Abstract
Objective
Perinatal mortality is an important outcome indicator for newborn care and directly mirrors the quality of prenatal, intra partum and newborn care. Therefore, this study was aimed at estimating perinatal mortality and its predictors in Eastern Ethiopia using data from Kersa Health and Demographic Surveillance System (KHDSS).
Design, settings and participants
An open dynamic cohort design was employed among pregnant women from 2015 to 2020 at KHDSS. A total of 19 687 women were observed over the period of 6 years, and 29 719 birth outcomes were registered.
Outcome measures
Perinatal mortality rate was estimated for each year of cohort and the cumulative of 6 years. Predictors of perinatal mortality are identified.
Results
From a total of 29 306 births 783 (26.72 deaths per 1000 births; 95% CI 24.88 to 28.66) deaths were occurred during perinatal period. Rural residence (adjusted OR (AOR)=3.43; 95% CI 2.04 to 5.76), birth weight (low birth weight, AOR=3.98; 95% CI 3.04 to 5.20; big birth weight, AOR=2.51; 95% CI 1.76 to 3.57), not having antenatal care (ANC) (AOR=1.67; 95% CI 1.29 to 2.17) were associated with higher odds of perinatal mortality whereas the parity (multipara, AOR=0.46; 95% CI 0.34 to 0.62; grand multipara, AOR=0.31; 95% CI 0.21 to 0.47) was associated with lower odds of perinatal mortality.
Conclusions
The study revealed relatively high perinatal mortality rate. Place of residence, ANC, parity and birth weight were identified as predictors of perinatal mortality. Devising strategies that enhance access to and utilisations of ANC services with due emphasis for rural residents, primipara mothers and newborn with low and big birth weights may be crucial for reducing perinatal mortality.
Keywords: EPIDEMIOLOGY, PERINATOLOGY, Fetal medicine
Strengths and limitations of this study.
The study used prospectively collected data over the period of 6 years.
Medical, obstetric factors and nutritional status of the mother were not well addressed.
Maternal report about newborn size at birth may result in some misclassification due to recall bias or subjective assessment.
The perinatal mortality was only captured after the death had occurred as the result difficult to determine the causes.
Introduction
Perinatal mortality is defined as the number of fetal deaths past 22 (or 28) completed weeks of pregnancy plus the number of deaths among live-born children up to 7 completed days of life. Perinatal mortality rate is presented per 1000 total births (live births and stillbirths).1 Perinatal mortality is a public health as well as a development problem in low-income and middle-income regions. Perinatal mortality is an important outcome indicator for country’s socioeconomic situation, quality of life and directly mirrors the quality of prenatal, intra partum, and newborn care.2
Globally in 2019, 4.3 million perinatal deaths occurred—that is one perinatal death every 7 seconds.3 The number of perinatal deaths decreased from 5.7 million in 2000 to 4.1 million in 2015,4 with 95% of these untimely deaths occurring in South Asia and sub-Saharan Africa.4 5 In sub-Saharan Africa perinatal mortality has continued to be the prevailing problem with the highest rate of 34.7 deaths per 1000 live births.6 Ethiopia is among the countries with the highest perinatal mortality in the world with 33 per 1000 live births.7 Besides, Ethiopia has shared sustainable development goals (SDGs) to achieve the target for reduction of neonatal mortality to below 12 per 1000 live births by 2030.8
Access to modern healthcare such as antenatal care (ANC), skilled birth attendance and postnatal care (PNC) are among the key maternal health interventions to have made undeniable differences in reducing perinatal mortality worldwide.9 Distance from health facility and road inaccessibility contributes to the delayed and poor access to services which in turn associated with increased maternal, fetal and infant mortality and morbidity.10 Despite the improvement in access to maternal health services in Africa over the years, it has remained relatively low in Ethiopia.7
The causes of stillbirths and early neonatal deaths are closely linked, and it can be difficult to determine whether a death is attributable to one cause or the other.11 Nevertheless, studies revealed that sex of neonate,12 birth weight,13 14 place of residence,15 wealth index, maternal education, maternal age,6 16 parity17 and prior preterm delivery,16 18 as predictors of perinatal mortality. Utilisation of obstetrics care such as ANC, delivery by skilled attendant and PNCs had positive contributions in reducing perinatal deaths.19 Moreover, home delivery is identified as an important determinant of perinatal mortality, and accounts for more than 75% of the perinatal deaths.20
Population-based surveillance system provides reliable data that are significant to tracking the progress of SDGs. In low-income countries like Ethiopia, where only 48% of deliveries occur in health facilities and 34% receive a PNC check-up,21 facility-based data hardly reflect the burden of perinatal mortality in the population. In addition, the risk factors for the perinatal mortality are poorly documented and understood in Eastern Ethiopia. Therefore, this study aimed at estimating perinatal mortality and its predictors using prospectively data from Kersa Health and Demographic Surveillance System, Eastern Ethiopia. Moreover, this study provides factual insights to support the development of strategies that helps achieve perinatal mortality and child mortality reduction targets of SDGs.
