Abstract
Supported by the 10% set-aside funds in the Community Mental Health Block grant, distributed at the state level, coordinated specialty care (CSC) have been widely disseminated throughout the U.S. This study explores variations in the geographical accessibility of CSC programs by neighborhood level characteristics in Washington State. CSC locations were geocoded. Socioeconomic neighborhood deprivation (i.e., Area deprivation index) and rurality (i.e., Rural–Urban Commuting Area codes) were neighborhood level characteristics extracted from the 2018 American Community Survey. Geographic accessibility of CSC was assessed using a two-step floating catchment area technique and multilevel linear models were used to examine the association between specific neighborhood characteristics and geographic accessibility. The association between access and socioeconomically deprived neighborhoods varied differentially by neighborhood rurality (an interaction effect). Model estimates indicated that the least deprived, metropolitan neighborhoods had the best access (M = 0.38; CI: 0.34, 0.42) and rural neighborhoods in the second most deprived quartile had the worst access (M = 0.16; CI: 0.11, 0.21) to CSC. There was a clear decrease in accessibility for more rural neighborhoods, regardless of other neighborhood characteristics. In conclusions, findings provide important insight into how resource distribution contributes to geographic disparities in access to CSC. The use of spatial analytic techniques has the potential to identify specific neighborhoods and populations where there is a need to expand and increase availability of CSC to ensure access to rural and socioeconomically deprived neighborhoods.
Keywords: Geographic Accessibility, Coordinated Specialty Care, Social Determinants, First-episode psychosis, Washington State
Introduction
In the U.S. coordinated specialty care (CSC) is comprised of multiple evidence-based practices, designed to provide acute care for individuals experiencing the early phases of psychosis (Correll et al., 2018). Similar to early intervention programs implemented in other countries, such as Australia, Canada, and Great Britain, CSC includes family education and support, individual or group psychotherapy, medication management (i.e., low doses of antipsychotic medications), and supported employment and education, delivered by a multidisciplinary team (Wright et al., 2019). The Recovery After an Initial Schizophrenia Episode-Early Treatment Program (RAISE-ETP) demonstrated that CSC improved quality of life and reduced symptom severity among individuals experiencing their first episode of psychosis (FEP) relative to those who received standard outpatient mental health care (Kane et al., 2015). Since the RAISE-ETP study, and supported by the 5–10% set-aside in the Community Mental Health Block Grant which provides funds for states in the U.S. to implement evidence-based early intervention, there are approximately 300 CSC distributed throughout the U.S. (Everett & Heinssen, 2019; Rosenblatt, 2018). Washington State serves as an example of using these allocated funds to support the implementation of ten CSC across the state, with the aim of reducing the duration of untreated psychosis and providing specialized mental health services for FEP (Oluwoye, Reneau, et al., 2019).
Several studies have examined the pathways to CSC programs among individuals experiencing FEP and their family members (Cabassa et al., 2018; Oluwoye, Cheng, et al., 2019; Stain et al., 2018). Findings from these studies suggest that limited accessibility of CSC is a contributing factor to delays in seeking treatment, further extending the duration of untreated psychosis. Recently, studies have demonstrated geographic variations in the duration of untreated psychosis, specifically for low socioeconomic neighborhoods which tend to have a significantly longer duration of untreated psychosis (Ku et al., 2020; O’Donoghue et al., 2016; Reichert & Jacobs, 2018). Similarly, studies have shown that neighborhood-level determinants (e.g., socioeconomic deprivation, rurality) also contribute to variations in the access to mental health services (Chow et al., 2003; Cummings et al., 2016, 2017).
Geographic or spatial accessibility can be defined as the distance or time travelled to the point of service (Guagliardo, 2004). The assessment of spatial accessibility to services has been frequently used to examine accessibility of primary care providers and other behavioral health services (e.g., suicide prevention) to identify geographic disparities and inform health system policies (Cummings et al., 2017; Graves et al., 2020; McGrail, 2012). Given the importance of mental health services being available in proximity to an individual’s community (Moe et al., 2018), it is surprising that very few studies have examined the geographic accessibility of CSC. To date there has been one study to use spatial analytic techniques to examine the geographic distribution of CSC enrollees in Connecticut, U.S. (Mathis et al., 2018). They found that that there were less residents from specific neighborhoods (i.e., high income households, racially homogeneous neighborhoods) enrolled in their CSC, identifying potential neighborhoods that may experience more difficult pathways to CSC.
Rather than focusing on the geographical distribution of individuals’ residence, we postulate that the first step to understanding variations in duration of untreated psychosis and inequities in CSC service utilization is to assess whether there are geographical variations in the accessibility of CSC. Thus, the objective of the present study is to characterize the geographical distribution of CSC in Washington State and to identify potential geographic disparities in access to these specialty mental health services. Specifically, this study will explore variations in accessibility of CSC across levels of rurality and socioeconomic neighborhood deprivation in Washington State.
