Abstract
Purpose
To highlight the eye movement disturbances in anti-IgLON5 disease.
Methods
Case report.
Results
Anti-IgLON5 is a heterogenous neurodegenerative and autoimmune disease manifested by a variety of signs and symptoms including sleep disorder, bulbar dysfunction, movement disorder, cognitive impairment, and autonomic dysfunction.
Conclusions and Importance
Eye movement disturbances (e.g., nystagmus, gaze palsy, slow saccadic velocities) can be a prominent clinical feature of anti-IgLON5 disease.
Keywords: Gaze palsy, IgLON5, Autoimmunity, Sleep disorder, Bulbar dysfunction
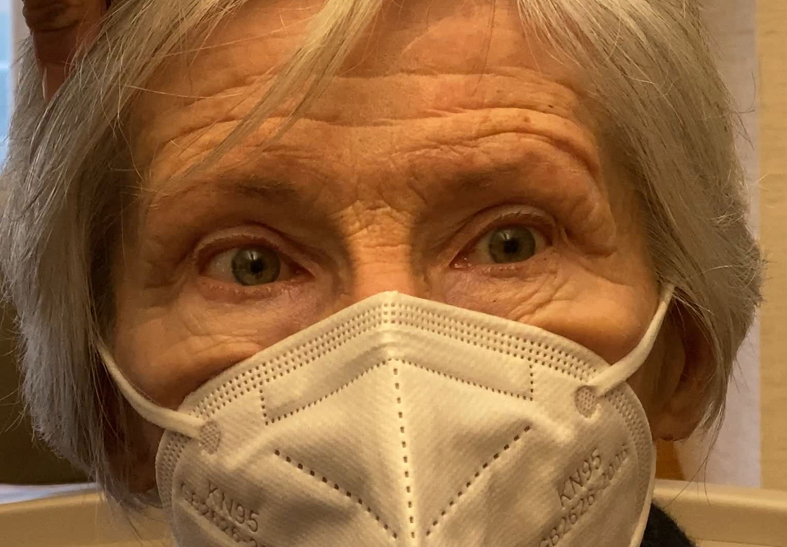
A 75-year-old woman presented with progressive neurological symptoms that started 10 years prior to evaluation. Her initial symptoms were of facial tightening and throat pulsations. The neurological examination was noted to be normal at the time. Magnetic resonance imaging of the brain with contrast detected only an incidental right middle cranial fossa arachnoid cyst. Anti-GAD and anti-ANNA1 were negative. She was diagnosed with oromandibular dystonia for which botulinum toxin injections were performed. One year prior to evaluation at our institution she was noted to have mild hyperkinetic movement of the face and upper extremities. She complained of poor sleep and difficulty walking occasionally leading to falls. She did not have double vision but when moving about felt a sense of unsteadiness. There was no ptosis in either eye. Eye movement examination demonstrated absence of nystagmus with intact vertical smooth pursuit eye movements including normal saccadic accuracy and velocity in both directions. Both horizontal smooth pursuit and saccadic eye movements were limited particularly in left gaze but also in right gaze with mild slowing of the rightward saccades (video), that could not be overcome with oculocephalic maneuver. Serum cell-based assay for anti-IgLON5 was positive. Due to her neurological disability she was started on intravenous immunoglobulin by her neurologist.
Anti-IgLON5 disease is an autoimmune and neurodegenerative disorder that was first described in 2014 with a commercially available assay to detect antibodies against IgLON5 becoming available in 2015.1 IgLON5 is an immunoglobulin-like cell adhesion molecule found in the central nervous system. It is not clear if anti-IgLON5 disease is a primary tauopathy that incites an immune response or a primary autoimmune disorder resulting in abnormal tau phosphorylation and deposition in neurons. Pathologically the predominant 2 areas of pathology are the hypothalamus and brainstem tegmentum.2
It is a heterogenous disorder with mean age of presentation of approximately 60 years with no gender predilection. The clinical course is often chronic with progressive symptomology over time. There is often a delay in diagnosis due to the chronic and diverse clinical manifestations. The neurological symptoms are typically dominated by disturbances in sleep and movement. The clinical manifestations of anti-IgLON5 disease can overlap with progressive supranuclear palsy (PSP).3
The disease is clinically characterized by the following:3,4
-
•
Sleep disorder (e.g., rapid eye movement (REM) and non-REM sleep parasomnia, sleep disordered breathing)
-
•
Bulbar dysfunction (e.g., dysphagia, dysarthria, laryngeal stridor, sialorrhea)
-
•
Movement disorder (e.g., postural instability, stiffness, dystonia, chorea)
-
•
Cognitive impairment
-
•
Autonomic dysfunction (e.g., orthostatic dysregulation, sexual dysfunction, urinary urgency, nocturnal enuresis, bradycardia, perspiration)
-
•
Eye movement dysfunction (e.g., nystagmus, gaze palsy, slow saccadic velocities)
Ophthalmologists should be familiar with anti-IgLON5 disease because dysfunction of eye movements can be a prominent feature of the clinical manifestations.4,5 There are few eye movement videos published in the literature that highlight the variable horizontal, vertical, smooth pursuit and saccade eye movement dysfunction that can be seen in individual patients with anti-IgLON5 disease.6,7 Recognition of these ocular motility disturbances in the context of the other neurological and systemic symptoms can assist the neurologist in establishing the correct diagnosis.
Patient consent
Consent to publish this case report has been obtained from the patient(s) in writing.
Funding
No funding or grant support
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Declaration of competing interest
The following authors have no financial disclosures: MTB.
Acknowledgements
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ajoc.2022.101574.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
figs1.
References
- 1.Nissen M.S., Blaabjerg M. Anti-IgLON5 disease: a case with 11-year clinical course and review of the literature. Front Neurol. 2019 Oct 2;10:1056. doi: 10.3389/fneur.2019.01056. PMID: 31632341; PMCID: PMC6783555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gelpi E., Höftberger R., Graus F., et al. Neuropathological criteria of anti-IgLON5-related tauopathy. Acta Neuropathol. 2016 Oct;132(4):531–543. doi: 10.1007/s00401-016-1591-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Heidbreder A., Philipp K. Anti-IgLON 5 disease. Curr Treat Options Neurol. 2018 Jun 23;20(8):29. doi: 10.1007/s11940-018-0515-4. [DOI] [PubMed] [Google Scholar]
- 4.Gaig C., Graus F., Compta Y., et al. Clinical manifestations of the anti-IgLON5 disease. Neurology. 2017 May 2;88(18):1736–1743. doi: 10.1212/WNL.0000000000003887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Macher S., Milenkovic I., Zrzavy T., et al. Ocular motor abnormalities in anti-IgLON5 disease. Front Immunol. 2021 Sep 30;12:753856. doi: 10.3389/fimmu.2021.753856. PMID: 34659261; PMCID: PMC8514941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Villacieros-Álvarez J., Ordás C.M., Torres-Gaona G., Díez-Barrio A., Prieto-Jurczynska C., Gaig C. Teaching video NeuroImages: anti-IgLON5 disease: a long-course presentation with a response to immunotherapy. Neurology. 2021 Jun 8;96(23):e2901–e2902. doi: 10.1212/WNL.0000000000011381. [DOI] [PubMed] [Google Scholar]
- 7.Montojo T., Piren V., Benkhadra F., Codreanu A., Diederich N.J. Gaze palsy, sleep and gait disorder, as well as Tako-Tsubo Syndrome in a patient with IgLON5 antibodies. Mov Disord Clin Pract. 2016 Jul 28;4(3):441–443. doi: 10.1002/mdc3.12407. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.