Methods
Study setting and period
Kersa Health and Demographic Surveillance System (HDSS) field site is located in Kersa district in East Hararghe zone. Kersa HDSS was established in 2007, starting with an initial census in 12 kebeles (small administrative unit in Ethiopia) to define the baseline denominator population; the initial census did not contain vital events (birth and death).22 Currently, the HDSS covers 36 kebeles (24 kebeles from Kersa districts and 12 kebeles from Harar town) which includes 41 056 households and a total population of 197 268.23
Study design and population
Kersa HDSS employs an open dynamic cohort study design that prospectively follows individuals living within a specific geographical boundary. All individuals who are living in Kersa HDSS has visited every 6 months. During each visit, reproductive age (15–49 years) women from the households are interviewed about their pregnancy, and their birth outcome. Birth outcome was categorised as live birth, stillbirth and abortion and miscarriage. Child born alive is followed for other event like death. Those new born who died within 7 days were considered as early neonatal death. Stillbirth and early neonatal death were considered to be perinatal deaths.
Patient and public involvement
There was no patient or public involvement in this research.
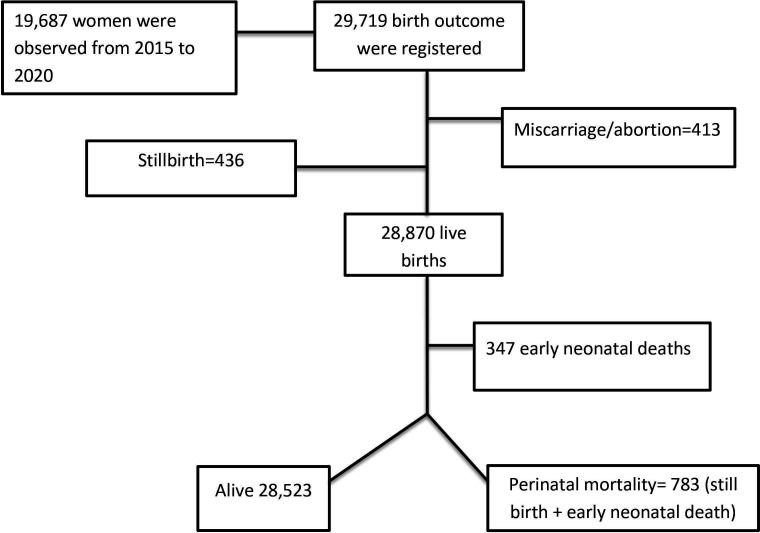
Sample size and sampling techniques
A total of 19 687 women were observed from 1 January 2015 through 31 December 2020. Temporary visitors or those individuals living for less than 6 months in the study site are not considered residents. A total of 29 719 birth outcomes (live birth, stillbirth and miscarriage/abortion) occurred over the follow-up period. Four hundred and thirteen events (miscarriage/abortion) were excluded from the study as they do not fulfil the definition of perinatal deaths (both stillbirth and neonatal deaths). Researchers extracted a 6 years (1 January 2015 to 31 December 2020) data from Kersa HDSS database system. Events which happened between 1 January 2015 and 31 December 2020 were recorded. Four hundred and thirty-six stillbirth and 347 early neonatal deaths give us 783 perinatal mortalities. All birth outcome and early neonatal death were retrieved by years, and perinatal mortality rate was calculated by dividing stillbirth (436) and early neonatal death (347) per 1000 all birth for each year (figure 1).
Figure 1.
Pregnancy observation flow chart, in Kersa Health and Demographic Surveillance System from 2015 to 2020.
Data collection procedure
Data were collected by well-trained regular HDSS staffs through face-to-face interview using tablet computer with Open Data Kit (ODK) collect application. Supervisors were assigned to supervise data collectors in the field. Field supervisors checked data quality before it was sent to the database system. If supervisors found a data quality problem, they sent back to data collectors for correction. Collected data using a tablet computer in the field was temporarily stored on ODK aggregate. The data manager approved the quality of data and transferred data from temporary storage to the final storage Openhds database system. Personal identifiers were removed from extracted data.
Study variables
Outcome variable
The perinatal mortality was outcome variable, categorised ‘yes’ if perinatal deaths occurred and ‘no’ if no perinatal deaths occurred as defined below in the operational definitions.
Explanatory variables
Potential predictors for perinatal death were place of residence, mother’s age, age at first child birth, mother occupation, mother educational status, parity, ANC follow-up, child sex and newborn weight at birth.
Operational definitions
Perinatal mortality
Perinatal mortality is defined as stillbirths plus early neonatal deaths. Perinatal mortality rate was calculated by dividing total perinatal deaths by all births (including stillbirths) that had pregnancy duration of 28 or more weeks. Stillbirth was defined as the number of fetal deaths in pregnancy of 7 or more months.7 An early neonatal death is defined as a death in the first 7 days (days 0–6) of a child born alive.24 Dummy variables were created for this variable for presence of perinatal mortality and was assigned ‘yes’ (coded as 1) and the absence of perinatal mortality was coded as ‘no’ (coded as 0).
