Abstract
The circle of Willis (CoW) is an anastomotic arterial network located on the base of the brain. Studies have shown that it demonstrates considerable anatomical variation in humans. This systematic review aimed to identify and catalogue the described anatomical variations of the CoW in humans to create a new, comprehensive variation classification system. An electronic literature search of five databases identified 5899 studies. A two‐phase screening process was performed, and studies underwent quality assessment. A total of 42 studies were included in the review. Data were extracted and circles were reconstructed digitally using graphics software. The classification system contains 82 CoW variations in five continuous groups. Group one contains 24 circles with one or more hypoplastic segments only. Group two contains 11 circles with one or more absent segments only. Group three contains 6 circles with hypoplastic and absent segments only. Group four contains 26 circles with one or more accessory segments. Group five contains 15 circles with other types of anatomical variation. Within each group, circles were subcategorised according to the number or type of segments affected. An original coding system was created to simplify the description of anatomical variations of the CoW. The new classification system provides a comprehensive ontology of the described anatomical variations of the CoW in humans. When used with the coding system, it allows the description and categorisation of recorded and unrecorded variants identified in past and future studies. It is applicable to current clinical practice and the anatomical community, including human anatomy education and research.
Keywords: cerebrovascular anatomy, classification, neuroanatomy, variation
The classification system provides a comprehensive ontology of the described anatomical variations of the circle of Willis in humans. Group one contains 24 circles with one or more hypoplastic segments only. Group two contains 11 circles with one or more absent segments only. Group three contains six circles with hypoplastic and absent segments only. Group four contains 26 circles with one or more accessory segments. Group five contains 15 circles with other types of anatomical variation.

1. INTRODUCTION
The circle of Willis (CoW) is an anastomotic arterial network located on the base of the brain. It functions to prevent cerebral and cerebellar ischaemia by maintaining tissue perfusion given an impaired or decreased blood flow through one or more of its component vessels (Hartkamp et al., 1999; Kapoor et al., 2008).
The CoW is divided into two sections. The anterior communicating artery (AComA) and A1 segments of the anterior cerebral arteries (A1) form the anterior half of the circle (Gray, 2016; Moore et al., 2014). The posterior communicating arteries (PComA) and P1 segments of the posterior cerebral arteries (P1) form the posterior half of the circle (Gray, 2016; Moore et al., 2014). The arteries create a symmetrical polygonal‐shaped connection between the internal carotid and vertebrobasilar systems.
Four criteria are classically used to define ‘normal’ (non‐variant) anatomy of the CoW: (1) all segments (AComA, A1s, PComAs and P1s) are present (De Silva et al., 2011; Eftekhar et al., 2006; Kapoor et al., 2008; Klimek‐Piotrowska et al., 2015; Vasović et al., 2013), (2) all segments arise from their natural origins (De Silva et al., 2011; Kapoor et al., 2008; Klimek‐Piotrowska et al., 2015), (3) no accessory arteries are present (De Silva et al., 2011; Kapoor et al., 2008; Klimek‐Piotrowska et al., 2015; Vasović et al., 2013), and (4) all segments have an external diameter of >1 mm (De Silva et al., 2011; Kapoor et al., 2008; Klimek‐Piotrowska et al., 2013, 2015; Vasović et al., 2013).
The prevalence of anatomical variation of the CoW in the neurologically healthy human population is estimated to be 68.22 ± 14.32% (Jones et al., 2020). For this review, anatomical variation was defined using two criteria: (1) the variation is embryologically derived, and (2) the variation does not demonstrate the potential to directly progress to a pathological consequence. Commonly recorded variation types include hypoplasia (Cilliers et al., 2018; De Silva et al., 2011; Eftekhar et al., 2006), absence (Hafez et al., 2007; Klimek‐Piotrowska et al., 2013; Li et al., 2020), and duplication (Iqbal, 2013; Klimek‐Piotrowska et al., 2015). The most common variant segment is the posterior communicating artery (Eftekhar et al., 2006; Hindenes et al., 2020; Klimek‐Piotrowska et al., 2015).
An awareness of the anatomical variations of the CoW is important for clinical practice (Jones et al., 2020; Raikos & Smith, 2015). Circle variation is associated with an increased risk of a number of cerebrovascular diseases (Henry et al., 2015; Oumer et al., 2021; Ryan et al., 2015; Stojanović et al., 2019), and affects patient response to therapeutic intervention (Leng et al., 2016; Wufuer et al., 2017). It has implications for preoperative planning and is important in selecting the most appropriate method of cerebral protection (Papantchev et al., 2013). Anatomical variation influences a range of intraoperative factors which determine patient outcome and increases the risk of misinterpretation and surgical error. Despite this, there is lack of consensus in the literature on a system that comprehensively documents and classifies such variations.
Three classification systems are commonly used to categorise anatomical variations of the CoW in humans. The Riggs classification system (Riggs & Rupp, 1963) contains 21 variations. Circle order in this classification has no relation to anatomy, only segment hypoplasia is included, and complete anatomical descriptions are not provided. No single diagram of the included circles is available. In contrast, the Lazorthes classification system (Lazorthes et al., 1979) contains 22 variations. Here, only segment hypoplasia is included, and circle order has no relation to anatomy. The illustration of segment hypoplasia is inconsistent, creating ambiguity regarding the anatomy of variation numbers five, seven, eight, 13 and 17 (Lazorthes et al., 1979). Finally, the Krabbe‐Hartkamp classification system (Krabbe‐Hartkamp et al., 1998) contains 18 variations. Complete circle anatomy is not shown, and artery hypoplasia and absence are not differentiated.
Four studies (De Silva et al., 2011; Eftekhar et al., 2006; Klimek‐Piotrowska et al., 2015; Vasović et al., 2013) assert that Riggs (Riggs & Rupp, 1963) and Lazorthes (Lazorthes et al., 1979) describe, and include in their classification systems, a variant circle with a hypoplastic AComA, a unilateral hypoplastic A1 and an ipsilateral hypoplastic PComA. However, both classification systems (Lazorthes et al., 1979; Riggs & Rupp, 1963) contain a circle with a unilateral hypoplastic A1 and an ipsilateral hypoplastic PComA without a hypoplastic AComA. As such, Riggs (Riggs & Rupp, 1963) and Lazorthes (Lazorthes et al., 1979) classification systems have been incorrectly used throughout the literature. Interestingly, no study in this review, nor those aforementioned, has recorded a circle with a hypoplastic AComA, a unilateral hypoplastic A1 and an ipsilateral hypoplastic PComA. In view of this lack of consensus in the literature, a recent review (Jones et al., 2020) on the prevalence of anatomical variation of the CoW recommended the development of a new, comprehensive classification system.
This article, therefore, presents a systematic review of published empirical research on anatomical variation of the CoW in humans, performed with the following aims: (1) to identify and catalogue the described anatomical variations of the CoW in humans, and (2) to characterise the described variants to produce a new, comprehensive classification system.
2. METHODS
The review was conducted according to the recommendations set out in the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) statement (Shamseer et al., 2015).
A systematic search of the published peer‐reviewed literature was conducted on the Ovid Medline (1946 to May 27, 2020), Ovid Embase (1974 to May 27, 2020), Web of Science Core Collection (all years 1900–2020), Scopus and The Cochrane Library databases on 27 May 2020. The search strategy was made up of two sections. The first section contained alternative terms for ‘circle of Willis’ and its component arteries. The second section contained synonyms of the term ‘variation’ used in anatomical description. The strategy was adapted to each database to increase search sensitivity (Table 1). No limitations on language or publication format were applied.
TABLE 1.
