Abstract
Health concerns in Indigenous people are often greater in comparison to those in non-Indigenous populations, including increased rates of chronic diseases and mental health concerns. Adverse childhood experiences (ACEs) may be an explanatory variable for such heightened rates of mental and physical health difficulties for Indigenous populations as these communities have experienced a lack of adequate health care due to remoteness, historical traumas, cultural insensitivity, racism, and perpetuating systemic discrimination. To date, relatively few studies have examined ACEs within an Indigenous population and their relevance to both physical and mental health outcomes. The present study explored existing ACE literature relevant to Indigenous populations and mental or physical health outcomes by retrieving and organizing available ACE literature. A systematic review was conducted using 14 electronic databases of peer-reviewed literature and 18 grey literature databases. Twenty-one publications investigating general health outcomes and prevalence of ACEs met eligibility criteria. ACEs were reported to be higher in Indigenous populations when compared to non-Indigenous population. Higher ACE scores for Indigenous participants were associated with increased rates of suicidality and psychological distress. Protective factors to reduce the impact of ACEs were cultural identity and connectedness, education, social support, and psychological resilience. Future research may further explore the relationship between ACE scores and protective factors, varying prevalence within specific sub-populations, and consistent reporting of outcomes across studies. Ongoing research has the potential to clarify existing dose–response relationships between early traumatic experiences and current health disparities experienced within some Indigenous communities.
Keywords: Systematic review, Indigenous health, Adverse childhood experiences, Preventative care, First Nations health
Indigenous populations are more likely to report poorer physical and mental health outcomes compared to non-Indigenous populations in Canada (Statistics Canada, 2017a). Rates of chronic physical conditions (e.g., obesity, diabetes, arthritis/rheumatism, high blood pressure, and heart disease) and mental health difficulties (e.g., depression, anxiety) all appear to be higher among Indigenous people than non-Indigenous people (First Nations Centre, 2005; Kumar & Tjepkema, 2019; Statistics Canada, 2018). Many of these reported health difficulties appear to be stable over time, despite trajectories for the aforementioned health outcomes improving for non-Indigenous populations in recent decades (Statistics Canada, 2018).
Increased rates of mental and physical health problems in Indigenous populations are related to, and potentially exacerbated by, chronic inaccessibility to factors that facilitate positive development of the social determinants of health (Canadian Public Health Association, 2019). Indigenous populations are at increased risk for unstable housing, lower socioeconomic status, and increased malnutrition (Statistics Canada, 2017b, 2018), all of which can increase risk for infectious diseases, delayed development in childhood, substance-use related health concerns, and prevalence of lifestyle diseases (including diabetes, hypertension, cardiovascular diseases, and chronic renal diseases; Gracey & King, 2009). Indigenous peoples are also more likely to be confronted with stressful experiences such as witnessing traumatic events (e.g., violence, assault, and homicide), experiencing poverty, and unemployment (Bombay et al., 2011; Statistics Canada, 2018). For example, Indigenous women are approximately 3 times as likely as non-Indigenous women to be a victim of a violent crime while Indigenous boys and men are 7 times more likely than non-Indigenous boys and men to be a homicide victim (Statistics Canada, 2018). As Indigenous people are more likely to be victims of homicide, as well as experience higher rates of infant and child mortality, and accidental death, these experiences may contribute to decreased life expectancies for Indigenous people in Canada (Statistics Canada, 2018).
Continuous exacerbation of these health concerns is partially attributed to experiences of discrimination, historical experiences of cultural assimilation and oppression, and systemic underfunding of health services (Truth and Reconciliation Commission of Canada [TRCC], 2015). Particularly profound historical stressors experienced by Indigenous peoples in Canada include the residential school system, where the Canadian government mandated cultural assimilation beginning in 1863 and ending in 1996 (Bombay et al., 2009, 2011; TRCC, 2015). This system perpetuated childhood maltreatment including neglect and physical, sexual, and psychological abuse and also actively disciplined children for cultural or spiritual participation, such as speaking one’s Indigenous language (TRCC, 2015).
The oppressive acts perpetrated in residential schools have been associated with increased isolation from family, attachment difficulties, parenting challenges, and loss of cultural identity (Hackett et al., 2016; RHS National Team, 2007; Ross et al., 2015), all of which have ramifications to physical and mental health outcomes across generations (Bombay et al., 2009). Indeed, individuals whose parents attended residential schools are at increased risk for greater depressive symptoms, suicide, post-traumatic stress disorder (PTSD), and general psychological distress (Bombay et al., 2008, 2009). Persistent effects of trauma experienced from residential school attendance, coupled with the current health conditions and continued discrimination experienced by Indigenous peoples, contribute to a transmission of health concerns experienced across generations (Bombay et al., 2009). This concept of intergenerational trauma, and experiences of trauma spanning across generations, has been discussed and has specific implications within Indigenous communities (Nelson & Wilson, 2017).
Adverse Childhood Experiences
The effects of colonization and associated historical trauma inflicted on Indigenous peoples also appear to be associated with adverse childhood experiences (ACEs) across generations. It is possible that the increased rates of mental and physical health-related issues among Indigenous peoples may be partially attributed to a higher prevalence of ACEs in this population. According to this framework, there are ten ACEs defined as exposure to abuse (i.e., physical, sexual, emotional), neglect (i.e., physical and emotional), and household dysfunction (i.e., parental incarceration, violence to one’s mother within the home, household substance abuse, household mental illness, and parental separation) that occur within the developmental years (i.e., 0–18 years old; Felitti et al., 1998). Twenty years of research on ACEs has exemplified that exposure to these adversities is associated with an array of negative health outcomes and behaviours such as depression, PTSD, substance use problems, and suicide, among others (Dube, 2019; Fuller-Thompson et al., 2016).
Researchers have postulated a dose–response relationship between the number of childhood exposures and risk factors for the leading causes of death such that the more ACEs an individual is exposed to, the higher they are at risk for detrimental outcomes (i.e., smoking, severe obesity, depressed mood, suicide attempts, alcoholism, drug abuse, a high lifetime number of sexual partners, and a history of having a sexually transmitted disease; Felitti et al., 1998). Researchers have identified avenues of biological interference in response to ACEs. The biological effects of ACEs have made it difficult to mitigate the effects of intergenerational transmission of these experiences. This has led to an ancestral transmission of biopsychosocial responses to stress thereby exacerbating mental and physical outcomes.
ACEs Across Generations
ACEs appear to be transmitted intergenerationally among Indigenous peoples, such that adults who had a parent attend a residential school report increased ACEs themselves (Bombay et al., 2008, 2009). Similarly, Indigenous adults report that their parents’ attendance at a residential school negatively affected the quality of parenting they received as children (RHS National Team, 2007). Indigenous peoples’ who have had a family member attend residential school have been found to experience a greater likelihood of having lower self-perceived mental health, great psychological distress, suicidal ideation and attempts (Hackett et al., 2016).
The Indigenous population in Canada has grown by 43% since 2006, more than four times the growth rate of the non-Aboriginal population over the same time (Statistics Canada, 2018). The Indigenous population is also significantly younger than the non-Indigenous population (32% versus 41% in 2016, respectively; Statistics Canada, 2018), with proportionally more children and youth, and fewer seniors. Further, generations tend to be shorter and Aboriginal people are having children at a younger age (Statistics Canada, 2018). This census data suggests that, should ACEs continue to be transmitted intergenerationally among Indigenous peoples, prevention efforts will be essential for those at risk.
Ultimately, understanding how ACEs contribute to the transmission of mental and physical health symptoms between generations of Indigenous peoples can help inform prevention and intervention initiatives. There are significant health disparities seen in Indigenous populations that may be in part explained by the long-term associations between ACEs and adult health risk behaviours, health status, and diseases (Adelson, 2005; Basu & Isaacs, 2019; First Nations Centre, 2005; Statistics Canada, 2018). Significant health disparities that have been identified in this population include diabetes, arthritis, high blood pressure, as well as mental health difficulties (Adelson, 2005). Understanding how the ACE model can be applied within Canadian Indigenous contexts allows for comparison and differentiation of the model compared to the existent model that is largely conceptualized using data from non-Indigenous populations.