For this study, the mother’s perception of the newborns size is defined as small being equivalent to less than 2500 g, normal (average) 2500–4000 g and large greater than 4000 g. This estimate was obtained because birth weight is unknown for most newborns in Ethiopia. Mother educational status was categorised as ‘literate’ if she attended any formal school, and had literacy and numeracy skills; if she has no formal education but can read and write, she was labelled as ‘can read and write’; if the mother was not able to read nor write she was labelled as ‘neither read nor write’. Parity refers to the number of children born to the women; if she gave birth to only one child she was categorised as ‘prim parous’ and if she gave birth to more than one child, she was labelled as ‘multipara’. Age at first childbirth: if the women gave birth to her first child at 20 years old or less, it was categorised as ‘≤20 years’ otherwise labelled as ‘>20 years’. Place of delivery: the place where the child is born; if the child is born at a health centre, health post or hospital, then it is labelled as ‘deliver at health facility’, if the women gave birth at home, it was labelled as ‘deliver at home’. ANC: if the pregnant woman attended the ANC unit during her pregnancy at least once, researchers categorised it as ‘yes’ otherwise ‘no’. Place of residence: a place where individuals live; individuals living in Harar City were labelled as ‘urban’, those living in the small town in Kersa were labelled as ‘semi-urban’ and those living in Kersa rural area were labelled as ‘rural mother’. For this study, the mother’s perception of the
Newborn weight at birth
Newborn weight at birth is defined as small being equivalent to less than 2500 g, normal (average) 2500–4000 g and large greater than 4000 g. This estimate was obtained because birth weight is unknown for most newborns in Ethiopia.25
Mother educational status
Mother educational status is categorised as ‘literate’ if she attended any formal school, and had literacy and numeracy skills; if she has no formal education but can read and write, she was labelled as ‘can read and write’; if the mother was neither able to read nor write she was labelled as ‘neither read nor write’.
Parity
Refers to the number of children born to the women; if she gave birth to only 1 child she was categorised as ‘primipara’, if she gave birth to 2 to 4 children, she was labelled as ‘multipara’, and if ≥5 births labelled as ‘grand multipara’.26
ANC) follow-up
If the pregnant women attended the ANC unit during her pregnancy at least once, categorised as ‘yes’ otherwise ‘no’.
Birth attendant
Birth attendant is categorised as ‘health professional’ and ‘non-health professional’. Health professional attendant is when the delivery is attended by health worker having the essential midwifery skills to manage normal labour and delivery, recognise complications early and perform any essential interventions including early referral.27 Non-health professional attendant is when the delivery is attended by person other than trained health professional.
Wealth index
Households were given scores based on the number and kinds of consumer goods they own, these scores are derived using principal component analysis. Wealth index are compiled by assigning the household score to each usual household member, ranking each person in the household population by her or his score and grouped individuals into three quartiles (poor, middle and rich).
Data processing and analysis
The collected data were checked for completeness and consistencies. It was also coded, entered and cleaned using Epi Data V.3.1 and then it was exported to STATA V.14 for analysis. Descriptive analysis including frequency distribution and the percentage was computed to determine the perinatal mortality by year, to describe socioeconomic and demographic and other determinants. Mortality rates and trends were described by rates with 95% CIs. Before fitting the model, χ2 was used to evaluate whether there is an association between the outcome and independent variables which are categorical. Multi-collinearity assumptions were checked by VIF (variance inflation factor) and variables with VIF larger than 10 were omitted from the final model. A binary logistic regression was fitted in a series of steps. First step, a bivariate analysis was carried out to examine the relationship between perinatal death and the potential predictors without adjusting for potential confounders. Second step, all potential predictors with p value less than 0.25 in the bivariable analysis were selected for multiple logistic regressions to examine their effects after adjusting for potential confounders. In the multivariate analysis model, predictor variables were presented with adjusted ORs (AORs) and 95% CIs with significance level of p value <0.05. The goodness of fit of final model was checked using Hosmer-Lemeshow.
Results
A total of 19 687 women were followed from 2015 to 2020 in Kersa HDSS. During this period 29 719 birth outcomes were registered of which 436 (1.46%) of them were stillbirth and 28 870 (97%) of them were alive birth. Among the alive birth, 347 (1.2%) died within 7 days of birth (figure 1). More than two-thirds (71.41) of the mothers were from rural residence. Majority (56.88%) of the women had no formal education (table 1).
Table 1.