The search strategies
| Database | Search strategy |
|---|---|
| Ovid Medline (1946 to May 27, 2020) |
(exp “Circle of Willis”/OR circle of Willis OR cerebral arterial circle OR circulus arteriosus cerebri OR circulus arteriosus Willis* OR circulus Willis* OR Willis* circle OR Willis* polygon OR exp Anterior Cerebral Artery/OR anterior cerebral arter* OR arteria cerebri anterior OR exp PCA/OR posterior cerebral arter* OR arteria cerebri posterior OR anterior communicating arter* OR arteria communicans anterior OR posterior communicating arter* OR arteria communicans posterior) AND (exp Anatomic Variation/OR varia* OR anomal* OR abnormal* OR atypical OR incomplete OR unusual) |
| Ovid Embase (1974 to May 27, 2020) |
(exp brain circulus arteriosus/OR circle of Willis OR cerebral arterial circle OR circulus arteriosus cerebri OR circulus arteriosus Willis* OR circulus Willis* OR Willis* polygon OR Willis* circle OR exp anterior cerebral artery/ OR anterior cerebral arter* OR arteria cerebri anterior OR exp PCA/OR posterior cerebral arter* OR arteria cerebri posterior OR exp anterior communicating artery/ OR anterior communicating arter* OR arteria communicans anterior OR exp posterior communicating artery/OR posterior communicating arter* OR arteria communicans posterior) AND (exp anatomic variation/OR varia* OR anomal* OR abnormal* OR atypical OR incomplete OR unusual) |
| Web of Science Core Collection (all years 1900–2020) |
(TS = (“circle of Willis” OR “cerebral arterial circle” OR “circulus arteriosus cerebri” OR “circulus arteriosus Willis*” OR “circulus Willis*” OR “Willis* polygon” OR “Willis* circle” OR “anterior cerebral arter*” OR “arteria cerebri anterior” OR “posterior cerebral arter*” OR “arteria cerebri posterior” OR “anterior communicating arter*” OR “arteria communicans anterior” OR “posterior communicating arter*”)) AND (TS = (“varia*” OR “abnormal*” OR “anomal*” OR “atypical” OR “incomplete” OR “unusual”)) |
| Scopus |
(TITLE‐ABS‐KEY(“circle of Willis” OR “cerebral arterial circle” OR “circulus arteriosus cerebri” OR “circulus arteriosus Willis*” OR “circulus Willis*” OR “Willis* polygon” OR “Willis* circle” OR “anterior cerebral arter*” OR “arteria cerebri anterior” OR “posterior cerebral arter*” OR “arteria cerebri posterior” OR “anterior communicating arter*” OR “arteria communicans anterior” OR “posterior communicating arter*” OR “arteria communicans posterior”)) AND (TITLE‐ABS‐KEY(“varia*” OR “abnormal*” OR “anomal*” OR “atypical” OR “incomplete” OR “unusual”)) |
| The Cochrane Library |
(exp Circle of Willis/ OR circle of Willis OR cerebral arterial circle OR circulus arteriosus Willis* OR circulus Willis* OR Willis* circle OR exp Anterior Cerebral Artery/OR anterior cerebral arter* OR arteria cerebri anterior OR exp PCA/OR posterior cerebral arter* OR anterior communicating arter* OR posterior communicating arter*) AND (exp Anatomic Variation/OR varia* OR anomal* OR abnormal* OR atypical OR incomplete OR unusual) |
2.1. Screening process
Following deduplication, studies underwent a two‐phase screening process against inclusion and exclusion criteria (Table 2). In phase one, titles and abstracts were screened against criteria In1, In5, and Ex1‐5. Criteria In2, 3, 4 and 6 were not applied as titles and abstracts provided insufficient evidence to inform decisions on their fulfilment. For studies meeting all inclusion criteria and no exclusion criteria, full texts were sought, and English translations obtained when freely available.
TABLE 2.
The inclusion and exclusion criteria
| Inclusion criteria | Exclusion criteria |
|---|---|
|
|
In phase two, full texts were screened against all inclusion and exclusion criteria. To meet criterion In2, studies were required to describe or illustrate the anatomy of the AComA, A1 segments, PComAs and P1 segments of the variant circle. To meet criterion In4, studies were required to describe or illustrate the type of variation identified. Angiographic studies which did not differentiate between artery hypoplasia and absence were excluded. This included the Krabbe‐Hartkamp classification (Krabbe‐Hartkamp et al., 1998). Studies meeting one or more exclusion criteria were removed, while studies with one or more circles meeting all inclusion criteria were included in the review. Two independent reviewers screened two random samples of 15 studies using the inclusion and exclusion criteria. No difference to the original study selection was found.
2.2. Data extraction
Data were extracted on the background of the study (first author and publication year), its characteristics (location, design, population, modality, and definition of hypoplasia), and its description of variant circles (variant segment(s), variation type(s), position of the variation, and the number of different variant circles).
2.3. Quality assessment
A bespoke quality assessment tool was created, adapting the modified Anatomical Quality Assessment Tool (Henry et al., 2017) and Critical Appraisal Skills Programme Checklist for Case‐Control and Cohort Studies (Critical Appraisal Skills Programme, 2018a, 2018b) criteria. Case‐control, cohort and cross‐sectional studies underwent quality assessment. Case studies and case series were not assessed as the tool was incompatible with the study types. The quality assessment tool is shown in Table S1.
Seven study domains were scored: clearly defined and focused aim(s), appropriate study design, representative population characteristics, reproducible methodology, clarity of descriptive anatomy, accuracy in reporting of results, and acknowledgement of limitations. A quality threshold score was subjectively determined. Studies scoring ≥14 out of 25 were considered high quality, while studies scoring <14 out of 25 were considered low quality. Studies were not excluded from the review on the basis of quality score.
2.4. Data synthesis
The circles were reconstructed digitally using Paint 3D (Microsoft Corporation, 6.2003.4017.0). A1 and P1 segments were drawn using the 4‐point curve tool at 11 px (pixel). The AComA and PComAs were drawn using the 2‐point line tool at 7 px. Internal carotid and middle cerebral arteries, drawn using the 2‐point line tool at 18 px, were included for anatomical completeness. Artery hypoplasia was shown by line width conversion to 1 px.
The left‐right orientation of variant segments is rarely reported within the literature. For standardisation, the most anterior variation was drawn on the right side of the circle.
The circles were grouped according to variation type. Within each group, circles were subcategorised according to the number or type of variant segment. A coding system was created to simplify anatomical description of the circles.
3. RESULTS
A summary of the study selection process is shown in Figure 1. The search identified 14,437 studies. After removal of 8538 duplicates, 5899 studies underwent title and abstract screening, of which 5375 did not meet the assessed criteria. Of the resulting 524 studies, 29 full texts were unobtainable. The remaining 495 studies underwent full‐text screening. A total of 42 studies were included in the review.
FIGURE 1.

A flow diagram summarising the study selection process
3.1. Study characteristics and results
A summary of the study characteristics and results is shown in Table 3. Studies were published between 1903 and 2020. Five different study designs were used: cross‐sectional (n = 19), case report (n = 17), case‐control (n = 2), case series (n = 2) and prospective cohort (n = 2). The study locations spanned Asia (n = 15), Europe (n = 14), North America (n = 9), Africa (n = 3) and South America (n = 1). A range of investigative modalities were used: cadaveric dissection (n = 22), computed tomography angiography (n = 4), digital subtraction angiography (n = 3) and magnetic resonance angiography with or without 3D time‐of‐flight capability (n = 15). Three studies used two investigative modalities and one study used cerebral cast angiography.
TABLE 3.
