Abstract
Background
Inhaled corticosteroids (ICS) are commonly used to treat COPD and are associated with increased risk of pneumonia. The aim of this study was to assess if accumulated use of ICS is associated with a dose-dependent risk of a positive airway culture with Pseudomonas aeruginosa in patients with COPD.
Methods
We conducted a multiregional epidemiological cohort study including Danish COPD patients followed in outpatient clinics during 2010–2017. ICS use was categorised based on accumulated prescriptions redeemed 365 days prior to cohort entry. Cox proportional hazard regression model was used to estimate the risk of acquiring P. aeruginosa. Propensity score matched models were used as sensitivity analyses.
Results
A total of 21 408 patients were included in the study, of which 763 (3.6%) acquired P. aeruginosa during follow-up. ICS use was associated with a dose-dependent risk of P. aeruginosa (low ICS dose: HR 1.38, 95% CI 1.03 to 1.84, p=0.03; moderate ICS dose: HR 2.16, 95% CI 1.63 to 2.85, p<0.0001; high ICS dose: HR 3.58, 95% CI 2.75 to 4.65, p<0.0001; reference: no ICS use). A propensity matched model confirmed the results (high ICS dose compared with no/low/moderate ICS dose: HR 2.05, 95% CI 1.76 to 2.39, p p<0.0001).
Conclusion
Use of ICS in patients with COPD followed in Danish outpatient clinics was associated with a substantially increased and dose-dependent risk of acquiring P. aeruginosa. Caution should be taken when administering high doses of ICS in severely ill patients with COPD. These results should be confirmed in comparable cohorts and other settings.
Keywords: respiratory infection, COPD epidemiology
Key messages.
What is the key question?
Do inhaled corticosteroids (ICS) increase the risk of acquiring Pseudomonas aeruginosa in patients with COPD?
What is the bottom line?
Use of inhaled corticosteroids is associated with a significant and dose-related risk of acquiring P. aeruginosa in patients with COPD.
Why read on?
This is the first study to assess the risk of acquiring a positive airway culture with P. aeruginosa after use of ICS in a large and well-characterised population of patients with COPD.
Introduction
Inhaled corticosteroids (ICS) are commonly used as pharmacological treatment in patients with COPD and are currently recommended to reduce the risk of recurrent exacerbations in patients with severe disease.1–3 However, ICS appear to have minimal or no impact on lung function and may not be needed or effective in patients with mild to moderate COPD and in those without eosinophilic inflammation.4 5 Furthermore, their usefulness is currently being debated due to potential side effects with increased risk of pneumonia and mycobacterial infections.6–9 Concordantly, evidence suggests that the risk of infection is dose related10 11 and highest among patients with more severe airflow obstruction.12
Previous observational studies have shown that presence of positive airway culture with Pseudomonas aeruginosa in patients with COPD is associated with severe disease, frequent hospitalisations and death.13–16 Thus, this subgroup of patients with COPD might be extra susceptible to the possible harmful effects of pharmacotherapy with ICS.
Few data are available on ICS as a risk factor for P. aeruginosa. Smaller prospective studies investigating patients admitted to hospital with an exacerbation of COPD have found that P. aeruginosa was associated with prior systemic corticosteroid treatment and use of antibiotics.17 18 So far, no studies have specifically investigated the potential association between use of ICS and risk of P. aeruginosa in patients with COPD. Thus, we conducted a large cohort study to explore the risk of P. aeruginosa in patients with COPD related to the accumulated dose of ICS given during the last twelve months prior to their first outpatient clinic visit.
Methods
Data sources
For this study, the authors were granted access to data in nationwide and regional administrative registries in accordance with current Danish laws (Data Protection Agency: 2012-58-0004; The Danish National Committee on Health Research Ethics: H-15010949). According to these laws, informed consent is not required for registry-based studies. The linkage between registries was done by using unique personal identification numbers, which allows an exact linkage on patient level and ensures complete follow-up.19
The following registries was used:
The Danish Register of COPD (DrCOPD) was used to identify patients with COPD. DrCOPD is a nationwide register that holds individual patient data on demographics and all outpatient visits and hospital admissions due to exacerbation of COPD, in patients aged 30 years or above, at all hospital-based pulmonary clinics since 2010.20
The Danish National Patient Registry holds data on all hospital admissions since 1977 and all hospital outpatient visits since 1995 and was used to characterise comorbidities in the study population.21
The Danish National Database of Reimbursed Prescriptions (DNDRP) was used to identify prescribed and redeemed medication, including the exposure to ICS. The DNDRP is nationwide and includes data on all reimbursed prescriptions redeemed at Danish community and hospital-based outpatient pharmacies since 2004.22
Microbiological data from the Clinical Microbiology Departments in Eastern Denmark (Region Zealand and Capital Region), consisting of approximately 2.6 million inhabitants, were used to identify patients with P. aeruginosa.