Methods
Data Sources
This cross-sectional study was conducted at the Census block group level, the smallest level of geography for which the U.S. Census Bureau reports socio-demographics data (U.S. Census Bureau, n.d.). Block groups commonly contains 600 to 3000 residents and provide high-quality statistical data about the demographics and socioeconomic status of U.S. population. Consistent with the age eligibility criteria for CSC programs in Washington State, data on the population of people aged 15 to 40 years was extracted from the 2018 American Community Survey (ACS) 5-year estimates (Oluwoye, Reneau, et al., 2019). The physical locations of CSC in Washington State was collected from the directory listed on the Washington Center of Excellence in Early Psychosis website (www.wa-ceep.org). These data provided the addresses for ten programs actively providing CSC in Washington State. Nine of the ten programs are state-funded CSC programs, known as New Journeys, implemented in outpatient mental health agencies. Additional details about New Journeys program characteristics are available elsewhere (Oluwoye, Cheng, et al., 2019; Oluwoye, Reneau, et al., 2019). One program is located in a university-hospital outpatient program that utilizes a CSC model similar to New Journeys. This study did not require IRB review because it used publicly available socio-demographic and CSC data.
Measures
Outcome Variables (Access Score per 100,000 People)
Geographic accessibility to CSC programs was quantified using a two-step floating catchment area method (Guagliardo, 2004; McGrail, 2012). This technique accounted for: (1) the supply of CSC relative to the population size; (2) proximity of CSC relative to the population distribution in block groups; and (3) time as a barrier. The two-step floating catchment area method used floating catchment areas, where the size of the catchments was determined by maximum travel time. A distance decay function was incorporated into the analysis, recognizing that different population groups are not equally likely to seek services from CSC and that the interaction between population and facilities decreases as distance between them increase (Amiri et al., 2020; McGrail, 2012). After geocoding the address of each CSC, the travel time between the longitude and latitude of block group population weighted centroids and each CSC was calculated using the ESRI ArcGIS Network analyst OD matrix. For each CSC, a search for all block groups that were within a 120-min drive from each treatment facility was performed. No decay was applied to travel times less than 10 min. The decay for travel times between 10 and 120 min increased linearly and proportionally to the travel time. These time cut-offs have been previously used and were therefore chosen to accommodate differences in population and access to primary care and other healthcare services (Amiri et al., 2020). Next, we calculated a demand ratio for CSC by taking into account the population and travel time impedance for CSC and Census block groups. Lastly, for each block group centroid, we searched all treatment facilities that were within a 120-min drive from each block group. An access score for block groups was calculated by summing up the demand score for CSC that serve each block group. Access scores represent a ratio of CSC (supply) to the population of block groups served (demand) with only selected treatment facilities and block group population entering the numerator and denominator. Larger access scores represent greater accessibility to CSC accounting for the three components of geographic access. (Schuurman et al., 2010). Supplemental Fig. 1 illustrates application of two-step floating catchment area method for measuring access to CSC.
Explanatory Variables
Rurality
The Rural–Urban Commuting Area (RUCA) codes were used for categorizing Census block groups into metropolitan, micropolitan, or small town or rural areas (USDA, n.d.; WWAMI Rural Health Research Center, n.d.). Census block groups with RUCA primary codes of 1–3 were classified as metropolitan areas, those with RUCA primary codes of 4–6 were classified as micropolitan areas, and those with RUCA primary codes of 7–10 were classified as small towns or rural areas (USDA, n.d.; WWAMI Rural Health Research Center, n.d.). Socioeconomic neighborhood deprivation: Area deprivation index (ADI) represented the social and economic characteristics of block groups (Knighton et al., 2016; Singh, 2003). ADI is a validated composite score of socioeconomic disadvantage and was developed based on 17 Census variables in four domains of poverty, housing, employment, and education (Knighton et al., 2016; Singh, 2003). ADI scores ranged from 1 to 10 with higher scores indicating greater deprivation (Kind & Buckingham, 2018). Census block groups were categorized into quartiles of deprivation (Q1 = least deprived to Q4 = most deprived). Covariates included percent of Black/African American and Hispanic population, which were obtained from the 2018 ACS 5-year estimates (U.S. Census Bureau, n.d.).
