Abstract
Background
For the general population, the positive effects of paid employment on health and wellbeing are well established. However, less is known for people from refugee and asylum-seeking backgrounds. This review aims to systematically summarise the quantitative literature on the relationship between employment and health and wellbeing for refugees and asylum seekers.
Method
A search strategy was conducted in online databases, including MEDLINE, PsychINFO, EMCARE, SCOPUS, CINHAL, ProQuest and Web of Science. Articles were screened against inclusion and exclusion criteria. Studies published in English between 2000 to October 2021 were included if they used quantitative methods to consider the relationship between employment and health for refugees and asylum seekers in resettlement countries. Study quality was assessed using The Joanna Briggs Institute's Critical Appraisal Tools. Findings were synthesised using a narrative approach.
Results
Seventy-two papers were identified. The majority of papers (N = 58, 81%) examined the association between employment and mental health outcomes. Overall, while there were inconsistencies in the findings, employment had a positive effect on mental health particularly in reducing levels of psychological distress and depression. Though more limited in number, the papers examining physical health suggest that people who are employed tend to have better physical health than unemployed persons. There was some evidence to support the bi-directional relationship between employment and health. Poor mental and physical health negatively impacted the odds of employment and occupational status of refugees.
Conclusion
Good quality employment is an essential component of refugee resettlement and this review found that in general employment is also beneficial for refugee health, particularly aspects of mental health. More research regarding the effects of employment on physical health is required. The effects of refugee-specific factors such as gender roles, torture, and trauma on the relationship between employment and health also require further investigation.
Keywords: Refugee, Asylum seeker, Employment, Social determinants of health, Occupational health
1. Introduction
Employment is an important social determinant of health (Marmot et al., 2008). There is a strong body of evidence supporting the benefit of paid employment for health and wellbeing (van der Noordt, Ijzelenberg, Droomers, & Proper, 2014; Modini et al., 2016; Hergenrather, Zeglin, McGuire-Kuletz, & Rhodes, 2015). The World Health Organisation (WHO) Commission on Social Determinants of Health highlighted that fair employment and good working conditions provide financial security, enhanced social status, and personal development which are protective for mental and physical health (Marmot et al., 2008).
For people from refugee and asylum-seeking backgrounds, stable and appropriate employment is a significant contributor towards successful resettlement (Olliff, 2010). However, refugees and asylum seekers face unique barriers entering the labour market including discrimination, language barriers, lack of local experience and referees, and limited knowledge of local labour markets (Olliff, 2010). There is growing research to suggest that difficulties in securing employment and experiences at work affect health and wellbeing for refugees and asylum seekers (Blight, Ekblad, Persson, & Ekberg, 2006; Bridekirk, Hynie, & SyRia.lth, 2021; Sundquist, Ostergren, Sundquist, & Johansson, 2003). However, to date, there has been no comprehensive consideration of the quantifiable health effects of employment in this population, nor how health itself may influence employment experiences. This paper aims to systematically review the existing quantitative literature on the relationship between employment and health and wellbeing for people of refugee and asylum-seeking backgrounds living in resettlement countries.
1.1. Terminology
Refugees are defined as people who meet the criteria for refugee status according to the United Nations High Commissioner for Refugees and asylum seekers are defined as those awaiting their claims to refugee status to be determined (UNHCR, 2021). For brevity, this review uses the term ‘refugee’ to describe both refugees and asylum seekers unless there is something specifically of relevance to either group.
Resettlement countries are those that have established and ongoing resettlement programs in cooperation with the United Nations High Commissioner for Refugees (UNHCR, 2011). The focus of this review was to understand the relationship between employment and health in resettlement countries.
The World Health Organisation (WHO) defines health as ‘a state of complete physical, mental and social wellbeing not merely the absence of disease or infirmity’ (World Health Organiz, 2021). As such, in this paper, the term ‘health’ is used to refer to both health and broader wellbeing.
1.2. Background
The health benefits of employment for the general population are documented in several systematic reviews and meta-analyses (Milner, Page, & LaMontagne, 2014; Modini et al., 2016; Hergenrather et al., 2015; Paul & Moser, 2009; Pinto, Hassen, & Craig-Neil, 2018; van der Noordt et al., 2014). A meta-review of 11 qualitative and quantitative systematic reviews established that having a job is associated with improved self-reported wellbeing, mental health, and fewer symptoms of depression, anxiety, and psychological distress (Modini et al., 2016). Relatedly, unemployment is associated with mental health illness (Hergenrather et al., 2015.; Milner et al., 2014), poor physical health outcomes (van der Noordt et al., 2014; Hergenrather et al., 2015), and mortality in particular due to suicide (Modini et al., 2016).
In examining the complex links between employment and health several pathways of influence have been highlighted (Benach, Muntaner, Solar, Santana, & Quinlan, 2010). The WHO Commission on Social Determinants of Health highlighted macro and micro-level pathways by which employment may affect health (Benach, Muntaner, et al., 2010). Macro-level pathways describe the institutional factors including governmental (e.g welfare regimes, social policies) and labour market conditions (e.g labour regulations, trade union power) that are ‘upstream’ determinants of the employment and working conditions (Benach, Muntaner, et al., 2010; Muntaner et al., 2010). At the micro-level employment conditions (nature of working arrangements – e.g. secure, precarious, informal, unemployed) and working conditions (physical and psychological conditions related to work tasks – e.g. occupational injuries, psychosocial stressors) influence health outcomes (Benach, Muntaner, et al., 2010, Benach, Solar, et al., 2010).
Bi-directional pathways have also been identified between health and employment (van der Noordt et al., 2014). Although the causation hypothesis, which asserts that employment influences health outcomes, has more evidence, research also supports the selection hypothesis which posits that health is a determinant of labour market participation (McDonough & Amick, 2001; Pelkowski & Berger, 2004; Schuring et al., 2007). For example, rates of unemployment are generally higher among people with disabilities or poor health (Schuring et al., 2007), and people with better health status have higher odds of obtaining and maintaining a job (McDonough & Amick, 2001; Pelkowski & Berger, 2004). The effects of mental health on employment have also been documented in several studies which found that mental ill-health is a risk factor for unemployment, while good mental health promotes employment (Frijters, Johnston, & Shields, 2014; Olesen et al., 2013).
In considering these pathways, the relationship between employment and health is also influenced by individual and contextual factors such as race, ethnicity, immigration status, and social class (Benach, Muntaner, et al., 2010). Population groups that are more marginalised are likely to be more affected by underemployment and health inequities (Benach, Muntaner, et al., 2010). Refugees represent one of the most vulnerable population groups and there is a high unemployment rate amongst refugees globally (Dumont et al., 2016). For example, studies conducted in the USA and UK have shown that refugees are twice as likely to be unemployed compared to other immigrants, even when controlling for differences in age, gender, and level of education (Jamil, Aldhalimi, & Arnetz, 2012; Ruiz & Vargas-Silva, 2018). It is important to note, however, that refugees are a heterogeneous group of people with widely differing experiences, cultural backgrounds, religious affiliations, and resettlement needs. These cross-cultural elements play a fundamental role in the way people from refugee backgrounds perceive health, employment and the relationship between the two (Sullivan, Vaughan, & Wright, 2020).
Additionally, understanding the relationship between employment and health for refugees is an important economic and public health issue. At the end of 2020, there were an estimated 82.4 million forcibly displaced people worldwide, including 26.4 million refugees and 4.1 million asylum seekers (UNHRC, 2021a). With higher rates of mental health issues for refugees (Gleeson et al., 2020), understanding the role of employment in health is crucial. To date, no systematic review has considered the quantifiable relationship between employment and refugee health. This review aims to summarise the existing quantitative literature on the relationship between employment and health for refugees and asylum seekers in resettlement countries.
2. Methods
The review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) and Joanna Briggs Institute (JBI) guidelines. The protocol was registered with the International Prospective Register of Systematic Reviews (PROSPERO CRD42020151228).
2.1. Inclusion/Exclusion criteria
Studies needed to be empirical, peer-reviewed, published from 2000 to October 2021, and available in English. Only quantitative studies describing the association between employment and mental or physical health for refugee and/or asylum seeker populations were included. Participants had to be aged 18 years or over. Studies that did not disaggregate the data of refugee or asylum seekers from other groups or only focused on non-refugee migrants were excluded. The focus of this review was resettlement countries, studies involving internally displaced populations or people in detention centres, refugee camps, or transition countries were excluded.
Consistent with the WHO definition and biopsychosocial model of health, this review included all outcomes that pertain specifically to health. Predictors and antecedents of health such as self-esteem, sense of identity, social inclusion, and studies that focussed on health care access were excluded. Unpaid forms of employment such as training programs and volunteer work were also excluded.
2.2. Search strategy and screening
A search strategy was developed using a combination of Medical Subline Headings (MeSH) and keywords search. Three blocks of search terms were combined with the Boolean operator ‘AND’: (1) terms for refugees and asylum seekers (refugee* OR asylum seeker* OR “humanitarian entrant*”); (2) terms for employment (employ*OR unemploy* OR occupation* OR job* OR work* OR labour OR labor OR salary OR salaries OR wage); and (3) terms for health outcomes (health OR wellbeing OR stress OR “mental health” OR “quality of life” OR “post traumatic stress” OR PTSD OR anxiety OR depress*).
Electronic database searches were executed with the assistance of a librarian in MEDLINE, PsychINFO, EMCARE, SCOPUS, CINHAL, ProQuest and Web of Science. The searches were initially performed in March 2020 and finalised on October 25, 2021 (See Appendix 1).
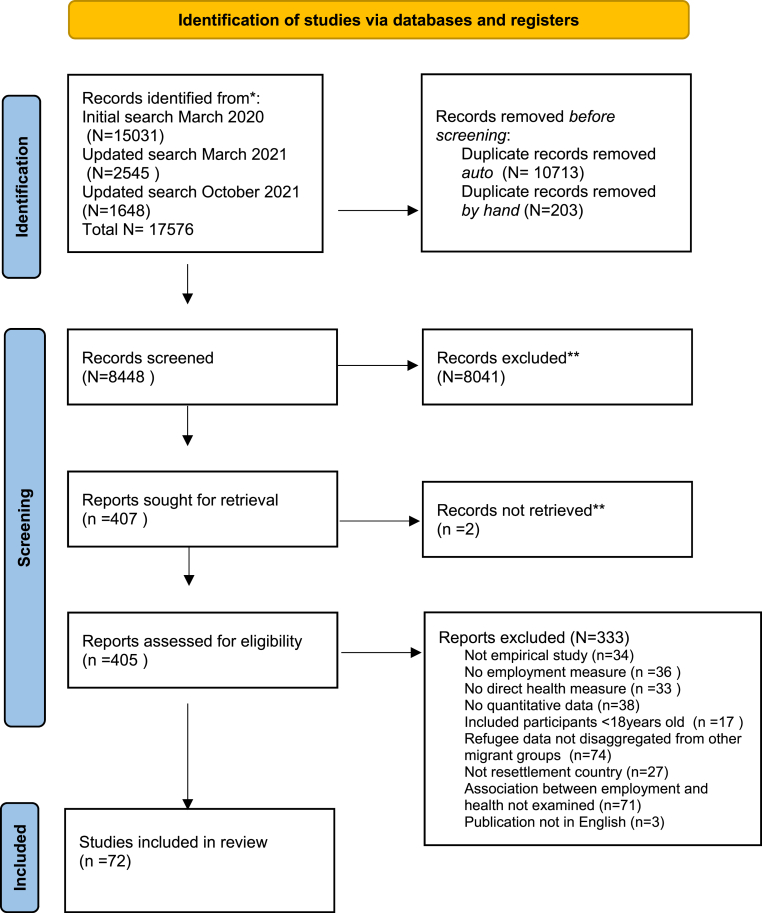
Articles retrieved were compiled into EndNote X9 and duplicates were removed. The remaining articles (N = 8448) were uploaded to Covidence for title and abstract screening by the lead author. Titles and abstracts not within the scope of the review were excluded (N=8041). The full texts of the remaining articles (N = 407) were screened against the inclusion and exclusion criteria. See Fig. 1 for details. At both stages of screening, a 10% sample was assessed by the second and third authors. Any disagreements about inclusion/exclusion were discussed by all three authors until consensus was reached (overall agreement 90.9%; Kappa 0.757).
Fig. 1.
PRISMA flowchart of study selection.
2.3. Data extraction and synthesis
Key information from full-text articles was extracted into a table. These included the study design, country, study population, employment-related variable, measure of health, statistical analysis, and findings relating to employment and health. A narrative summary of the results concerning the mental, physical, and general health outcomes was conducted. Due to the variation in measured outcomes of the included studies, no meta-analyses were performed.
2.4. Quality assessment
The quality of the included studies was evaluated using the Joanna Briggs Institute's (JBI) Critical Appraisal Checklist for Analytical Cross-Sectional Studies, Critical Appraisal Checklist for Cohort Studies, and the Checklist for Randomised Controlled Trials. The quality assessment was independently conducted by the lead author based on the published version of the papers. The question responses were determined based on the employment and health aspects even if the papers did not set out to specifically examine this relationship. A 20% sample of 14 papers was assessed by the second and third authors. Any disagreements between the reviewers were resolved by discussion (overall agreement 93%; Kappa 0.834). One point was assigned to any question where the answer was ‘Yes’. The positive scores were summed and a percentage calculated for each paper. The quality of each study was rated as high (80–100%), moderate (50–79%) or low (<50%) (Lam et al., 2019; Poudel et al., 2018) (Appendix 2). No articles were excluded based on quality assessments to provide a comprehensive overview of all available studies on employment and refugee health.
3. Results
Electronic database searches identified 17576 references, of which 72 met the inclusion criteria after the two-stage screening process (Fig. 1). The main reasons for exclusion after full-text review were lack of employment (N = 36) or direct health measure (N = 33), refugee or asylum seeker data was not disaggregated from other groups (N = 74), and the study did not explore the relationship between employment and health (N = 71).
An overview of the study characteristics is outlined in Table 1 and the studies are described in detail in Table 2, Table 3, Table 4. Of the 72 papers, the majority (N = 59) included participants who were refugees. Five papers included only asylum seekers, and 8 papers included both refugees and asylum seekers. More than half (N=39) were published between 2016 and 2021, indicating this is a growing area of research. All the studies were conducted in high-income countries of resettlement. Except for the three papers from South Korea, most studies were from nominally “Western” Countries with the largest number from the United States (USA) (N = 22), followed by Scandinavia (N = 14), Australia, and New Zealand (N = 9). The sample size of the studies varied significantly, ranging from 41 participants to populations of over 200,000 people. Employment status was the most commonly examined employment variable (N=55). Other aspects of employment explored in the articles included job satisfaction, occupational quality, and work-related stressors. Several health outcomes were reported within individual papers. Most of the reviewed papers (N=58) included a mental health outcome. Twelve papers examined physical health outcomes, eight papers included general health and seven papers reported on life satisfaction.
Table 1.