Study population
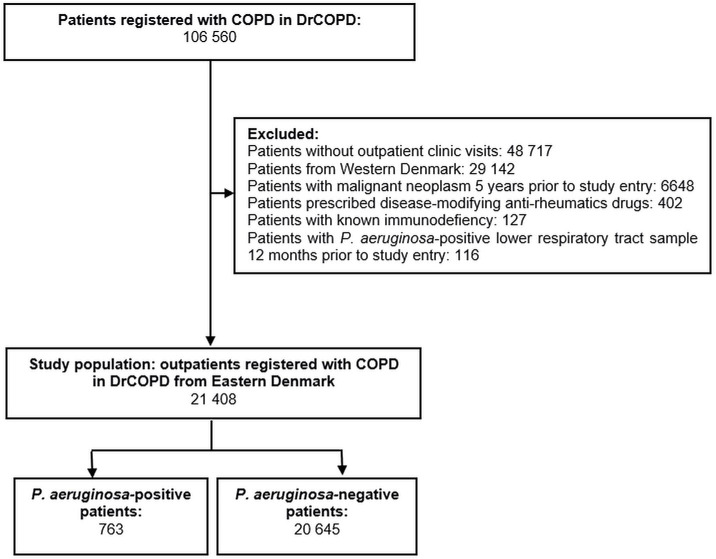
The study considered all patients registered with an outpatient clinic visit from 1 January 2010 to 31 October 2017 in DrCOPD. Figure 1 illustrates an overview of the study. Cohort entry was defined as the date for the patients first outpatient clinic visit in DrCOPD. Patients with only in-hospital-registrations were not included since these registrations do not hold information on essential patient characteristics (severity of airflow obstruction, degree of dyspnoea, body mass index (BMI) and smoking status). Patients from the western part of Denmark were not included, since we could not gain access to microbiological data from these patients. P. aeruginosa was defined as any positive lower respiratory tract culture (ie, sputum, tracheal secretion, bronchial secretion and bronchial alveolar lavage) after cohort entry. Patients with P. aeruginosa-positive lower respiratory tract sample 12 months prior to cohort entry were excluded.
Figure 1.
Study population: 21 408 patients registered with COPD in the Danish Register of COPD (DrCOPD) from 1 January 2010 to 31 October 2017.
Patients with malignant neoplasm (International Classification of Disease (ICD)−10 codes: C00–C97) or immunodefiency (ICD-10 codes: D80-84, D85, D89) 5 years prior to cohort entry or prescription of disease-modifying antirheumatics drugs (Anatomical Therapeutic Chemical-codes: L04AX03, L01AA01, A07EC01, L04AD01, L04AA13, L04AX01, L04AA06, P01BA02) 12 months prior to cohort entry were excluded since these conditions and drugs were suspected to be associated with the study outcome and may affect the ability to interpret the results of the study exposure. Online supplemental table 1, lists the ICD-10 codes used to define comorbidities. All patients were followed from cohort entry until the first P. aeruginosa-positive sample, death or 31 October 2017.
thoraxjnl-2021-217160supp001.pdf (130.1KB, pdf)
Exposure to ICS
All prescriptions for ICS, alone or in combination inhaler, redeemed 365 days prior to cohort entry were identified. These included: beclomethasone, budesonide, fluticasone, ciclesonide and mometasone.
All doses of ICS were converted to budesonide-equivalent doses: beclomethasone and mometasone were considered equivalent to budesonide. Fluticasone proprionate and ciclesonide were converted to budesonide doses using a ratio of 2:1 respectively 2.5:1. Categorisation of ICS doses was assessed by dividing ICS exposure into low (<400 μg), moderate (400–800 μg) and high (>800 μg) daily dose according to international Global Initiative for Asthma guidelines23 based on the accumulated dose in the year prior to the cohort entry. Non-use during the entire period was used as reference category.
Statistical analysis
Continuous variables are presented as median values and IQRs. Group comparisons were performed using a non-parametric test (Wilcoxon two-sample test) and t-test when appropriate. Categorical variables are reported as frequencies and proportions and compared between groups using Fisher’s exact test. A p value less or equal to 0.05 was considered statistically significant. Statistical analyses were performed using SAS statistical software (V.3.71 Enterprise Edition, SAS Institute).
The risk of P. aeruginosa associated with use of ICS was estimated using a Cox proportional hazard regression model. Death was handled as a competing risk in the model since it impedes the occurrence of P. aeruginosa. The model was adjusted for suspected confounders and markers of disease severity based on previous literature in the field: age (continuous, year), sex (male vs female), severity of airway obstruction (percentage of predicted FEV1; stage 1–4), BMI (class 1–5), smoking status (active vs not active), antibiotic use (yes vs no) and accumulated dose of oral corticosteroids (high vs low) 365 days prior to cohort entry and calendar year for entry in DrCOPD. We report both unadjusted results of univariate analyses for each covariate above and results from the adjusted multivariate analyses with all covariates included in the same model
In patients with unknown FEV1 and BMI, measurements from the first following outpatient clinic visit were used. Patients with unknown smoking status were classified as non-active smokers (most common among the patients with known status). We conducted a sensitivity analysis where missing BMI was categorised as ≥35 and missing FEV1 was classified as <30 (online supplemental table 2). Exposure to oral corticosteroids was divided into low-dose and high-dose categories based on the dose corresponding to a daily intake of <5 mg, respectively, ≥5 mg (low dose:<1825 mg; high dose ≥1825 mg). Non-use of oral corticosteroids in the entire prior year was used as reference group.
