Summary
Background
Vaccine hesitancy continues to limit global efforts in combatting the COVID-19 pandemic. Emerging research demonstrates the role of social media in disseminating information and potentially influencing people's attitudes towards public health campaigns. This systematic review sought to synthesize the current evidence regarding the potential role of social media in shaping COVID-19 vaccination attitudes, and to explore its potential for shaping public health interventions to address the issue of vaccine hesitancy.
Methods
We performed a systematic review of the studies published from inception to 13 of March2022 by searching PubMed, Web of Science, Embase, PsychNET, Scopus, CINAHL, and MEDLINE. Studies that reported outcomes related to coronavirus disease 2019 (COVID-19) vaccine (attitudes, opinion, etc.) gathered from the social media platforms, and those analyzing the relationship between social media use and COVID-19 hesitancy/acceptance were included. Studies that reported no outcome of interest or analyzed data from sources other than social media (websites, newspapers, etc.) will be excluded. The Newcastle Ottawa Scale (NOS) was used to assess the quality of all cross-sectional studies included in this review. This study is registered with PROSPERO (CRD42021283219).
Findings
Of the 2539 records identified, a total of 156 articles fully met the inclusion criteria. Overall, the quality of the cross-sectional studies was moderate – 2 studies received 10 stars, 5 studies received 9 stars, 9 studies were evaluated with 8, 12 studies with 7,16 studies with 6, 11 studies with 5, and 6 studies with 4 stars. The included studies were categorized into four categories. Cross-sectional studies reporting the association between reliance on social media and vaccine intentions mainly observed a negative relationship. Studies that performed thematic analyses of extracted social media data, mainly observed a domination of vaccine hesitant topics. Studies that explored the degree of polarization of specific social media contents related to COVID-19 vaccines observed a similar degree of content for both positive and negative tone posted on different social media platforms. Finally, studies that explored the fluctuations of vaccination attitudes/opinions gathered from social media identified specific events as significant cofactors that affect and shape vaccination intentions of individuals.
Interpretation
This thorough examination of the various roles social media can play in disseminating information to the public, as well as how individuals behave on social media in the context of public health events, articulates the potential of social media as a platform of public health intervention to address vaccine hesitancy.
Funding
None.
Keywords: COVID-19 vaccines, Vaccine hesitancy, Public health, Social media, Global health, Systematic review, Viral infections, Pandemics, Social behaviors
Research in context.
Evidence before this study
Prior to conducting our systematic review, we searched PubMed and Web of Science without language restrictions and using keywords such as “social media”, “COVID-19″ and “vaccine” to identify previous evidence in the form of a systematic review on our topic of interest. Prior to and during the conduction of this systematic review, we identified several other systematic reviews that have addressed the issue of social media and attitudes towards a COVID-19 vaccination. Prior research has demonstrated the role that social media plays as a platform for mass media and information transmission. Additionally, given that many patients and individuals refer to social media as their source of information, emerging research has been placing considerable emphasis on how social media can influence attitudes toward public health interventions and campaigns. It has been shown that vaccine hesitancy plays a major role in affecting vaccination rates, as well as the potential in reaching herd immunity in the context of the COVID-19 pandemic. Consequently, an abundance of research has emerged in the literature studying the potential role of social media in shaping attitudes regarding COVID-19 vaccination, as well as social media's role as an intervention platform to address vaccine hesitancy. However, to date and to the best of our knowledge, no systematic review has been published synthesizing all the evidence relating social media and vaccine attitudes. Upon those bases, and on March 13th, 2022, we conducted a systematic review of the literature using developed keywords. Studies that reported outcomes related to coronavirus disease 2019 (COVID-19) vaccine (attitudes, opinion, etc.) gathered from the social media platforms, and those analyzing the relationship between social media use and COVID- 19 hesitancy/acceptance were included. Studies that reported no outcome of interest or analyzed data from sources other than social media (websites, newspapers, etc.) will be excluded. The Newcastle Ottawa Scale (NOS) was used to assess the quality of all cross-sectional studies included in this review.
Added value of this study
Our systematic review, carried out according to best practices, included 156 peer-reviewed articles, most of which have been published in the past year. Overall, our review exemplified the association between social media reliance for information and hesitant attitudes, as well as a demonstrated strong potential for social media as an intervention area to address vaccine hesitancy and aid in reaching herd immunity globally.
Implications of all the available evidence
The evidence we found have important implications for public health research and practice. Firstly, our findings exemplify that understanding social media usage patterns can provide an opportunity for targeted intervention. Additionally, the findings of this review demonstrate that there is a strong potential for polarized views to be amplified using social media, which presents an opportunity for targeting misinformation. Furthermore, utilizing social media to understand public's sentiment allows for tailored and targeted intervention, specific to the current views held by the public. Finally, given that specific events trigger people's emotions regarding vaccination, it is crucial for the government to adjust vaccination policies promptly in response to the public health events to promote massive vaccination via dynamic monitoring public sentiments.
Alt-text: Unlabelled box
Introduction
In 2019, The World Health Organization (WHO) listed vaccine hesitancy as one of the top 10 threats to world health.1 In the context of public health responses, vaccination campaigns are considered to be one of the most successful public health interventions and a cornerstone for the prevention of communicable infectious diseases. While vaccine hesitancy is perceived to be a long-standing problem, it has recently assumed great urgency in light of the coronavirus disease 2019 (COVID-19) pandemic.2 Vaccine hesitancy, defined as delay in acceptance or refusal of vaccination despite availability of vaccination services, may be the product of an array of factors and held views.3 Emerging research in the literature has investigated such factors in relation to COVID-19 vaccine hesitancy and demonstrated that hesitancy may stem from concerns relating to vaccine efficacy, safety, side effects, convenience, price, beliefs that the vaccine is not necessary, the idea that testing for the vaccine was insufficient and that the pace of its development was too quick, as well as the financial motivation of the authorities/pharmaceutical companies.4 Among the many barriers that contribute to vaccine hesitancy and were identified globally, a recurrent theme continues to be that hesitancy is due to misinformation regarding the benefits and the adverse effects of vaccines.
Given that people increasingly refer to the internet and social media networks to seek information, emerging research in the literature has recently placed special emphasis on investigating the association between social media usage and attitudes towards public health interventions, specifically COVID-19 vaccinations.5, 6, 7, 8 The ongoing mitigating efforts to control the spread of SARS-CoV-2, including physical distancing, quarantine requirements, and travel bans across the world, may intensify the use of social media as individuals try to remain connected while physically apart. This increased reliance on social media networks may be concerning due to its ability to spread misinformation and contribute to increased hesitancy, especially among populations who may be vulnerable to increased hesitancy rates (e.g., those in low socioeconomic status groups).9,10 Previous research has shown that vaccine hesitant groups on social media have an alarming footprint and report that anti-vaccination messages are large proportions of the content about vaccines on popular social media sites,11, 12, 13, 14, 15, 16, 17, 18 which engenders more user engagement.19,20Another important point is the existence of echo chamber effect on social media platforms, by gathering individuals and surrounding them by like-minded people in terms of ideological orientation.21 For example, such echo chambers existon Facebook, and it is confirmed that pro- and anti-vaccination attitudes polarize the users’ opinion.22 Therefore, studying networked communities can help in understanding online discussions/public opinions on vaccine hesitancy and exploring how they can impact society and science communities.23 On the other hand, it is recognized that utilizing social media data can offer advantages over traditional survey methods in this critical times, by enabling timely monitoring of public attitudes/opinions, which altogether supports the notion of analyzing social media data with the aim to better understand vaccination intentions and attitudes regarding the ongoing immunization campaign.24
Although the latest updates derived from surveys/polls conducted around the world indicate that vaccine hesitancy shows a decreasing trend over time,25 this issue deserves further attention and deeper investigation in order to enhance the willingness to vaccinate even more, and to prevent such phenomenon in case of similar future scenarios. Upon these bases, this systematic review of the literature sought to summarize the available data in the literature on the various associations between social media usage and attitudes toward COVID-19 vaccination campaigns worldwide. To the best of our knowledge, this is one of the first and most extensive systematic review to be conducted on this extremely important association.
Methods
Search strategy and selection criteria
This systematic review of the literature was performed according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Several databases were selected for searching potential eligible articles: PubMed, Embase, ISI (Web of Science), Scopus, PsycNET, Medline and CINAHL. We also performed a manual search of reference lists of included articles. The initial systematic search was performed in September 2021, and as part of the review process we performed the updated systematic search of all databases in March 2022. The protocol related to this systematic review is registered with PROSPERO (CRD42021283219).
The search criteria were defined by combining the keywords related to the general exposure of interest (social media), the outcome of interest (vaccination) and was further focused by adding keywords related to the specific disease (COVID-19). The detailed search strategy is presented in Supplementary Table S1.
We included studies that reported any outcome related to COVID-19 immunization campaigns gathered from social media (related to opinions, attitudes, etc.). We also included studies that determined the rate of vaccine hesitancy/acceptance in a population, and reported the associations observed with social media use. Studies that analyzed data from sources other than social media (websites, newspapers, etc.) were excluded. Only studies published in the English language published before September 2021 were included. The detailed definition of the inclusion/exclusion criteria is given in Supplementary Table S2.
Data analysis
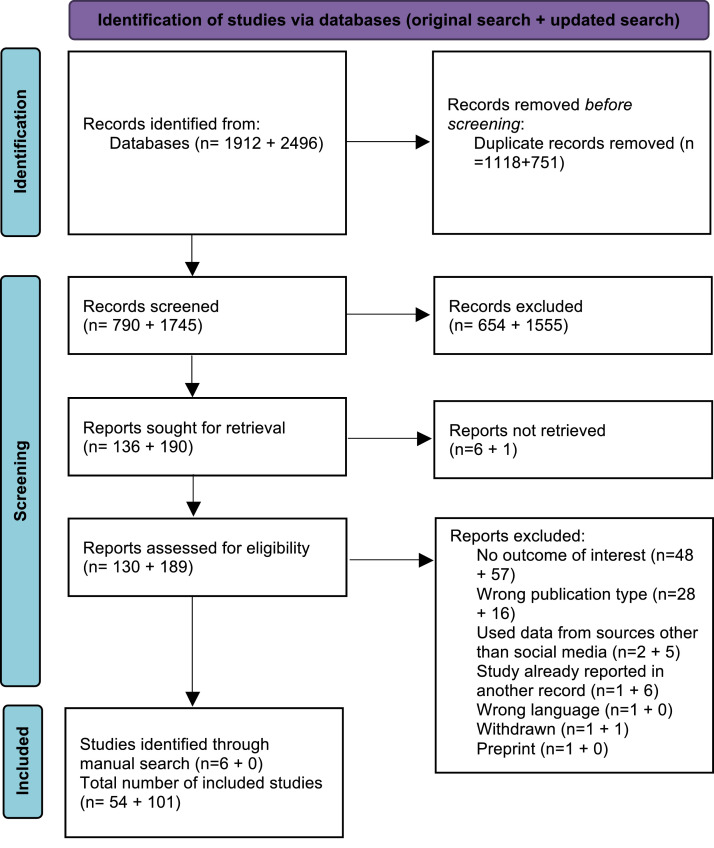
After performing the systematic search of all electronic databases, we retrieved the articles, removed the duplicates, and imported the references in Rayyan.26 As illustrated in Figure 1, titles and abstracts were screened by two reviewers independently (AL and VP). All conflicts were resolved by contacting the third reviewer (AP). After this step, we performed the full-text assessment in the same manner, thereby identifying the final list of eligible articles.
Figure 1.
Preferred reporting items for systematic reviews and meta-analyses (PRISMA) study selection flow diagram for the systematic search performed in September 2021 and the Updated search performed in March 2022.
The data extraction was performed by two reviewers (A.P. and Y.A.A), and every disagreement was resolved by discussion with the third reviewer (F.C.).The data from the eligible studies were extracted in a pre-defined Excel sheet, defined by the following columns: (1) the name of the first author, (2) the geographical context, (3) the aim, (4) the study design (5) the study period when the assessment/analysis was performed, (6) the study population or study content, (7) vaccination status (where applicable), (8) the main results related to the reported associations/correlations between social media use and vaccine acceptance/hesitancy, (9) the main results related to the content gathered from the social media that were related to COVID-19 vaccination. After summarizing all the data in the Excel sheet, we were able to identify all studies that fulfilled the inclusion criteria, and to remove those that initially passed the full text screening but were deemed inadequate to be included in the systematic review.
The data are presented in a tabulated form and were either presenting associations between social media utilization and vaccine hesitancy, reporting analyses of public opinion on COVID-19 vaccines, analyzing the sentiments of the population regarding the current immunization campaigns and lastly, or reporting the change and fluctuations in the vaccine-related discussions caused by some driver/trigger events. Due to the nature of the data, we were not able to perform any visual presentations.
We evaluated the quality of only cross-sectional studies that reported the associations between vaccine intentions and social media use. The quality of these studies were evaluated with the Newcastle-Ottawa Scale (NOS) for non-randomized studies.27 NOS uses a star system, where a study can have a maximum of 9 stars after evaluating for 3 main categories: selection (for which a study can have a maximum of 4 stars), comparability (a maximum of 2 stars) and outcome (a maximum of 3 stars).
Results
Search results
The initial systematic search of electronic databases identified a total of 4408 studies. Overall, a total of 155 studies were included as part of this updated systematic search, and the full process for both searches is presented on a separate PRISMA flow-chart (Figure 1)
Summary characteristics of the included studies
The included studies were categorized into the following four categories:
-
(1)
cross-sectional studies reporting the association between reliance on social media and vaccine hesitancy and/or acceptance.
-
(2)
studies that performed thematic analyses of extracted social media data, thereby reporting discussions related to COVID-19 vaccine intentions/opinions;
-
(3)
studies that explored the degree of polarization of specific social media contents related to COVID-19 vaccines (the degree of positive vs. negative sentiments);
-
(4)
studies that explored the fluctuations of vaccination attitudes/opinions gathered from social media depending on specific events that were identified as trigger events.
The studies from the first category were all cross-sectional in nature (Table 1), and mainly employed anonymous online surveys for assessments. From a total of 61 studies (62 records), USA had the highest numbers of studies per country (n = 11). Two studies were conducted across multiple countries, while no studies were reported from South America or Africa.
Table 1.
Summary characteristics and main results of studies that reported the association between the reliance on social media and COVID-19 vaccination intentions.
| Reference | Study design /location | Study period | Assessment Tool | Study population | Vaccination status | Main results |
|---|---|---|---|---|---|---|
| Alfatease et al., 2021136 | Cross-sectional study/ Saudi Arabi | April and May 2021 | Questionnaire o social media (Twitter, WhatsApp, and Facebook) | 613 persons older than 18 years | NR | Male participants were less likely to be influenced by social media when deciding to take COVID-19 vaccines (p = 0.041, OR: 0.679, 95% CIs: 0.468–0.985). Participants with university education level or with postgraduate degree level were less likely to share information obtained from social media on the vaccine without making sure that the information were correct (p = 0.01, OR: 0.546, 95% CIs (0.344–0.866) and (p = 0.003, OR: 0.331, 95%CIs: 0.158–0.693) . |
| Al-Hasan, et al., 2021135 | Cross -sectional/multiple regions, (North America, the Middle East, Europe, and Asia) | December 2020 and- January 2021 | Online questionnaire | 372 subjects | NR | Compared to other social media platforms (such as informational, community-based, and short video-based) that had no significant influences on vaccination intent, social media platforms for entertainment and social purposes (e.g., Whatsapp, Instagram, and YouTube) negatively influences willingness to vaccinate (p = 0.061). |
| Alley et al., 2021134 | Repeated cross-sectional study/Australia | April and August 2020 | Online questionnaire | 2343 Australian residents aged 18 years or over | Subjects have not taken the vaccine yet (it was not available) | There were no significant associations between willingness to vaccinate and social media use. |
| Allington et al., 2021133 | Cross-sectional study / UK and US | June and August 2020 | Online questionnaires | Samples from the US and the UK in June 2020 (N = 1198, N = 3890, N = 1663, N = 2237) | NR | The three studies which operationalized media usage in terms of frequency found no effect for social media. However, the study which operationalized media use in terms of informational reliance found a negative effect for social media. |
| Allington et al., 2021137 | Longitudinal study/UK | 21 November - 21 December 2020 | Online survey | 4343 UK residents, aged 18–75 | NR | Informational reliance on all social media platforms is positively correlated with vaccine hesitancy, this correlation is strongest with regards to Facebook and YouTube (rs = 0.15 and rs = 0.18, respectively) |
| Al-Marshoudi et al., 2021130 | Cross sectional study / Oman | 15–31 December 2020 | Questionnaire via telephone | 3000 randomly selected adults (66.7% Omani, 76% male, mean age was 38.27 years (SD = 10.45) | Subjects have not taken the vaccine yet (it was not available) | The majority of the participants (88%) had heard of COVID-19, and the most common source of information was social media (67%); there was a 34% rate of COVID-19 vaccine refusal by the participants, influenced mainly by friends and social media. |
| Al-Mulla et al., 2021131 | Cross-sectional study / Qatar | 3 weeks in February | Online questionnaire | 231 University students and 231 University employees/february 2021 | Subjects have not taken the vaccine yet (it was not available) | Social media had no influence in accepting or rejecting the vaccine in our cohort. |
| Aloweidi et al., 202130 | Correlational cross-sectional study / Jordan | January / February 2021 | Online self-administered questionnaire | 646 individuals of which 169 (26.2%) were males, the mean age of the studied population was 28.2 ± 10.8 years; 287 were medical field workers, and 359 non-medical personnel. | Subjects have not taken the vaccine yet, and did not have any family member who has been administered the vaccine yet | The effect of social media (OR = 1.21; 95% CIs: 1.04 to 1.41; p = 0.012) was significantly associated with the willingness to take COVID-19 vaccine once available. |
| Al-Wutayd et al., 2021132 | Cross-sectional study / Pakistan | From December 27, 2020 to March 6, 2021 | Online questionnaire on social media | 1014 participants younger than 40 years old, educated, and employed | NR | There was a non-significant association between trusting the information given by social media and vaccine hesitancy (AOR 1.37, 95% CIs: 0.92, 2.03, p = 0.118). |
| Barry et al., 2021139 | Cross-sectional study / Kingdom of Saudi Arabia | December 2020 / January 2021 | Online self-administered questionnaire | 1058 healthcare workers, 704 (66.5%) were female, 44.5% were aged 31–40, 69.6% were expatriates, 59.2% were nurses | 352 (33.27%) were enrolled to receive or had already received the vaccine | The respondents who were inclined to receive the vaccine were significantly less dependent on using social media as a source of information. |
| Berenson et al., 202141 | Cross-sectional study / Texas (USA) | November / December 2020 | Paper survey | 342 women of reproductive age, 18–45 years of age receiving care in 1 of 3 reproductive clinics in south Texas; more than half were Hispanic, mean age 29.4 years | NR | Social media was positively associated with the likelihood of accepting the vaccine if recommended by a doctor (42% of those who were likely to get the vaccine agreed that social media was an important influence compared to 29% of those who were unlikely to get the vaccine). |
| Bhagianadh and Arora 2021140 | Cross-sectional study / USA | October–November 2020 | Survey (Medicare Current Beneficiary Survey) | 5784 older adults using data from the Medicare Current Beneficiary Survey, 57% were women, 80.2% were White, 55% were older than 75 years | NR | Relative to those relying on regular news, those depending on social media, other internet/ web pages, as the main information source on COVID-19 expressed higher negative vaccine intent. Individuals with social media (OR 3.36; 95% CIs: 1.44 - 7.82) as the main COVID-19 information source were more likely to express a negative intent compared with those with regular news as their main information source. |
| Brailovskaia et al., 2021138 | Cross sectional study / China, France, Germany, Poland, Russia, Spain, Sweden, U.K., U.S. | May 2021 | Population-based online-panel surveys | 9264 participants | NR | The use of social media was a significant negative predictor in three countries (OR=0.886 for Poland, OR=0.862 for Sweden, OR=0.861 for US). |
| Burger et al., 2022117 | Longitudinal Study Design/ South Africa | February-March 2021 April-May 2021 | Questionnaire administration via telephone | Wave 4- 5629 respondents (weighted to be 48% male, mean age = 41.48 years) Wave 5 −5862 respondents (weighted to be 48% male, mean age = 41.57 years) | 2.1% of the Wave 5 sample had already been vaccinated | Those who reported trust in social media as a source of COVID-19 information (p = 0.01) were significantly more likely to be hesitant in receiving COVID-19 vaccine. |
| Citu et al., 2022118 | Cross-sectional / Romania | October -December 2021 | Online self-administered survey | 345 women in which 184 were pregnant and 161 were non-pregnant | Participants were not vaccinated against COVID-19. | The independent risk factors for hesitancy was trusting social media rumors (OR = 2.38). |
| Coughenour et al.,2021141 | Cross-sectional study / Nevada (USA) | December 21 to 28, 2020 | Telephone survey via landline telephone (n = 408) and cell phone (n = 592) | 1000 responders | NR | There was no significant association between the use of social media and vaccine hesitancy (OR=1.07, 95%CIs: 0.77–1.48, p = 0.70). |
| Cui et al., 2022119 | Cross-sectional / USA | Between April and June 2021 | Web-based questionnaire | 247 patients at 11- 28 weeks of pregnancy | NR | Participants in the low likelihood of receiving the COVID-19 vaccine group identified TV and social media to be the major sources of vaccine information (p< 0.01) |