Summary table of study characteristics.
| Number of studies (N = 72) | |
|---|---|
| Year of publication | |
| 2000–2005 | 7 |
| 2006–2010 | 11 |
| 2011–2015 | 15 |
| 2016–2021 | 39 |
| Informant group | |
| Refugees | 59 |
| Asylum seekers | 5 |
| Refugees and asylum seekers | 8 |
| Region of study | |
| South Korea | 3 |
| Italy | 4 |
| United Kingdom | 5 |
| Germany | 8 |
| Netherlands | 4 |
| Greece | 1 |
| Scandinavia (Denmark, Norway, Sweden, Switzerland) | 14 |
| United States | 22 |
| Canada | 7 |
| Australia/New Zealand | 9 |
| Employment variables | |
| Employment status | 55 |
| Unable to find work | 6 |
| Job quality/satisfaction | 5 |
| Employment-related stressors | 3 |
| Occupational status | 3 |
| Other | 3 |
| Health variables | |
| Mental health | 58 |
| General health | 8 |
| Life satisfaction | 7 |
| Physical health | 12 |
Table 2.
Description of studies on employment and mental health.
| Authors Date |
Country | Study design | Study population | Measure of employment | Measure of health | Statistical Analysis | Main findings of employment and health | Quality |
|---|---|---|---|---|---|---|---|---|
| Ahmad, 2020 | Canada | Cross sectional survey | N = 49 Afghan refugees |
Employment status | PTSD: HTQ | Chi square | Employment was significantly associated with lower PTSD scores: prevalence of PTSD was zero in those employed and 59.1% in those unemployed (p = 0.02). | High |
| Ahmad, 2020 | Canada | Longitudinal study | N = 1924 Syrian refugees |
Employment status | Depression: PHQ-9 | Chi square Logistical regression |
Unemployment was significantly associated with higher prevalence of depression symptoms at both baseline (x2 = 16.7, p < 0.001) and year 2 (x2 = 7.8, p = 0.005). In the multinomial logistic model, employment was not significantly associated with depressive symptoms. |
Moderate |
| Alemi, 2015 | USA | Cross sectional survey | N = 130 Afghan refugees |
Employment status | General psychological distress: Afghan Symptom Checklist | Multivariate linear regression | Employment was not a significant predictor of psychological distress. | Moderate |
| Ao, 2016 | USA | Cross sectional survey | N = 423 Bhutanese refugees |
Employment status Unable to find work |
Suicide risk, ideation, and exposure: 19-item measure | Logistic regression | Inability to find work (aOR = 11.1; 95% CI = 2.4–51.5) was one of the main post-migration difficulties associated with past suicidal ideation. | Moderate |
| Aragon, 2019 | Italy | Cross sectional survey | N = 67 Chinese Asylum seekers |
Unemployment Problems at work Unable to find work |
PTSD: HTQ | Logistical regression | 52.2% of the participants reported being unable to find work as a post migration living difficulty and this significantly increased the likelihood of having PTSD (OR = 2.22, 95% CI = 1.16–4.27, p = 0.016). | Moderate |
| Baranik, 2018 | USA | Cross sectional survey | N = 159 Refugees |
Vocational stressor | Anxiety: Warr's measure. Depression: CES-D scale Sleep disturbance: 3 items questionnaire |
T-test and Regression Analysis | Refugees experiencing discrimination as a vocational stressor reported higher levels of depression (p < 0.01), anxiety (p < 0.05) and sleep disturbances (p <0.01) than those who did not report discrimination. Only the association between discrimination and depression and anxiety held after controlling for other variables. | Moderate |
| Beiser, 2001 | Canada | Prospective longitudinal study | N = 608 South-East Asian Refugees |
Employment status | Depression: Inventory of 45 items | Covariance structural equation model | Unemployment only became significantly related to depression at year 2 (r = 0.113) and year 10 (r = 0.095). At 10 years follow up unemployment was associated with increased levels of depression among men but not among women. | High |
| Beiser, 2006 | Canada | Cross sectional survey | N = 647 South-East Asian refugees |
Employment status | Depression: Depressive Affect Measure Scale | Multivariate regression | Unemployment had significant and positive associations with depression levels (B = 1.57, SE = 0.64), p < 0.05. Unemployed refugees who had a strong commitment to their ethnic identity had a higher depression score (p < 0.001). For refugees endorsing a weak ethnic identity, unemployment had no impact on depression scores (p > 0.05). | High |
| Barbieri, 2020 | Italy | Cross sectional survey | N = 122 African refugees and asylum seekers |
Employment status | PTSD: PCL-5 | Logistic regression | Employment status did not significantly predict PTSD symptom severity. | High |
| Brigg, 2013 | New Zealand | Cross sectional survey and interview | N = 100 Refugees |
Employment status | Demoralisation: Demoralisation Scale | ANOVA | Participants who were unemployed had a significantly higher demoralisation score than those who were employed (p < 0.001). | Low |
| Bhui, 2006 | UK | Cross sectional survey | N = 143 Somali refuges |
Employment status | Mental disorders: M.I.N.I | Logistical regression | In the regression model, employment (full time or part-time) was associated with lower levels of mental disorder (aOR = 0.03, 95% CI = 0.01–0.61, p < 0.05) | High |
| Blight, 2006 | Sweden | Cross sectional survey | N = 413 Bosnia-Herzegovina refugees |
Employment status Yearly Economic Activity (EA) |
General mental health: Goteborg Quality of Life instrument | Logistical regression | Unemployment was associated with a higher level of symptoms of poor mental health for men (OR = 8.01 (2.36–27.23) p = 0.001) but not women (OR 1.16 (0.46–2.40), p = 0.75). For women, working for longer periods was associated with poor mental health (OR 4.52 (1.25–16.31), p = 0.02). | Moderate |
| Bogic, 2012 | Germany Italy UK |
Cross sectional survey | N = 854 Former Yugoslavia Refugees |
Employment status | Mental Disorders: M.I.N.I | Multivariate logistical regression | Higher rates of mood disorders (major depression, dysthymia, hypomania, mania) were associated with being unemployed (aOR = 1.99(1.35–2.93, p = 0.001). Unemployment was not significantly associated with other mental disorders including PTSD anxiety disorders and substance use disorders. | High |
| Briderkirk, 2021 | Canada | Longitudinal study | N = 577 Syrian refugees |
Hourly wage Quality of employment Satisfaction with wage and job Job appropriateness |
Stress: PSS-10 General mental health: RAND-36 |
Correlations Hierarchical regression |
General mental health was positively correlated with satisfaction with current wage (r = 0.28, p < 0.001), job appropriateness (r = 0.15, p < 0.001), job satisfaction (r = 0.32, p < 0.001), perceived control, (r = 0.51, p < 0.001). In the regression, general mental health was higher among refugees making enough money (B = 0.74, p = 0.01) and satisfied with their job (B = 0.64, p = 0.04). Job appropriateness and hourly wage did not significantly predict general mental health | Moderate |
| Bryant, 2019 | Australia | Cross sectional study | N = 1767 Refugees |
Work as a post migration stressor | Prolonged Grief Disorder: 4 item self reported-screening measure | Chi square | Refugees with probable Prolonged Grief Disorder were more likely to be unemployed. Only 5% those with PGD were employed compared to 27.8% with no PGD (p < 0.001) | Low |
| Campbell, 2018 | UK | Longitudinal study | N = 5678 baseline N = 939 at the third follow-up, 21 months after baseline |
Employment status Current job appropriateness for skills and qualifications |
Emotional wellbeing: Question from (SF-36) |
Ordered logistic regression | In the unadjusted cross-sectional analyses, refugees who were unemployed or have a job lower than one's skills and qualifications had higher odds of poorer emotional wellbeing in (p < 0.05). However, in the longitudinal analysis it was no longer significant. | High |
| Carlsson, 2006 | Denmark | Longitudinal study | N = 139 Refugees from Iran, Iraq and Lebanon |
Employment status | PTSD: HTQ Anxiety & Depression: HSCL-25 Wellbeing: WHOQOL-Bref |
Multiple linear regression | Being employed was negatively correlated with depression and anxiety scores, HSCL-25 total (β = −0.33, p < 0.001), HSCL-25 depression (β = −0.33, p < 0.001), HSCL-25 anxiety(β = -0.29, p < 0.01), HTQ PTSD (β = -0.32, p < 0.01). Employment/self-employment was positively correlated with WHOQOL Bref mental (β = 0.49, p < 0.001) and WHOQOL Bref physical (β = 0.27, p < 0.001) |
High |
| Cetrez, 2021 | Sweden | Cross sectional survey | N = 140 Iraqi Refugees |
Employment status | Mental health: self-perceived health from the PC-PTSD screen | Descriptive statistics | Unemployment (68.4%) was one of the most commonly given explanations of mental ill-health | Moderate |
| Cochran, 2013 | USA | Cross sectional survey | N = 579 Bhutanese refugees |
Being unable to find work | Suicide ideation | Logistic regression | Being unable to find work (AOR = 11.1, CI (2.4–51.1) was one of the main post-arrival difficulties associated with suicidal ideation. | Moderate |
| Cooper, 2019 | Australia | Longitudinal study | Baseline, N = 2399 Wave 2, N = 2009 Wave 3, N = 1894 Refugees and asylum seekers |
Employment status | High Risk of Mental Illness: K6 PTSD: PTSD-8 |
Generalized linear mixed models | Unemployment was not a significant predictor of mental illness. | High |
| De Vroome, 2010 | Netherlands | Cross sectional survey | N = 3269 Refugees |
Employment status Occupational status: International Socio-Economic Index (ISEI) |
Depression: 4 item measure created for the study General health: self-rated 5-point scale |
Binary logistic regression (employment variable) Linear regression (occupational status variable) |
Depression was negatively associated with the odds of employment (OR = −0.192, SE = 0.044, p < 0.01) and occupational status (B = −2.110, SE = 0.750, p < 0.05). General health problems were negatively associated with odds of employment (OR = −0.274, SE = 0.030, p < 0.01) and occupational status (B = −3.951, SE = 0.545, p < 0.01) |
Moderate |
| Di Thiene, 2021 | Sweden | Prospective longitudinal study | N = 2895 refugees N = 3684 Migrants N = 26936 Swedish born |
Long-term unemployment (LTU) Long-term sickness absence (LTSA) Disability pension (DP) |
Common mental disorders (depressive, anxiety, stress-related disorder according to the ICD-10) | Cox proportional hazard regression models | For those with common mental disorders, the adjusted risk estimates of long-term unemployment were higher for refugees from Africa, Asia and Europe outside EU25 (HR: 2.39, HR: 2.16 and HR: 1.61, respectively), compared to Swedish born individuals | High |
| Drescher, 2021 | Switzerland Jordan Turkey |
Cross sectional survey | N = 57 Switzerland N = 61 Jordan N = 46 Turkey Refugees and asylum seekers |
Employment | Psychological distress: K10 Psychological functioning: WHODAS |
Descriptive statistics | In the Switzerland sample those who showed increased psychological distress (K10) and decreased psychological functioning (WHODAS), 18 (32%) expressed employment concerns, 16 (28%) stated concerns about finding a job/suitable job. | Moderate |
| Drydakis, 2022 | Greece | Longitudinal study | N= Refugees | Written work contract: Y/N Exposure to workplace abuse/threats: Y/N Hourly wage lower than the corresponding national minimum wage: Y/N |
Physical health: EQ-VAS Depression: CESD |
Correlation Random effect regression Model |
Physical health is negatively associated with the probability of workers not having a written contract of employment (r = − 0.61, p < 0.01) and with the probability of workers experiencing insults and/or threats in their present job (r = −0.45, p < 0.01). The estimates suggest a positive association between depression and workers not having a written contract of employment (coef = 4.312, p < 0.01, or 18.5%), workers receiving a net hourly wage lower than the corresponding national minimum (coef = 5.005, p < 0.01, or 28.5%), and workers experiencing insults and/or threats in their present job (coef = 3.915, p <0.01, or 13.3%) |
Moderate |
| Eisen, 2020 | USA | Longitudinal study | N = 78 Torture surviving asylum seekers |
Employment status | PTSD: HTQ-30 Anxiety and Depression: HSCL-25 |
Multiple regression analysis | Employment status was not independently associated with a change in PTSD symptom levels or depressive symptom levels. Participants' symptoms improved over time (B = −0.254, p = 0.001), independent of changes in measured post-migratory factors such as employment and housing. | Low |
| Grochtdreis, 2020 | Germany | Cross sectional survey | N = 6821 Refugees and asylum seekers |
Employment status | Physical and mental health status: SF12 | Linear regressions | Persons that were employed had higher mean PCS and MCS scores than unemployed persons (56.0 and 50.8 vs. 53.1 and 47.6). Unemployed persons had lower PCS scores than employed persons (B = −1.6 (95% CI-2.42; −0.77), p < 0.001). Unemployment was statistically associated with lower MCS scores (B = −2.9 (95% CI = −4.01; 1.76), p < 0.001) |
High |
| Helgesson, 2021 | Sweden | Longitudinal study | N = 239,742 Refugees N = 4133898 Swedish-born |
Employment status Disability pension |
ICD-10 somatic/mental disorders | Multivariate Cox Regression models | Refugees with specific somatic/mental disorders especially neoplasms (HR: 1.72; 95% CI: 1.56 to 1.91), diseases in the musculoskeletal system (HR: 1.57; 95% CI: 1.47 to 1.67)) and circulatory system (HR: 1.33; 95% CI: 1.22 to 1.45) and depressive disorders (HR: 1.31; 95% CI: 1.21 to 1.41) had a higher risk of disability pension compared with Swedish- born individuals with similar disorders. | High |
| Hermansson, 2003 | Sweden | Longitudinal study | Total = 44 male refugees tortured (n = 22) non-tortured (n = 22) | Employment status | Anxiety & Depression: HSCL-25 PTSD: PTSS-10 Psychological Well-being: Self-rating scale, “How do you feel?” |
Spearman correlation | In the non-tortured group, being employed was negatively correlated with HSCL-25 anxiety (rs = −0.70, p < 0.001), HSCL-25 depression (rs = −0.66, p < 0.01) and HSCL-25 total (rs = −0.69, p < 0.001. There was also a significant negative correlation between employment and PTSS-10 (rs = −0.56, p < 0.01). There was a significant positive correlation between being employed and well-being (rs = 0.49, p < 0.05). No significant associations between employment and mental health measures were observed in the tortured group. |
Moderate |
| Hermansson, 2002 | Sweden | Longitudinal study | Same sample as above | Employment status | Anxiety & Depression: HSCL-25 PTSD: PTSS-10 Psychological Well-being: Self-rating scale |
Wilcoxon rank sum | Unemployment was associated with a lower level of mental health according to the measure of HSCL-25 anxiety (W = −2.28, p < 0.05) and PTSS-10 (W = −2.06, p < 0.05). Unemployment was not significantly associated with depression or psychological wellbeing. | Moderate |
| Hocking, 2015 | Australia | Cross sectional survey | N = 98 Asylum seekers |
Employment status | PTSD: HTQ Anxiety & Depression: HSCL-25 |
Mann-Whitney test Multiple regression analyses |
Mann-Whitney showed that being employed was associated with reduced severity of anxiety (U = 793, p = 0.03, n = 95) and depressive (U = 807, p = 0.04, n = 95) symptoms. Asylum seekers who were not employed were more likely to be diagnosed with MDD (OR = 2.61, 95% CI, 1.11–6.13; p = 0.03, n = 95). |
High |
| Hunkler, 2020 | Germany | Cross sectional survey | N = 275 Syrian Refugees |
Employment status | General health: self-rated 5-point scale Mental health: “generally feel anxious, depressed and/or stressed” Y/N |
Structural integration model | Overall health significantly increased the probability of employment by 3 percent (p < 0.05), while mental state showed no significant effect. | High |
| Jeon, 2009 | South Korea | Cross sectional survey | N = 367 North Korean Refugees |
Employment status | Depression: The Korean version of CES-D | Multiple regression | People without occupations were 2.289 times (95% CI, 1.386–3.780) more likely to report depressive symptoms than those with occupations. In the multiple regression analysis, having no occupation [OR = 2.198, 95% CI, 1.247–3.873] was correlated with depressive symptoms. | High |
| Kashyap, 2019 | USA | Longitudinal study | N = 323 Refugees and asylum seekers |
Employment status | Depression: PHQ-9 PTSD: HTQ Self-reported chronic pain: Y/N |
Linear regression | Employment alone was not significantly associated with PTSD or depression. However, employment and stable housing together significantly moderated the relationship between lower chronic pain and reduced PTSD. Among individuals who reported experiencing chronic pain at the 6-month follow-up assessment (N = 170), lower chronic pain was associated with having stable housing (B = −0.89 (SE = 0.44), p < 0.05, β = −0.16) and with being employed (B = −0.83 (SE = 0.37), p < 0.05, β = −0.17. | Moderate |