Sociodemographic characteristics of study participants, Kersa Health and Demographic Surveillance System, Eastern Ethiopia, 2015–2020
| Variables | Frequency | Per cent |
| Mother’s age (n=19 342) | ||
| Less than 20 years | 2565 | 13.26 |
| 20–29 years | 9338 | 48.28 |
| ≥30 years | 7439 | 38.46 |
| Mean (±SD)=28.18 (±7.10) | ||
| Mothers educational status (n=19 561) | ||
| Has formal education | 8083 | 41.32 |
| Only read and or write | 352 | 1.80 |
| Has no formal education | 11 126 | 56.88 |
| Mothers occupation (n=19 491) | ||
| House wife | 14 978 | 76.85 |
| Daily labourer | 488 | 2.50 |
| Merchant | 771 | 3.96 |
| Unemployed | 2424 | 12.44 |
| Paid employer | 830 | 4.26 |
| Wealth index (n=18 679) | ||
| Poor | 6217 | 33.28 |
| Middle | 6370 | 34.10 |
| Rich | 6092 | 32.61 |
| Residence (n=19 561) | ||
| Urban | 5593 | 28.59 |
| Rural | 13 968 | 71.41 |
| Age at first child birth (n=19 524) | ||
| 13–19 years | 11 088 | 56.79 |
| 20–35 years | 8436 | 43.21 |
| Antenatal care follow-up (n=29 306) | ||
| Yes | 13 499 | 46.06 |
| No | 15 807 | 53.94 |
| Place of child birth (n=29 306) | ||
| Home | 16 850 | 57.50 |
| Health facility | 12 456 | 42.50 |
| Birth attendant (n=29 305) | ||
| Non-health professional | 17 107 | 58.38 |
| Health professional | 12 198 | 41.62 |
| Gravidity (n=29 243) | ||
| Primigravida | 5596 | 19.14 |
| Multigravida | 14 144 | 48.37 |
| Grand multigravida | 9503 | 32.50 |
| Parity (n=29 209) | ||
| Primipara | 6047 | 20.70 |
| Multipara | 14 358 | 49.16 |
| Grand multipara | 8804 | 30.14 |
| Newborn weight at birth (n=28 653) | ||
| Small | 2213 | 7.72 |
| Normal | 23 317 | 81.38 |
| Large | 3123 | 10.90 |
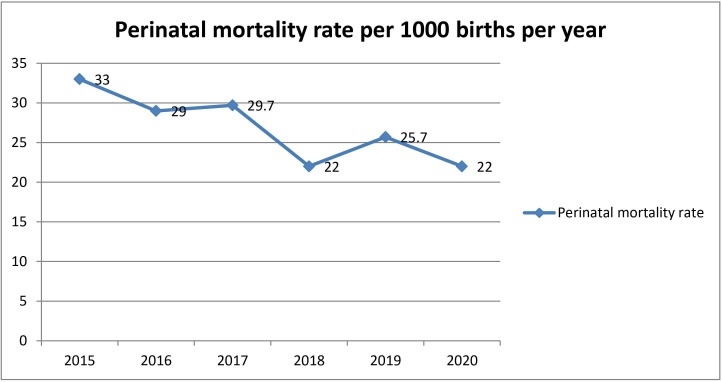
Perinatal mortality rate
The cumulative perinatal mortality rate over the period of 6 years was 26.72 per 1000 births (95% CI 24.88 to 28.66). The mortality rate has declined from 2015 to 2020 with fluctuating trends. In 2015 it was 32.96/1000 births (95% CI 27.56 to 39.12) and 22.10/1000 birth (95% CI 18.07 to 26.75) in 2020 (figure 2). Perinatal mortality rate was 30.4 per 1000 births in rural residents and 14.9 per 1000 births in urban residents. Perinatal mortality rate among mothers in the group <20 years was 39.4 per 1000 births and 26.4 per 1000 births for those in the age group 30 years and above (table 2).
Figure 2.
Perinatal mortality rate from 2015 to 2020 in Kersa Health and Demographic Surveillance System, Eastern Ethiopia.
Table 2.
Perinatal mortality rate by sociodemographic characteristics
| Variable | Perinatal mortality rate per 1000 births | 95% CI |
| Wealth index | ||
| Rich | 25.2 | 22.1 to 28.6 |
| Middle | 28.3 | 25.2 to 31.8 |
| Poor | 27.5 | 24.4 to 31.0 |
| Mother educational status | ||
| Literate | 23.3 | 20.7 to 26.3 |
| Read and write | 15.3 | 7.7 to 30.5 |
| Neither read or write | 29.3 | 26.9 to 31.9 |
| Place of residence | ||
| Rural | 30.4 | 28.3 to 32.8 |
| Urban | 14.9 | 12.3 to 18.0 |
| Mother’s age | ||
| Less than 20 years | 39.4 | 33.1 to 46.9 |
| 20–29 years | 24.4 | 22.0 to 27.1 |
| ≥30 years | 26.4 | 23.7 to 29.4 |
| Mother occupations | ||
| Housewife | 27.5 | 25.5 to 29.7 |
| Daily labourer | 29.9 | 19.1 to 46.5 |
| Merchant | 19.9 | 12.7 to 31.0 |
| Unemployed | 27.7 | 22.8 to 33.6 |
| Paid employee | 10.1 | 5.5 to 18.8 |
| Age at first child birth | ||
| Less than 20 years | 28.4 | 26.1 to 30.1 |
| ≥20 years | 23.9 | 21.3 to 26.9 |
Predictors of perinatal mortality
In bivariable analysis place of residence, mother’s age, mother’s occupation, mother’s education, age at first birth, parity, ANC follow-up, child sex and birth weight were found to be associated with perinatal mortality. To adjust for potential confounders, multi-variable logistic regression was fitted for place of residence, current mother’s age, mother’s occupation, mother’s educational status, wealth index, age at first child birth, parity, ANC follow-up, parity, child sex and birth weight. After adjusting for potential confounders place of residence, ANC follow-up, parity and birth weight were independently associated with perinatal mortality.
Multivariable logistic regression revealed that being from rural setting increased the odds of perinatal mortality by 3.43 compared with those from urban setting (AOR=3.43; 95% CI 2.04 to 5.76). The odds of perinatal mortality were decreased by 54% for multipara and 69% for grand multipara mothers compared with the primipara mothers (multipara, AOR=0.46; 95% CI 0.34 to 0.62; grand multipara, AOR=0.31; 95% CI 0.21 to 0.47). The odds of perinatal mortality among women who did not attend ANC were higher by 67% compared with those who attended ANC (AOR=1.67; 95% CI 1.29 to 2.17).
