Abstract
Background:
Knowledge about the impacts of child abuse and neglect (CAN) experiences on late adolescent psychopathology has been limited by a failure to consider the frequent co-occurrence of CAN types and potential unique impacts of specific combinations.
Objective:
Using person-centered analyses, we aimed to identify unobserved groups of youth with similar patterns of lifetime CAN experiences before age 16 and differences in psychopathology symptom counts between groups two years later.
Participants and Setting:
Participants were 919 adolescent-caregiver dyads (56% female; 56% Black, 7% Latina/o, 13% mixed/other).
Methods:
Prospective, multi-informant data, including child protective services records and caregiver and youth reports were collected, and youth completed a diagnostic interview at age 18.
Results:
Latent Class Analyses classified adolescents into four distinct groups based on patterns of physical neglect, supervisory neglect, and physical, sexual, and psychological abuse: “Low-Risk” (37%), “Neglect” (19%), “Abuse” (11%), and “Multi-type CAN” (33%). The Multi-type CAN class had significantly more major depressive, generalized anxiety, and nicotine use symptoms than the Low-Risk class, and more post-traumatic stress, antisocial personality, and illicit substance use symptoms, than Low-Risk and Neglect classes. The Abuse class had significantly more generalized anxiety and attention deficit/hyperactivity symptoms than the Low-Risk class, and more major depressive, antisocial personality, and illicit substance use symptoms, than Low-Risk and Neglect classes. The Neglect class did not have elevated psychopathology symptoms.
Conclusion:
Findings highlight important differences in the associations between lifetime CAN experience patterns and psychopathology. Researchers should explore mechanisms underlying psychopathology that are impacted by different CAN experience patterns.
Keywords: Child abuse, Child neglect, Psychopathology, Substance use, Latent class analysis
In 2018, more than 3.5 million children in the U.S. were the subjects of investigations from child protective services (CPS) agencies for suspicion of child abuse and/or neglect (U.S. Department of Health and Human Services; 2020). CAN disrupts multiple physiological, cognitive, emotional, and behavioral developmental processes, which contribute to psychopathology beginning in childhood and persisting into adulthood (Cicchetti, 2016). Considering the effects of different CAN experiences, as well as their putative combined impacts on psychopathology, is particularly important during late adolescence, a period characterized by heightened risk for psychological disorders (Costello, Copeland, & Angold, 2011). However, methodological limitations in the extant literature have resulted in inconsistent evidence for these associations, limiting prevention efforts during late adolescence. Using a person-centered analysis strategy, the present study integrated multi-informant, prospective data to identify groups of adolescents with distinct patterns of CAN experiences prior to age 16 and examined group differences in psychopathology symptoms between ages 17 and 18.
The Impact of Child Abuse and Neglect on Psychopathology
CAN increases risk for psychopathology across the lifespan. Multiple meta-analytic studies confirm that neglect and physical, sexual, and psychological abuse are each linked to an increased risk for later depression and anxiety (Gardner, Thomas, & Erskine, 2019; Hillberg, Hamilton-Giachritsis, & Dixon, 2011; Lindert et al., 2014; Norman et al., 2012). Physical, sexual, and psychological abuse have most consistently been associated with risk for adult post-traumatic stress disorder (PTSD), alcohol, and substance use problems, but the evidence for an association between neglect and adult PTSD, alcohol, and substance use problems has been less consistent across studies (Gardner et al., 2019; Halpern et al., 2018; Hillberg et al., 2011; Messman-Moore & Bhuptani, 2017; Norman et al., 2012). Neglect and psychological abuse, and to a lesser degree physical abuse, are associated with risk for attention-deficit/hyperactivity disorder (ADHD), while no association between sexual abuse and ADHD has been identified (Clayton, Lee, Cheung, Theule, & Henrikson, 2018). Neglect, physical, and psychological abuse have also each been associated with both general and aggressive forms of antisocial behavior during late adolescence, while sexual abuse has primarily been associated with aggressive forms of antisocial behavior (Braga, Gonçalves, Basto-Pereira, & Maia, 2017).
However, attempts to isolate the unique effects of individual CAN types ignore the inherent co-occurrence of CAN experiences common among maltreated youth. Youth who experience one type of CAN are at increased risk of experiencing other types of CAN, as well as other forms of victimization and adversity (Finkelhor, Turner, Hamby, & Ormond, 2011; Herrenkohl & Herrenkohl, 2009). To account for this overlap, summed indices of the number of CAN, and broader adversity and victimization types, an individual has experienced have become important tools for screening and identification (Evans, Li, & Whipple, 2013; Finkelhor, Turner, Shattuck, & Hamby, 2015; McLaughlin & Sheridan, 2016). Though well-validated and broadly used, these cumulative risk indices are limited, as they assume that the effects of specific forms of adversity on children’s development are equivalent. It is possible that combinations of CAN experiences could have synergistic effects that have greater impacts than any one CAN experience.
Person-Centered Approaches
Whereas variable-centered models focus on the effects of individual or summed indices of CAN experiences or the interactive effects of different CAN types, person-centered models attempt to identify unobservable groups of people with similar traits, characteristics, and/or experiences (Collins & Lanza, 2010). Latent Class and Latent Profile Analysis (LC/PA) are person-centered latent variable analysis methods that can be used for identifying unobserved groups (i.e., classes or profiles) of individuals who share similar patterns of CAN experiences (Roesch, Villodas, & Villodas, 2010). Numerous CAN studies have identified groups of individuals with different patterns of co-occurring CAN types (see Debowska, Willmott, Boduszek, & Jones, 2017; Rivera, Fincham, & Bray, 2018 for reviews). However, the number of groups and specific patterns that characterize these groups have varied widely across studies. Some studies have identified groups that have experienced individual CAN types, such as neglect or physical or sexual abuse. Other studies have identified groups with specific patterns of multiple CAN experiences, such as physical and psychological abuse or all/multiple CAN types. Discrepancies in these findings are likely the result of methodological variability among studies.
A fairly consistent finding across studies is a group of individuals, often the largest group, who did not experience CAN (Debowska et al., 2017; Rivera et al., 2018). However, samples that selectively include individuals with CAN histories are not able to identify this group. Relatedly, Debowska et al. (2017) noted that studies in samples from pre-specified, high-risk populations (e.g., incarcerated, maltreated, or clinical samples) identified large groups of individuals that experienced a single CAN type (e.g., neglect, sexual abuse). Importantly, the authors also noted that these studies tended to identify larger groups of individuals who experienced multiple CAN types. Additionally, the findings of studies focused on younger samples may differ from those focused on older samples, as the overall prevalence of lifetime CAN, as well as the prevalence of certain types of CAN (e.g., sexual abuse) increases with age (Kim, Wildeman, Jonson-Reid, & Drake, 2017).
The source of CAN data could also contribute to variability in findings. The validity of retrospective CAN self-reports has been questioned for decades, and preference has been given to prospective CAN reports (C. S. Widom, Raphael, & DuMont, 2004). A recent meta-analysis reported poor agreement between prospective and retrospective CAN self-reports (Baldwin, Reuben, Newbury, & Danese, 2019). However, the authors noted that each method may identify distinct groups of victims, and that conclusions about the prevalence of CAN experiences and their associations with psychopathology could vary by method. For example, Shenk, Noll, Peugh, Griffin, and Bensman (2015) demonstrated that the strength of associations between CAN, based on CPS records, and physical and mental health outcomes increased after removing “contaminated” cases (i.e., those that retrospectively reported CAN) from the non-maltreated comparison group. CPS records are known to underrepresent CAN experiences as they only include CAN that is detected by CPS agencies (Kim et al., 2017). Importantly, Baldwin et al. (2019) reported poor agreement between prospective and retrospective CAN data regardless of the source (i.e., CPS records vs. youth or caregiver report) of prospective CAN data.
Given the limitations of each method of CAN assessment, multi-informant (e.g., CPS record, caregiver/youth report) and multi-method (e.g., prospective, retrospective) measurement is needed to maximize sensitivity for detecting CAN experiences and to obtain more robust and generalizable findings about the impact of CAN experiences on psychopathology. However, to our knowledge, no previous LC/PA study has used more than one informant or method of CAN assessment. This could explain inconsistent and non-specific findings regarding differences in psychopathology among groups. The most consistent finding across studies has been that individuals with any CAN experiences tend to exhibit more psychopathology, including depression, anxiety, PTSD, substance use, ADHD, and antisocial behavior, than individuals without CAN experiences (Debowska et al., 2017; Rivera et al., 2018). Several studies found that classes with multi-type CAN histories that included physical and/or sexual abuse had more externalizing psychopathology in childhood (Petrenko, Friend, Garrido, Taussig, & Culhane, 2012; Villodas et al., 2012) and adulthood (Charak & Koot, 2015; Vaughn, Salas-Wright, Underwood, & Gochez-Kerr, 2015) than classes with histories of neglect and/or psychological abuse, but few other differences have been consistently detected.