| Kim, 2011 | South Korea | Cross sectional survey | N = 144 North Korean refugees |
Employment status | Psychological problems: Symptom Checklist-90-Revised (SCL-90-R): Depression: CES-D |
Stepwise logistic regression | Unemployment was related to a higher prevalence of obsessive-compulsive symptoms (B = 2.769(0.022), p = 0.05) and psychoticism (B = 2.013(0.037), p < 0.05). No significant relationship between employment status and other psychiatric symptoms including somatization, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation | High |
| Kim, 2016 | USA | Cross sectional survey | N = 656 Latino and Asian refugees |
Employment status | Self-rated mental health: 5 point scale Mental disorders: CIDI interview |
OLS regressions Logistic regression analyses |
Being unemployed was not significantly associated with self-reported mental health, mood disorders or anxiety disorders. Refugees who were not in the labor force had significantly higher odds (OR = 6.48 95% CI (2.05–20.49), p < 0.01) of being diagnosed with any of the three mood disorders (ie major depression, dysthymia, and intermittent explosive) measured in the survey |
High |
| Laban, 2005 | Netherlands | Cross sectional Survey and interview |
N = 294 Asylum seekers |
Employment status - No permission to work - Work below skill level |
Mental disorders: CIDI interview | Multivariate logistic regression | Almost 75% of the asylum seekers who stayed more than 2 years in the Netherlands mentioned lack of work as an important stressor. No work/work below level had the highest OR for lifetime prevalence of depressive disorder (OR = 1.32 95%CI (1.08–1.61), one or more psychiatric disorders (OR 1.44, 95%CI (1.15–1.81) and one or more psychiatric disorders (excluding PTSD) (OR = 1.37, 95% CI (1.11–1.69). No work/work below level was not significantly associated with anxiety disorder. | High |
| Marshall, 2005 | USA | Cross sectional Interview |
N = 490 Cambodian refugees |
Employment status | PTSD and depression: CIDI interview Alcohol use disorder: Alcohol Use Disorders Identification Test |
Bivariate Odds Ratio | Unemployment was associated with higher rates of major depression (OR = 4.44, 95% CI (2.51–7.87), but not PTSD or alcohol use disorder. | Moderate |
| Maximova, 2010 | Canada | Cross sectional interview | N = 525 Refugees |
Employment Status | Self-rated changes in mental and physical health status | Linear regression | Of the post-migratory factors studied being employed (either part-time or full time) was associated with greater improvements in mental health (Beta = 0.13, 95%CI (0.01–0.19), p < 0.025). Employment status did not have a significant relationship with physical health. |
Moderate |
| Newman, 2018 | Australia | Cross sectional survey | N = 190 Refugees |
Perceived organizational support (POS): 6 items scale Perceived supervisor support (PSS): 6 item questionnaire |
Psychological wellbeing: Satisfaction with life scale | Ordinary least squares (OLS) regression | The relationship between POS and psychological wellbeing was fully mediated by psychological capital. The relationship between Perceived supervisor support (PSS) and psychological wellbeing was not significant | High |
| Niederkrotenthaler, 2020 | Sweden | Longitudinal study | N = 2017 Refugees |
Duration of time unemployed Duration of Sickness absence Disability pension |
Suicide attempt: ICD-10: X60-84 or Y10-34 Suicide: ICD-10 codes X60-84 or Y10-34 in the Causes of Death Register |
Cox regression models | No significant interaction effects were found for refugee status and employment measures regarding suicide attempts and suicide. | Moderate |
| Niederkrotenthaler, 2020 | Sweden | Longitudinal study | N = 216, 930 Refugees |
Long term unemployment (>180 days) | Mental disorders: ICD-10 codes | Cox proportional-hazard regression models. | Refugees without a mental disorder had an adjusted long-term unemployment HR of 2.68 (95% CI 2.65–2.71), which was above the aHR of refugees (aHR 2.33, 95% CI 2.29–2.38) with mental disorders. Regarding the risk of long-term unemployment due to specific mental disorders, the highest aHRs were seen for anxiety disorders (aHR 2.09), PTSD (aHR 2.03), and other stress-related disorders (aHR 2.25). Refugee status was a strong risk factor of long-term unemployment (HR 2.7), and neither mental disorders in general nor specific mental disorders further added to this risk. |
Moderate |
| Renner, 2021 | Germany | Cross sectional survey | N = 133 Syrian refugees |
Employment status | Anxiety: GAD-7 Depression: PHQ-9 PTSD: PDS-5 Somatization: PHQ-15 |
Multiple linear regression | Employment status was not significantly associated with PTSD, anxiety, depression or somatization. | High |
| Salo, 2015 | USA | Cross sectional survey | N = 203 Vietnamese refugees |
Job satisfaction: 11-item scale | Psychological distress: Indochinese version of HSCL-25 | Structural equation model (SEM) | Job satisfaction was the only direct predictor of psychological distress in this study (b = −0.15, SE = 0.05, 95% CI (−0.25, −0.05), p < 0.01). Job satisfaction fully mediated the relationship between acculturation and psychological distress with a small effect (b = −0.07, p < 0.05). | Moderate |
| Sidorchuk, 2017 | Sweden | Cross sectional survey | N = 3619 Refugees |
Employment status | Psychological distress: GHQ-12 | Logistic regression | Unemployed or temporarily employed refugees had higher odds of distress (OR 2.91, 95% CI 2.20 to 3.85) when compared with permanently/self-employed refugees. Refugee women belonging to the temporarily employed group (OR 2.59 (1.53–4.39)) had higher odds of psychological distress compared with their male counterparts (OR 1.67 (0.88–3.14). | High |
| Sonne, 2021 | Denmark | Randomised Control Trial | N = 321 Refugees |
Full time employment | PTSD: HTQ Anxiety and depression: HSCL-25, HAM-D and HAM-A |
Hierarchical multiple regression analyses | Full-time occupation was positively associated with improvement in HSCL-anxiety and HSCL-depression, but this effect disappeared when the level of functioning (baseline GAF-F) was added. Full-time occupation was not significantly associated with the other treatment outcomes including HTQ, HAM-A, and HAM-D | Moderate |
| Sulaiman-Hill, 2012 | New Zealand Australia |
Mixed methods Cross sectional survey + qualitative interview |
N = 81 Afghan and Kurdish refugees |
Employment status | Subjective Wellbeing: Personal Well Being Index Psychological distress: K10 |
Mann Whitney U test | Refugees who were not working had a higher risk of psychological distress (Median K10 score = 19), than those who were working (Median K10 score = 16) Z = 2.016, p < 0.05. There was no significant difference in subjective wellbeing between the employed and unemployed groups (p = 0.242). | Moderate |
| Teodorescu, 2012 | Norway | Cross sectional survey | N = 61 Refugees |
Employment status | PTSD: Structured Clinical Interview for DSM-IV-TR PTSD Module (SCID) Mental disorders: MINI, Structured Interview for Disorders of Extreme Stress (SIDES) Psychological distress: HSCL-25 PTSD: Life events checklist, impact of event scale-revised |
Kendall's tau-bs Spearman's rho correlations |
Unemployment status was positively associated with PTSD (τb = 0.316, p < 0.01) and PTSD + Disorders of extreme stress not otherwise specified (DESNOS) (τb = 0.276, p < 0.05) and total mental health diagnoses (τb = 0.290 p < 0.05). Unemployment was also positively associated with depression symptom severity HSCL-25 (r = 0.289 p < 0.05). |
Moderate |
| Tonsing, 2020 | USA | Cross Sectional Survey | N = 242 Chin-Burmese Refugees |
Employment related stressors | Psychological distress: K10 | Hierarchical regression analysis | PMLD4 employment stressors were not significantly associated with psychological distress. | High |
| Vinokurov, 2000 | USA | Cross sectional Survey |
N = 206 Former Soviet Union refugees |
Work status - Unemployed - Underemployed - Employed in one's field of professional expertise |
Life satisfaction: Perceived Quality of Life scale | MANOVA | Those employed in a similar job to before arrival reported significantly higher life satisfaction than the underemployed who in turn reported a greater degree of life satisfaction than the unemployed (F = 20.75, p < 0.0005) | Moderate |
| Walther, 2020 | Germany | Cross sectional survey | N = 4325 Asylum seekers and refugees |
Employment status | Psychological distress: PHQ-4 Life satisfaction: Single item measure |
Pooled multiple, hierarchical linear regressions | Currently working is associated with reduced levels of distress (p < 0.01), but only for male respondents. Employment is not associated with life satisfaction | High |
| Walther, 2020 | Germany | Cross sectional survey | N = 2639 Refugees |
Employment: Y/N | Psychological distress: RHS-13 | Poisson regression model | Male refugees who reported psychological distress had a lower likelihood of employment (risk ratio 0.67 (0.52–0.86)) and reduced participation in integration courses (RR 0.90 (0.81–0.99)). | High |
| Warfa, 2012 | UK USA |
Cross sectional survey | N = 189 Somali refugees London group = 143 Minneapolis = 43 |
Employment: Y/N Type of work: Skilled/Not skilled |
Mental disorders: M.I.N.I | Logistic Regression | Employment status was found to have one of the biggest impacts on reducing the odds of major depression and aggregated psychological disorders (OR = 2.419, 0.70–8.34, 0.162; OR = 2.372, 0.51–10.95, 0.269) respectively. | High |
| Wright, 2016 | USA | Longitudinal study | N = 286 Iraqi refugees |
Employment: Y/N | PSTD: PCL—Civilian version Depression: HADS |
Hierarchical Logistic regression | None of the mental health factors alone (baseline PTSD, baseline depression, pre-displacement trauma, post displacement trauma) was significant in predicting unemployment two years after arrival to the US. However, the interaction of the pre-and post-displacement trauma was predictive of employment status (β = 0.05, Wald = 4.19, OR = 1.05, p < 0.05). | High |
| Yalim, 2020 | USA Turkey |
Cross sectional survey | N = 185 Syrians refugees USA sample N = 82 Turkey sample N = 103 |
Employment status | Anxiety and Depression: HSCL-25 | Hierarchical regression model | Employment status was not associated with HSCL-25 total score in the Turkey or USA sample. | High |
Table 3.
Description of studies on employment and general health/wellbeing.
| Authors | Country | Study design | Study population | Measure of employment | Measure of health | Statistical Analysis | Main findings of employment and health | Quality |
|---|---|---|---|---|---|---|---|---|
| Ambrosetti, 2021 | Germany | Longitudinal study | N = 3957 refugees and asylum seekers | Employment status | Self-rated health: 5 point scale Life satisfaction: 11 point scale |
Ordinary least squares regression | Transition to permanent and temporary work contracts was significantly associated with increases in self-rated health by 0.112(p < 0.01) and 0.081 (p < 0.05) points respectively. Transitions to permanent work from non-permanent employment or inactivity result in higher life satisfaction levels by 0.159 points. |
High |
| Birman, 2014 | USA | Cross sectional survey | N = 391 Refugees from the Former Soviet Union |
Occupational adjustment measures 1) Occupational prestige: 1989 Socioeconomic Index of Occupations 2) Job satisfaction: 11 item measure. |
Life satisfaction: Russian version of the Perceived Quality of Life scale Anxiety & depression: HSCL-25 |
Structural Equation Modelling | Occupational adjustment (job satisfaction and occupational prestige) had a direct effect on life satisfaction (0.31, p < 0.05), and an indirect effect on HSCL (−0.10, p < 0.001) through life satisfaction, indicating mediation. Occupational adjustment also mediated the relationship between acculturation and life satisfaction (0.15, p < 0.001). | High |
| Colic-Peisker, 2009 | Australia | Cross sectional survey and interview | N = 150 Refugees |
Employment status Job satisfaction Discrimination in the job market |
Life satisfaction: 2 items (4 point scale) ‘general life satisfaction’ and ‘life back to normal’. Refugee life satisfaction score’ (RLS score): Combined the two overall life satisfaction variable |
T-test Correlation and regression analyses |
The RLS score of refugees who had ‘experienced discrimination in the job market’ was significantly lower, compared to those who had not (p = 0.006). Job satisfaction was one of the strongest predictors (p < 0.01) of life satisfaction, especially for Bosnian refugees. Employment status showed a weak correlation with overall satisfaction (p = 0.05). |
Moderate |
| Jamil, 2012 | USA | Cross sectional survey | N = 148 Iraqi refugees |
Employment status Self-rated job quality: Poor/Good |
Self-rated health: SF36 item | Logistic regression | Job quality but not employment status was significantly associated with self-rated health. Those who rated their jobs favorably were more likely to report better health, (OR = 38.67, 95% CI [4.44–342.35]). | High |
| Khawaj 2019 | Australia | Cross sectional survey and interviews | N = 197 Refugees |
Employment status | Life satisfaction: Study specific scale. | ANOVA | Participants who were employed (M = 11.32, SD = 2.14, p = 0.004) or unemployed (M = 11.32, SD = 2.66, p = 0.01) had significantly higher scores on life satisfaction than participants who were unemployed and undertaking vocational training (M = 9.8, SD = 2.67) | Low |
| Khoo, 2010 | Australia | Longitudinal study | 1ST Cohort N = 728 2nd cohort: N = 479 Refugees and asylum seekers |
Employment status | Long term health condition: Self-reported chronic health conditions Self-rated health: 5 point scale Mental Health Status: GHQ-12 |
Multivariate logistic regression | Male refugees who reported having very good health (OR = 0.969, p < 0.05), no long-term health conditions (OR = 0.474, p < 0.05) and lower mental health scores (OR = −0.029, p < 0.05) were significantly more likely to be in the workforce than those whose health was worse, had a health condition or higher mental health scores. The relationship was not significant for the female cohort. | Moderate |
| Koch-Weser, 2006 | USA | Cross sectional survey | N = 381 Cambodian refugees |
Employment status | Self-rated health: SF36 item | Bivariate analysis Multivariate logistic regression |
Compared to respondents who were working, people who identified themselves as homemakers or retired were less likely to report better health (OR = 0.41, 95%CI 0.21–0.80) as were those who reported they were unable to work (OR = 0.09, 95% CI 0.05–0.17). The multivariate analysis showed that the likelihood of reporting better health was the lowest for adults unable to work due to disability (OR = 0.14, 95% CI 0.07,0.29) |
High |
| Mantanov, 2013 | Germany, Italy UK |
Cross sectional interview | N = 627 Refugees from Former Yugoslavia |
Employment status | Life satisfaction: MANSA | Linear regression | Unemployment was associated with significantly lower subjective quality of life satisfaction (MANSA score) in both univariable regression (B = −0.381, 95% CI (−0.503 to 0.259),p < 0.001) and multivariable regression (B = −0.258, 95% CI (−0.379 to −0.138), p < 0.001) | High |
| Salman, 2020 | USA | Cross sectional Survey | N = 107 Refugees |
Employment status | Self-rated health status: 3 point item | Cross tabulation table | Full-time employed participants reported excellent health more frequently than part-time employees (34 vs. 28). In addition, the number of those who reported poor health was higher than those who were employed (11 vs.7). | Moderate |
| Schuring, 2009 | Netherlands | Cross sectional survey | N = 100 Refugees |
Employment status | Self-rated health: 5 point scale Health: SF-36 |
Logistic regression | Poor self-rated health was more common among unemployed refugees (OR = 1.6) than refugees in paid employment. Those unemployed or receiving a disability pension also had significantly lower scores on all dimensions of physical and mental health compared with those employed. | High |
| Shaw, 2015 | USA | Longitudinal study | N = 434 Refugee households. |
Employment status | Self-rated wellbeing: 5-point scale | Multivariate generalized estimating equations models | Households with at least one person employed during the 24 months scored significantly higher in total wellbeing (B = 1.19, 95% CI (0.59–1.79), p < 0.001), than households without someone employed. | Moderate |
Table 4.
