cervical pre-cancer.8,9,11 The other widely accepted screening method is cytology-based method; this method needs especially trained personnel and adequate resources.8,11
The World Health Organization (WHO) recommended regular screening for women from the age of 25 years. 9 The WHO established a 90-70-90 target for low- and middle-income countries by 2030, with the goal of achieving 90% HPV vaccination of girls by the age of 15 years, screening 70% of women by the age of 35 years and again by 45 years, and treating 90% of women diagnosed with the diseases. 3
The Ethiopian Federal Ministry of Health (FMOH) has also been undertaking several prevention and treatment initiatives, such as integration of cervical cancer prevention and treatment services in other women’s healthcare services, including gynaecology clinics, reproductive and child health clinics, and outpatient departments. In addition to this, health extension workers (HEWs) and health development army (HDA) have been playing an important role in promoting an uptake of cervical cancer prevention services. 12 Women’s awareness and attitudes towards HPV vaccination and screening are fundamental. Unawareness and misconception were identified as important variables impacting screening utilization in a study conducted in Nigeria, as well as the adverse effect of poor knowledge on cervical cancer prevention. 13
Healthcare providers are role models for their clients, having sufficient knowledge and a positive attitude towards the care they deliver, which may increase service uptake among clients. They are a source of information about the causes, risk factors, and screening methods of cervical cancer. They can also educate and influence clients’ screening behaviour.14–17
Little has been previously known regarding the knowledge, attitude, and practice of cervical cancer screening among female healthcare workers. The purpose of this study was to assess the knowledge, attitudes, and practices of female healthcare providers in public hospitals in Northwest Ethiopia.
Methods
Study area, design, and period
Institution-based cross-sectional study was conducted in east Gojjam zone public hospitals of Northwest Ethiopia from 4 March to 20 April 2019. The area is bordered on the south by the Oromia Regional State, on the west by west Gojjam, on the north by south Gondar, and on the east by south Wollo, and the rest of the zone is bounded by the bend of the Abay River (Blue Nile). The study area encompasses 22 districts and 4 administrative cities. Regarding hospital coverage, the area has 10 public hospitals in which a total of 1240 healthcare providers were working. Of these, 798 were males and 442 were females.
Study participants and eligibility criteria
All female healthcare providers who were working in public hospitals in the area were considered the source population. All permanent employees or employers (who had ⩾6 months of experience) were included. On the contrary, those who were absent (on maternity leave, annual vacation, training leave, or severely sick) during data collection were excluded from this study.
Sampling size and sampling techniques
To make the sample more representative, we have calculated the sample size for all objectives and used the maximum sample size. A single population proportion formula was used, with assuming a 95% confidence interval (CI), 5% margin of error, and a population proportion of 60.9%, 71.7%, and 2.2% for knowledge, attitude, and practice, respectively. 18 Accordingly, the calculated total sample size was 367, 312, and 33, respectively, for knowledge, attitude, and practice. The largest sample, n = 367, was used for this study by adding a 10% non-response rate, so the total sample size was n = 404.
To select the study participants, first, zones in Northwest Ethiopia were clustered. So, the east Gojjam zone was randomly selected using the lottery method, and all 10 public hospitals in the zone were purposefully included. Since it is unfair to sample 404 from 442 female healthcare providers in the 10 public hospitals of the zone, they were entirely included in the study.
Data collection tool, procedure and study variables
A self-administered questionnaire contained questions on cervical cancer screening knowledge, attitude, and practice as outcome variable and socio-demographic features such as age, marital status, educational level, religion, ethnicity, profession, number of parity, and family history; institutional factors such as screening service availability, materials/instrument availability, and trained personnel availability; and family planning utilization and personal characteristics as independent variables. The tool was adapted after reviewing different literatures.13,14,18–22 Five trained non-employed BSc nurses and two supervisors (public health professionals) were involved in the data collection.
Data quality control
To ensure data quality, an English version of the questionnaire was translated to Amharic (the local language) and back to English to assure consistency; training was given for both data collectors and supervisors regarding the aim of the study and data collection procedures, and a pre-test was conducted among 20 female HCPs outside of the selected zone. Moreover, the data collection process was checked by supervisors and investigators on a daily basis to ensure data completeness and consistency.
Statistical analysis
Data are filtered and double-checked for accuracy after collection before being entered into EpiData version 3.2 and analysed using SPSS version 25. The descriptive statistics were presented using tables, pie charts, and graphs. The association between outcome and explanatory variables was tested using binary logistic regression analysis after checking for multicollinearity. In multivariate analysis, all variables with a p-value of less than 0.2 in bivariate analysis were included, and independent association was declared at a p-value of ⩽0.05. To choose the optimal model, the Hosmer–Lemeshow goodness of fit test was used.