We did not model ICS as a time-dependent variable, as glucocorticoid use is associated with increased risk of long-term adverse effects,24 25 including infection with other microbial agents than P. aeruginosa, that can occur even months after discontinuation.26 The models were tested for linearity of continuous variables and proportion of hazards, using cumulative score residuals, and were found to be valid. Interactions between accumulated exposure of oral corticosteroids 365 days prior to cohort entry (p=0.93) as well as type of ICS (p=0.48) were tested and not found to be present. We reported data for all degrees of oral corticosteroid exposure and all types of ICS together. We conducted a supplemental analysis in a subgroup of patients with no use of OCS in the study population (online supplemental table 3) and also performed an analysis on ICS type (online supplemental table 4).
A propensity score matched model was applied as a sensitivity analysis using the greedy-match algorithm, created and maintained by biomedical statisticians at the Mayo Clinic.27 Patients exposed to high ICS dose were matched 1:2 with patients who were exposed to no, low or moderate ICS dose based on the same variables used in the adjusted main analysis. An unadjusted Cox proportional hazard regression model, treating death as competing event, was then used to estimate the risk of P. aeruginosa associated with high ICS dose versus no/low/moderate ICS dose. The estimate was retested using a robust variance estimator, accounting for the lack of independence in outcome induced by the matching.28
Results
The study cohort included 21 408 patients with COPD (figure 1). The median follow-up time was 1026 days (IQR: 417–1846), during which 763 (3.6%) patients were identified with a P. aeruginosa-positive respiratory tract sample. Patients with P. aeruginosa were more likely to have lower BMI (p<0.0001) and FEV1 (p<0.0001) and a higher rate of previous hospital-demanding exacerbations (p<0.0001) at cohort entry compared with P. aeruginosa negative patients (table 1). Prescriptions of respiratory drugs, oral corticosteroids and antibiotics were also more frequently filled in the group of P. aeruginosa-positive patients (table 1). As shown in table 2, the prevalence of use of ICS was markedly higher in patients with P. aeruginosa (90.2%) compared with P. aeruginosa-negative patients (68.3%). Budesonide and fluticasone were the most frequently used types of ICS in both groups.
Table 1.
Patient characteristics at cohort entry and by Pseudomonas aeruginosa event in 21 408 patients with COPD
| All patients | P. aeruginosa-positive patients | P. aeruginosa-negative patients | P value* | Adjusted OR (95% CI)† | |
| No of subjects | 21 408 (100) | 763 (3.6) | 20 645 (96.4) | ||
| Demographics | |||||
| Age (year), median (IQR) | 69 (62–76) | 70 (64–76) | 69 (62–76) | 0.0007 | 1.08 (1.08 to 1.09) |
| Male | 9619 (44.9) | 346 (45.4) | 9273 (44.9) | 0.8241 | 1.25 (1.17 to 1.34) |
| BMI, median (IQR) | 25 (21–29) | 23(20-27) | 25 (21–29) | <0.0001 | |
| Unknown BMI | 4527 (21.1) | 130 (17.0) | 4397 (21.3) | ||
| BMI class: | |||||
| <18.5 kg/m2 | 1681 (7.9) | 95 (12.5) | 1586 (7.7) | <0.0001 | 0.81 (0.78 to 0.84) |
| 18.5–24.9 kg/m2 | 6398 (29.9) | 268 (35.1) | 6130 (29.7) | ||
| 25–29.9 kg/m2 | 5018 (23.4) | 180 (23.6) | 4838 (23.4) | ||
| 30–34.9 kg/m2 | 2457 (11.5) | 61 (8.0) | 2396 (11.6) | ||
| ≥35 kg/m2 | 5854 (27.3) | 159 (20.8) | 5695 (27.6) | ||
| Pulmonary parameters | |||||
| MRC, median (IQR) | 3 (2–4) | 3 (3–4) | 3 (2–4) | ||
| Unknown MRC | 4823 (21.9) | 173 (19.1) | 4650 (22.0) | <0.0001 | |
| FEV1% predicted, median (IQR) | 49 (36–63) | 39 (30–50) | 49 (36–63) | ||
| Unknown FEV1% | 4293 (20.1) | 126 (16.5) | 4167 (20.2) | <0.0001 | |
| FEV1% predicted, severity of spirometric obstruction: | |||||
| ≥80 | 1108 (5.2) | 15 (2.0) | 1093 (5.3) | <0.0001 | 1.77 (1.69 to 1.86) |