Current Study
The purpose of the current study was to identify unobserved groups of adolescents with distinct patterns of lifetime CAN experiences that occurred between birth and age 16 using LCA and examine group differences in mental health symptoms during late adolescence (i.e., between ages 17 and 18 years old). This study builds on prior studies in several important ways. First, the present study takes a “sensitivity” approach to identifying CAN experiences. Given the limitations of each source of CAN data, we integrated all available indicators of each CAN type, including whenever possible, CPS records, caregiver reports, and youth reports. Second, data were collected prospectively as well as retrospectively to ensure that our lifetime estimates of CAN include as many cases as possible (Baldwin et al., 2019; Kim et al., 2017). Third, our sample was drawn from a cohort that was characterized as being at-risk for CAN during early childhood and followed prospectively through age 18 in a multi-site, longitudinal study. This facilitates detection of the full range of lifetime CAN experiences in adolescents at elevated risk. Although participants were sampled to overrepresent youth with CPS investigations, just less than one-half of the participants were not investigated and were considered at-risk based on demographic risk factors for CAN.
The number of classes was considered exploratory and no a priori hypotheses were made. Based on the previous literature, we expected to find a class with no or low CAN experiences. We also expected to find at least one class with combinations of multiple CAN types. Given that our sample was recruited based on CAN risk during early childhood, when the prevalence of neglect is the highest, we also expected to identify a class primarily characterized by experiences of neglect. Consistent with previous research and theory, we hypothesized that individuals in all CAN classes would have a greater number of past year major depressive (MDD), generalized anxiety (GAD), PTSD, ADHD, antisocial personality (ASPD), and substance use disorder symptoms relative to the class with no CAN experiences. We also anticipated that classes characterized by histories of multiple CAN types that included physical and/or sexual abuse would have more PTSD, ASPD, and substance use symptoms than classes with histories of neglect and/or psychological abuse, but not physical and/or sexual abuse.
Method
Sample
The present study included data from 919 youth and their caregivers who participated in the Longitudinal Studies of Child Abuse and Neglect (LONGSCAN). LONGSCAN is an ongoing multisite consortium of prospective studies that investigate the antecedents and outcomes of childhood maltreatment. Five research sites throughout the United States (e.g., Eastern, Midwestern, Northwestern, Southern, and Southwestern) recruited participants who were identified as being at-risk for abuse and/or neglect (e.g., families investigated by CPS for maltreatment allegations, families screened as high-risk due to demographic factors at pediatric clinics; see Runyan et al. (2014) for a more detailed description)1. Of the original sample enrolled in the study (N=1,354), 919 adolescents (69%) completed the age 18 interview and were included in the present study (mean age = 18.51 years, SD = .61). The current sample included 52% female participants and 53% Black, 26% White, 7% Hispanic, and 14% mixed/other ethnicity individuals (see Table 1 for demographic data).
Table 1.
Sample descriptive statistics.
| N (%) Total N = 919 |
M (SD) | |
|---|---|---|
|
| ||
| Poverty | 741 (80.6%) | |
| Female | 513 (55.8%) | |
| Age | 18.51 (.61) | |
| Race/Ethnicity | ||
| White | 227 (24.7%) | |
| Black | 511 (55.6%) | |
| Latinx | 61 (6.6%) | |
| Other | 120 (13.1%) | |
| Physical neglect | 470 (51.1%) | |
| Supervisory neglect | 388 (42.2%) | |
| Psychological abuse | 443 (48.2%) | |
| Physical abuse | 567 (61.7%) | |
| Sexual abuse | 196 (21.3%) | |
| Major depressive symptoms | 4.42 (4.46) | |
| Generalized anxiety symptoms | 1.91 (2.16) | |
| Post-traumatic stress symptoms | 1.14 (2.83) | |
| Attention-deficit/hyperactivity symptoms | 3.44 (4.14) | |
| Antisocial personality symptoms | .81 (1.22) | |
| Nicotine use symptoms | .47 (1.36) | |
| Alcohol use symptoms | .40 (1.46) | |
| Marijuana use symptoms | .56 (1.69) | |
| Illicit substance use symptoms | .13 (1.12) | |
Note: M = mean; SD = standard deviation.
Procedures
Each LONGSCAN site obtained approval from their respective institutional review boards and written, informed consent/assent was acquired from all participating caregivers and children. Briefly, at-risk children and their caregiver1s were recruited to participate before they were 4 years old and were subsequently interviewed in-person, in their homes, biannually between ages 4 and 18 years. These interviews included questions regarding the child’s development and experiences of physical, sexual, and psychological abuse and were completed on laptop computers, using Audio Computer-Assisted Self-Interviews (ACASI) for privacy. Each LONGSCAN site also systematically reviewed CPS records continuously until the youth reached 16 years of age to identify reports of alleged maltreatment for each youth/family and coded the maltreatment narratives by type and severity using the Modified Maltreatment Classification System (MMCS; English & Investigators, 1997). Coders at each site were trained to use the MMCS by experienced coders until they reached 90% agreement with the gold standard. To further ensure reliable coding, coders at all five sites coded a subsample (n = 109) of the CPS narratives that represented cases from each site. The decision to include allegations of CAN was based on previous findings that CAN substantiations underestimate the prevalence of CAN and children with alleged and substantiated maltreatment are at a similarly increased risk for CAN recidivism and mental health and behavioral consequences (Hussey et al., 2005; Kohl, Jonson-Reid, & Drake, 2009) and is consistent with our focus on maximizing the sensitivity of identifying CAN experiences.
Measures
A full description of the LONGSCAN measures is available elsewhere. Here we describe the measures used in the present study.
Sociodemographics
Children’s sex and race/ethnicity were collected during the baseline interview at age 4. A sociodemographic measure was completed by caregivers at each interview, which included reports of household income and the number of dependent individuals. These data were used to calculate whether each family’s income fell above or below the federal poverty level for the year during which they completed each interview. Based on this information, a dichotomous indicator of whether or not adolescents ever lived in a family with an income below the federal poverty limit between birth and the age 16 interview was created.
Neglect
Two dichotomous indicators were created based on the MMCS coded CPS reports to represent whether or not there was any evidence that adolescents experienced physical or supervisory neglect between birth and the age 16 interview.
Physical abuse
A dichotomous indicator was created to assess physical abuse between birth and the age 16 interview based on all available data. In addition to the MMCS, caregivers reported whether they engaged in any physically aggressive behaviors toward the youth in the past year on the Conflict Tactics Scales-Parent-Child version (CTSPC; Straus, Hamby, Finkelhor, Moore, & Runyan, 1998). They completed the severe physical assault scale (3 items; e.g., hit child with fist or kicked hard) at the age 8, 12, 14, and 16 interviews, and the extreme physical assault scale (4 items; e.g., burned or scalded child on purpose) at the age 12, 14, and 16 interviews. Although these scales demonstrated discriminant and construct validity, they tend to show weak evidence of internal consistency because of the relatively low frequency of each of the behaviors (Straus et al., 1998). At the age 12 and 16 interviews, adolescents completed a 15-item self-report measure of physical abuse experiences, between birth and age 12 and since age 12, respectively, derived from the corresponding MMCS categories (e.g., endangerment, physical injury). It was designed to maximize construct validity and demonstrated evidence of discriminant validity in the LONGSCAN sample (Knight, Smith, Martin, Lewis, & the LONGSCAN Investigators, 2008; Knight, Smith, Martin, & the LONGSCAN Investigators, 2009). If any adolescent, caregiver, or CPS indicator was endorsed physical abuse was coded 1 = present.
Sexual abuse
A dichotomous indicator was created to assess sexual abuse between birth and the age 16 interview based on all available data. In addition to the MMCS, at the age 12 and 16 interviews, adolescents completed an 11-item self-report measure of sexual abuse experiences, between birth and age 12 and since age 12, respectively, derived from the corresponding MMCS categories (e.g., non-contact, fondling, oral-genital contact, penetration). This measure was designed to maximize construct validity and demonstrated evidence of discriminant validity in the LONGSCAN sample (Knight et al., 2008; Knight et al., 2009). If adolescents endorsed any self-report items or had a CPS allegation, sexual abuse was coded 1 = present.