A table showing the characteristics and results of studies included in the review
| Study code | Study | Study location | Study design (study population [n]) | Study modality | Definition of artery hypoplasia | Distinct variants (n) | Quality assessment score (n/25) |
|---|---|---|---|---|---|---|---|
| S1 | Al‐Hussain et al. (2001) | Jordan | CSS (50) | CD | <1 mm | 4 | 11 |
| S2 | Benson et al. (1986) | Canada | CR (1) | CD | N/A | 1 | N/A |
| S3 | Cilliers et al. (2018) | South Africa | CSS (59) | CD | <1 mm | 10 | 15 |
| S4 | De Silva et al. (2011) | Sri Lanka | CSS (225) | CD | <1 mm | 15 | 18 |
| S5 | Ding et al. (2019) | China | CR (1) | CD | N/A | 1 | N/A |
| S6 | Drummond et al. (2006) | USA | CR (1) | TOF MRA | N/A | 1 | N/A |
| S7 | Drummond et al. (2012) | USA | CR (1) | TOF MRA | N/A | 1 | N/A |
| S8 | Eftekhar et al. (2006) | Iran | CSS (102) a | CD | <1 mm | 10 | 15 |
| S9 | Giglio et al. (2010) | Italy | CR (1) | MRA | N/A | 1 | N/A |
| S10 | Gurdal et al. (2004) | Turkey | CR (2) | CD | N/A | 2 | N/A |
| S11 | Hafez et al. (2007) | Egypt | CSS (130) | 3D TOF MRA and CD | <1 mm | 7 | 11 |
| S12 | Hashemi et al. (2013) | Iran | CSS (200) | CD | <1 mm | 9 | 12 |
| S13 | He et al. (2016) | China | PCS (102) | CTA | <1 mm | 1 | 15 |
| S14 | Howe (1903) | USA | CR (1) | CD | N/A | 1 | N/A |
| S15 | Howie (1959) | USA | CCS (256) | CD | N/A | 10 | 4 |
| S16 | Ibrahim et al. (2017) | Sudan | CCS (146) | 3D TOF MRA | N/A | 5 | 10 |
| S17 | Iqbal (2013) | India | CSS (50) | CD | <1 mm (AComA and PComA <0.5 mm) | 5 | 13 |
| S18 | Jensen et al. (2017) | USA | CR (1) | DSA | N/A | 1 | N/A |
| S19 | Karatas et al. (2016) | Turkey | CSS (100) | CD | N/A | 2 | 14 |
| S20 | Klimek‐Piotrowska et al. (2013) | Poland | CSS (250) | CTA | N/A | 3 | 14 |
| S21 | Klimek‐Piotrowska et al. (2015) | Poland | CSS (100) | CD | <1 mm | 30 | 17 |
| S22 | Li et al. (2020) | China | CSS (819) | 3D TOF MRA and DSA | <1 mm | 7 | 16 |
| S23 | Loh and Sharma (2010) | Singapore | CR (1) | TOF MRA | N/A | 1 | N/A |
| S24 | Malamateniou et al. (2009) | UK | CSS (103) | 3D TOF MRA | N/A | 3 | 18 |
| S25 | Manninen et al. (2009) | Finland | CSS (92) | Cerebral cast angiography | N/A | 1 | 19 |
| S26 | Matsuda et al. (2017) | Japan | CR (1) | MRA | N/A | 1 | N/A |
| S27 | McCullough (1962) | USA | CS (77) | CD | N/A | 4 | N/A |
| S28 | Ozturk et al. (2008) | Turkey | CR (1) | CD | N/A | 1 | N/A |
| S29 | Papantchev et al. (2007) | Bulgaria | CSS (112) | CD | <1 mm | 3 | 12 |
| S30 | Papantchev et al. (2013) | Bulgaria | CSS (500) | CD and CTA | <1 mm | 6 | 16 |
| S31 | Riggs and Rupp (1963) | USA | CSS (994) | CD | N/A | 20 | 7 |
| S32 | Sabau et al. (2012) | Romania | CR (1) | 3D TOF MRA | N/A | 1 | N/A |
| S33 | Saikia et al. (2014) | India | CSS (70) | TOF MRA | <1 mm | 2 | 14 |
| S34 | Saphir (1935) | USA | CR (3) | CD | N/A | 3 | N/A |
| S35 | Sonobe et al. (2019) | Japan | CR (1) | MRA | N/A | 1 | N/A |
| S36 | Sonobe et al. (2020) | Japan | CR (1) | MRA | N/A | 1 | N/A |
| S37 | Stefani et al. (2013) | Brazil | CSS (30) | MRA | N/A | 4 | 14 |
| S38 | Tripathi et al. (2003) | India | CR (1) | DSA | N/A | 1 | N/A |
| S39 | Uchino et al. (2015) | Japan | CR (2) | 3D TOF MRA | N/A | 2 | N/A |
| S40 | Urbanski et al. (2008) | Germany | PCS (99) | CTA | N/A | 4 | 12 |
| S41 | Vasović et al. (2010) | Serbia | CS (4) | CD | N/A | 2 | N/A |
| S42 | Vasović et al. (2013) | Serbia | CSS (333) | CD | <1 mm | 11 | 11 |
Abbreviations: CCS, case‐control study; CD, cadaveric dissection; CR, case report; CS, case series; CSS, cross‐sectional study; CTA, computed tomography angiography; DSA, digital subtraction angiography; ICoA, intermediate communicating artery; MRA, magnetic resonance angiography; N/A, not available; P1c, P1 segment of carotid origin; PCS, prospective cohort study; TOF, time‐of‐flight.
Results of only 92 out of 102 participants were recorded.
Artery hypoplasia was defined as a diameter <1 mm in 13 studies. 28 studies did not provide a definition, of which 17 identified a circle with one or more hypoplastic arteries. One study defined AComA and PComA hypoplasia as a diameter <0.5 mm. Of the 199 extracted variants, 117 were duplicates. A total of 82 distinct variations of the CoW were recorded.
3.2. Quality assessment results
Excluding case reports and case series, 23 studies underwent quality assessment. Cross‐sectional, case‐control and prospective cohort studies were reviewed using the quality assessment tool. Thirteen studies were considered high quality, scoring ≥14 out of 25. Ten studies were considered low quality, scoring <14 out of 25. Individual quality assessment scores are shown in Table 3.
3.3. Variation coding system
A coding system was created to simplify anatomical description of variations of the CoW. Symbols, used to abbreviate anatomical descriptors, were inserted into relevant sections of an original formula to generate a descriptive code. The symbols are listed in Table 4.
TABLE 4.
A table showing the anatomical descriptors and their symbols
| Descriptor | Symbol |
|---|---|
| Section one (anatomical relationship) | |
| Bilateral | B |
| Ipsilateral | I |
| Contralateral | C |
| Section two (artery) | |
| Anterior communicating artery | ACOMA |
| Anterior cerebral artery | ACA |
| A1 segment | A1 |
| A2 segment | A2 |
| A1/A2 junction | A1/A2 |
| Posterior communicating artery | PCOMA |
| Posterior cerebral artery | PCA |
| P1 segment | P1 |
| P2 segment | P2 |
| Intermediate communicating artery | ICOA |
| P1 segment of carotid origin | P1C |
| Section three (variation type) | |
| Absent | A |
| Azygous | Az |
| Duplicated | D |
| Elongated | E |
| Fenestrated | F |
| Hypoplastic | H |
| Plexiform | P |
| Triplicated | T |
| Triplicated (medial) | Tm |
| Triplicated (lateral) | Tl |
| Trident‐shaped | Ts |
| V‐shaped | Vs |
| X‐shaped | Xs |
The coding formula and two examples are shown in Figure 2. Each unit of the code is made up of three sections and describes the anatomy of one artery in a variant circle. Section one represents the anatomical relationship of the variant artery within the circle. This section was not required when describing the AComA or single unilateral variations. Section two identifies the variant artery and section three represents the type of anatomical variation present. Section one and three were written in superscript for ease of identification.
FIGURE 2.
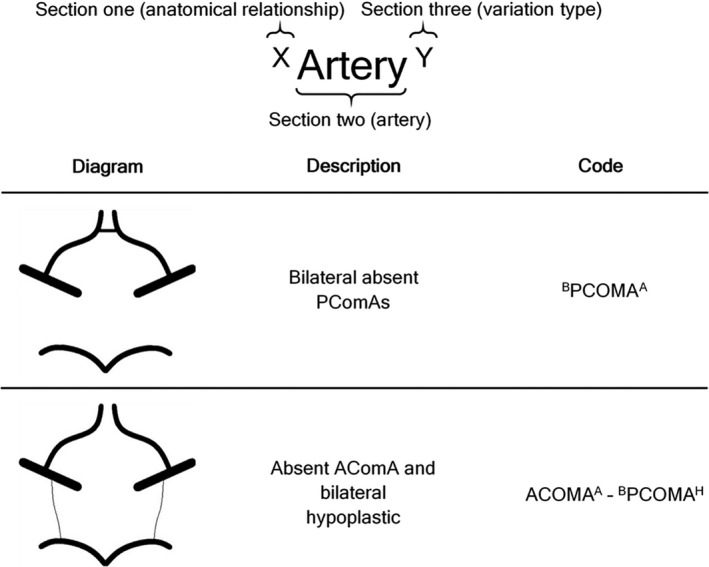
The coding formula and two examples
Units were connected by hyphenation to describe the anatomy of a circle with multiple variations. In this case, units were ordered according to the anterior‐to‐posterior location of the coded arteries.