Purpose
The goal of the present study was to conduct a systematic review of existent ACE literature among Indigenous populations and mental or physical health outcomes. Many Indigenous populations have unique experiences that may differ from non-Indigenous cultures, and as a result, have reported unique health needs. Although much literature has been dedicated to ACE literature in general, a synthesis of this information that is relevant for Indigenous populations has yet to be completed. Given that this study was exploratory in nature, no hypotheses were assessed in this review. Rather, the goal of the study was to retrieve and organize available ACE literature pertaining to Indigenous populations to further our understanding of existent literature and to provide a foundation for future research in this area. Specifically, some questions of interest for this review were: (a) what are the mental health difficulties associated with exposure to ACEs? and (b) what are the physical health difficulties associated with exposure to ACEs? For the context of this review, the term “Indigenous” is used to describe specific groups of people in Canada, the United States of America, Australia, and Greenland including Canadian First Nations, Métis, Inuit, and Aboriginal, American Indian, Alaska Native, and Native Hawaiian populations in order to be inclusive of the many Indigenous groups globally. Although the term Indigenous broadly encompasses many distinct groups of people with different languages, traditions, and experiences, one goal of this review was to remain inclusive toward studies that met these criteria and/or self-identified their participants as First Peoples or Indigenous.
Method
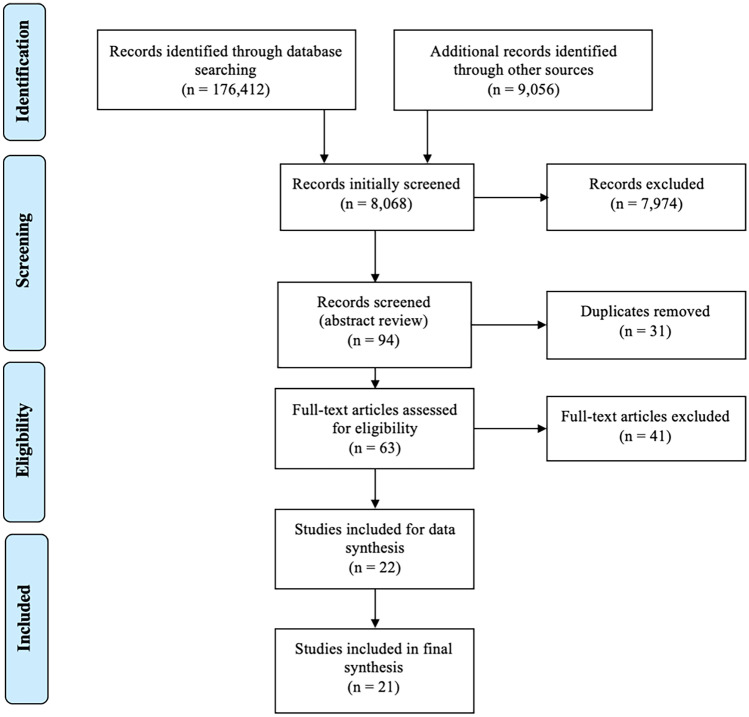
Searches were completed and subsequent results reported in adherence with Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guidelines. Figure 1 summarizes the complete study selection process (PRISMA diagram). Although the goal was to initially review literature specifically for Canadian Indigenous populations, the search terms were broadened due to a preliminary lack of results and thus were subsequently expanded to encompass Indigenous populations globally (i.e., United States of America, Australia, Greenland). Fourteen electronic databases were searched using search terms developed to identify ACEs in Indigenous populations internationally (Table 1). Searches were completed between September 1 and October 30, 2019.
Fig. 1.
PRISMA Diagram of Included Studies
Table 1.
Databases and Search Terms
| Academic Databases | Grey Literature |
|---|---|
|
Academic Search Premier ERIC (via EBSCO) ERIC (via PROQuest) Evidence-Based Medicine (EBM) Reviews JSTOR ProQuest PsycARTICLES PsycINFO PubMed ScienceDirect Social Sciences Citation Index Social Services Abstracts Social Science Research Network (SSRN) Web of Science |
Ontario Centre of Excellence for Child and Youth Mental Health McCreary Centre Society Canadian Child Welfare Research Portal Child Welfare League of Canada First Nations Child & Family Caring Society Canadian Coalition for the Rights of Children PLEA Community Services Open Grey Repository Mental Health Commission of Canada Centre for Children and Youth in Challenging Contexts Ementalhealth.ca Institute of Mental Health Research (IMHR) CHEO Research Institute Ottawa Hospital Research Institute (OHRI) ClinicalTrials.gov Indigenous Studies Portal |
|
Search Terms “adverse child* experience*” OR “ACE” OR “adverse child* event*” AND "Indigenous" OR "Aboriginal" OR "Inuit" OR "First Nation*" OR "Métis" OR "Native" OR "Indian" | |
Studies were included if they (a) comprised of participants who identified as Indigenous, (b) identified any type of formally classified ACEs, (c) were written in English language, (d) were peer-reviewed, and (e) were published from 2000 to present. Searches were modified to list by relevance and the first 1,000 results were searched in each database. Studies were included if they reported any physical or mental health outcomes. Any broad definition or measurement of mental and physical health were included. For example, self-perceived, self-report measurement, objective measurement, and/or clinical diagnoses were included. Researchers screened all titles and abstracts based on eligibility criteria and saved to a reference manager. Full-text literature reviews were then conducted for each article included. Consultation was held between researchers to ensure included articles met eligibility requirements. Data relating to ACEs and general physical and mental health outcomes were extracted from the included studies. Data included sample size and composition, study design, ACEs reviewed, and outcomes.
Results
Of the 10,846 articles screened, 21 publications reporting results investigating general health outcomes and prevalence of ACEs in any global Indigenous populations met eligibility criteria. All 21 publications were identified from peer-reviewed databases. One study was conducted as a qualitative study, six studies were conducted as a mixed-methods study, and 18 were conducted as a quantitative study. Within the quantitative studies, six studies utilized logistic regression to calculate odds ratio, one Poisson Ratios, one relative risk ratios, two descriptive studies, one longitudinal, while the remainder (seven studies) used linear regressions, correlations, and chi squared analyses. All studies (N = 21) reported that increased ACEs were associated with detrimental health outcomes. Four studies reported that participant ACE scores were related to self-reported physical health outcomes (Brockie et al., 2018; Moon et al., 2015; Remigio-Baker et al., 2017; Twizeyemariya et al., 2017). One study reported ACEs associated with sleep problems (Klest et al., 2013), and another study examined ACEs and parenting satisfaction (Libby et al., 2008) (Table 2).
Table 2.
Data Extraction Table
| Author | Participant Description | Study Method | ACEs Reviewed | Outcomes |
|---|---|---|---|---|
| (Basu & Isaacs, 2019) |
Australian Aboriginal n = 48 Non-aboriginal Australians n = 53 Total sample 60% male; Aboriginal males less than half Patients with a transcultural background who attended the Child and Adolescent Mental Health Service of Latrobe Regional Hospital in Gippsland, Victoria from 2013 to 2017 |
Quantitative Descriptive analysis |
Physical Abuse Sexual Abuse Emotional Abuse Neglect Parental substance abuse Parent in jail Parental Separation Parent/sibling with mental illness |
In the full sample the most commonly reported psychosocial stressors were family conflict and death (44.6%), domestic violence (41.6%) and emotional abuse (34.7%). Females were more likely than boys to be sexually abused (p < .001) Higher rates of male and female Aboriginal incarceration (p < .005), domestic violence (p < .005), disconnection from culture, perceived loss of cultural identity, and conduct disorder diagnoses (p < .005). Aboriginal Australian children had a higher chance of being removed from their family by the child protective services than other Australian children |
| (Bjerregaard & Larsen, 2018) |
Data obtained from the 2014 Greenland Health Survey, whereas: ~ 90% Inuit ~ 10% Non-Inuit; Greenland |
Qualitative Review |
Sexual Abuse Parental Substance Use Household Violence |
The majority of the sample (66%) reported childhood exposure to: (A) alcohol problems in the home; (B) physical abuse; (C) sexual abuse; (D) a combination of two or more of the above ACEs. Approximately 60% of adults and up to one-third of youth (15–17 years) reported losing friends or family members to suicide |
| (Bombay et al., 2011) |
First Nation Female, n = 107 First Nation Male, n = 36 Canadian |
Quantitative Correlation |
Physical Abuse Sexual Abuse Emotional Abuse Emotional Neglect Physical Neglect Single parent household Household Violence Household Substance Abuse Household Mental Illness Household Criminal Behaviour |
Number of ACEs correlated with depressive symptoms (r = .42, p < .001), greater risk of revictimization (r = .47, p < .001), and lower household income (r = -.24, p < .01) Individuals whose parents had attended residential schools reported greater depressive symptoms than individuals whose parents did not attend F (1, 139) = 10.34, p < .01, as well as more frequent ACEs F (1, 115) = 9.09, p < .01 |
| (Brockie et al., 2015) |
Native American N = 288 15–24 years (15–19 year age group = 59%; Mean = 19.25 years) Female: n = 147 (51%) Male: n = 135 (49%) Attending school: 48% |
Quantitative Cross-sectional, self-report Chi-square Odds ratio/ Logistic regression |
Physical Abuse Sexual Abuse Emotional Abuse Physical Neglect Emotional Neglect Witness to IPV |