Psychological abuse
A dichotomous indicator was created to assess psychological abuse between birth and the age 16 interview based on all available data. In addition to the MMCS, at the age 12 and 16 interviews, adolescents completed an 18-item self-report measure of sexual abuse experiences, between birth and age 12 and since age 12, respectively, derived from the corresponding MMCS categories (e.g., threats of harm, humiliation). This measure was designed to maximize construct validity and demonstrated evidence of discriminant validity in the LONGSCAN sample (Knight et al., 2008; Knight et al., 2009). If adolescents endorsed any self-report items or had a CPS allegation, psychological abuse was coded 1 = present.
Psychopathology symptoms
Adolescents completed the Computerized National Institute of Mental Health Diagnostic Interview Schedule for Children (DISC-IV) (Shaffer, Fisher, Lucas, Dulcan, & Schwab-Stone, 2000) at age 18. The DISC-IV was designed to assess for symptoms of MDD, GAD, PTSD, ADHD, ASPD, and substance use disorders, including tobacco use, marijuana use, alcohol use, and “other” substance use disorder. The DISC-IV has been empirically validated and scoring algorithms have been developed to calculate symptom counts for each disorder. Symptoms of other illicit substance use disorders, including stimulant, sedatives/tranquilizer, cocaine/crack, heroin, opiate, PCP, hallucinogen, amyl nitrite, inhalant, unprescribed steroid, or illicit substances are not differentiated and count toward the illicit substance use symptom count.
Data Analysis
LCA in Mplus version 8 (Muthén & Muthén, 2017) was used to identify classes of adolescents based on five dichotomous indicators of CAN between birth and age 16: (1) physical neglect, (2) supervisory neglect, (3) physical abuse, (4) sexual abuse, and (5) psychological abuse. Each of these indicators included information coded from CPS records using the MMCS, as well as all available information about adolescents’ CAN experiences. The sexual and psychological abuse indicators also included adolescent self-reports, while the physical abuse indicator included adolescent self-reports and caregiver reports. Consistent with recommendations (Nylund, Asparouhov, & Muthén, 2007) the fit of models with increasing numbers of latent classes was compared sequentially until adding an additional class increased the sample-size-adjusted Bayesian Information Criterion (BIC) value and the Boot-strapped Likelihood Ratio (BLRT) and Lo-Mendell Rubin Likelihood Ratio (LMR) tests were not significant. Model entropy was considered as an index of classification accuracy and identified classes were interpreted based on Latent Class Probabilities (i.e., the probability that each case would be assigned to each class) and Conditional Response Probabilities (CRPs; i.e., the probability that an individual in a particular class would have each CAN experience; Collins & Lanza, 2010)
Next, sex, race/ethnicity, and poverty history were tested in a multinomial logistic regression as predictors of adolescents’ most likely class membership using a modification of the manual Bolck, Croon, and Hagenaars (BCH) method (Bakk & Vermunt, 2016), described by Asparouhov and Muthén (2014). We then tested group differences in past year symptom counts for MDD, GAD, PTSD, ADHD, ASPD, nicotine use, alcohol use, marijuana use, and illicit substance use disorders at age 18, based on adolescents’ most likely class membership, controlling for sex, race/ethnicity, and poverty history using negative binomial regression via the manual BCH method. Given our focus on identifying distinct patterns of lifetime CAN experiences that occurred any time between birth and age 16, we were unable to establish temporal precedence by controlling for prior psychopathology. As a result, we were unable to predict late adolescent psychopathology or predict changes in psychopathology over time. Instead, we were able to examine associations between lifetime CAN patterns and late adolescent psychopathology. Odds ratios (ORs), incident rate ratios (IRRs), and their respective 95% confidence intervals (CIs) are reported accordingly.
Results
Missing Data
The 919 adolescents who completed the age 18 interview and were included in the present study did not significantly differ from adolescents who did not complete the age 18 interview on race/ethnicity, χ2 (3) = 6.92, p > .05, risk for child maltreatment before study recruitment, χ2 (1) = .06, p > .05, or clinically elevated baseline (age 4) internalizing, χ2 (1) = 1.81, p > .05, or externalizing problems, χ2 (1) = .01, p > .05. A significantly higher proportion of females (74%) completed the age 18 interview than males (62%; χ2 (1) = 21.62, p < .001). Full information Maximum Likelihood estimation was used in all models and sex was included as a covariate.
Latent Class Analysis
A four-class solution provided the best fit to the data; adding a fifth class resulted in an increased BIC and non-significant BLRT and LMR (Table 2). The first class characterized 346 adolescents (37%) with low CRPs for each CAN indicator (Figure 1). Although the CRP for physical abuse was somewhat elevated (.386), this was expected given that the sample was high risk, and this probability was substantially lower than the sample average probability (.617). This was labeled the “Low-Risk” class. The second class characterized 171 adolescents (18%) with high probabilities for supervisory and physical neglect, probabilities for psychological abuse that were similar to the sample average probabilities, and low probabilities for physical and sexual abuse, relative to the sample averages. This was labeled the “Neglect” class. The third class characterized 301 adolescents (33%) with high probabilities of all CAN indicators relative to the sample average probabilities. This was labeled the “Multi-type CAN” class. Finally, the fourth class characterized 101 adolescents (11%) with low probabilities of supervisory and physical neglect, high probabilities of psychological and physical abuse, and approximately sample-average probabilities of sexual abuse. This was labeled the “Abuse” class.
Table 2.
Latent Class Analysis fit indicators.
| BIC | BLRT | LMR | Entropy | |
|---|---|---|---|---|
|
| ||||
| 1-Class | 5992.05 | -- | -- | -- |
| 2-Class | 5438.06 | 575.87* | 562.14* | .69 |
| 3-Class | 5409.93 | 50.02* | 48.82* | .72 |
| 4-Class | 5398.13 | 38.83 * | 37.89 * | .65 |
| 5-Class | 5417.32 | 2.70 | 2.64 | .69 |
Note: BIC = Sample-size-adjusted Bayesian Information Criterion; BLRT = Bootstrapped Likelihood Ratio Test; LMR = Lo-Mendell-Rubin Likelihood Ratio Test.
p < .05
Figure 1.
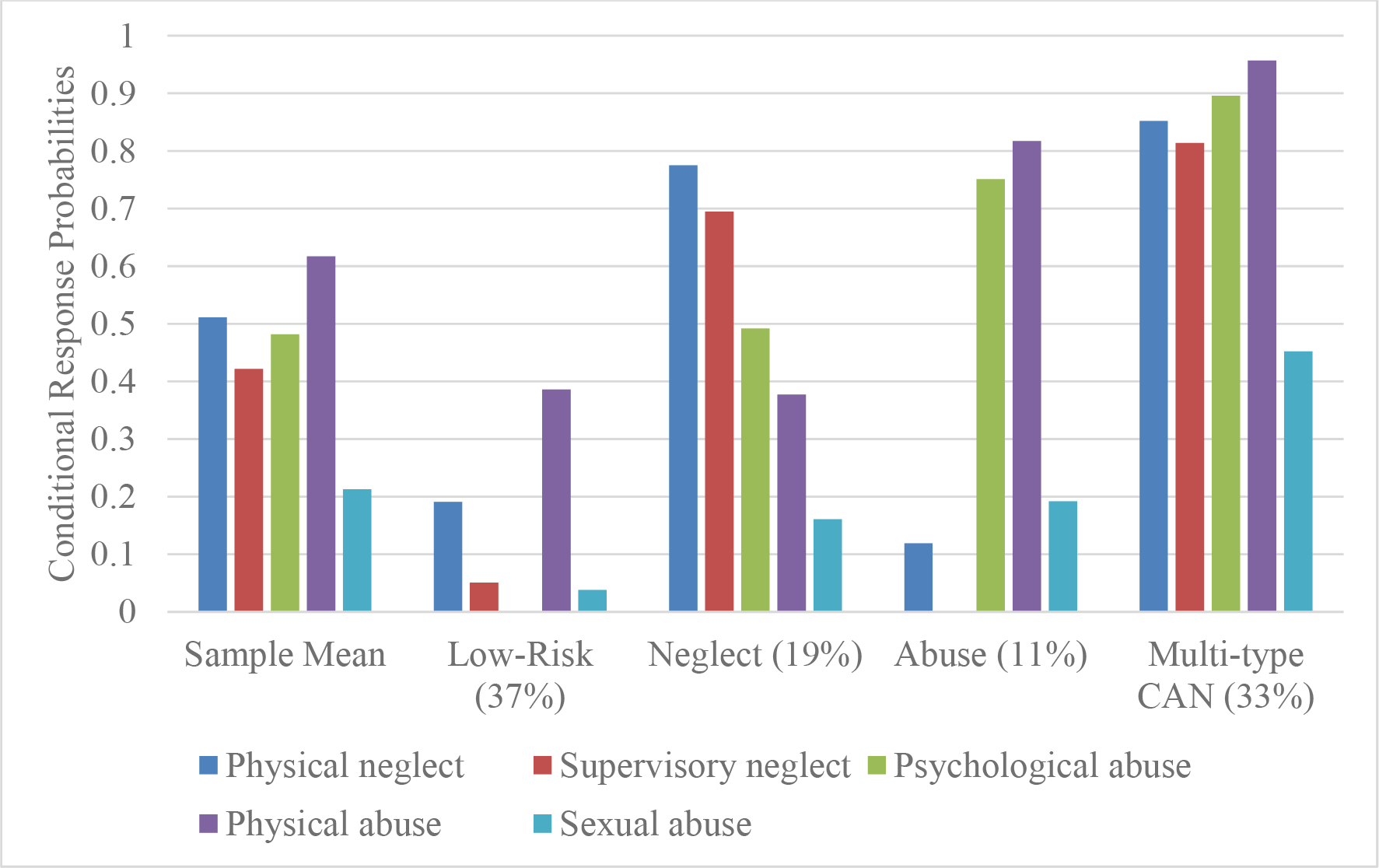
Conditional Response Probabilitlies in Each Latent Class.