| Dambadarjaa et al., 2021142 | Cross-sectional design/ Mongolia | 16 February 2021 and 25 March 2021 | Online survey | 2875 respondents having age 18 and over | NR | Participants who preferred social media posts and podcasts as a source of COVID-19 vaccine information were the most likely to reject the vaccine (8.7%), compared with individuals who preferred other sources. Participants who reported social media and general websites (AOR: 2.10, 95% CIs: 1.02–4.31) as sources of COVID-19 vaccine information were more reluctant to be vaccinated than those who received information from official health and government websites. |
| Fazel et al., 2021102 | Cross-sectional study / UK | 14th May and 21st July 2021 | School-based online self-report survey | 27,910 students aged 12–18 years | Non-vaccinated participants | In comparison with those who spent less than four hours on social media a day, those who spent more than four hours had increased odds of describing themselves as being undecided about a vaccination (OR=1.49, 95%CIs: 1.36–1.63, p < 0.001), or opting-out of a vaccination (OR=1.51, 95% CIs: 1.33–1.72, p < 0.001) |
| Fontenot et al., /202135 | Cross –sectional / USA | December 2020 | Online survey | 772 nursing students; the majority of participants were 18–23 years (78.8%), female (87.6%), and Non-Hispanic (NH) White (58.3%) | Unvaccinated | Consulting social media as a source of information was associated with the primary intention for vaccination (OR = 1.56; 95% CIs: 1.23–1.97). |
| Gewirtz-Meydan et al., 202233 | Cross-sectional / Israel | May to June 2021. | Online internet survey | 150 participants aged 12–18 years | Over half (64.0%) of participants had received the COVID-19 vaccine (25.5% received one dose and 38.9% two doses). | Social media use was related to a higher likelihood of being vaccinated at the bivariate level: the more time spent on social media networks the higher the odds of vaccination (OR = 1.3, p = 0.02), and specifically, use of Facebook (OR = 3.1, p = 0.004) and Instagram (OR = 2.8, p = 0.02) was related to being vaccinated; other social media platforms like TikTok, Snapchat, YouTube, and Twitter were not influential. |
| Ghaddar et al., 2022120 | Cross-sectional study / Lebanon | July–August 2020 | Mobile phone questionnaire | 1052 randomly selected participants | Unvaccinated | Trust in certain information sources (Watsapp, Facebook) reduced vaccination intent against COVID-19. |
| Ghaffari-Rafi et al., 202136 | Cross-sectional/Hawaii (USA) | Between 23 January 2021 and 13 February 2021 | Telephone survey | 363 Hawaii Pacific adult patients with neurological disorders | Unvaccinated | Multivariable logistic regression identified the best predictors of vaccine hesitancy to be, among others, social media use to obtain COVID-19 information. Participants whose primary source of COVID-19 information was from traditional media had a greater odds of vaccine acceptance (1.82, IQR: 1.02, 3.28; p = 0.042), contrary to those whose primary source was social media (0.26, IQR: 0.11, 0.63; p = 0.001 |
| Hatton et al., 2021143 | Cross sectional/ UK | December 2020 to February 2021 | Remote interview/ Online survey | 621 adults with Intellectual Disability and 48 family carers or support workers of adults with Intellectual Disability with greater needs | NR | People who got information about coronavirus from the television were 15% more likely to be willing to take a COVID‐19 vaccine (Fisher's exact p = 0.002; RR = 1.15), and people who got information from social media were 12% less likely to be willing to take a COVID‐19 vaccine (Fisher's exact p = 0.003; RR = 0.88). |
| Horiuchi et al., 2021144 | Cross sectional study/Japan | Between May 25 and June 3, 2021 | Online questionnaire on panel of the Nippon Research Center | 1200 parents who had children aged 3–14 years | NR | Those who trusted social media as a source of information were three times more likely to show no intention to vaccinate their child (OR 2.80, 95% CIs: 1.53–5.12) |
| Huang et al., 202137 | Cross-sectional / China | January and February 2021 | Online survey | Study participants included individuals aged 18 to 65 years who have been diagnosed with HIV or AIDS | Non- vaccinated participants | The overall opinion supporting COVID-19 vaccination for people living with AIDS and HIV on the internet or social media was also positively associated with willingness to receive COVID-19 vaccination (AOR 1.59, 95% CIs: 1.31–1.94; p<0.001). |
| Jabbour et al., 2022121 | Cross-sectional study/ Lebanon | 6th and 27th of June 2021 | Online Survey | 440 students, aged between 18 and 60 | NR | 121 (27.4%) of the participants described social media impacted moderately their vaccination decision. Attitude towards vaccination was higher in participants who do not trust social media (25.71 ± 5.89), when compared to those who trust social media (p= 0.038). Better attitude towards vaccination was positively associated with use of Twitter (B = 2.646, 95% CIs: 0.922–4.37; p < 0.001) and trust of people sharing posts on social media (B = 1.948, 95% CIs: 0.788–3.109; p< 0.001).It was inversely associated with Facebook use (B = −2.251, 95% CIs: 3.572 −0.929; p < 0.001) and being affected by social media (B = −0.79, 95% CIs: 1.234 −0.345; p < 0.001). |
| Jafar et al., 2022122 | Cross-sectional study / Malaysia | March 30, 2021 to April 15, 2021 | Online Google form | 1024 respondents from Sabah State | NR | Social media influence (variance = 6.38) impacted the respondents’ decisions to not participate in National COVID-19 Immunization Program. |
| Jain et al., 2021145 | Cross-sectional study / India | 2 February–7 March 2021 | Online structured questionnaire | 1068 medical students | NR | Contribution of social media as a source of information was significantly greater among vaccine-hesitant students. |
| Jennings et al., 202142 | Cross-sectional study / UK | December 2020 | Online survey | 1476 adults in the UK, aged 18–87 years | NR | Individuals who obtain more information from the Internet are more willing to be vaccinated but seeking online health information is widespread and heterogeneous. Only YouTube users were significantly less willing to be vaccinated, with a two-thirds likelihood of vaccine willingness compared to non-users. Instagram, TikTok, and Snapchat users were more hesitant, but when social media sources were disaggregated, the sample size was too small to draw firm conclusions. Facebook and Twitter users have slightly higher odds of vaccine willingness, but not significant at the 95% confidence level, and should therefore be judged with caution. |
| Lee & You 2022123 | Cross-sectional / South Korea | January 20–25, 2021 | Online self-administered survey | Among the 1016 participants, 48.8% (496/1016) were men and 51.2% (520/1016) were women, with a mean age of 47.04 (SD 15.04) years | Non-vaccinated participants | Seeking COVID-19 vaccine-related information via social medias was related to higher tendency of vaccine hesitancy (OR 1.46, 95% CIs: 1.10–1.92; p = 0.01). Higher perception on barriers of vaccination was associated with social media use (β=0.184, p<0.001). |
| Luo et al., 202131 | Cross-sectional study / China | November 2020 | Online anonymous survey | 6922 Chinese university students; around two-thirds of the sample (63.6%) were female, and their mean age was 19.4 years (SD = 1.51). | NR | Both the simple and multivariable logistic regressions found that behavioural intentions to receive free COVID-19 vaccinations was all positively associated with the frequency of passive social media exposure (AOR = 1.32, p < 0.001), the frequency of active social media interaction (AOR = 1.13, P < 0.001). Similarly, behavioural intentions to receive self-paid COVID-19 vaccinations was positively associated with the frequency of passive social media exposure (AOR = 1.44, p < 0.001), the frequency of active social media interaction (AOR = 1.28, p < 0.001). |
| Marinos et al., 2021146 | Cross-sectional study / Greece | 25 February to 13 March 2021 | Online questionnaire | The total number of physicians was 1993. Among them, 1192 (59.8%) were male and 801 (40.2%) were female. The mean age was 52.9 years (SD = 10.73). | NR | Physicians who were being informed about the COVID-19 vaccines by independent websites and social media recorded lower COVID-19 vaccination coverage than health workers who were being informed by other sources p = 0.001. |
| Mascherini & Nivakoski 2022124 | Cross-sectional study / 27 European Union Countries | February 15th to March 30th 2021 | Online structured questionnaire survey | 29,755 adult participants aged 18 years and over | Participants were not vaccinated against COVID −19 | Groups with higher vaccine hesitancy are more reliant on social media as a source of news. |
| Mir et al., 2021147 | Cross-sectional study / India | NR | Online questionnaire | 254 responders −56% of the participants were males, 38% were aged between 18 −30 years and 53% were postgraduates. | NR | Social media exposure showed an insignificant relationship on attitudes and intentions towards COVID - 19 vaccine uptake. |
| Mo et al., 2021148 | Cross-sectional study / China | November 2020 | Online anonymous survey | 6922 Chinese university students; around two-thirds of the sample (63.6%) were female, and their mean age was 19.4 years (SD = 1.51). | NR | Social media use for COVID-19 vaccine information had significant association with the intention to receive the COVID-19 vaccination (free) (β = 0.06, p < 0.01), but no association with the intention to receive the COVID-19 vaccination (self-paid). |
| Mose et al., 2022125 | Cross-sectional study / Ethiopia | March 1 to 30, 2021 | Online questionnaires | 420 medical and health science students of Wolkite University249 (59.3%) of study participants were male. 324 (77.1%) were aged between 19 and 23 years | Not vaccinated | The odds of COVID-19 vaccine hesitancy among medical and health science students who had received information about the COVID-19 vaccine from social media were approximately 2.7 times more likely than those who had received information about the COVID-19 vaccine via television/radio (AOR = 2.68, 95% CIs: 1.58–4.54). |
| Nur Karabela et al., 2021149 | Cross-sectional and correlational study/Turkey | Period between February 01, 2021 and February 28, 2021 | E-survey link via Google forms- there is used tool Perception of Causes of COVID-19 (PCa-COVID-19) Scale | 1216 subjects, aged 35.9 ± 12.3 years. 62.5% women, 59.0% married, and 62.1% university graduates | NR | The source of information trusted most was YouTube for the participants who stated that they would be vaccinated, WhatsApp groups for the ones who stated that they would not be vaccinated and social media for the participants who stated that they were undecided. |
| Othman et al., 2022126 | Cross sectional / Saudi Arabia | June 17 to June 19, 2021 | Three-part online questionnaire | 504 participants of the general population | A total of 335 of 504 individuals had already received the vaccine | Basing the decision to be vaccinated on social media information was found to significantly influence vaccination acceptance (OR = 0.260, p= 0.006). |
| Ouyang et al., 2022127 | Cross-sectional / China | April 10 to April 14, 2020. | Questionnaires | 463 participants in mainland China | NR | Frequency of social media use (for lack of confidence r = −0.14, p < .01; for risk r = −0.17, p < .001), diverse use of social media (for lack of confidence r = −0.14 p < 0.01), media trust (for lack of confidence r = −0.62 p < 0.001; for risk r = −0.56, p < .001) were significantly correlated with COVID-19 vaccine hesitancy. |
| Park et al., 2021150 | Cross-sectional study / USA | October / November 2020 | Survey (Medicare Current Beneficiary Survey) | 6478 Medicare beneficiaries from the Fall 2020 Medicare Current Beneficiary Survey COVID-19 Supplement, 42.4% were older than 75, 55.9% were women, 76.3% were non-Hispanic white | NR | Compared to those relying on traditional news sources as their primary source of COVID-19 information, the likelihood of COVID-19 vaccine uptake was significantly lower among those relying on social media (OR = 0.40, 95% CIs: 0.25–0.65). |
| Piltch-Loeb et al., 2021151 | Cross-sectional study /USA | Between December 13 and 23, 2020 | Online survey via mobile devices on the Pollfish survey platform | 2650 responders in a vaccine priority group at the time the survey was administered [ healthcare workers (61.4% of participants) and, per CDC guidance, essential frontline workers | Not vaccinated | There was a clear decrease in acceptance if individuals exclusively used social media (RRR 0.45, 95%CIs: 0.32–0.64) or used both social media and traditional media channels (RRR 0.81, 95% CIs: 0.66–1.00) compared to those who only used traditional media. |
| Rad et al., 2022128 | Cross-sectional study / Iran | May - July 2021 | Online questionnaire | 2556 people participated in the study with a mean age of 37.76 (10.7) years (age range = 18–75) | Participants were not vaccinated against COVID-19 | The use of social media (β = 0.050, 95% CIs: 0.004, 0.648; p= 0.043) predicts the intention to receive the COVID-19 vaccine. |
| Reno et al., 2021156 | Cross-sectional study/ Italy | January 2021 | Online survey | 1011 citizens from the Emilia-Romagna region in Italy | Not vaccinated | There was a strong positive relationship between social media use and vaccine hesitancy (p< 0.001). |
| Riad et al., 2021152 | Cross-sectional study / International (22 countries) | February 2021 | Online questionnaire | 6639 students; 4682 (70.5%) were females, the mean age of participants was 22.06 ± 2.79 (17–40) years | NR | Globally, the dependence on media and social media to inform vaccine-related decisions was significantly (p< 0.01) associated with a decreased level of vaccine acceptance (3.71±1.21). |
| Riad et al., 2021155 | Cross-sectional study / Czech Republic | August–October 2021 | Onsite self-administered questionnaire/ online self-administered questionnaire | Out of the 362 included participants, 278 were pregnant, and 84 were lactating women. The participants’ mean age was 31.48 ± 4.56 (19–44) years old, and their median age was 31 years old. | Non-vaccinated participants | The impact of media/social media on participants’ decisions about the COVID-19 vaccine was reported by only 8.3% of the participants. |
| Riad et al., 2021155 | Cross-sectional study/ Czech Republic | Between 21 April and 15 June 2021 | Self-administered questionnaire | 1351 University students | Not vaccinated | The students who depended on media and social media were 3.086 times (95% CIs: 1.928–4.941, p < 0.001) more likely to be vaccine-hesitant. |
| Romer and Jamieson, 2021153 | Cross-sectional study / USA | March of 2020 and again in July 2020 | Online questionnaire | 840 participants from a national US probability sample, 55.6% were women, 31% were older than 60, 74.7% were White | NR | Use of social media in March was also predictive of vaccination in July, with an overall negative indirect relation of –0.041, 99% CI –0.071 to –0.014. However, this relation as mediated by change in conspiracy beliefs was weaker than for the other media, with only about 39% (–0.016/–0.041) attributable to this source (–0.016, 99% CIs –0.035 to –0.001). |
| Ruiz and Bell, 2021154 | Cross-sectional study / USA | June 2020 | Online questionnaire | 804 compensated English-speaking adults residing in the US, 53.6% were women, 65.3% were White, the age range was distributed evenly in the sample | NR | Respondents relying on social media for information about COVID-19 anticipated a lower likelihood of COVID-19 vaccine acceptance. |
| Sallam et al., 2021157 | Cross-sectional study / Jordan | January 2021 | Online-based survey | 1106 students, 75.3% were older than 21, 75% were Jordanian | NR | Dependence on social media platforms was significantly associated with lower intention to get COVID-19 vaccines (19.8%) compared to dependence on medical doctors, scientists, and scientific journals (47.2%, p < 0.001). |
| Sheiner et al., 2021158 | Cross-sectional study / Israel | NR | Self-administered online survey | 484 participants were included in which 57% females and 43% males. The age of participants ranged from 18 to 55 years (M = 36.6, SD = 10.6). | Among the total participants, 41% were vaccinated against the COVID-19. | Social media trust has a direct negative relationship with attitude toward vaccination (β = −0.18, p < 0.001). People who believe that social media is a credible information source were negatively influenced toward COVID-19 vaccination and formed a negative attitude toward the vaccination. |
| Šiđanin et al., 2021164 | Cross-sectional study/ Serbia | From 6 to 26 July 2021 | Electronic questionnaire created via the Google Forms platform, distributed via email, Facebook and Viber | 345 students at the University of Novi Sad; average age of the respondents was 23 years | 42% of students had not been vaccinated and did not plan to do so, 37.4% had received at least one dose of vaccine and 20.6% had not been vaccinated even though they planned to do so | There was no difference in the level of confidence in social media (p = 0.69) between the two groups of students depending on their decision to get vaccinated. |
| Silva et al., 202234 | Cross-sectional study / Portugal | April and May 2021 | Telephonic interview | 605 older adults (≥65 years old) | More than 65% of the older adults were already vaccinated against COVID-19, and around 3.3% did not want or had no intention to get the vaccine. | Older population trusts the information released by the social media (OR = 0.34) leading to a decrease in vaccine hesitancy and refusal. |
| Singh et al., 2021160 | Cross-sectional/ Hong Kong | May 1–31, 2021. | Web-based survey | 245 South Asian people aged 18 years or older | 81 participants were vaccinated | Higher exposure to information about deaths and other serious conditions caused by COVID-19 vaccination on social media was associated with lower uptake (AOR 0.54, 95% CI 0.33–0.86; p = 0.01). |
| Sirikalyanpaiboon et al., 2021159 | Cross-sectional study design/ Thailand | March 31,2021 to April 30, 2021 | Google-service based survey | Physicians (N = 705) working at the Chulalongkorn University, Bangkok, Thailand | NR | Physicians who received information from the hospital channel had a significantly higher rate of being Acceptors (p < 0.01), while those who received information primarily through social media were slightly less likely to be Acceptors (p = 0.04). |
| Strathdee et al., 2021161 | Correlational cross-sectional study / US- Mexico border region | October2020 and September 2021 | Interviewer-administered surveys at baseline and approximately one week later computer-assisted personal interviews | 393 participants aged ≥ 18 years who injected drugs within the last month | 7.6% of the total sample (N = 393) had received at least 1 dose by 10 September 2021. | Citing social media as one's most important source of COVID-19 information were independently associated with vaccine hesitancy. |
| Tan et al., 2022129 | Longitudinal study / Singapore | Modules fielded in August and November 2020, and June 2021 | Self-administered survey/ Telephonic interview | Data from a nationally representative panel survey of Singaporeans aged 56–75 (Sample I N = 6094, (Sample II N = 5677) was utilized | Vaccinated with one dose (86% of the total participants from sample I and 87% of the total participants from sample II) | Social media only slightly predicted vaccination status (p = 0.09), with those who placed greater trust in social media being less likely to have received at least 1 dose of the vaccine. |
| Wang et al., 2021163 | Cross-sectional study / China | October to November 2020 | Online survey | 1332 health workers who had at least one child under the age of 18 years | NR | Higher frequency of information exposure through social media (AOR: 1.08, 95% CI: 1.04, 1.13, p < .001) and interpersonal communication (AOR: 1.24, 95% CI: 1.15 −1.34, p < .001) related to COVID-19 vaccination were associated with higher parental acceptability of COVID-19 vaccination. |
| Xin et al., 202138 | Cross sectional study / China | 9 October to 26 November 2020, | Online survey | 1902 nurses in which 96.7% were females. The mean (standard deviation (SD)) age of this sample was 31.72 (6.74). | Non-vaccinated participants | Frequent social media exposure and interpersonal discussion were positively associated with vaccination intentions (social media exposure: β = 0.88 to 0.89; interpersonal discussion: β = 0.80 to 0.82; p < 0.001). |
| Zhang et al., 2020165 | Cross-sectional study / Shenzhen, China | September 2020 | Online questionnaire | 1052 factory workers who had at least one child under the age of 18 years | Subjects have not taken the vaccine yet (it was not available) | Higher exposure to positive information related to COVID-19 vaccination was associated with higher parental acceptability of COVID-19 vaccination (AOR 1.35, 95% CI: 1.17–1.56). Higher exposure to negative information related to COVID-19 vaccination was negatively associated with the dependent variable (AOR 0.85, 95% CIs: 0.74–0.99). |
| Zhang et al., 2021162 | Cross-sectional study / Shenzhen (China) | September 2020 | Online survey | 2053 full-time employees 18 years or older who worked in factories in Shenzhen, over half of the participants were younger than 40 years (n = 1490, 72.6%), were female (n = 1179, 57.4%), were married (n = 1455, 70.9%), had children (n = 1466, 71.4%) | NR | Frequency of exposure to positive information related to COVID-19 vaccinations on social media was positively correlated with positive attitudes (r = 0.083; p<0.001), perceived subjective norm (r = 0.101; p<0.001), and perceived behavioral control (r = 0.064; p = 0.004) related to a COVID-19 vaccination. A negative correlation was found between social media exposure and negative attitudes toward a COVID-19 vaccination (r=–0.090; p<0.001). |
Abbreviations: NR – not reported; OR – odds ratio; CI – confidence interval; SD – standard deviation; AOR – adjusted odds ratio; RR – risk ratio.
The other 3 categories of studies mainly focused on some specific (or several specific) social networks. Notably, Twitter was the predominant site utilized in these studies - 62 out of 94 studies that analyzed COVID-19 vaccination social media content used solely Twitter as the main source of data. These studies also used tools for data extraction (such as R libraries to assess the Twitter premium application programming interface service and collect the posts). Some of the studies focused on posts obtained from a specific location, thereby exploring the state of mind of one population, while others did not focus their analysis on any geographical basis. Almost all studies scraped posts published by the users, some studies focused on organizations,28,29 while there were several studies that analyzed users’ comments posted on news media pages.
Quality of the included studies
Out of total of 155 studies, quality was evaluated only in cross-sectional (n = 61, Supplementary Table S3). It should be noted that the study published by Luo et al., 2021 and Mo et al., 2021 are separate records of the same study, thus we reported only the quality of the study reported by Luo and colleagues. Overall, the quality of the cross-sectional studies was moderate – 2 studies received 10 stars, 5 studies received 9 stars, 9 studies were evaluated with 8, 12 studies with 7, 16 studies with 6, 11 studies with 5, and 6 studies with 4 stars.
The associations between social media use and vaccine hesitancy/acceptance
The main results and characteristics of studies assessing the relationship between vaccine intentions-attitudes and utilization of social media are presented in Table 1. The studies reported variable conclusions, however, the number of studies that observed a negative association between social media use and vaccine acceptance was higher.