| 50–79 | 7227 (33.8) | 152 (19.9) | 7075 (34.3) | ||
| 30–49 | 6416 (30.0) | 314 (41.1) | 6102 (29.6) | ||
| <30 | 6657 (31.1) | 282 (37.0) | 6375 (30.9) | ||
| Smoking status | |||||
| Active | 6590 (30.8) | 217 (28.4) | 6373 (30.8) | <0.0001 | 1.39 (1.28 to 1.49) |
| Former ≤6 months | 591 (2.8) | 10 (1.3) | 581 (2.8) | ||
| Former >6 months | 9386 (43.8) | 395 (51.8) | 8991 (43.6) | ||
| Never | 576 (2.7) | 17 (2.2) | 559 (2.7) | ||
| Unknown | 4265 (19.9) | 124 (16.3) | 4141 (20.1) | ||
| Hospital-requiring COPD exacerbation 12 months prior to cohort entry | |||||
| 0 | 10 301 (48.1) | 281 (36.8) | 10 020 (48.5) | <0.0001 | |
| 1 | 4082 (19.1) | 134 (17.6) | 3948 (19.1) | ||
| ≥2 | 7025 (32.8) | 348 (45.6) | 6677 (32.3) | ||
| All-cause hospitalisation 12 months prior to cohort entry | 11 840 (55.3) | 459 (60.2) | 11 381 (55.1) | 0.0061 | |
| Comorbidity | |||||
| Inflammatory polyarthropathy | 477 (2.2) | 6 (0.79) | 471 (2.3) | 0.0037 | |
| Systemic connective tissue disorder | 497 (2.3) | 23 (3.0) | 474 (2.3) | 0.2186 | |
| Myocardial infarction | 1661 (7.8) | 60 (7.9) | 1601 (7.8) | 0.8904 | |
| Atrial fibrillation | 3106 (14.5) | 104 (13.6) | 3002 (14.5) | 0.5298 | |
| Heart failure | 3511 (16.4) | 119 (15.6) | 3392 (16.4) | 0.5839 | |
| Hypertension | 6670 (31.1) | 228 (29.9) | 6442 (31.2) | 0.4498 | |
| Renal failure | 936 (4.4) | 34 (4.5) | 902 (4.4) | 0.8571 | |
| Peripheral vascular disease | 1706 (8.0) | 58 (7.6) | 1648 (8.0) | 0.7853 | |
| Cerebrovascular disease | 2041 (9.5) | 63 (8.3) | 1978 (9.6) | 0.2334 | |
| Diabetes mellitus, type 2 | 2654 (12.1) | 106 (11.7) | 2548 (12.0) | 0.2334 | |
| Asthma | 3097 (14.5) | 145 (19.0) | 2952 (14.3) | 0.0004 | |
| Bronchiectasis | 209 (0.98) | 14 (1.8) | 195 (0.94) | 0.0223 | |
| Use of medication 12 months prior to cohort entry | |||||
| Oral corticosteroids‡ | |||||
| No use | 13 159 (61.5) | 315 (41.3) | 12 844 (62.2) | <0.0001 | |
| Low dose | 6119 (28.6) | 306 (40.1) | 5813 (28.2) | ||
| High dose | 2130 (10.0) | 142 (18.6) | 1988 (9.6) | ||
| Accumulated dose (mg), median (IQR) | 625 (250–000) | 1000 (500–2500) | 500 (250–2000) | <0.0001 | |
| Respiratory inhalation medicine | |||||
| Long-acting beta2-agonist or long-acting muscarin-antagonist | 13 869 (64.8) | 662 (86.8) | 13 207 (64.0) | <0.0001 | |
| Antibiotics § | 12 324 (57.6) | 598 (78.4) | 11 726 (56.8) | <0.0001 | 1.14 (1.07 to 1.23) |
| Theophylline | 691 (3.2) | 55 (7.2) | 636 (3.1) | <0.0001 |
Data are presented as n (%) or median (IQR), unless otherwise specified.
*Group comparison was performed using non-parametric test (Wilcoxon two-sample test) and Fisher’s exact test.
†The model is adjusted for all variables displayed in this column, calendar year and the accumulated ICS dose 365 days prior to cohort entry.
‡Low dose: accumulated dose <1825 mg; high dose: accumulated dose ≥1825 mg.
§Any antibiotic drug.
BMI, body mass index; ICS, inhaled corticosteroids; MRC, Medical Research Council Dyspnoea Scale.
Table 2.
Use of ICS 365 days prior to cohort entry in 21 408 patients with COPD
| All patients |
Pseudomonas aeruginosa-
positive patients |
P. aeruginosa-negative patients | |
| Patients with ICS use | 14 785 (69.1) | 688 (90.2) | 14 097 (68.3) |
| ICS exposure in ICS users, n (%)* | |||
| Low | 5030 (37.4) | 126 (18.3) | 5405 (38.3) |
| Moderate | 4180 (28.3) | 179 (26.0) | 4001 (28.4) |
| High | 5075 (34.3) | 383 (55.7) | 4692 (33.3) |
| Daily dose of ICS (μg), median (IQR) | 559 (263–1026) | 924 (493–1644) | 530 (247–986) |
| Number of prescriptions by ICS type† | |||
| Budesonide | 51 445 (61.0) | 2681 (50.5) | 48 764 (61.7) |
| Fluticasone | 31 678 (37.5) | 2582 (48.6) | 29 096 (36.7) |
| Beclomethasone | 756 (0.90) | 16 (0.30) | 740 (0.94) |
| Momethasone | 328 (0.39) | 17 (0.32) | 311 (0.39) |
| Ciclesonide | 156 (0.18) | 12 (0.23) | 144 (0.18) |
Data are presented as n (%) or median (IQR), unless otherwise specified.