There were no significant differences in the likelihood of being assigned to each class based on sex and poverty history (see Table 3). White adolescents were significantly more likely than Black adolescents to be assigned to the Neglect, Abuse, and Multi-type CAN classes, relative to the Low-Risk class. They were also more likely than Black adolescents to be assigned to the Multi-type CAN class relative to the Neglect class.
Table 3.
Predictors of most likely class membership.
| Neglect (vs. Low-Risk) | Multi-type CAN (vs. Low-Risk) | Abuse (vs. Low-Risk) | Multi-type CAN (vs. Neglect) | Abuse (vs. Neglect) | Multi-type CAN (vs. Abuse) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | |
|
| ||||||||||||
| Female | 1.07 | [0.66, 1.74] | 1.22 | [0.79, 1.88] | 1.06 | [0.60, 1.87] | 1.14 | [0.69, 1.86] | 1.14 | [0.61, 2.12] | 1.29 | [0.73, 2.30] |
| Poverty | 1.31 | [0.90, 1.90] | 1.37 | [0.99, 1.90] | 1.34 | [0.86, 2.11] | 1.05 | [0.71, 1.54] | 1.03 | [0.62, 1.69] | 1.02 | [0.64, 1.62] |
| White1 | 1.98* | [1.25, 3.14] | 3.25* | [2.16, 4.85] | 1.95* | [1.12, 3.38] | 1.64* | [1.03, 2.60] | 1.02 | [0.56, 1.85] | 1.67 | [0.96, 2.90] |
| Latinx2 | 1.16 | [0.51, 2.65] | 1.10 | [0.55, 2.16] | 1.62 | [0.55, 4.78] | 1.06 | [0.49, 2.30] | 1.40 | [0.45, 4.39] | 1.48 | [0.52, 4.24] |
| Other2 | 1.25 | [0.62, 2.53] | 1.28 | [0.73, 2.23] | 1.09 | [0.49, 2.40] | 1.59 | [0.84, 3.02] | 1.35 | [0.58, 3.18] | 1.18 | [0.57, 2.45] |
Note: AOR = adjusted odds ratio; CI = confidence interval.
P< .05
Black reference group
White reference group.
Psychopathology
Each outcome was significantly over-dispersed, αs ranging from .89 to 135.25, ps < .001, so negative binomial regressions were conducted. See Table 4 for IRRs and 95% Cis.
Table 4.
Differences in psychopathology symptoms between classes.
| Major Depressive | Generalized Anxiety | Post-Traumatic Stress | Attention-Deficit/Hyperactivity | Antisocial Personality Disorder | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| IRR | 95%CI | IRR | 95%CI | IRR | 95%CI | IRR | 95%CI | IRR | 95%CI | |
|
| ||||||||||
| Poverty | 0.94 | [0.80, 1.11] | 0.97 | [0.80, 1.17] | 1.25 | [0.77, 2.01] | 0.78* | [0.63, 0.97] | 0.81 | [0.63, 1.04] |
| Female | 1.12 | [0.98, 1.29] | 1.15 | [0.99, 1.34] | 1.33 | [0.92, 1.93] | 0.90 | [0.76, 1.06] | 0.62* | [0.51, 0.75] |
| Race/Ethnicity | ||||||||||
| Black1 | 0.96 | [0.82, 1.14] | 1.06 | [0.88, 1.29] | 1.20 | [0.79, 1.83] | 1.03 | [0.83, 1.28] | 0.97 | [0.76, 1.23] |
| Latinx1 | 0.67* | [0.49, 0.91] | 0.85 | [0.60, 1.22] | 0.67 | [0.24, 1.84] | 0.82 | [0.55, 1.23] | 1.12 | [0.73, 1.72] |
| Other1 | 0.87 | [0.70, 1.08] | 0.90 | [0.69, 1.19] | 0.51 | [0.26, 1.01] | 1.03 | [0.77, 1.38] | 1.08 | [0.77, 1.52] |
| Classes | ||||||||||
| Neglect2 | 1.16 | [0.94, 1.43] | 1.24 | [0.99, 1.55] | 0.93 | [0.54, 1.59] | 1.25 | [0.98, 1.61] | 0.94 | [0.68, 1.29] |
| Abuse2 | 1.65* | [1.35, 2.01] | 1.45* | [1.13, 1.85] | 1.60 | [0.95, 2.71] | 1.40* | [1.09, 1.80] | 1.47* | [1.06, 2.04] |
| Multi-type CAN2 | 1.36* | [1.14, 1.62] | 1.26* | [1.04, 1.52] | 1.60* | [1.06, 2.42] | 1.21 | [0.98, 1.49] | 1.38* | [1.09, 1.75] |
| Abuse3 | 1.41* | [1.13, 1.78] | 1.17 | [0.89, 1.54] | 1.72 | [0.92, 3.22] | 1.12 | [0.84, 1.49] | 1.57* | [1.07, 2.30] |
| Multi-type CAN3 | 1.17 | [0.96, 1.43] | 1.02 | [0.81, 1.27] | 1.72* | [1.01, 2.93] | 0.96 | [0.75, 1.23] | 1.48* | [1.09, 2.00] |
| Multi-type CAN4 | 0.83 | [0.68, 1.00] | 0.87 | [0.68, 1.11] | 1.00 | [0.60, 1.67] | 0.86 | [0.67, 1.11] | 0.94 | [0.69, 1.29] |
Note: CI = confidence interval; IRR = Incident Rate Ratio
p < .05
White reference group
Low-Risk reference group
Neglect reference group
Abuse reference group
Major Depressive Disorder
Adolescents in the Multi-type CAN class, B = .31, p < .001, and the Abuse class, B = .50, p < .001, had 1.36 and 1.65 times more MDD symptoms, respectively, than adolescents in the Low-Risk class. Adolescents in the Abuse class also had 1.41 times more MDD symptoms than those in the Neglect class, B = .35, p = .003. The Multi-type CAN class did not significantly differ from the Neglect or Abuse classes.
Generalized Anxiety Disorder
Adolescents in the Multi-type CAN class, B = .23, p = .018, and the Abuse class, B = .37, p = .005, had 1.26 and 1.45 times more GAD symptoms, respectively, than adolescents in the Low-Risk class. The Neglect class did not significantly differ from the other classes and the Abuse and Multi-type CAN classes were not significantly different from each other.
Post-Traumatic Stress Disorder
Adolescents in the Multi-type CAN class had 1.60 times and 1.72 times more PTSD symptoms than adolescents in the Low-Risk class, B = .47, p = .027, or the Neglect class, B = .54, p = .047, respectively, but did not significantly differ from the Abuse class. The Neglect and Abuse classes were not significantly different from the Low-Risk class, and also did not differ from each other.