Data Analysis
Measures of central tendency and variability for continuous variables and percentages and frequencies for categorical variables describing geographic accessibility to CSC program and Census block group characteristics were calculated (including mean access scores). Multilevel linear models were used to assess the relationship between Census block group characteristics and CSC program accessibility while accommodating the clustering of block groups within counties. Our models included a random intercept, allowing the likelihood of access to CSC programs to vary across counties. The main effects model was fitted with rurality and socioeconomic neighborhood deprivation. Control variables for the percent of Hispanic and Black/African American populations were included as fixed effects, which is consistent with previous studies to examine geographic accessibility (Cummings et al., 2014; Dinwiddie et al., 2013). To determine whether geographic accessibility varied over rurality and differentially over rurality by socioeconomic neighborhood disadvantage quartiles, a model was also fitted with a rurality by socioeconomic neighborhood disadvantage interaction and used a likelihood ratio test to detect whether the interaction was statistically significant. Based on the fitted multilevel model with interaction effects, contrasts between increasing levels of rurality were calculated within socioeconomic neighborhood deprivation quartiles. All statistical analyses were performed in R version 3.6.3. Multilevel models were fit via the lme4 package and contrasts were calculated via the emmeans package. Statistical significance was set to an alpha level of 0.05.
Results
Geographic Characteristics
Table 1 displays descriptive information of neighborhood (i.e., Census block groups) characteristics in Washington State. The average population size for those between 15 and 40 years of age, at the Census block group level, was similar for metropolitan and micropolitan neighborhoods and lower for rural neighborhoods. Population size varied across level of neighborhood rurality. There was a uniform distribution of socioeconomic deprivation level in metropolitan neighborhoods, but there was a higher proportion of micropolitan and rural neighborhoods classified as socioeconomically deprived (Q3-Q4). Of the ten CSC located in Washington State, nine (90%) were in metropolitan neighborhoods, one (10%) was in a micropolitan neighborhood, and there were no programs located in rural neighborhoods. Additionally, seven CSC programs were in the highest deprivation quartile (Q4), two programs were in the second highest deprivation quartile (Q3), and one program was in a lowest deprivation quartile (Q1).
Table 1.
Neighborhood characteristics by rurality
| Metropolitan (N = 4098) | Micropolitan (N = 345) | Rural/Small Town (N = 320) | Combined (N = 4763) | |
|---|---|---|---|---|
| Population (Aged 15–40) | ||||
| Mean (SD) | 545 (356) | 534 (460) | 307 (249) | 528 (363) |
| Median [Min, Max] | 462 [0, 3940] | 406 [11, 3670] | 258 [7, 2390] | 442 [0, 3940] |
| Socioeconomic Neighborhood Deprivation | ||||
| Q1 | 927 (22.6%) | 6 (1.7%) | 20 (6.2%) | 953 (20.0%) |
| Q2 | 886 (21.6%) | 42 (12.2%) | 25 (7.8%) | 953 (20.0%) |
| Q3 | 1241 (30.3%) | 120 (34.8%) | 68 (21.2%) | 1429 (30.0%) |
| Q4 | 1044 (25.5%) | 177 (51.3%) | 207 (64.7%) | 1428 (30.0%) |
| Hispanic | ||||
| Mean (SD) | 1.06 (1.29) | 1.85 (2.43) | 1.43 (2.10) | 1.14 (1.48) |
| Median [Min, Max] | 0.64 [0, 9.94] | 0.81 [0, 9.65] | 0.56 [0, 9.60] | 0.64 [0, 9.94] |
| Black/African American | ||||
| Mean (SD) | 0.39 (0.680) | 0.13 (0.322) | 0.05 (0.146) | 0.35 (0.646) |
| Median [Min, Max] | 0.11 [0, 6.44] | 0 [0, 3.15] | 0 [0, 1.65] | 0.074 [0, 6.44] |
Geographic Accessibility of CSC Programs by Socioeconomic Neighborhood Deprivation and Rurality
Figure 1 illustrates the accessibility of CSC programs in Washington at the Census block group level. The least deprived (Q1) metropolitan neighborhoods had the highest accessibility to CSC, based on mean access scores. While accessibility decreased as rurality increased and differences across socioeconomic neighborhood deprivation levels were not as pronounced. Mean access scores by socioeconomic neighborhood deprivation and rurality are displayed in Table 2.
Fig. 1.