Overall, 78% of participants reported at least one ACE, 58.6% reported two, and 4% reported all six ACES. 63% had a low ACE score (0–2), 37% had a high ACE score (3–6). Emotional neglect, physical neglect, witnessed IPV (against mother) reported by 30% of participants; 40% reported emotional abuse. Males were more likely to report physical neglect than females (χ2(1) = 5.01, p < .05), whereas females were more likely to report emotional abuse (χ2 (1) = 4.12, p < .05) and sexual abuse (χ2 (1) = 5.26, p < .05) Older participants (20–24 years) reported higher prevalence of physical (χ2(1) = 4.14, p < .05) and sexual abuse (χ2 (1) = 4.60, p < .05), as well as overall ACE scores relative to younger participants (15–19 years). Individuals not attending school had higher ACE scores than those attending school. Individuals who were not attending school were more likely than those attending school to report physical abuse (χ2(1) = 6.7, p < .05), witnessing IPV (χ2 (1) = 5.35, p < .05), and emotional neglect (χ2 (1) = 5.3, p < .05) Five of six ACEs were independently, significantly related to: (A) Depression symptoms (all except sexual abuse); (B) Poly-drug use (all except physical neglect) and; (C) Suicide attempt (all except sexual abuse). Four ACES (except sexual abuse and emotional neglect) were related to PTSD symptoms. Individuals with high ACE scores more likely to report depression symptoms (p < .05), poly-drug use (p < .001), PTSD symptoms p < .001), and suicide attempt (p < .001) Exposure to IPV (OR = 2.96, p < .001) strongly and significantly increased the odds of PTSD symptoms and poly-drug use (OR = 5.3, p < .001). Depression symptoms (OR = 3.68, p < .001) and suicide attempt (OR = 2.90, p < .001) most strongly predicted by physical abuse |
| (Brockie et al., 2018) |
American Indian men and women with Type 2 Diabetes N = 192 55.7% Female Mage = 46.3, (12.2) AI Tribal Clinics in five reservations in the Upper Midwest, USA |
Mixed Method OLS Regression |
Physical Abuse Sexual Abuse Emotional Abuse Physical Neglect Emotional Neglect Witness to IPV Parental Separation Family Incarcerated Family with Mental Illness Family Substance Abuse |
Participants reported an average of 3.05 ACES; 81.9% reported experiencing at least one ACE. ACEs were negatively associated with self-reported mental and physical health (p < .05). Mental and physical health were positively associated with connectedness and social support. High ACE scores associated with lower ratings of physical health; this relationship was moderated by perceived social support and diabetes-specific social support. Mental health positively associated with participant’s involvement in spiritual activities |
| (Burnette et al., 2017) |
American Indian and Caucasian participants Age: 50 years + N = 479 American Indian /Alaskan Native (AI/AN) n = 231 Mage = 60.6 Male: 45.6% Non AI/AN: n = 248 Mage = 74.0 United States |
Quantitative Survey Chi-square, t-test Hierarchical regression |
Physical Abuse Sexual Abuse Emotional Abuse Physical Neglect Emotional Neglect Witness to IPV Parental Separation Family Incarcerated Family with Mental Illness Family Substance Abuse |
Higher overall ACE scores (M = 2.55) in American Indian/Alaskan Native older adults than non-AI/AN individuals (M = 0.83). Significantly higher scores on childhood abuse, childhood neglect, and childhood household dysfunction subscales for AI/AN older adults (mean scores: 0.68,0.32, and 1.59) than non-AI/AN older adults (mean scores: 0.27, 0.14, and 0.42) Higher levels of depressive symptoms reported among AI/AN older adults living alone (β = .368, p ≤ .05), with high levels of childhood abuse (β = .275, p ≤ .05), or childhood household dysfunction (β = .232, p ≤ .05). Being employed (β = -.337, p ≤ .05) and adult social support (β = –.030, p ≤ .01) were significantly associated with lower levels of depressive symptoms |
| (De Ravello et al., 2008) |
American Indian/Alaskan Native women who were incarcerated in New Mexico N = 36 Mage = 36 years Age Range 20–60 years |
Mixed Method Frequencies, multivariate analyses |
Physical Abuse Sexual Abuse Emotional Abuse Physical Neglect Witness to IPV Family Substance Use Family Incarcerated Family with Mental Illness |
35 of 36 participants reported at least one ACE; 81% had two or more ACES. Individuals with high ACE scores (4–5) were seven times more likely to have attempted suicide (RR = 7.19, 95% CI = 1.9226.99, p < .001) than women with low ACE scores (0–2). The majority of participants reported experiencing IPV (83%), alcohol use at a younger age (54% < 15 years), illicit drug use (84%), poly-drug use (49%), mental health problem diagnosis (36%). Half of participants reported that they had considered suicide; of these 83% had attempted suicide 75% of women had an immediate family member with an alcohol or drug problem; 72% witnessed domestic violence; 69% had an immediate family member incarcerated; 53% had been sexually abused by a family member or loved one; 42% had been physically abused; 42% family member with mental illness; 33% both sexually and physically abused by family member or loved one; 22% experienced physical neglect |
| (Fuller-Thomson & Lewis, 2015) |
18 years + With data regarding ACEs and ADHD dx Male: n = 10 496 Female: n = 12 877 10 Canadian provinces 2012 Canadian Community Health Survey – Mental Health: Statistics Canada |
Quantitative Logistic Regression |
Physical Abuse Sexual Abuse IPV |
In the full sample, childhood physical (men OR = 1.66, p < .001; women OR = 1.95, p < .001) and sexual abuse (men OR: 2.57, p < .001; women OR 2.55, p < .001) associated with higher odds of ADHD diagnosis. Exposure to IPV increased odds of ADHD diagnosis in women (OR: 1.54, p < .03) |
| (Hamdullahpur et al., 2018) |
Aboriginal women: n = 83 Non-Aboriginal women: n = 89 16 years + in Canada Referrals from centers providing: social services, basic need support, mental health supports, and medical services |
Semi-structured interview Questionnaires T-Test, Chi square, Linear regression |
Physical Abuse Sexual Abuse Neglect Witness IPV |
Aboriginal and non-Aboriginal women reporting childhood sexual abuse (CSA) were more likely to experience other ACEs, reporting: parental psychological problems (63.2%; χ2(1) = 5.37,p = .02); parental drug/alcohol abuse (70.1%; χ2(1) = 6.92, p = .009); fear of being sexually abused when a parent was intoxicated, (χ2(1) = 16.38, p < .001); and to have verbally abusive parents (χ2(1) = 23.28,p = .0001) Half of the CSA sample was comprised of Aboriginal women. These women were more likely to report witnessing verbal abuse between parents (77%: χ2(1) = 11.24, p = .002); witnessing IPV (80.8%; χ2(1) = 20.67,p < .001); witnessing sexual abuse of a family member (44.2%; χ2(1) = 9.06, p = .006); and physical abuse (χ2(1) = 19.81, p < .001) than the non-CSA sample. They were more likely to have attempted suicide (χ2(1) = 6.89,p = .009); have relationship problems with parents (χ2(1) = 6.01, p = .014); and to have previously received treatment for psychological problems (75.0%, χ2(1) = 11.02,p = .001) |
| (Kenney & Singh, 2016) |
American Indians n = 1453 Male: 54.2% Female: 45.8% Non-Hispanic White n = 61,381 Male: 51.6% Female: 48.4% 2011–2012 National Survey of Children’s Health |
Cross-sectional Z-scores, Logistic regression |
Witness IPV Parent Mental Illness Parent Substance Abuse Parent Incarceration |
American Indian (AI) children were more likely to have parent incarcerated, witness/be victim to violence, and live with individual abusing substances. AI children were 2–3 times as likely as non-Hispanic white children to have multiple ACEs. Two or more ACEs associated with increased prevalence of depression, ADHD, and anxiety disorders in AI children |
| (Klest et al., 2013) |
N = 833 Hawaiians (n = 148 Native Hawaiian) 47% Men 53% Women Age 51–60 years; Mage = 55.05, SD = 2.00 Members of the Hawaii Personality and Health cohort (elementary students between 1959–1967) |
Longitudinal Cohort Study |
Physical Abuse Sexual Abuse Emotional Neglect Physical Neglect Witness to IPV Family Substance Use Family Incarcerated Family with Mental Illness |
In the full sample 78.6% of participants reported exposure to one or more traumatic events (68.1% low betrayal trauma [LB; e.g., natural disasters]; 47.8% high betrayal trauma [HB; e.g., sexual/physical abuse]); 45.3% reported experiencing neglect or household dysfunction In the full sample women reported greater exposure to HB traumas (M = 1.86, SD = 2.56) than men (M = 1.48, SD = 2.61), t(811) = 2.12, p < .05. Men reported greater exposure to LB traumas (M = 2.70, SD = 3.18) than women (M = 2.05, SD = 2.57), t(811) = − 3.22, p < .01. Women reported more household dysfunction exposure (M = 1.19 SD = 1.56) than men (M = 0.88, SD = 1.38), t(780) = 2.88,p < .01. In the full sample = 2.57), t(811) = − 3.22, p < .01. Women reported more household dysfunction exposure (M = 1.19 SD = 1.56) than men (M = 0.88, SD = 1.38), t(780) = 2.88,p < .01. In the full sample M = 2.57), t(811) = − 3.22, p < .01. Women reported more household dysfunction exposure (M = 1.19 SD = 1.56) than men (M = 0. SD = 1.38), t(780) = 2.88, p < .01. In the full sample HB trauma and neglect/household dysfunction were the greatest predictors of symptom outcomes whereas LB trauma exposure significantly predicted PTSD and dissociative symptoms Native Hawaiians experienced significantly more trauma exposure and related symptoms (dissociation, depression, and anxiety symptoms, sleep problems) than high status groups, and reported higher levels of exposure to high betrayal trauma than other ethnic groups |
| (Koss et al., 2003) |
Native American N = 1660 in 7 tribes 41% Male Mage = 40.5 59% Female Mage = 39.5 United States |
Quantitative Logistic regression |
Physical Abuse Sexual Abuse Emotional Abuse Physical Neglect Emotional Neglect Parental Alcohol Use Out-of-home placement |