Attention-Deficit/Hyperactivity Disorder
Adolescents in the Abuse class had 1.40 times more ADHD symptoms than adolescents in the Low-Risk class, B = .34, p = .009, but did not significantly differ from any other classes. The Multi-type CAN and Neglect classes did not differ significantly from each other or from the Low-Risk class.
Antisocial Personality Disorder
Adolescents in the Multi-type CAN class had 1.38 times and 1.48 times more ASPD symptoms than adolescents in the Low-Risk class, B = .32, p = .008, or the Neglect class, B = .39, p = .012, respectively. Adolescents in the Abuse class had 1.47 times and 1.57 times more ASPD symptoms than adolescents in the Low-Risk class, B = .39, p = .021, or the Neglect class, B = .45, p = .020, respectively. Adolescents in the Multi-type CAN class did not significantly differ from adolescents in the Abuse class, and adolescents in the Neglect class did not differ significantly from adolescents in the Low-Risk class.
Substance Use Disorders
Adolescents in the Multi-type CAN class had 1.88 times more nicotine use disorder symptoms than adolescents in the Low-Risk class, B = .63, p = .020, but did not significantly differ in nicotine use disorder symptoms from the Abuse or Neglect classes. The difference between Abuse, Neglect, and Low-Risk classes in their nicotine use disorder symptoms was not significant. None of the classes statistically differed in their alcohol use or marijuana use disorder symptoms. Adolescents in the Multi-type CAN class had 7.31 and 9.04 times more illicit substance use symptoms than adolescents in the Low-Risk class, B = 1.99, p = .030, or the Neglect class, B = 2.20, p = .003, respectively. Adolescents in the Abuse class had 7.91 times and 9.78 times more illicit substance use symptoms than adolescents in the Low-Risk class, B = 2.07, p = .043, or the Neglect class, B = 2.28, p = .014, respectively. Adolescents in the Multi-type CAN class did not differ significantly from adolescents in the Abuse class with regard to their illicit substance use disorder symptoms, and adolescents in the Neglect class did not significantly differ from adolescents in the Low-Risk class.
Discussion
Using a person-centered analysis strategy (i.e., LCA), the present study identified four groups of adolescents characterized by distinct combinations of lifetime CAN experiences, as well as group differences in psychopathology symptoms during late adolescence. This study builds from previous investigations and had unique strengths, including the use of multi-informant CAN data from a prospective cohort of youth identified as at risk of CAN during early childhood. As expected, adolescents who experienced multiple forms of CAN that included physical and/or sexual abuse had more MDD, GAD, ASPD, and substance use disorder symptoms between ages 17 and 18 than adolescents who were less likely to have experienced CAN. Although adolescents who primarily experienced neglect did not have significantly more symptoms of any disorders than adolescents at low risk for CAN, all participants were considered to be at-risk for CAN before the study. Also unexpectedly, adolescents with primarily physical, psychological, and sexual abuse experiences had elevated symptoms of ADHD relative to adolescents at low risk for CAN; however, adolescents who experienced these forms of abuse in addition to neglect and adolescents who primarily experienced neglect did not. Adolescents at risk for multi-type CAN experiences only differed from youth with primarily neglect experiences on PTSD, ASPD, and illicit substance use symptoms. They did not significantly differ from youth with primarily physical, psychological, and sexual abuse experiences on symptoms of any disorder considered here. These findings extend our understanding of the associations between lifetime CAN experiences and late adolescent psychopathology and provide important implications for mental health prevention.
Patterns of Lifetime Child Abuse and Neglect
Among maltreated youth, there is a high likelihood of experiencing more than one type of CAN, with some studies reporting rates of multi-type CAN as high as 94% (Finkelhor et al., 2011; Herrenkohl & Herrenkohl, 2009). Indeed, in the present study there were high rates of overlap in adolescents’ lifetime experiences of CAN. Consistent with previous LC/PA studies, the largest class was at relatively low risk for most forms of CAN across their lifetimes (Debowska et al., 2017; Rivera et al., 2018). However, the second largest class, comprising approximately one-third of the sample, was characterized by elevated probabilities of having experienced all types of CAN. Previous LC/PAs of CAN experiences have often identified a similar class as the smallest class/profile (Debowska et al., 2017; Rivera et al., 2018). Our findings likely result from several methodological aspects of the current study. First, our sample was identified as at-risk for CAN during early childhood and just over one-half had reports of CAN before joining the study. It is likely that we were able to differentiate more individuals with this particular pattern of CAN experiences because of the increased prevalence of CAN in this sample. We also applied a sensitivity approach to maximize our detection of each type of CAN using all available data from multiple informants, as well as prospective and retrospective data. Findings indicate that experiencing many types of CAN across childhood and adolescence is quite common.
Interestingly, two distinct classes characterized primarily by different forms of neglect and different forms of abuse, respectively, were delineated. The class characterized primarily by neglect comprised nearly one-fifth of the sample. Although neglect is the most prevalent form of CAN, especially during early childhood, findings from this sample illustrate that, when considering lifetime experiences, more youth experience abuse in addition to neglect than neglect alone. Similarly, experiencing abuse in the absence of neglect was fairly uncommon, with just over one-tenth of the sample comprising this pattern of lifetime CAN experiences. Recently, the Dimensional Model of Adversity and Psychopathology (DMAP), a dimensional cumulative risk model that differentiates experiences of deprivation from experiences of threat, has emphasized the unique impacts of these experiences on underlying developmental systems (McLaughlin & Sheridan, 2016). Though accumulating evidence supports the existence of distinctive clusters of deprivation and threat experiences among children who have experienced adversity (e.g., Sheridan, Shi, Miller, Sahali, & McLaughlin, 2019), our findings indicate that, in this high-risk sample, overlapping experiences of deprivation (e.g., neglect) and threat (e.g., abuse) are more common than experiencing these forms of adversity in isolation. Thus, studies attempting to identify the impacts of deprivation and threat experiences should be careful to consider the co-occurrence of these two dimensions.
Psychopathology Symptoms
In the present study, adolescents with CAN experiences that included physical, sexual, and/or psychological abuse had more symptoms of psychopathology during late adolescence than adolescents at low risk for CAN and those with primarily neglect experiences, in general. This pattern was particularly pronounced for symptoms of MDD, GAD, ASPD, and illicit substance use. Several previous LC/PA studies found that groups with similar patterns of CAN experiences had elevated externalizing psychopathology than groups with patterns of CAN experiences that did not include physical, sexual, and/or psychological (Charak & Koot, 2015; Petrenko et al., 2012; Vaughn et al., 2015; Villodas et al., 2012). Also, each of these forms of abuse have been linked to depression, anxiety, alcohol and substance use problems, and antisocial behavior previously (Braga et al., 2017; Gardner et al., 2019; Halpern et al., 2018; Hillberg et al., 2011; Lindert et al., 2014; Norman et al., 2012). However, experiences of neglect have also been linked to depression, anxiety, and antisocial behavior. Our findings indicate that, when considering the co-occurrence of lifetime experiences of CAN, neglect may not be independently associated with these forms of psychopathology in the absence of abuse experiences during late adolescence. These findings are also aligned with empirical and theoretical literature examining the mechanisms through which threatening experiences impact youth. For example, studies indicate that difficulties with differentiating and paying disproportionate attention to threatening cues, and increased stress reactivity and deficits in emotion regulation underlie a variety of psychological disorders, including anxiety, depressive, and substance use disorders (McLaughlin & Lambert, 2017). These difficulties may also underlie social-information processing deficits (e.g., hostile attribution bias; Dodge, Pettit, Bates, & Valente, 1995) that underlie aggressive and violent antisocial behaviors among abused youth, and deficits in emotional processing likely contribute to a lack of empathy.
Deficits in threat processing and emotion regulation are also thought to underlie many PTSD symptoms. Although a similar pattern emerged for PTSD symptoms (i.e., classes with physical, sexual, and/or psychological abuse experiences had more symptoms), only the Multi-type CAN class significantly differed from the Low-Risk and Neglect classes. The mean number of symptoms in the Abuse class was nearly identical to that of the Multi-type CAN class, but the magnitude of differences between the Abuse class and the other classes may have been too small to reliably identify, given that the Abuse class was the smallest identified. Previous studies have consistently identified an association between physical, sexual, and psychological abuse and PTSD symptoms, and less consistently between neglect and PTSD symptoms (Gardner et al., 2019; Hillberg et al., 2011; Messman-Moore & Bhuptani, 2017; Norman et al., 2012). Moreover, using the DMAP framework, Heleniak, McLaughlin, Ormel, and Riese (2016) found that threat-related adversities, independent of deprivation experiences, contribute to heightened threat-sensitivity and stress reactivity, increasing risk for PTSD symptoms, such as intrusive memories, increased arousal and reactivity, hypervigilance, avoidance, cognitive and affective disturbance.