The odds of perinatal mortality was higher for low and big birth weight compared with the term normal birth weight (small birth weight, AOR=3.98; 95% CI 3.04 to 5.20; large birth weight, AOR=2.51; 95% CI 1.76 to 3.57) (table 3).
Table 3.
Multivariable logistic regressions for predictors of perinatal mortality in Kersa Health and Demographic Surveillance System, Eastern Ethiopia
| Variables | COR (95% CI) | P value | AOR (95% CI) | P value |
| Place of residence | ||||
| Urban | 1 | 1 | ||
| Rural | 2.08 (1.69 to 2.56) | 0.000 | 3.43 (2.04 to 5.76) | 0.000 |
| Mother’s age | ||||
| <20 years | 1 | 1 | ||
| 20–29 years | 0.61 (0.49 to 0.75) | 0.000 | 0.93 (0.65 to 1.33) | 0.705 |
| ≥30 years | 0.66 (0.53 to 0.82) | 0.000 | 1.45 (0.93 to 2.26) | 0.100 |
| Mother occupation | ||||
| Unemployed | 1 | 1 | ||
| House wife | 0.99 (0.80 to 1.23) | 0.952 | 0.83 (0.60 to 1.15) | 0.263 |
| Daily labourer | 1.08 (0.66 to 1.78) | 0.758 | 1.04 (0.44 to 2.48) | 0.924 |
| Merchant | 0.71 (0.43 to 1.17) | 0.180 | 1.34 (0.53 to 3.36) | 0.537 |
| Paid employee | 0.36 (0.18 to 0.69) | 0.002 | 0.20 (0.03 to 1.55) | 0.125 |
| Mother education status | ||||
| Has formal education | 1 | 1 | ||
| Read and or write | 0.65 (0.32 to 1.33) | 0.239 | 0.73 (0.29 to 1.82) | 0.505 |
| Neither read nor write | 1.26 (1.09 to 1.47) | 0.002 | 1.17 (0.89 to 1.53) | 0.260 |
| Wealth index | ||||
| Rich | 1 | 1 | ||
| Poor | 1.09 (.91 to 1.31) | 0.315 | 0.88 (0.67 to 1.17) | 0.379 |
| Middle | 1.13 (0.94 to 1.35) | 0.182 | 1.06 (0.81 to 1.39) | 0.660 |
| Age at first child birth | ||||
| ≥20 years | 1 | 1 | ||
| <20 years | 1.19 (1.03 to 1.38) | 0.020 | 1.06 (0.83,1.35) | 0.642 |
| Parity | ||||
| Primipara | 1 | 1 | ||
| Multipara | 0.45 (0.38 to 0.53) | 0.000 | 0.46 (0.34 to 0.62) | 0.000 |
| Grandmultipra | 0.42 (0.35 to 0.51) | 0.000 | 0.31 (0.21 to 0.47) | 0.000 |
| Antenatal care follow-up | ||||
| Yes | 1 | 1 | ||
| No | 1.79 (1.54 to 2.09) | 0.000 | 1.67 (1.29 to 2.17) | 0.000 |
| Child sex | ||||
| Male | 1 | 1 | ||
| Female | 3.24 (2.76 to 3.81) | 0.000 | 0.82 (0.66 to 1.02) | 0.073 |
| Newborn weight at birth | ||||
| Normal | 1 | 1 | ||
| Small | 3.63 (2.79 to 4.72) | 0.000 | 3.98 (3.04 to 5.20) | 0.000 |
| Large | 1.40 (1.01 to 1.95) | 0.041 | 2.51 (1.76 to 3.57) | 0.000 |
Bold: significant at p-value <0.05
AOR, adjusted odds ratio; COR, crude odds ratio.
Discussions
The perinatal mortality among the population of Kersa HDSS of Eastern Ethiopia was 26.72 deaths per 1000 births which is high as compared with other studies in Ethiopia; North Shewa (16.5 deaths per 1000 deaths),16 and Tigray region of Ethiopia (6.2 deaths per 1000 deaths).28 However, this finding is lower than the recent reports from Ethiopian demographic and health survey and longitudinal study from northwest Ethiopia.19 29 Meta-analysis study conducted in eastern Africa presents higher perinatal mortality rate (34.5 per 1000 births) than the finding of this study.6 This discrepancy may be due to differences in study design, study period and socioeconomic characteristics of study participants.