Operational definition
Knowledge
The knowledge of cervical cancer was assessed using 12 questions, which were composed of yes or no questions. Participants who scored above the mean were regarded as knowledgeable, and those who scored below the mean were regarded as not knowledge.19,20
Attitude
Attitude was assessed by 11 Likert-type scale questions. The questions on the Likert-type scale have positive and negative responses that range from strongly agree, agree, neither agree nor disagree, disagree and strongly disagree. Those who scored above the mean were considered to have a favourable attitude and those who scored below the mean had an unfavourable attitude.18,20
Screening practice
The practice was assessed by looking at the respondent’s actions towards screening for cervical cancer in the past 5 years. Those who have been screened in the last 5 years are considered to have regular screening. Individuals who have been screened for more than 5 years are considered to have irregular screening. 18
Results
Socio-demographic feature of the participants
A total of 404 female healthcare providers participated in this study, which means a response rate of 91.1%. The mean age of participants was 30 years (standard deviation (SD) ±5). About half of the participants were nurses, and more than half were diploma holders (Table 1).
Table 1.
The socio-demographic features of female healthcare providers at public hospitals of Northwest Ethiopia (n = 404).
| Variables | Categories | Frequency | Percentage |
|---|---|---|---|
| Age (in years) | ⩽30 | 146 | 36.1 |
| ⩾31 | 258 | 63.9 | |
| Religion | Orthodox | 395 | 97.8 |
| Muslim | 6 | 1.5 | |
| Others a | 3 | 0.7 | |
| Ethnicity | Amhara | 400 | 99 |
| Oromo | 4 | 1 | |
| Marital status | Single | 180 | 44.6 |
| Married | 216 | 53.5 | |
| Divorced | 4 | 1 | |
| Widowed | 4 | 1 | |
| Profession | Doctor | 27 | 6.7 |
| Health officer | 7 | 1.7 | |
| Laboratory | 47 | 11.6 | |
| Midwifery | 60 | 15.0 | |
| Nurse | 203 | 50.2 | |
| Pharmacy | 55 | 13.6 | |
| Others b | 5 | 1.2 | |
| Qualification level | Diploma | 235 | 58.5 |
| Degree and above | 169 | 41.8 | |
| Experience (in years) | 1–5 | 315 | 78.0 |
| 6–10 | 64 | 15.8 | |
| 11 or more | 25 | 6.2 | |
| Number of pregnancies | 0 | 243 | 60.1% |
| 1–4 | 156 | 38.7% | |
| ⩾5 | 5 | 1.2% |
Others: protestant (2) and catholic (1).
Others: ISO (1) and radiographer (4).
Family planning utilization and personal characteristics of study participants
Participants used modern contraceptives in 42.1% of cases, with implants accounting for 73 (18.6%), injectables accounting for 54 (13.4%), combined oral contraceptive (COC) and progestogen-only pill (POP) 47 (11.6%), intrauterine contraceptive device (IUCD) 9 (2.2%), and condoms accounting for 3 (0.7%). Fortunately, none of the participants reported substance use in this study.
Health institutions’ characteristics
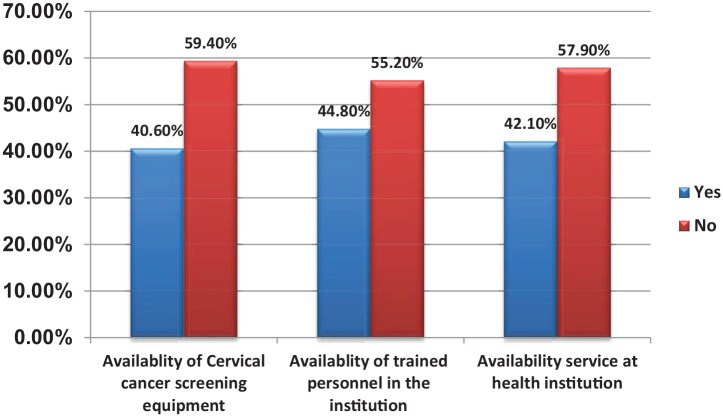
In this study, more than half of the health institutions (55.2%) did not have cervical cancer screening equipment, and also more than half of the institutions (55.2%) did not have trained personnel who provide screening (Figure 1).
Figure 1.
The health institutions’ characteristics where the participants are working (n = 404).
Knowledge about cervical cancer
A total of 177 (43.8%) participants were adequately informed about cervical cancer screening. Among the participants, 118 (29.2%) were aware of the cause of cervical cancer, whereas 179 (44.3%) were aware of the risk factors. Nearly half of the participants were aware of cervical cancer prevention methods (Table 2).
Table 2.
Participants’ knowledge about cervical cancer screening (n = 404).