Patients with no ICS use (n=6623) 365 days prior to cohort entry are not included in the table.
*Daily budesonide equivalent doses based on the accumulated ICS dose 365 days prior to cohort entry, μg : low <400; moderate 400–800; high >800.
†Last prescription redeemed prior to cohort entry.
ICS, inhaled corticosteroids.
Outcome
Use of ICS was associated with an increased risk of P. aeruginosa compared with non-use in unadjusted analyses (HR 3.74, 95% CI 2.95 to 4.75, p<0.0001) and the risk remained significantly increased after adjusting for covariates (HR 2.26, 95% CI 1.76 to 2.89, p<0.0001). There was a strong relationship between ICS dose and outcome, with stepwise increase of the P. aeruginosa-risk with the exposure to ICS (table 3). The risk was 3.6-fold increased (HR 3.58, 95% CI 2.75 to 4.65, p<0.0001) in patients with the highest ICS exposure. Figure 2A illustrates the cumulative incidence. The results remained stable after conducting a modified data imputation (online supplemental table 2) and after excluding patients (n=8249) with use of OCS 365 days prior to cohort entry (online supplemental table 3). Data on associations between ICS type and outcome are presented in online supplemental table 4.
Table 3.
Cox regression hazard estimates for risk of Pseudomonas aeruginosa with use of inhaled corticosteroids in the study population (N=21 408)
| P. aeruginosa event | Unadjusted HR (95% CI) | P value | Adjusted HR (95% CI) | P value |
| ICS exposure, μg * | ||||
| No use | ref | ref | ||
| Low <400 | 1.77 (1.33 to 2.36) | <0.0001 | 1.38 (1.03 to 1.84) | 0.0296 |
| Moderate 400–800 | 3.37 (2.58 to 4.42) | <0.0001 | 2.16 (1.63 to 2.85) | <0.0001 |
| High >800 | 6.41 (5.00 to 8.20) | <0.0001 | 3.58 (2.75 to 4.65) | <0.0001 |
| Accumulated OCS dose 365 days prior to cohort entry, mg | ||||
| No use | ref | ref | ||
| Low <1825 | 2.18 (1.86 to 2.55) | <0.0001 | 1.28 (1.09 to 1.52) | 0.0035 |
| High ≥1825 | 3.23 (2.65 to 3.94) | <0.0001 | 1.48 (1.20 to 1.83) | 0.0003 |
| Active smoking † | 0.91 (0.77 to 1.06) | 0.217 | 1.11 (0.95 to 1.31) | 0.200 |
| Age (per year increased) | 1.03 (1.03 to 1.04) | <0.0001 | 1.03 (1.02 to 1.04) | <0.0001 |
| Male | 1.08 (0.93 to 1.24) | 0.309 | 1.31 (1.14 to 1.52) | 0.0002 |
| BMI (per class increase; 1–5) ‡ |
0.73 (0.67 to 0.79) | <0.0001 | 0.80 (0.74 to 0.87) | <0.0001 |
| GOLD stage (per increase to next stage; 1–4)§ | 1.95 (1.76 to 2.16) | <0.0001 | 1.47 (1.32 to 1.63) | <0.0001 |
| Prescription of any antibiotics 365 days prior to cohort entry | 2.88 (2.42 to 3.42) | <0.0001 | 2.09 (1.74 to 2.50) | <0.0001 |
The model is adjusted for calendar year for study entry and all variables displayed in the table.
*Daily budesonide equivalent doses based on the accumulated ICS dose 365 days prior to cohort entry.
†Reference: never or former smoking.
‡BMI class (kg/m2); 1: <18.5, 2: 18.5–24.9, 3: 25–29.9, 4: 30–34.9, 5: ≥35.
§Increase in predicted FEV1% severity stage defined by the GOLD: 1: ≥80, 2: 50–79; 3: 30–49, 4:<30.
¶.
BMI, body mass index; GOLD, Global Initiative for Chronic Obstructive Lung Disease; ICS, Inhaled Corticosteroids; OCS, Oral Corticosteroids.
Figure 2.
Cumulative incidence of Pseudomonas aeruginosa event according to exposure to inhaled corticosteroids in (A) 21 408 patients with COPD (brown line: high exposure, green line: moderate exposure, red line: low exposure, blue line: no exposure) and (B) 13 332 propensity matched patients with COPD (red line: high exposure, blue line: no/low/moderate exposure).
Sensitivity analyses
A subgroup of 13 332 patients with COPD in the cohort population was formed using a propensity matched model, consisting of 4931 (37%) patients with high ICS exposure matched 1:2 with 8401 (63%) patients with no/low/moderate ICS exposure. Patient characteristics of the two groups are presented in online supplemental table 5. High exposure to ICS (reference: no, low or moderate ICS exposure) was associated with a twofold increased risk of P. aeruginosa (HR 2.05, 95% CI 1.76 to 2.39, p<0.0001). The difference remained significant when assessed by a stratified long-rank test (p<0.0001). The cumulative incidence is illustrated in figure 2B.