86% of participants reported experiencing at least one ACE. More than half of participants reported having a parent with alcohol problems. Physical neglect (men: 45%; women: 43%) and physical abuse (men: 40%; women: 42%) most prevalent Single exposures to physical (men OR: 1.47, CI: 1.02–2.11; women OR: 2.02, CI: 1.43–2.86) and/or sexual abuse (men OR: 1.46, CI: 0.98–2.18; women OR: 2.40, CI: 1.68–3.43; combined: men OR:1.58, CI: 1.10–2.27; women OR: 2.31, CI: 1.60–3.35), emotional abuse (men OR: 1.33, CI: 0.88–1.99; women OR: 2.08, CI: 1.47–2.94) emotional neglect (women OR: 2.16, CI: 1.49–3.13), and parental alcoholism (men OR: 2.14, CI: 1.45–3.15; women OR: 2.51, CI: 1.62–3.89) increased risk of alcohol dependence. Multiple exposures to combined physical and sexual abuse for men (men OR: 1.58, CI: 1.10–2.27) and sexual abuse (women OR: 1.79, CI: 1.21–2.66) and boarding school attendance (women OR: 1.57, CI: 1.03–2.40) for women increased risk of alcohol dependence For women there was a linear increase between alcohol dependence and number of ACEs; for men, the relationship was concave, with the most significant effects noted at 3 ACE |
| (Libby et al., 2008) |
American Indian parents from 2 tribes (Southwest and Northern Plains) n = 2221 Age: 15–54 years United States |
Quantitative Correlation and Regression Models |
Physical Abuse Sexual Abuse Witness IPV |
Childhood physical abuse was more prevalent than childhood sexual abuse, and childhood sexual abuse was more prevalent in women. Substance use disorders were more prevalent for males than females Childhood physical abuse and witnessing IPV decreased parenting satisfaction and increased parenting role impairment, however, perceived social support increased parenting satisfaction. Tribal differences in the prevalence and influence of childhood abuse on parenting outcomes. Substance use mediated the relationship between parenting outcomes and childhood abuse (Stats for above, if necessary) Lifetime substance use fully mediated the relationship between parenting role impairment and (A) childhood physical abuse in Northern Plains tribes (with mediator OR: 1.56, p = .131; without mediator OR: 1.85, p = .033) and (B) sexual abuse in Southwest tribes (with mediator OR: 3.56, p = .014; without mediator OR: 4.51, p = .004) |
| (Moon et al., 2018) |
N = 735 American Indian: n = 233 Mage = 60.69 Non-American Indian: n = 502 South Dakota, United States |
Cross-sectional T test Chi square Correlation Regression |
All ten ACEs | AI individuals had higher ACE scores (M = 2.58), lower incomes, lower self-perceived physical health, (t(728) = -3.10; p = .002), more negative previous experience related to mental health service use (t (733) = 25.601, p < .000), a lesser knowledge of depression (t (629) = − 2.30, p = .022), and less frequent mental health service use than Caucasian participants. Further, for AI participants higher ACE scores, higher levels of depressive symptoms, younger age, and better perceived physical health were significantly associated with more frequent use of mental health services |
| (Moon et al., 2015) |
American Indian: n = 182 Caucasian adults: n = 167 55% Female Age: 50 years + South Dakota, United States |
Cross-sectional T test Chi square Correlation OLS regression |
All ten ACEs | American Indians (AI) reported more ACEs (M = 2.73; t (300) = -5.892, p < .00), more chronic diseases and conditions (t(347) = − 2.357, p = .012), greater prevalence of obesity, lower self-perceived physical health, and lower alcohol intake (t (347) = 3.666, p < .000) than Caucasian participants |
| (Remigio-Baker et al., 2017) |
Women N = 3354 Hawaii Data from 2010 Hawaiian Behavioral Risk Factor Surveillance System Survey |
Survey data T-test, chi square Poisson regression |
Physical Abuse Sexual Abuse Emotional Abuse Witness to IPV Family Substance Use Family Incarcerated Family with Mental Illness |
More than half (52.5%) of participants reported one or more ACEs, 41.6% of participants reported ACEs associated with household dysfunction. Greater number of ACEs associated with greater prevalence of smoking (Prevalence rate [PR] = 1.40 [1 ACE]; to PR = 2.55 [5 + ACEs]) and obesity (PR = 1.00 [1 ACE] to PR = 1.85 [5 + ACEs]). Physical and verbal abuse, as well as household dysfunction predicted likelihood of smoking, whereas household dysfunction, physical, verbal, and sexual abuse were significantly associated with obesity in adulthood |
| (Roh et al., 2015) |
American Indian N = 233 Age: 50 years + |
Cross-sectional Survey Correlation, Hierarchical multivariate regression |
All ten ACEs | The mean ACE prevalence was 2.6; 5.6% of respondents reported one or more ACEs and 31.8% reported exposure to four or more ACEs. Depressive symptoms were positively associated with childhood abuse (β = .24, p < .001), childhood neglect (β = .33, p < .001), and childhood household dysfunction (β = .29, p < .001). Negative relationship between depressive symptoms and: (A) living alone (β = .36, p < .05); and (B) social support (β = .35, p < .001) |
| (Roh et al., 2019) |
American Indian/Alaska Native women cancer survivors N = 73 |
Cross sectional Hierarchical regression |
All ten ACEs | Mean ACE score = 2.5; ACEs were not significantly associated with depressive symptoms. However, psychological resilience was positively correlated with social support (r = 0.36, p ≤ .01) |
| (Twizeyemariya et al., 2017) | N = 1671 cohort of Indigenous infants (Australian) |
Descriptive Study Longitudinal |
Parent incarceration Physical Abuse Sexual Abuse Verbal Abuse Witness IPV Neglect Parent with problematic drinking Household with drug/alcohol problem Divorce/Separation Parental Distress Family conflict |
Psychological distress associated with high exposure rate to adversities. Only 4% of Indigenous children reported experiencing ≤ 1 adversity; 43% of children (6–10 years) had 6 or more risk factors for mental illness, and 23% were currently experiencing psychological distress. The majority of children (> 67%) were exposed to 3 or more stressful life events (e.g., incarceration, death of family member, lost job) Indigenous children in the 6- to 7-year-old cohort were more likely to: (A) witness IPV; (B) live in a household with a substance abuse problem; (C) experience poor physical health; (D) have 3 or more indicators of family financial stress than non-Indigenous Australian children |
| (Warne et al., 2017) |
American Indian: n = 516 Non-American Indian: n = 7078 Males: 42.5% Females: 57.47% |
Health Survey Chi square Regression |
All ten ACEs |
AI participants reported higher prevalence of household dysfunction, abuse, and neglect, as well as a higher total number of ACEs relative to the non-AI sample Having 6 or more ACEs for both samples associated with increased mental health concerns (e.g., PTSD, anxiety), alcohol use, and tobacco use. AI individuals had a significantly higher prevalence of PTSD (p < .01) than non-AI individuals |
| (Yuan et al., 2006) |
Native American: N = 1368 Females: n = 793 Males: n = 575 Data from Ten Tribes Study |
Survey Chi square Regression |
Parent Substance Use Physical Abuse Physical Neglect Sexual Abuse Emotional Abuse Emotional Neglect |
In women, having an alcoholic parent (OR = 1.65, 95% CI = 1.15–2.43), having an alcohol dependence diagnosis, and experiencing childhood physical and/or sexual abuse predicted physical assault likelihood. Emotional abuse (OR = 2.19, 95% CI = 1.35–3.55), as well as combined physical and sexual abuse (OR = 2.12, 95% CI = 1.36–3.12) predicted adult physical victimization in men |
Mental Health Difficulties
Prevalence of ACEs in Indigenous groups were associated with broader mental health concerns. Increased ACEs were associated with higher diagnoses of conduct disorder (Basu & Isaacs, 2019), post-traumatic stress disorder (Brockie et al., 2015; Klest et al., 2013; Warne et al., 2017), attention-deficit hyperactivity disorder (Fuller-Thomson & Lewis, 2015; Kenney & Singh, 2016), anxiety-related symptoms (Kenney & Singh, 2016; Warne et al., 2017), and depressive symptoms (Bombay et al., 2011; Brockie et al., 2015; Burnette et al., 2017; Kenney & Singh, 2016; Klest et al., 2013; Moon et al., 2018; Roh et al., 2015). Of note, one study (Roh et al., 2019) did not find a relationship between ACE scores and depressive symptoms. Studies found that some ACEs were associated with increased suicide attempts (Brockie et al., 2015; De Ravello et al., 2008; Hamdullahpur et al., 2018), previous treatment for psychological concerns (Hamdullahpur et al., 2018), and increased psychological distress (Twizeyemariya et al., 2017). Five studies found that ACEs were associated with increased substance use (Brockie et al., 2015; Koss et al., 2003; Libby et al., 2008; Remigio-Baker et al., 2017; Warne et al., 2017). Among these studies, one found that Native American women who experienced a single exposure to physical (OR = 2.02) and/or sexual abuse (OR = 2.40), emotional abuse (OR = 2.08), emotional neglect (OR = 2.16), and parental alcoholism (OR = 2.51) were roughly 2 times more likely to be at an increased risk for alcohol dependence (Koss et al., 2003). However, only some types of childhood exposures, but not all, were associated with alcohol dependence for men. Risk of alcohol dependence was greater among men who reported parental alcoholism, physical abuse, physical neglect, or combined physical and sexual abuse (Koss et al., 2003).