| Knowledge questions | Response category | Frequency | Percentage |
|---|---|---|---|
| Cause of cervical cancer | Yes | 118 | 29.2 |
| No | 286 | 70.8 | |
| Family history of risk for cervical cancer | Yes | 150 | 37.1 |
| No | 254 | 62.9 | |
| Risk factors of cervical cancer | Yes | 179 | 44.3 |
| No | 225 | 55.7 | |
| Symptom of cervical cancer | Yes | 192 | 47.5 |
| No | 212 | 52.5 | |
| The outcome of cervical cancer if not treated early | Yes | 173 | 43 |
| No | 231 | 57 | |
| Cervical cancer screening procedure | Yes | 153 | 37.9 |
| No | 251 | 62.1 | |
| Types of screening | Yes | 196 | 48.5 |
| No | 208 | 51.5 | |
| Group of women recommend for cervical cancer screening | Yes | 193 | 47.8 |
| No | 211 | 52.2 | |
| Frequency of cervical cancer screening | Yes | 185 | 45.8 |
| No | 219 | 54.2 | |
| Cervical cancer prevention method | Yes | 194 | 48 |
| No | 210 | 52 |
Attitude of participants towards practice of cervical cancer screening
Cervical cancer screening was viewed favourably by nearly one-third of participants (30.7%), while it was viewed negatively by 69.3%. Fifty-eight (14.3%) of participants agreed that the burden of cervical cancer in Ethiopia is high; 79 (19.5%) agreed that carcinoma of the cervix is the leading cause of women’s death among all malignancies; 54 (13.4%) agreed that cervical cancer screening is effective when performed by female healthcare providers; and 83 (20.5%) agreed that screening can detect cervical cancer before symptoms appear. However, 79 (19.5%) of participants agreed that screening is unnecessary if asymptomatic; 125 (31.0%) of them agreed that the cervical cancer screening procedure is painful; and 116 (28.7%) agreed that having cervical cancer screening is embarrassing (Table 3).
Table 3.
Participants’ attitude towards cervical cancer screening (n = 404).
| Attitude questions | Response categories | ||||
|---|---|---|---|---|---|
| Strongly agree | Agree | Neutral | Disagree | Strongly disagree | |
| Burden of cervical cancer in Ethiopia is high | 8 (2%) | 58 (14.3%) | 37 (9.2%) | 194 (48%) | 107 (26.5%) |
| Carcinoma of the cervix is a leading cause of women death amongst all malignancy | 5 (1.2%) | 79 (19.5%) | 30 (7.5%) | 184 (45.5%) | 106 (26.3%) |
| Carcinoma of the cervix is highly prevalent amongst all malignancies in Ethiopia | 5 (1.2%) | 72 (17.8%) | 41 (10.2%) | 192 (47.5%) | 94 (23.3%) |
| Cervical cancer screening is embarrassing | 33 (8.1%) | 116 (28.7%) | 49 (12.1%) | 157 (39.0%) | 49 (12.1%) |
| Cervical cancer screening procedure is painful | 39 (9.6%) | 125 (31.0%) | 72 (17.8%) | 131 (32.4%) | 37 (9.2%) |
| Cervical cancer screening causes no harm | 27 (6.7%) | 88 (21.8%) | 34 (8.4%) | 136 (33.7%) | 119 (29.4%) |
| Screening service is good if done by female healthcare providers | 20 (4.9%) | 54 (13.4%) | 25 (6.2%) | 149 (36.9%) | 156 (38.6%) |
| Screening should be done only when a woman developed a symptom | 22 (5.4%) | 85 (21.0%) | 34 (8.4%) | 153 (38.0%) | 110 (27.2%) |
| Female healthcare providers susceptible for cervical cancer | 24 (6.0%) | 73 (18.0%) | 42 (10.4%) | 232 (57.5%) | 33 (8.1%) |
| Screening is not necessary if there are no signs and symptoms | 18 (4.5%) | 79 (19.5) | 8 (2%) | 177 (43.8%) | 122 (30.2%) |
| Screening can detect cervical cancer before symptoms appear | 14 (3.5%) | 83 (20.5%) | 4 (1.0%) | 136 (33.7%) | 167 (41.3%) |
Cervical cancer screening practice
Surprisingly, only 35 (8.7%) participants did regular cervical cancer screening. From these, 27 (6.7%) participants were screened by inspection, whereas the remaining 8 (2.0%) were screened via a Pap smear (Figure 2).
Figure 2.
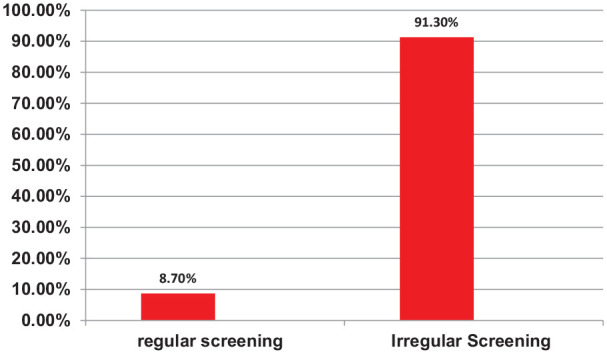
The screening practice of female healthcare providers in public hospitals of Northwest Ethiopia (n = 404).
Reasons participants did not do cervical cancer screening
One hundred fifty-one (37.4%) of participants mentioned the inaccessibility of the service delivery as a reason for not having screening. About one-third of participants perceived screening as unnecessary (27.5%) (Figure 3).
Figure 3.
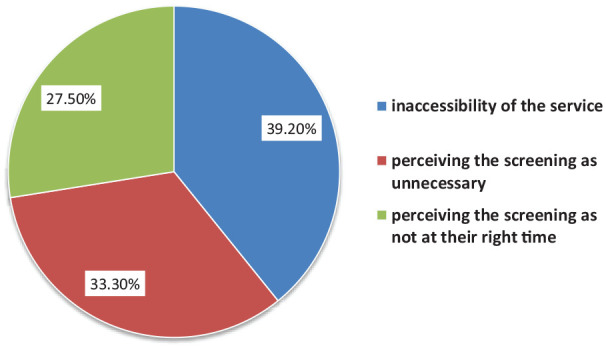
The reasons why female healthcare providers did not screen for cervical cancer in public hospitals of Northwest Ethiopia.