One group of studies found a direct positive association between the utilization of social media and vaccine acceptance, with 2 of the reports referring to the same study.30, 31, 32, 33, 34, 35, 36, 37, 38 These positive results were observed among a young population divided into medical and non-medical personnel, with the majority of them being women (mean age of 28 years), among nursing students aged 18–23 years, participants aged 12–18 years, among older adults (older than 65 years), adult patients with neurological disorders, adults who have been diagnosed with HIV or AIDS, young nurses. Interestingly, parents who were healthcare workers and were more reliant on social media were also more inclined towards vaccinating their children against COVID-19.39 There were also studies that reported a positive indirect association between social media utilization and vaccine acceptance. For example, Zhang et al.,40 observed that the association between social media usage and attitudes toward vaccination depends on the type of content the individuals are exposed to (positive content was positively associated with the intention to vaccinate and vice versa), as observed in their sample of factory workers. Another study highlighted the importance of doctors as social media influencers, which was also positively associated with higher vaccine acceptance, as observed in a study conducted on women of reproductive age.41
There was the group of studies that did not observe any effect of social media exposure on the intention to vaccinate against COVID-19 (n = 8). The rest and the great majority of the studies (n = 41) reported that social media imposed a negative impact on the participants' intention to vaccinate. These negative associations were confirmed among all age groups of people, originating from different geographical locations from all continents (except Australia), and who were characterized as either students (medical and non-medical), healthcare workers, the general population, women of reproductive age, pregnant women, Medicare beneficiaries. Finally, Jennings and co-workers distinguished the different types of social media and their relations with vaccine acceptance. Compared with non-users, YouTube users showed a lower willingness, while those relying on Facebook and Twitter showed a higher intention to receive the COVID-19 vaccine.42
Themes emerging from discussions among social media users
The summary characteristics and results from studies that analyzed posts extracted from social media are presented in Table 2. The first category of studies reported the most frequent topics relating to discussions about vaccines, which were predominantly classified as hesitant attitudes (n = 29). The most frequently discussed reasons against COVID-19 immunization on social media platforms include: concerns regarding the safety of the vaccine,43, 44, 45, 46, 47, 48 concerns regarding the efficacy of the vaccines,46,49, 50, 51 the fast pace of vaccine approval,46,51, 52, 53 the long-term health implications as well as the side effects,52,54,55 distrust in the efficacy of the vaccines within the context of rapidly emerging mutant viruses,46,52 distrust in the production and transport of the vaccines,56,57 and controversy around the vaccines’ ingredients (toxins, mercury).43 Topics categorized as misinformation58 and conspiracies were also frequent and included population control via microchips that was planned by Bill Gates,46,52,54 adverse effects of vaccination such as cancer and sterility, and many more.52 A few studies reported themes such as distrust in government and their activities in handling the pandemic, as well as distrust in major health regulatory bodies (e.g., Food and Drug Administrationor Centers for Disease Control and Prevention).45,49,57 Topics that were discussed as providing justification against vaccination and were related to COVID-19 specifically included considerations that the severity of the disease was not so high,59 comparisonswith other diseases (such as Ebola or H1N1), as well as the opinion that one does not belong to the category that is athigher risk of more severe symptoms.46,54 Apart from vaccine-hesitant topics, a few studies identified those that support the current immunization campaign, and the reported reasons are mainly trust in science and healthcare professionals, trust in vaccine as a solution,29 the reliance on peer-reviewed publications for making informed decisions.51 Finally, there were several studies that were not geo-located that explored vaccine-related topics in general that reported noteworthy observations. Namely, the peaks of the topics were affected by the events reported by the media and posted on social media.60 Further, vaccine-supportive tweets showed temporal variations over time, while those related to barriers remained mainly constant through time.61 After conducting the updated search,we were able to locate new studies that focused social data mining on specific regions, thereby providing more insights into themes that were specific to a certain location. However, the topics identified as vaccine-hesitant were unique regardless of the location – such as mistrust into the manufacturing process, science, and reliance on conspiracy theories in Turkey,62 distrust in the scientific and manufacturing process in China,63 non-necessity of the vaccine, concerns over safety and side effects, in Canada.29 These topics were mainly identified through our initial search conducted up to September 2021, and we could observe that themes that were discussed by the public and were oriented against vaccination were repetitive throughout different geographical locations throughout different study periods. Furthermore, eighteenstudies reported different topics providing a difference between the anti- and pro-vaccination discussions. One group of studies focused on describing the discussions and reasons provided by the opposing parties - vaccine refusers mainly focused on side effects and safety coupled with conspiracy theories and misinformation.64, 65, 66, 67, 68, 69 Alternatively, vaccine supporters believed that the immunization would help return life to normal and it gave them hope in ending the pandemic, as well as provided a sense of safety.53,70, 71, 72, 73 The second group of studies focused on exploring the strategies employed by these two opposing communities. The anti-vaccination community was described as spreading misinformation, spinning conspiracies andinstigatinghysteria.74 It was also described as spreading a non-focused discussion thereby appealing to a wider range of groups (for example, by providing suggestions for alternative remedies for those seeking them).75 Johnson and co-workers observed that anti-vaccination clusters are better connected with the undecided clusters in the main online network, while pro-vaccination clusters remain peripheral. Thus, theanti-vaccination clusters predict their domination in a decade, as observed from the analysis of posts obtained from Facebook pages.76 On the other hand, pro-vaccination communities reportedly act by trying to convince skeptics by touting prior successes of immunizations and expressing concern because of the rise of “anti-vax” movement on Facebook and Twitter, however they also mock and make insults of anti-vax communities in disrespectful and derogatory tones.74,77 Again, anti-vaccination communities were regarded as being better connected than pro-vaccination clusters, as suggested by the comparison of the social features of their tweets.74 When one study analyzed the 2000 most active Twitter accounts in the vaccine discourse from 2019, it reported that up to 45% were identified as opposing vaccination, while only 24% were in favor.71 Finally, one study provided an insight about what type of actor is behind the anti-vaccination movement.78 identified that it was primarily led by political and non-medical Twitter users, with less than 10% of these users being from the medical community. This also points to that problem of health care professionals’ inactivity in addressing COVID-19 misinformation and spreading scientific evidence in order to combat this issue. Specifically in Turkey, an analysis of pre and post COVID-19 tweets showed that the number of anti-vaccine supporters was 22 greater than of those who are pro-vaccine, and the increase in the number of anti-vaccination supporters after COVID-19 has begun was huge (from 1.7% to 26.51%).79 One study pointed to the fact that Donald Trumpwas the main driver of vaccine misinformation on Twitter, before his profile was suspended.80 On the other hand, an analysis of tweets containing #yomevacuno hashtag found that healthcare professionals comprise only 11.38% of users, generating only 6.35% of impressions, and that although the traffic information produced by them is not significant compared with institutions it is compared with regular users.81
Table 2.
Summary characteristics of studies that reported public opinions/discussions generated on social media platforms.
| Topics identified from predominantly vaccine-hesitant discussions | |||||
|---|---|---|---|---|---|
| Reference | Location | Study period | Study content | Social media utilized | Main results |
| Baines et al., 202154 | No location restrictions | November 2020 - January 2021 | Public posts | Parler | (1)Reasons to refuse the COVID-19 vaccine (40%) - justifications with hesitancy statistics, no scientific reasons; (2)side effects of the COVID-19 vaccine (28%) - possible adverse reactions such as getting Bell's Palsy or even dying; (3)Population control through the COVID-19 vaccine (23%) - Bill Gates and Dr. Anthony Fauci using microchips; (4) Children getting vaccinated without parental consent (5%), (5) comparison of other health issues with COVID-19 (2%) - with other pandemics such as H1N1 and Ebola |
| Baj-Rogowska 2021169 | Poland | 1st to 30th May 2021 | Public posts in Polish language | Covid-19 vaccine acceptance depends mostly on the characteristics of new vaccines (i.e. their safety, side effects, effectiveness, etc.), and the national vaccination strategy (i.e. immunization schedules, quantities of vaccination points and their localization, etc.), which should focus on increasing citizens’ awareness, among various other factors. | |
| Bi et al., 202163 | China | December 2020 to April 2021 | Public posts | Douban platform | Topics around the negative attitude had the highest number of opinions, with a total of six kinds - the idea that the vaccine is “not yet mature and will have many side effects,” “the validity period of only six months is too short,” “clinical trials are only going into phase three,” “other vaccines are being used, or I have a fear of any vaccine,” “the current method for controlling the situation in China is safer, so I think it is unnecessary to be vaccinated,” and “I have relevant medical history, and it is not convenient for me to be injected with vaccines.” The main attitudes of this positive view are “The vaccine has no side effects or the side effects are small,” “the country currently implements free vaccination,” “the sample size of injections is already large,” “the vaccine is an inactivated vaccine and thus very safe,” and “everyone meets the requirements. People with conditions should be vaccinated to achieve herd immunity.” |
| Bonnevie et al., 202043 | USA | Comparison of data obtained from the four months prior to the COVID-19 increase in the USA (15 October 2019–14 February 2020) to the subsequent four months (15 February 2020–14 June 2020) | Public posts | (1)Negative health impacts of vaccination (SIDS, autism, etc.); (2)Pharma industry: overall, or a specific pharmaceutical company; (3)Policies & Politics: related to state or national vaccine requirements such as ColoradoSB163; (4) Vaccine Ingredients: within vaccines, such as toxins, mercury, or lead; (5)Federal Health Authorities: such as the Centers for Disease Control and Prevention, Food and Drug Administration; (6)Research & Clinical Trials: related to vaccines, such as studies showing negative health outcomes; (7)Religion: in reference to vaccination or vaccine exemptions; (8)Vaccine Safety: Concerns or questions around the safety of vaccines; (9)Disease Prevalence: predominantly around vaccine-caused diseases; for example, vaccine-derived poliovirus; (10)School: School grades or levels, homeschooling or vaccine requirements; (11) Family: The impacts of vaccination on family members. There was a decrease in opposition conversation from 1st to the 2nd time point in themes 1–3, 7–11, and an increase in 4–6 | |
| Boucher et al., 202144 | NR | November 2020, after the announcement of initial COVID-19 vaccine trials | Public posts (English and French) | Vaccine hesitancy topics: safety, efficacy, and freedom, and mistrust in institutions, safety and efficacy of mRNA technology and side effects. Nearly one-third (45,628/146,191, 31.2%) of the conversations on COVID-19 vaccine hesitancy clusters expressed concerns for freedom or mistrust of institutions (either the government or multinational corporations) and nearly a quarter (34,756/146,191, 23.8%) expressed criticism toward the government's handling of the pandemic. | |
| Criss et al., 202158 | NR | From October 2020 to January 2021 | Public posts | The tweets revealed vaccine support through vaccine affirmation, advocacy through reproach, a need for a vaccine, COVID-19 and racism, vaccine development and efficacy, racist vaccine humor, and news updates. Vaccine opposition was demonstrated through direct opposition, vaccine hesitancy, and adverse reactions. Conspiracy and misinformation included scientific misinformation, political misinformation, beliefs about immunity and protective behaviors, and race extermination conspiracy. Equity and access focused on overcoming history of medical racism, pointing out health disparities, and facilitators to vaccine access. Representation touted pride in development and role models, and politics discussed the role of politics in vaccines and international politics. | |
| Engel-Rebitzer et al., 202228 | USA | Between February 01, 2020, and December 11, 2020 | 14,519 tweets generated by 1463 state legislators and 521 federal legislators | The topics with the highest percent topic representation were (1) Operation Warp Speed success; (2) vaccine effectiveness; (3) COVID-19 vaccine updates; (4) COVID-19 relief package content; and (5) non-pharmaceutical interventions as a bridge to vaccines. | |
| Ginossar et al., 2022166 | NR | Between 1 February and 23 June 2020 | 930,539 unique tweets in English that discussed vaccinations posted out of which links to 2097 unique YouTube videos that were tweeted were identified and analyzed | YouTube videos posted on Twitter | Following the World Health Organization's declaration of the COVID-19 outbreak as a public health emergency of international concern, anti-vaccination frames rapidly transitioned from claiming that vaccines cause autism to pandemic conspiracy theories, often featuring Bill Gates. Content analysis of the 20 most tweeted videos revealed that the majority (n = 15) opposed vaccination and included conspiracy theories. Their spread on Twitter was consistent with spamming and coordinated efforts. These findings show the role of cross-platform sharing of YouTube videos over Twitter as a strategy to propagate primarily anti-vaccination messages. |
| Griffith et al., 2021170 | Canada | December 2020 | Public posts | Vaccine hesitancy themes: concerns over safety, suspicion about political or economic forces driving the COVID-19 pandemic or vaccine development, a lack of knowledge about the vaccine, anti-vaccine or confusing messages from authority figures, and a lack of legal liability from vaccine companies. This study also examined mistrust toward the medical industry not due to hesitancy, but due to the legacy of communities marginalized by health care institutions. | |
| Guntuku et al., 2021171 | USA | Between December 1, 2020 and February 28, 2021 | Public posts | Urban suburbs posted about equitable distribution in communities, college towns talked about in-clinic vaccinations near universities, evangelical hubs posted about operation warp speed and thanking God, exurbs posted about the 2020 election, Hispanic centers posted about concerns around food and water, and counties in the ACP African American South posted about issues of trust, hesitancy, and history. The graying America ACP community posted about the federal government's failures; rural middle American counties posted about news press conferences. Topics related to allergic and adverse reactions, misinformation around Bill Gates and China, and issues of trust among Black Americans in the healthcare system were more prevalent in December, topics related to questions about mask wearing, reaching herd immunity and natural infection, and concerns about nursing home residents and workers increased in January, and themes around access to black communities, waiting for appointments, keeping family safe by vaccinating and fighting online misinformation campaigns were more prevalent in February. | |
| Herrera-Peco et al., 202156 | NA | December 2020 | Public posts written in Spanish language, under the hashtag #yonomevacuno | Vaccine hesitancy topics: 1) vaccines are not safe (63.36% of tweets), 2) the vaccine effectiveness is questionable (8.9%), and 3) vaccines are business (8.7%), as well as 4) tweets which divulged unverified information framed as beliefs about the effect and even the production and transport of the vaccines (18.83%). | |
| Hou et al., 202157 | New York (United States), London (United Kingdom), Mumbai (India), and Sao Paulo (Brazil), and Beijing (China) | June/July 2020 | Posts from Twitter from New York (United States), London (United Kingdom), Mumbai (India), and Sao Paulo (Brazil), and Sina Weibo posts from Beijing (China) | Twitter and Sina Weibo (Chinese version of Twitter) | Hesitancy topics: New York - a lack of confidence in vaccine safety, distrust in governments and experts, and widespread misinformation or rumors; Mumbai, São Paulo, and Beijing - vaccine production and supply; New York and London - vaccine distribution and inequity. Negative tweets expressing lack of vaccine confidence and misinformation or rumors had more followers and attracted more public engagement online. |
| Hughes et al., 2021172 | NR | NR | Public posts and videos | YouTube, Twitter, Facebook and Instagram | This study identified twenty-two narrative tropes coded, out of which, four key common narrative tropes were: (1) “Vaccine Injury'' - these injuries were often vaguely described and only infrequently accompanied by claims to an actual diagnosis of malady. (2) “Corrupt Elite” - this offered a standard populist appeal in which an innocent put disempowered “silent majority” suffer under the tyranny of a powerful and corrupt minority) (3) “Heroes and Freedom Fighters” - presenting anti-vaccine or COVID-denialist medical doctors (as well as chiropractors and naturopaths) as brave whistleblowers, risking their reputations and careers by speaking truth to power) and (4) “Sinister Motives.” Of the sixteen rhetorical strategies coded, four key, common rhetorical strategies were: (1) the “Brave Truth Teller,” (2) “Do Your Own Research (DYOR)” - DYOR works by trying to empower the audience to develop their own bodies of evidence and methods of reasoning in order to reach a preordained conclusion; (3) “Mountains and Molehills” - in this rhetorical strategy, vaccines’ risks and benefits are presented without a proper sense of proportion) and (4) “A Global Movement/Sleeping Giants” - honest, everyday citizens who are on the cusp of rising up against an oppressive “global elite”—was a common rhetorical strategy that cut across narratives targeting all categories of antagonists. |
| Jacobs et al., 202148 | NR | Between January 1, 2020 and May 1, 2020 | Public posts | Personal freedom was the most prevalent theme, followed by vaccine safety and private/government involvement. | |
| Jiang et al., 2021173 | USA | February 21 to March 20, 2020 | Public posts | Seven major topics - 26.3% (26,234/100,209) of the tweets as News Related to Coronavirus and Vaccine Development, 25.4% (25,425/100,209) as General Discussion and Seeking of Information on Coronavirus, 12.9% (12,882/100,209) as Financial Concerns, 12.7% (12,696/100,209) as Venting Negative Emotions, 9.9% (9908/100,209) as Prayers and Calls for Positivity, 8.1% (8155/100,209) as Efficacy of Vaccine and Treatment, and 4.9% (4909/100,209) as Conspiracies about Coronavirus and Its Vaccines. Different themes demonstrated some changes over time, mostly in close association with news or events related to vaccine developments. Twitter users who discussed conspiracy theories, the efficacy of vaccines and treatments, and financial concerns had more followers than those focused on other vaccine themes. | |
| Klimiuk et al., 202147 | Poland | May/July 2019 | Public comments posted to a leading Polish vaccination opponents’ Facebook page | Out of 18,685 comments analyzed, 4042 contained the following themes: conspiracy theories (28.2%), misinformation and unreliable premises (19.9%), content related to the safety and effectiveness of vaccinations (14.0%), noncompliance with civil rights (13.2%), own experience (10.9%), morality, religion, and belief (8.5%), and alternative medicine (5.4%). There were also 1223 pro-vaccine comments, of which 15.2% were offensive, mocking, or non-substantive. | |
| Küçükali et al., 202262 | Turkey | Between 9 December 2020 and 8 January 2021 | Public posts | 90.5% of the tweets were about vaccines, 22.6% (n = 213) of the tweets mentioned at least one COVID-19 vaccine by name, and the most frequently mentioned COVID-19 vaccine was CoronaVac (51.2%). 22.0% (n = 207) of the tweets included at least one anti-vaccination theme. Poor scientific processes (21.7%), conspiracy theories (16.4%), and suspicions towards manufacturers (15.5%) were the most frequently mentioned themes. The most co-occurring themes were “poor scientific process” with “suspicion towards manufacturers” (n = 9), and “suspicion towards health authorities” (n = 5). | |
| Lee et al., 2021174 | NR | November 1, 2020, to November 16, 2020 | Public posts | Nine topics were identified from the LDA topic modeling approach comprising T1: Administration of local vaccine program, T2: Complementary measures to vaccine, T3: Social aspects of vaccine, T4: Efficacy of vaccine, T5: Global distribution and access of vaccine, T6: Myths about vaccine, T7: Legal and economic aspect of vaccine, T8: Pace of vaccine development and T9: Political aspects of vaccine. There were temporal differences in the nine topics depending on the events. | |
| Liew and Lee, 202161 | NR | 11-week period after November 18, 2020, following a press release regarding the first effective vaccine | Public posts | Tweets related to COVID-19 vaccines were posted by individuals around the world (N = 672,133). Six overarching themes were identified: (1) emotional reactions related to COVID-19 vaccines (19.3%), (2) public concerns related to COVID-19 vaccines (19.6%), (3) discussions about news items related to COVID-19 vaccines (13.3%), (4) public health communications about COVID-19 vaccines (10.3%), (5) discussions about approaches to COVID-19 vaccination drives (17.1%), and (6) discussions about the distribution of COVID-19 vaccines (20.3%). Tweets with negative sentiments largely fell within the themes of emotional reactions and public concerns related to COVID-19 vaccines. Tweets related to facilitators of vaccination showed temporal variations over time, while tweets related to barriers remained largely constant throughout the study period. | |
| Liu and Liu 202153 | NR | November 2020 | Public posts | Theme regarding capability: lack of users’ knowledge about the COVID-19 vaccines and influence by misinformation (such as alteration of DNA by mRNA vaccines, causing sterility, containing microchips, etc.); concern about side effects/long term health implications. Physical opportunities category - lack of will to pay for the vaccine, refuse mandatory vaccination, concern over availability of information. Behavioral intentions category - consideration that the disease was not severe or life-threatening and the vaccine was not effective (because of low efficiency and mutation of the virus), consideration that the rushed vaccine to be more harmful than COVID-19. | |
| Monselise et al., 202160 | NR | Exactly 60 days starting from December 16, 2020 | Public posts | 12 important topics were selected for analysis. The 3 most important topics with the highest topic ratio were “Vaccination of Frontline Workers,” “Access of Vaccines–Signing Up Online,” and “South African Variant.” The other topics were mostly related to the concerns about the vaccines as well as their supply and distribution. There were also topics related to the stimulus plan, profits of pharmaceutical companies, and conspiracy theories. Through the trend analysis, it was found that the peaks of the topics were impacted by the events reported in the news and spread through social media. | |
| Shim et al., 202150 | Korea | February - March 2020 | Public posts | Identified topics: vaccine hesitancy” - the most frequent topic with a 14.2% relative weight; followed by “development of vaccine” (13.1%) and “quarantine prevention policy” (13.0%); “efficacy of vaccination” (12.6%), “priority vaccination of hospital workers” (12.0%), “media on COVID-19 vaccines” (11.9%), “medical association's response” (11.8%), and “adverse reactions” (11.4%) | |
| Tang et al., 202129 | Canada | Between July and September 2020 | Public posts on the Twitter and Facebook accounts of six Canadian news organizations | Twitter and Facebook | Four main themes were identified: 1) COVID-19 vaccine safety and efficacy concerns; 2) conspiracy theories stemming from mistrust in government and other organizations; 3) a COVID-19 vaccine is unnecessary because the virus is not dangerous; and 4) trust in COVID-19 vaccines as a safe solution. Theme 1 captured concerns about perceived factors that may influence the safety and efficacy of the vaccine including political pressures, development speed and testing, ingredients and potential immune-escaping variants. Theme 2 characterized the conspiracy theories, including microchips and changes to DNA, expressed on social media rooted in a general mistrust of government and organizations involved in COVID-19 vaccine development. Theme 3 captured the level of concern related to the perceived seriousness of becoming infected with COVID-19 expressed on social media. Commenters felt that severity was being over exaggerated and a healthy immune system was sufficient to overcome the virus. A minority of commenters expressed confidence in COVID-19 vaccines to prevent infection. Those with confidence in the vaccine conveyed trust in science and their healthcare professional, expressed concerns about potential long-term COVID-19 effects and felt that the vaccine was necessary to return to normal. |
| Thelwall et al., 202146 | Most of the tweets with a user declaring a location (80%) were from the USA, UK and Canada. | March - December 2020 | Public (vaccine hesitant) posts | The three major vaccine hesitation topics on Twitter accounted for half (50.2%) of the 446 tweets manually categorised: conspiracies (23.5%), development speed (16.1%) and safety (10.5%). Conspiracies - microchips, population control; development speed - due to the fast pace of vaccine approval, users considered it unsafe. Category efficacy - users argued that it is pointless to receive the vaccine as they belong to a low risk category of COVID-19 symptoms, thus not considering the fact of transmission, other doubt in the efficacy due to the mutation of the virus. Surprisingly, a substantial minority of tweets were simple statements that the tweeter would not take a Covid-19 vaccine, without giving a reason. Of the 117 vaccine hesitant tweeters, most (67) mentioned the deep state concept in at least one of their tweets and a further 12 tweeted general right-wing politics. A few focused on (Christian) religion (3), frequently tweeted anti-vaxxer sentiments (6), anti-lockdown (3) or anti-abortion (1). | |
| Tsao et al., 2022167 | Canada | From December 5, 2020, to March 6, 2021 | Public posts (569,467 from Toronto and 141,469 from Ottawa) | 6 topics emerged - opinions toward COVID-19 vaccine approval, access, availability, etc.; impacts of the COVID-19 on life; reviews, supports, and impacts of the COVID-19 pandemic on businesses, markets, and economics; opinions toward the second lockdown; opinions toward wearing masks; things happened in Ontario. There were temporal variations in the sentiments of the topics, depending on some key events (such as Christmass, vaccine accessibility etc.). | |