One study (Brockie et al., 2015) found no significant association between sexual abuse and symptoms of depression, post-traumatic stress disorder (PTSD), or suicide attempts. Further, Brockie et al. (2015) reported that emotional neglect was not significantly associated with PTSD symptoms, and that physical neglect was not significantly associated with poly-drug use. No significant associations were found between exposure to parental domestic violence and the prevalence of attention deficit hyperactivity disorder (ADHD) among men (Fuller-Thomson & Lewis, 2015). Burnette et al. (2017) reported that no significant racial differences existed for social support and depressive symptoms in a population of AI/AN older adults. Further, they reported that childhood neglect did not significantly predict depressive symptoms (Burnette et al., 2017).
Physical Health Difficulties
The prevalence of ACEs has been found to be associated with physical health difficulties (Brockie et al., 2018; Moon et al., 2018; Twizeyemariya et al., 2017; Warne et al., 2017). Among a sample of American Indian/Alaska Natives (AI/AN) with Type 2 Diabetes, ACEs were negatively associated with physical health after controlling for variables such as gender, age, and income (Brockie et al., 2018). For participants reporting lower ACEs and increased support (i.e., diabetes-specific support), self-reported physical health ratings were higher (better; Brockie et al., 2018). However, though physical health ratings were highest (better) for individuals reporting low ACE exposure, those in high social support contexts with high ACE exposure reported better physical health than those with low ACE scores and low support environments. Furthermore, Brockie et al. (2018) identified a negative relationship between household income and health status, whereby individuals with lower income reported worse physical health. Low income may be a consequence of managing chronic physical illnesses and/or mental health difficulties and may be a driver for increased difficulties with physical health (Brockie et al., 2018; Moon et al., 2018). Similarly, Moon et al. (2018) found that AI adults reported lower self-perceived physical health. ACE scores in AI participants, compared to non-AI participants, were associated with current cigarette smoking (35.2% AI, 15.1% non-AI; Warne et al., 2017). One study expanded the age range for adverse experiences to incorporate prenatal exposures and found that approximately 50% of Indigenous children were prenatally exposed to nicotine and 22% to alcohol (Twizeyemariya et al., 2017). Moreover, children were found to be 5.3 times more likely than a general Australian sample to have poor physical health (Twizeyemariya et al., 2017). The number of ACEs was positively associated with likelihood of being overweight or obese, with greater numbers of ACEs associated with increased rates of obesity (Remigio-Baker et al., 2017). No ACE type was associated with being overweight when considered in isolation, however women who experienced household dysfunction in addition to physical, verbal, and sexual abuse during childhood had significantly higher likelihood of being obese in adulthood (Remigio-Baker et al., 2017). This relationship did not differ by race/ethnicity.
A greater likelihood of physical victimization and assault later in life following exposure to ACEs was found in one study (Yuan et al., 2006). Namely, Yuan et al. (2006) found that Native American women who experienced specific ACEs (i.e., having a parent with substance use difficulties, childhood physical and/or sexual abuse) predicted a greater likelihood of physical assault as an adult. Additionally, Native American men who experienced ACEs such as emotional abuse and combined physical and sexual abuse predicted adult physical victimization in men (Yuan et al., 2006).
Protective Factors
Some studies examined possible protective factors that can reduce the impact of ACEs on both physical and mental health outcomes. For example, studies found that involvement in spiritual activities (Brockie et al., 2018) and having a sense of cultural identity and connectedness (Basu & Isaacs, 2019) were associated with positive mental health outcomes despite ACE experience. Two studies found that social support and psychological resilience may offer a promising mechanism to bolster resilience among AI and AN people as social support was negatively associated with depressive symptoms (Burnette et al., 2017; Roh et al., 2015, 2019). Furthermore, in AI and AN people who have cancer, perceived health was inversely related to depressive symptoms (Roh et al., 2019). Disparities among social determinants of health experienced by Indigenous people appear to contribute to increased ACE scores. A large scale study in the US obtained data from 23 states for eight ACEs, excluding physical and emotional neglect (Merrick et al., 2018). Those who were unemployed or not able to work had higher mean ACE scores (M = 2.30; M = 2.33) than those who were employed (M = 1.58). Comparable findings from Burnette et al. (2017) found that employment (β = −0.337, p ≤ 0.05) and adult social support (β = –0.030, p ≤ 0.01) were significantly associated with lower levels of depressive symptoms. Similarly, those with a higher education, such as being a college graduate, had been found to have a lower mean ACE scores than those with less than a high school degree (M = 1.23; M = 1.97; Merrick et al., 2018). This was also seen with school attendance, whereby those who did not attend school were more likely to report physical abuse (χ2 (1) = 6.7, p < 0.05), emotional neglect (χ2 (1) = 5.3, p < 0.05), and witnessing intimate partner violence (IPV) (χ2 (1) = 5.35, p < 0.05; Brockie et al., 2015).
Examination of Dose–Response Relationships
Six studies discovered a dose–response relationship among those who experience ACEs. For example, one study found separate patterns of dose–response relationships between Native American men and women. In their study, the pattern for men represented a concave curve whereby men who reported three different ACEs experienced a fourfold increased risk of alcohol dependence whereas men with four or more different ACEs had a threefold increased risk (Koss et al., 2003). For women, the pattern was linear whereby those who reported three ACEs had a fivefold increased risk and those with four ACEs had a sevenfold increased risk for alcohol dependence (Koss et al., 2003). Odds ratios provided in each study were calculated based on the number of ACEs included. Because not all studies included all 10 ACEs, it is challenging to make comparisons across studies when examining prevalence rates and inferential dose–response relationships in models that use different ACE scores.
Participants1
Most retrieved studies examined ACEs data relevant to Native American populations residing in the United States of America (n = 15). Meanwhile, three studies described Aboriginal populations in Canada, two in Australia, and one included data from an Inuit population living in Greenland. Specific subpopulations included in these studies included people living with Type 2 Diabetes, (Brockie et al., 2018), people who were incarcerated (De Ravello et al., 2008), and cancer survivors (Roh et al., 2019).