Factors associated with knowledge of cervical cancer screening
The availability of trained personnel and regular screening service were variables found to be significantly associated with knowledge of cervical cancer screening in multivariate analysis.
In view of that, those participants who had worked in health facilities with trained personnel were 1.8 (adjusted odds ratio (AOR) = 1.8, 95% CI (1.12–3.35)) times more likely to be knowledgeable compared to those participants working in health facilities that had no trained personnel. Participants who screened on a regular basis were 5.3 (AOR = 5.3, 95% CI (2.38–9.12)) times more likely to be knowledgeable compared to those who had irregular screening practice (Table 4).
Table 4.
A bivariate and multivariate analysis results showing factors associated with knowledge of cervical cancer screening practice among female healthcare providers at public hospitals of Northwest Ethiopia (n = 404).
| Variables | Categories | Knowledge | COR (95% CI) | AOR (95% CI) | |
|---|---|---|---|---|---|
| Knowledgeable | Not knowledgeable | ||||
| Age | ⩾31 | 55 (13.6%) | 91 (22.5%) | 1 | 1 |
| ⩽30 | 122 (30.2%) | 136 (33.7%) | 0.7 (0.51–0.99) | 0.6 (0.42–1.16) | |
| Educational level | Degree | 77 (19.1%) | 92 (22.8%) | 1 | 1 |
| Diploma | 100 (24.7%) | 135 (33.4%) | 0.9 (0.66–1.32) | 0.9 (0.69–1.43) | |
| Availability equipment | Yes | 73 (18.0%) | 90 (22.3%) | 1 | 1 |
| No | 104 (26.0%) | 136 (33.7%) | 1 (0.73–1.60) | 0.9 (0.6–1.5) | |
| Availability of trained person | No | 90 (22.3%) | 91 (22.5%) | 1 | 1 |
| Yes | 87 (21.5%) | 136 (33.7%) | 1.6 (0.86–1.80) | 1.8 (1.12–3.35)* | |
| Availability of service at health facilities | Yes | 79 (19.5%) | 91 (22.5%) | 1 | 1 |
| No | 98 (24.3%) | 136 (33.7%) | 1.2 (0.18–2.38) | 0.8 (0.46–1.52) | |
| Attitude | Unfavourable attitude | 135 (33.4%) | 145 (35.9%) | 1 | 1 |
| Favourable attitude | 42 (10.4%) | 82 (20.3%) | 1.8 (1.26–3.87) | 2.3 (1.4–3.8) | |
| Screening practice | Irregular screening | 152 (37.6%) | 217 (53.7%) | 1 | 1 |
| Regular screening | 25 (6.2%) | 10 (2.5%) | 0.3 (0.13–0.64) | 5.3 (2.38–9.12)* | |
COR: crude odds ratio; AOR: adjusted odds ratio.
p-value ⩽ 0.05 and 1 = reference group.
Factors associated with attitude towards cervical cancer screening
In bivariate analysis, participants’ attitudes towards cervical cancer screening were related to their level of education, profession, year of experience, availability of screening equipment, availability of trained personnel, availability of service at a health facility, cervical cancer screening procedure, knowledge, and screening practice.
However, levels of education, participants’ profession, and knowledge towards screening were found to be independently associated variables with attitude in multivariate analysis. As a result, participants who held at least a degree were 2.5 (AOR = 2.5, 95% CI (1.63–3.94)) times more likely than those who held a diploma to have a favourable attitude towards cervical cancer screening.
In this study, physicians were 2.4 (AOR = 2.4, 95% CI (1.03–6.25)) times more likely than others (radiographers and integrated emergency surgery officers) to have a favourable attitude. Similarly, midwives were 1.3 (AOR = 1.3, 95% CI (1.03–3.34)) times more likely to have positive attitude than radiographers and integrated emergency obstetrics surgery officers.
When compared to those who were not knowledgeable about cervical cancer screening, those who were knowledgeable were 1.6 (AOR = 1.6, 95% CI (1.04–2.86)) times more likely to have a favourable attitude (Table 5).
Table 5.
A bivariate and multivariate analysis results showing factors associated with attitude of cervical cancer screening practice among female healthcare providers at public hospitals of Northwest Ethiopia (n = 404).