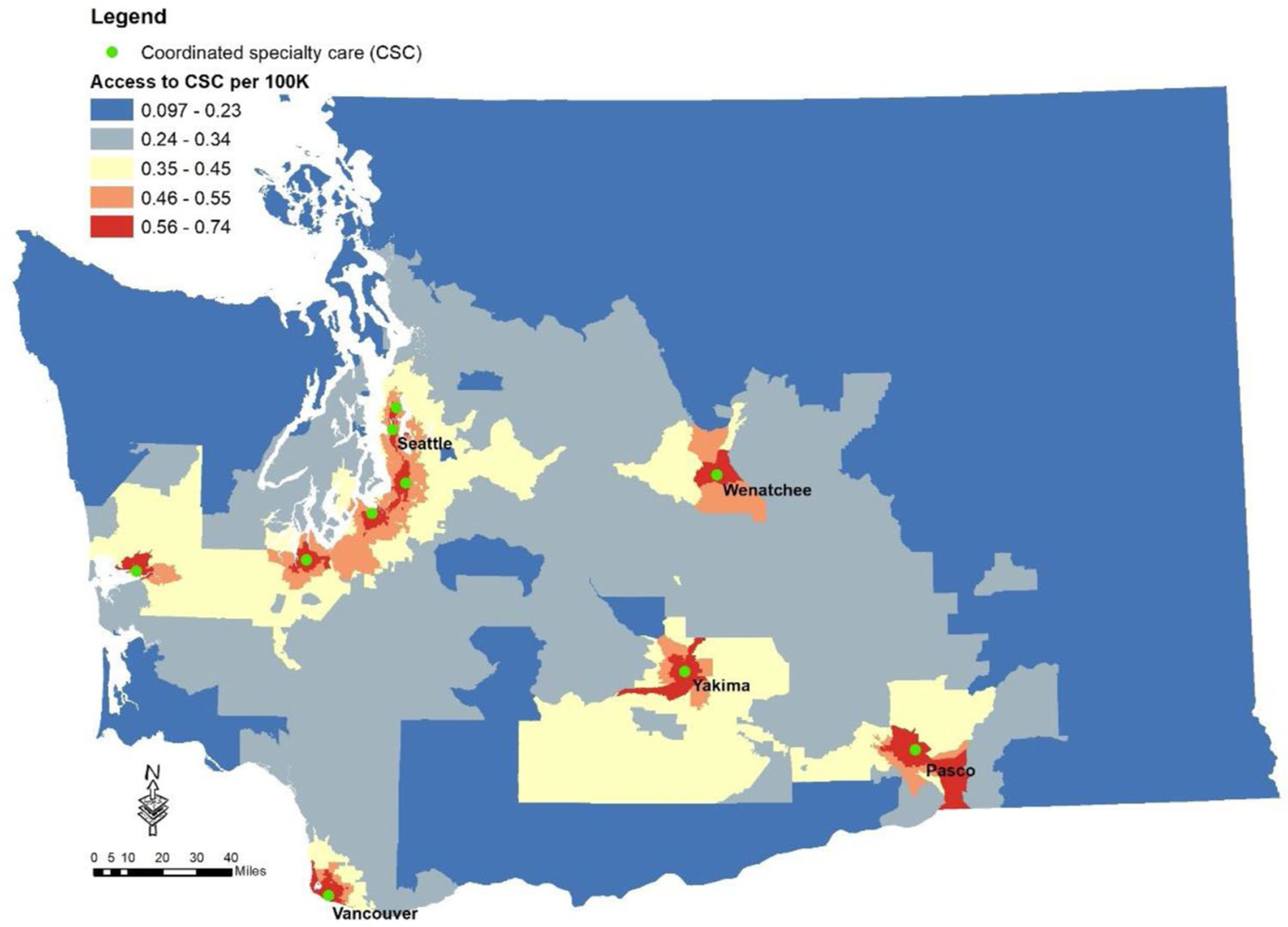
Access to coordinated specialty care (CSC) programs in Washington State. Access to was calculated using a two-step floating catchment area method with a distance decay function. Larger values represent greater accessibility to CSC programs
Table 2.
Estimated CSC access levels [mean (SD)] across rurality and deprivation quartiles (Q1 is least deprived and Q4 is most deprived)
| Rurality | Q1 | Q2 | Q3 | Q4 |
|---|---|---|---|---|
| Metropolitan | 0.424 (0.095) | 0.402 (0.119) | 0.399 (0.142) | 0.409 (0.181) |
| Micropolitan | 0.216 (0.056) | 0.204 (0.062) | 0.251 (0.103) | 0.345 (0.159) |
| Rural/small town | 0.171 (0.073) | 0.195 (0.053) | 0.211 (0.095) | 0.211 (0.081) |
Neighborhood‑Level Characteristics Associated with the Geographic Accessibility CSC Programs
The main effects of rurality and socioeconomic neighborhood deprivation were examined. Results indicated a 9% (M: − 0.093; CI − 0.104, − 0.082) decrease in accessibility for micropolitan neighborhoods and 17% (M: − 0.173; CI: − 0.186, − 0.160) decrease in accessibility for rural/small town neighborhoods, compared to metropolitan neighborhoods. While there were increases of 1% (M: 0.015; CI: 0.009, 0.021) for neighborhoods in the second lowest deprivation quartile (Q2), 2% (M = 0.024; CI: 0.018, 0.03) increase for second highest deprivation quartile (Q3), and a 4% (M = 0.042; CI: 0.035, 0.049) increase the highest deprivation quartile (Q4), compared to neighborhoods in the lowest deprivation quartile (Q1).