Only the Abuse class had significantly more ADHD symptoms than the Low-Risk class. Previous studies have identified that neglect and psychological abuse were most consistently associated with ADHD, while the association between physical abuse and ADHD was less consistent and no association was found between sexual abuse and ADHD (Clayton et al., 2018). Studies have reported that the inherent absence of cognitive and social inputs among youth who experience deprivation, such as neglect, are associated with impairments in cognitive control, working memory, and inhibition; deficits associated with ADHD symptoms (Bos, Fox, Zeanah, & Nelson Iii, 2009; Machlin, Miller, Snyder, McLaughlin, & Sheridan, 2019). We would have expected that each of the classes that experienced CAN would have increased risk for ADHD, relative to the Low-Risk class and that this difference would be pronounced for classes that included neglect and psychological abuse (e.g., the Neglect and Multi-type CAN classes). On the other hand, abuse experiences can disrupt core cognitive and regulatory processes, such as attention, concentration, memory, and response inhibition, which are known to underlie deficits similar to those seen in ADHD (Kelly et al., 2015; Monahan, King, Shulman, Cauffman, & Chassin, 2015; Perkins, Smith-Darden, Ametrano, & Graham-Bermann, 2014). It is worth noting that disruptions in many of these processes have also been found to underlie cognitive disturbances that are common to PTSD (Adams et al., 2015), suggesting that the elevated ADHD symptoms observed here may overlap with PTSD symptoms.
Finally, we were surprised that adolescents who experienced primarily neglect did not have significant elevations in any mental health symptoms. Extensive research has documented the pernicious effects of neglect experiences on multiple developmental domains, as well as psychopathology (e.g., depression, anxiety, ADHD, antisocial behavior; for review, see Braga et al., 2017; Clayton et al., 2018; Norman et al., 2012). It should be noted that all participants in the present study were recruited because they were at risk for CAN and a substantial proportion of the “Low-Risk” class had experienced physical abuse. Also, given that the prevalence of neglect is highest during early childhood and declines across development, it is possible that the distal impact of most youths’ neglect experiences diminished by age 18. Indeed, recent studies have shown that adolescent neglect was most strongly associated with substance use in early adulthood (Dubowitz et al., 2019). However, given the hierarchical nature of development, as well as previous findings demonstrating long-term impacts of early childhood neglect (Chapple, Tyler, & Bersani, 2005; Cathy Spatz Widom & Nikulina, 2012), we would still expect to find evidence that early experiences impact psychopathology during late adolescence.
Limitations
Despite these promising findings, this study has several limitations that should be noted. Given that the sample was recruited on the basis of being at-risk for maltreatment during early childhood, the findings may not generalize to broader populations. Despite the large, prospective at-risk sample included in this study, some of the specific classes identified were relatively small and may be difficult to detect in smaller and/or lower-risk samples. Although we were able to integrate information from multiple sources about CAN experiences, the sources that were available varied for different types of CAN. To maximize the sensitivity of our measures, we used all available information for each CAN type. However, caregiver and self-report measures of neglect are scarce and retrospective measures of neglect had the poorest agreement with prospective measures (Baldwin et al., 2019). Thus, we relied only on CPS records of neglect experiences. Given our integration of multiple sources of information that each used different scales, we were not able to preserve the dimensional nature of some of the original variables. We also were not able to examine the developmental timing of CAN experiences. This will be important for future studies to consider, as the effects of CAN that occurs during different developmental periods on late adolescent adjustment may vary (Thornberry, Henry, Ireland, & Smith, 2010). We could not determine the temporal precedence of the effects of specific CAN experience patterns on psychopathology symptoms while accounting for psychopathology during earlier developmental periods. Finally, though we used an empirically validated measure of psychopathology symptoms (DISC-IV), we relied on a single informant of those symptoms, which is not ideal. Future studies using more robust psychopathology assessment strategies are warranted.
Implication and Conclusions
This study provides critical new insights into patterns of lifetime CAN experiences and their associations with psychopathology during late adolescence. Cumulative risk screening tools that create an index score of an individual’s number of lifetime adversities or victimization experiences have been increasingly integrated in clinical and CPS settings to account for the frequent co-occurrence among different victimization experiences (Evans et al., 2013; Finkelhor et al., 2015). For example, California recently started training and reimbursing providers for conducting adverse childhood experiences screenings across health care settings. However, these indices obscure the qualitative differences in the effects of particular combinations of CAN experiences. Our findings suggest that considering an individual’s CAN experiences from a person-centered perspective is crucial, as experiencing different combinations of CAN types are associated with different late adolescent psychopathology symptoms. It may be more useful to identify dimensions of adversity experiences, such as those identified by frameworks such as DMAP (McLaughlin & Sheridan, 2016), that will provide more nuanced and accurate information about mental health risk. Additional research is need to examine whether the impact of these patterns of experiences is moderated by individual characteristics (e.g., age, sex).
Youth whose lifetime experiences included physical, psychological, and/or sexual abuse generally had the highest number of late adolescent psychopathology symptoms, including symptoms of MDD, GAD, ASPD, and substance use. Given the lack of specificity in the effects of these abuse experiences, it will be important for future researchers to consider their developmental impacts on systems that underlie each of these disorders. For example, research using the DMAP framework (McLaughlin & Sheridan, 2016) has focused on identifying the mechanisms that account for associations between specific dimensions of adversity and psychopathology. Though extensive research has documented the impact of childhood neglect experiences on later psychopathology, the impact of these experiences independent of abuse experiences were not pronounced in the current study. Our findings highlight the importance of considering the potential combined effects of abuse and neglect experiences on psychopathology. Given the high rates of co-occurrence among CAN experiences, it will be important for research using dimensional frameworks to consider the overlapping and potentially synergistic effects of co-occurring dimensions of adversity. Unfortunately, this approach has been utilized in a limited number of extant studies to date. Identifying the mechanisms underlying the unique and combined effects of different CAN types on psychopathology symptoms is critical to the design and/or refinement of interventions more precisely targeted to address the specific deficits experienced by the heterogeneous population of CAN victims.
Table 5.
Differences in substance use between classes.
| Nicotine Use | Alcohol Use | Marijuana Use | Illicit Substance Use | |||||
|---|---|---|---|---|---|---|---|---|
| IRR | 95%CI | IRR | 95%CI | IRR | 95%CI | IRR | 95%CI | |
|
| ||||||||
| Poverty | 0.88 | [0.54, 1.45] | 1.06 | [0.56, 2.01] | 0.59 | [0.34, 1.01] | 0.93 | [0.28, 3.13] |
| Female | 0.73 | [0.47, 1.14] | 0.55* | [0.32, 0.92] | 0.49* | [0.32, 0.74] | 0.12* | [0.04, 0.32] |
| Race/Ethnicity | ||||||||
| Black1 | 0.42* | [0.27, 0.66] | 0.32* | [0.17, 0.60] | 0.94 | [0.52, 1.69] | 0.04* | [0.02, 0.11] |
| Latinx1 | 0.54 | [0.23, 1.26] | 0.82 | [0.39, 1.71] | 1.60 | [0.63, 4.08] | 0.35 | [0.04, 3.10] |
| Other1 | 0.80 | [0.46, 1.40] | 0.76 | [0.37, 1.57] | 1.40 | [0.69, 2.83] | 0.18* | [0.04, 0.88] |
| Classes | ||||||||
| Neglect2 | 1.13 | [0.59, 2.17] | 0.61 | [0.27, 1.40] | 1.41 | [0.73, 2.71] | 0.81 | [0.12, 5.32] |
| Abuse2 | 1.82 | [0.86, 3.86] | 1.20 | [0.47, 3.08] | 1.85 | [0.97, 3.53] | 7.91* | [1.06, 58.79] |
| Multi-type CAN2 | 1.88* | [1.10, 3.19] | 0.80 | [0.40, 1.59] | 1.35 | [0.79, 2.29] | 7.31* | [1.21, 44.08] |
| Abuse3 | 1.62 | [0.74, 3.55] | 1.96 | [0.73, 5.26] | 1.31 | [0.62, 2.77] | 9.78* | [1.59, 60.16] |
| Multi-type CAN3 | 1.66 | [0.93, 2.96] | 1.30 | [0.63, 2.70] | 0.95 | [0.49, 1.87] | 9.04* | [2.16. 37.86] |
| Multi-type CAN4 | 1.03 | [0.52, 2.04] | 0.66 | [0.27, 1.64] | 0.73 | [0.38, 1.38] | 0.92 | [0.19, 4.41] |
Note: CI = confidence interval; IRR = Incident Rate Ratio
p < .05
White reference group
Low-Risk reference group
Neglect reference group
Abuse reference group
Funding
The Longitudinal Studies of Child Abuse and Neglect were by 90CA1744, 90CA1745, 90CA1746, 90CA1747, 90CA1748, and 90CA1749 grants funded by the Office on Child Abuse and Neglect, Children’s Bureau, Administration of Children and Family. Dr. Villodas’ research is funded by the National Institute for Minority Health and Health Disparities (U54MD012397). Dr. Picci’s research is currently funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (P50HD089922). Dr. Fishbein’s research is currently funded by the Office of National Drug Control Policy (Gl999ONDCP06A) and the National Center of Complementary and Integrative Health (R61AT009856–02).