| Variables | Categories | Attitude | COR (95% CI) | AOR (95% CI) | |
|---|---|---|---|---|---|
| Favourable | Unfavourable | ||||
| Age | ⩾31 | 65 (16.1%) | 81 (20.0%) | 1 | 1 |
| ⩽30 | 59 (14.6%) | 199 (49.3%) | 2.7 (1.7–4.2) | 0.54 (0.4–0.9) | |
| Profession | Physician | 22 (5.4%) | 5 (1.2%) | 2.9 (1.08–5.32) | 2.4 (1.03–6.25)* |
| Public health officer | 3 (0.7%) | 4 (1.0%) | 0.5 (0.09–0.97) | 0.2 (0.06–0.75) | |
| Laboratory | 22 (5.4%) | 25 (6.2%) | 0.6 (0.03–0.88) | 0.5 (0.07–0.87) | |
| Midwifery | 41 (10.1%) | 19 (4.7%) | 1.4 (1.07–3.05) | 1.3 (1.03–3.34)* | |
| Nurse | 143 (35.4%) | 60 (15.0%) | 1.6 (1.10–2.98) | 1.5 (1.08–3.03) | |
| Pharmacy | 24 (6.0%) | 31 (7.7%) | 0.8 (0.07–0.97) | 0.7 (0.09–0.99) | |
| Others a | 3 (0.7%) | 2 (0.5%) | 1 | 1 | |
| Level of educational | Diploma | 52 (12.9%) | 183 (45.3%) | 1 | 1 |
| Degree and above | 72 (17.8%) | 97 (24.0%) | 0.5 (0.39–0.80) | 2.5 (1.63–3.94)** | |
| Availability of screening equipment | Yes | 66 (16.3%) | 98 (24.3%) | 1 | 1 |
| No | 58 (14.4%) | 182 (45.0%) | 2.1 (1.45–3.30) | 1 (0.62–3.73) | |
| Availability of trained personnel | Yes | 63 (15.7%) | 118 (29.2%) | 1 | 1 |
| No | 61 (15.1%) | 162 (40.0%) | 0.7 (0.47–1.41) | 1.5 (0.70–3.08) | |
| Availability of service at health facility | Yes | 69 (17.1%) | 101 (25.0%) | 1 | 1 |
| No | 55 (13.6%) | 179 (44.3%) | 0.45 (1.10–4.64) | 0.7 (0.44–1.25) | |
| Cervical cancer screening procedure | Yes | 46 (11.4%) | 107 (26.5%) | 1 | 1 |
| No | 78 (19.3%) | 173 (42.8%) | 1.1 (0.65–2.06) | 1.2 (0.66–2.30) | |
| Knowledge | Knowledgeable | 82 (20.3%) | 145 (35.9%) | 1.8 (1.01–2.99) | 1.6 (1.04–2.86)* |
| Not knowledgeable | 42 (10.4%) | 135 (33.4%) | 1 | 1 | |
| Screening practice | Regular screening | 268 (66.3%) | 101 (25.0%) | 1.38 (1.03–3.06) | 1.93 (1.07–3.99) |
| Irregular screening | 23 (5.7%) | 12 (3.0%) | 1 | 1 | |
COR: crude odds ratio; AOR: adjusted odds ratio.
Others: IEOS (1) and radiographer (4).
p-value ⩽ 0.05; **p-value ⩽ 0.001 and 1 = reference group.
Factors associated with practice of cervical cancer screening
In multivariate analysis, knowing about the causes of cervical cancer and the availability of screening equipment were found to be factors affecting cervical cancer screening practice. The likelihood of cervical cancer screening was 9 (AOR = 9.0, 95% CI (8.12–17.95)) times higher among participants who did know the causes of cervical cancer when compared to those who did not know. Participants who were knowledgeable about cervical cancer screening were 3.2 (AOR = 3.2, 95% CI (1.08–8.45)) times more likely to undergo regular screening compared to those not knowledgeable (Table 6).
Table 6.
A bivariate and multivariate analysis results showing factors associated with cervical cancer screening practice among female healthcare providers at public hospitals of Northwest Ethiopia (n = 404).
| Variable category | Screening practice | COR (95%CI) | AOR (95%CI) | ||
|---|---|---|---|---|---|
| Regular practice | Irregular practice | ||||
| Age | ⩾31 | 15 (3.7%) | 243 (60.1%) | 1 | 1 |
| ⩽30 | 20 (5.0%) | 126 (31.2%) | 0.4 (0.2–0.8) | 1.75 (0.77–3.96) | |
| Use of modern contraceptive | Yes | 165 (40.8%) | 69 (17.1%) | 3.4 (1.05–7.09) | 2.7 (1.56–7.45) |
| No | 70 (17.3%) | 100 (24.8%) | 1 | 1 | |
| Knew cause of cervical cancer | Yes | 212 (52.5%) | 74 (18.3%) | 13.2 (7.10–19.05) | 9.0 (8.12–17.95)* |
| No | 21 (5.2%) | 97 (24.0%) | 1 | 1 | |
| Knowledge | Not knowledgeable | 25 (6.2) | 152 (37.6%) | 1 | 1 |
| Knowledgeable | 10 (2.5%) | 217 (53.7%) | 3.5 (1.13–8.60) | 3.2 (1.08–8.45)** | |
| Availability of screening equipment | No | 23 (5.7%) | 141 (35.0%) | 1 | 1 |
| Yes | 12 (2.9%) | 228 (56.4%) | 3.10 (1.75–6.07) | 1.6 (0.69–3.98) | |
COR: crude odds ratio; AOR: adjusted odds ratio.
p-value ⩽ 0.05; **p-value ⩽ 0.001 and 1 = reference group.