Discussion
In our multiregional cohort study of over 20 000 outpatients with COPD, we found that ICS use was associated with a substantially and independent increased risk of acquiring a P. aeruginosa-positive lower respiratory airway culture. There was a strong dose-dependent 3.5-fold increased risk of P. aeruginosa in patients with the highest ICS exposure (no use of ICS as reference).
Few data are available on risk factors for P. aeruginosa in the setting of COPD. To our knowledge, this is the first study reporting ICS as a potential risk factor of P. aeruginosa in a large and unselected population of patients with COPD. Previous studies on risk factors for P. aeruginosa have primarily been conducted in smaller cohorts of hospitalised patients with exacerbation of COPD17 18 and who might have been P. aeruginosa-positive prior to admission.
Despite lack of high-level evidence of an effect, ICS is widely used in cystic fibrosis, where P. aeruginosa is a well-known determinant of a subsequent worsening of prognosis.29 Interestingly, an earlier double-blind placebo-controlled study investigating the effect of fluticasone in children 6–17 years was terminated prematurely due to an increase of first-time isolation of P. aeruginosa in the group treated with ICS compared with the placebo group.29 However, data from a recent and similar trial found no increase in isolation of the bacteria in patients treated with ICS.30
Along the line with infectious lung complications to ICS, multiple larger population-based studies have demonstrated increased risk of pneumonia and mycobacterial infections with ICS use in patients with COPD.7–11 Results from these studies cannot be directly compared with ours due to differences in methodologies, but several similarities are apparent. First, the high proportion of ICS-users in our cohort is comparable to the previous studies.8–10 Second, like ours, these studies also report a robust dose-related risk8 10 using similar dose categories.10 Nevertheless, our risk estimates for acquiring P. aeruginosa seem to be substantially higher compared with the observed pneumonia risk increase associated with ICS use (not segregated in accumulated doses). Several COPD trials have also reported increased risk of pneumonia with ICS use,12 31 and the risk of pneumonia is also seen when lower daily doses of ICS are used.32 33 Like in other studies, fluticasone and budesonide were the most commonly prescribed types of ICS. However, in comparison to previous observational studies10 11 that reported an increased risk of pneumonia in fluticasone-users compared with budesonide-users, we did not find any association between risk of P. aeruginosa and ICS type when testing for interaction. A sensitivity analysis revealed that users of fluticasone were characterised by using a much higher (approximately double) dose of ICS in comparison to other ICS users. Thus, testing for fluticasone use actually tested whether high doses increased the risk of outcome (ie, not testing purely whether this specific chemical formulation increases the risk). Thus, based on our data, it seems that fluticasone is not associated with an excess risk.
Strengths of the study include observations based on a large and well-characterised population of patients diagnosed with COPD. Thus, we were able to adjust for several clinically important and potential cofounders. Moreover, the results were tested in several sensitivity analyses and the signal remained strong.
As in any database study, we cannot report actual intake of the ICS and some patients may have been non-adherent. However, repetitive collection of the prescribed medicine suggests that adherence is sufficient. Additionally, the proportion of patients with COPD on ICS correlates well with previous population studies.8 10 Furthermore, in case of frequent non-adherence, a lower intake of ICS than registered would tend to underestimate the actual observed risk of P. aeruginosa infection among the ICS-users.
Although the results suggest a biological plausibility, no causal relationship can be determined due to the observational design of the study. However, taking into account that we have access to and controlled for some of the most important confounders, it is unlikely that confounding could explain an observed risk ratio of this magnitude. Possible biological mechanisms include ICS-induced alternations of the innate and adaptive immune system,34 35 which has been reported to increase the bacterial load and change the microbial composition in the airways.36 The possible causal association between ICS and P. aeruginosa is illustrated in a directed acyclic graph (DAG) in online supplemental figure 1.
To conclude, use of ICS in patients with COPD followed in Danish outpatient clinics was associated with a high and dose-related risk of acquiring P. aeruginosa. Caution should be taken when administering high dose of ICS in severely ill patients with COPD. These results should be confirmed in comparable cohorts and other settings.
Footnotes
Twitter: @tslapperre
Contributors: JE contributed to the conception and design of the study, data collection and analysis, data interpretation and writing the manuscript. JUSJ, TSI, RS, TW, NS, EFH, TSL and HM contributed to the conception and design of the study and data interpretation. CO, JBB, JB, RBD and USJ contributed to data collection. IAA, MIS and PS contributed to data analysis. All authors critically revised the manuscript and approved the final version of the work.
Funding: The study was financed by grants from The Independent Research Fund Denmark (8020-00425B) and The Research committee at Herlev and Gentofte University Hospital.
Disclaimer: The foundations had no role in design, implementation, interpretation or reporting of the study.