The likelihood ratio test results from the multilevel model analyses detected an interaction between rurality and socioeconomic neighborhood deprivation (F = 3.73, p < 0.001). Within each quartile of deprivation, there was a decrease in accessibility based on level of rurality (Fig. 2). Estimates based on the interaction model indicated that metropolitan neighborhoods in the highest deprivation quartile (Q4) had best access (M = 0.38; CI: 0.34, 0.42) and rural neighborhoods in the second lowest deprivation quartile (Q2) had the worst access (M = 0.16; CI: 0.11, 0.21) to CSC. Marginal means of rurality within each deprivation quartile were compared. There was a significant decrease in accessibility for all increases in rurality, however there was no significant difference between micropolitan and metropolitan access in the lowest deprivation quartile (Q1; see Supplemental Table 1).
Fig. 2.
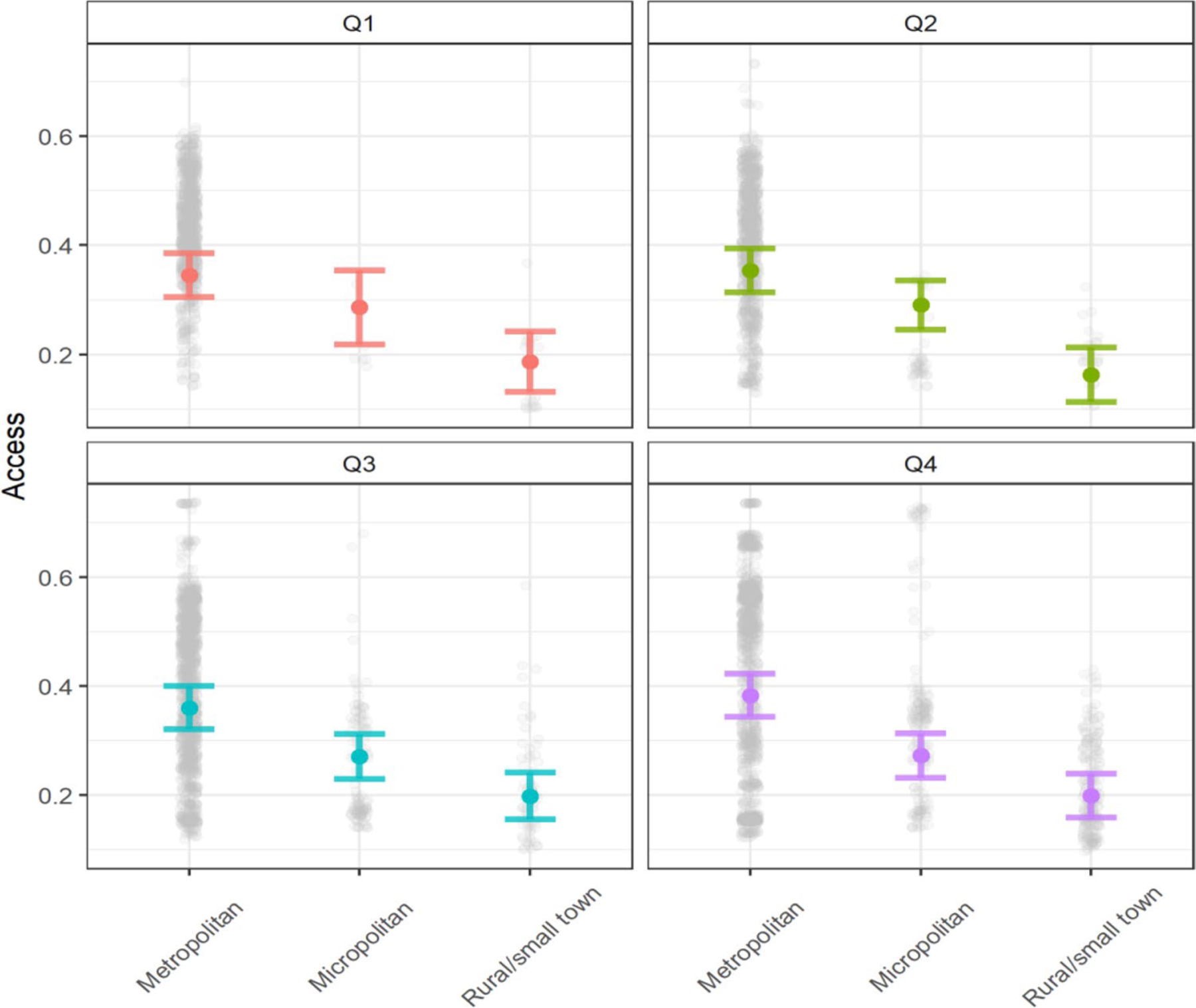
The differential association between access and rurality across socioeconomic neighborhood deprivation quartiles (Q1 is least deprived and Q4 is most deprived) from model predictions. Estimates are adjusted for a neighborhood with Hispanic proportion of 11.43% and Black/African American proportion of 3.47%, the average proportions
Discussion
This study used spatial techniques to provide estimates of the geographic accessibility to CSC programs for FEP in Washington State. The majority of CSC were located in metropolitan (i.e., urban; 90%) and socioeconomically deprived (Q4; 70%) neighborhoods. Using a two-step floating catchment area method, results identified that rural neighborhoods in the second lowest neighborhood deprivation had the lowest accessibility to CSC programs. In recent years, across the U.S. there has been an increase in CSC by approximately 400% (Everett & Heinssen, 2019), and as CSC continues to expand, in Washington State and nationally, understanding the impact of their geographic distribution is imperative.