Footnotes
A full list of publications that have used data from the LONGSCAN study can be found at: https://www.zotero.org/groups/421939/candl/tags/LONGSCAN/items/YVXS9D6G/library
Conflicts of interest/Competing interests
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Ethic approval
The Longitudinal Studies of Child Abuse and Neglect obtained approval from the appropriate Institutional Review Boards (IRBs) prior to data collection. The analyses performed for the present study were approved by the IRB at San Diego State University.
References
- Asparouhov T, & Muthén B (2014). Auxiliary Variables in Mixture Modeling: Three-Step Approaches Using Mplus. Structural Equation Modeling: A Multidisciplinary Journal, 21(3), 329–341. doi: 10.1080/10705511.2014.915181 [DOI] [Google Scholar]
- Bakk Z, & Vermunt JK (2016). Robustness of Stepwise Latent Class Modeling With Continuous Distal Outcomes. Structural Equation Modeling: A Multidisciplinary Journal, 23(1), 20–31. doi: 10.1080/10705511.2014.955104 [DOI] [Google Scholar]
- Baldwin JR, Reuben A, Newbury JB, & Danese A (2019). Agreement Between Prospective and Retrospective Measures of Childhood Maltreatment: A Systematic Review and Meta-analysis. JAMA Psychiatry, 76(6), 584–593. doi: 10.1001/jamapsychiatry.2019.0097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bos KJ, Fox N, Zeanah CH, & Nelson Iii CA (2009). Effects of early psychosocial deprivation on the development of memory and executive function. Frontiers in behavioral neuroscience, 3, 16–16. doi: 10.3389/neuro.08.016.2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braga T, Gonçalves LC, Basto-Pereira M, & Maia  (2017). Unraveling the link between maltreatment and juvenile antisocial behavior: A meta-analysis of prospective longitudinal studies. Aggression and Violent Behavior, 33, 37–50. doi: 10.1016/j.avb.2017.01.006 [DOI] [Google Scholar]
- Chapple CL, Tyler KA, & Bersani BE (2005). Child neglect and adolescent violence: examining the effects of self-control and peer rejection. Violence and Victims, 20(1), 39–53. doi: 10.1891/088667005780927638 [DOI] [PubMed] [Google Scholar]
- Charak R, & Koot HM (2015). Severity of maltreatment and personality pathology in adolescents of Jammu, India: A latent class approach. Child Abuse & Neglect, 50, 56–66. doi: 10.1016/j.chiabu.2015.05.010 [DOI] [PubMed] [Google Scholar]
- Cicchetti D (2016). Socioemotional, Personality, and Biological Development: Illustrations from a Multilevel Developmental Psychopathology Perspective on Child Maltreatment. Annu Rev Psychol, 67(1), 187–211. doi: 10.1146/annurev-psych-122414-033259 [DOI] [PubMed] [Google Scholar]
- Clayton K, Lee JB, Cheung K, Theule J, & Henrikson B (2018). Quantifying the Relationship between Attention-Deficit/Hyperactivity Disorder and Experiences of Child Maltreatment: A Meta-Analysis. Child Abuse Review, 27(5), 361–377. doi: 10.1002/car.2530 [DOI] [Google Scholar]
- Collins LM, & Lanza ST (2010). Latent Class and Latent Transition Analysis with Applications in the Social, Behavioral, and Health Sciences. Hoboken, NJ: John Wiley and Sons, inc. [Google Scholar]
- Costello EJ, Copeland W, & Angold A (2011). Trends in psychopathology across the adolescent years: What changes when children become adolescents, and when adolescents become adults? Journal of Child Psychology and Psychiatry, 52(10), 1015–1025. doi: 10.1111/j.1469-7610.2011.02446.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Debowska A, Willmott D, Boduszek D, & Jones AD (2017). What do we know about child abuse and neglect patterns of co-occurrence? A systematic review of profiling studies and recommendations for future research. Child Abuse & Neglect, 70, 100–111. doi: 10.1016/j.chiabu.2017.06.014 [DOI] [PubMed] [Google Scholar]
- Dodge KA, Pettit GS, Bates JE, & Valente E (1995). Social information-processing patterns partially mediate the effect of early physical abuse on later conduct problems. Journal of Abnormal Psychology, 104(4), 632–643. doi: 10.1037/0021-843X.104.4.632 [DOI] [PubMed] [Google Scholar]
- Dubowitz H, Roesch S, Arria AM, Metzger R, Thompson R, Kotch JB, & Lewis T (2019). Timing and chronicity of child neglect and substance use in early adulthood. Child Abuse & Neglect, 94, 104027. doi: 10.1016/j.chiabu.2019.104027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- English D, & Investigators L (1997). Modified maltreatment classification system (MMCS). For more information visit the LONGSCAN website at http://www.iprc.unc.edu/longscan.
- Evans GW, Li D, & Whipple SS (2013). Cumulative risk and child development. Psychological Bulletin, 139(6), 1342–1396. doi: 10.1037/a0031808 [DOI] [PubMed] [Google Scholar]
- Finkelhor D, Turner HA, Hamby S, & Ormond R (2011). Polyvictimization: Children’s Exposure to Multiple Types of Violence, Crime, and Abuse. Retrieved from www.ncjrs.gov/pdffiles1/ojjdp/235504.pdf
- Finkelhor D, Turner HA, Shattuck A, & Hamby SL (2015). Prevalence of Childhood Exposure to Violence, Crime, and Abuse: Results From the National Survey of Children’s Exposure to Violence. JAMA Pediatr, 169(8), 746–754. doi: 10.1001/jamapediatrics.2015.0676 [DOI] [PubMed] [Google Scholar]
- Gardner MJ, Thomas HJ, & Erskine HE (2019). The association between five forms of child maltreatment and depressive and anxiety disorders: A systematic review and meta-analysis. Child Abuse & Neglect, 96, 104082. doi: 10.1016/j.chiabu.2019.104082 [DOI] [PubMed] [Google Scholar]
- Halpern SC, Schuch FB, Scherer JN, Sordi AO, Pachado M, Dalbosco C, . . . Von Diemen L. (2018). Child Maltreatment and Illicit Substance Abuse: A Systematic Review and Meta-Analysis of Longitudinal Studies. Child Abuse Review, 27(5), 344–360. doi: 10.1002/car.2534 [DOI] [Google Scholar]
- Heleniak C, McLaughlin KA, Ormel J, & Riese H (2016). Cardiovascular reactivity as a mechanism linking child trauma to adolescent psychopathology. Biological Psychology, 120, 108–119. doi: 10.1016/j.biopsycho.2016.08.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrenkohl RC, & Herrenkohl TI (2009). Assessing a child’s experience of multiple maltreatment types: Some unfinished business. Journal of Family Violence, 24(7), 485–496. doi: 10.1007/s10896-009-9247-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hillberg T, Hamilton-Giachritsis C, & Dixon L (2011). Review of Meta-Analyses on the Association Between Child Sexual Abuse and Adult Mental Health Difficulties: A Systematic Approach. Trauma, Violence, & Abuse, 12(1), 38–49. doi: 10.1177/1524838010386812 [DOI] [PubMed] [Google Scholar]
- Hussey JM, Marshall JM, English DJ, Knight ED, Lau AS, Dubowitz H, & Kotch JB (2005). Defining maltreatment according to substantiation: Distinction without a difference? Child Abuse & Neglect, 29(5), 479–492. doi: 10.1016/j.chiabu.2003.12.005 [DOI] [PubMed] [Google Scholar]
- Kelly PA, Viding E, Puetz VB, Palmer AL, Mechelli A, Pingault J-B, . . . McCrory EJ. (2015). Sex differences in socioemotional functioning, attentional bias, and gray matter volume in maltreated children: A multilevel investigation. Development and Psychopathology, 27(4pt2), 1591–1609. doi: 10.1017/S0954579415000966 [DOI] [PubMed] [Google Scholar]