3.4. Classification system
The 82 distinct anatomical variations of the CoW extracted from the included studies fall into five continuous groups, which form the core of the new classification system as described below. As a comparison, Figure 3 shows the classically described anatomy of the CoW.
FIGURE 3.

A labelled diagram showing the normal anatomy of the CoW
Group one contains 24 circles with one or more hypoplastic segments only (Figure 4; Table 5). Circles with one (n = 4), two (n = 10), three (n = 8), five (n = 1) and six (n = 1) hypoplastic segments are included. No circle with four hypoplastic segments was recorded.
FIGURE 4.

Group one of the classification system containing circles with one or more hypoplastic segments only
TABLE 5.
A table of the circles in group one of the classification system
| Circle number | Description of the variant circle | Variation code | Study code(s) |
|---|---|---|---|
| One hypoplastic segment | |||
| 1 | Hypoplastic AComA | ACOMAH | S3, S4, S12, S21, S30, S31, S42 |
| 2 | Unilateral hypoplastic A1 | A1H | S3, S4, S12, S15, S19, S22, S29, S30, S31, S40 |
| 3 | Unilateral hypoplastic PComA | PCOMAH | S2, S3, S4, S8, S12, S16, S21, S22, S29, S31, S37, S42 |
| 4 | Unilateral hypoplastic P1 | P1H | S3, S4, S8, S15, S21, S22, S30, S31, S37, S42 |
| Two hypoplastic segments | |||
| 5 | Hypoplastic AComA and unilateral hypoplastic PComA | ACOMAH—PCOMAH | S3, S4, S8, S12, S21, S29, S30, S31, S42 |
| 6 | Hypoplastic AComA and unilateral hypoplastic P1 | ACOMAH—P1H | S4, S8, S31, S42 |
| 7 | Unilateral hypoplastic A1 and ipsilateral hypoplastic PComA | A1H—IPCOMAH | S3, S31 |
| 8 | Unilateral hypoplastic A1 and contralateral hypoplastic PComA | A1H—CPCOMAH | S4, S31 |
| 9 | Unilateral hypoplastic A1 and ipsilateral hypoplastic P1 | A1H—IP1H | S4, S8, S15, S21, S31 |
| 10 | Unilateral hypoplastic A1 and contralateral hypoplastic P1 | A1H—CP1H | S30, S31 |
| 11 | Bilateral hypoplastic PComAs | BPCOMAH | S3, S4, S8, S12, S16, S21, S31, S34, S37, S42 |
| 12 | Unilateral hypoplastic PComA and contralateral hypoplastic P1 | PCOMAH—CP1H | S4, S8, S21, S31, S42 |
| 13 | Bilateral hypoplastic P1s | BP1H | S4, S15, S31, S37, S42 |
| 14 | Unilateral hypoplastic P1 and P2 | P1H—IP1H | S15 |
| Three hypoplastic segments | |||
| 15 | Hypoplastic AComA and bilateral hypoplastic PComAs | ACOMAH—BPCOMAH | S3, S4, S8, S12, S17, S19, S21, S31, S42 |
| 16 | Hypoplastic AComA, unilateral hypoplastic PComA and contralateral hypoplastic P1 | ACOMAH—PCOMAH—CP1H | S8, S31, S42 |
| 17 | Hypoplastic AComA and bilateral hypoplastic P1s | ACOMAH—BP1H | S4, S31 |
| 18 | Unilateral hypoplastic A1 and bilateral hypoplastic PComAs | A1H—BPCOMAH | S1, S4, S31 |
| 19 | Unilateral hypoplastic A1, ipsilateral hypoplastic PComA and contralateral hypoplastic P1 | A1H—IPCOMAH—CP1H | S31 |
| 20 | Unilateral hypoplastic A1, contralateral hypoplastic PComA and ipsilateral hypoplastic P1 | A1H—CPCOMAH—IP1H | S3, S31 |
| 21 | Unilateral hypoplastic A1 and bilateral hypoplastic P1s | A1H—BP1H | S4, S15, S24, S31 |
| 22 | Bilateral hypoplastic PComAs and unilateral hypoplastic P1 | BPCOMAH—P1H | S3 |
| Five hypoplastic segments | |||
| 23 | Hypoplastic AComA, bilateral hypoplastic PComAs and unilateral hypoplastic P1 and P2 | ACOMAH—BPCOMAH—P1H—IP2H | S8 |
| Six hypoplastic segments | |||
| 24 | Hypoplastic AComA, bilateral hypoplastic A1s and A2s and unilateral hypoplastic PComA | ACOMAH—BA1H—BA2H—PCOMAH | S27 |
Group two contains 11 circles with one or more absent segments only (Figure 5; Table 6). Circles with one (n = 4), two (n = 3), three (n = 3) and four (n = 1) absent segments were recorded.
FIGURE 5.

Group two of the classification system containing circles with one or more absent segments only
TABLE 6.
A table of the circles in group two of the classification system
| Circle number | Description of the variant circle | Variation code | Study code(s) |
|---|---|---|---|
| One absent segment | |||
| 25 | Absent AComA | ACOMAA | S11, S20, S22 |
| 26 | Unilateral absent A1 | A1A | S22, S27, S33 |
| 27 | Unilateral absent PComA | PCOMAA | S1, S11, S12, S16, S21, S27, S30 |
| 28 | Unilateral absent P1 | P1A | S9, S12, S22 |
| Two absent segments | |||
| 29 | Absent AComA and unilateral absent PComA | ACOMAA—PCOMAA | S7 |
| 30 | Unilateral absent A1 and ipsilateral absent PComA | A1A—IPCOMAA | S40 |
| 31 | Bilateral absent PComAs | BPCOMAA | S1, S12, S16, S20, S21, S22, S24, S27, S40 |
| Three absent segments | |||
| 32 | Absent AComA and bilateral absent PComAs | ACOMAA—BPCOMAA | S11, S20, S25 |
| 33 | Unilateral absent A1 and bilateral absent PComAs | A1A—BPCOMAA | S36 |
| 34 | Unilateral absent A1 and bilateral absent P1s | A1A—BP1A | S24 |
| Four absent segments | |||
| 35 | Bilateral absent PComAs and unilateral absent P1 and P2 | BPCOMAA—P1A—IP2A | S21 |
Group three contains six circles with hypoplastic and absent segments only (Figure 6; Table 7). Three circles with one hypoplastic and one absent segment were recorded. Circle 39 had one hypoplastic and two absent segments. Circles 40 and 41 had one absent and two hypoplastic segments.
FIGURE 6.

Group three of the classification system containing circles with hypoplastic and absent segments only
TABLE 7.
A table of the circles in group three of the classification system
| Circle number | Description of the variant circle | Variation code | Study code(s) |
|---|---|---|---|
| Two variant segments | |||
| 36 | Unilateral absent A1 and contralateral hypoplastic P1 | A1A—CP1H | S13 |
| 37 | Unilateral hypoplastic PComA and contralateral absent PComA | PCOMAH—CPCOMAA | S16, S21, S34 |
| 38 | Unilateral absent PComA and contralateral hypoplastic P1 | PCOMAA—CP1H | S11, S34 |
| Three variant segments | |||
| 39 | Hypoplastic AComA and bilateral absent PComAs | ACOMAH—BPCOMAA | S6 |
| 40 | Absent AComA and bilateral hypoplastic PComAs | ACOMAA—BPCOMAH | S14 |
| 41 | Unilateral absent A1 and bilateral hypoplastic P1s | A1A—BP1H | S35, S40 |
Group four contains 26 circles with accessory segments (Figure 7; Table 8). Circles with one or more accessory AComA (n = 11), anterior cerebral artery (ACA) (n = 8), A1 (n = 3), P1 (n = 3), posterior cerebral artery (PCA) (n = 2) and PComA (n = 1) were recorded. Circles 48, 49 and 61 showed a hypoplastic accessory segment, and circles 66 and 67 showed duplication of multiple segments.
FIGURE 7.

Group four of the classification system containing circles with one or more accessory segments
TABLE 8.