Description of studies on employment and physical health.
| Authors Date |
Country | Study design | Study population | Measure of employment | Measure of health | Statistical Analysis | Main findings of employment and health | Quality |
|---|---|---|---|---|---|---|---|---|
| Azaroff, 2004 | USA | Cross sectional Survey | N = 160 Refugees (Cambodia, Laos) |
Work hazards: Open-ended questions Employment conditions: Working hours and employment type |
Health problems Work-related symptoms |
Descriptive statistics Prevalence Ratio |
Prevalent workplace hazards reported included exposures to chemicals; inadequate ventilation; prolonged sitting or standing and awkward postures; unguarded machinery; long work hours. 26% of the respondents reported work-related backache and 9% reported work-related skin rashes. Working over 40 hours yielded a prevalence ratio of 1.4 (95% CI 1.1, 1.7) for reporting a work-related health symptom, and working a late shift had a prevalence ratio of 1.5 (95% CI 1.0, 2,3) for reporting a work-related sign. |
Low |
| Jen, 2018 | USA | Longitudinal study | Iraqi refugees N = 298 at baseline N = 290 refugees Y1 follow up N = 282 at Y2 follow up |
Employment status | Body Mass Index (BMI) Non-communicable Disease (NCD): composite score of self-reported NCD |
Linear regression | Unemployment at year 2 was associated with a higher number of non-communicable diseases (B = 0.35, SE = 0.13, p < 0.0001) and increased NCDs from baseline (B = 0.23, SE = 0.13, p < 0.01). Unemployment was not significantly associated with BMI or changes in BMI over the 2 years (p > 0.05) | Moderate |
| Kraeh, 2016 | South Korea | Cross sectional survey | N = 394 North Korean Refugees |
Employment status | Physical health: Resting heart rate Psychological adjustment: Korean version of CES-D |
Linear regression | Employment status had a significant effect on psychological adjustment (B = 0.12, SE = 0.06, p = 0.028) and resting heart rate (B = −4.63, SE = 1.66, p = 0.006). Further analyses, found a significant indirect effect of employment status on resting heart rate via socio-cultural adjustment and psychological adjustment. | Moderate |
| Ruiz, 2018 | UK | Cross sectional Survey |
N = 2360 Refugees N = 279,634 UK born |
Employment status Hours worked (weekly) |
Self-reported health problem | Linear regression models | 69% of refugees with health problems reported that this limits the kind or amount of work they can engage in compared with half of the natives and other migrants with health problems. Refugees are 14% more likely than non-refugees to report a health problem that limits the type of work they can do and 17% more likely to report a health problem that limits the amount of work they can engage in. | High |
| Sundquist, 2003 | Sweden | Cross sectional survey | N = 333 Refugees |
Job demand: High/Low Decision latitude: High/Low Job strain: Yes/No Support: Low/Heigh |
Self-reported long-term illness. | Logistic regression | Refugees experiencing both high job demands and low decision latitude had an increased risk (OR = 1.74; 95% CI: 1.42–2.13) of long-term illness. There was no interaction between migration status and high job strain. However, refugees with low social support at work had nearly twice (OR = 1.91, 95%CI (1.44–2.54)) as high a risk of long-term illness as Swedes with high-level work-related social support | Moderate |
| Van Hanegem, 2011 | Netherlands | Longitudinal study | N = 40 Asylum seekers |
Employment status | Severe acute maternal morbidity (SAMM) | Risk Ratio | Unemployment was one of the specific risk indicators for asylum seekers to experience SAMM (RR = 3.1, 95% CI 1.5–6.6) | Moderate |
| Zhang, 2021 | USA | Cross-sectional survey | N = 218 Burmese and Bhutanese refugees |
Employed as essential worker: Y/N | COVID 19 infection | Logistic regression | Being an essential worker was associated with COVID 19 infection (OR = 5.25; 95% CI, 1.21–22.78). The prevalence of COVID-19 was 13.6% among essential workers and 2.3% among nonessential workers. |
Moderate |
Abbreviations: Composite International Diagnostic Interview (CIDI), Center for Epidemiological Studies-Depression (CES-D), EuroQol-visual analogue scales (EQ-VAS), General Anxiety Disorder Assessment (GAD-7), General Health Questionnaire (GHQ), Hospital Anxiety and Depression Scale (HADS), Hopkins Symptom Checklist-25 (HSCL-25), Hamilton Anxiety Rating Scale (HAM-A), Hamilton Depression Rating Scale (HAM-D), The Manchester Short Assessment of Quality of Life (MANSA), Mini International Neuropsychiatric Interview (MINI), PTSD Checklist for DSM-5 (PCL-5), the Primary Care PTSD Screen for DSM-5 (PC-PTSD-5), Posttraumatic Symptom Scale (PTSS) Perceived Stress Scale (PSS), Patient Health Questionnaire (PHQ), Posttraumatic Diagnostic Scale (PDS), Refugee Health Screener (RHS), World Health Organization Quality of Life Brief Version (WHOQOL-BREF), World Health Organization Disability Assessment Schedule (WHODAS).
The aims of the papers were wide-ranging, 21 papers explicitly aimed to examine the relationship between employment and health for refugees and asylum seekers (Azaroff, Levenstein, & Wegman, 2004; Baranik, Hurst, & Eby, 2018; Beiser & Hou, 2001; Blight et al., 2006; Bridekirk et al., 2021; Campbell, Mann, Moffatt, Dave, & Pearce, 2018; de Vroome & van Tubergen, 2010; Di Thiene et al., 2021; Drydakis, 2022; Grochtdreis, König, Riedel-Heller, & Dams, 2020; Hocking, Kennedy, & Sundram, 2015; Jamil et al., 2012; Neitzel, Krenz, & de Castro, 2014; Helgesson, Rahman, Saboonchi, & Ellenor Mittendorfer, 2021; Niederkrotenthaler, Mittendorfer-Rutz, Saboonchi, & Helgesson, 2020; Ruiz & Vargas-Silva, 2018; Schuring, Burdorf, Kunst, Voorham, & Mackenbach, 2009; Sidorchuk et al., 2017; Sundquist et al., 2003; Warfa et al., 2012; Wright et al., 2016). The remainder of the papers in this review considered employment as a control variable or as part of other post-migratory factors within a study which explored resettlement more broadly.
3.1. Methodological quality assessment
Of the 72 included papers, 32 (44%) were rated as high quality, while 35 (49%) were rated as moderate quality. A total of five papers (7%) were rated to be low quality, mainly due to poor description of the inclusion criteria, a lack of valid and reliable measurement of the outcome, and statistical analysis that did not adjust for confounding factors. See Appendix 2.
3.2. Post-traumatic stress disorder (PTSD)
Seventeen papers reported the relationship between employment and post-traumatic stress disorder (PTSD) (Ahmad, Othman, & Lou, 2020; Aragona et al., 2019; Barbieri et al., 2021; Bogic et al., 2012; Carlsson et al., 2006; Cooper et al., 2019; Eisen, Howe, & Cogar, 2021; Hermansson et al., 2002, 2003; Hocking et al., 2015; Kashyap, Page, & Joscelyne, 2019; Marshall et al., 2005; Niederkrotenthaler, Mittendorfer-Rutz, Saboonchi, et al., 2020; Renner et al., 2021; Sonne et al., 2021; Teodorescu, Heir, Hauff, Wentzel-Larsen, & Lien, 2012; Wright et al., 2016). The most frequently used PTSD measure was the Harvard Trauma Questionnaire (HTQ), used by seven of the 16 papers (Ahmad et al., 2020; Aragona et al., 2019; Carlsson et al., 2006; Eisen et al., 2021; Hocking et al., 2015; Kashyap et al., 2019; Sonne et al., 2021). Other measures included the Post Traumatic Symptom Scale (PTSS-10) (Hermansson et al., 2002, 2003), PTSD Checklist (Barbieri et al., 2021; Wright et al., 2016) and Posttraumatic Diagnostic Scale (PDS-5) (Renner et al., 2021). Diagnosis of PTSD was also used in two papers through the Internal Neuropsychiatric Interview (MINI) (Bogic et al., 2012; Teodorescu, Heir, et al., 2012) and in one paper through the Composite International Diagnostic Interview version 2.1 (Marshall et al., 2005).
Seven of the 17 papers found a significant association between employment status and PTSD (Ahmad et al., 2020; Aragona et al., 2019; Carlsson et al., 2006; Hermansson et al., 2002, 2003; Hocking et al., 2015; Teodorescu, Heir, et al., 2012). Three of these papers found that being employed was associated with lower PTSD levels (Ahmad et al., 2020; Carlsson et al., 2006; Hermansson et al., 2003). Ahmad et al. conducted a cross-sectional survey of 49 Afghan refugees in Canada and found the prevalence of PTSD was zero in those employed and 59% in those unemployed (Ahmad et al., 2020). A longitudinal study of 139 refugees in Denmark who had experienced torture showed that at 10-year follow-up employment/self-employment was significantly associated with lower HTQ trauma score (Carlsson et al., 2006). A Swedish longitudinal study of the mental health of refugees with a war injury showed that employment was associated with a lower PTSS-10 score only for the non-tortured group but not the tortured group (Hermansson et al., 2003). Four papers, three of which were cross-sectional showed that unemployment was positively associated with higher PTSD levels (Aragona et al., 2019; Hermansson et al., 2002; Hocking et al., 2015; Teodorescu, Heir, et al., 2012).
Employment status was not significantly associated with PTSD in eight studies, six longitudinal and two cross-sectional. (Barbieri et al., 2021; Bogic et al., 2012; Cooper et al., 2019; Eisen et al., 2021; Kashyap et al., 2019; Marshall et al., 2005; Renner et al., 2021; Sonne et al., 2021). Two longitudinal studies in the USA found that employment status was not independently associated with PTSD (Eisen et al., 2021; Kashyap et al., 2019). Kashyap et al. found that employment status only moderated PTSD score when it was examined with stable housing (Kashyap et al., 2019). Another study of 78 torture surviving asylum seekers found that PTSD symptoms improved over time, independent of employment status changes (Eisen et al., 2021). Five papers found that unemployment was not associated with higher levels of PTSD (Barbieri et al., 2021; Bogic et al., 2012; Cooper et al., 2019; Marshall et al., 2005; Renner et al., 2021). A randomised control trial that examined predictors of treatment outcomes for 321 trauma-affected refugees in Denmark found that full-time employment had no significant effect on treatment outcomes (Sonne et al., 2021).
Two studies examined trauma as a predictor of unemployment (Niederkrotenthaler, Mittendorfer-Rutz, Saboonchi, et al., 2020; Wright et al., 2016). Niederkrotenhaler et al. found that refugee status was the strongest risk factor of long-term unemployment and PTSD did not add further to this risk (Niederkrotenthaler, Mittendorfer-Rutz, Saboonchi, et al., 2020). Wright et al. found that none of the trauma factors alone (baseline PTSD, pre-displacement trauma, post displacement trauma) predicted unemployment two years after arrival to the USA, but those who experienced both high pre-displacement trauma and high post-displacement trauma had the highest predicted probability of unemployment (91%) (Wright et al., 2016).
3.3. Depression and anxiety
Twenty-one papers examined the relationship between employment and depression (Ahmad et al., 2020; Baranik et al., 2018; Beiser & Hou, 2001; Beiser & Hou, 2006; Carlsson et al., 2006; de Vroome & van Tubergen, 2010; Drydakis, 2022; Eisen et al., 2021; Hermansson et al., 2002; Hermansson et al., 2003; Hocking et al., 2015; Jeon et al., 2009; Kashyap et al., 2019; Kim, 2016; Kim et al., 2011; Marshall et al., 2005; Renner & Salem, 2009; Sonne et al., 2021; Teodorescu, Heir, et al., 2012; Warfa et al., 2012; Wright et al., 2016). Depression scales included the Hopkins Symptom Checklist (Carlsson et al., 2006; Eisen et al., 2021; Hermansson et al., 2002, 2003; Hocking et al., 2015; Sonne et al., 2021; Teodorescu, Heir, et al., 2012), Patient Health Questionnaire (PHQ-9) (Ahmad et al., 2020; Kashyap et al., 2019; Renner et al., 2021) and the Centre for Epidemiological Studies Depression (CES-D) scale (Baranik et al., 2018; Drydakis, 2022; Jeon et al., 2009; Kim et al., 2011).
Ten papers, four longitudinal and six cross-sectional, found that employment status was significantly associated with both depression symptom severity and prevalence (Beiser and Hou, 2001, Beiser & Hou, 2006; Carlsson et al., 2006; Hermansson et al., 2002; Hocking et al., 2015; Jeon et al., 2009; Marshall et al., 2005; Sonne et al., 2021; Teodorescu, Siqveland et al., 2012; Warfa et al., 2012). Unemployment was consistently shown to be significantly associated with higher levels of depression. For example, two cross-sectional studies conducted in Australia and South Korea found that unemployed people were approximately twice as likely to report depressive symptoms than those with employment (Hocking et al., 2015; Jeon et al., 2009). In their study of Southeast Asian refugees in Canada, Beiser et al. found that the unemployed refugees who identified more deeply with their ethnicity reported higher depression levels than their counterparts who had a weaker sense of ethnic identity (Beiser & Hou, 2006).
Two studies found that poor working conditions such as discrimination, lack of written contract of employment, hourly wage lower than national minimal wage, and harassment in the workplace increased levels of depression in refugee workers (Baranik et al., 2018; Drydakis, 2022).