| Wong et al., 202151 | NR | 16 November 2020 | 3652 comments from the two BBC postings and 1728 comments from CNN were extracted from Instagram. A total of 4325 comments from a BBC posting on Facebook were extracted | Instagram and Facebook - comments from CNN and BBC pages | The analyses uncovered several major issues concerning COVID-19 vaccine hesitancy. The production of the COVID-19 vaccine at an unprecedented speed evoked the fear of skipping steps that would compromise vaccine safety. The unknown long-term effects and duration of protection erode confidence in taking the vaccines. There were also persistent concerns with regard to vaccine compositions that could be harmful or contain aborted foetal cells. The rate of COVID-19 death was viewed as low. Many interpreted the 95% effectiveness of the COVID-19 vaccine as insufficient. Preference for immunity gains from having an infection was viewed as more effective. Peer-reviewed publication-based data were favoured as a source of trust in vaccination decision-making. |
| Yin et al., 202155 | China | January to October 2020 | Weibo messages | Weibo (Chinese Twitter) | Topics 1: price - Weibo users claimed that the vaccine was overpriced, making up 18.3% (n = 899) of messages; 38.1% (n = 81,909) of relevant topics on Weibo received likes. On the contrary, the number of messages that considered the vaccine to be reasonably priced was twice as high but received fewer likes, accounting for 25.0% (n = 53,693). Topic 2: side effects - 441 (47.7%) positive and 295 (31.9%) negative Weibo messages about side effects. Interestingly, inactivated vaccines instigated more heated discussions than any other vaccine type. |
| Zakharchenko et al., 2022168 | Ukraine | From September-November 2020 | Dataset gathered by the Center for the Content Analysis containing almost 64,000 posts from social media, namely, Facebook, Vkontakte, Odnoklassniki, Twitter, YouTube, and Telegram | Facebook, Vkontakte, Odnoklassniki, Twitter, YouTube, and Telegram | 5 information campaigns: 1)Anti-vaccine narrative: the messages of this campaign apply specific frightening fake reasoning about 'world government's plans, dangerous manufacturing, and so on. 2)Official campaigns by WHO and by the Ministry of Heals - these messages formed anticipation of vaccines and covered not just efficiency issues but also economic and lifestyle implications of mass immunization. 3)President Zelenskiy - Ministry's support to the Ukrainian team of vaccine developers and the unicity of Ukrainian vaccines. Some esteemed doctors related skepticism to these statements and called them just an electoral instrument to help the president's party win these elections. 4) Sputnik V - this vaccine is considered a Russian geopolitical instrument in a hybrid war. The campaign aims to defy all western vaccines and stress the importance of Russia's contribution to COVID-19 overcoming. Specifically for Ukraine, they also defamed the hypothetical Ukrainian vaccine promised by Zelenskiy. 5)Ukrainian social media users campaign - this campaign was conducted by bloggers and journalists and made fun of the Russian vaccine and emphasized that it was not tested enough, so it is potentially dangerous |
| Zhang et al., 2021175 | USA | January 1, 2020, to April 30, 2021 | Public posts | The regression analyses showed that 8 topics positively predicted likes and 7 topics positively predicted retweets, among which the topic of vaccine development and people's views and that of vaccine efficacy and rollout had relatively larger effects. Network analysis and visualization revealed that the 2500 most liked and most retweeted retweets clustered around the topics of vaccine access, vaccine efficacy and rollout, vaccine development and people's views, and vaccination status. The overall valence of the tweets was positive. | |
|
Anti-vaccine and Pro-vaccine views | |||||
| Reference | Location | Study Period | Study Content | Social Media Utilized | Main Results |
| Blane et al., 202272 | NR | 1-week periods before, during, and 6 weeks after the initial Pfizer-BioNTech rollout (December 2020 to January 2021) | Public posts | Both the pro-vaccine and anti-vaccine communities used combinations of the 16 BEND maneuvers to persuade their target audiences of their particular stances. Our analysis showed how each side attempted to build its own community while simultaneously narrowing and neglecting the opposing community. Pro-vaccine users primarily used positive maneuvers such as excite and explain messages to encourage vaccination and backed leaders within their group. In contrast, anti-vaccine users relied on negative maneuvers to dismay and distort messages with narratives on side effects and death and attempted to neutralize the effectiveness of the leaders within the pro-vaccine community. Furthermore, nuking through platform policies showed to be effective in reducing the size of the anti-vaccine online community and the quantity of anti-vaccine messages. | |
| Durmaz and Hengirmen, 202279 | Turkey | Two datasets: June 1, 2019, and March 11, 2020, and March 11, 2020, and January 1, 2021 | Public posts gathered before COVID-19 and after the start of COVID-19. | In the pre-COVID-19 network, media figures and authors who had anti-vaccine views were the most influential users. In the post-COVID-19 network, the Turkish minister of health was the most influential figure. After COVID-19, there was a huge increase in these numbers. After COVID-19, anti-vaccine supporters were 22 times greater than pro-vaccine supporters. In addition, anti-vaccination supporters made up 26.51% of the networks in the post-COVID-19 network compared to 1.7% in the pre-COVID-19 network. | |
| Germani and Biller-Andorno, 202180 | NR | NR | Control, anti-Vaccine and pro-Vaccine groups contained 50 profiles for each group which were identified automatically through the use of hashtags. | Anti-vaccination supporters are more engaged in discussions on Twitter and share their contents from a pull of strong influencers. The movement's success relies on a strong sense of community, based on the contents produced by a small fraction of profiles, with the community at large serving as a sounding board for anti-vaccination discourse to circulate online. The data demonstrate that Donald Trump, before his profile was suspended, was the main driver of vaccine misinformation on Twitter. | |
| Gokhale 2020180 | NA | May 20, 2020, a few days after President Trump announced the “Operation Warp Speed” initiative | Public posts | Anti-vaccination tweets lead to four themes: 1) lack of safety especially due to rushed development, 2) conspiracy and conflict of interest, 3) ideology, globalism and new world order, and 4) loss of personal choice and freedom. Pro-vaccination tweets try to convince skeptics by touting prior success of immunizations and express concern at the rise of anti-vaxx movement on Facebook and Twitter. Furthermore, they accuse anti-vaxxers of spreading falsehoods and misinformation. In addition to these concerns, however, pro-vaxxers mock, ridicule and insult anti-vaxxers in unflattering, disrespectful and derogatory tones. | |
| Hernandez et al., 202178 | NA | July 2020 | Public posts | Results show highly polarized and active anti vaccine conversations that were primarily influenced by political and nonmedical Twitter users. Less than 10% of the tweets stemmed from the medical community, demonstrating a lack of active health care professional connectivity in addressing COVID-19 misinformation. The authors introduce the concept of Health Care Provider Social Media Hesitancy to refer to the public health threat of health care providers' nonaction in providing pro-vaccine and scientific information about the vaccine on social media. | |
| Herrera-Peco et al., 2021177 | Spain | Between 14 December and 28 December 2020 | Tweets containing the hashtag #yomevacuno | The results show that healthcare professionals represent only 11.38% of users, being responsible for 6.35% of impressions generated by the network #yomevacuno. We can observe that traffic information generated by healthcare professionals is not significant in comparison with institutions (p = 0.633), but it is compared to common users (p = 0.0014).From original content generated by healthcare professionals, only 78.95% had a favorable storytelling on the vaccine, but without sharing information about vaccines or vaccination. | |
| Jamison et al., 202071 | NA | February 2020 | Posts from 2000 most active Twitter accounts in the vaccine discourse from 2019, identifying both vaccine opponents and proponents | 45% (n = 905) of the accounts opposed vaccination, 24% (n = 479) were in favor of vaccination, 15% (n = 311) were no longer publicly available on Twitter, and 15% (n = 305) did not indicate a clear position on vaccines. Only 17% of this sample appeared to be bots. Topics were categorized as: more reliable (public health updates & news), less reliable (discussion), and unreliable (misinformation). Misinformation included conspiracy theories, unverifiable rumors, and scams promoting untested prevention/cures. Vaccine opponents shared the greatest proportion (35.4%) of unreliable information topics including a mix of conspiracy theories, rumors, and scams. Vaccine proponents shared a much lower proportion of unreliable information topics (11.3%). | |
| Johnson et al., 202076 | NA | NR | Public posts | Facebook pages | Although smaller in overall size, anti-vaccination clusters manage to become highly entangled with undecided clusters in the main online network, whereas pro-vaccination clusters are more peripheral. The theoretical framework of this study reproduces the recent explosive growth in anti-vaccination views, and predicts that these views will dominate in a decade. |
| Kwok et al., 202170 | Australia | January and October 2020 | Public posts | Nearly two-thirds of the sentiments of all tweets expressed a positive public opinion about the COVID-19 vaccine; around one-third were negative. Vaccine supporters - they considered that measures should be taken to cope with the rising number of infections, deaths, health care burden, and costs due to COVID-19. They scorned those who pretended to be experts or posted misinformation such as claiming that deaths from COVID-19 were attributable to other diseases. Vaccine hesitant - were skeptical about conspiracy theories such as the “mark of the beast” and microchips in vaccines. The sudden pause of vaccine trials also triggered worries among users about the safety of vaccination. Some Twitter users claimed that they would not get vaccinated because of previous experience with vaccination-related adverse effects. Other Twitter users disregarded COVID-19, expressing that COVID-19 had a much lower death rate than the flu, thus making it insignificant for vaccination, which they deemed would only benefit pharmaceutical firms or be politicized. | |
| Liu et al., 202152 | NR | November 1, 2020 to January 31, 2021 | Public posts | Topics related to negative attitudes: safety issues of the COVID-19 vaccines, unknown side effects, rushing the development process. Some users even questioned the existence of COVID-19 or COVID-19 vaccines and indicated a lack of trust in the government or scientists. Some users feared that the virus mutation would render the vaccine ineffective and thus had negative attitudes toward vaccines. Topics related to positive attitudes: relevant key terms included “safe,” “stay,” “end,” pandemic,” “news,” “effective,” “trial,” “continue,” and “hope.” This indicates that some positive attitudes might be derived from news of effective trial results and some users hoped that COVID-19 vaccines could end the pandemic. Relevant terms for topic 4 were “hope,” “normal,” “life,” “return,” “start,” “new,” “world,” and “great.” Some users expressed positive attitudes toward vaccines because of the desire to return to a normal life. | |
| Lyu et al., 2022176 | USA | September 28 to November 4, 2020 | Public posts | Overall, 57.65% (6218 of 25,407) are pro-vaccine, 19.30% (2469 of 25,407) are vaccine-hesitant, and the rest are anti-vaccine. Socioeconomically disadvantaged groups were more likely to hold polarized opinions on COVID-19 vaccines, either pro-vaccine (p<0.001,OR=1.49;95%CI=1.26–1.75) or anti-vaccine (p<0.001,OR=1.69;95%CI=1.49–1.91). People who had the worst personal pandemic experience were more likely to hold the anti-vaccine opinion (p<0.001,OR=0.84;95%CI=0.77–0.90). The US public is most concerned about the safety, effectiveness, and political issues regarding vaccines for COVID-19, and improving personal pandemic experience increases the vaccine acceptance level. | |
| Muric et al., 202164 | NR | October 2020 and December 2020 | Data set of Twitter posts and Twitter accounts that publicly exhibit a strong anti vaccine stance | Anti Vaccine Narratives - 3 distinct communities identified; all of them contained anti vaccine keywords, but with different focuses on topics. The largest topic community focuses on debunked claims around the conspiracy narrative that the vaccine is a plot by rich people to reduce the world population. The second topic community mostly focuses on vaccine safety, as hashtags such as #doctorsspeakup, #vaccinesafety, and #vaccineinjury appear often. The smallest topic community contains a mixture of various hashtags that range from strongly antivaccine, such as #informedconsent, #learntherisk, and #vaxxed, to some neutral hashtags, such as #vaccine, to some provaccine hashtags, such as #vaccineswork. | |
| Paul and Gokhale 202074 | NA | May 2020 | Public posts | The anti vaccination community is vociferous in opposing the vaccine, spreading misinformation, spinning conspiracies and whipping hysteria. Significant hesitation about the safety of the Covid-19 vaccine is also expressed in particular because of its rapid deployment. The pro-vaccination community counters this opposition by pointing to prior successes of immunizations as well as by mocking the anti-vaxx attitudes. A comparison of the social features of the anti-vaccination and pro-vaccination tweets suggests that the anti-vaxx community has gained steam on social media platforms and is better connected than the pro-vaccination community, which may lead to a penetration of discordant information through the online world. | |
| Scannell et al., 202166 | NR | July 14–23, 2020 | Public posts | Results found Anti-Vaccine messages predominantly used Anecdotal stories, Humor/Sarcasm, and Celebrity figures as persuasion techniques, while Pro-Vaccine messages primarily used Information, Celebrity figures, and Participation. Results also showed the Anti-Vaccine messages primarily focused on values related to the categories of Safety, Political/Conspiracy Theories, and Choice. Finally, results revealed Anti-Vaccine messages primarily used Perceived Severity and Perceived Susceptibility, which are fear appeal elements. The findings for messages by bots were comparable to the messages in the larger corpus of tweets. | |
| Sear et al., 202075 | NA | January - February 2020 | Public posts | Facebook pages | The anti-vaccination community is developing a less focused debate around COVID-19 than its counterpart, the pro-vaccination community. However, the anti-vaccination community exhibits a broader range of “flavors” of COVID-19 topics, and hence can appeal to a broader cross-section of individuals seeking COVID-19 guidance online, e.g. individuals wary of a mandatory fast-tracked COVID-19 vaccine or those seeking alternative remedies. Hence the anti-vaccination community looks better positioned to attract fresh support going forward than the pro-vaccination community. |
| Wawrzuta et al., 2021178 | Poland | Five events of the introduction of COVID-19 vaccines—announcements of the efficacy of the Pfizer-BioNTech (09.11.2020), Moderna (16.11.2020), and AstraZeneca (23.11.2020) vaccines, registration of the Pfizer-BioNTech vaccine by the European Medicines Agency (21.12.2020), and the first vaccination in Poland (27.12.2020) | Facebook comments | Five themes are new and specific to COVID-19 anti-vaccine sentiment. They argue that these vaccines have been developed too quickly without a proper test. They also suggest that vaccines do not exist despite the information from pharmaceutical companies and governments. Some users remind about the development of the swine flu vaccine. This vaccine was also developed quickly, but, over time, it caused more side effects than expected. On the other hand, conspiracy theories suggest that vaccines against COVID-19 existed before the official announcement, even before the pandemic. The last specific argument implies that people should avoid vaccination because no one takes responsibility for the potential side effects of the vaccine. Only 15% of the comments were positive, while 85% were negative. The most popular anti-vaccine arguments in our dataset are: the lack of trust in the government, the danger of vaccines, and the lack of faith in the existence of an effective vaccine. A share of pro-vaccine comments have increased from 7% to 22% during the event of first vaccination. | |
| Wawrzuta et al., 202165 | Poland | NR | Posts published by the biggest Polish media, then they selected the highest commented events related to the registration and introduction of the COVID-19 vaccines and analyzed user comments related to those events. | The arguments of vaccine opponents about the COVID-19 vaccines can be divided into 12 categories. Seven of them also apply to other vaccines but five types are COVID-19′ specific. Two new arguments say that vaccines were not properly tested or do not exist. The third topic mentions the history of the swine flu vaccine and the following narcolepsy cases. The fourth category suggests that vaccines against COVID-19 existed before the pandemic. The last argument says that no one takes responsibility for the side effects of the vaccine. The frequency of arguments from a given category varies over time. We also noticed that, while the comments were mostly negative, the reactions were positive. | |
| Yan et al., 2021179 | Canada | Between July 13, 2020, and June 14, 2021 | Comments on posts providing regular updates on COVID-19 statistics in the Vancouver (r/vancouver, n = 49,291), Toronto (r/toronto, n = 20,764), and Calgary (r/calgary, n = 21,277) subreddits | From the comments, 13 topics were identified. Two were related to vaccines, 1 regarding vaccine uptake and the other about vaccine supply. The levels of discussion for both topics were linked to the total number of vaccines administered (Granger test for causality, P<0.001). Comments pertaining to either topic displayed higher scores for joy than for other topics (P<0.001). Calgary and Toronto also discussed vaccine uptake. Sentiment scores for this topic differed across the 3 cities (P<0.001). | |
| Miscellaneous topics identified from social media discussions | |||||
| Reference | Location | Study Period | Study Content | Social Media Utilized | Main Results |
| Amanatidis et al., 2021181 | NA | Post downloaded from December 2020 and onwards, as it is the month just before and during the first vaccinations took place | Public posts | Instagram accounts of Pfizer (pfizerinc), AstraZeneca (Astrazeneca) and Johnson and Johnson (jnj) | For December 2020, there were 646 public posts for #pfizer, 738 public posts for #astrazeneca, and 70 public posts for #jnj. Deploying a model on 675 English language posts, the study obtained a list of sentiment polarity scores (0 to 1, negative to positive). The overall score was 0.38 (0.45) (Pfizer 0.42 (0.46), Astrazeneca 0.34 (0.44), JnJ 0.39 (0.43)). Finally, polarity analysis on users’ posts, leveraging a convolutional neural network, reveals a rather neutral to negative sentiment, with highly polarized user posts’ distributions. |
| Batra et al., 2021182 | For reliable cross culture polarity measurement, six countries were selected from three continents; two from each that share similar cultures. The selected countries were India and Pakistan from Asia, Norway and Sweden from Europe, and Canada and the USA from North America. | Second wave of the coronavirus | Public posts | The Pearson's correlation values indicate a high correlation in both positive and negative emotions of people from Pakistan and India (positive r = 0.837, negative r = 0.865), USA and Canada (positive r = 0.623, negative r = 0.624), Norway and Sweden (positive r = 0.703, negative r = 0.616). The examinations of Pearson's correlations for emotions (joy, surprise, anger, fear, sadness) between neighbouring countries showed a similar trend to sentiment polarity. The highest Pearson's correlation values across all the five emotions are shown for Pakistan and India, followed by the USA and Canada. | |
| Gawel et al., 202186 | NR | 6 January 2021–21 February 2021 | Data include 1803 tweets related to the phrase pope vaccine | Pope Francis’ voice on the COVID-19 vaccination has certainly been noticed and registered worldwide, but the effectiveness of his message and direct impact on Catholics’ decisions to accept or refuse the COVID-19 vaccination is quite questionable and would require further precise research. Comparing this to the regularities known from political marketing, one would think that the pope's statement would not convince the firm opponents of vaccination. | |
| Jemielniak and Krempovych, 2021183 | NR | From 1 January 2021 to 22 March 2021 | 221,922 tweets containing ‘#AstraZeneca’, 50,080 tweets in the English language were analyzed | The most retweeted (2656 retweets as of 26 March 2021) tweet overall from the first time period was one by Robert Kennedy Jr, a known anti-vaxxer advocate, whose account on Instagram was terminated in February 2020 because of COVID-19 disinformation. The tweet was discrediting AstraZeneca vaccine as ‘controversial’, ‘heavily invested in by Bill Gates’ and ‘being rejected over widespread concerns’. Tweet coordination analysis has revealed 10,728 instances in the coordination carried out by 1137 unique handles, of which 2278 instances and 616 unique handles are related to automatic bot accounts, according to the Botometer Complete Automation Probability score of ≥0.76. | |
| Lee et al., 202182 | Korea | December 2020 - February 2021 | In total 8100 posts in NAVER and 5291 posts in Instagram were sampled through web crawling. | NAVER and Instagram | The findings revealed a negative perception of COVID-19 vaccines; of the words crawled, the proportion of negative words for AstraZeneca was 71.0% (476/670) and for Pfizer was 56.3% (498/885). Among words crawled with “vaccine,” “good” ranked first, with a frequency of 13.43% (312/2323). Meanwhile, “side effect” ranked highest, with a frequency of 29.2% (163/559) for “AstraZeneca,” but 0.6% (4/673) for “Pfizer.” With “vaccine,” positive words were more frequently used, whereas with “AstraZeneca” and “Pfizer” negative words were prevalent. |
| Luo et al., 2021184 | USA and China | December 1, 2020, to February 20, 2021 | Public posts | Twitter and Sina Weibo | By implementing semantic network analysis, results demonstrate that the two countries' social media users overlapped in themes concerning domestic vaccination policies, priority groups, challenges from COVID-19 variants, and the global pandemic situation. |
| Sattar and Arifuzzaman, 202183 | USA | April–May 2021 | Public posts | For all of the vaccines, positive sentiment is 20–25%, negative sentiment is around 10%, and the rest is neutral. Negative sentiments: For both the Johnson & Johnson vaccine and the Oxford-AstraZeneca vaccine, “Blood Clot”. Around 30% of positive sentiment for wearing a mask and the negative sentiment is half that of the positive one. Vaccinated people have become more open to travel and social gatherings, as reflected by around 5% difference between positive and negative sentiments. It is optimistic that negative sentiments do not override positive sentiments for any of the topics related to maintaining a healthy lifestyle after vaccination. The tweets also revealed that many people have fever and headache after taking the Moderna vaccine. | |
| Sharevski et al., 202285 | USA | The online survey was conducted between January and February 2021 | This was a 319-participants study with both verified and misleading Tweets covered or tagged with the COVID-19 misinformation warnings to investigate how Twitter users perceive the accuracy of COVID-19 vaccine content on Twitter. | This study found that such “belief echoes” do exist among Twitter users in relation to the perceived safety and efficacy of the COVID-19 vaccine as well as the vaccination hesitancy for themselves and their children. These “belief echoes” manifested as skepticism of adequate COVID-19 immunization particularly among Republicans and Independents as well as female Twitter users. Surprisingly, we found that the belief echoes are strong enough to preclude adult Twitter users to receive the COVID-19 vaccine regardless of their education level. | |
| Thelwall 202184 | 8 countries | December 2020 - March 2021 | Public posts | There was no independent health expert in the USA tweet terms examined. The study identified the presence of non-scientific influencers from the business community in Ireland and South Africa which could be a potential cause for concern on this sensitive topic, although mainstream news sources may also be non-expert influential commentators. | |
Abbreviations: NR – not reported; NA – not applicable.
Ninestudies were classified as miscellaneous regarding the thematic discussions obtained from social media data. Lee and co-workers observed a high negative sentiment towards COVID-19 vaccines from posts obtained from Korean Instagram and NAVER users - namely the proportion of negative words for AstraZeneca vaccine was 71%, while for Pfizer it was 56.3%.82 Another study that analyzed public Twitter posts observed that the positive sentiment towards vaccines in general was 20–25%, negative was around 10% and the rest was neutral.83 Interestingly, the USA tweets revealed no existence of an independent health expert, while non-scientific influencers from the business community were observed to be active in the Twitter community in Ireland and South Africa.84 Only one study conducted an online survey on 319 participants to explore the phenomena of belief echoes and it found that they can be strong enough to affect adult Twitter users’ intention to vaccinate regardless of their education level.85 Gawel and co-workers explored did Pope Francis words have an effect on Catholics’ decisions to accept or refuse the COVID-19 vaccination, and although it is estimated that it did reach the public its’ effectiveness is quite questionable.86
The degree of polarization of views / content regarding COVID-19 vaccination on social networks
There were 28 studies that examined the degree of polarization of social media content related to COVID-19 vaccines (Table 3). The degree of polarization mainly reflected the rate of positive versus negative views on specific COVID-19 vaccine-related content, expressed as either likes vs. dislikes or supporting vs. disapproving content. Analysis of TikTok videos revealed a similar distribution of videos both encouraging/discouraging COVID-19 immunization,87 and similar results were obtained for YouTube as well.88 On the other hand, an analysis of Tik-Tok videos revealed that the vaccine produced by Moderna gained considerably greater portion of positive sentiments compared with the one produced by Pfizer (56.8% vs 20.6%, respectively).89 It is encouraging that videos produced by health experts obtained a greater number of likes, compared with those posted by media.88 Studies that analyzed the tone from Twitter posts report that in December 2020, the rate of negative sentiment towards COVID-19 immunization was 14% (with 34% neutral and the rest positive),90 while another study observed around 30% negative sentiment in posts analyzed in December 2020, however, it focused on posts published in the Spanish language under the hashtag #yonomevacunoand only focused on the movement against vaccination passports.56 Studies that were geo-located observed that among the Indian Twitter users, almost half of the posts were in a neutral tone with only 17% being classified as negative,91 while another study that focused on posts regarding vaccine-related side effects identified around 20% were negatively-oriented and more than 30% were positive, implying that nearly 80% of the tweets were either positive or neutral.92 On the other hand, Indonesian Twitter users seem to express mostly negative attitudes towards the current immunization campaigns, with 75% of posts being classified as having a negative opinion.93 In Bangladesh, Facebook users mostly reacted to vaccine-related posts positively.94 Interestingly, the Iranian Twitter users reported similar rates of positive and negative emotions towards foreign and homegrown vaccines explored between April and September 2021 (43 vs 40% were positive and 45 vs 40% were negative, for foreign and domestic vaccines, respectively).95 The USA general public sentiment showed a decrease in negative sentiment during the first two months after starting the vaccination (after December 2020) with a total of one-third negatively oriented tweets.96 Another study on USA users found that they expressed similar rates of positive and neutral sentiment towards COVID-19 vaccination in February/March 2021 (the portion of those expressing negative sentiment was the lowest).97 Finally, in July 2021 the UK Twitter users expressed similar rates of negative and positive sentiments towards current immunization campaign, as shown by the portion of positive and negative tweets obtained from the study period.98
Table 3.