A table of the circles in group four of the classification system
| Circle number | Description of the variant circle | Variation code | Study code(s) |
|---|---|---|---|
| Accessory AComA | |||
| 42 | Duplicated AComA | ACOMAD | S21 |
| 43 | Duplicated AComA and unilateral hypoplastic PComA | ACOMAD—PCOMAH | S21 |
| 44 | Duplicated AComA and bilateral hypoplastic PComAs | ACOMAD—BPCOMAH | S21 |
| 45 | Duplicated AComA, unilateral hypoplastic PComA and contralateral absent PComA | ACOMAD—PCOMAH—CPCOMAA | S21 |
| 46 | Duplicated AComA and unilateral absent PComA | ACOMAD—PCOMAA | S11, S21 |
| 47 | Duplicated AComA and bilateral absent PComAs | ACOMAD—BPCOMAA | S21 |
| 48 | Duplicated AComA (one AComA hypoplastic) | ACOMAD(1H) | S5, S17 |
| 49 | Duplicated AComA (one AComA hypoplastic) and unilateral hypoplastic PComA | ACOMAD(1H)—PCOMAH | S17 |
| 50 | Duplicated AComA (one AComA plexiform) and unilateral hypoplastic PComA | ACOMAD(1P)—PCOMAH | S21 |
| 51 | Triplicated AComA | ACOMAT | S17 |
| Accessory ACA | |||
| 52 | Medial triplicated ACA | ACATm | S17, S21 |
| 53 | Medial triplicated ACA and unilateral hypoplastic A1 | ACATm—A1H | S21 |
| 54 | Medial triplicated ACA and unilateral hypoplastic PComA | ACATm—PCOMAH | S21 |
| 55 | Medial triplicated ACA and bilateral hypoplastic PComAs | ACATm—BPCOMAH | S42 |
| 56 | Medial triplicated ACA and unilateral absent PComA | ACATm—PCOMAA | S21 |
| 57 | Lateral triplicated ACA | ACATl | S21 |
| 58 | Lateral triplicated ACA, hypoplastic AComA and ipsilateral hypoplastic PComA | ACATl—ACOMAH—IPCOMAH | S21 |
| Accessory A1 | |||
| 59 | Unilateral duplicated A1 | A1D | S15, S21 |
| 60 | Unilateral duplicated A1 and ipsilateral hypoplastic P1 | A1D—IP1H | S15 |
| Accessory PComA | |||
| 61 | Triplicated PComA (one PComA hypoplastic), contralateral hypoplastic PComA and ipsilateral hypoplastic P1 | PCOMAT(1H)—CPCOMAH—IP1H | S1 |
| Accessory P1 | |||
| 62 | Unilateral duplicated P1 | P1D | S15 |
| 63 | Unilateral absent A1 and contralateral duplicated P1 origin | A1A—CP1D | S26 |
| Accessory PCA | |||
| 64 | Unilateral duplicated PCA with ICoA | PCAD | S41 |
| 65 | Unilateral duplicated PCA with hypoplastic P1c and ICoA | PCAD—P1CH—ICOAH | S41 |
| Multiple accessory segments | |||
| 66 | Lateral triplicated ACA and duplicated AComA | ACATl—ACOMAD | S21 |
| 67 | Unilateral duplicated A1 and ipsilateral duplicated P1 | A1D—IP1D | S15 |
Group five contains 15 circles with other types of anatomical variation (Figure 8; Table 9). Circles with a variant AComA (n = 3), variant ACA union (n = 4), segment fenestration (n = 6) and segment elongation (n = 2) were recorded. The description of circle 70 as ‘trident‐shaped AComA’ is original to this review.
FIGURE 8.

Group five of the classification system containing circles with other types of anatomical variation
TABLE 9.
A table of the circles in group five of the classification system
| Circle number | Description of the variant circle | Variation code | Study code(s) |
|---|---|---|---|
| Variant AComA structure | |||
| 68 | V‐shaped AComA and unilateral hypoplastic PComA | ACOMAVs—PCOMAH | S21 |
| 69 | V‐shaped AComA and bilateral hypoplastic PComAs | ACOMAVs—BPCOMAH | S21 |
| 70 | Trident‐shaped AComA | ACOMATs | S10 |
| Variant ACA union | |||
| 71 | Azygous ACA and unilateral absent P1 | ACAAz—P1A | S23 |
| 72 | Azygous ACA and bilateral absent P1s | ACAAz—BP1A | S11 |
| 73 | X‐shaped ACA union and bilateral hypoplastic PComAs | ACAXs—BPCOMAH | S28 |
| 74 | X‐shaped ACA union, unilateral hypoplastic A1, ipsilateral absent PComA and contralateral hypoplastic P1 | ACAXs—A1H—IPCOMAA—CP1H | S11 |
| Segment fenestration | |||
| 75 | V‐shaped AComA and fenestrated A1/A2 junction | ACOMAVs—A1/A2F | S10 |
| 76 | Absent AComA, unilateral absent A1, ipsilateral absent A2, contralateral fenestrated A1/A2 junction, contralateral absent PComA and ipsilateral absent P1 | ACOMAA—A1A—IA2A—CA1/A2F—CPCOMAA—IP1A | S32 |
| 77 | Unilateral fenestrated A1 and ipsilateral absent PComA | A1F—IPCOMAA | S33 |
| 78 | Unilateral fenestrated PComA | PCOMAF | S38 |
| 79 | Unilateral fenestrated P1 | P1F | S18 |
| 80 | Unilateral fenestrated A1 and ipsilateral fenestrated A2 | A1F—IA2F | S21 |
| Segment elongation | |||
| 81 | Elongated PComA and contralateral absent PComA | PCOMAE—CPCOMAA | S39 |
| 82 | Unilateral hypoplastic A1, ipsilateral absent PComA and contralateral elongated PComA | A1H—IPCOMAA—CPCOMAE | S39 |
4. DISCUSSION
The new classification system we have proposed in Section 3.4 has several advantages. Containing more distinct variations and types (groups) of variation than previously established systems, it demonstrates a greater potential for the categorisation of circles identified in future studies. Grouping of circles allows users to select a variation type, while group subcategorisation allows users to methodically identify and categorise specific structures. The grouping of circles according to anatomy is not a feature of previously established systems, and it allows original circles to be categorised alongside similar variants. Overall, the new classification system provides a more comprehensive summary of the anatomical variations of the CoW in humans, increasing the simplicity, flexibility, and efficiency of cataloguing, and improving the accuracy of CoW ontology.
Circles included in the classification system are shown in three formats. The figures provide an accessible, visual guide to the classification system, and their standardised design creates illustrative consistency between the groups. The circles were reconstructed digitally to reduce the risk of misinterpretation. The tables provide a complete, standardised anatomical description of each circle, and should be reviewed in combination with the relevant figure. The coding system provides a simple, abbreviated description of the anatomy of each variation.
The coding system allows the description of recorded circles from past and future studies, and its design permits future description of novel variations. It has a capacity for new symbols, enabling the description of circles from future studies identifying exceptional anatomical findings. Use of the coding system reduces the need for complicated and error‐prone written descriptions.
4.1. Clinical application
Circle variation has implications for clinical practice. It is associated with an increased risk of ischaemic stroke (Oumer et al., 2021; van Seeters et al., 2015), aneurysm rupture (Lazzaro et al., 2012; Stojanović et al., 2019), white matter disease (Chuang et al., 2011; Ryan et al., 2015) and migraine (Henry et al., 2015). It is also associated with an increased risk of vasospasm post‐subarachnoid haemorrhage (Jacquens et al., 2020). The classification system may therefore be used to identify patients at risk of disease and employ targeted preventative therapies. In addition, a good collateral circulation predicts favourable outcomes in patients with acute ischaemic stroke receiving reperfusion therapies (Leng et al., 2016; Wufuer et al., 2017). With anatomy being a factor in determining patient outcome, the classification system may have a role in guiding therapeutic decision‐making.
Circle variation has implications for preoperative planning. Variation predisposes one‐sixth of patients to cerebral ischaemia during carotid artery closure (Manninen et al., 2009) and may impair the protective effects of unilateral selective cerebral perfusion (Papantchev et al., 2013). In such cases, protective effects may be maintained through the use of bilateral selective cerebral perfusion (Papantchev et al., 2013). An awareness of circle variation is therefore fundamental in selecting the most appropriate method of cerebral protection. Recognition of the classification system, particularly groups two and three, in the preoperative stage may reduce the risk of cerebral ischaemia and prevent neurological sequelae. Yet function is not determined by anatomy alone. With physiological manipulation, only 1 in 15 patients may need shunting during carotid endarterectomy (Musicki et al., 2017). Adequate cerebral cross‐perfusion may therefore be maintained when both anatomical and physiological factors are considered.