Competing interests: RBD reports grants and personal fees from Roche, outside the submitted work. TSI reports personal fees from AstraZeneca, outside the submitted work. PS reports non-financial support from Novartis and personal fees from Boehringer Ingelheim, outside the submitted work. HM is a member of ALK-Abelló Nordic A/S advisory board.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data may be obtained from a third party and are not publicly available. Due to the Danish legislation regarding sharing of population data, source data collected for this study cannot be made available for others. However, Danish citizens who have a legitimate reason can apply for access to the data via the Danish National Health Authority (https://sundhedsdatastyrelsen.dk/da/forskerservice/ansog-om-data).
Ethics statements
Patient consent for publication
Not required.
References
- 1. Hurst JR, Vestbo J, Anzueto A, et al. Susceptibility to exacerbation in chronic obstructive pulmonary disease. N Engl J Med 2010;363:1128–38. 10.1056/NEJMoa0909883 [DOI] [PubMed] [Google Scholar]
- 2. Price D, West D, Brusselle G, et al. Management of COPD in the UK primary-care setting: an analysis of real-life prescribing patterns. Int J Chron Obstruct Pulmon Dis 2014;9:889–905. 10.2147/COPD.S62750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Global Initiative for Chronic Obstructive Lung Disease . 2019 global strategy for prevention, diagnosis and management of COPD. Available: www.goldcopd.org [Accessed 5 Sep 2019].
- 4. Bafadhel M, Peterson S, De Blas MA, et al. Predictors of exacerbation risk and response to budesonide in patients with chronic obstructive pulmonary disease: a post-hoc analysis of three randomised trials. The Lancet Respiratory Medicine 2018;6:117–26. 10.1016/S2213-2600(18)30006-7 [DOI] [PubMed] [Google Scholar]
- 5. Magnussen H, Disse B, Rodriguez-Roisin R, et al. Withdrawal of inhaled glucocorticoids and exacerbations of COPD. N Engl J Med 2014;371:1285–94. 10.1056/NEJMoa1407154 [DOI] [PubMed] [Google Scholar]
- 6. Kew K, Seniukovich A. Inhaled steroids and risk of pneumonia for chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2014;3:CD010115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Brassard P, Suissa S, Kezouh A, et al. Inhaled corticosteroids and risk of tuberculosis in patients with respiratory diseases. Am J Respir Crit Care Med 2011;183:675–8. 10.1164/rccm.201007-1099OC [DOI] [PubMed] [Google Scholar]
- 8. Andréjak C, Nielsen R, Thomsen Vibeke Ø, et al. Chronic respiratory disease, inhaled corticosteroids and risk of non-tuberculous mycobacteriosis. Thorax 2013;68:256–62. 10.1136/thoraxjnl-2012-201772 [DOI] [PubMed] [Google Scholar]
- 9. Ernst P, Gonzalez AV, Brassard P, et al. Inhaled corticosteroid use in chronic obstructive pulmonary disease and the risk of hospitalization for pneumonia. Am J Respir Crit Care Med 2007;176:162–6. 10.1164/rccm.200611-1630OC [DOI] [PubMed] [Google Scholar]
- 10. Suissa S, Patenaude V, Lapi F, et al. Inhaled corticosteroids in COPD and the risk of serious pneumonia. Thorax 2013;68:1029–36. 10.1136/thoraxjnl-2012-202872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Brode SK, Campitelli MA, Kwong JC, et al. The risk of mycobacterial infections associated with inhaled corticosteroid use. Eur Respir J 2017;50:1700037–10. 10.1183/13993003.00037-2017 [DOI] [PubMed] [Google Scholar]
- 12. Crim C, Calverley PMA, Anderson JA, et al. Pneumonia risk in COPD patients receiving inhaled corticosteroids alone or in combination: TORCH study results. Eur Respir J 2009;34:641–7. 10.1183/09031936.00193908 [DOI] [PubMed] [Google Scholar]
- 13. Renom F, Yáñez A, Garau M, et al. Prognosis of COPD patients requiring frequent hospitalization: role of airway infection. Respir Med 2010;104:840–8. 10.1016/j.rmed.2009.12.010 [DOI] [PubMed] [Google Scholar]
- 14. Almagro P, Salvadó M, Garcia-Vidal C, et al. Pseudomonas aeruginosa and Mortality after Hospital Admission for Chronic Obstructive Pulmonary Disease. Respiration 2012;84:36–43. 10.1159/000331224 [DOI] [PubMed] [Google Scholar]
- 15. Eklöf J, Sørensen R, Ingebrigtsen TS, et al. Pseudomonas aeruginosa and risk of death and exacerbations in patients with chronic obstructive pulmonary disease: an observational cohort study of 22 053 patients. Clinical Microbiology and Infection 2020;26:227–34. 10.1016/j.cmi.2019.06.011 [DOI] [PubMed] [Google Scholar]
- 16. Garcia-Clemente M, de la Rosa D, Máiz L, et al. Impact of Pseudomonas aeruginosa Infection on Patients with Chronic Inflammatory Airway Diseases. J Clin Med 2020;9:3800. 10.3390/jcm9123800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Garcia-Vidal C, Almagro P, Romaní V, et al. Pseudomonas aeruginosa in patients hospitalised for COPD exacerbation: a prospective study. Eur Respir J 2009;34:1072–8. 10.1183/09031936.00003309 [DOI] [PubMed] [Google Scholar]
- 18. Monsó E, Garcia-Aymerich J, Soler N, et al. Bacterial infection in exacerbated COPD with changes in sputum characteristics. Epidemiol Infect 2003;131:799–804. 10.1017/S0950268803008872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Thygesen LC, Daasnes C, Thaulow I, et al. Introduction to Danish (nationwide) registers on health and social issues: structure, access, legislation, and archiving. Scand J Public Health 2011;39:12–16. 10.1177/1403494811399956 [DOI] [PubMed] [Google Scholar]
- 20. Lange P, Tøttenborg S, Sorknæs A, et al. Danish register of chronic obstructive pulmonary disease. Clin Epidemiol 2016;8:673–8. 10.2147/CLEP.S99489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lynge E, Sandegaard JL, Rebolj M. The Danish national patient register. Scand J Public Health 2011;39:30–3. 10.1177/1403494811401482 [DOI] [PubMed] [Google Scholar]
- 22. Johannesdottir SA, Horváth-Puhó E, Ehrenstein V, et al. Existing data sources for clinical epidemiology: the Danish national database of Reimbursed prescriptions. Clin Epidemiol 2012;4:303–13. 10.2147/CLEP.S37587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Global Strategy for Asthma Management and Prevention . Global initiative for asthma: 2019 GINA report. Available: https://ginasthma.org/ [Accessed 17 May 2021].