Seven papers found no significant association between depression and employment status (Ahmad et al., 2020; Eisen et al., 2021; Hermansson et al., 2002, 2003; Kashyap et al., 2019; Kim et al., 2011; Renner et al., 2021). Three of the seven papers were longitudinal studies that specifically examined survivors of torture (Eisen et al., 2021; Hermansson et al., 2003; Kashyap et al., 2019). For example, Eisen et al. showed that depressive symptom levels improved over time for asylum seekers who survived torture, independent of changes in measured post-migratory factors such as employment and housing (Eisen et al., 2021).
Two papers examined the effect of depression on refugee employment status with conflicting findings (de Vroome & van Tubergen, 2010; Wright et al., 2016). A cross-sectional study in the Netherlands found that depression was negatively associated with the odds of employment and occupational status (de Vroome & van Tubergen, 2010). However, a longitudinal study that examined unemployment in Iraqi refugees living in the USA found that depression alone was not significant in predicting unemployment two years after resettlement (Wright et al., 2016).
Eleven papers investigated the effect of employment on anxiety (Baranik et al., 2018; Birman, Simon, Chan, & Tran, 2014; Bogic et al., 2012; Carlsson et al., 2006; Hermansson et al., 2003; Hocking et al., 2015; Kim, 2016; Kim et al., 2011; Laban et al., 2005; Sonne et al., 2021; Yalim, 2020). Notably, a significant effect was found in the longitudinal studies (Carlsson et al., 2006; Hermansson et al., 2003; Sonne et al., 2021), whereas the findings from the cross-sectional studies were mixed (Baranik et al., 2018; Birman et al., 2014; Bogic et al., 2012; Hocking et al., 2015; Kim, 2016; Kim et al., 2011; Laban et al., 2005; Yalim, 2020). Anxiety was most frequently reported as part of the Hopkins Symptoms Checklist-25 (Birman et al., 2014; Carlsson et al., 2006; Hermansson et al., 2003; Hocking et al., 2015; Sonne et al., 2021; Yalim, 2020) and short structured diagnostic interviews such as the Mini-International Neuropsychiatric Interview (MINI) (Bogic et al., 2012), World Mental Health Composite International Diagnostic Interview (Kim, 2016), and Composite International Diagnostic Interview (CIDI) (Laban et al., 2005). Being in employment was significantly associated with lower anxiety levels in all four papers reporting the HSCL-25 anxiety score (Carlsson et al., 2006; Hermansson et al., 2003; Hocking et al., 2015; Sonne et al., 2021). One study used a three-item measure to assess anxiety (Baranik et al., 2018). This study showed that refugees experiencing discrimination stressors in employment reported significantly higher levels of anxiety than those who did not report discrimination, including after controlling for past trauma events (Baranik et al., 2018).
Two papers using the HSCL-25 reported it as a total score combining both anxiety and depression (Birman et al., 2014; Yalim, 2020). One cross-sectional study found that employment status was not associated with the HSCL-25 total score (Yalim, 2020). Another showed that occupational adjustment which encompasses job satisfaction and occupational prestige had an indirect effect on HSCL through life satisfaction (Birman et al., 2014). Four cross-sectional papers examined anxiety as part of a structured diagnostic interview (Bogic et al., 2012; Kim, 2016; Kim et al., 2011; Laban et al., 2005). None of these found a significant relationship between employment status and diagnosis of anxiety disorder.
3.4. General mental illness and psychological distress
Seven papers, six cross-sectional and one longitudinal, explored the effect of employment status on having a mental disorder but did not differentiate between diagnoses (Bhui et al., 2006; Bogic et al., 2012; Cooper et al., 2019; Kim et al., 2011; Laban et al., 2005; Teodorescu, Heir, et al., 2012; Warfa et al., 2012). Mental disorders were mainly assessed using structured interviews such as the Mini Neuropsychiatric Interview (MINI) (Bhui et al., 2006; Bogic et al., 2012; Teodorescu, Heir, et al., 2012; Warfa et al., 2012) and the Composite International Diagnostic Interview (CIDI)(Laban et al., 2005). The cross-sectional studies consistently found a significant association between employment status and mental disorders (Bhui et al., 2006; Bogic et al., 2012; Kim et al., 2011; Laban et al., 2005; Teodorescu, Heir, et al., 2012; Warfa et al., 2012). Unemployment was shown to be positively associated with being diagnosed with a mental disorder (Bogic et al., 2012; Kim et al., 2011; Laban et al., 2005; Teodorescu, Heir, et al., 2012). One study explored ‘work below skill level’ and found that it significantly increased the odds of lifetime prevalence of having one or more psychiatric disorders in Iraqi asylum seekers in the Netherlands (Laban et al., 2005). Two studies found that for Somali refugees living in the UK and USA, employment had one of the biggest impacts on reducing the odds of psychological disorders (Bhui et al., 2006; Warfa et al., 2012). In contrast, the only longitudinal study which included 2000 refugees in Australia found that unemployment was not a significant predictor of mental illness (Cooper et al., 2019).
Nine papers reported on outcomes relating to psychological distress more generally (Alemi et al., 2015; Bridekirk et al., 2021; Drescher et al., 2021; Salo & Birman, 2015; Sidorchuk et al., 2017; Sulaiman-Hill & Thompson, 2012; Tonsing & Vungkhanching, 2020; Walther, Fuchs, Schupp, & Von Scheve, 2020, Walther, Kroger, et al., 2020). A variety of measures of psychological distress were used; the Kessler Psychological Distress Scale was the only measure used by more than one study (Drescher et al., 2021; Sulaiman-Hill & Thompson, 2012; Tonsing & Vungkhanching, 2020). Several of the papers reported measures developed for specific population groups including the Afghan Symptom Checklist (Alemi et al., 2015), the Indochinese version of the Hopkins Symptom Checklist (Salo & Birman, 2015), and the Refugee Health Screener (Walther, Kroger, et al., 2020).
Seven of the nine papers, six cross-sectional and one longitudinal, reported an association between psychological distress and employment. (Bridekirk et al., 2021; Drescher et al., 2021; Salo & Birman, 2015; Sidorchuk et al., 2017; Sulaiman-Hill & Thompson, 2012; Walther, Fuchs, et al., 2020, Walther, Kroger, et al., 2020). Unemployment was associated with a higher risk of psychological distress (Sidorchuk et al., 2017; Sulaiman-Hill & Thompson, 2012). For example, a population-based study in Sweden found that unemployed refugees were nearly three times more likely to experience psychological distress when compared with those who were in employment (Sidorchuk et al., 2017). Gender differences were noted in this study; refugee women who were temporarily employed and permanently/self-employed had higher odds of psychological distress compared to refugee men (Sidorchuk et al., 2017). Evidence from a large-scale German Survey showed that currently working was significantly associated with reduced levels of distress, however, only for men (Walther, Fuchs, et al., 2020).
Other employment factors found to influence psychological distress include job satisfaction and the education level of employed individuals. Job satisfaction was a direct predictor of psychological distress in Vietnamese refugees living in the USA (Salo & Birman, 2015). A longitudinal study of Syrian refugees in Canada found satisfaction with current wage, job appropriateness, job satisfaction, and perceived control to be significantly correlated with psychological distress. Employed refugees with high education reported higher levels of stress on the PSS-10 than those with low education (Bridekirk et al., 2021).
No significant relationship between employment and psychological distress was found in two out of the nine papers (Alemi et al., 2015; Tonsing & Vungkhanching, 2020). Both were cross-sectional studies conducted in the USA. One found that employment status was not a significant predictor of psychological distress in Afghan refugees (Alemi et al., 2015). In the study of 242 Chin-Burmese refugees, employment-related stressors such as working conditions and lack of working permits were not significantly associated with psychological distress (Tonsing & Vungkhanching, 2020).
3.5. General mental health
Seven papers examined general mental health status using scales such as the revised Gotebrog quality of life instrument (Blight et al., 2006), RAND-36 health survey (Bridekirk et al., 2021), Short Form-12 survey (Grochtdreis et al., 2020), 12-item General Health Questionnaire (Khoo, 2010), Primary Care PTSD screen (Cetrez et al., 2021) and single-item self-rated mental health (Kim, 2016; Maximova & Krahn, 2010). Only one of the seven papers, a cross-sectional study which examined post-resettlement factors and mental health outcomes among Latino and Asian refugees in the USA, found no significant association between employment status and self-reported mental health (Kim, 2016). The other studies, two longitudinal and four cross-sectional, consistently showed that refugees who were employed had significantly better mental health than their unemployed counterparts (Blight et al., 2006; Bridekirk et al., 2021; Grochtdreis et al., 2020; Khoo, 2010; Maximova & Krahn, 2010). In a Swedish study of Iraqi refugees, unemployment was one of the most commonly given explanations of mental ill-health (Cetrez et al., 2021). Blight et al. found gender differences in the relationship between employment and mental health for Bosnia-Herzegovina refugees in Sweden. For men, unemployment was associated with high levels of poor mental health whereas for women it was working for longer periods during 1993–1999 (Blight et al., 2006). A longitudinal study of Syrian refugees in Canada highlighted the impact of employment quality on mental health status. The findings showed that among refugees who were employed, mental health was higher among those making enough money and satisfied with their work, and those who reported more perceived control and less stress. However, no significant association between job appropriateness and mental health was found (Bridekirk et al., 2021).
Five papers, four longitudinal and one cross-sectional study examined the impact of general mental health on employment (Di Thiene et al., 2021; Helgesson et al., 2021; Hunkler & Khourshed, 2020; Khoo, 2010; Niederkrotenthaler, Mittendorfer-Rutz, Saboonchi, et al., 2020). The cross-sectional study of 275 Syrian refugees in Germany found that an individual's mental state had no significant effect on their probability of employment (Hunkler & Khourshed, 2020). Two Swedish studies found that refugees with mental disorders had a higher risk for long-term unemployment or disability pension compared with Swedish-born individuals with similar disorders (Di Thiene et al., 2021; Helgesson et al., 2021). In an Australian study, mental health status was shown to negatively affect the employment status of male but not female refugees (Khoo, 2010). A Swedish register study of over 210, 000 refugees found that refugee status was the strongest risk factor of long-term unemployment and neither mental disorder in general nor specific mental disorders added further to this risk (Niederkrotenthaler, Mittendorfer-Rutz, Saboonchi, et al., 2020).
Six studies, two cross-sectional and four longitudinal, examined psychological wellbeing (Campbell et al., 2018; Hermansson et al., 2002, 2003; Newman, Nielsen, Smyth, & Hirst, 2018; Shaw & Poulin, 2015; Sulaiman-Hill & Thompson, 2012). Well-being was largely measured through a single item self-rating scale unique to each study (Campbell et al., 2018; Hermansson et al., 2002, 2003; Shaw & Poulin, 2015). In both cross-sectional studies, no significant relationship was found between psychological wellbeing and the employment variable of interest. An Australian study examined the effect of workplace support from the organization and supervisor on psychological wellbeing and found no significant association (Newman, Nielsen, et al., 2018). Another cross-sectional study conducted in Australia and New Zealand found no significant differences in the subjective wellbeing and the employed and unemployed refugee groups (Sulaiman-Hill & Thompson, 2012). The longitudinal studies consistently found a significant relationship between employment status and psychological wellbeing (Campbell et al., 2018; Hermansson et al., 2002, 2003; Shaw & Poulin, 2015). A study conducted in the USA of 434 refugee households found that households where at least one person was employed, reported higher levels of wellbeing and lower health needs compared to households without someone employed (Shaw & Poulin, 2015). Refugees who were unemployed or underemployed with a job lower than their skills and qualifications in the UK had significantly higher odds of poorer emotional wellbeing (Campbell et al., 2018). Hermansson et al. conducted two longitudinal studies in Sweden on the mental health of 44 refugees who were injured in war (Hermansson et al., 2002, 2003). The initial study found that unemployment was not significantly associated with psychological wellbeing (Hermansson et al., 2002). In a subsequent paper where exposure to torture was examined, being employed had a positive correlation with well-being only for refugees who had not experienced torture (Hermansson et al., 2003).
3.6. Other mental health outcomes
Two studies examined the relationship between employment and suicide (Ao et al., 2016; Niederkrotenthaler, Mittendorfer-Rutz, Mehlum, Qin, & Björkenstam, 2020). A study of Bhutanese refugees in the USA showed that the inability to find work was one of the main post-migratory difficulties associated with past suicidal ideation (Ao et al., 2016). Niederkrotenhaler et al. found no significant interaction between different markers of labour market marginalization and suicide attempt or suicide for refugees resettled in Sweden (Niederkrotenthaler, Mittendorfer-Rutz, et al., 2020). An Australian study found that refugees with prolonged grief disorder (PGD) were more likely to be unemployed than those with no PGD (Bryant et al., 2019).
3.7. Life satisfaction
Seven studies explored life satisfaction as an outcome (Ambrosetti et al., 2021; Birman et al., 2014; Colic-Peisker, 2009; Khawaj & Hebbani, 2019; Matanov et al., 2013; Vinokurov, Birman, & Trickett, 2000; Walther, Fuchs, et al., 2020). The studies used a variety of measures ranging from validated tools such as the Perceived Quality of Life Scale (PQOL) (Birman et al., 2014; Vinokurov et al., 2000), the Manchester Short Assessment of Quality of life (MANSA) to study specific scales (Ambrosetti et al., 2021; Colic-Peisker, 2009; Khawaj & Hebbani, 2019) and single-item questionnaires (Walther, Fuchs, et al., 2020). Six out of the seven studies found a significant association between employment and life satisfaction (Ambrosetti et al., 2021; Birman et al., 2014; Colic-Peisker, 2009; Khawaj & Hebbani, 2019; Matanov et al., 2013; Vinokurov et al., 2000). Refugees who were employed, particularly those who had a permanent working contract (Ambrosetti et al., 2021) had significantly higher scores of life satisfaction than those who were unemployed or in vocational training (Ambrosetti et al., 2021; Colic-Peisker, 2009; Khawaj & Hebbani, 2019; Matanov et al., 2013). Job satisfaction and occupational prestige are also strong predictors of life satisfaction (Birman et al., 2014; Colic-Peisker, 2009). Data collected from 206 Jewish refugees in the USA found that those who were employed in a similar field to their original profession reported significantly higher life satisfaction than the underemployed, who in turn reported a greater degree of life satisfaction than the unemployed (Vinokurov et al., 2000). Colic-Peisker et al., found that experiences of discrimination in the job market negatively affected life satisfaction (Colic-Peisker, 2009).
3.8. General and physical health
Eight papers examined the relationship between employment and general health (Ambrosetti et al., 2021; de Vroome & van Tubergen, 2010; Hunkler & Khourshed, 2020; Jamil et al., 2012; Khoo, 2010; Koch-Weser, Liang, & Grigg-Saito, 2006; Salman, Turek, & Donovan, 2021; Schuring et al., 2009). All but one paper measured general health using the 5 point scale Self-Rated Health question (Salman et al., 2021). Four studies, three cross-sectional and one longitudinal reported a significant association between employment status and general health. (Ambrosetti et al., 2021; Koch-Weser et al., 2006; Salman et al., 2021; Schuring et al., 2009). People who were in full-time employment or had a permanent working contract reported better health than those in nonpermanent or part-time employment (Ambrosetti et al., 2021; Salman et al., 2021). Refugees who were unemployed or unable to work due to disability and other reasons had significantly increased odds of poor health (Koch-Weser et al., 2006; Schuring et al., 2009). One study found that job satisfaction and not employment status were significantly associated with self-rated health. Those who rated their jobs favorably were more likely to report better health (Jamil et al., 2012).