Circle variation has intraoperative implications. Unusual anatomy is the leading patient‐related factor contributing to technical error in surgery (Regenbogen et al., 2007), and intraoperative vessel damage is a common factor in successful litigation claims (Markides et al., 2008). Variation, particularly hypoplasia and duplication, may affect surgical approach, surgical difficulty, aneurysm exposure, accuracy of endovascular coil or aneurysm clip placement, and postoperative complications. An awareness of circle variation, and the classification system, is therefore important in reducing surgical error, and improving patient safety and clinical outcome.
It is important that healthcare professionals use a common language. Unsystematic, and often extensive, descriptions are used to report the anatomy of variant circles. This increases the risk of misinterpretation and interventional error. As such, the coding system may be used in clinical practice. It provides healthcare professionals with a simple method for describing the anatomy of circles identified in patients. It is of relevance to neurosurgery, radiology, and interventional neuroradiology. A standardised description would reduce the risk of error, improving patient outcomes. It would also enable direct communication of circle anatomy between healthcare professionals, hospitals, trusts, and healthcare systems.
4.2. Educational application
The classification system may be used in postgraduate anatomical education. A significant proportion of surgical and radiology training curricula include anatomical variation, yet over half do not suggest specific variation classification systems for trainees to use (Raikos & Smith, 2015). With 21.4% of experienced clinicians encountering anatomical variation daily (Raikos & Smith, 2015), an understanding of variation in humans is important for patient presentation, examination, investigation, and surgical management. The classification system is the most comprehensive summary of anatomical variation of the CoW in humans. As such, it may function as a learning and reference tool.
It may also be used in undergraduate anatomical education. Early exposure to human variation in medical courses is recommended, and students should have the opportunity to discuss the significance of variation with experienced tutors (Willan & Humpherson, 1999). The classification system provides students undertaking theoretical and practical learning with a concise, visual summary of variation of an important anatomical structure. It may be used within problem‐based learning to stimulate discussion surrounding the clinical significance of anatomical variation in humans.
4.3. Future directions
Group one (22 out of 24) and three (4 out of 6) circles were most recorded in studies conducted in North America. Group two (8 out of 11), four (18 out of 26) and five (7 out of 15) circles were most recorded in studies conducted in Europe. However, conclusions on geographical location and type of variation are limited. It is suggested that further cross‐sectional cadaveric and angiographic studies are performed to identify possible associations between sex, ethnicity, and geographical location and type of variation. Studies should be performed in a variety of geographical locations using large, diverse population groups. The results may be used to expand the classification system.
CoW variation is associated with an increase in aneurysm rupture (Lazzaro et al., 2012; Stojanović et al., 2019). It is suggested that future studies investigate the association between variation type, as described in the classification system, and the risk of aneurysm rupture. Identification of anatomical risk factors may assist in the selection of patients for preventative treatment.
While use of the coding system is encouraged, a regular systematic search of the literature should be performed to update the classification system. This would ensure that a single, up‐to‐date collection of the recorded variations is available. This may be the responsibility of an anatomical organisation.
4.4. Limitations
Criteria In2 and In3 may have excluded studies that used non‐description to represent normal anatomy. A complete description or illustration of the circle was necessary as it could not be assumed that unreported arteries were of normal anatomy.
The searching and initial appraisal of studies were performed by a single investigator, introducing the potential for observer bias. However, a representative sample of studies was screened by two independent reviewers, with no difference to the original study selection found.
Some circles included in the classification system are described to have hypoplastic segments despite the original study not providing a definition for the variation type. These circles were included on account of the consistency in the use of a diameter of <1 mm as a definition of artery hypoplasia within the literature.
5. CONCLUSION
The new classification system provides a comprehensive ontology of the described anatomical variations of the CoW in humans. When used with the coding system, it allows the description and categorisation of recorded and unrecorded variants identified in past and future studies. It is applicable to current clinical practice and the anatomical community, including human anatomy education and research.
CONFLICT OF INTEREST
No conflicts of interest.
AUTHOR CONTRIBUTIONS
The systematic review was designed by J.R.A. and K.A.S. The project was conceptualised by K.A.S and P.J.B. Figures were designed by J.R.A. The study samples were independently reviewed by M.A and H.N.M. Manuscript was written by J.R.A. All authors read and critically revised the manuscript.
Supporting information
Table S1
ACKNOWLEDGEMENTS
None declared.
Ayre, J.R. , Bazira, P.J. , Abumattar, M. , Makwana, H.N. & Sanders, K.A. (2022) A new classification system for the anatomical variations of the human circle of Willis: A systematic review. Journal of Anatomy, 240, 1187–1204. Available from: 10.1111/joa.13616
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- Al‐Hussain, S.M. , Shoter, A.M. & Bataina, Z.M. (2001) Circle of Willis in adults. Neurosciences, 6(4), 209–212. [PubMed] [Google Scholar]
- Benson, L.N. , Freedom, R.M. , Wilson, G.J. & Halliday, W.C. (1986) Cerebral complications following balloon angioplasty of coarctation of the aorta. CardioVascular and Interventional Radiology, 9(4), 184–186. [DOI] [PubMed] [Google Scholar]
- Chuang, Y.‐M. , Huang, K.‐L. , Chang, Y.‐J. , Chang, C.‐H. , Chang, T.‐Y. , Wu, T.‐C. et al. (2011) Associations between circle of Willis morphology and white matter lesion load in subjects with carotid artery stenosis. European Neurology, 66(3), 136–144. [DOI] [PubMed] [Google Scholar]
- Cilliers, K. , Vorster, W. & Page, B.J. (2018) The anatomical variation of the circulus arteriosus cerebri in a cadaver cohort representing the population dynamics of the Western Cape. British Journal of Neurosurgery, 32(1), 61–67. [DOI] [PubMed] [Google Scholar]
- Critical Appraisal Skills Programme . (2018a) CASP case‐control study checklist. Available at: http://www.casp‐uk.net/checklists [Accessed June 2020] [Google Scholar]
- Critical Appraisal Skills Programme . (2018b) CASP cohort study checklist. Available at: http://www.casp‐uk.net/checklists [Accessed June 2020] [Google Scholar]
- De Silva, K.R.D. , Silva, R. , Amaratunga, D. , Gunasekera, W.S.L. & Jayesekera, R.W. (2011) Types of the cerebral arterial circle (circle of Willis) in a Sri Lankan population. BMC Neurology, 11, 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ding, R. , Xu, X. , Guan, D. , Zhu, B. , Zhang, G. & Wu, X. (2019) Fatal subarachnoid hemorrhage caused by rupture of variant anterior communicating artery: a case report and literature review. Forensic Science, Medicine and Pathology, 15(1), 97–101. [DOI] [PubMed] [Google Scholar]