Summary characteristics of studies that reported the degree of polarization of views / content regarding COVID-19 vaccination on social networks.
| Reference | Country | Study period | Study content | Social media | Main results |
|---|---|---|---|---|---|
| Alam et al., 2021188 | NR | December 21,2020 to July21,2021 | Public posts | Initializing the polarities of the obtained sentiments into three groups (positive, negative, and neutral) helped us visualize the overall scenario; our findings included 33.96% positive, 17.55% negative, and 48.49% neutral responses. | |
| Ali et al., 2021189 | USA | February to March of 2021 | Public posts | Among the February tweets, about 40% were mature positive, 21.15% were mature negative, and 33.15% were mature neutral tweets. On the other hand, in March 2021, 35.30% were mature positive, 22.09% were mature negative, and 36.40% were mature neutral tweets. It can be observed that, both among February and March tweets, positive sentiment was higher than negative sentiment among the mature users. Additionally, the percentage of neutral sentiment increased among the mature users from February to March. | |
| Al-Zaman et al., 202194 | Bangladesh | 8 March to 2 December 2020 | 10,000 most popular Facebook posts with the highest interactions on the vaccine issue | The results show that Facebook users prioritize more vaccine-related news links (71.22%) over other content. The declining interactions on the issue suggest that interaction growth mainly depends on positive news on the vaccine. Finally, users’ reaction to the vaccine issue is dominantly positive, though they may show a highly negative attitude toward vaccine misinformation. | |
| Ansari &Khan 2021190 | NR | May 15, 2021, to June 25, 2021, | Public posts | Overall global findings of COVID-19 vaccination sentiment analysis suggested 1.23% strong positive sentiments and 6.43% strong negative sentiments. According to gender based COVID-19 sentiment analysis male very strong positive sentiment is 0.22% and very strong negative sentiment is 0.33% while in case of female gender the very strong positive sentiment is 0.00% and very strong negative sentiment is 0.81%. | |
| Basch et al., 202187 | NA | NA | Videos | Tik-Tok | The number of videos discouraging the vaccine was 38, while of those encouraging the vaccine was 36. Videos encouraging a vaccine garnered over 50% of the total cumulative views and just around 50% of the total likes, while the opposite accounted for 39.6% of the total cumulative views, 44.3% of likes, and 47.4% of comments. |
| Baumel et al., 202289 | NR | NR | Videos using the search function under both “#Pfizer” and “#Moderna,” the 100 “most liked” videos under each “hashtag” were chosen for analysis. | TikTok | According to the comments, there were 20.6% positive sentiments towards Pfizer and 56.8% positive sentiments towards Moderna. 35.2% neutral sentiments towards Pfizer and 14.4% neutral sentiments towards Moderna. 44.2% negative sentiments towards Pfizer and 28.8% negative sentiments towards Moderna |
| Biswas et al., 2022185 | Kingdom of Saudi Arabia, Egypt, United Arab Emirates, Jordan, and Qatar | 01 August 2009 to 31 December 2019 (T1) and 01 January 2020 to 15 February 2021(T2). Users who posted at least one tweet in both periods were included in the study data | Public posts | In T1, 48.05% of tweets were positive, and 16.47% of tweets were negative. In T2, 43.03% of tweets were positive, and 20.56% of tweets were negative. Among the Twitter users, the sentiment of 15.92% users shifted towards positive, and the sentiment of 17.90% users shifted towards negative. Public sentiment that have shifted towards positive may be due to the hope of vaccine efficacy, whereas public sentiment that have shifted towards negative may be due to the concerns related to vaccine side effects and misinformation. | |
| Carrasco-Polaino et al., 2021191 | NR | Data was obtained during the first four days after efficacy data were announced for each of the four vaccines that had made their results public before November 30, 2020 (Pfizer, November 9; Sputnik V, November 11; Moderna, November 16; Oxford-AstraZeneca, November 23) | 49,776 interactions by 25,692 Twitter users, of which 2970 were original tweets. | The polarity analysis tool used indicated that the average overall sentiment towards all COVID-19 vaccines was moderately favorable or positive (M = 0.11; SD=0.19). When polarity or sentiment towards each vaccine was analyzed, the results showed that polarity values could be grouped into three levels with Pfizer (M = 0.16; SD=0.198) and Moderna (M = 0.16; SD=0.19) as the vaccines with the highest positive values. A second group was found within the set of three vaccines of Chinese origin (M = 0.13; SD=0.17) and the Oxford vaccine (M = 0.12; SD=0.18) with lower mean relative positive sentiment values for the Russian Sputnik V vaccine (M = 0.098; SD=0.19). The analysis revealed that these differences were statistically significant (p<0.001). | |
| Gao et al., 2021192 | China | December 25, 2020 to January 7, 2021 | Weibo posts with the key search word “COVID-19 vaccines” | Sina Weibo | Both positive and negative emotions increased among the public after the official announcement. “Good” was the most increased positive emotion and indicated great public appreciation for the production capacity and free vaccination. “Fear” was the significantly increased negative emotion and reflected the public concern about the safety of the vaccines. |
| Gao et al., 2021193 | China | 23 to 26 July 2021 | Weibo posts with the hashtag #most of the confirmed cases in Nanjing had been vaccinated | Sina Weibo | 45.14% of the Weibo posts (n = 1542) supported the COVID-19 vaccine, 12.97% were neutral, and 7.26% were doubtful, which indicated that the public did not question the vaccine's effectiveness due to the breakthrough cases in Nanjing. There were 66.47% posts that reflected significant negative emotions. Among these, 50.44% of posts with negative emotions were directed towards the media, 25.07% towards the posting users, and 11.51% towards the public, which indicated that the negative emotions were not directed towards the COVID-19 vaccine. |
| Gori et al., 2021194 | Italy | October 2020-January 2021 | Public posts | Based on the annotated tweets, 29.6% of the 2538 unique users as anti-Vax and 12.1% as pro-Vax were identified, with a strong disagreement in annotation in 7.1% of the tweets. | |
| Hernandez-Garcia et al., 202188 | 63.6% of the videos originated from Mexico and the USA | February 2021 | Videos | YouTube | A total of 118 videos were analyzed; the media created 57.6% of the videos. Positive tone was observed in 53.4%. The most discussed topics were target groups for vaccination (38.9%) and safety (43.2%). A significantly smaller number of likes was obtained in videos of media compared to those created by health professionals (p = 0.004). Videos made by health professionals, compared to those of media, showed a greater positive tone (OR = 3.09). Hoaxes/conspiracy theories were identified in 1.7% of the videos. |
| Herrera-Peco et al., 202156 | NA | December 2020 | Public posts written in Spanish language, under the hashtag #yonomevacuno | The anti-COVID-19 vaccine stream accounted for a total of 31.05% of the tweets, followed by the group of tweets that did not express any specific opinion (28.85%), with conspiracy theory tweets (16.97%) being the third main tendency. There is the existence of a series of tweets from users in favor of the COVID-19 vaccine (4.15%). | |
| Huangfu et al., 2022186 | NR | December 14, 2020, to April 30, 2021 | Public posts | Overall, 398,661 (46.51%) were positive, 204,084 (23.81%) were negative, 245,976 (28.70%) were neutral, 6899 (0.80%) were highly positive, and 1508 (0.18%) were highly negative sentiments. The main topics of positive and highly positive tweets were planning for getting vaccination (251,979/405,560, 62.13%), getting vaccination (76,029/405,560, 18.75%), and vaccine information and knowledge (21,127/405,560, 5.21%). The main concerns in negative and highly negative tweets were vaccine hesitancy (115,206/205,592, 56.04%), extreme side effects of the vaccines (19,690/205,592, 9.58%), and vaccine supply and rollout (17,154/205,592, 8.34%). | |
| Jahanbin et al., 202190 | NA | December 2020 | Public posts | The result of this study showed that 591,053 tweet (52%) were in positive sentiment, 382,431 (34%) neutral sentiment and 152,653(14%) negative sentiment about vaccine of COVID-19. | |
| Jin et al., 2020200 | NA | January-July 2020 | Public videos | YouTube | Coronavirus video content was divided into three subgroups of public-health intervention-related videos: individual interventions, government interventions, and medical interventions, as well as seven video title narratives. Over time, engagement for the intervention video subgroups has increased whereas the diffusion for other non-intervention videos has decreased suggesting that information about COVID-19 interventions has become more popular as the pandemic develops. Engagement is lowest overall on medical intervention videos, which may be due to vaccine and treatment development as a topic being downgraded quickly from YouTube's search results. |
| Karami et al., 202196 | USA | November 2020 and February 2021 | Public posts | The negative sentiment regarding the COVID-19 vaccine had a decreasing trend between November 2020 and February 2021. The vaccination in the U.S. was started on 14 December 2020. This result indicates that U.S. public sentiment has become less negative during the two months after starting the vaccination. In total, 33.64% and 66.36% of tweets were negative and non-negative, respectively. | |
| Melton et al., 2021195 | NR | Dec 1, 2020, to May 15, 2021 | 13 Reddit communities consisted of 1401 posts and 10,240 comments (11,641 in total) focusing on the COVID-19 vaccine | The polarity analysis found that 56.68% of the posts measured positive, 27.69% were negative, and 15.63% neutral. The subjectivity analysis reported 73.15% of the comments measured in between [0.25, 0.75] and considered "neutrally subjective", 18.13% were reported to be minimally subjective (less than 0.25) while the remaining 8.72% were highly subjective (greater than 0.75). Public sentiment in Reddit communities is overall positive regarding discussions about the Covid-19 vaccine or experiences with taking the vaccine, keywords and topics were detected that indicate some hesitancy amongst these users. | |
| Mir and Gul 2021196 | NR | NR | Tweets with hashtags “covid19vaccine” and “coronavirusvaccine” | Tweets expressing positive sentiments have the highest impact both in terms of likes (mean = 10.48) and retweets (mean = 3.07) compared to those that express neutral or negative sentiments. | |
| Nezhad and Deihimi 202195 | Iran | April 1, 2021 and September 30, 2021 | Tweets, mentioning COVIran Barekat (the homegrown vaccine), Pfizer/BioNTech, AstraZeneca/Oxford, Moderna, and Sinopharm (imported vaccines) | The positive sentiments towards foreign vaccines accounted for 43% of tweets (n = 173,048), followed by the negative sentiments for 45% and the neutral sentiments for 12%, respectively. On the other hand, the positive sentiments towards the homegrown vaccine accounted for 40% of the tweets (n = 160,335), followed by the negative sentiments for 40% and the neutral sentiments for 20%. | |
| Pratama et al., 202193 | Indonesia | NR | Public posts | The results of this study imply that the sentiment in the form of negative opinions is very large, namely 75%, positive opinions 20% and neutral opinions 5%. | |
| Praveen et al., 202191 | India | Across different months of the year 2020 | Public posts | 47% of social media posts discussing vaccines were in a neutral tone, and nearly 17% of the social media posts discussing the COVID-19 vaccine were in a negative tone. Fear of health and allergic reactions towards the vaccine are the two prominent issues that concern Indian citizens regarding the COVID-19 vaccine. | |
| Roe et al., 202198 | UK | 1 July 2021 and 21 July 2021 | 137,781 tweets being specifically related to COVID and Online questionnaire distributed through email and social media platforms of Twitter and Facebook | The majority of tweets were found to be negative in sentiment (53,899), followed by positive (53,071) and neutral (30,811). The negative tweets displayed a higher intensity of sentiment than positive tweets. Through questionnaire analysis it has been found that most of the participants (85.7%) had previously accepted all vaccines they had been offered), 73.8% were not concerned about receiving a COVID-19 vaccination, 17.1% were slightly concerned, 4.3% were very concerned and 4.3% stated that they were impartial. | |
| Sv et al., 202192 | India | March and April 2021 | Public posts | Tweets with positive sentiments about the side effects of the vaccine were 33.6% (n = 63,848 tweets). Tweets with negative sentiments recorded for 21.3% (n = 40,633 tweets). It is an encouraging sign that, even while posting about the side effects of the COVID-19 vaccine, nearly 78.5% of the tweets were with either neutral or positive sentiments. It can also be concluded that the positive sentiments towards the side effects of the COVID-19 vaccine increased to a greater extent from the 2nd week of April (when the total COVID-19 cases began to see a drastic increase). | |
| Yoder et al., 2021197 | NR | January 12, 2020- February 28, 2021 | First fifty accounts with the following terms: fertility doctor, fertility, OBGYN, infertility, TTC, VAX and IVF. | Twitter and Instagram | Sentiments toward the VAX were largely positive for all groups (Physician 90.3%, Individual 71.4%, Fertility Center 70%), or neutral (Physician 9.7%, Individual 28.6%, Fertility Center 30%), with no negative posts identified. Trends in mentions and sentiments were similar on both Instagram and Twitter platforms. |
| Yousefinaghani et al., 2021198 | NR | January 2020 to January 2021 | Public posts | The neutral category accounted for the 41% of the tweets, followed by the positive category accounting for 34% and negative category accounting for 25%. The negative sentiments were related to a range of concerns, but the majority usually focused on vaccine development being time-consuming, doubts in vaccine safety or reaction to governments, political figures and manufacturers. On the other hand, positive tweets were usually about scientific breakthroughs, medical advice and spreading hope. | |
| Zhang et al., 2021199 | China | October 18, 2020, and May 15, 2021 | Public posts | The positivity toward COVID-19 vaccines in China tends to fluctuate over time in the range of 45.7% to 77.0% and is intuitively correlated with public health events. In terms of gender, males were more positive (70.0% of the time) than females. | |
| Zhang et al., 2022187 | NR | June 2020 to July 2021 | Public posts | The whole population's attentiveness toward vaccines was strongly correlated (Pearson r = 0.9512) with official COVID-19 statistics, including confirmed cases and deaths. The attentiveness ratios toward vaccines of organizations were higher than that of individuals at all the time points, with the OR ranging from 1.44 (95% CI 1.28–1.61) to 2.01 (95% CI 1.70–2.39). |
Abbreviations: NR – not reported; NA – not applicable; OR – odds ratio.
Studies reporting fluctuation trends of vaccine sentiments on social networks caused by some driver events
Nine studies reported how social media vaccine sentiments varied depending on some key events (Table 4). Events that were identified as those that triggered an increase in the positive emotions towards vaccination were: the announcement about the vaccines’ effectiveness,99, 100, 101, 102 the arrival of the vaccines in UK hospitals,99 the announcement of the first human vaccine trial (UK Twitter and Facebook users) and Donald Trump's announcement regarding a vaccine being ready in a few weeks (US Twitter and Facebook users),100 as well as the decrease in number of positive COVID-19 cases in Korea.50 Some of the events that were classified as stimulating negative discussions surrounding COVID-19 vaccines were: popularity of conspiracy theories (related to Bill Gates and microchips),103 the authorization in the UK of the Pfizer BioNTech COVID19 vaccine,99 the UK opting out of the European Union vaccination scheme and halting of the phase III vaccine trials at the University of Oxford owing to safety concerns (documented among the UK and USA users),100 the growth in the occurrence of “fake news” and “misinformation” on social media,100 the increase in the number of COVID-19 infected cases in Korea (as observed among Korean Twitter users).50
Table 4.
Summary characteristics of the studies reporting fluctuation trends of vaccine sentiments on social networks caused by some driver events.
| Reference | Location | Study period | Study content | Social media utilized | Main results |
|---|---|---|---|---|---|
| Chang et al., 2021201 | NA | March to June of 2020 | Public posts | The theme on vaccines did not appear throughout the entire time period and was heavily driven by news stories and updates about the progress made in developing vaccines and discovering various treatment options for COVID-19. There are discussions of updates from the different vaccine trials like the Oxford and AstraZeneca trial, but also discussions of conspiracy theories like tweets related to Bill Gates and vaccines. | |
| Cotfas et al., 202199 | NA | November / December 2020 | Public posts | For both the neutral and in favor tweets it has been observed that some of the events in media have entrained a series of spikes (the announcement about vaccines effectiveness, the arrival of the vaccines in the UK hospitals, etc.), which are not encountered in the case of against tweets, where the major spike has been represented by the authorization in the UK of the Pfizer BioNTech COVID19 vaccine. | |
| Fazel et al., 2021202 | UK | November 2020 to January 2021 | Public posts | The percentage of negative sentiment tweets varied from 20.7% to 51.1% (excluding the reference week). The percentage of negative sentiment dropped with every new announcement (e.g., 24.4% with Phase 3 trial results from Pfizer/BioNTech, 20.9% with Phase 3 trial results from Oxford/AstraZeneca, 21.5% with the UK starting its vaccine campaign), but then reverted to a higher level (36.4%) after each news announcement. When the first trial results were released in November, negative tweets had higher engagement rates than positive tweets, but negative engagement rates declined after the release of Oxford/AstraZeneca Phase 3 results (week 3). | |
| Gerts et al., 2021203 | NA | Late January to early May 2020 | Public posts | The vaccine data showed high weighting for the word bakker and a brief increase in the word microchip in early April. The term bakker refers to the tele-evangelist Jim Bakker, who promoted myths about possible COVID-19 cures, including the use of colloidal silver, on his show. A linguistic shift in referring to the virus was also observable within the vaccine theory, with coronavirus highly weighted until mid-March, when COVID became more frequently used. | |
| Hu et al., 2021204 | NA | March 2020 - February 2021 | Public posts | This study identified 11 key dates as turning points in sentiment scores or in the number of geotweets with a total of 33 topics. Some of the key dates that induced fluctuations in the sentiment related to vaccine posts are: conspiracy theories related to Bill Gates, Phase 1 clinical trials by Moderna, Pfizer and Moderna authorization for emergency use by the US Food and Drug Administration, Department of Defense pausing a plan to give COVID-19 vaccines to detainees in the Guantanamo Bay prison camp. | |
| Hussain et al., 2021100 | UK and USA | March - November 2020 | Public posts | Facebook and Twitter | UK - positive sentiments displayed the most prominent trend, showing a small peak at the end of April and July of 2020, the former related to the first human vaccine trial. The negative sentiment trend on Twitter displayed peaks in July and October of 2020, simultaneously with the UK opting out of the European Union vaccination scheme and halting of the phase III vaccine trials at the University of Oxford owing to safety concerns. USA - positive sentiments displayed the most prominent trend, showing major peaks from end-September to end-November of 2020, which was related to claims by ex-President Donald Trump regarding a vaccine being ready in a few weeks. A small peak in the negative trend graph in mid-September 2020 was related to halting of the phase III vaccine trial at the University of Oxford. For both the UK and the USA, there was a marked increase in the positive sentiment trend, since end-October 2020, which was related to recent breakthrough announcements by Pfizer Inc and Moderna Inc. A notable peak in the negative sentiment trends for both countries, in approximately mid-October 2020, was associated with the growing anti vaccination movement and with concerns regarding “fake news” and “misinformation.” |
| Kumar et al., 2022205 | NR | January 1st 2020 - December 14 2020, | Public posts | There was an association between a Pfizer press release reporting 90% efficacy and increased discussion on vaccine misinformation. We observed an association between Johnson and Johnson temporarily halting its vaccine trials and reduced misinformation. | |
| Lyi et al., 2021101 | NA | March 2020 | Public posts | The most tweeted topic - opinions about vaccination (227,840/1499,421 tweets, 15.2%). August 11, 2020, when Russia approved the world's first COVID-19 vaccine - vaccine progress around the world became the most discussed topic around. With the advancement of vaccine administration, the topic of instruction on getting vaccines gradually became more salient and became the most discussed topic after the first week of January 2021. Weekly mean sentiment scores showed that despite fluctuations, the sentiment was increasingly positive in general. Emotion analysis further showed that trust was the most predominant emotion, followed by anticipation, fear, sadness, etc. The trust emotion reached its peak on November 9, 2020, when Pfizer announced that its vaccine is 90% effective. | |
| Shim et al., 202150 | Korea | February - March 2020 | Public posts | The number of tweets with positive sentiment and tweets with negative sentiment tended to increase before the commencement of vaccinations on 26 February, and both displayed a decreasing tendency after vaccination. Then, from 1 March, as the number of confirmed cases of COVID-19 increased again, the number of negative tweets increased in comparison to the number of positive tweets. From 13 to 15 March, the number of new COVID-19 cases decreased by about 23%. On 15 March, the number of positive tweets temporarily increased in comparison to other days. The tweets posted on 15 March were related to keywords such as “relief” and “experience”. |
Abbreviations: NA – not applicable.
Finally, Table 5 presents a synthetic summary the main findings of each category of studies included in this systematic review, in addition to their implications for public health policy, which is discussed further in the discussion section below.
Table 5.