- 24. Sivapalan P, Ingebrigtsen TS, Rasmussen DB, et al. COPD exacerbations: the impact of long versus short courses of oral corticosteroids on mortality and pneumonia: nationwide data on 67 000 patients with COPD followed for 12 months. BMJ Open Resp Res 2019;6:e000407–8. 10.1136/bmjresp-2019-000407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Sullivan PW, Ghushchyan VH, Globe G, et al. Oral corticosteroid exposure and adverse effects in asthmatic patients. J Allergy Clin Immunol 2018;141:110–6. 10.1016/j.jaci.2017.04.009 [DOI] [PubMed] [Google Scholar]
- 26. Gensler LS. Glucocorticoids: complications to anticipate and prevent. Neurohospitalist 2013;3:92–7. 10.1177/1941874412458678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Biomedical statistics and informatics software packages, 2018. Available: http://bioinformaticstools.mayo.edu/research/gmatch/ [Accessed 10 Nov 2018].
- 28. Austin PC. The use of propensity score methods with survival or time‐to‐event outcomes: reporting measures of effect similar to those used in randomized experiments. Stat Med 2014;33:1242–58. 10.1002/sim.5984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Balfour-Lynn IM, Welch K, Smith S. Inhaled corticosteroids for cystic fibrosis. Cochrane Database Syst Rev 2019;7:CD001915. 10.1002/14651858.CD001915.pub6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. De Boeck K, De Baets F, Malfroot A, et al. Do inhaled corticosteroids impair long-term growth in prepubertal cystic fibrosis patients? Eur J Pediatr 2007;166:23–8. 10.1007/s00431-006-0198-9 [DOI] [PubMed] [Google Scholar]
- 31. Calverley PMA, Stockley RA, Seemungal TAR, et al. Reported pneumonia in patients with COPD: findings from the INSPIRE study. Chest 2011;139:505–12. 10.1378/chest.09-2992 [DOI] [PubMed] [Google Scholar]
- 32. Ferguson GT, Anzueto A, Fei R, et al. Effect of fluticasone propionate/salmeterol (250/50μg) or salmeterol (50μg) on COPD exacerbations. Respir Med 2008;102:1099–108. 10.1016/j.rmed.2008.04.019 [DOI] [PubMed] [Google Scholar]
- 33. Anzueto A, Ferguson GT, Feldman G, et al. Effect of fluticasone propionate/salmeterol (250/50) on COPD exacerbations and impact on patient outcomes. COPD 2009;6:320–9. 10.1080/15412550903140881 [DOI] [PubMed] [Google Scholar]
- 34. Singanayagam A, Glanville N, Cuthbertson L, et al. Inhaled corticosteroid suppression of cathelicidin drives dysbiosis and bacterial infection in chronic obstructive pulmonary disease. Sci Transl Med 2019;11:eaav3879. 10.1126/scitranslmed.aav3879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Barnes PJ. Corticosteroid effects on cell signalling. Eur Respir J 2006;27:413–26. 10.1183/09031936.06.00125404 [DOI] [PubMed] [Google Scholar]
- 36. Contoli M, Pauletti A, Rossi MR, et al. Long-term effects of inhaled corticosteroids on sputum bacterial and viral loads in COPD. Eur Respir J 2017;50:1700451. 10.1183/13993003.00451-2017 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
thoraxjnl-2021-217160supp001.pdf (130.1KB, pdf)
Data Availability Statement
Data may be obtained from a third party and are not publicly available. Due to the Danish legislation regarding sharing of population data, source data collected for this study cannot be made available for others. However, Danish citizens who have a legitimate reason can apply for access to the data via the Danish National Health Authority (https://sundhedsdatastyrelsen.dk/da/forskerservice/ansog-om-data).