- Drummond, J.C. , Englander, R.N. & Gallo, C.J. (2006) Cerebral ischemia as an apparent complication of anterior cervical discectomy in a patient with an incomplete circle of Willis. Anesthesia and Analgesia, 102(3), 896–899. [DOI] [PubMed] [Google Scholar]
- Drummond, J.C. , Lee, R.R. & Howell, J.P. Jr (2012) Focal cerebral ischemia after surgery in the “beach chair” position: the role of a congenital variation of circle of Willis anatomy. Anesthesia and Analgesia, 114(6), 1301–1303. [DOI] [PubMed] [Google Scholar]
- Eftekhar, B. , Dadmehr, M. , Ansari, S. , Ghodsi, M. , Nazparvar, B. & Ketabchi, E. (2006) Are the distributions of variations of circle of Willis different in different populations? Results of an anatomical study and review of literature. BMC Neurology, 6, 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giglio, M. , Caggiano, G. , De Blasi, R. , Brienza, N. , Bucaria, V. , Ladisa, P. et al. (2010) A fatal rhino‐cerebral zygomycosis in a young woman with latent diabetes mellitus and cerebral blood vessel agenesis. Medical Mycology, 48(2), 394–397. [DOI] [PubMed] [Google Scholar]
- Gray, H. (2016) Neuroanatomy. In: Standring, S. (Ed.) Gray’s anatomy: the anatomical basis of clinical practice, 41st edition. Philadelphia, PA: Elsevier, pp. 280–285. [Google Scholar]
- Gurdal, E. , Cakmak, O. , Yalcinkaya, M. , Uzun, I. & Cavdar, S. (2004) Two variations of the anterior communicating artery: a clinical reminder. Neuroanatomy, 3, 32–34. [Google Scholar]
- Hafez, K.A. , Afifi, N.M. & Saudi, F.Z. (2007) Anatomical variations of the circle of Willis in males and females on 3D MR angiograms. The Egyptian Journal of Hospital Medicine, 26(1), 106–121. [Google Scholar]
- Hartkamp, M.J. , van Der Grond, J. , van Everdingen, K.J. , Hillen, B. & Mali, W.P. (1999) Circle of Willis collateral flow investigated by magnetic resonance angiography. Stroke, 30(12), 2671–2678. [DOI] [PubMed] [Google Scholar]
- Hashemi, S.M.R. , Mahmoodi, R. & Amirjamshidi, A. (2013) Variations in the Anatomy of the Willis′ circle: a 3‐year cross‐sectional study from Iran (2006‐2009). Are the distributions of variations of circle of Willis different in different populations? Result of an anatomical study and review of literature. Surgical Neurology International, 4(1), 2006–2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He, Y. , Li, Y. , Jiang, H. , Teng, F. & Nie, Z. (2016) Is incomplete circle of Willis associated with white matter lesion. International Journal of Clinical Experimental Medicine, 9(6), 11657–11662. [Google Scholar]
- Henry, B.M. , Roy, J. , Ramakrishnan, P.K. , Vikse, J. , Tomaszewski, K.A. & Walocha, J.A. (2015) Association of migraine headaches with anatomical variations of the circle of Willis: evidence from a meta‐analysis. Neurologia I Neurochirurgia Polska, 49(4), 272–277. [DOI] [PubMed] [Google Scholar]
- Henry, B.M. , Tomaszewski, K.A. , Ramakrishnan, P.K. , Roy, J. , Vikse, J. , Loukas, M. et al. (2017) Development of the anatomical quality assessment (AQUA) tool for the quality assessment of anatomical studies included in meta‐analyses and systematic reviews. Clinical Anatomy, 30(1), 6–13. [DOI] [PubMed] [Google Scholar]
- Hindenes, L.B. , Håberg, A.K. , Johnsen, L.H. , Mathiesen, E.B. , Robben, D. & Vangberg, T.R. (2020) Variations in the circle of Willis in a large population sample using 3D TOF angiography: the Tromsø study. PLoS One, 15(11), e0241373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howe, W.C. (1903) Anomalies in the circle of Willis. With the report of a case in which the communicating arteries were absent. Annals of Surgery, 38(6), 878–887. [PMC free article] [PubMed] [Google Scholar]
- Howie, D.L. (1959) Incidence of anomalies of the circle of Willis in psychiatric patients. Archives of Neurology, 1(4), 425–426. [DOI] [PubMed] [Google Scholar]
- Ibrahim, S.M.H. , El Magzoub, M.S. , Nour, A.M. , Nurein, M.S. , Abdalla, S.F. & Jaber, A. (2017) Abnormal circle of Willis among migraineurs in Sudan. Journal of Neurology and Stroke, 7(7), 00264. [Google Scholar]
- Iqbal, S. (2013) A comprehensive study of the anatomical variations of the circle of Willis in adult human brains. Journal of Clinical and Diagnostic Research, 7(11), 2423–2427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacquens, A. , Shotar, E. , Bombled, C. , Glémain, B. , Sourour, N.‐A. , Nouet, A. et al. (2020) Is anatomical variations a risk factor for cerebral vasospasm in anterior communicating complex aneurysms rupture? Stroke, 51(3), 998–1001. [DOI] [PubMed] [Google Scholar]
- Jensen, C.J. , Shereen, R. , Tubbs, R.S. & Griessenauer, C. (2017) Fenestration in the P1 segment of the posterior cerebral artery. Cureus, 9(7), e1528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones, J.D. , Castanho, P. , Bazira, P. & Sanders, K. (2020) Anatomical variations of the circle of Willis and their prevalence, with a focus on the posterior communicating artery: a literature review and meta‐analysis. Clinical Anatomy, 1–13. [DOI] [PubMed] [Google Scholar]
- Kapoor, K. , Singh, B. & Dewan, I.J. (2008) Variations in the configuration of the circle of Willis. Anatomical Science International, 83(2), 96–106. [DOI] [PubMed] [Google Scholar]
- Karatas, A. , Yilmaz, H. , Coban, G. , Koker, M. & Uz, A. (2016) The anatomy of the circulus arteriosus cerebri (circle of Willis): a study in Turkish population. Turkish Neurosurgery, 26(1), 54–61. [DOI] [PubMed] [Google Scholar]
- Klimek‐Piotrowska, W. , Kopeć, M. , Kochana, M. , Krzyżewski, R.M. , Tomaszewski, K.A. , Brzegowy, P. et al. (2013) Configurations of the circle of Willis: a computed tomography angiography based study on a Polish population. Folia Morphologica, 72(4), 293–299. [DOI] [PubMed] [Google Scholar]
- Klimek‐Piotrowska, W. , Rybicka, M. , Wojnarska, A. , Wójtowicz, A. , Koziej, M. & Hołda, M.K. (2015) A multitude of variations in the configuration of the circle of Willis: an autopsy study. Anatomical Science International, 91(4), 325–333. [DOI] [PubMed] [Google Scholar]
- Krabbe‐Hartkamp, M.J. , van der Grond, J. , de Leeuw, F.E. , de Groot, J.C. , Algra, A. , Hillen, B. et al. (1998) Circle of Willis: morphologic variation on three‐dimensional time‐of‐flight MR angiograms. Radiology, 207(1), 103–111. [DOI] [PubMed] [Google Scholar]
- Lazorthes, G. , Gouazé, A. , Santini, J. & Salamon, G. (1979) Le cercle artériel du cerveau (circulus arteriosus cerebri). Anatomia Clinica, 1(3), 241–257. [Google Scholar]
- Lazzaro, M.A. , Ouyang, B. & Chen, M. (2012) The role of circle of Willis anomalies in cerebral aneurysm rupture. Journal of NeuroInterventional Surgery, 4(1), 22–26. [DOI] [PubMed] [Google Scholar]
- Leng, X. , Lan, L. , Liu, L. , Leung, T.W. & Wong, K.S. (2016) Good collateral circulation predicts favourable outcomes in intravenous thrombolysis: a systematic review and meta‐analysis. European Journal of Neurology, 23(12), 1738–1749. [DOI] [PubMed] [Google Scholar]
- Li, J. , Wang, J. , Wei, X. , Zhao, Y. , Wang, F. & Li, Y. (2020) Examination of structural variations of the circle of Willis by 3D time‐of‐flight magnetic resonance angiography. Frontiers in Neuroscience, 14, 71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loh, P.K. & Sharma, V.K. (2010) Neurological pictures. Atherosclerosis in congenital azygous solitary A2 anterior cerebral artery with simultaneous bifrontal infarctions. Journal of Neurology, Neurosurgery and Psychiatry, 81(2), 203. [DOI] [PubMed] [Google Scholar]