Synthetic summary of the main findings of each category of studies included in this systematic review, in addition to their implications for public health policy.
| Characteristic of studies | Summary of main findings | Implications for public health policy |
|---|---|---|
| (1) Cross-sectional studies reporting the association between reliance on social media and vaccine hesitancy and/or acceptance | Overall, reliance on social media was associated with increased hesitancy. Further research is warranted to explore the role age plays in this association, given that two studies conducted among young adult populations reporting an opposing association. | Understanding social media usage patterns can provide an opportunity for targeted intervention. Studies of this characteristic provide evidence that users derive their information from social media. Hence, targeting appropriate public health communication and battling misinformation has the potential to shape people's attitudes regarding public health efforts. |
| (2) Studies that performed thematic-analyses of extracted social media data, thereby reporting discussions related to COVID-19 vaccine intentions/opinions | Overall, anti-vaccination discussions were more prevalent on various social media platforms. Additionally, echo chambers phenomena were observed relating to anti-vaccination campaigns. Discussions on social media provided valuable insights regarding reasons regarding vaccine hesitancy or acceptance. Finally, there is a potential role for social media influencers, especially doctors, to increase vaccine acceptance among the public. | Studies in this category demonstrated the potential for polarized views to be amplified using social media. Understanding this notion has profound benefits for targeting misinformation and combating false-news preaching “bubbles” that can be formed on social media. When designing intervention measures, it may be more beneficial to target specific anti-vaccine campaigns and misinformation rather than solely increasing the number of vaccine-encouraging content on social media |
| (3) Studies that explored the degree of polarization of specific social media contents related to COVID-19 vaccines (the degree of positive vs negative sentiments); | In general, studies reported a similar degree of positive and negative toning in terms of social media content relating to vaccination. | Social media provides an opportunity to evaluate and understand public sentiment about vaccinations in real-time, in a quick and efficient manner. Utilizing social media to understand public's sentiment allows for tailored and targeted intervention, specific to the current views held by the public. |
| (4) Studies that explored the fluctuations of vaccination attitudes/opinions gathered from social media depending on specific events that were identified as trigger events. | People's sentiment regarding COVID-19 vaccination varies greatly with specific key events relating to vaccination, both positively and negatively. | A thorough understanding of how specific events trigger people's emotions can be crucial for governments and public health officials to identify appropriate times of intervention to maximize benefit and guarantee the population's cooperation and engagement. Findings from those studies demonstrate that it is crucial for the government to adjust vaccination policies promptly in response to the public health events to promote massive vaccination via dynamic monitoring public sentiments. |
Discussion
This systematic review of the literature sought to explore the diverse role social media can play in understanding, as well as shaping, attitudes toward COVID-19 vaccination among a variety of populations. The data from cross-sectional studies that explored the associations between social media use and vaccination intentions were mainly driven from US-based populations, followed by Chinese-based ones. Among the studies that used different data mining approaches for investigating public opinion related to COVID-19 vaccines, less than half of them (40%) were geo-specific and analyzed posts from users across the world. The rest of these studies did not limit their search to any geographical location. In our analysis, we identified that most eligible studies used Twitter as the main social media platform for gathering information about COVID-19 vaccine attitudes and opinions. Twitter has been recognized as a social media platform that enables the capturing of real-time data, as one study reported a similarity between 2018 vaccine hesitancy survey data and data obtained from Twitter.104 The study even suggested that it can be used as a substitute for surveys where such purpose is justified.104 Another study identified Twitter as a “sentinel tool” which can be used for exploring vaccination public opinion specifically,105 which additionally justifies its frequent use in the studies included in our systematic review that are exploring the ongoing COVID-19 immunization attitudes and opinions.
The studies that investigated the associations between social media utilization and vaccine intentions mainly observed a negative relationship. However, there was also a group of studies reporting a positive association. This positive relationship was confirmed among the young population, which is inconsistent with previous literature that reported younger age groups were more hesitant towards vaccination. Consequently, it warrants future research to explore the potential differences in the pattern of social media usage among age groups. Additionally, it illustrates the need to stratify different age groups when studying the effect of social media on public health practices. Another interesting finding from our qualitative synthesis is that social media is positively associated with vaccine acceptance in some specific groups of people with chronic health conditions (such as AIDS/HIV or neurological disorders). This may be a noteworthy finding suggesting that people with adverse health conditions may be less vaccine hesitant in general, and that this group of people is more open to utilizing social media for deriving their health-related decisions. Policy makers aiming at increasing the vaccine uptake may consider this group of people as a target group when designing their strategies.
Furthermore, other studies confirming the positive association enlisted doctors as influencers or the type of content the participants have been exposed to, thus these additional covariates may have shaped the results. Only one study explored the impact of specific professionals as influencers on people's intentions to vaccinate, and this issue deserves further investigation.106 Emerging research has been documenting a clear role for the "public physician" (e.g., a physician who is "outward-facing" and is a face of medical authority on social media). Social media is an obvious tool for this engagement and can allow experts to debate topics openly and visibly, potentially identifying false information in real time.107 The research is still emerging regarding the specific role of a public physician on social media in regard to COVID-19 vaccination. However, this is an important finding and is consistent with research demonstrating the role of doctors on social media in significantly promoting the flu vaccine, including among hard-to-reach populations.108,109 Another important point derived from this group of studies is the impact of specific social media on vaccine acceptance/hesitancy. Only one survey explored this issue and observed different acceptance rates among YouTube, Facebook and Twitter users.42 The difference between such users may stem from the different content they have been exposed to on the specific social media platform, further implying that social media has a great challenge when it comes to combating and addressing COVID-19 related misinformation. Finally, it is important to note that while the studies aid in exploring an association, inferring causal relationships is difficult given the nature of the studies and hence the findings must be interpreted within such context.
In this systematic review, we identified one group of studies that explored topics discussed on social media related to views on vaccination. Overall, they reported domination of vaccine hesitant topics, and this domination remained stable over time after analyzing the studies that analyzed the data posted in different time points. This pattern was observed regardless of geographical context of participants. Even after performing the updated search in March 2022 and including a large number of recently published studies, we were able to observe that vaccine-hesitant themes are largely universal and repetitive across different geographical locations throughout different time-points. According to some studies, vaccine-related topics fluctuate over time and their popularity depends on the ongoing news published by the media and on social media, and it is interesting how topics that support immunization are mainly time-dependent while those against are mainly stable over time. Analyses of reasons relating to hesitancy included concerns regarding side effects, distrust in experts, and the vaccine development process and were intertwined with conspiracy theories and unreliable information without solid scientific evidence. These reasons for hesitancy are in line with previous research in the literature that did not utilize social media to analyze reasons for hesitancy, which demonstrates a consistency in hesitancy reasons despite expression on social media or not. Furthermore, some studies reported users expressing concern over vaccination price (China), vaccine supply (Mumbai, São Paulo, and Beijing), as well as vaccine distribution and supply (New York and London). These findings reiterate the notion that not all limitations regarding vaccination are merely related to hesitancy, and that lack of vaccination across the globe is not a homogenous issue. Consequently, public health policy targeting vaccination should be tailored to the specific concerns of the geographical context, and social media has the potential to demonstrate specific challenges that may be targeted across different countries. These findings resemble a strong call for addressing the social and cultural context of the specific population that could be affected by intervention measures. Tailoring intervention measures to the specific context of the population, which is shown to be unique for different geographical contexts, has the potential to enhance the outcome desired from an intervention.
The group of studies that focused on distinguishing between anti- and pro-vaccination online communities mainly suggests that the clusters against vaccination are better positioned to spread information than those in favor. Indeed, data derived from Turkish pro- and anti-vaccine networks pointed to a considerable increase in the anti-vaccination cluster after the pandemic began. One of the proposed problems might be the lack of activity of the medical community on social media in combating the spread of misinformation and providing sound scientific evidence surrounding current immunization programs. Another may include the strategies employed by the opposing communities - the pro-vaccination community are described as using mockery and disrespectful tones against anti-vaxxers and trying to attract new followers by pointing to the previous successes of immunizations; the anti-vaccination community was identified as spreading hysteria with the use of misinformation and conspiracy theories, while they simultaneously found ways to connect with a broader group of people by attracting new followers with other topics (such as alternative medical solutions). According to the current available studies, this made anti-vax clusters better positioned and connected not only among their community, but also within the clusters that have not yet decided which path to follow. With respect to some specific influential figures, one study identified Donald Trump as spreading the most vaccine misinformation on Twitter, while another study that explored this question in pro-vaccine network found that healthcare professionals still comprise a very low portion of active users that are involved in disseminating information related to COVID-19 immunizations. These observations point to the lack of online involvement of medically trained personnel in pro-vaccine clusters. Another speculated reason for why anti-vaccination opinions is more prevalent is the "echo chambers" phenomena, where individuals gather and are surrounded by like-minded people in terms of political and ideological orientation. In turn, this allows opinion-reinforcing information and the creation of polarization on certain health topics, such as vaccination in this case. Previous research has demonstrated the role of such echo chambers,21,54,110 where individuals aggregate and amplify opinions in dispersing misinformation about infectious disease.111 Indeed one study included in our review, observed that belief echoes can actually be quite strong and impact adult Twitter users’ vaccination intention regardless of their education level.85 These findings are critical for shaping public health policy, especially in times of crises, to ensure there is proper science communication that is perceived as authoritative and to prevent misinformation on social media platforms. These findings can significantly aid in directing intervention measures to minimize misinformation and utilize social media as a platform for understanding behaviors and perceptions.
Studies included in this review attempted to analyze the type and/or tone of the content present on social media regarding vaccination. In general, studies observed dissimilar degree of positive and negative emotions expressed by social media users originating from different locations, and their emotions were not constant throughout time. One study points to the fact that the public sentiment depend on the vaccine manufacturer as well.89 These findings, combined with our analyses of anti-vaccination discussions receiving far more attention on social media, are essential for public health intervention. Firstly, these findings highlight that the issue is not merely an absence of promoting positive public health content on social media. Rather, polarized views against vaccination receive more attention from users and are promoted by heated discussions and echo chambers, as discussed earlier. Consequently, when designing intervention measures, it may be more beneficial to target specific anti-vaccine campaigns and misinformation rather than solely increasing the number of vaccine-encouraging content on social media.
The results of studies that investigated how the public vaccine-related sentiment changed after some specific events provided valuable insights into this significant cofactor that inevitably affects and shapes the vaccination intentions of individuals. Specifically, the positively stimulating events included those that announced some significant positive milestones in the vaccine development or distribution, while those that increased the rate of negative sentiments were concentrated on the emerging occurrence of misinformation/conspiracy theories on the social networks, or reported negative points related to vaccine development or immunization schemes. These findings are crucial for designing successful public health intervention for a multitude of reasons. First, social media provides an opportunity to evaluate and understand public sentiment about vaccinations in real-time, in a quick and efficient manner. This is supported by the huge dependence on social media across the globe, allowing it to be a medium for people to express their emotions and opinions. Consequently, this allows governments to promote COVID-19 vaccinations in a rational and orderly manner. A thorough understanding of how specific events trigger people's emotions can be crucial for governments and public health officials to identify appropriate times of intervention to maximize benefit and guarantee the population's cooperation and engagement. Similarly, it allows for an understanding of when it may not be appropriate to implement specific interventions over others. These results constitute a strong call for policy-makers to adjust vaccination policies rapidly in response to the public health events to promote massive vaccination via dynamic monitoring of public sentiment.112
Finally, in this systematic review we also observed that data mining and natural language processing techniques proved to be very useful and beneficial in analyzing and understanding public perspectives regarding this critical public health issue and thereby providing meaningful and valuable insights. This is also in line with more emerging research in the literature that was not within the scope of this review, but nevertheless reiterating such notions.113,114 The value of observations gained from these studies further justifies its widespread application in different fields including marketing, politics and, in this case, public opinion and public health.115,116 Overall, misinformation and the spread of anti-vaccination communities on social media platforms contributes to masking healthy behaviors and promotes practices that contribute to negative health outcomes. While restricting information spread on social media continues to be a complex issue, the findings of this review demonstrate the significant importance of building platforms for disseminating authentic public health messages. This include intervention measures to facilitate communication by figures perceived to be authoritative for the said topic (e.g., doctors, health experts).
This review provides a high level of evidence by thoroughly and systematically summarizing the literature regarding the associations between social media and COVID-19 vaccination. Additionally, this review seeks to exemplify the potential that social media has as a platform for public health intervention and a source of information that aids in directing policymaking to address vaccine hesitancy and further promote vaccination uptake worldwide. These issues are exceedingly important in the context of the COVID-19 pandemic, where population-level efforts are extremely necessary in reaching herd immunity and hence alleviating the public health burden of COVID-19. We suggest future studies to explore the impact of specific social media sources (for example, YouTube vs. Facebook), explore temporal trends in social media influence on vaccination attitudes (e.g., especially in relation to vaccine rollout), the role of specific types of professionals as influencers (such as doctors, politicians, celebrities, etc.), or the effects of different types of content on vaccination attitudes in more depth. To the best of our knowledge, this review is one of the first studies to review the literature on a very emerging topic in a time where interventions promoting vaccination uptake are indispensable to our progress against the pandemic
Despite those strengths, this review is not without limitations that must be acknowledged. Firstly, this review included several cross-sectional studies. While all cross-sectional studies were assessed for quality, the inability to establish causation is a limitation with all cross-sectional studies. Additionally, and given that such studies utilized self-reported measures to collect data, additional limitations include selection bias, social desirability bias, as well as recall bias. Due to the wide range of studies included in this review, no meta-analysis was conducted, limiting this study with the inability to provide a quantitative synthesis of results.
This review sought to capture the current evidence present in the literature regarding the role social media platforms can play in affecting attitudes and behaviors relating to COVID-19 vaccination. This is done through a variety of approaches, including misinformation as well as establishment of communities and campaigns to promote behaviors that are not in line with public health recommendations globally. Given the high public health burden of COVID-19 as well as the current limitations in reaching herd immunity partially due to vaccine hesitancy, public health interventions utilizing social media can be effective in promoting vaccine uptake.
Contributors
All authors contributed to revise work for important intellectual content, gave the final approval of the version to be published, and agreed on all aspects of the work, especially concerning its accuracy and integrity. Further specific activities have been distributed as follows: F.C. conceived the research hypothesis. F.C. and A.P. designed the study. A.P. and Y.A.A. performed the article screening. A.P., Y.A.A., G.F., V.P., A.M. and A.L. performed the data extraction and the quality assessment. All authors had access to data and verified it (F.C., A.P., Y.A.A., G.F., V.P., A.M., A.L., W.R.). F.C. and W.R. has shaped the manuscript with input from the entire team (written contributions of single paragraphs).
Data sharing statement
All data gathered for qualitative synthesis within this review are available with publication as supplementary files. No restrictions to access, neither investigator support, nor a data access agreement are required.
Declaration of Interests
The authors have no competing interest to declare.
Funding
None.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.eclinm.2022.101454.
Appendix. Supplementary materials
References
- 1.Wilson S.L., Wiysonge C. Social media and vaccine hesitancy. BMJ Glob Health. 2020;5(10) doi: 10.1136/bmjgh-2020-004206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chadwick A., Kaiser J., Vaccari C., et al. Online social endorsement and Covid-19 vaccine hesitancy in the United Kingdom. Soc Media+ Soc. 2021;7(2) [Google Scholar]
- 3.MacDonald N.E. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33(34):4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 4.Cascini F., Pantovic A., Al-Ajlouni Y., Failla G., Ricciardi W. Attitudes, acceptance and hesitancy among the general population worldwide to receive the COVID-19 vaccines and their contributing factors: a systematic review. eClinicalMedicine. 2021;40 doi: 10.1016/j.eclinm.2021.101113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Coomes E.A., Haghbayan H., Finken L.R., Quadros K.K., Bagai A., Cheema A.N. Information on cardiovascular disease in the digital era: results from a cross-sectional patient survey. Can J Cardiol. 2019;35(6):791–794. doi: 10.1016/j.cjca.2019.03.015. [DOI] [PubMed] [Google Scholar]
- 6.Gunaratne K., Haghbayan H., Coomes E.A. Tweeting authors: impact on research publicity and downstream citations. J Gen Intern Med. 2020;35(6):1926–1927. doi: 10.1007/s11606-019-05454-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Warren K.E., Wen L.S. Measles, social media and surveillance in Baltimore City. J Public Health. 2017;39(3):e73–e78. doi: 10.1093/pubmed/fdw076. (Bangkok) [DOI] [PubMed] [Google Scholar]
- 8.Daley M.F., Narwaney K.J., Shoup J.A., Wagner N.M., Glanz J.M. Addressing parents’ vaccine concerns: a randomized trial of a social media intervention. Am J Prev Med. 2018;55(1):44–54. doi: 10.1016/j.amepre.2018.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Donovan Joan. Social-Media companies must flatten the curve of misinformation. Nature. 2020 doi: 10.1038/d41586-020-01107-z. [DOI] [PubMed] [Google Scholar]
- 10.Donovan Joan. MIT Technology Review, MIT Technology Review; 1 May 2020. Covid Hoaxes Are Using a Loophole to Stay Alive-Even after Content Is Deleted.https://www.technologyreview.com/2020/04/30/1000881/covid-hoaxes-zombie-content-wayback-machine-disinformation/ [Google Scholar]
- 11.Davies P., Chapman S., Leask J. Antivaccination activists on the world wide web. Arch Dis Child. 2002;87(1):22–25. doi: 10.1136/adc.87.1.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Keelan J., Pavri V., Balakrishnan R., Wilson K. An analysis of the human papilloma virus vaccine debate on MySpace blogs. Vaccine. 2010;28(6):1535–1540. doi: 10.1016/j.vaccine.2009.11.060. [DOI] [PubMed] [Google Scholar]
- 13.Keelan J., Pavri-Garcia V., Tomlinson G., Wilson K. YouTube as a source of information on immunization: a content analysis. JAMA. 2007;298(21):2482–2484. doi: 10.1001/jama.298.21.2482. [DOI] [PubMed] [Google Scholar]
- 14.Ache K.A., Wallace L.S. Human papillomavirus vaccination coverage on YouTube. Am J Prev Med. 2008;35(4):389–392. doi: 10.1016/j.amepre.2008.06.029. [DOI] [PubMed] [Google Scholar]
- 15.Tafuri S., Gallone M.S., Cappelli M.G., Martinelli D., Prato R., Germinario C. Addressing the anti-vaccination movement and the role of HCWs. Vaccine. 2014;32(38):4860–4865. doi: 10.1016/j.vaccine.2013.11.006. [DOI] [PubMed] [Google Scholar]
- 16.Mitra T., Counts S., Pennebaker J.W. Proceedings of the Tenth International AAAI Conference on Web and Social Media. 2016. Understanding anti-vaccination attitudes in social media. [Google Scholar]
- 17.Evrony A., Caplan A. The overlooked dangers of anti-vaccination groups' social media presence. Hum Vaccin Immunother. 2017;13(6):1475–1476. doi: 10.1080/21645515.2017.1283467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smith N., Graham T. Mapping the anti-vaccination movement on Facebook. Inf Commun Soc. 2019;22(9):1310–1327. [Google Scholar]