Seven studies (Basu & Isaacs, 2019; Burnette et al., 2017; Hamdullahpur et al., 2018; Kenney & Singh, 2016; Klest et al., 2013; Moon et al., 2015; Warne et al., 2017) compared data from Indigenous to non-Indigenous populations. Among these studies, some found higher ACE scores in Indigenous population groups. For example, Burnette et al. (2017) found that the mean ACE score for Indigenous participants was 2.55 while it was 0.83 for non-Indigenous participants. One study found that AI children were 2 to 3 times more likely to have multiple ACEs than non-Indigenous children (Kenney & Singh, 2016). When Aboriginal and non-Aboriginal women reported similar rates of childhood sexual abuse, both groups were likely to experience other ACEs (Hamdullahpur et al., 2018). This may indicate that detrimental health outcomes are similar across ACE exposures, regardless of population group. Rates of ACEs may be higher in some populations due to higher risks of exposure. For example, AI children were more likely to have a parent incarcerated, witness and/or be a victim to violence, and live with an individual abusing substances compared to non-Indigenous children (Kenney & Singh, 2016). Similarly, Aboriginal Australian children had a higher risk of child welfare intervention compared to non-Aboriginal children (Basu & Isaacs, 2019). Continuous discrepancies in these types of rates may influence current ACE prevalence within Indigenous populations.
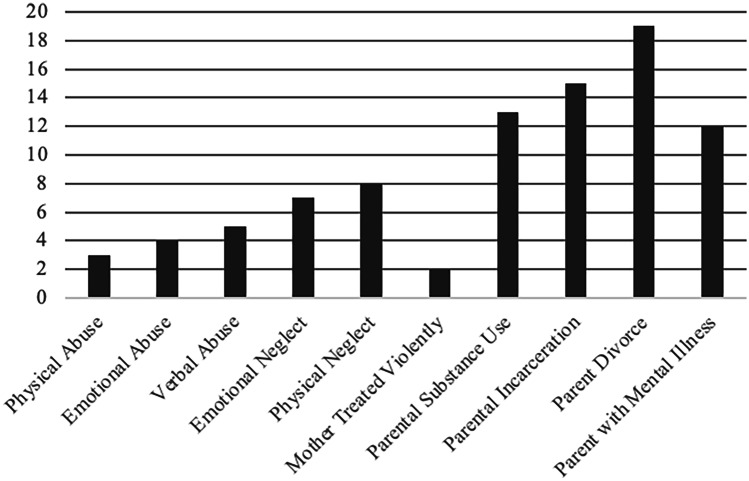
Reporting of ACEs Across Studies
Most studies (n = 8) included all 10 ACEs, while four studies included eight ACEs. Three studies included six ACEs, two studies included four ACEs, and three studies included only three ACEs. The most commonly included ACE among the included studies was sexual abuse during childhood (n = 20), with physical abuse during childhood included in 19 of these studies (see Fig. 2). The ACEs that were included less were related to divorce or parental separation (n = 10). Additional adverse experiences included in these studies at a lesser extent include: parental distress, family conflict, and out of home placement (one study for each of these variables). In studies that examined nine to 10 ACEs (Brockie et al., 2018; Burnette et al., 2017; Moon et al., 2015, 2018; Roh et al., 2015, 2019), the mean number of ACE scores ranged from 2.5 to 3.05 (the mean ACE score 3.05 was calculated based on people living with Type 2 Diabetes). For comparison, a large-scale general American population reported the mean ACE score as 1.36 (Centers for Disease Control and Prevention & Kaiser, 2016).
Fig. 2.
Number of Retrieved Studies that Examined each ACE
Classification of ACEs varied within studies, particularly for ACEs that pertained to household dysfunction. Many studies varied in the way these variables were reported as well. Some studies specified dysfunction present in the household by any family member, while others focused specifically on parent experiences of these events. This type of classification may decrease prevalence rates and make it challenging to compare ACEs across studies.
Discussion
The goal of this review was to synthesize relevant ACE research in Indigenous populations in North America. Due to the lack of literature with Canadian Indigenous populations, the review was broadened to encompass other countries’ Indigenous populations. Of the 21 studies included in this review, all described relationships between ACEs and mental or physical health outcomes for such populations. The mean number of ACE scores for non-clinical sample Indigenous populations ranged from 2.5 to 3.05, higher than a large-sample population ACE mean of 1.36 collected from 2011 to 2014 in 23 American States (Merrick et al., 2018). In Canada, large population-based ACE data, such as the Ontario Health Survey, has typically excluded Indigenous people living on reserve, and has not described all ACEs, making it not feasible to compare prevalence rates (Chartier et al., 2010). Although the majority of studies found associations between ACEs and adverse health outcomes, few studies found that particular ACEs were not associated with negative physical or mental health outcomes. This may be due to the significant variation in the conceptualization and definition of ACEs among studies.
Much of literature dedicated to Indigenous mental health does not typically incorporate ACE models, despite novel dose–response relationships described in the retrieved studies. A scoping review of mental health articles with Indigenous people in Canada (Nelson & Wilson, 2017), identified that of over 200 articles retrieved, the majority of articles related to either social determinants of Indigenous health (36% of all articles) or mental health services (30%) within communities. Secondary themes of the retrieved articles were prevalence of mental illness, mental health promotion, and mental health research approaches. Nelson and Wilson (2017) noted that papers frequently referenced the maladaptive effect of colonialism on Indigenous mental health, through detrimental governmental practices and child welfare policies, a past history of residential schooling, and ongoing funding disparities. Many papers described the intergenerational transmission of these effects on current generations of Indigenous peoples, but do not describe a causal mechanism of transmission of current health concerns.
A developmental model of early childhood trauma, such as the ACE framework, may extend such frequently cited relationships to quantifiable and measurable predictors of Indigenous mental health. Disruption of typical developmental milestones can fundamentally change both structure and function in brain regions such as the amygdala, hippocampus, and medial prefrontal cortex, which in turn, can affect one’s ability to accurately assess and respond to stressors. Research has indicated that experiencing ACEs in a dose-dependent manner is associated with blunted cortisol reactivity, dysregulation of the hypothalamic-pituitary adrenal (HPA) axis, and epigenetic alterations of the glucocorticoid receptor in the hippocampus (Dymov et al., 2009; Voellmin et al., 2014; Walsh et al., 2019). The consequence of such alterations in stress reactivity could compromise psychological well-being resulting in depression, substance use disorders, and physical health resulting in obesity, fibromyalgia, and chronic pain syndromes (Voellmin et al., 2014). For example, children in New Zealand who were exposed to ACEs demonstrated difficulty with executive functions and cognitive performance (Walsh et al., 2019).
By accurately understanding specific relationships between predictors of mental health and subsequent outcomes, it is possible to better improve both preventative, primary, and tertiary interventions related to Indigenous mental health. The ACE model, although useful, is likely not entirely explanatory of all health outcomes, however such limitations have yet to be explored. Well described dose–response relationships may not account for various distal or contextual factors within Indigenous communities, and such relationships may not accurately represent the role of social determinants of health as moderating or mediating variables within these cumulative health concerns. Indeed, the breadth of historic and contemporary variables that influence health and mental health of Indigenous communities at the population-level (i.e., Reading & Wien, 2009) create a complex array of independent and dependent variables at the individual-level. Thoughtful consideration of how social determinants of health manifest and influence broad systems of health is required to accurately recognize and respond to ACEs within Indigenous communities.
Additionally, these types of developmental frameworks can be situated within existing models of Indigenous well-being, such as the First Nations Mental Wellness Continuum Framework (FNMWCF; Assembly of First Nations & Health Canada, 2015). Specific components of these models have aligned with other indicators of Indigenous well-being, such as the medicine wheel, which promotes a balance between physical, emotional, mental, and spiritual well-being (King et al., 2009). Use of indicators that align best with Indigenous well-being may better contextualize relationships between health and ACEs to potentially generate more useful early-childhood interventions. For example, the FNMWCF situates increased individual hope, belonging, meaning, and purpose facilitates increased well-being. It is conceptualized that such constructs are culturally-embedded protective factors that could offset detrimental health effects of ACEs and contribute to healing, though such relationships have yet to be explored.
When models robustly explain relationships of health disparities experienced within Indigenous communities, prevention and treatment of health may be improved. Literature describing ACEs specific to Indigenous health outcomes is relatively new, with the earliest study retrieved in this review published in 2006. Although these relationships may be newly conceptualized, potential pathways for treatment of individual ACEs are well-established, particularly those related to trauma, depression, and anxiety. Such gold-standard interventions may require modification to meet the complexity of need within some Indigenous communities, but may be a useful initial approach dependent on community need. Any research or treatment process must reflect approaches requested and approved by communities, and address the explicit needs within each region. The usefulness of cultural approaches for both prevention and treatment of health concerns could be examined in relation to ACE relationships. Few studies in this review examined the use of culture as a protective factor, however did note that when ACE scores were higher, individuals were less likely to engage in culture. Examination of ACEs within Indigenous communities is a viable endeavor, and can inform existing health approaches to potentially generate novel, culturally-relevant treatment and prevention strategies.