- Kim H, Wildeman C, Jonson-Reid M, & Drake B (2017). Lifetime Prevalence of Investigating Child Maltreatment Among US Children. American Journal of Public Health, 107(2), 274–280. doi: 10.2105/ajph.2016.303545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knight ED, Smith JB, Martin LM, Lewis T, & the LONGSCAN Investigators. (2008). Measures for Assessment of Functioning and Outcomes in Longitudinal Research on Child Abuse Volume 3: Early Adolescence (Ages 12–14). Retrieved from LONGSCAN web site; (http://www.unc.edu/depts/sph/longscan/). [Google Scholar]
- Knight ED, Smith JB, Martin LM, & the LONGSCAN Investigators. (2009). Measures for Assessment of Functioning and Outcomes in Longitudinal Research on Child Abuse and Neglect Volume 4: Middle Adolescence (Age 16). Retrieved from LONGSCAN web site; (http://www.unc.edu/depts/sph/longscan/). [Google Scholar]
- Kohl PL, Jonson-Reid M, & Drake B (2009). Time to leave substantiation behind: Findings from a national probability study. Child maltreatment, 14(1), 17–26. doi: 10.1177/1077559508326030 [DOI] [PubMed] [Google Scholar]
- Lindert J, von Ehrenstein OS, Grashow R, Gal G, Braehler E, & Weisskopf MG (2014). Sexual and physical abuse in childhood is associated with depression and anxiety over the life course: systematic review and meta-analysis. International Journal of Public Health, 59(2), 359–372. doi: 10.1007/s00038-013-0519-5 [DOI] [PubMed] [Google Scholar]
- Machlin L, Miller AB, Snyder J, McLaughlin KA, & Sheridan MA (2019). Differential associations of deprivation and threat with cognitive control and fear conditioning in early childhood. Frontiers in Behavioral Neuroscience, 13. doi: 10.3389/fnbeh.2019.00080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, & Lambert HK (2017). Child trauma exposure and psychopathology: Mechanisms of risk and resilience. Current Opinion in Psychology, 14, 29–34. doi: 10.1016/j.copsyc.2016.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, & Sheridan MA (2016). Beyond Cumulative Risk:A Dimensional Approach to Childhood Adversity. Current Directions in Psychological Science, 25(4), 239–245. doi: 10.1177/0963721416655883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messman-Moore TL, & Bhuptani PH (2017). A Review of the Long-Term Impact of Child Maltreatment on Posttraumatic Stress Disorder and Its Comorbidities: An Emotion Dysregulation Perspective. Clinical Psychology: Science and Practice, 24(2), 154–169. doi: 10.1111/cpsp.12193 [DOI] [Google Scholar]
- Monahan KC, King KM, Shulman EP, Cauffman E, & Chassin L (2015). The effects of violence exposure on the development of impulse control and future orientation across adolescence and early adulthood: Time-specific and generalized effects in a sample of juvenile offenders. Development & Psychopathology, 27(4pt1), 1267–1283. doi: 10.1017/S0954579414001394 [DOI] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (2017). Mplus User’s Guide (8th ed.). Los Angeles: Muthén & Muthén. [Google Scholar]
- Norman RE, Byambaa M, De R, Butchart A, Scott J, & Vos T (2012). The Long-Term Health Consequences of Child Physical Abuse, Emotional Abuse, and Neglect: A Systematic Review and Meta-Analysis. PLOS Medicine, 9(11), e1001349. doi: 10.1371/journal.pmed.1001349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nylund KL, Asparouhov T, & Muthén BO (2007). Deciding on the Number of Classes in Latent Class Analysis and Growth Mixture Modeling: A Monte Carlo Simulation Study. Structural Equation Modeling, 14(4), 569–569. doi: 10.1080/10705510701575396 [DOI] [Google Scholar]
- Perkins S, Smith-Darden J, Ametrano R, & Graham-Bermann S (2014). Typologies of Violence Exposure and Cognitive Processing in Incarcerated Male Adolescents. Journal of Family Violence, 29(4), 439–451. doi: 10.1007/s10896-014-9600-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petrenko CLM, Friend A, Garrido EF, Taussig HN, & Culhane SE (2012). Does subtype matter? Assessing the effects of maltreatment on functioning in preadolescent youth in out-of-home care. Child Abuse & Neglect, 36(9), 633–644. doi: 10.1016/j.chiabu.2012.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rivera PM, Fincham FD, & Bray BC (2018). Latent Classes of Maltreatment: A Systematic Review and Critique. Child maltreatment, 0(0), 1077559517728125. doi: 10.1177/1077559517728125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roesch SC, Villodas M, & Villodas F (2010). Latent class/profile analysis in maltreatment research: a commentary on Nooner et al., Pears et al., and looking beyond. Child Abuse Negl, 34(3), 155–160. doi: 10.1016/j.chiabu.2010.01.003 [DOI] [PubMed] [Google Scholar]
- Runyan D, Dubowitz H, English DJ, Kotch JB, Litrownik AJ, Thompson R, & The LONGSCAN Investigator Group. (2014). Longitudinal Studies of Child Abuse and Neglect (LONGSCAN) Assessments 0–18 [Dataset]. Retrieved from http://www.ndacan.cornell.edu
- Shaffer D, Fisher P, Lucas CP, Dulcan MK, & Schwab-Stone ME (2000). NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child & Adolescent Psychiatry, 39(1), 28–38. doi: 10.1097/00004583-200001000-00014 [DOI] [PubMed] [Google Scholar]
- Shenk CE, Noll JG, Peugh JL, Griffin AM, & Bensman HE (2015). Contamination in the Prospective Study of Child Maltreatment and Female Adolescent Health. Journal of Pediatric Psychology, 41(1), 37–45. doi: 10.1093/jpepsy/jsv017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheridan MA, Shi F, Miller AB, Sahali C, & McLaughlin KA (2019). Network structure reveals clusters of associations between childhood adversities and development outcomes. Developmental Science, n/a, e12934. doi: 10.1111/desc.12934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Straus MA, Hamby SL, Finkelhor D, Moore DW, & Runyan D (1998). Identification of child maltreatment with the Parent–Child Conflict Tactics Scales: Development and psychometric data for a national sample of American parents. Child Abuse & Neglect, 22(4), 249–270. doi: 10.1016/S0145-2134(97)00174-9 [DOI] [PubMed] [Google Scholar]
- Thornberry TP, Henry KL, Ireland TO, & Smith CA (2010). The causal impact of childhood-limited maltreatment and adolescent maltreatment on early adult adjustment. Journal of Adolescent Health, 46(4), 359–365. doi: 10.1016/j.jadohealth.2009.09.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services, Administration for Children, Youth and Families, & Children’s Bureau. (2020). Child Maltreatment 2018. Retrieved from https://www.acf.hhs.gov/cb/research-data-technology/statistics-research/child-maltreatment.
- Vaughn MG, Salas-Wright CP, Underwood S, & Gochez-Kerr T (2015). Subtypes of Non-Suicidal Self-Injury Based on Childhood Adversity. Psychiatric Quarterly, 86(1), 137–151. doi: 10.1007/s11126-014-9313-7 [DOI] [PubMed] [Google Scholar]
- Villodas MT, Litrownik AJ, Thompson R, Roesch SC, English DJ, Dubowitz H, . . . Runyan DK. (2012). Changes in youth’s experiences of child maltreatment across developmental periods in the LONGSCAN consortium. Psychology of Violence, Vol. 2(4), 325–338. doi: 10.1037/a0029829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Widom CS, & Nikulina V (2012). Long-term consequences of child neglect in low-income families. In The Oxford handbook of poverty and child development. [Google Scholar]
- Widom CS, Raphael KG, & DuMont KA (2004). The case for prospective longitudinal studies in child maltreatment research: commentary on Dube, Williamson, Thompson, Felitti, and Anda (2004). Child Abuse Neglect, 28(7), 715–722. doi: 10.1016/j.chiabu.2004.03.009 [DOI] [PubMed] [Google Scholar]