To date, no studies have described the accessibility of CSC however prior research has examined the accessibility of outpatient mental health services in the U.S.. Findings from studies, primarily conducted by Cummings and colleagues, have found that low socioeconomic neighborhoods (Cummings et al., 2017), neighborhoods with a higher percentage of Black residents (Cummings et al., 2014), and rural neighborhoods (Cummings et al., 2014, 2016) have limited accessibility to mental health services. Although the present study is conducted on a state level, findings demonstrated limited accessibility to specialty services for early psychosis for rural and low socioeconomic neighborhoods, which is consistent with previous studies in other areas.
The geographic distribution of CSC significantly contributes geographic disparities in accessibility of services. Further, the limited number of programs in rural neighborhoods further highlights additional logistical barriers (e.g., transportation, travel time) accessing and utilizing services not in close proximity to individuals residing in these neighborhoods. While findings indicate the need to increase the availability of CSC in rural neighborhoods to improve accessibility, additional fiscal support and strengthening the current infrastructure of community-based mental health agencies may be needed to provide specialty services in these areas. Alternatively, there is a need to explore other options for CSC, such as mobile CSC units to expand reach of services to rural and low socioeconomic neighborhoods. The present study expands our understanding of the distribution of CSC at the state level and identifies gaps in potential accessibility to specialty services. Findings from this study can be replicated and used to aid decision-making by state level officials and community stakeholders to identify neighborhoods with limited accessibility and inform on the placement of future programs.
The pathway to CSC may include delays in accessing services and subsequently a longer duration of untreated psychosis, which varies based on neighborhood characteristics (e.g., longer duration for deprived neighborhoods) (Ku et al., 2020; O’Donoghue et al., 2016). The Andersen-Newman Behavioral Health Model of Health Services suggests that the inequitable accessibility to enabling factors (e.g., mental health services) has a trickle down impact on the use of health services (Andersen, 1995). Several studies have reported service utilization disparities among racially and ethnically diverse and low-income individuals (Oluwoye et al., 2018; van der Ven et al., 2020). It is quite possible that the limited geographic accessibility of CSC contributes to these disparities and should be further explored in subsequent research.
Limitations
There are several limitations that should be considered. Geographical data was limited to Washington State and geographic accessibility may differ in states with higher number of programs such as Oregon or California. It should also be noted that analyses did not incorporate geographic accessibility for CSC in boarding states (e.g., Oregon, Idaho) for residents who may seek services outside of the Washington State. While generalizability may be limited to Washington State, these findings serve as an important foundation to examine geographic accessibility and placement of CSC nationally. Another limitation is that geographic accessibility only accounted for access scores for CSC and did not include accessibility to outpatient mental health services where providers utilize Cognitive Behavior Therapy for psychosis (CBTp). Future research should expand and examine accessibility to mental health services that provide CBTp, especially in areas that have limited availability of CSC.
Conclusions
This is the first study to explore geographic accessibility of CSC at the state level and to identify geographic disparities in accessibility of CSC in Washington State. Study findings are relevant and of great importance, as the 5–10% set aside in the Mental Health Block Grant provided to states across the U.S. are used to fund the implementation of evidencebased early interventions, such as CSC (Everett & Heinssen, 2019; Rosenblatt, 2018). Future research replicating the present study on a national level would aid policymakers to consider additional criteria regarding how funds should be distributed to address geographic inequities and downstream (e.g., service utilization) inequities, as the expansion of CSC continues.