Study Limitations and Future Research Directions
This review included various Indigenous populations across various countries when amalgamating study outcomes, however experiences of specific groups of Indigenous people are specific to reserve and region. Although many Indigenous peoples have shared experiences (e.g., colonization, assimilation, intergenerational trauma), consolidation of Indigenous-specific literature must also recognize the cultural heterogeneity among the many distinct Indigenous groups. Due to the lack of research in this area, this review was tailored to be broad in order to capture existing literature on Indigenous populations globally. Initially, many articles were identified for the review and while they discussed adversity in Indigenous populations, the results did not capture prevalence and/or physical or mental health outcomes in relation to ACEs. Therefore, this review may not be generalizable to all Indigenous groups and future research may focus on understanding the prevalence of ACEs in Indigenous populations across regions. Many studies included in the review focused on mental health outcomes while only a minority of studies reported on physical health outcomes. As Indigenous populations have been found to experience poorer physical health and greater physical illnesses, future research may focus on the consequences ACEs may have on physical health for this population. As this review included information using keywords related to adverse childhood experiences, additional literature may exist that describes other outcomes related to individual ACE variables. Further review of how each of these variables affect health outcomes may provide a broader analysis of ACEs within Indigenous populations. Such a review may potentially synthesize literature not currently classified as ACE-specific but are not currently classified as such in the literature. Ongoing ACE research could be broadened to focus on specific Indigenous populations and contexts, including on-reserve/off reserve populations, Métis, and Inuit populations, and can specifically incorporate ACEs that may be increasingly pertinent to Indigenous populations, such as residential school attendance or frequent involvement with child welfare services.
It may be worthwhile to expand ACE research to incorporate additional aspects of health and well-being that are particularly relevant for some Indigenous communities. For example, studies endorsed that engagement in spiritual or cultural activities can be a protective factor against mental or physical health challenges, yet none of the retrieved studies examined the influence of ACEs on such practices. Additionally, given the range of how ACEs were reported across studies, future research may explore how to best capture ACE data in a way that can facilitate sharing of such information across communities (if such goals are aligned with community needs and Ownership, Control, Access, and Possession™ [OCAP] principles; First Nations Information Governance Centre, 2014). Similar to reporting standards for Cochrane Reviews or PRISMA, standardization of reporting these types of ACE relationships may facilitate better knowledge translation. For studies with smaller participant samples, standardized reporting may facilitate comparison across studies, particularly for those completed in similar regions.
Conclusion
Research examining ACEs within Indigenous populations has the potential to clarify existing dose–response relationships between early traumatic experiences and current health disparities experienced in some communities. Further examination of these relationships can begin to inform community-based best practices for both diagnosis and treatment of health concerns, and provide contextualization of current disease prevalence rates. Prioritizing the incorporation of existing cultural and two-eyed seeing approaches to ongoing ACE prevention and treatment efforts will be essential to reducing the effects of ACEs across a lifespan.
Declarations
Conflict of Interest
The authors do not have any real or potential conflicts of interest to declare. Christopher J. Mushquash’s participation in this project is partially supported by the Canada Research Chairs Program.
Footnotes
Specific terminology used to describe Indigenous groups used in retrieved studies include: Aboriginal, Alaskan Native, American Indian, Australian Aboriginal, First Nations, Inuit, Native American, and Native Hawaiian.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Adelson N. The Embodiment of Inequity: Health Disparities in Aboriginal Canada. Canadian Journal of Public Health. 2005;96(S2):S45–S61. doi: 10.1007/BF03403702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Assembly of First Nations & Health Canada. (2015). First Nations Mental Wellness Continuum Framework. http://health.afn.ca/uploads/files/24-14-1273-fn-mental-wellness-frameworken05_low.pdf
- Basu S, Isaacs AN. Profile of transcultural patients in a regional Child and Adolescent Mental Health Service in Gippsland, Australia: The need for a multidimensional understanding of the complexities. International Journal of Social Psychiatry. 2019;65(3):217–224. doi: 10.1177/0020764019835264. [DOI] [PubMed] [Google Scholar]
- Bjerregaard P, Larsen CVL. Three lifestyle-related issues of major significance for public health among the Inuit in contemporary Greenland: A review of adverse childhood conditions, obesity, and smoking in a period of social transition. Public Health Reviews. 2018;39(1):5. doi: 10.1186/s40985-018-0085-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bombay, A., Matheson, K., & Anisman, H. (2008). The Impact of Stressors on Second Generation Indian Residential School Survivors. Poster presented at the annual meeting of the National Network for Aboriginal Mental Health Research, Montreal, Quebec.
- Bombay A, Matheson K, Anisman H. Intergenerational trauma: Convergence of multiple processes among First Nations peoples in Canada. International Journal of Indigenous Health. 2009;5(3):6–47. doi: 10.3138/ijih.v5i3.28987. [DOI] [Google Scholar]
- Bombay A, Matheson K, Anisman H. The impact of stressors on second generation Indian residential school survivors. Transcultural Psychiatry. 2011;48(4):367–391. doi: 10.1177/1363461511410240. [DOI] [PubMed] [Google Scholar]
- Brockie TN, Dana-Sacco G, Wallen GR, Wilcox HC, Campbell JC. The Relationship of Adverse Childhood Experiences to PTSD, Depression, Poly-Drug Use and Suicide Attempt in Reservation-Based Native American Adolescents and Young Adults. American Journal of Community Psychology. 2015;55(3–4):411–421. doi: 10.1007/s10464-015-9721-3. [DOI] [PubMed] [Google Scholar]
- Brockie TN, Elm JHL, Walls ML. Examining protective and buffering associations between sociocultural factors and adverse childhood experiences among American Indian adults with type 2 diabetes: A quantitative, community-based participatory research approach. British Medical Journal Open. 2018;8(9):e022265. doi: 10.1136/bmjopen-2018-022265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burnette CE, Roh S, Lee KH, Lee YS, Newland LA, Jun JS. A comparison of risk and protective factors related to depressive symptoms among American Indian and Caucasian older adults. Health and Social Work. 2017;42(1):e15–e23. doi: 10.1093/hsw/hlw055. [DOI] [PubMed] [Google Scholar]
- Canadian Public Health Association. (2019). What are the social determinants of health? https://www.cpha.ca/what-are-social-determinants-health
- Centres for Disease Control and Prevention, & Kaiser, P. (2016). The ACE Study Survey Data. Atlanta, Georgia: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention.
- Chartier MJ, Walker JR, Naimark B. Separate and cumulative effects of adverse childhood experiences in predicting adult health and health care utilization. Child Abuse & Neglect. 2010;34(6):454–464. doi: 10.3402/ejpt.v5.24585. [DOI] [PubMed] [Google Scholar]
- De Ravello L, Abeita J, Brown P. Breaking the cycle/mending the hoop: Adverse childhood experiences among incarcerated American Indian/Alaska native women in New Mexico. Health Care for Women International. 2008;29(3):300–315. doi: 10.1080/07399330701738366. [DOI] [PubMed] [Google Scholar]
- Dube S. Twenty years and counting: The past, present, and future of ACE research. In: Asmundson GJ, Afifi TO, editors. Adverse Childhood Experiences: Using Evidence to Advance Research, Practice, Policy, and Prevention. Academic Press; 2019. pp. 3–14. [Google Scholar]
- Dymov S, Sasaki A, D’Alessio A, Labonté B, Turecki G, Meaney M, McGowan P, Szyf M. Epigenetic regulation of the glucocorticoid receptor in human brain associates with childhood abuse. Nature Neuroscience. 2009;12(3):342–348. doi: 10.1038/nn.2270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Marks JS. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine. 1998;14(4):245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- First Nations Centre . First Nations Regional Longitudinal Health Survey (RHS) 2002/03: Results for Adults, Youth, and Children Living in First Nations Communities. First Nations Centre; 2005. [Google Scholar]
- First Nations Information Governance Centre. (2014, May). Ownership, Control, Access and Possession (OCAP™): The Path to First Nations Information Governance. Ottawa: The First Nations Information Governance Centre.