The perinatal mortality in the study area has decreased from 32.96/1000 births in 2015 to 22.09/1000 births in 2020, with a slightly fluctuating trend. This positive change could be attributed to the success of millennium development goals (MDG Goal 4)30 and it also helps as a good indicator for tracking the progress of post-MDGs agenda; SDGs.8
The odds of perinatal mortality were higher among those from rural residence than those from urban settings. This finding is supported by the studies conducted in Ethiopia31 and Brazil.15 This might be related to longer physical distance and lack of transportation that delays using timely and appropriate emergency obstetrics care like ANC, delivery and PNCs.32–34
The odds of perinatal mortality were lower for multipara and grand multipara mothers compared with the primipara mothers. This finding is supported by meta-analysis study that depicts higher odds of perinatal mortality among primipara mothers.35 Study conducted in rural Uganda also showed a decline in risk of stillbirth as parity increases.36 This may be due to pregnancy complications such as fetal distress, preterm labour and obstructed labour that are more common in primigravid pregnancy.37
The odds of perinatal mortality were higher among mothers who did not have ANC follow-up. This finding is in line with studies conducted in Sudan, Uganda and Ethiopia.16 38–40 This could be related to absence of birth preparedness, complication readiness and counselling on optimal infant feeding during ANC,41 and lack of universal access to safe, affordable, and timely skilled birth attendants.42–44 The utilisation of ANC would have a significant impact on perinatal outcome and would be an important strategy to incorporate in planning initiatives aimed at reducing the perinatal mortality. Identifying the barriers, which affect utilisation of ANC visits, might be important to implement strategies. The WHO recommended eight or more contacts for ANC to reduce perinatal deaths by 8 per 1000 births.45
Neonate born with small and large birth weight had higher odds of perinatal mortality compared with neonate born with normal birth weight. This finding is supported by the studies done in northern and Eastern Ethiopia.46 47 Neonates with small birth weight might have neurodevelopmental and growth impairment, and for those with large birth weight the risk of obstructed labour increases which result may result in birth injury and perinatal mortality. The increased odds of perinatal mortality among small birth weight might be related to preterm gestational age that associated to lung immaturity causing low surfactant production to air the lung of the neonates during extra uterine life.48–51
The high rate of perinatal mortality pinpoints the need to reducing perinatal deaths to meet global and national targets of reducing perinatal and child mortality. Acting on the identified factors may reverse the high level of perinatal mortality. Moreover, active surveillance system for tracking any fetal or neonatal deaths at community and health facility level may contribute to the reduction of perinatal deaths and identification of the cause of deaths.
Strengths and limitations of the study
The study used prospectively collected data over the period of 6 years. However, the study was not without limitations. Medical, obstetric factors and maternal nutritional status of the mother were not well addressed. Maternal report about size at birth may result in some misclassification due to recall bias or subjective assessment. Moreover; the perinatal mortality was only captured after the death had occurred as the result difficult to determine the causes. Therefore, in interpreting the findings of this study one should take into account the mentioned limitations.
Conclusions
The study revealed perinatal mortality in the study area was relatively high. Place of residence, ANC, parity and birth weight were identified as predictors of perinatal mortality. Devising strategies that enhance access to and utilisations of ANC services with due emphasis for rural residents, primipara mothers and newborn with low and big birth weights may be crucial for reducing perinatal mortality.
Supplementary Material
Acknowledgments
The authors are thankful to Haramaya University for giving us permission to access the data. We are also grateful to collectors for their genuine effort to bring reliable data and participants for their participation.
Footnotes
Contributors: MD, GD, GF, BTM and BB contributed to the conception of the paper, study design, data collection, analysis and writing up. GMA, BN, TBR, YD and AA contributed to the study design, data processing and analysis and contributed to all drafts of the paper. All authors have agreed on the journal to which the article will be submitted, gave their final approval for submission and the version to be published, and agreed to be accountable for all aspects of the work. MD and BTM are guarantors
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available upon reasonable request. The datasets used in this study can be available from Kersa Demographic and Health Surveillance System (http://www.indepth-network.org/member-centres/kersa-0) up on reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by Haramaya University College of health and medical science and institutional health research ethical review committee (IHRERC) with reference number of Ref. No. IHRERC/27/11/2014. Participants gave informed consent to participate in the study before taking part.
References
- 1.Bakketeig LS, Bergsjø P, Epidemiology P. International encyclopedia of public health. Oxford: Academic Press, 2008: 45–53. [Google Scholar]
- 2.Madaj B, Smith H, Mathai M, et al. Developing global indicators for quality of maternal and newborn care: a feasibility assessment. Bull World Health Organ 2017;95:445–52. 10.2471/BLT.16.179531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.EMI SUZUKI HK . A neglected burden: the global tragedy of stillbirths stillbirths: report of the un Inter-Agency group for child mortality estimation, 2020. Available: https://blogs.worldbank.org/opendata/first-ever-un-report-global-stillbirths-reveals-enormous-and-neglected-toll
- 4.Wang H, Bhutta ZA, Coates MM, et al. Global, regional, National, and selected subnational levels of stillbirths, neonatal, infant, and under-5 mortality, 1980-2015: a systematic analysis for the global burden of disease study 2015. Lancet 2016;388:1725–74. 10.1016/S0140-6736(16)31575-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Estimation UNIGfCM . Levels & Trends in Child Mortality: Report 2017: Estimates Developed by the UN Inter-Agency Group for Child Mortality Estimation. United Nations Children’s Fund, 2017. [Google Scholar]
- 6.Akombi BJ, Renzaho AM. Perinatal mortality in sub-Saharan Africa: a meta-analysis of demographic and health surveys. Ann Glob Health 2019;85. 10.5334/aogh.2348. [Epub ahead of print: 12 07 2019]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Central Statistical Agency E . Ethiopia demographic and health survey 2016. Addis Ababa, Ethiopia, and Rockville, Maryland, USA: CSA and ICF, 2016. [Google Scholar]
- 8.Assembly UG. Sustainable development goals (SDGs), transforming our world: the, 2030. United Nations New York, 2015. [Google Scholar]
- 9.Say L, Raine R. A systematic review of inequalities in the use of maternal health care in developing countries: examining the scale of the problem and the importance of context. Bull World Health Organ 2007;85:812–9. 10.2471/BLT.06.035659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Haddrill R, Jones GL, Mitchell CA, et al. Understanding delayed access to antenatal care: a qualitative interview study. BMC Pregnancy Childbirth 2014;14:1–14. 10.1186/1471-2393-14-207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.EDHS . Ethiopia demographic and health survey. Available: https://dhsprogram.com/pubs/pdf/FR328/FR328.pdf [Accessed 21 Oct 2020].