Discussion
Strong health services that are sufficiently armed with skilled human resources are very important in awareness creation, information propagation, delivering screening tests, diagnosis, treatment, and follow-up, as well as evaluation of screening programmes. 7 The knowledge, attitude, and practice of frontline (healthcare workers) are crucial in the early detection and treatment of cases. Therefore, the purpose of this study was to assess knowledge, attitude, and screening practice of cervical cancer screening among female healthcare providers.
In this study, 43.8% of participants had adequate knowledge about cervical cancer screening. This finding is higher compared to a previous study conducted in Saudi Arabia where only 4% of participants had good knowledge. 22 The possible reasons for this difference could be variations in personal beliefs, information, and policy and time differences. The finding is lower than previous studies conducted in Turkey (48.58%), Jordan (47.2%), India (58.9%), Nigeria (100%), Uganda (83%), southern Ethiopia (86.9%), and Hawassa University (56.8%).15,17,19–21,23,24 This discrepancy could be due to differences in training opportunities for the care givers in the study areas, and it might also be due to variations in healthcare policies in the areas.
In this study, 44.3% of participants knew the risk factors for cervical cancer. This result is lower than studies conducted in Chennai, India (85%), and Uganda (40%).23,24 The likely discrepancy could be training gaps between the two populations. About half of the participants were aware of cervical cancer prevention methods. This finding is larger than a previous study conducted in Nigeria in which only 8% of participants knew about cervical cancer prevention methods. 13 However, this result is less than studies conducted in Albania, India, and Addis Ababa where 100%, 92.5%, and 93.5% of participants were aware of the cervical cancer prevention strategies, respectively.23,25,26 The possible reasons for this discrepancy could be availability and media coverage for information dissemination and also due to the utilization of training on about cervical cancer prevention. In this study, 37.9% of participants had awareness of cervical screening procedures; that is, a lower number compared to a study conducted in India (95.3%). 23 The possible difference might be the availability of the screening service and either pre-serve or in-service training in the previous study area.
In this study, participants who had been working in health facilities that had trained personnel were 1.8 times more likely to be knowledgeable than those participants who had been working in health facilities with no trained personnel. This finding is congruent with a study conducted in Jordan. 21 Noticeably, regular practice of a certain procedure increases the understanding of that specific procedure; participants having had regular cervical screening were 5.3 times more knowledgeable than those who had had irregular screening. This finding was supported by a study conducted in King Fahad Medical City, Saud Arabia. 22
Regarding to participants’ attitudes, nearly one-third (30.7%) viewed cervical cancer screening favourably. The current finding is lower compared to a previous study conducted at Hawassa University (55.3%). 20 The likely discrepancy might be variations in values and beliefs in the current and previous study populations and areas in general. Moreover, it could be due to exposures to training in the study population. In this study, 58 participants agreed that cervical cancer is a public health burden, which was supported by different literatures.14,24,27 In this study, participants who were knowledgeable about cervical cancer had 1.6 times more probability of having a favourable attitude than those who were not knowledgeable. This finding was consistent with a previous study conducted at Hawassa University. 20 In this study, participants’ profession was found to be a significant factor affecting the attitude of participants. Accordingly, the likelihood of having a favourable attitude was 2.4 times higher among physicians than among radiographers and integrated emergency and obstetrics surgery officers. Likewise, it was 1.5 times higher among midwives than among radiographers and integrated emergency and obstetrics surgery officers. This finding was not supported by the literature, but the possible reason for this association could be due to curricular variations among the professions. In addition, the level of education was significantly associated with the attitudes of participants. Participants whose education level was at least a degree were 2.5 times more likely to have favourable attitudes than those who studied only diplomas. Despite evidence of a relationship between education level and attitude, 28 a similar study did not support this finding. It is understandable that an individual’s health beliefs and attitudes increase with their level of education.
Unlike a similar study conducted in Addis Ababa, where none of the participants had regular cervical cancer screening, 14 in this study, 8.7% of participants said that they had regular cervical cancer screening. This change may be due to time variation and study design. This finding is comparable with a previous study in Southeastern Nigeria, which found that 9% of female health workers had already been screened. 29 This result is slightly higher than a previous study conducted in rural India, where only 7% of participants were screened. 30 This mismatch could be attributed to time variation, a lack of screening services in the previous area, or discrepancies in levels between the two populations. Unfortunately, this result falls short of studies conducted in Singapore, Ankara, Jordan, south-south Nigeria, Uganda, Tanzania, and Addis Ababa, where 42.2%, 14.87%, 19.1%, 17.1%, 15.4%, and 40% of health workers, respectively, had regular screening.14,17,21,24,27,31,32 This variation could be due to dissimilarities in socio-demographics, availability of the screening service, and having had training among the populations. Of the reasons the participants reported not having had screening, 39.2% were due to inaccessibility of the screening service, which was supported by a previous study conducted in Vlora City, Albania, and Nigeria, where participants mentioned non-availability of the screening service as the main reason for not having had screening.26,29
A study conducted in Nigeria shown a significant association between knowledge and screening practice. 13 Equally, in this study, participants who had knowledge of screening practice were 3.2 times more likely to having had regular practice than others.
Participants who had having awareness of the causes/aetiology of cervical cancer were nine times more likely to have had regular screening compared to those who have had irregular screening. This correlation could be due to participants’ expectation and fear of the disease outcome.