- Fuller‐Thomson, E., Baird, S. L., Dhrodia, R., & Brennenstuhl, S. (2016). The association between adverse childhood experiences (ACEs) and suicide attempts in a population‐based study. Child: Care, Health and Development, 42(5), 725–734. 10.1111/cch.1235 [DOI] [PubMed]
- Fuller-Thomson E, Lewis DA. The relationship between early adversities and attention-deficit/hyperactivity disorder. Child Abuse & Neglect. 2015;47:94–101. doi: 10.1016/j.chiabu.2015.03.005. [DOI] [PubMed] [Google Scholar]
- Gracey M, King M. Indigenous health part 1: Determinants and disease patterns. Lancet. 2009;374(9683):65–75. doi: 10.1016/S0140-6736(09)60914-4. [DOI] [PubMed] [Google Scholar]
- Hackett C, Feeny D, Tompa E. Canada’s residential school system: Measuring the intergenerational impact of familial attendance on health and mental health outcomes. Journal of Epidemiology and Community Health. 2016;70(11):1096–1105. doi: 10.1136/jech-2016-207380. [DOI] [PubMed] [Google Scholar]
- Hamdullahpur K, Jacobs KJ, Gill KJ. Mental Health Among Help-Seeking Urban Women: The Relationships Between Adverse Childhood Experiences, Sexual Abuse, and Suicidality. Violence against Women. 2018;24(16):1967–1981. doi: 10.1177/1077801218761602. [DOI] [PubMed] [Google Scholar]
- Kenney MK, Singh GK. Adverse Childhood Experiences among American Indian/Alaska Native Children: The 2011–2012 National Survey of Children’s Health. Scientifica. 2016;2016:1–14. doi: 10.1155/2016/7424239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King M, Smith A, Gracey M. Indigenous health part 2: The underlying causes of the health gap. The Lancet (british Edition) 2009;374(9683):76–85. doi: 10.1016/S0140-6736(09)60827-8. [DOI] [PubMed] [Google Scholar]
- Klest B, Freyd JJ, Foynes MM. Trauma exposure and posttraumatic symptoms in Hawaii: Gender, ethnicity, and social context. Psychological Trauma: Theory, Research, Practice, and Policy. 2013;5(5):409–416. doi: 10.1037/a0029336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koss MP, Yuan NP, Dightman D, Prince RJ, Polacca M, Sanderson B, Goldman D. Adverse childhood exposures and alcohol dependence among seven Native American tribes. American Journal of Preventive Medicine. 2003;25(3):238–244. doi: 10.1016/S0749-3797(03)00195-8. [DOI] [PubMed] [Google Scholar]
- Kumar, M. B., & Tjepkema, M. (2019). Suicide among First Nations people, Métis and Inuit (2011–2016): Findings from the 2011 Canadian Census Health and Environment Cohort (CanCHEC). Catalogue no. 99–011-X2019001. https://www150.statcan.gc.ca/n1/en/pub/99-011-x/99-011-x2019001-eng.pdf?st=VFU5JqBO
- Libby A, Orton H, Beals J, Buchwald D, Manson S. Childhood abuse and later parenting outcomes in two American Indian tribes. Child Abuse & Neglect. 2008;32:195–211. doi: 10.1016/j.chiabu.2007.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merrick MT, Ford DC, Ports KA, Guinn AS. Prevalence of adverse childhood experiences from the 2011–2014 Behavioral Risk Factor Surveillance System in 23 states. JAMA Pediatrics. 2018;172(11):1038–1044. doi: 10.1001/jamapediatrics.2018.2537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moon H, Lee YS, Roh S, Burnette CE. Factors Associated with American Indian Mental Health Service Use in Comparison with White Older Adults. Journal of Racial and Ethnic Health Disparities. 2018;5(4):847–859. doi: 10.1007/s40615-017-0430-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moon H, Roh S, Lee YS, Turner Goins R. Disparities in health, health care access, and life experience between American Indian and white adults in South Dakota. Journal of Racial and Ethnic Health Disparities. 2015;3(2):301–308. doi: 10.1007/s40615-015-0146-3. [DOI] [PubMed] [Google Scholar]
- Nelson SE, Wilson K. The mental health of Indigenous peoples in Canada: A critical review of research. Social Science & Medicine. 2017;176:93–112. doi: 10.1016/j.socscimed.2017.01.021. [DOI] [PubMed] [Google Scholar]
- Reading, C.L. & Wien, F. (2009). Health Inequalities and Social Determinants of Aboriginal Peoples’ Health. Prince George, BC: National Collaborating Centre for Aboriginal Health. https://www.nccah-ccnsa.ca/docs/social%20determinates/nccah-loppie-wien_report.pdf
- Remigio-Baker, R. A., Hayes, D. K., & Reyes-Salvail, F. (2017). The Relationship of Adverse Childhood Events to Smoking, Overweight, Obesity and Binge Drinking Among Women in Hawaii. Maternal and Child Health Journal; New York, 21(2), 315–325. 10.1007/s10995-016-2116-8 [DOI] [PMC free article] [PubMed]
- Roh S, Burnette CE, Lee YS, Giger JT, Goins RT, Petereit DG, Lee KH. Identifying risk and protective factors related to depressive symptoms among Northern Plains American Indian women cancer survivors. Women and Health. 2019;59(6):646–659. doi: 10.1080/03630242.2018.1544965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roh S, Burnette CE, Lee KH, Lee Y-S, Easton SD, Lawler MJ. Risk and protective factors for depressive symptoms among American Indian older adults: Adverse childhood experiences and social support. Aging & Mental Health. 2015;19(4):371–380. doi: 10.1080/13607863.2014.938603. [DOI] [PubMed] [Google Scholar]
- RHS National Team . First Nations Regional Longitudinal Health Survey (RHS) 2002/03: Results for Adults, Youth, and Children Living in First Nations Communities, Revised. 2. Assembly of First Nations/First Nations Information Governance Committee; 2007. [Google Scholar]
- Ross A, Dion J, Cantinotti M, Collin-Vézina D, Paquette L. Impact of residential schooling and of child abuse on substance use problem in Indigenous Peoples. Addictive Behaviors. 2015;51:184–192. doi: 10.1016/j.addbeh.2015.07.014. [DOI] [PubMed] [Google Scholar]
- Statistics Canada. (2017a). Aboriginal peoples in Canada: Key results from the 2016 Census. The Daily. https://www150.statcan.gc.ca/n1/daily-quotidien/171025/dq171025a-eng.htm
- Statistics Canada. (2017b). The housing conditions of Aboriginal people in Canada. Catalogue no. 99–200-X. https://www12.statcan.gc.ca/census-recensement/2016/as-sa/98–200-x/2016021/98–200-x2016021-eng.cfm
- Statistics Canada. (2018). First Nations People, Métis, and Inuit in Canada: Diverse and growing populations. Catalogue no. 89–659-X. https://www150.statcan.gc.ca/n1/pub/89-659-x/89-659-x2018001-eng.htm
- Truth and Reconciliation Commission of Canada [TRCC]. (2015). Truth and Reconciliation Commission of Canada: Calls to Action. Winnipeg, MB: Author. http://trc.ca/assets/pdf/Calls_to_Action_English2.pdf
- Twizeyemariya A, Guy S, Furber G, Segal L. Risks for Mental Illness in Indigenous Australian Children: A Descriptive Study Demonstrating High Levels of Vulnerability. Milbank Quarterly. 2017;95(2):319–357. doi: 10.1111/1468-0009.12263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voellmin A, Winzeler K, Hug E, Wilhelm F, Schaefer V, Gaab J, La Marca R, Pruessner J, Bader K. Blunted endocrine and cardiovascular reactivity in young healthy women reporting a history of childhood adversity. Psychoneuroendocrinology. 2014;51:58–67. doi: 10.1016/j.psyneuen.2014.09.008. [DOI] [PubMed] [Google Scholar]
- Walsh, M. C., Joyce, S., Maloney, T., Vaithianathan R. (2019). Adverse childhood experiences and school readiness outcomes: Results from the Growing up in New Zealand study. Ministry of Social Development. Retrieved from https://www.msd.govt.nz/documents/about-msd-and-our-work/publications-resources/research/children-and-families-research-fund/children-and-families-research-fund-report-adverse-childhood-experiences-and-school-readiness-outcomes-april-2019-final.pdf [PubMed]
- Warne D, Dulacki K, Spurlock M, Meath T, Davis MM, Wright B, McConnell KJ. Adverse childhood experiences (ACE) among American Indians in South Dakota and associations with mental health conditions, alcohol use, and smoking. Journal of Health Care for the Poor and Underserved. 2017;28(4):1559–1577. doi: 10.1353/hpu.2017.0133. [DOI] [PubMed] [Google Scholar]
- Yuan NP, Koss MP, Polacca M, Goldman D. Risk factors for physical assault and rape among six Native American tribes. Journal of Interpersonal Violence. 2006;21(12):1566–1590. doi: 10.1177/0886260506294239. [DOI] [PubMed] [Google Scholar]