The effect of health on refugee employment was explored in three papers (de Vroome & van Tubergen, 2010; Hunkler & Khourshed, 2020; Khoo, 2010). All three studies showed that overall health significantly increased the odds of employment (de Vroome & van Tubergen, 2010; Hunkler & Khourshed, 2020; Khoo, 2010). A study of the employment experience of refugees in the Netherlands showed that general poor health not only reduced the odds of employment but was also associated with occupational status (de Vroome & van Tubergen, 2010).
Twelve studies included physical health as a variable (Sundquist et al., 2003; Ruiz & Vargas-Silva, 2018; Grochtdreis et al., 2020; Azaroff et al., 2004; Drydakis, 2022; Khoo, 2010; Maximova & Krahn, 2010; Helgesson et al., 2021; Zhang et al., 2021; Jen, Jamil, Zhou, Breejen, & Arnetz, 2018; Kraeh, Froese, & Kim, 2016; Van Hanegem et al., 2011). Four explored the negative impacts of adverse working conditions on physical health (Azaroff et al., 2004; Drydakis, 2022; Sundquist et al., 2003; Zhang et al., 2021). A longitudinal study in Greece found that refugee workers with no written employment contract, receiving lower than national minimum hourly wages, and experiencing insults and/or threats in their present job experienced worse physical health (Drydakis, 2022) A Swedish study reported that refugees who experienced job strain had nearly twice as high a risk of long term illness than the Swedish born population (Sundquist et al., 2003). Azaroff et al.’s, survey of 160 Cambodian and Laotian refugees in the USA found they were mainly employed in manufacturing industries and were commonly exposed to hazards such as poor manual handling and chemical irritants. Self-reports of work-related health problems were associated with working long hours and night shifts (Azaroff et al., 2004). More recently, a study of Bhutanese and Burmese refugees in the USA highlighted work in essential industries as a risk factor for COVID-19 infection (Zhang et al., 2021).
Eight papers reported on the association between employment status and physical health through measures such as SF12 (Grochtdreis et al., 2020), resting heart rate (Kraeh et al., 2016), self-reported illness (Khoo, 2010; Maximova & Krahn, 2010; Ruiz & Vargas-Silva, 2018), and physician-diagnosed health conditions (Helgesson et al., 2021; Jen et al., 2018; Van Hanegem et al., 2011). Four of the five studies which examined the effect of employment on physical health showed that refugees who were employed had better physical health than their unemployed counterparts (Grochtdreis et al., 2020; Jen et al., 2018; Kraeh et al., 2016; Van Hanegem et al., 2011). Unemployment was associated with a higher number of non-communicable diseases (Jen et al., 2018) and a specific risk indicator for severe acute maternal morbidity (SAMM) in asylum seeker pregnant women (Van Hanegem et al., 2011). Only one study, which examined the health status of refugees resettled in Canada, reported that employment status did not have a significant relationship with self-rated physical health status (Maximova & Krahn, 2010).
Three of the eight papers assessed the potential impact of physical health on the workforce participation of refugees. The studies, two longitudinal and one cross-sectional consistently showed that physical illness reduced the likelihood of employment and increased the risk of disability pension for refugees (Helgesson et al., 2021; Khoo, 2010; Ruiz & Vargas-Silva, 2018). For example, a longitudinal study in Australia found that refugees who had no health conditions were more likely to be in the workforce than their counterparts who had a health condition. Notably, the difference was greater for men than women (Khoo, 2010).
4. Discussion
This systematic review presented findings from 72 papers that quantitatively explored the relationship between employment and health for refugees in resettlement countries. The overall evidence, although not always consistent, found a significant association between refugee health and aspects of paid employment including employment status and job quality. The relationship was moderated by factors such as gender, exposure to torture, and discrimination.
On balance, the review found that for refugees being employed is generally good for mental health. There was strong evidence to show that employment is significantly associated with positive mental health including lower levels of psychological distress and depression. In the included studies, refugees who were employed also had significantly higher life satisfaction than those who were unemployed. The findings of this review are consistent with previous systematic reviews in the general population which found a significant relationship between employment status and mental health particularly depression and psychological distress; especially where there are favourable workplace conditions (van der Noordt et al, 2014; Modini et al., 2016; Hergenrather et al., 2015). Specifically for the refugee population, a meta-analysis of 56 studies investigating factors associated with mental health found that economic opportunity (right to work, access to employment, and maintenance of socioeconomic status) was associated with better mental health (Porter & Haslam, 2005). Qualitative explorations of the impact of employment upon refugee health indicate that paid work can engender a sense of self-fulfillment, self-worth, and belonging. Employment also facilitates successful resettlement and better health (Hess et al., 2019; Wood et al., 2019).
There was insufficient evidence to support the relationship between employment and PTSD, anxiety, suicidal ideation, and suicide due to a lack of studies or inconsistent findings in the reviewed literature. This suggests that individual elements of mental illness may be affected differently by employment, although given the heterogeneity of the included studies more research is needed. There are suggestions in the included papers that the relationship between some mental illnesses and employment could be moderated by factors such as torture (Carlsson et al., 2006; Eisen et al., 2021; Hermansson et al., 2003; Kashyap et al., 2019), and levels of identification with ethnic background (Beiser & Hou, 2006).
Notably in this review, the number of papers (N=12) exploring physical health outcomes was significantly less than those focusing on mental health (N = 58). The reviewed literature consistently showed that people who are employed tend to have better physical health than unemployed persons who have a higher risk of long-term illness. Several of the included papers also highlighted that refugees are at higher risk of work-related health problems resulting from exposure to material hazards, musculoskeletal injuries, and long working hours. In the wider literature, refugees and immigrants are often labeled as vulnerable workers (Sterud et al., 2018). A systematic review of working conditions and occupational health among immigrants in Europe and Canada found that immigrants have a higher risk of work-related injuries than natives (Sterud et al., 2018). Compared to their non-immigrant counterparts, people from refugee backgrounds are more likely to perform physically demanding jobs and be exposed to occupational health and safety hazards (Ronda Perez et al., 2012).
As reported in previous systematic reviews in the general population, the bi-directional relationship between employment and health was also evident in the refugee populations. The few studies that examined the effect of health on employment found that the workforce participation of refugees in countries of resettlement was related to their overall health. Poor general health and mental disorders such as depression were found to be negatively associated with odds of employment and occupational status for refugees. There is substantial evidence in the health literature that refugees suffer from substantial health inequalities as a result of pre and post-migration stressors, including exposure to torture and trauma (Gleeson et al., 2020). Refugees are generally less likely to be employed and earn less than native-born and other migrant populations. There is a need for future research to explicitly examine the role that health disparities, particularly mental health, may play in these labour market gaps.
Findings from this review indicate that job satisfaction and quality significantly influence the relationship between employment and health for refugees. The reviewed papers reported that job satisfaction was associated with higher levels of life satisfaction, mental and general health. There appears to be a progressive relationship between the extent to which employment matches one's skills and qualifications and life satisfaction and emotional wellbeing. This is consistent with a previous meta-analysis of refugee studies which found that refugees who were more educated and had higher pre-displacement socioeconomic status had worse mental health outcomes (Porter & Haslam, 2005). People from refugee backgrounds often experience downward social mobility during resettlement (Newman, Bimrose, Nielsen, & Zacher, 2018). Overseas qualifications are generally not recognised in countries of resettlement and refugees often struggle to gain employment commensurate with their level of skills, education, and expertise (Newman, Bimrose, et al., 2018). It appears that for some refugees, especially those with higher levels of education, job satisfaction and quality of work may be more important than employment per se. However, more research is required to elucidate this relationship further.
Refugees face discrimination in a range of settings including employment (Ziersch, Due, & Walsh, 2020). In this review, discrimination in the job market was linked with lower life satisfaction and higher levels of depression. The participants in the studies reported that they faced discrimination not only based on their race, ethnicity but also their refugee status. The findings of this review are consistent with the growing body of evidence that discrimination is a health hazard for people of refugee and asylum-seeking backgrounds (Ziersch et al., 2020).
Refugees and asylum seekers are not a homogenous group and this systematic review found group differences in the relationship between employment and health. A striking result was the differences in mental health effects of employment on refugees who experienced torture compared to those who did not. Of the four longitudinal studies of refugee survivors of torture (Carlsson et al., 2006; Eisen et al., 2021; Hermansson et al., 2003; Kashyap et al., 2019) three found that employment alone was not significantly associated with mental outcomes such as PTSD, depression, and psychological wellbeing (Eisen et al., 2021; Hermansson et al., 2003; Kashyap et al., 2019). It is unclear why refugees who have experienced torture were not mentally affected by their employment status; however the health consequences of torture can be long-lasting, survivors continue to have mental and physical health symptoms many years after their exposure despite changes in their living conditions (Carlsson, Mortensen, & Kastrup, 2005). The review findings suggest that impacts of torture may not be ameliorated by employment alone. Concerning mental health more broadly, however, it is important to again note that diversity in cultural understandings of mental health and employment likely plays a role in the relationship between the two. It was beyond the scope of the review to explore specific cultural differences in this regard; this would be a useful direction for future research (Sullivan et al., 2020).
Compared to refugees, asylum seekers face additional vulnerabilities. In many countries, asylum seekers do not have the legal right to work (Burchett & Ruth, 2010). For asylum seekers specifically, the reviewed studies consistently cited the lack of work rights as an important stressor and predictor of psychiatric morbidity (Aragona et al., 2019; Hocking et al., 2015; Laban et al., 2005; Van Hanegem et al., 2011), having a depressive disorder, PTSD, or one of more DSM-IV psychiatric disorders (Aragona et al., 2019; Hocking et al., 2015; Laban et al., 2005) and severe acute maternal morbidity (Van Hanegem et al., 2011). Qualitative research from Australia and UK has found that living without the right to work left many asylum seekers with long periods with “nothing to do” (Burchett & Ruth, 2010; Fleay & Hartley, 2016). This was associated with a sense of shame and lack of autonomy as well as an inability to afford basic living necessities such as housing and food (Hartley & Fleay, 2017). Overall, the lack of work rights has profoundly negative effects on health and well-being (Burchett & Ruth, 2010; Fleay & Hartley, 2016; Hartley & Fleay, 2017). It is important to note that within this review, only 5 papers exclusively included asylum seekers highlighting a need for more research focusing on this particularly vulnerable group.
From the small sample of papers that examined gender differences, the data found that more men than women refugees were employed and that being employed was significantly associated with better mental health, particularly depression for men but not women. For women, the relationship between health and employment is less clear. For example, one study found temporary employment was associated with higher psychological distress for women than men and another found worse mental health symptoms amongst women who had been working for longer periods (Blight et al, 2006). Working women may experience worse health due to poor working conditions and the need to balance work and family duties (Wong, 2000). Overall, little attention has been devoted to gender differences in the mental health of refugee samples, and available data have yielded mixed findings and this highlights another important area for further research.
In terms of understanding the pathways linking employment and health for refugees, the systematic review findings highlight several micro-pathways (Benach, Solar, et al., 2010). Employment conditions including being employed and having a quality job that is commensurate with pre-displacement professional levels appear to be important in promoting good mental and physical health. Though less explored, the work environment particularly exposure to discrimination, material hazards, and poor working hours was associated with lower life satisfaction and health status. Macro-pathways were more difficult to assess within this review as many of the studies did not explicitly set out to explore this (Muntaner et al., 2010). The included studies had a wide-ranging study design and aims. Of the 72 included papers, only 10 studies specifically examined the link between employment and health, the remaining studies included employment as part of a conglomerate of other variables. The studies that did discuss the role of government policies relating to the exclusion of asylum seekers from the labour market by denying the right to work, consistently found this to be detrimental to health.
As a whole, the reviewed literature supports both the causative and selection hypothesis in the bi-directional relationship between employment and health for refugees, though the focus was more on causative pathways. Employment status and conditions can affect both the mental and physical health of refugees, but more evidence is available for some outcomes than others. The findings that refugees with poor health generally have lower odds of employment and occupational status are in keeping with the selection hypothesis (McDonough & Amick, 2001).
4.1. Limitations and future research
The findings of this systematic review are subject to limitations of the evidence and the review processes. Concerning the quality of the evidence, the majority of the included studies were cross-sectional (N=50) studies which limit causal determination. Some of the longitudinal studies only followed the participants over a short time which may not be sufficient to observe changes in employment or health status. For several health outcomes including anxiety, psychological wellbeing, and general mental health there were notable differences in the findings of the cross-sectional and longitudinal studies. For example, in the majority of cross-sectional studies, no significant relationship between anxiety, psychological wellbeing, general mental health and employment was found. By contrast, the longitudinal studies consistently found a significant association between employment and these mental health outcomes. It is likely that longitudinal studies provide a more sensitive and balanced exploration of the relationship between employment and health throughout the resettlement period. Hence more prospective longitudinal studies are required to further elucidate the causal pathways between employment and health. Except for the few studies conducted in Scandinavia and Australia which included national data sets, the majority of the studies used convenience snowball sampling methods which limit the generalisability of some of the study findings. The studies utilised a disparate range of measures for physical and mental health. Many of the measures were self-reported and have not been validated in asylum seeker or refugee populations, therefore the internal reliability of the findings is uncertain. The included studies were very heterogeneous, precluding a meta-analysis and making it difficult to draw unifying conclusions. There is a paucity in the literature examining the bi-directional relationship between employment and health, particularly the selection hypothesis and how health determines refugee labour market participation. Only ten of the 72 included papers examined the effect of health on employment status. There was a particular gap regarding the impact of mental health on employment.
There are several limitations regarding the review itself. The inclusion criteria were limited to articles available in English and published after 2000. This could have missed important studies especially those from countries where English is not the primary language. As the review only included quantitative data, the measures of employment utilised in the studies were less nuanced and mainly focused on employment status. Thus the review was less able to examine the various aspects of employment and the cross-cultural meanings of work. A future review including qualitative data would be beneficial in providing a more nuanced and detailed insight into potential pathways between employment and health for refugees, including cultural understandings of employment and health.
5. Conclusion
In conclusion, this review indicates that in general employment is beneficial for refugee mental health, particularly psychological distress, depression and overall wellbeing.
Good quality employment is also an essential component of refugee life satisfaction post resettlement. The limited number of studies reporting physical health outcomes shows that refugees who are employed have better physical health and less long-term illness than those who are unemployed. However, more research regarding the effects of employment on physical health is required. The effects of refugee-specific factors such as gender roles, torture, and trauma on the relationship between employment and health also require further investigation.
Further, the findings of this systematic have important implications for practice. The evidence for the bi-directional relationship between employment and health underscores the need for better coordination between health and employment services for refugees. The unique experiences of refugees, including exposure to torture and discrimination, means that policies and programs should be specifically tailored to the refugee context in order to reduce the inequalities in health and employment for this population group. Policies seeking to improve employment and health outcomes need to be culturally appropriate and reflect different conceptualisations of both employment and health.
Footnotes
The work did not receive funding. The authors have no conflicts of interest to declare.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2022.101075.