- 12.Roro EM, Sisay MM, Sibley LM. Determinants of perinatal mortality among cohorts of pregnant women in three districts of North Showa zone, Oromia region, Ethiopia: community based nested case control study. BMC Public Health 2018;18:1–11. 10.1186/s12889-018-5757-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Andegiorgish AK, Andemariam M, Temesghen S, et al. Neonatal mortality and associated factors in the specialized neonatal care unit Asmara, Eritrea. BMC Public Health 2020;20:1–9. 10.1186/s12889-019-8118-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yemisrach G, Mesganaw F. Factors associated with perinatal mortality among public health deliveries in Addis Ababa, Ethiopia, an unmatched case control study. BMC Pregnancy Childbirth 2017;17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kassar SB, Melo AMC, Coutinho SB, et al. Determinants of neonatal death with emphasis on health care during pregnancy, childbirth and reproductive history. J Pediatr 2013;89:269–77. 10.1016/j.jped.2012.11.005 [DOI] [PubMed] [Google Scholar]
- 16.Roro EM, Sisay MM, Sibley LM. Determinants of perinatal mortality among cohorts of pregnant women in three districts of North Showa zone, Oromia region, Ethiopia: community based nested case control study. BMC Public Health 2018;18:888. 10.1186/s12889-018-5757-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gardosi J, Clausson B, Francis A. The value of customised centiles in assessing perinatal mortality risk associated with parity and maternal size. BJOG 2009;116:1356–63. 10.1111/j.1471-0528.2009.02245.x [DOI] [PubMed] [Google Scholar]
- 18.Chinkhumba J, De Allegri M, Muula AS, et al. Maternal and perinatal mortality by place of delivery in sub-Saharan Africa: a meta-analysis of population-based cohort studies. BMC Public Health 2014;14:1–9. 10.1186/1471-2458-14-1014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yadeta TA, Mengistu B, Gobena T, et al. Spatial pattern of perinatal mortality and its determinants in Ethiopia: data from Ethiopian demographic and health survey 2016. PLoS One 2020;15:e0242499. 10.1371/journal.pone.0242499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Network EURC . Trends and causes of perinatal death in Ethiopia, 2010-2014, 2016. [Google Scholar]
- 21.CSA I . Key indicators: mini demographic and health survey, 2019. [Google Scholar]
- 22.Assefa N, Lakew Y, Belay B, et al. Neonatal mortality and causes of death in Kersa health and demographic surveillance system (Kersa HDSS), Ethiopia, 2008-2013. Matern Health Neonatol Perinatol 2016;2:7. 10.1186/s40748-016-0035-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Assefa N, Oljira L, Baraki N, et al. HDSS profile: the kersa health and demographic surveillance system. Int J Epidemiol 2016;45:94–101. 10.1093/ije/dyv284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Organization WH . Neonatal and perinatal mortality: country, regional and global estimates. World Health Organization, 2006. [Google Scholar]
- 25.Kassaw MW, Abebe AM, Kassie AM, et al. Trends of proximate low birth weight and associations among children under-five years of age: evidence from the 2016 Ethiopian demographic and health survey data. PLoS One 2021;16:e0246587. 10.1371/journal.pone.0246587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Opara EI, Zaidi J. The interpretation and clinical application of the word 'parity': a survey. BJOG 2007;114:1295–7. 10.1111/j.1471-0528.2007.01435.x [DOI] [PubMed] [Google Scholar]
- 27.Organization WH . Making pregnancy safer: the critical role of the skilled attendant: a joint statement by WHO, ICM and FIGO. World health organization, 2004. [Google Scholar]
- 28.Woldeamanuel BT, Gelebo KK. Statistical analysis of socioeconomic and demographic correlates of perinatal mortality in Tigray region, Ethiopia: a cross sectional study. BMC Public Health 2019;19:1301. 10.1186/s12889-019-7642-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Andargie G, Berhane Y, Worku A, et al. Predictors of perinatal mortality in rural population of northwest Ethiopia: a prospective longitudinal study. BMC Public Health 2013;13:1–7. 10.1186/1471-2458-13-168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Haileamlak A. Ethiopia successfully attaining the millennium development goals. Ethiop J Health Sci 2015;25:109–10. 10.4314/ejhs.v25i2.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tesfaye Assebe Y, Bizatu M, Tesfaye G. Spatial pattern of perinatal mortality and its determinants in Ethiopia: data from Ethiopian demographic and health survey 2016. PLoS ONE 2020;15. 10.1371/journal.pone.0242499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Girmatsion F, Berhane Yemane A, Alemayehu W. Distance from health facility and mothers’ perception of quality related to skilled delivery service utilization in northern Ethiopia. Int J Womens Health 2017. 10.2147/IJWH.S140366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Keyes EB, Haile-Mariam A, Belayneh NT, et al. Ethiopia's assessment of emergency obstetric and newborn care: setting the gold standard for national facility-based assessments. Int J Gynaecol Obstet 2011;115:94–100. 10.1016/j.ijgo.2011.07.009 [DOI] [PubMed] [Google Scholar]