- 19.Blankenship Elizabeth. Sentiment, contents, and retweets: a study of two vaccine-related twitter datasets. Pem J. 2018;22:17–138. doi: 10.7812/tpp/17-138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Basch C.H., MacLean S.A. A content analysis of HPV related posts on instagram. Hum Vaccin Immunother. 2019;15(7–8):1476–1478. doi: 10.1080/21645515.2018.1560774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Van Raemdonck N. The echo chamber of anti-vaccination conspiracies: mechanisms of radicalization on Facebook and Reddit. Institute for Policy, Advocacy and Governance. December 22, 2019. The Digital Age, Cyber Space, and Social Media: The Challenges of Security & Radicalization (IPAG Knowledge Series Book 6)
- 22.Schmidt A.L., Zollo F., Scala A., Betsch C., Quattrociocchi W. Polarization of the vaccination debate on Facebook. Vaccine. 2018;36(25):3606–3612. doi: 10.1016/j.vaccine.2018.05.040. [DOI] [PubMed] [Google Scholar]
- 23.Puri N., Coomes E.A., Haghbayan H., Gunaratne K. Social media and vaccine hesitancy: new updates for the era of COVID-19 and globalized infectious diseases. Hum Vaccin Immunother. 2020;16(11):2586–2593. doi: 10.1080/21645515.2020.1780846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Milinovich G.J., Williams G.M., Clements A.C.A., Hu W. Internet-based surveillance systems for monitoring emerging infectious diseases. Lancet Infect Dis. 2014;14(2):160–168. doi: 10.1016/S1473-3099(13)70244-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Padamsee T.J., Bond R.M., Dixon G.N., et al. Changes in COVID-19 vaccine hesitancy among black and white individuals in the US. JAMA Netw Open. 2022;5(1) doi: 10.1001/jamanetworkopen.2021.44470. e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ouzzani M., Hammady H., Fedorowicz Z., Elmagarmid A. Rayyan-A web and mobile app for systematic reviews. Syst Rev. 2016;5(1):1–10. doi: 10.1186/s13643-016-0384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wells G.A., Shea B., O'Connell D., et al. Oxford; 2000. The Newcastle-Ottawa Scale (NOS) For Assessing the Quality of Nonrandomised Studies in Meta-Analyses. [Google Scholar]
- 28.Engel-Rebitzer E., Stokes D.C., Meisel Z.F., Purtle J., Doyle R., Buttenheim A.M. Partisan differences in legislators' discussion of vaccination on twitter during the COVID-19 era: natural language processing analysis. JMIR Infodemiology. 2022;2(1):e32372. doi: 10.2196/32372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tang L., Douglas S., Laila A. Among sheeples and antivaxxers: social media responses to COVID-19 vaccine news posted by Canadian news organizations, and recommendations to counter vaccine hesitancy. Can Commun Dis Rep. 2021;47(12):524–533. doi: 10.14745/ccdr.v47i12a03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Aloweidi A., Bsisu I., Suleiman A., et al. Hesitancy towards COVID-19 vaccines: an analytical cross-sectional study. Int J Environ Res Public Health. 2021;18(10):5111. doi: 10.3390/ijerph18105111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Luo Sitong, et al. Behavioural intention of receiving COVID-19 vaccination, social media exposures and peer discussions in China. Epidemiol Infect. 2021;149:e158. doi: 10.1017/S0950268821000947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mo P.K.H., Luo S., Wang S., et al. Intention to receive the COVID-19 vaccination in China: application of the diffusion of innovations theory and the moderating role of openness to experience. Vaccines. 2021;9(2):129. doi: 10.3390/vaccines9020129. (Basel) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gewirtz-Meydan A., Mitchell K., Shlomo Y., Heller O., Grinstein-Weiss M. COVID-19 among youth in Israel: correlates of decisions to vaccinate and reasons for refusal. J Adolesc Health. 2022;70(3):396–402. doi: 10.1016/j.jadohealth.2021.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Silva Tânia Magalhães, Estrela Marta, Roque Vítor, et al. Perceptions, knowledge and attitudes about COVID-19 vaccine hesitancy in older Portuguese adults. Age and Ageing. 2022;51(3) doi: 10.1093/ageing/afac013. afac013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fontenot H.B., Mattheus D.B., Lim E., et al. Undergraduate nursing students' COVID-19 vaccine intentions: a national survey. PLoS ONE. 2021;16(12) doi: 10.1371/journal.pone.0261669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ghaffari-Rafi A., Teehera K.B., Higashihara T.J., et al. Variables associated with coronavirus disease 2019 vaccine hesitancy amongst patients with neurological disorders. Infect Dis Rep. 2021;13(3):763–810. doi: 10.3390/idr13030072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Huang X., Yu M., Fu G., et al. Willingness to receive COVID-19 vaccination among people living with HIV and AIDS in China: nationwide cross-sectional online survey. JMIR Public Health Surveill. 2021;7(10):e31125. doi: 10.2196/31125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Xin M., Luo S., She R., et al. The impact of social media exposure and interpersonal discussion on intention of COVID-19 vaccination among nurses. Vaccines. 2021;9(10) doi: 10.3390/vaccines9101204. (Basel) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wang Z., She R., Chen X., et al. Parental acceptability of COVID-19 vaccination for children under the age of 18 years among Chinese doctors and nurses: a cross-sectional online survey. Hum Vaccin Immunother. 2021;17(10):3322–3332. doi: 10.1080/21645515.2021.1917232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zhang K.C., Fang Y., Cao H., et al. Behavioral intention to receive a COVID-19 vaccination among Chinese factory workers: cross-sectional online survey. J Med Internet Res. 2021;23(3) doi: 10.2196/24673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Berenson A.B., Chang M.H., Hirth J.M., Kanukurthy M. Intent to get vaccinated against COVID-19 among reproductive-aged women in Texas. Hum Vaccin Immunother. 2021;17(9):2914–2918. doi: 10.1080/21645515.2021.1918994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jennings W, Stoker G, Bunting H, et al. Lack of Trust, Conspiracy Beliefs, and Social Media Use Predict COVID-19 Vaccine Hesitancy. Vaccines. 2021;9(6):593. doi: 10.3390/vaccines9060593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bonnevie E., Gallegos-Jeffrey A., Goldbarg J., Byrd B., Smyser J. Quantifying the rise of vaccine opposition on Twitter during the COVID-19 pandemic. J Commun Healthc. 2021;14(1):12–19. [Google Scholar]
- 44.Boucher J.C., Cornelson K., Benham J.L., et al. Analyzing social media to explore the attitudes and behaviors following the announcement of successful COVID-19 vaccine trials: infodemiology study. JMIR Infodemiology. 2021;1(1):e28800. doi: 10.2196/28800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hou Z, Tong Y, Du F, et al. Assessing COVID-19 Vaccine Hesitancy, Confidence, and Public Engagement: A Global Social Listening Study. J Med Internet Res. 2021;23(6):e27632. doi: 10.2196/27632. PMID: 34061757; PMCID: PMC8202656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Thelwall M, Kousha K, Thelwall S. Covid-19 vaccine hesitancy on english-language twitter. Prof De La Inf. 2021;30(2):1–13. [Google Scholar]
- 47.Klimiuk K., Czoska A., Biernacka K., Balwicki Ł. Vaccine misinformation on social media–topic-based content and sentiment analysis of Polish vaccine-deniers’ comments on Facebook. Hum Vaccin Immunother. 2021;17(7):2026–2035. doi: 10.1080/21645515.2020.1850072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jacobs K.D., Zori G., Collins S.L., Wood E. Exploration of the COVID-19 content within a vaccine choice social media platform: a case study. J Consum Health Internet. 2021;25(4):366–382. [Google Scholar]
- 49.Boucher J.C., Cornelson K., Benham J.L., et al. Analyzing social media to explore the attitudes and behaviors following the announcement of successful COVID-19 vaccine trials: infodemiology study. JMIR Infodemiology. 2021;1(1):e28800. doi: 10.2196/28800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Shim J.G., Ryu K.H., Lee S.H., Cho E.A., Lee Y.J., Ahn J.H. Text mining approaches to analyze public sentiment changes regarding COVID-19 vaccines on social media in Korea. Int J Environ Res Public Health. 2021;18(12) doi: 10.3390/ijerph18126549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wong LP, Lin Y, Alias H, Bakar SA, Zhao Q, Hu Z. COVID-19 Anti-vaccine sentiments: analyses of comments from social media. Healthcare. 2021;9(11):1530. doi: 10.3390/healthcare9111530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Liu S, Liu J. Understanding behavioral intentions toward COVID-19 vaccines: theory-based content analysis of tweets. J Med Internet Res. 2021;23(5):e28118. doi: 10.2196/28118. PMID: 33939625; PMCID: PMC8117955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Liu S, Li J, Liu J. Leveraging transfer learning to analyze opinions, attitudes, and behavioral intentions toward covid-19 vaccines: social media content and temporal analysis. J Med Internet Res. 2021;23(8):e30251. doi: 10.2196/30251. PMID: 34254942; PMCID: PMC8360338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Baines A, Ittefaq M, Abwao M. #Scamdemic, #Plandemic, or #Scaredemic: what parler social media platform tells us about COVID-19 vaccine. Vaccines. 2021;9(5):421. doi: 10.3390/vaccines9050421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yin F, Wu Z, Xia X, Ji M, Wang Y, Hu Z. Unfolding the determinants of COVID-19 vaccine acceptance in China. J Med Internet Res. 2021;23(1):e26089. doi: 10.2196/26089. PMID: 33400682; PMCID: PMC7813210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Herrera-Peco I, Jiménez-Gómez B, Romero Magdalena CS, et al. Antivaccine movement and COVID-19 negationism: a content analysis of Spanish-written messages on twitter. Vaccines (Basel) 2021;9(6):656. doi: 10.3390/vaccines9060656. PMID: 34203946; PMCID: PMC8232574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hou Z, Tong Y, Du F, et al. Assessing COVID-19 vaccine hesitancy, confidence, and public engagement: a global social listening study. J Med Internet Res. 2021;23(6):e27632. doi: 10.2196/27632. PMID: 34061757; PMCID: PMC8202656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Criss S, Nguyen TT, Norton S, et al. Advocacy, hesitancy, and equity: exploring u.s. race-related discussions of the COVID-19 vaccine on twitter. Int J Environ Res Public Health. 2021;18(11):5693. doi: 10.3390/ijerph18115693. PMID: 34073291; PMCID: PMC8198507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wong LP, Lin Y, Alias H, Bakar SA, Zhao Q, Hu Z. COVID-19 anti-vaccine sentiments: analyses of comments from social media. Healthcare. 2021;9(11):1530. doi: 10.3390/healthcare9111530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Monselise M, Chang CH, Ferreira G, Yang R, Yang CC. Topics and sentiments of public concerns regarding COVID-19 vaccines: social media trend analysis. J Med Internet Res. 2021;23(10):e30765. doi: 10.2196/30765. Published 2021 Oct 21. doi:10.2196/30765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Liew T.M., Lee C.S. Examining the utility of social media in COVID-19 vaccination: unsupervised learning of 672,133 twitter posts. JMIR Public Health Surveill. 2021;7(11):e29789. doi: 10.2196/29789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Küçükali H, Ataç Ö, Palteki AS, Tokaç AZ, Hayran O. Vaccine hesitancy and anti-vaccination attitudes during the start of COVID-19 vaccination program: a content analysis on twitter data. Vaccines (Basel) 2022;10(2):161. doi: 10.3390/vaccines10020161. PMID: 35214620; PMCID: PMC8876163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Bi D., Kong J., Zhang X., Yang J. Analysis on health information acquisition of social network users by opinion mining: case analysis based on the discussion on COVID-19 vaccinations. J Healthc Eng. 2021;2021 doi: 10.1155/2021/2122095. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 64.Muric G., Wu Y., Ferrara E. COVID-19 vaccine hesitancy on social media: building a public twitter data set of antivaccine content, vaccine misinformation, and conspiracies. JMIR Public Health Surveill. 2021;7(11):e30642. doi: 10.2196/30642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Wawrzuta D., Jaworski M., Gotlib J., Panczyk M. The Arguments of the COVID-19 vaccines opponents on facebook in poland: textual analysis study. Eur J Public Health. 2021;31:157. [Google Scholar]
- 66.Scannell D., Desens L., Guadagno M., et al. COVID-19 vaccine discourse on twitter: a content analysis of persuasion techniques, sentiment and mis/disinformation. J Health Commun. 2021;26(7):443–459. doi: 10.1080/10810730.2021.1955050. [DOI] [PubMed] [Google Scholar]
- 67.Liu S., Li J., Liu J. Leveraging transfer learning to analyze opinions, attitudes, and behavioral intentions toward COVID-19 vaccines: social media content and temporal analysis. J Med Internet Res. 2021;23(8):e30251. doi: 10.2196/30251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kwok S.W.H., Vadde S.K., Wang G. Tweet topics and sentiments relating to COVID-19 vaccination among Australian twitter users: machine learning analysis. J Med Internet Res. 2021;23(5):e26953. doi: 10.2196/26953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Jamison A.M., Broniatowski D.A., Dredze M., Sangraula A., Smith M.C., Quinn S.C. Not just conspiracy theories: vaccine opponents and proponents add to the COVID-19 'infodemic' on Twitter. Harv Kennedy Sch Misinf Rev. 2020;1 doi: 10.37016/mr-2020-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kwok SWH, Vadde SK, Wang G. Tweet topics and sentiments relating to COVID-19 vaccination among australian twitter users: machine learning analysis. J Med Internet Res. 2021;23(5):e26953. doi: 10.2196/26953. PMID: 33886492; PMCID: PMC8136408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Jamison A.M., Broniatowski D.A., Dredze M., Sangraula A., Smith M.C., Quinn S.C. Not just conspiracy theories: vaccine opponents and proponents add to the COVID-19 ‘infodemic'on Twitter. Harv Kennedy Sch Misinf Rev. 2020;1(3) doi: 10.37016/mr-2020-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Blane JT, Bellutta D, Carley KM. Social-Cyber maneuvers during the COVID-19 vaccine initial rollout: content analysis of tweets. J Med Internet Res. 2022;24(3):e34040. doi: 10.2196/34040. PMID: 35044302; PMCID: PMC8903203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Blane J.T., Bellutta D., Carley K.M. Social-cyber maneuvers during the COVID-19 vaccine initial rollout: content analysis of tweets. J Med Internet Res. 2022;24(3):e34040. doi: 10.2196/34040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Paul N., Gokhale S.S. Proceedings of the 8th IEEE International Conference on Big Data (Big Data) 2020. Analysis and classification of vaccine dialogue in the coronavirus era. Dec 10-13Electr Network2020. [Google Scholar]
- 75.Sear R.F., Velasquez N., Leahy R., et al. Quantifying COVID-19 content in the online health opinion war using machine learning. IEEE Access. 2020;8:91886–91893. doi: 10.1109/ACCESS.2020.2993967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Johnson N.F., Velasquez N., Restrepo N.J., et al. The online competition between pro- and anti-vaccination views. Nature. 2020;582(7811) doi: 10.1038/s41586-020-2281-1. 230-+ [DOI] [PubMed] [Google Scholar]
- 77.Gokhale S.S. Proceedings of the 18th IEEE International Symposium on Parallel and Distributed Processing with Applications (ISPA) 2020. Monitoring the perception of Covid-19 vaccine using topic models. 10th IEEE Int Conf On Big Data and Cloud Comp (BDCloud) / IEEE Int Symp On Social Comp and Networking (SocialCom) / IEEE Int Conf On Sustainable Comp and Commun (SustainCom)Dec 17-19; Electr Network2020. [Google Scholar]
- 78.Hernandez R.G., Hagen L., Walker K., O'Leary H., Lengacher C. The COVID-19 vaccine social media infodemic: healthcare providers’ missed dose in addressing misinformation and vaccine hesitancy. Hum Vaccines Immunother. 2021;17(9):2962–2964. doi: 10.1080/21645515.2021.1912551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Durmaz N, Hengirmen E. The dramatic increase in anti-vaccine discourses during the COVID-19 pandemic: a social network analysis of Twitter. Hum Vaccin Immunother. 2022;18(1) doi: 10.1080/21645515.2021.2025008. Epub 2022 Feb 3. PMID: 35113767; PMCID. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Germani F., Biller-Andorno N. The anti-vaccination infodemic on social media: a behavioral analysis. PLoS ONE. 2021;16(3) doi: 10.1371/journal.pone.0247642. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 81.Herrera-Peco I, Jiménez-Gómez B, Peña Deudero JJ, Benitez De Gracia E, Ruiz-Núñez C. Healthcare professionals' role in social media public health campaigns: analysis of spanish pro vaccination campaign on Twitter. Healthcare (Basel) 2021;9(6):662. doi: 10.3390/healthcare9060662. PMID: 34199495; PMCID: PMC8227422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Lee H, Noh EB, Park SJ, et al. COVID-19 Vaccine perception in South Korea: web crawling approach. JMIR Public Health Surveill. 2021 8;7(9):e31409. 10.2196/31409. PMID: 34348890; PMCID: PMC8428376 [DOI] [PMC free article] [PubMed]
- 83.Sattar NS, Arifuzzaman S. COVID-19 vaccination awareness and aftermath: public sentiment analysis on Twitter data and vaccinated population prediction in the USA. Applied Sciences. 2021;11(13):6128. doi: 10.3390/app11136128. [DOI] [Google Scholar]
- 84.Thelwall Mike. Can Twitter give insights into international differences in Covid-19 vaccination? Eight countries’ English tweets to 21 March 2021. Profesional de la información. 2021;30(3) doi: 10.3145/epi.2021.may.11. [DOI] [Google Scholar]
- 85.Sharevski F., Alsaadi R., Jachim P., Pieroni E. Misinformation warnings: twitter's soft moderation effects on COVID-19 vaccine belief echoes. Comput Secur. 2022;114 doi: 10.1016/j.cose.2021.102577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Gaweł A, Mańdziuk M, Żmudziński M, et al. Effects of Pope francis' religious authority and media coverage on Twitter user's attitudes toward COVID-19 vaccination. Vaccines (Basel) 2021;9(12):1487. doi: 10.3390/vaccines9121487. PMID: 34960233; PMCID: PMC8707322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Basch C.H., Meleo-Erwin Z., Fera J. A global pandemic in the time of viral memes: COVID-19 vaccine misinformation and disinformation on TikTok. Human Vaccines & Immunotherapeutics, 2021;17(8):2373–2377. doi: 10.1080/21645515.2021.1894896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Hernández-García I., Gascón-Giménez I., Gascón-Giménez A., Giménez-Júlvez T. Information in Spanish on YouTube about covid-19 vaccines. Human Vaccines & Immunotherapeutics, 2021;17(11):3916–3921. doi: 10.1080/21645515.2021.1957416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Baumel N.M., Spatharakis J.K., Baumel L.D., Sellas E.I. Disparity in public perception of Pfizer and Moderna COVID-19 vaccines on TikTok. J Adolesc Health. 2022;70(3):514. doi: 10.1016/j.jadohealth.2021.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Jahanbin K., Rahmanian V., Sharifi N., Rahmanian F. Sentiment analysis and opinion mining about COVID-19 vaccines of twitter data. Pak J Med Health Sci. 2021;15(1):694–695. [Google Scholar]
- 91.Praveen S.V., Ittamalla R., Deepak G. Analyzing the attitude of Indian citizens towards COVID-19 vaccine-a text analytics study. Diabetes and metabolic syndrome. Clin Res Rev. 2021;15(2):595–599. doi: 10.1016/j.dsx.2021.02.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Sv P, Tandon J, Vikas Hinduja H. Indian citizen's perspective about side effects of COVID-19 vaccine - A machine learning study. Diabetes Metab Syndr. 2021;15(4) doi: 10.1016/j.dsx.2021.06.009. Epub 2021 Jun 10. PMID: 34186350; PMCID: PMC8189737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Pratama G.Y., Udin C.A., Aprilian D.A., Erliansyah M.R., Rumaisa F. Public sentiment towards the Covid 19 Vaccine in Indonesia. Turk J Physiother Rehabil. 2021;32(3):6081–6084. [Google Scholar]
- 94.Al-Zaman MS. An exploratory study of social media users’ engagement with COVID-19 vaccine-related content. F1000Res. 2021;10:236. doi: 10.12688/f1000research.51210.3. Published 2021 Jun 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Bokaee Nezhad Z., Deihimi M.A. Twitter sentiment analysis from Iran about COVID 19 vaccine. Diabetes Metab Syndr. 2022;16(1) doi: 10.1016/j.dsx.2021.102367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Karami A, Zhu M, Goldschmidt B, Boyajieff HR, Najafabadi MM. Covid-19 vaccine and social media in the U.S.: exploring emotions and discussions on twitter. Vaccines. 2021;9(10):1059. doi: 10.3390/vaccines9101059. (Basel) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Ali RN, Rubin H, Sarkar S. Countering the potential re-emergence of a deadly infectious disease—Information warfare, identifying strategic threats, launching countermeasures. PLOS ONE. 2021;16(8) doi: 10.1371/journal.pone.0256014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Roe C, Lowe M, Williams B, Miller C. Public perception of SARSCoV-2 vaccinations on social media: questionnaire and sentiment analysis. Int J Environ Res Public Health. 2021;18(24):13028. doi: 10.3390/ijerph182413028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Cotfas L.A., Delcea C., Roxin I., Ioanas C., Gherai D.S., Tajariol F. The longest month: analyzing COVID-19 vaccination opinions dynamics from tweets in the month following the first vaccine announcement. IEEE Access. 2021;9:33203–33223. doi: 10.1109/ACCESS.2021.3059821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Hussain A, Tahir A, Hussain Z, et al. Artificial intelligence-enabled analysis of public attitudes on facebook and Twitter toward COVID-19 vaccines in the United Kingdom and the United States: Observational Study. J Med Internet Res. 2021;23(4):e26627. doi: 10.2196/26627. PMID: 33724919; PMCID: PMC8023383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Lyu JC, Han EL, Luli GK. COVID-19 Vaccine-related disussion on Twitter: topic modeling and sentiment analysis. J Med Internet Res. 2021;23(6):e24435. doi: 10.2196/24435. PMID: 34115608; PMCID: PMC8244724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Fazel S., Zhang L., Javid B., Brikell I., Chang Z. Harnessing Twitter data to survey public attention and attitudes towards COVID-19 vaccines in the UK. Sci Rep. 2021;11(1):23402. doi: 10.1038/s41598-021-02710-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Chang CH., Monselise M., Yang C.C. What are people concerned about during the pandemic? Detecting evolving topics about COVID-19 from Twitter. J Healthc Inform Res. 2021;5:70–97. doi: 10.1007/s41666-020-00083-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Nowak S.A., Chen C., Parker A.M., Gidengil C.A., Matthews L.J. Comparing covariation among vaccine hesitancy and broader beliefs within Twitter and survey data. PLoS ONE. 2020;15(10) doi: 10.1371/journal.pone.0239826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Tavoschi L., Quattrone F., D'Andrea E., et al. Twitter as a sentinel tool to monitor public opinion on vaccination: an opinion mining analysis from September 2016 to August 2017 in Italy. Hum Vaccines Immunother. 2020;16(5):1062–1069. doi: 10.1080/21645515.2020.1714311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Berenson AB, Chang M, Hirth JM, Kanukurthy M. Intent to get vaccinated against COVID-19 among reproductive-aged women in Texas. Hum Vaccin Immunother. 2021;17(9):2914–2918. doi: 10.1080/21645515.2021.1918994. Epub 2021 Jun 3. PMID: 34081572; PMCID: PMC8381790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Gottlieb M, Dyer S. Information and disinformation: social media in the COVID-19 crisis. Acad Emerg Med. 2020;27(7):640–641. doi: 10.1111/acem.14036. Epub 2020 Jun 24. PMID: 32474977; PMCID: PMC7300599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Bonnevie E., Rosenberg S.D., Kummeth C., Goldbarg J., Wartella E., Smyser J. Using social media influencers to increase knowledge and positive attitudes toward the flu vaccine. PLoS ONE. 2020;15(10) doi: 10.1371/journal.pone.0240828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Bonnevie E., Smith S.M., Kummeth C., Goldbarg J., Smyser J. Social media influencers can be used to deliver positive information about the flu vaccine: findings from a multi-year study. Health Educ Res. 2021;36(3):286–294. doi: 10.1093/her/cyab018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Colleoni E., Rozza A., Arvidsson A. Echo chamber or public sphere? Predicting political orientation and measuring political homophily in Twitter using big data. J Commun. 2014;64(2):317–332. [Google Scholar]