Contributor Information
Huyen Lai, Email: lai0153@flinders.edu.au.
Clemence Due, Email: clemence.due@adelaide.edu.au.
Anna Ziersch, Email: anna.ziersch@flinders.edu.au.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Ahmad F., Othamn N., Hynie M., Bayoumi A.M., Oda A., McKenzie K. Depression-level symptoms among Syrian refugees: Findings from a Canadian longitudinal study. Journal of Mental Health. 2021;30:246–254. doi: 10.1080/09638237.2020.1765998. [DOI] [PubMed] [Google Scholar]
- Ahmad F., Othman N., Lou W. Posttraumatic stress disorder, social support and coping among Afghan refugees in Canada. Community Mental Health Journal. 2020;56(4) doi: 10.1007/s10597-019-00518-1. [DOI] [PubMed] [Google Scholar]
- Alemi Q., James S., Siddiq H., Montgomery S. Correlates and predictors of psychological distress among Afghan refugees in San Diego County. International Journal of Culture and Mental Health. 2015;8(3):274. doi: 10.1080/17542863.2015.1006647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ambrosetti E., Dietrich H., Kosyakova Y., Patzina A. The impact of pre- and postarrival mechanisms on self-rated health and life satisfaction among refugees in Germany. Frontiers in Sociology. 2021;6 doi: 10.3389/fsoc.2021.693518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ao T., Shetty S., Sivilli T., Blanton C., Ellis H., Geltman P.L.…Lopes Cardozo B. Suicidal ideation and mental health of Bhutanese refugees in the United States. Journal of Immigrant and Minority Health. 2016;18(4):828–835. doi: 10.1007/s10903-015-0325-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aragona M., Castaldo M, Cristina Tumiati M., Schillirò C., Dal Secco A., Agrò F.…Mirisola C. Influence of post-migration living difficulties on post-traumatic symptoms in Chinese asylum seekers resettled in Italy. International Journal of Social Psychiatry. 2019 doi: 10.1177/0020764019888960. [DOI] [PubMed] [Google Scholar]
- Azaroff L.S., Levenstein C., Wegman D.H. The occupational health of Southeast Asians in Lowell: A descriptive study. International Journal of Occupational and Environmental Health. 2004;10(1):47–54. doi: 10.1179/oeh.2004.10.1.47. [DOI] [PubMed] [Google Scholar]
- Baranik L.E., Hurst C.S., Eby L.T. The stigma of being a refugee: A mixed-method study of refugees' experiences of vocational stress. Journal of Vocational Behavior. 2018;105:116. [Google Scholar]
- Barbieri A., Visco-Comandini F., Alunni Fegatelli D., Dessi A., Cannella G., Stellacci A., Pirchio S. Patterns and predictors of PTSD in treatment-seeking African refugees and asylum seekers: A latent class analysis. International Journal of Social Psychiatry. 2021;67(4):386–396. doi: 10.1177/0020764020959095. [DOI] [PubMed] [Google Scholar]
- Beiser M., Hou F. Language acquisition, unemployment and depressive disorder among Southeast Asian refugees: A 10-year study. Social Science & Medicine. 2001;53(10):1321–1334. doi: 10.1016/s0277-9536(00)00412-3. [DOI] [PubMed] [Google Scholar]
- Beiser M.N., Hou F. Ethnic identity, resettlement stress and depressive affect among Southeast Asian refugees in Canada. Social Science & Medicine. 2006;63(1):137–150. doi: 10.1016/j.socscimed.2005.12.002. [DOI] [PubMed] [Google Scholar]
- Benach J., Muntaner C., Solar O., Santana V., Quinlan M. Introduction to the WHO Commission on Social Determinants of Health Employment Conditions Network (EMCONET) study, with a glossary on employment relations. International Journal of Health Services. 2010;40:195–207. doi: 10.2190/HS.40.2.a. [DOI] [PubMed] [Google Scholar]
- Benach J., Solar O., Santana V., Castedo A., Chung H., Muntaner C., Network E. A micro-level model of employment relations and health inequalities. International Journal of Health Services. 2010;40:223–227. doi: 10.2190/HS.40.2.d. [DOI] [PubMed] [Google Scholar]
- Bhui K., Craig T., Mohamud S., Warfa N., Stansfeld S.A., Thornicroft G.…Mccrone P. Mental disorders among Somali refugees : Developing culturally appropriate measures and assessing socio-cultural risk factors. Social Psychiatry and Psychiatric Epidemiology. 2006;41(5):400–408. doi: 10.1007/s00127-006-0043-5. [DOI] [PubMed] [Google Scholar]
- Birman D., Simon C.D., Chan W.Y., Tran N. A life domains perspective on acculturation and psychological adjustment: A study of refugees from the former soviet Union. American Journal of Community Psychology. 2014;53(1–2):60–72. doi: 10.1007/s10464-013-9614-2. [DOI] [PubMed] [Google Scholar]
- Blight K.J., Ekblad S., Persson J-O., Ekberg J. Mental health, employment and gender. Cross-sectional evidence in a sample of refugees from Bosnia-Herzegovina living in two Swedish Regions. Social Science & Medicine. 2006;62(7):1697–1709. doi: 10.1016/j.socscimed.2005.08.019. [DOI] [PubMed] [Google Scholar]
- Bogic M., Ajdukovic D., Bremner S., Franciskovic T., Galeazzi G.M., Abdulah K.…Priebe S. Factors associated with mental disorders in long-settled war refugees: Refugees from the former Yugoslavia in Germany, Italy and the UK. The British Journal of Psychiatry. 2012;200(3):216–223. doi: 10.1192/bjp.bp.110.084764. [DOI] [PubMed] [Google Scholar]
- Bridekirk J., Hynie M., SyRia.lth The impact of education and employment quality on self-rated mental health among Syrian refugees in Canada. Journal of Immigrant and Minority Health. 2021;23(2):290–297. doi: 10.1007/s10903-020-01108-0. [DOI] [PubMed] [Google Scholar]
- Bryant R.A., Edwards B., Creamer M., O’donnell M., Forbes D., Felmingham K.L.…Hadzi-Pavlovic D. A population study of prolonged grief in refugees. Epidemiology and Psychiatric Sciences. 2019;29:e44. doi: 10.1017/S2045796019000386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burchett N., Ruth M. The need for belonging: The impact of restrictions on working on the well-being of an asylum seeker. Journal of Occupational Science. 2010;17(2):85–91. [Google Scholar]
- Campbell M.R., Mann K.D., Moffatt S., Dave M., Pearce M.S. Social determinants of emotional well-being in new refugees in the UK. Public Health. 2018;164:72. doi: 10.1016/j.puhe.2018.07.022. [DOI] [PubMed] [Google Scholar]
- Carlsson J.M., Mortensen E.L., Kastrup M. A follow-up study of mental health and health-related quality of life in tortured refugees in multidisciplinary treatment. The Journal of Nervous and Mental Disease. 2005;193(10):651–657. doi: 10.1097/01.nmd.0000180739.79884.10. [DOI] [PubMed] [Google Scholar]
- Carlsson J.M., Olsen D.R., Mortensen E.L., Kastrup M. Mental health and health-related quality of life - a 10-year follow-up of tortured refugees. The Journal of Nervous and Mental Disease. 2006;194(10):725–731. doi: 10.1097/01.nmd.0000243079.52138.b7. [DOI] [PubMed] [Google Scholar]
- Cetrez O.A., Demarinis V., Sundvall M., Fernandez-Gonzalez M, Borisova L., Titelman D. A public mental health study among Iraqi refugees in Sweden: Social determinants, resilience, gender, and cultural context. Frontiers in Sociology. 2021;6 doi: 10.3389/fsoc.2021.551105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colic-Peisker V. Visibility, settlement success and life satisfaction in three refugee communities in Australia. Ethnicities. 2009;9(2):175–199. [Google Scholar]
- Cooper S., Enticott J.C., Shawyer F., Meadows G. Determinants of mental illness among humanitarian migrants: Longitudinal analysis of findings from the first three waves of a large cohort study. Frontiers in Psychiatry. 2019;10 doi: 10.3389/fpsyt.2019.00545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Thiene D., Helgesson M., Rahman S., Alexanderson K., Tiihonen J., La Torre G., Mittendorfer-Rutz E. Risk of labour market marginalisation among young refugees and non-refugee migrants with common mental disorders. Social Psychiatry and Psychiatric Epidemiology. 2021;56(6):1025–1034. doi: 10.1007/s00127-020-02022-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drescher A., Kiselev N., Akhtar A., Acarturk C., Bryant R.A., Ilkkursun Z.…Morina N. Problems after flight: Understanding and comparing Syrians’ perspectives in the Middle East and Europe. BMC Public Health. 2021;21(1):717. doi: 10.1186/s12889-021-10498-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drydakis N. Adverse working conditions and immigrants’ physical health and depression outcomes: a longitudinal study in Greece. International Archives of Occupational and Environmental Health. 2022;95:539–556. doi: 10.1007/s00420-021-01757-0. [DOI] [PubMed] [Google Scholar]
- Dumont J.-C., Liebig T., Peschner J., Tanay F., Xenogiani T. How are refugees faring on the labour market in Europe? A first evaluation based on the 2014 EU labour force survey Ad Hoc module. European Commission. 2016 [Google Scholar]
- Eisen E., Howe G., Cogar M. The impact of post-migration factors on posttraumatic stress and depressive symptoms among asylum seekers in the United States. Journal of Immigrant & Refugee Studies. 2021;19:573–586. [Google Scholar]
- Fleay C., Hartley L. 'I feel like a beggar': Asylum seekers living in the Australian community without the right to work. Revue de l'integration et de la migration internationale. 2016;17(4):1031–1048. [Google Scholar]
- Frijters P., Johnston D.W., Shields M.A. The effect of mental health on employment: Evidence from Australian panel data. Health Economics. 2014;23(9):1058–1071. doi: 10.1002/hec.3083. [DOI] [PubMed] [Google Scholar]
- Gleeson C., Frost R, Sherwood L., Shevlin M., Hyland P., Halpin R.…Silove D. Post-migration factors and mental health outcomes in asylum-seeking and refugee populations: A systematic review. European Journal of Psychotraumatology. 2020;11(1) doi: 10.1080/20008198.2020.1793567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grochtdreis T., König H.H., Riedel-Heller S.G., Dams J. Health-related quality of life of asylum seekers and refugees in Germany: A cross-sectional study with data from the German Socio-Economic Panel. Applied Research in Quality of Life. 2020;17(1):109–127. [Google Scholar]
- Hartley L., Fleay C. “We are like animals”: Negotiating Dehumanising experiences of asylum-seeker policies in the Australian community. Refugee Survey Quarterly. 2017;36(4):45–63. [Google Scholar]
- Helgesson M., Rahman S., Saboonchi F., Ellenor Mittendorfer R. Disability pension and mortality in individuals with specific somatic and mental disorders: Examining differences between refugees and Swedish-born individuals. Journal of Epidemiology & Community Health. 2021;75(8):721–728. doi: 10.1136/jech-2019-213436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hergenrather K.C., Zeglin R., McGuire-Kuletz M., Rhodes S.C. Employment as a social determinant of health: A systematic review of longitudinal studies exploring the relationship between employment status and physical health. Rehabilitation Research Policy and Education. 2015;29(1):2–26. [Google Scholar]
- Hermansson A.-C., Thyberg M., Timpka T. The long-term impact of torture on the mental health of war-wounded refugees: Findings and implications for nursing programmes. Scandinavian Journal of Caring Sciences. 2003;17(4):317–324. doi: 10.1046/j.0283-9318.2003.00241.x. [DOI] [PubMed] [Google Scholar]
- Hermansson A.-C., Timpka T., Thyberg M. The mental health of war-wounded refugees: An 8-year follow-up. The Journal of Nervous and Mental Disease. 2002;190(6):374–380. doi: 10.1097/00005053-200206000-00005. [DOI] [PubMed] [Google Scholar]
- Hess J.M., Isakson B.L., Amer S., Ndaheba E., Baca B., Goodkind J.R. Refugee mental health and healing: Understanding the impact of policies of rapid economic self-sufficiency and the importance of meaningful work. Journal of International Migration and Integration. 2019;20(3):769–786. doi: 10.1007/s12134-018-0628-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hocking D.C., Kennedy G.A., Sundram S. Mental disorders in asylum seekers: The role of the refugee determination process and employment. The Journal of Nervous and Mental Disease. 2015;203(1):28–32. doi: 10.1097/NMD.0000000000000230. [DOI] [PubMed] [Google Scholar]
- Hunkler C., Khourshed M. The role of trauma for integration the case of Syrian refugees. SOZIALE WELT-ZEITSCHRIFT FUR SOZIALWISSENSCHAFTLICHE FORSCHUNG UND PRAXIS. 2020;71(1–2):90–122. [Google Scholar]
- Jamil H., Aldhalimi A., Arnetz B.B. Post-displacement employment and health in professional Iraqi refugees vs. Professional Iraqi immigrants. Journal of Immigrant & Refugee Studies. 2012;10(4):395–406. doi: 10.1080/15562948.2012.717826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jen K-L.C., Jamil H., Zhou K., Breejen K., Arnetz B.B. Sex differences and predictors of changes in body weight and noncommunicable diseases in a random, newly-arrived group of refugees followed for two years. Journal of Immigrant and Minority Health. 2018;20(2):283–294. doi: 10.1007/s10903-017-0565-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeon B.H., Kim M.D., Hong S.C., Kim N.R., Lee C.I., Kwak Y.S.…Kim D.S. Prevalence and correlates of depressive symptoms among North Korean defectors living in South Korea for more than one year. Psychiatry Investigation. 2009;6(3):122–130. doi: 10.4306/pi.2009.6.3.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kashyap S., Page A.C., Joscelyne A. Post-migration treatment targets associated with reductions in depression and PTSD among survivors of torture seeking asylum in the USA. Psychiatry Research. 2019;271:565–572. doi: 10.1016/j.psychres.2018.12.047. [DOI] [PubMed] [Google Scholar]
- Khawaj N.G., Hebbani A. Factors impacting life satisfaction of refugees in Australia: A mixed method study. Australian Community Psychologist. 2019;30(1):30–50. [Google Scholar]
- Khoo S.-E. Health and humanitarian migrants' economic participation. Journal of Immigrant and Minority Health. 2010;12(3):327–339. doi: 10.1007/s10903-007-9098-y. [DOI] [PubMed] [Google Scholar]
- Kim I. Beyond trauma: Post-resettlement factors and mental health outcomes among Latino and Asian refugees in the United States. Journal of Immigrant and Minority Health. 2016;18(4):740–748. doi: 10.1007/s10903-015-0251-8. [DOI] [PubMed] [Google Scholar]
- Kim H.H., Lee Y.J., Kim H.K., Kim J.E., Kim S.J., Bae S.M., Cho S.J. Prevalence and correlates of psychiatric symptoms in North Korean defectors. Psychiatry Investigation. 2011;8(3):179–185. doi: 10.4306/pi.2011.8.3.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koch-Weser S., Liang S.L., Grigg-Saito D.C. Self-reported health among Cambodians in Lowell, Massachusetts. Journal of Health Care for the Poor and Underserved. 2006;17(2):133–145. doi: 10.1353/hpu.2006.0089. [DOI] [PubMed] [Google Scholar]
- Kraeh A., Froese F.J., Kim S.G. Does socio-cultural and psychological adjustment influence physical health? The case of North Korean refugees in South Korea. International Journal of Intercultural Relations : IJIR. 2016;51:54. [Google Scholar]