- Malamateniou, C. , Adams, M.E. , Srinivasan, L. , Allsop, J.M. , Counsell, S.J. , Cowan, F.M. et al. (2009) The anatomic variations of the circle of Willis in preterm‐at‐term and term‐born infants: an MR angiography study at 3T. American Journal of Neuroradiology, 30(10), 1955–1962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manninen, H. , Mäkinen, K. , Vanninen, R. , Ronkainen, A. & Tulla, H. (2009) How often does an incomplete circle of Willis predispose to cerebral ischemia during closure of carotid artery? Postmortem and clinical imaging studies. Acta Neurochirurgica, 151(9), 1099–1105. [DOI] [PubMed] [Google Scholar]
- Markides, G.A. , Subar, D. & Al‐Khaffaf, H. (2008) Litigation claims in vascular surgery in the United Kingdom’s NHS. European Journal of Vascular & Endovascular Surgery, 36(4), 452–457. [DOI] [PubMed] [Google Scholar]
- Matsuda, M. , Uchino, A. , Saito, N. , Neki, H. , Kohyama, S. & Yamane, F. (2017) Duplicate origin and extremely long P1 segment of the posterior cerebral artery diagnosed by MR angiography. Surgical and Radiological Anatomy, 39(6), 699–702. [DOI] [PubMed] [Google Scholar]
- McCullough, A.W. (1962) Some anomalies of the cerebral arterial circle (of Willis) and related vessels. The Anatomical Record, 142(4), 537–543. [Google Scholar]
- Moore, K.L. , Dalley, A.F. & Agur, A.M.R. (2014) Clinically orientated anatomy, 7th edition. Philadelphia, PA: Wolters Kluwer, pp. 882–885. [Google Scholar]
- Musicki, K. , Hurst, K.V. , Molnár, Z. , Hardy, E. & Handa, A. (2017) Cerebral cross‐perfusion and the circle of Willis: does physiology trump anatomy? Journal of Vascular Diagnostics and Interventions, 5, 35–40. [Google Scholar]
- Oumer, M. , Mekuriaw, A. & Abebe, M. (2021) Association between circle of Willis and ischemic stroke: a systematic review and meta‐analysis. BMC Neuroscience, 22(1), 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozturk, H.A. , Sanli, E.C. & Kurtoglu, Z. (2008) Absent anterior communicating artery and varied distribution of anterior cerebral artery. Neurosciences, 13(4), 441–444. [PubMed] [Google Scholar]
- Papantchev, V. , Hristov, S. , Todorova, D. , Naydenov, E. , Paloff, A. , Nikolov, D. et al. (2007) Some variations of the circle of Willis, important for cerebral protection in aortic surgery – a study in Eastern Europeans. European Journal of Cardio‐Thoracic Surgery, 31(6), 982–989. [DOI] [PubMed] [Google Scholar]
- Papantchev, V. , Stoinova, V. , Aleksandrov, A. , Todorova‐Papantcheva, D. , Hristov, S. , Petkov, D. et al. (2013) The role of Willis circle variations during unilateral selective cerebral perfusion: a study of 500 circles. European Journal of Cardio‐Thoracic Surgery, 44(4), 743–753. [DOI] [PubMed] [Google Scholar]
- Raikos, A. & Smith, J.D. (2015) Anatomical variations: how do surgical and radiology training programs teach and assess them in their training curricula. Clinical Anatomy, 28(6), 717–724. [DOI] [PubMed] [Google Scholar]
- Regenbogen, S.E. , Greenberg, C.C. , Studdert, D.M. , Lipsitz, S.R. , Zinner, M.J. & Gawande, A.A. (2007) Patterns of technical error among surgical malpractice claims: an analysis of strategies to prevent injury to surgical patients. Annals of Surgery, 246(5), 705–711. [DOI] [PubMed] [Google Scholar]
- Riggs, H.E. & Rupp, C. (1963) Variation in form of circle of Willis. The relation of the variations to collateral circulation: anatomic analysis. Archives of Neurology, 8(1), 8–14. [DOI] [PubMed] [Google Scholar]
- Ryan, D.J. , Byrne, S. , Dunne, R. , Harmon, M. & Harbison, J. (2015) White matter disease and an incomplete circle of Willis. International Journal of Stroke, 10(4), 547–552. [DOI] [PubMed] [Google Scholar]
- Sabau, M. , Comanescu, A. & Popa, I. (2012) A complex abnormality of the circle of Willis: case presentation. Romanian Journal of Neurology, 11(1), 44–48. [Google Scholar]
- Saikia, B. , Handique, A. , Phukan, P. , Lynser, D. & Jamil, M. (2014) Study of anomalies in the circle of Willis using magnetic resonance angiography in north eastern India. Journal of the Anatomical Society of India, 63(1), 67–73. [Google Scholar]
- Saphir, O. (1935) Anomalies of the circle of Willis with resulting encephalomalacia and cerebral hemorrhage. The American Journal of Pathology, 11(5), 775–788. [PMC free article] [PubMed] [Google Scholar]
- Shamseer, L. , Moher, D. , Clarke, M. , Ghersi, D. , Liberati, A. , Petticrew, M. et al. (2015) Preferred reporting items for systematic review and meta‐analysis protocols (PRISMA‐P) 2015: elaboration and explanation. BMJ, 349(jan02 1), g7647. Available from: 10.1136/bmj.g7647 [DOI] [PubMed] [Google Scholar]
- Sonobe, A. , Kato, H. , Mathis, B.J. & Hiramatsu, Y. (2019) Catastrophic cerebral infarction during extracorporeal life support due to rare anomaly in the circle of Willis. Interactive CardioVascular and Thoracic Surgery, 29(5), 816–817. [DOI] [PubMed] [Google Scholar]
- Sonobe, A. , Kato, H. , Mathis, B.J. & Hiramatsu, Y. (2020) Surgical correction of coarctation of the aorta featuring an incomplete circle of Willis. Interactive CardioVascular and Thoracic Surgery, 30(5), 794–795. [DOI] [PubMed] [Google Scholar]
- Stefani, M.A. , Schneider, F.L. , Marrone, A.C.H. & Severino, A.G. (2013) Influence of the gender on cerebral vascular diameters observed during the magnetic resonance angiographic examination of Willis circle. Brazilian Archives of Biology and Technology, 56(1), 45–52. [Google Scholar]
- Stojanović, N.N. , Kostić, A. , Mitić, R. , Berilažić, L. & Radisavljević, M. (2019) Association between circle of Willis configuration and rupture of cerebral aneurysms. Medicina, 55(7), 338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tripathi, M. , Goel, V. , Padma, M.V. , Jain, S. , Maheshwari, M.C. , Gaikwad, S. et al. (2003) Fenestration of the posterior communicating artery. Neurology India, 51(1), 75–76. [PubMed] [Google Scholar]
- Uchino, A. , Suzuki, C. & Tanaka, M. (2015) Extremely long posterior communicating artery diagnosed by MR angiography: report of two cases. Surgical and Radiologic Anatomy, 37(5), 565–568. [DOI] [PubMed] [Google Scholar]
- Urbanski, P.P. , Lenos, A. , Blume, J.C. , Ziegler, V. , Griewing, B. , Schmitt, R. et al. (2008) Does anatomical completeness of the circle of Willis correlate with sufficient cross‐perfusion during unilateral cerebral perfusion. European Journal of Cardiothoracic Surgery, 33(3), 402–408. [DOI] [PubMed] [Google Scholar]
- van Seeters, T. , Hendrikse, J. , Biessels, G.J. , Velthuis, B.K. , Mali, W.P.T.M. & Kappelle, L.J. et al. (2015) Completeness of the circle of Willis and risk of ischaemic stroke in patients without cerebrovascular disease. Neuroradiology, 57, 1247–1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasović, L. , Trandafilović, M. , Jovanović, I. , Antović, A. , Stojanović, J. , Zdravković, M. et al. (2010) An excess vessel in the posterior part of the human cerebral arterial circle (CAC): a case series. BMC Neurology, 10, 53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasović, L. , Trandafilović, M. , Jovanović, I. , Ugrenović, S. , Vlajković, S. , Milić, M. et al. (2013) Morphology of the cerebral arterial circle in the prenatal and postnatal period of Serbian population. Child’s Nervous System, 29(12), 2249–2261. [DOI] [PubMed] [Google Scholar]
- Willan, P.L.T. & Humpherson, J.R. (1999) Concepts of variation and normality in morphology: important issues at risk of neglect in modern undergraduate medical courses. Clinical Anatomy, 12(3), 186–190. [DOI] [PubMed] [Google Scholar]
- Wufuer, A. , Wubuli, A. , Mijiti, P. , Zhou, J. , Tuerxun, S. , Cai, J. et al. (2017) Impact of collateral circulation status on favourable outcomes in thrombolysis treatment: a systematic review and meta‐analysis. Experimental and Therapeutic Medicine, 15(1), 707–718. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