Supplementary Material
Funding
This work was supported by the National Institute of Mental Health [Grant Number K01MH117457].
Footnotes
Supplementary Information The online version contains supplementary material available at https://doi.org/10.1007/s10488-021-01137-3.
Declarations
Conflict of interest The authors have no conflicts of interest to disclose.
Ethical Approval The Washington State University Institutional Review Board (IRB) determined that this study did not require IRB review because it was not classified as human subjects’ research.
References
- Amiri S, McDonell MG, Denney JT, Buchwald D, & Amram O (2020). Disparities in access to opioid treatment programs and office-based buprenorphine treatment across the rural-urban and area deprivation continua: A US nationwide small area analysis. Value in Health 10.1016/j.jval.2020.08.2098 [DOI] [PubMed]
- Andersen RM (1995). Revisiting the behavioral model and access to medical care: Does it matter? Journal of Health and Social Behavior, 36(1), 1–10. 10.2307/2137284 [DOI] [PubMed] [Google Scholar]
- Cabassa LJ, Piscitelli S, Haselden M, Lee RJ, Essock SM, & Dixon LB (2018). Understanding pathways to care of individuals entering a specialized early intervention service for first-episode psychosis. Psychiatric Services, 69(6), 648–656. 10.1176/appi.ps.201700018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chow JC-C, Jaffee K, & Snowden L (2003). Racial/ethnic disparities in the use of mental health services in poverty areas. American Journal of Public Health, 93(5), 792–797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Correll CU, Galling B, Pawar A, Krivko A, Bonetto C, Ruggeri M, Craig TJ, Nordentoft M, Srihari VH, Guloksuz S, Hui CLM, Chen EYH, Valencia M, Juarez F, Robinson DG, Schooler NR, Brunette MF, Mueser KT, Rosenheck RA, … Kane JM (2018). Comparison of early intervention services vs treatment as usual for early-phase psychosis: A systematic review, meta-analysis, and meta-regression. JAMA Psychiatry, 75(6), 555–565. 10.1001/jamapsychiatry.2018.0623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummings JR, Allen L, Clennon J, Ji X, & Druss BG (2017). Geographic access to specialty mental health care across high- and low-income U.S. communities. JAMA Psychiatry, 74(5), 476–484. 10.1001/jamapsychiatry.2017.0303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummings JR, Case BG, Ji X, & Marcus SC (2016). Availability of youth services in U.S. mental health treatment facilities. Administration and Policy in Mental Health and Mental Health Services Research, 43(5), 717–727. 10.1007/s10488-015-0685-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummings JR, Wen H, Ko M, & Druss BG (2014). Race/ethnicity and geographic access to medicaid substance use disorder treatment facilities in the United States. JAMA Psychiatry, 71(2), 190–196. 10.1001/jamapsychiatry.2013.3575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dinwiddie GY, Gaskin DJ, Chan KS, Norrington J, & McCleary R (2013). Residential segregation, geographic proximity and type of services used: Evidence for racial/ethnic disparities in mental health. Social Science & Medicine, 1982(80), 67–75. 10.1016/j.socscimed.2012.11.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Everett A, & Heinssen R (2019). Agency priority goal action plan: Serious mental illness Department of Health and Human Services. Retrieved from https://www.performance.gov/health_and_human_services/2019_dec_HHS_Serious_Mental_Illness.pdf [Google Scholar]
- Graves JM, Amiri S, Mackelprang JL, Abshire DA, Beck A, & Olsen M (2020). Nowhere to go for help: Geographic disparities in access to mental health facilities for youth Retrieved from https://apha.confex.com/apha/2020/meetingapi.cgi/Paper/482179?filename=2020_Abstract482179.html&template=Word
- Guagliardo MF (2004). Spatial accessibility of primary care: Concepts, methods and challenges. International Journal of Health Geographics, 3(1), 3. 10.1186/1476-072X-3-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kane JM, Schooler NR, Marcy P, Correll CU, Brunette MF, Mueser KT, Rosenheck RA, Addington J, Estroff SE, & Robinson J (2015). The RAISE early treatment program for first-episode psychosis: Background, rationale, and study design. The Journal of Clinical Psychiatry, 76(3), 240–246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kind AJH, & Buckingham WR (2018). Making neighborhood-disadvantage metrics accessible—The neighborhood Atlas. The New England Journal of Medicine, 378(26), 2456–2458. 10.1056/NEJMp1802313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knighton AJ, Savitz L, Belnap T, Stephenson B, & VanDerslice J (2016). Introduction of an area deprivation index measuring patient socioeconomic status in an integrated health system: Implications for population health. EGEMs, 4(3), 9. 10.13063/2327-9214.1238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ku BS, Pauselli L, Manseau M, & Compton MT (2020). Neighborhood-level predictors of age at onset and duration of untreated psychosis in first-episode psychotic disorders. Schizophrenia Research 10.1016/j.schres.2019.12.036 [DOI] [PMC free article] [PubMed]