- 111.Mønsted B., Lehmann S. Characterizing polarization in online vaccine discourse-a large-scale study. PLoS ONE. 2022;17(2) doi: 10.1371/journal.pone.0263746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Zhang Z., Feng G., Xu J., et al. The impact of public health events on COVID-19 vaccine hesitancy on Chinese social media: national infoveillance study. JMIR Public Health Surveill. 2021;7(11):e32936. doi: 10.2196/32936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Alam KN, Khan MS, Dhruba AR, et al. Deep learning-based sentiment analysis of COVID-19 vaccination responses from Twitter data. Comput Math Methods Med. 2021;2021:1–15. doi: 10.1155/2021/4321131. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 114.Yu L., Chen H., Luo W., Li C. Online public opinion evaluation through the functional resonance analysis method and deep analysis. PLoS ONE. 2021;16(12) doi: 10.1371/journal.pone.0261009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Tasnim S., Hossain M.M., Mazumder H. Impact of rumors and misinformation on COVID-19 in social media. J Prev Med Public Health. 2020;53(3):171–174. doi: 10.3961/jpmph.20.094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Baj-Rogowska A. Mapping of the Covid-19 vaccine uptake determinants from mining Twitter data. IEEE Access. 2021;9:134929–134944. doi: 10.1109/ACCESS.2021.3115554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Burger R., Köhler T., Golos A.M., et al. Longitudinal changes in COVID-19 vaccination intent among South African adults: evidence from the NIDS-CRAM panel survey, February to May 2021. BMC Public Health. 2022;22(1):422. doi: 10.1186/s12889-022-12826-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Citu IM, Citu C, Gorun F, et al. Determinants of COVID-19 vaccination hesitancy among romanian pregnant women. Vaccines (Basel) 2022;10(2):275. doi: 10.3390/vaccines10020275. PMID: 35214732; PMCID: PMC8874778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Cui Y., Binger K.S., Tsaih S.W., Palatnik A. Factors of COVID-19 vaccine hesitancy during pregnancy: a cross-sectional study. Am J Obstet Gynecol. 2022;226(1):S306. [Google Scholar]
- 120.Ghaddar A., Khandaqji S., Awad Z., Kansoun R. Conspiracy beliefs and vaccination intent for COVID-19 in an infodemic. PLoS ONE. 2022;17(1) doi: 10.1371/journal.pone.0261559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Jabbour D, Masri JE, Nawfal R, Malaeb D, Salameh P. Social media medical misinformation: impact on mental health and vaccination decision among university students. Ir J Med Sci. 2022:1–11. doi: 10.1007/s11845-022-02936-9. Epub ahead of print. PMID: 35119644; PMCID: PMC8814778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Jafar A, Mapa MT, Sakke N, et al. Vaccine hesitancy in East Malaysia (Sabah): a survey of the national COVID-19 immunisation programme. Geospat Health. 2022;17(s1):1037. doi: 10.4081/gh.2022.1037. [DOI] [PubMed] [Google Scholar]
- 123.Lee C., Holroyd T.A., Gur-Arie R., et al. COVID-19 vaccine acceptance among Bangladeshi adults: understanding predictors of vaccine intention to inform vaccine policy. PLoS ONE. 2022;17(1) doi: 10.1371/journal.pone.0261929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Mascherini M, Nivakoski S. Social media use and vaccine hesitancy in the European Union. Vaccine. 2022;40(14):2215–2225. doi: 10.1016/j.vaccine.2022.02.059. Epub 2022 Mar 3. PMID: 35249775; PMCID: PMC8893322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Mose A., Haile K., Timerga A. COVID-19 vaccine hesitancy among medical and health science students attending Wolkite University in Ethiopia. PLoS ONE. 2022;17(1) doi: 10.1371/journal.pone.0263081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Othman S.S., Alsuwaidi A., Aseel R., et al. Association between social media use and the acceptance of COVID-19 vaccination among the general population in Saudi Arabia - a cross-sectional study. BMC Public Health. 2022;22(1):375. doi: 10.1186/s12889-022-12757-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Ouyang H., Ma X., Wu X. The prevalence and determinants of COVID-19 vaccine hesitancy in the age of infodemic. Hum Vaccines Immunother. 2022;18(1) doi: 10.1080/21645515.2021.2013694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Ezati Rad R., Kahnouji K., Mohseni S., et al. Predicting the COVID-19 vaccine receive intention based on the theory of reasoned action in the south of Iran. BMC Public Health 22. 2022;229:12889. doi: 10.1186/s12889-022-12517-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Tan M., Straughan P.T., Cheong G. Information trust and COVID-19 vaccine hesitancy amongst middle-aged and older adults in Singapore: a latent class analysis approach. Soc Sci Med. 2022;296 doi: 10.1016/j.socscimed.2022.114767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Al-Marshoudi S, Al-Balushi H, Al-Wahaibi A, et al. Knowledge, attitudes, and practices (KAP) toward the COVID-19 vaccine in Oman: a pre-campaign cross-sectional study. Vaccines (Basel) 2021;9(6):602. doi: 10.3390/vaccines9060602. PMID: 34200001; PMCID: PMC8228881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Al-Mulla R., Abu-Madi M., Talafha Q.M., Tayyem R.F., Abdallah A.M. COVID-19 vaccine hesitancy in a representative education sector population in Qatar. Vaccines. 2021;9(6) doi: 10.3390/vaccines9060665. (Basel) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Al-Wutayd O., Khalil R., Rajar A.B. Sociodemographic and behavioral predictors of COVID-19 vaccine hesitancy in Pakistan. J Multidiscip Healthc. 2021;14:2847–2856. doi: 10.2147/JMDH.S325529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Allington D., McAndrew S., Moxham-Hall V.L., Duffy B. Media usage predicts intention to be vaccinated against SARS-CoV-2 in the US and the UK. Vaccine. 2021;39(18):2595–2603. doi: 10.1016/j.vaccine.2021.02.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Alley S.J., Stanton R., Browne M., et al. As the pandemic progresses, how does willingness to vaccinate against COVID-19 evolve? Int J Environ Res Public Health. 2021;18(2) doi: 10.3390/ijerph18020797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Al-Hasan A., Khuntia J., Yim D. Does seeing what others do through social media influence vaccine uptake and help in the herd immunity through vaccination? A cross-sectional analysis. Front Public Health. 2021;9 doi: 10.3389/fpubh.2021.715931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Alfatease A., Alqahtani A.M., Orayj K., Alshahrani S.M. The impact of social media on the acceptance of the COVID-19 vaccine: a cross-sectional study from Saudi Arabia. Patient Prefer Adherence. 2021;15:2673–2681. doi: 10.2147/PPA.S342535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Allington D, McAndrew S, Moxham-Hall V, Duffy B. Coronavirus conspiracy suspicions, general vaccine attitudes, trust and coronavirus information source as predictors of vaccine hesitancy among UK residents during the COVID-19 pandemic. Psychol Med. 2021:1–12. doi: 10.1017/S0033291721001434. Epub ahead of print. PMID: 33843509; PMCID: PMC8111194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Brailovskaia J., Schneider S., Margraf J. To vaccinate or not to vaccinate!? Predictors of willingness to receive Covid-19 vaccination in Europe, the U.S., and China. PLoS ONE. 2021;16(12) doi: 10.1371/journal.pone.0260230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Barry M, Temsah MH, Aljamaan F, et al. COVID-19 vaccine uptake among healthcare workers in the fourth country to authorize BNT162b2 during the first month of rollout. Vaccine. 2021;39(40):5762–5768. doi: 10.1016/j.vaccine.2021.08.083. Epub 2021 Sep 2. PMID: 34481700; PMCID: PMC8410227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Bhagianadh D, Arora K. Covid-19 vaccine hesitancy among community-dwelling older adults: The role of information sources. Journal of Applied Gerontology. 2021;41(1):4–11. doi: 10.1177/07334648211037507. [DOI] [PubMed] [Google Scholar]
- 141.Coughenour C., Gakh M., Sharma M., Labus B., Chien L.C. Assessing determinants of COVID-19 vaccine hesitancy in Nevada. Health Secur. 2021;19(6):592–604. doi: 10.1089/hs.2021.0079. [DOI] [PubMed] [Google Scholar]
- 142.Dambadarjaa D, Altankhuyag GE, Chandaga U, et al. Factors Associated with COVID-19 Vaccine Hesitancy in Mongolia: A Web-Based Cross-Sectional Survey. Int J Environ Res Public Health. 2021 Dec 7;18(24):12903. doi: 10.3390/ijerph182412903. PMID: 34948511; PMCID: PMC8701794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Hatton C., Bailey T., Bradshaw J., et al. The willingness of UK adults with intellectual disabilities to take COVID-19 vaccines. J Intellect Disabil Res. 2021;65(11):949–961. doi: 10.1111/jir.12884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Horiuchi S., Sakamoto H., Abe S.K., et al. Factors of parental COVID-19 vaccine hesitancy: a cross sectional study in Japan. PLoS ONE. 2021;16(12) doi: 10.1371/journal.pone.0261121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Jain L., Vij J., Satapathy P., et al. Factors Influencing COVID-19 vaccination intentions among college students: a cross-sectional study in India. Front Public Health. 2021;9 doi: 10.3389/fpubh.2021.735902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Marinos G, Lamprinos D, Georgakopoulos P, et al. Reported COVID-19 vaccination coverage and associated factors among members of athens medical association: results from a cross-sectional study. Vaccines (Basel) 2021;9(10):1134. doi: 10.3390/vaccines9101134. PMID: 34696242; PMCID: PMC8540685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Mir H.H., Parveen S., Mullick N.H., Nabi S. Using structural equation modeling to predict Indian people's attitudes and intentions towards COVID-19 vaccination. Diabetes Metab Syndr. 2021;15(3):1017–1022. doi: 10.1016/j.dsx.2021.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Mo PK, Luo S, Wang S, et al. Intention to receive the COVID-19 vaccination in China: application of the diffusion of innovations theory and the moderating role of openness to experience. vaccines (Basel). 2021;9(2):129. 10.3390/vaccines9020129. PMID: 33562894; PMCID: PMC7915878 [DOI] [PMC free article] [PubMed]
- 149.Karabela Ş.N., Coşkun F., Hoşgör H. Investigation of the relationships between perceived causes of COVID-19, attitudes towards vaccine and level of trust in information sources from the perspective of Infodemic: the case of Turkey. BMC Public Health. 2021;21(1):1195. doi: 10.1186/s12889-021-11262-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Park Y.J., Farooq J., Cho J., et al. Fighting the war against COVID-19 via cell-based regenerative medicine: lessons learned from 1918 Spanish Flu and other previous pandemics. Stem Cell Rev Rep. 2021;17(1):9–32. doi: 10.1007/s12015-020-10026-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Piltch-Loeb R., Savoia E., Goldberg B., et al. Examining the effect of information channel on COVID-19 vaccine acceptance. PLoS ONE. 2021;16(5) doi: 10.1371/journal.pone.0251095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Riad A, Abdulqader H, Morgado M, et al. Global prevalence and drivers of dental students' COVID-19 vaccine hesitancy. Vaccines (Basel) 2021;9(6):566. doi: 10.3390/vaccines9060566. PMID: 34072500; PMCID: PMC8226539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Romer D., Jamieson K.H. Patterns of media use, strength of belief in COVID-19 conspiracy theories, and the prevention of COVID-19 from March to July 2020 in the United States: survey study. J Med Internet Res. 2021;23(4):e25215. doi: 10.2196/25215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Ruiz J.B., Bell R.A. Predictors of intention to vaccinate against COVID-19: results of a nationwide survey. Vaccine. 2021;39(7):1080–1086. doi: 10.1016/j.vaccine.2021.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Riad A, Jouzová A, Üstün B, et al. COVID-19 vaccine acceptance of pregnant and lactating women (PLW) in Czechia: an analytical cross-sectional study. Int J Environ Res Public Health. 2021;18(24):13373. doi: 10.3390/ijerph182413373. PMID: 34948987; PMCID: PMC8708407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Reno C., Maietti E., Di Valerio Z., Montalti M., Fantini M.P., Gori D. Vaccine hesitancy towards COVID-19 vaccination: investigating the role of information sources through a mediation analysis. Infect Dis Rep. 2021;13(3):712–723. doi: 10.3390/idr13030066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Sallam M., Dababseh D., Eid H., et al. Low covid-19 vaccine acceptance is correlated with conspiracy beliefs among university students in Jordan. Int J Environ Res Public Health. 2021;18(5):2407. doi: 10.3390/ijerph18052407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Zimand-Sheiner D, Kol O, Frydman S, Levy S. To Be (Vaccinated) or not to be: the effect of media exposure, institutional trust, and incentives on attitudes toward COVID-19 vaccination. Int J Environ Res Public Health. 2021;18(24):12894. doi: 10.3390/ijerph182412894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Sirikalyanpaiboon M., Ousirimaneechai K., Phannajit J., et al. COVID-19 vaccine acceptance, hesitancy, and determinants among physicians in a university-based teaching hospital in Thailand. BMC Infect Dis. 2021;21:1174. doi: 10.1186/s12879-021-06863-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Singh A., Lai A.H.Y., Wang J., et al. Multilevel determinants of COVID-19 vaccine uptake among south Asian ethnic minorities in Hong Kong: cross-sectional web-based survey. JMIR Public Health Surveill. 2021;7(11):e31707. doi: 10.2196/31707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Strathdee SA, Abramovitz D, Harvey-Vera A, et al. Correlates of coronavirus disease 2019 (COVID-19) vaccine hesitancy among people who inject drugs in the San Diego-Tijuana Border Region. Clin Infect Dis. 2021:ciab975. doi: 10.1093/cid/ciab975. Epub ahead of print. PMID: 35024825; PMCID: PMC8690110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Zhang K.C., Fang Y., Cao H., et al. Behavioral intention to receive a COVID-19 vaccination among Chinese factory workers: cross-sectional online survey. J Med Internet Res. 2021;23(3):e24673. doi: 10.2196/24673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Wang K., Wong E.L., Cheung A.W., et al. Influence of vaccination characteristics on COVID-19 vaccine acceptance among working-age people in Hong Kong, China: a discrete choice experiment. Front Public Health. 2021;9 doi: 10.3389/fpubh.2021.793533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Šiđanin I, Njegovan BR, Sokolović B. Students' Views on Vaccination against COVID-19 virus and trust in media information about the vaccine: the case of Serbia. Vaccines (Basel) 2021;9(12):1430. doi: 10.3390/vaccines9121430. PMID: 34960176; PMCID: PMC8704984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Zhang K.C., Fang Y., Cao H., et al. Parental acceptability of COVID-19 vaccination for children under the age of 18 years: cross-sectional online survey. JMIR Pediatr Parent. 2020;3(2):e24827. doi: 10.2196/24827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Ginossar T., Cruickshank I.J., Zheleva E., Sulskis J., Berger-Wolf T. Cross-platform spread: vaccine-related content, sources, and conspiracy theories in YouTube videos shared in early Twitter COVID-19 conversations. Hum Vaccines Immunother. 2022;18(1):1–13. doi: 10.1080/21645515.2021.2003647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Tsao S.F., MacLean A., Chen H., Li L., Yang Y., Butt Z.A. Public attitudes during the second lockdown: sentiment and topic analyses using tweets from Ontario, Canada. Int J Public Health. 2022;67 doi: 10.3389/ijph.2022.1604658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Zakharchenko O., Avramenko R., Zakharchenko A., et al. Multifaceted nature of social media content propagating COVID-19 vaccine hesitancy: Ukrainian case. Proced Comput Sci. 2022;198:682–687. doi: 10.1016/j.procs.2021.12.306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Baj-Rogowska A. Mapping of the Covid-19 vaccine uptake determinants from mining Twitter data. IEEE Access. 2021;9:134929–134944. doi: 10.1109/ACCESS.2021.3115554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Griffith J., Marani H., Monkman H. COVID-19 vaccine hesitancy in Canada: content analysis of Tweets using the theoretical domains framework. J Med Internet Res. 2021;23(4):e26874. doi: 10.2196/26874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Guntuku S.C., Buttenheim A.M., Sherman G., Merchant R.M. Twitter discourse reveals geographical and temporal variation in concerns about COVID-19 vaccines in the United States. Vaccine. 2021;39(30):4034–4038. doi: 10.1016/j.vaccine.2021.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Hughes B, Miller-Idriss C, Piltch-Loeb R, Goldberg B, White K, Criezis M, Savoia E. Development of a codebook of online anti-vaccination rhetoric to manage COVID-19 vaccine misinformation. Int J Environ Res Public Health. 2021;18(14):7556. doi: 10.3390/ijerph18147556. PMID: 34300005; PMCID: PMC8304769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Jiang L.C., Chu T.H., Sun M. Characterization of vaccine tweets during the early stage of the COVID-19 outbreak in the united states: topic modeling analysis. JMIR Infodemiology. 2021;1(1):e25636. doi: 10.2196/25636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Lee C.S., Goh D.H.L., Tan H.W., Zheng H., Theng Y.L. Understanding the temporal effects on tweetcussion of COVID-19 vaccine. Proc Assoc Inf Sci Technol. 2021;58(1):768–770. doi: 10.1002/pra2.556. Association for Information Science and Technology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Zhang J., Wang Y., Shi M., Wang X. Factors driving the popularity and virality of COVID-19 vaccine discourse on Twitter: text mining and data visualization study. JMIR Public Health Surveill. 2021;7(12):e32814. doi: 10.2196/32814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Lyu H., Wang J., Wu W., et al. Social media study of public opinions on potential COVID-19 vaccines: informing dissent, disparities, and dissemination. Intell Med. 2022;2(1):1–12. doi: 10.1016/j.imed.2021.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Herrera-Añazco P., Uyen-Cateriano Á., Urrunaga-Pastor D., et al. Prevalence and factors associated with the intention to be vaccinated against COVID-19 in Peru. Rev Peru Med Exp Salud Publica. 2021;38(3):381–390. doi: 10.17843/rpmesp.2021.383.7446. [DOI] [PubMed] [Google Scholar]
- 178.Wawrzuta D, Jaworski M, Gotlib J, Panczyk M. What arguments against COVID-19 vaccines run on facebook in Poland: content analysis of comments. Vaccines. 2021;9(5):481. doi: 10.3390/vaccines9050481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Yan C, Law M, Nguyen S, Cheung J, Kong J. Comparing public sentiment toward COVID-19 vaccines across canadian cities: analysis of comments on reddit. J Med Internet Res. 2021;23(9):e32685. doi: 10.2196/32685. PMID: 34519654; PMCID: PMC8477909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Gokhale S.S. Proceedings of the IEEE International Conference On Parallel & Distributed Processing with Applications, Big Data & Cloud Computing, Sustainable Computing & Communications, Social Computing & Networking (ISPA/BDCloud/SocialCom/SustainCom) IEEE; 2020. Monitoring the perception of Covid-19 vaccine using topic models. [Google Scholar]
- 181.Amanatidis D, Mylona I, Kamenidou I, Mamalis S, Stavrianea A. Mining textual and imagery instagram data during the COVID-19 pandemic. Applied Sciences. 2021;11(9):4281. doi: 10.3390/app11094281. [DOI] [Google Scholar]
- 182.Batra R, Imran AS, Kastrati Z, Ghafoor A, Daudpota SM, Shaikh S. Evaluating polarity trend amidst the coronavirus crisis in peoples’ attitudes toward the vaccination drive. Sustainability. 2021;13(10):5344. doi: 10.3390/su13105344. [DOI] [Google Scholar]
- 183.Jemielniak D., Krempovych Y. An analysis of AstraZeneca COVID-19 vaccine misinformation and fear mongering on Twitter. Public Health. 2021;200:4–6. doi: 10.1016/j.puhe.2021.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Luo C., Chen A., Cui B., Liao W. Exploring public perceptions of the COVID-19 vaccine online from a cultural perspective: semantic network analysis of two social media platforms in the United States and China. Telemat Inform. 2021;65 doi: 10.1016/j.tele.2021.101712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Biswas R., Alam T., Househ M., Shah Z. Public Sentiment Towards Vaccination After COVID-19 Outbreak in the Arab World. Stud Health Technol Inform. 2022;289:57–60. doi: 10.3233/SHTI210858. [DOI] [PubMed] [Google Scholar]
- 186.Huangfu L., Mo Y., Zhang P., Zeng D.D., He S. COVID-19 vaccine Tweets after vaccine rollout: sentiment-based topic modeling. J Med Internet Res. 2022;24(2):e31726. doi: 10.2196/31726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Zhang C., Xu S., Li Z., Liu G., Dai D., Dong C. The evolution and disparities of online attitudes toward COVID-19 vaccines: year-long longitudinal and cross-sectional study. J Med Internet Res. 2022;24(1):e32394. doi: 10.2196/32394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Alam K.N., Khan M.S., Dhruba A.R., et al. Deep learning-based sentiment analysis of COVID-19 vaccination responses from Twitter data. Comput Math Methods Med. 2021;2021 doi: 10.1155/2021/4321131. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 189.Ali R.N., Rubin H., Sarkar S. Countering the potential re-emergence of a deadly infectious disease-Information warfare, identifying strategic threats, launching countermeasures. PLoS ONE. 2021;16(8) doi: 10.1371/journal.pone.0256014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Ansari M.T.J., Khan N.A. Worldwide COVID-19 vaccines sentiment analysis through twitter content. Electronic Journal of General Medicine. 2021;18(6) [Google Scholar]
- 191.Carrasco-Polaino R., Martin-Cardaba M.A., Villar-Cirujano E. Citizen participation in Twitter: anti-vaccine controversies in times of COVID-19. Comunicar. 2021;29(69):21–31. [Google Scholar]
- 192.Gao H., Guo D., Wu J., Zhao Q., Li L. Changes of the public attitudes of China to domestic COVID-19 vaccination after the vaccines were approved: a semantic network and sentiment analysis based on sina weibo texts. Front Public Health. 2021;9 doi: 10.3389/fpubh.2021.723015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Gao H, Zhao Q, Ning C, Guo D, Wu J, Li L. Does the COVID-19 vaccine still work that “most of the confirmed cases had been vaccinated”? A content analysis of vaccine effectiveness discussion on sina weibo during the outbreak of COVID-19 in Nanjing. Int J Environ Res Public Health. 2022;19(1):241. doi: 10.3390/ijerph19010241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Gori D., Durazzi F., Montalti M., et al. Mis-tweeting communication: a vaccine hesitancy analysis among twitter users in Italy. Acta Biomed. 2021;92(S6) doi: 10.23750/abm.v92iS6.12251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Melton C., Olusanya O.A., Shaban-Nejad A. Network analysis of COVID-19 vaccine misinformation on social media. Stud Health Technol Inform. 2021;287:165–166. doi: 10.3233/SHTI210839. [DOI] [PubMed] [Google Scholar]
- 196.Mir A.A., Rathinam S., Gul S. (2021, January 1). Public perception of covid-19 vaccines from the digital footprints left on Twitter: Analyzing positive, neutral and negative sentiments of Twitterati. Library Hi Tech. 2022 https://pesquisa.bvsalud.org/global-literature-on-novel-coronavirus-2019-ncov/resource/pt/covidwho-1476018 Retrieved January 1from. [Google Scholar]
- 197.Yoder N.D., Pecoriello J., Smith M.B., Blakemore J.K. Overall positive posts after introduction of Covid-19 vaccine on fertility-related social media. Fertil Steril. 2021;116(3):e298. doi: 10.1080/13625187.2023.2189501. -e. [DOI] [PubMed] [Google Scholar]
- 198.Yousefinaghani S., Dara R., Mubareka S., Papadopoulos A., Sharif S. An analysis of COVID-19 vaccine sentiments and opinions on Twitter. Int J Infect Dis. 2021;108:256–262. doi: 10.1016/j.ijid.2021.05.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Zhang J, Wang Y, Shi M, Wang X. Factors driving the popularity and virality of COVID-19 vaccine discourse on Twitter: text mining and data visualization study. JMIR Public Health Surveill. 2021;7(12):e32814. doi: 10.2196/32814. PMID: 34665761; PMCID: PMC8647971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Jin J., Lam S., Savas O., McCulloh I. Proceedings of the IEEE/ACM International Conference on Advances in Social Networks Analysis and Mining (ASONAM) 2020. Approaches for quantifying video prominence, narratives, & discussion: engagement on COVID-19 related YouTube Videos. Dec 07-10Electr Network2020. [Google Scholar]
- 201.Chang CH., Monselise M., Yang C.C. What are people concerned about during the pandemic? detecting evolving topics about COVID-19 from Twitter. J Healthc Inform Res. 2021;5:70–97. doi: 10.1007/s41666-020-00083-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Fazel M., Puntis S., White S.R., et al. Willingness of children and adolescents to have a COVID-19 vaccination: results of a large whole schools survey in England. eClinicalMedicine. 2021;40 doi: 10.1016/j.eclinm.2021.101144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Gerts D., Shelley C.D., Parikh N., et al. Thought I'd share first" and other conspiracy theory tweets from the COVID-19 infodemic: exploratory study. JMIR Public Health Surveill. 2021;7(4):e26527. doi: 10.2196/26527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Hu T, Wang S, Luo W, Zhang M. Revealing public opinion towards COVID-19 vaccines with twitter data in the United States: spatiotemporal perspective. J Med Internet Res. 2021;23(9):e30854. doi: 10.2196/30854. PMID: 34346888; PMCID: PMC8437406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Kumar N., Corpus I., Hans M., et al. COVID-19 vaccine perceptions in the initial phases of US vaccine roll-out: an observational study on reddit. BMC Public Health. 2022;22(1):446. doi: 10.1186/s12889-022-12824-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.