Limitation of the study
This study utilized an adequate sample size that guarantees generality. However, due to its cross-sectional nature, the findings could not secure a cause–effect relationship. And also, it would not overlook the hidden factors that possibly affect the attitude of the participant.
Conclusion
There is low adequate knowledge, low favourable attitude, and irregular screening practice of cervical cancer in the study area. An availability of trained personnel in the facilities and screening practice showed a significant association with knowledge of participants. Level of education, participants’ profession, and knowledge towards screening practice were variables found to be significantly associated with attitudes of participants. Moreover, knowing the causes of cervical cancer and the availability of screening equipment were variables shown a significant association with screening practice. Therefore, this finding urges the Amhara Regional Health Bureau, the Ethiopia Ministry of Health, and any interested non-governmental organizations to give special attention to reviewing the undergoing prevention strategies and to providing training for female staff in order to improve the knowledge, attitude, and practice of cervical cancer screening and to strengthen cervical cancer screening education programmes. Likewise, we recommend the Ministry of health and Ministry of education collaborate to evaluate the cervical cancer issue in educational curricula. In addition, we recommend interested researchers to consider qualitative studies to explore some concealed behaviours of participants regarding cervical cancer prevention.
Supplemental Material
Supplemental material, sj-docx-1-smo-10.1177_20503121221095931 for Female healthcare providers’ knowledge, attitude, and practice towards cervical cancer screening and associated factors in public hospitals of Northwest Ethiopia by Eden Abebaw, Mulugeta Tesfa, Wubishet Gezimu, Firomsa Bekele and Abdissa Duguma in SAGE Open Medicine
Acknowledgments
The authors express their heartfelt gratitude to all study participants, data collectors, and supervisors without whom this study would not have been expected.
Footnotes
Author contributions: E.A. contributed to the proposal development, methodology, analysis, and preparing the first draft of the manuscript. M.T., W.G., F.B., and A.D. were contributed to supervision, methodology, and data analysis and editing of the manuscript. Finally, all the team revised and approved the manuscript before submission.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: Before this study began, an institutional research ethics review committee of Debre Markos University, College of Health Science, had assessed the proposal for potential risks and benefits to the study participants (reference no. IHR/CHS/107/11).
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Each of the study participant was informed and willingly signed up to participate. Fortunately, all participants in this study were professionals (educated), so they all signed the written consent form after being informed about the study’s risks and benefits.
ORCID iDs: Wubishet Gezimu  https://orcid.org/0000-0002-5503-1360
https://orcid.org/0000-0002-5503-1360
Firomsa Bekele  https://orcid.org/0000-0002-7855-9838
https://orcid.org/0000-0002-7855-9838
Abdissa Duguma  https://orcid.org/0000-0001-7725-6061
https://orcid.org/0000-0001-7725-6061
Supplemental material: Supplemental material for this article is available online.
References
- 1. Arbyn M, Weiderpass E, Bruni L, et al. Estimates of incidence and mortality of cervical cancer in 2018: a worldwide analysis. Lancet Glob Health 2020; 8(2): e191–e203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Knaul FM, Rodriguez NM, Héctor Arreola-Ornelas JRO. Comment cervical cancer: lessons learned from neglected tropical diseases. Lancet Glob Health 2019; 7: 299–300, www.thelancet.com/lancetgh [DOI] [PubMed] [Google Scholar]
- 3. World Health Organization. Global strategy to accelerate the elimination of cervical cancer as a public health problem and its associated goals and targets for the period 2020–2030, vol. 2. New York: United Nations General Assembly, 2020. [Google Scholar]
- 4. Martin JY, Erickson BK, Huh WK. World Health Organization Regional Office for Africa: cervical cancer. Evidence-based Obstet Gynecol 2018; 2018: 165–72. [Google Scholar]
- 5. Bruni L, Albero G, Serrano B, et al. ICO/IARC information centre on HPV and cancer (HPV Information Centre). Human papillomavirus and related diseases in Ethiopia. Summary Report, 2016, www.hpvcentre.com
- 6. World Health Organization. Ethiopia Globocan2020. Int Agency Research Cancer 2021; 133: 2020–2021. [Google Scholar]
- 7. Sankaranarayanan R. Screening for cancer in low- and middle-income countries. Ann Glob Heal 2014; 80(5): 412–417. [DOI] [PubMed] [Google Scholar]
- 8. World Health Organization (WHO). Comprehensive Cervical Cancer Control A and guide to essential practice. 2nd ed. Geneva: WHO, 2014, pp. 366–78. [PubMed] [Google Scholar]
- 9. Ullrich BA, Garwood P, Clayes P, et al. Can we prevent cervical cancer? Eur Mag Sex Reprod Heal 2007; 64: 1–12. [Google Scholar]