- 34.Martins MCF, Feitosa FEdeL, Viana Júnior AB, et al. Pregnancies with an outcome of fetal death present higher risk of delays in obstetric care: a case-control study. PLoS One 2019;14:e0216037. 10.1371/journal.pone.0216037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Berhan Y, Berhan A. A meta-analysis of selected maternal and fetal factors for perinatal mortality. Ethiop J Health Sci 2014;24 Suppl:55–68. 10.4314/ejhs.v24i0.6S [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Asiki G, Baisley K, Newton R, et al. Adverse pregnancy outcomes in rural Uganda (1996–2013): trends and associated factors from serial cross sectional surveys. BMC Pregnancy Childbirth 2015;15:1–12. 10.1186/s12884-015-0708-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hoque M. Incidence of obstetric and foetal complications during labor and delivery at a community health centre, midwives obstetric unit of Durban, South Africa. ISRN Obstet Gynecol 2011;2011:1–6. 10.5402/2011/259308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ali AAA, Elgessim ME, Taha E, et al. Factors associated with perinatal mortality in Kassala, eastern Sudan: a community-based study 2010-2011. J Trop Pediatr 2014;60:79–82. 10.1093/tropej/fmt075 [DOI] [PubMed] [Google Scholar]
- 39.Nankabirwa V, Tumwine JK, Tylleskär T, et al. Perinatal mortality in eastern Uganda: a community based prospective cohort study. PLoS One 2011;6:e19674. 10.1371/journal.pone.0019674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tilahun D, Assefa T. Incidence and determinants of stillbirth among women who gave birth in Jimma university specialized Hospital, Ethiopia. Pan Afr Med J 2017;28:299. 10.11604/pamj.2017.28.299.1269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Anikwe CC, Okorochukwu BC, Ikeoha CC, et al. Birth preparedness and complication readiness among pregnant women in a secondary health facility in Abakaliki, Ebonyi state, Nigeria. Biomed Res Int 2020;2020:1–12. 10.1155/2020/9097415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Darby A. “Delayed Breastfeeding Initiation Increases Risk of Neonatal Mortality”(2006), by Karen Edmond Charles Zandoh, Maria Quigley, Seeba Amenga-Etego, Seth Oqusi-Agyei, and Betty Kirkwood. Embryo Project Encyclopedia 2019. [DOI] [PubMed] [Google Scholar]
- 43.Echoka E, Dubourg D, Makokha A, et al. Using the unmet obstetric needs indicator to map inequities in life-saving obstetric interventions at the local health care system in Kenya. Int J Equity Health 2014;13:1–9. 10.1186/s12939-014-0112-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.James K, Borchem I, Talo R, et al. Universal access to safe, affordable, timely surgical and anaesthetic care in Papua New Guinea: the six global health indicators. ANZ J Surg 2020;90:1903–9. 10.1111/ans.16148 [DOI] [PubMed] [Google Scholar]
- 45.Organization WH . WHO recommendations on antenatal care for a positive pregnancy experience. World Health Organization, 2016. [PubMed] [Google Scholar]
- 46.Eyeberu A, Shore H, Getachew T, et al. Neonatal mortality among neonates admitted to NICU of Hiwot Fana specialized university Hospital, eastern Ethiopia, 2020: a cross-sectional study design. BMC Pediatr 2021;21:125. 10.1186/s12887-021-02598-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gebreheat G, Tsegay T, Kiros D, et al. Prevalence and associated factors of perinatal asphyxia among neonates in general hospitals of Tigray, Ethiopia, 2018. Biomed Res Int 2018;2018:1–7. 10.1155/2018/5351010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Schürch D, Ospina OL, Cruz A, et al. Combined and independent action of proteins SP-B and SP-C in the surface behavior and mechanical stability of pulmonary surfactant films. Biophys J 2010;99:3290–9. 10.1016/j.bpj.2010.09.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chakraborty M, Kotecha S. Pulmonary surfactant in newborn infants and children. Breathe 2013;9:476–88. 10.1183/20734735.006513 [DOI] [Google Scholar]
- 50.Han S, Mallampalli RK. The role of surfactant in lung disease and host defense against pulmonary infections. 12, 2015: 765–74. 10.1513/AnnalsATS.201411-507FR [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Perez-Gil J, Weaver TE. Pulmonary surfactant pathophysiology: current models and open questions. Physiology 2010;25:132–41. 10.1152/physiol.00006.2010 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available upon reasonable request. The datasets used in this study can be available from Kersa Demographic and Health Surveillance System (http://www.indepth-network.org/member-centres/kersa-0) up on reasonable request.