- Laban C.J., Gernaat H.P.B.E., Komproe I.H., Van Der Tweel I., De Jong J.T. Postmigration living problems and common psychiatric disorders in Iraqi asylum seekers in the Netherlands. The Journal of Nervous and Mental Disease. 2005;193(12):825–832. doi: 10.1097/01.nmd.0000188977.44657.1d. [DOI] [PubMed] [Google Scholar]
- Lam N.C.-Y., Yeung H.-Y., Li W.-K., Lo H.-Y., Yuen C.-F., Chang R.C.-C., Ho Y.-S. Cognitive impairment in irritable bowel syndrome (IBS): A systematic review. Brain Research. 2019;1719:274–284. doi: 10.1016/j.brainres.2019.05.036. [DOI] [PubMed] [Google Scholar]
- Marmot M., Friel S., Bell R., Houweling T.A., Taylor S., Commission on the Social Determinants of Health Closing the gap in a generation: Health equity through action on the social determinants of health. The Lancet. 2008;372(9650):1661–1669. doi: 10.1016/S0140-6736(08)61690-6. [DOI] [PubMed] [Google Scholar]
- Marshall G.N., Schell T.L., Elliott M.N., Berthold S.M., Chun C.-A. Mental health of Cambodian refugees 2 decades after resettlement in the United States. Journal of the American Medical Association. 2005;294(5):571–579. doi: 10.1001/jama.294.5.571. [DOI] [PubMed] [Google Scholar]
- Matanov A., Giacco D., Bogic M., Ajdukovic D., Franciskovic T., Galeazzi G.M.…Priebe S. Subjective quality of life in war-affected populations. BMC Public Health. 2013;13 doi: 10.1186/1471-2458-13-624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maximova K., Krahn H. Health status of refugees settled in Alberta: Changes since arrival. Canadian journal of public health = Revue canadienne de sante publique. 2010;101(4):322–326. doi: 10.1007/BF03405295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonough P., Amick B.C., III The social context of health selection: A longitudinal study of health and employment. Social Science & Medicine. 2001;53(1):135–145. doi: 10.1016/s0277-9536(00)00318-x. [DOI] [PubMed] [Google Scholar]
- Milner A., Page A., LaMontagne A.D. Cause and effect in studies on unemployment, mental health and suicide: A meta-analytic and conceptual review. Psychological Medicine. 2014;44(5):909–917. doi: 10.1017/S0033291713001621. [DOI] [PubMed] [Google Scholar]
- Modini M., Joyce S., Mykletun A., Christensen H., Bryant R.A., Mitchell P.B., Harvey S.B. The mental health benefits of employment: Results of a systematic meta-review. Australasian Psychiatry. 2016;24(4):331–336. doi: 10.1177/1039856215618523. [DOI] [PubMed] [Google Scholar]
- Muntaner C., Chung H., Solar O., Santana V., Castedo A., Benach J, EMCONET Network A macro-level model of employment relations and health inequalities. International Journal of Health Services. 2010;40(2):215–221. doi: 10.2190/HS.40.2.d. [DOI] [PubMed] [Google Scholar]
- Neitzel R.M., Krenz J., de Castro A.B. Safety and health hazard observations in Hmong farming operations. Journal of Agromedicine. 2014;19(2):130. doi: 10.1080/1059924X.2014.886319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman A., Nielsen I., Smyth R., Hirst G. Mediating role of psychological capital in the relationship between social support and wellbeing of refugees. International Migration. 2018;56(2):117–132. [Google Scholar]
- Newman A., Bimrose J., Nielsen I., Zacher H. Vocational behavior of refugees: How do refugees seek employment, overcome work-related challenges, and navigate their careers? Journal of Vocational Behaviour. 2018;105(2):1–5. [Google Scholar]
- Niederkrotenthaler T., Mittendorfer-Rutz E., Mehlum L., Qin P., Björkenstam E. Previous suicide attempt and subsequent risk of re-attempt and suicide: Are there differences in immigrant subgroups compared to Swedish-born individuals? Journal of Affective Disorders. 2020;265:263–271. doi: 10.1016/j.jad.2020.01.013. [DOI] [PubMed] [Google Scholar]
- Niederkrotenthaler T., Mittendorfer-Rutz E., Saboonchi F., Helgesson M. The role of refugee status and mental disorders regarding subsequent labour market marginalisation: A register study from Sweden. Social Psychiatry and Psychiatric Epidemiology. 2020;55(6):697–704. doi: 10.1007/s00127-020-01842-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olesen S.C., Butterworth P., Leach L.S., Kelaher M., Pirkis J. Mental health affects future employment as job loss affects mental health: Findings from a longitudinal population study. BMC Psychiatry. 2013;13(1):1–9. doi: 10.1186/1471-244X-13-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olliff L. Refugee Council of Australia; Sydney: 2010. What works: Employment strategies for refugee and humanitarian entrants. [Google Scholar]
- Paul K.I., Moser K. Unemployment impairs mental health: Meta-analyses. Journal of Vocational Behavior. 2009;74(3):264–282. [Google Scholar]
- Pelkowski J.M., Berger M.C. The impact of health on employment, wages, and hours worked over the life cycle. The Quarterly Review of Economics and Finance. 2004;44(1):102–121. [Google Scholar]
- Pinto A.D., Hassen N., Craig-Neil A. Employment interventions in health settings: A systematic review and synthesis. The Annals of Family Medicine. 2018;16(5):447–460. doi: 10.1370/afm.2286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porter M., Haslam N. Predisplacement and postdisplacement factors associated with mental health of refugees and internally displaced persons: A meta-analysis. JAMA. 2005;294(5):602–612. doi: 10.1001/jama.294.5.602. [DOI] [PubMed] [Google Scholar]
- Poudel P., Griffiths R., Wong V.W., Arora A., Flack J.R., Khoo C.L., George A. Oral health knowledge, attitudes and care practices of people with diabetes: A systematic review. BMC Public Health. 2018;18(1):1–12. doi: 10.1186/s12889-018-5485-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Renner A., Jäckle D., Nagl M., Hoffmann R., Röhr R., Jung F.…Kersting A. Predictors of psychological distress in Syrian refugees with posttraumatic stress in Germany. PLoS One. 2021;16(8) doi: 10.1371/journal.pone.0254406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Renner W., Salem I. Post-traumatic stress in asylum seekers and refugees from Chechnya, Afghanistan, and West Africa: Gender differences in symptomatology and coping. International Journal of Social Psychiatry. 2009;55(2):99–108. doi: 10.1177/0020764008092341. [DOI] [PubMed] [Google Scholar]
- Ronda Perez E., Benavides F.G., Levecque K., Love J.G., Felt E., Van Rossem R. Differences in working conditions and employment arrangements among migrant and non-migrant workers in Europe. Ethnicity and Health. 2012;17(6):563–577. doi: 10.1080/13557858.2012.730606. [DOI] [PubMed] [Google Scholar]
- Ruiz I., Vargas-Silva C. Differences in labour market outcomes between natives, refugees and other migrants in the UK. Journal of Economic Geography. 2018;18(4):855–885. [Google Scholar]
- Salman K., Turek J.M., Donovan C. Community health and wellness fair: A strategy for assessment of social determinants of health, inclusion and engagement of newcomers. Journal of Community Health. 2021;46(3):527–537. doi: 10.1007/s10900-020-00901-0. [DOI] [PubMed] [Google Scholar]
- Salo C.D., Birman D. Acculturation and psychological adjustment of Vietnamese refugees: An ecological acculturation framework. American Journal of Community Psychology. 2015;56(3–4):395–407. doi: 10.1007/s10464-015-9760-9. [DOI] [PubMed] [Google Scholar]
- Schuring M., Burdorf L., Kunst A., Mackenbach J. The effects of ill health on entering and maintaining paid employment: Evidence in European countries. Journal of Epidemiology & Community Health. 2007;61(7):597–604. doi: 10.1136/jech.2006.047456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuring M., Burdorf A., Kunst A., Voorham T., Mackenbach J. Ethnic differences in unemployment and ill health. International Archives of Occupational and Environmental Health. 2009;82(8):1023–1030. doi: 10.1007/s00420-009-0408-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw S.A., Poulin P. Findings from an extended case management U.S. Refugee resettlement program. Journal of International Migration and Integration. 2015;16(4):1099–1120. [Google Scholar]
- Sidorchuk A., Engström K., Johnson C.M., Naima Kayser L., Möller J. Employment status and psychological distress in a population-based cross-sectional study in Sweden: The impact of migration. BMJ Open. 2017;7(4) doi: 10.1136/bmjopen-2016-014698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sonne C., Mortensen E.L., Silove D., Palic S., Carlsson J. Predictors of treatment outcomes for trauma-affected refugees - results from two randomised trials. Journal of Affective Disorders. 2021;282:194–202. doi: 10.1016/j.jad.2020.12.095. [DOI] [PubMed] [Google Scholar]
- Sterud T., Tynes T., Mehlum I.S., Veiersted K.B., Bergbom B., Airila A.…Flyvholm M.-A. A systematic review of working conditions and occupational health among immigrants in Europe and Canada. BMC Public Health. 2018;18(1):1–15. doi: 10.1186/s12889-018-5703-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sulaiman-Hill C.M.R., Thompson S.C. Afghan and Kurdish refugees, 8-20 years after resettlement, still experience psychological distress and challenges to well being. Australian & New Zealand Journal of Public Health. 2012;36(2):126–134. doi: 10.1111/j.1753-6405.2011.00778.x. [DOI] [PubMed] [Google Scholar]
- Sullivan C., Vaughan C., Wright J. School of Population and Global Health, University of Melbourne; Melbourne, Australia: 2020. Migrant and refugee women's mental health in Australia: A literature review. [Google Scholar]
- Sundquist J., Ostergren P.-O., Sundquist K., Johansson S.-E. Psychosocial working conditions and self-reported long-term illness: A population-based study of Swedish-born and foreign-born employed persons. Ethnicity and Health. 2003;8(4):307–317. doi: 10.1080/1355785032000163939. [DOI] [PubMed] [Google Scholar]
- Teodorescu D.-S., Heir T., Hauff E., Wentzel-Larsen T., Lien L. Mental health problems and post-migration stress among multi-traumatized refugees attending outpatient clinics upon resettlement to Norway. Scandinavian Journal of Psychology. 2012;53(4):316–332. doi: 10.1111/j.1467-9450.2012.00954.x. [DOI] [PubMed] [Google Scholar]
- Teodorescu D.-S., Siqveland J., Heir T., Hauff E., Wentzel-Larsen T., Lien L. Posttraumatic growth, depressive symptoms, posttraumatic stress symptoms, post-migration stressors and quality of life in multi-traumatized psychiatric outpatients with a refugee background in Norway. Health and Quality of Life Outcomes. 2012;10:84. doi: 10.1186/1477-7525-10-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tonsing K.N., Vungkhanching M. The relationship between postmigration living difficulties, social support, and psychological distress of Burmese refugees in the United States. Asian American Journal of Psychology. 2020;11(3):179–186. [Google Scholar]
- UNHCR . United Nations High Commissioner for Refugees; Geneva: 2011. UNHCR Resettlement Handbook. [Google Scholar]
- UNHCR What is a refugee? 2021. https://www.unhcr.org/en-au/what-is-a-refugee.html?query=what%20is%20a%20refugee [cited 2021 September ]; Available from:
- UNHCR . 2021. Refugee data finder.https://www.unhcr.org/refugee-statistics/ [cited 2021; Available from: [Google Scholar]
- van der Noordt M., Ijzelenberg H., Droomers M., Proper K.I. Health effects of employment: A systematic review of prospective studies. Occupational and Environmental Medicine. 2014;71(10):730–736. doi: 10.1136/oemed-2013-101891. [DOI] [PubMed] [Google Scholar]
- Van Hanegem N., Miltenburg A.S., Zwart J.J., Bloemenkamp K.W.M., Van Roosmalen J. Severe acute maternal morbidity in asylum seekers: A two-year nationwide cohort study in the Netherlands. Acta Obstetricia et Gynecologica Scandinavica. 2011;90(9):1010–1016. doi: 10.1111/j.1600-0412.2011.01140.x. [DOI] [PubMed] [Google Scholar]
- Vinokurov A., Birman D., Trickett E. Psychological and acculturation correlates of work status among Soviet Jewish refugees in the United States. International Migration Review. 2000;34(2):538–559. [Google Scholar]
- de Vroome T., van Tubergen F. The employment experience of refugees in the Netherlands. International Migration Review. 2010;44(2):376–403. doi: 10.1111/j.1747-7379.2011.00860.x. [DOI] [PubMed] [Google Scholar]
- Walther L., Fuchs L.M., Schupp J., Von Scheve C. Living Conditions and the Mental Health and Well-being of Refugees: Evidence from a Large-Scale German Survey. Journal of Immigrant and Minority Health. 2020;22(5):903–913. doi: 10.1007/s10903-019-00968-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walther L., Kroger H., Tibubos A.N., Ta T.M.T., Von Scheve C., Schupp J., Hahn E., Bajbouj M. Psychological distress among refugees in Germany: a cross-sectional analysis of individual and contextual risk factors and potential consequences for integration using a nationally representative survey. BMJ Open. 2020;10 doi: 10.1136/bmjopen-2019-033658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warfa N., Curtis S., Watters C., Carswell K., Ingleby D., Bhui K. Migration experiences, employment status and psychological distress among Somali immigrants: A mixed-method international study. BMC Public Health. 2012;12:749. doi: 10.1186/1471-2458-12-749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . 2021. World health organization constitution.https://www.who.int/about/governance/constitution [cited 2021 September]; Available from: [Google Scholar]
- Wong M. Ghanaian women in Toronto's labour market: Negotiating gendered roles and transnational household strategies. Canadian Ethnic Studies Journal. 2000;32(2):45–75. [Google Scholar]
- Wood N., Charlwood G., Zecchin C., Hansen V., Douglas M., Pit S.W. Qualitative exploration of the impact of employment and volunteering upon the health and wellbeing of African refugees settled in regional Australia: A refugee perspective. BMC Public Health. 2019;19 doi: 10.1186/s12889-018-6328-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright A.M., Dhalimi A., Lumley M.A., Jamil H., Pole N., Arnetz J.E., Arnetz B.B. Unemployment in Iraqi refugees: The interaction of pre and post-displacement trauma. Scandinavian Journal of Psychology. 2016;57(6):564–570. doi: 10.1111/sjop.12320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yalim A.C. The impacts of contextual factors on psychosocial wellbeing of Syrian refugees: Findings from Turkey and the United States. Journal of Social Service Research. 2020;47:104–117. [Google Scholar]
- Zhang M., Gurung A., Anglewicz P., Yun K. COVID-19 and immigrant essential workers: Bhutanese and Burmese refugees in the United States. Public Health Reports. 2021;136(1):117–123. doi: 10.1177/0033354920971720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ziersch A., Due C., Walsh M. Discrimination: A health hazard for people from refugee and asylum-seeking backgrounds resettled in Australia. BMC Public Health. 2020;20(1):108. doi: 10.1186/s12889-019-8068-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.