- Mathis WS, Woods S, & Srihari V (2018). Blind spots: Spatial analytics can identify nonrandom geographic variation in first episode psychosis program enrollments. Early Intervention in Psychiatry, 12(6), 1229–1234. 10.1111/eip.12681 [DOI] [PubMed] [Google Scholar]
- McGrail MR (2012). Spatial accessibility of primary health care utilising the two step floating catchment area method: An assessment of recent improvements. International Journal of Health Geographics, 11(1), 50. 10.1186/1476-072X-11-50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moe AM, Rubinstein EB, Gallagher CJ, Weiss DM, Stewart A, & Breitborde NJ (2018). Improving access to specialized care for first-episode psychosis: An ecological model. Risk Management and Healthcare Policy, 11, 127–138. 10.2147/RMHP.S131833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Donoghue B, Lyne JP, Renwick L, Lane A, Madigan K, Staines A, O’Callaghan E, & Clarke M (2016). Neighbourhood characteristics and the incidence of first-episode psychosis and duration of untreated psychosis. Psychological Medicine, 46(7), 1367–1378. 10.1017/S003329171500286X [DOI] [PubMed] [Google Scholar]
- Oluwoye O, Cheng SC, Fraser E, Stokes B, & McDonell MG (2019). Family experiences prior to the initiation of care for first-episode psychosis: A meta-synthesis of qualitative studies. Journal of Child and Family Studies, 29, 2530–2541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oluwoye O, Reneau H, Stokes B, Daughtry R, Venuto E, Sunbury T, Hong G, Lucenko B, Stiles B, & McPherson SM (2019). Preliminary evaluation of Washington State’s early intervention program for first-episode psychosis. Psychiatric Services, 71, 228–235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oluwoye O, Stiles B, Monroe-DeVita M, Chwastiak L, McClellan JM, Dyck D, Cabassa LJ, & McDonell MG (2018). Racial-ethnic disparities in first-episode psychosis treatment outcomes from the RAISE-ETP study. Psychiatric Services (Washington DC) 10.1176/appi.ps.201800067 [DOI] [PMC free article] [PubMed]
- Reichert A, & Jacobs R (2018). Socioeconomic inequalities in duration of untreated psychosis: Evidence from administrative data in England. Psychological medicine Cambridge University Press. [DOI] [PubMed] [Google Scholar]
- Rosenblatt A (2018). SAMHSA-Funded Programs for First Episode Psychosis Across the United States The NIMH Mental Health Services Research Conference. [Google Scholar]
- Schuurman N, Bérubé M, & Crooks VA (2010). Measuring potential spatial access to primary health care physicians using a modified gravity model. The Canadian Geographer / Le GéographeCanadien, 54(1), 29–45. 10.1111/j.1541-0064.2009.00301.x [DOI] [Google Scholar]
- Singh GK (2003). Area deprivation and widening inequalities in US mortality, 1969–1998. American Journal of Public Health, 93(7), 1137–1143. 10.2105/AJPH.93.7.1137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stain HJ, Halpin SA, Baker AL, Startup M, Carr VJ, Schall U, Crittenden K, Clark V, Lewin TJ, & Bucci S (2018). Impact of rurality and substance use on young people at ultra high risk for psychosis. Early Intervention in Psychiatry, 12(6), 1173–1180. 10.1111/eip.12437 [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. (n.d.). American Community Survey (ACS) Retrieved from http://www.census.gov/programs-surveys/acs
- USDA. (n.d.). Rural-Urban Commuting Area Codes Retrieved December 27, 2020 from https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes/
- van der Ven E, Susser E, Dixon LB, Olfson M, & Gilmer TP (2020). Racial-ethnic differences in service use patterns among young, commercially insured individuals with recent-onset psychosis. Psychiatric Services, 71(5), 433–439. 10.1176/appi.ps.201900301 [DOI] [PubMed] [Google Scholar]
- Wright A, Browne J, Mueser KT, & Cather C (2019). Evidencebased psychosocial treatment for individuals with early psychosis. Child and Adolescent Psychiatric Clinics, 29(1), 211–223 [DOI] [PubMed] [Google Scholar]
- WWAMI Rural Health Research Center. (n.d.). Rural urban commuting area codes—RUCA Retrieved December 27, 2020 from http://depts.washington.edu/uwruca/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