- 10. Clark J. Cervical cancer screening. BMJ 2003; 326(7392): 770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. WHO and guidance note: comprehensive cervical cancer prevention control: a healthier future for girls women. WHO, 2013, www.who.int/about/licensing/ [Google Scholar]
- 12. Federal Democratic Republic of Ethiopia Ministry of Health. Guideline for cervical cancer prevention control in Ethiopia, https://www.iccp-portal.org/system/files/plans/Guideline%20Eth%20Final.pdf
- 13. Mbamara SU, Ikpeze OC, Okonkwo JEN, et al. Knowledge, attitude and practice of cervical cancer screening among women attending gynecology clinics in a tertiary level medical care center in Southeastern Nigeria. J Reprod Med Obstet Gynecol 2011; 56(6): 491–496. [PubMed] [Google Scholar]
- 14. Kress CM, Sharling L, Owen-Smith AA, et al. Knowledge, attitudes, and practices regarding cervical cancer and screening among Ethiopian health care workers. Int J Womens Health 2015; 7: 765–772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ifemelumma CC, Anikwe CC, Okorochukwu BC, et al. Cervical cancer screening : assessment of perception and utilization of services among health workers in low resource setting. Int J Reprod Med 2019; 2019: 6505482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hweissa NA, Lim JN, Su TT. Health-care providers’ perceptions, attitudes towards and recommendation practice of cervical cancer screening. Eur J Cancer Care (Engl) 2016; 25(5): 864–870. [DOI] [PubMed] [Google Scholar]
- 17. Med A, Hastanesi D, Hekimli A, et al. Knowledge, attitudes and behaviors of health workers about cancer screenings. Ankara Med J 2017; 17(1): 73–83. [Google Scholar]
- 18. Tadesse A. Knowledge, Attitude and Practice (KAP) towards screening for cervical cancer among Adama University female students, Adama, Ethiopia, 2015, http://etd.aau.edu.et/bitstream/handle/123456789/3989/AlmazTadesse.pdf?sequence=1&isAllowed=y [DOI] [PMC free article] [PubMed]
- 19. Dulla D, Daka D, Wakgari N. Knowledge about cervical cancer screening and its practice among female health care workers in Southern Ethiopia: a cross-sectional study. Int J Womens Health 2017; 9: 365–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Gultie T. Knowledge and attitude towards cervical cancer screening and associated factors among female Hawassa University College of medicine and health sciences students. MOJ Public Heal 2018; 7(3): 151–158. [Google Scholar]
- 21. Obeidat BR, Amarin ZO, Alzaghal L. Awareness, practice and attitude to cervical Papanicolaou smear among female health care workers in Jordan. Eur J Cancer Care (Engl) 2012; 21(3): 372–376. [DOI] [PubMed] [Google Scholar]
- 22. Heena H, Durrani S, AlFayyad I, et al. Knowledge, attitudes, and practices towards cervical cancer and screening amongst female healthcare professionals: a cross-sectional study. J Oncol 2019; 2019: 5423130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Sudharshini S, Anantharaman V, Chitra A. A cross-sectional study on knowledge, attitude, and practice on cervical cancer and screening among female health care providers of Chennai corporation, 2013. J Acad Med Sci 2012; 2(4): 124. [Google Scholar]
- 24. Mutyaba T, Mmiro FA, Weiderpass E. Knowledge, attitudes and practices on cervical cancer screening among the medical workers of Mulago Hospital, Uganda. BMC Med Educ 2006; 4: 4–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Getahun F, Addissie A, Negash S, et al. Assessment of cervical cancer services and cervical cancer related knowledge of health service providers in public health facilities in Addis Ababa, Ethiopia. BMC Res Notes 2019; 12(1): 1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Fatjona K, Theodhosi G, Bilushi Y, et al. An overview of cervical cancer knowledge and screening among female healthcare practitioners. Eur Sci J 2020; 10: 173–184. [Google Scholar]
- 27. Urasa M, Darj E. Knowledge of cervical cancer and screening practices of nurses at a regional hospital in Tanzania. Afr Health Sci 2011; 11(1): 48–57. [PMC free article] [PubMed] [Google Scholar]
- 28. Zimmerman E, Woolf SH. Understanding the relationship between education and health. 2014. http://www.iom.edu/understandingtherelationship
- 29. Anya SE, Oshi DC, Nwosu SO, et al. Knowledge, attitude, and practice of female health professionals regarding cervical cancer and pap smear. Niger J Med 2005; 14(3): 283–286. [PubMed] [Google Scholar]
- 30. Shekhar S, Sharma C, Thakur S, et al. Cervical cancer screening: knowledge, attitude and practices among nursing staff in a tertiary level teaching institution of rural India. Asian Pac J Cancer Prev 2013; 14(6): 3641–3645. [DOI] [PubMed] [Google Scholar]
- 31. Eze GU, Obiebi IP, Umuago IJ. Perspectives of cervical cancer and screening practices among staff of a teaching hospital in South-South Nigeria. J Cancer Res Pract 2018; 5(2): 67–73. [Google Scholar]
- 32. Tay K, Tay SK, Tesalona KC, et al. Factors affecting the uptake of cervical cancer screening among nurses in Singapore. Int J Gynecol Obstet 2015; 130(3): 230–234. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-smo-10.1177_20503121221095931 for Female healthcare providers’ knowledge, attitude, and practice towards cervical cancer screening and associated factors in public hospitals of Northwest Ethiopia by Eden Abebaw, Mulugeta Tesfa, Wubishet Gezimu, Firomsa Bekele and Abdissa Duguma in SAGE Open Medicine