Graphical abstract

Keywords: Late embolization, Paravalvular, Plug, Vascular
Highlights
-
•
Vascular plugs used for PVL repair usually embolize late after deployment.
-
•
A low threshold for echo studies (namely TEE) is an essential part of clinical follow-up.
-
•
Redo percutaneous PVL closure should be considered in those at high surgical risk.
Introduction
Paravalvular regurgitation is known to be a delayed complication of the surgical replacement of mitral and aortic valves, occurring about twice as often in mitral replacements than in aortic replacements.1 In rare instances, patients can present with heart failure symptoms when the regurgitation is severe, especially when other cardiopulmonary comorbidities exist, resulting in a high surgical risk situation. In these cases, transcutaneous intervention is often the last resort to turn a known poor prognosis into a more favorable one. We report a case of late embolization of a vascular plug used for the closure of mitral paravalvular regurgitation. Figure 1 delineates the chronological sequence of events.
Figure 1.
The chronological progression of the patient's multiple mitral valve replacements and percutaneous deployment of multiple vascular plugs is shown. AV, Aortic valve; CT, computed tomography; HF, heart failure; HOCM, hypertrophic obstructive cardiomyopathy; MV, mitral valve.
Case Presentation
A 55-year-old morbidly obese woman presented with progressive shortness of breath consistent with New York Heart Association functional class III heart failure. Her medical history included coronary artery disease, paroxysmal atrial fibrillation, chronic kidney disease (stage III-a), sarcoidosis, pulmonary and systemic hypertension, biventricular implantable cardioverter-defibrillator placement, myomectomy for hypertrophic obstructive cardiomyopathy 10 years prior, and redo sternotomy with a 29 mm cinch porcine mitral valve and 23 mm pericardial aortic bioprosthesis for severe valvular regurgitation 4 years prior. She also had undergone a second redo sternotomy 2 years prior for severe mitral regurgitation secondary to both partial dehiscence of the valve prosthesis and a torn valvular cusp. At that time, a 29 mm bileaflet mechanical mitral valve was placed, requiring anticoagulation with warfarin, and her aortic bioprothesis was functioning normally. During her follow-up 1 year later, she was in functional class III heart failure and had hemolytic anemia. Further investigation with transesophageal echocardiography (TEE) showed a large anterolateral paravalvular leak (PVL) with the presence of systolic flow reversal in the pulmonary veins. The defect was measured to be 1.2 × 0.8 cm by three-dimensional planimetry. At that point, the PVL was treated by the percutaneous deployment of a 12 mm vascular plug device with a residual trace PVL around the plug.
The patient's cardiac status remained stable initially; however, she presented to the clinic 11 months postdeployment of the vascular plug with worsening dyspnea. TEE showed a normal motion of the tilting disks and a significant paravalvular mitral regurgitant jet around the vascular plug (Figure 2; Videos 1 and 2) with an effective regurgitant orifice area of 40 mm2 and a regurgitant volume of 56 mL using the proximal isovelocity surface area method.
Figure 2.
Transesophageal echocardiogram at 11-month follow-up after initial deployment of vascular plug. (A) Two-dimensional TEE, zoomed mitral valve view at 90°. The yellow arrow shows the plug, and the green arrow demonstrates the midsystolic color flow Doppler jet representing the PVL around the plug. (B) Three-dimensional TEE, zoomed “surgeon's view” of the mitral valve showing the 12 mm vascular plug (yellow arrow).
Escalation of diuresis was implemented and provided a short-lived relief before the patient's constellation of symptoms became refractory to the medication regimen. TEE was performed 17 months after vascular deployment, demonstrating the absence of the vascular plug in the paravalvular location and a worsening of the PVL (Figure 3; Video 3).
Figure 3.
Transesophageal echocardiogram at 17 months. (A) Two-dimensional TEE, midsystolic zoomed view of the mitral valve at 90° with the paravalvular gap (yellow arrow). (B) Two-dimensional TEE, midsystolic zoomed view of the mitral valve at the same angle with the color flow Doppler (green arrow) demonstrating the paravalvular regurgitant jet. (C) Three-dimensional TEE zoomed “surgeon's view” of the mitral valve demonstrating the absence of the 12 mm vascular plug (red arrow).
The strong suspicion of vascular plug embolization led to a computed tomography angiogram of the abdominal aorta and the iliofemoral system with leg runoffs bilaterally. The vascular plug was identified in the proximal left external iliac artery; there was no clinical evidence of associated vascular injury or occlusion as shown by multiplanar reconstruction and three-dimensional volume-rendered images from the computed tomography angiography. The vascular plug was successfully retrieved surgically (Figure 4).
Figure 4.
(A) Three-dimensional volume rendering of the pelvic arteries using 256-slice computed tomography angiography demonstrates the plug embolized into the proximal portion of the left external iliac artery (arrow). (B) Multiplanar reconstruction image showing the absence of vascular injury in all three planes. (C) Gross presentation of the retrieved 12 mm vascular plug.
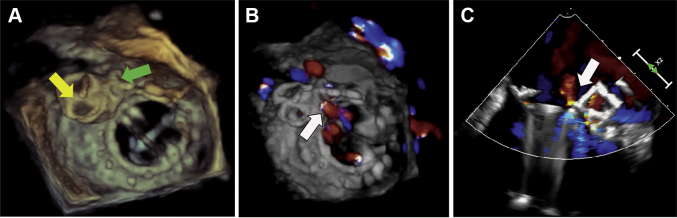
Owing to the high surgical risk associated with a third redo sternotomy, the patient was treated percutaneously with a transcatheter deployment of two side-by-side vascular plugs—16 × 12 mm and 10 × 7 mm (Figure 5A), resulting in a substantial improvement of the PVL (Figure 5B and C). It was confirmed by TEE that there was no leaflet impingement, and only a mild residual leak was noted around the device (Video 4). At her 1-month follow-up in the outpatient clinic, the patient's heart failure symptoms had improved.
Figure 5.
Postintervention TEE. (A) Three-dimensional TEE “surgeon's view” of the mitral valve showing the newly deployed 16 mm (yellow arrow) and 10 mm (green arrow) vascular plugs positioned side by side. (B) Three-dimensional TEE “surgeon's view” of the mitral valve and (C) two-dimensional TEE of the mitral valve; both are midsystolic views with color flow Doppler at 140° demonstrating a mild residual PVL (white arrows) adjacent to the device.
Discussion
The success rate of the percutaneous approach with transcatheter closure of PVLs has been well documented recently, and this approach has become a viable alternative to surgical valve repair of moderate to severe paravalvular regurgitation.2,3 Here we present a late embolization of an appropriately sized vascular plug in a patient at high surgical risk who previously had had two redo sternotomies and mitral valve replacements where the role of TEE to optimally visualize these plugs was essential.
One can hypothesize that the lack of sufficient endothelialization of the vascular plug—demonstrated by visual inspection upon surgical retrieval—is a possible explanation for progressive displacement of the device from its initially well-seated position. Further, having the patient on low-dose aspirin in addition to her much-needed warfarin could have truncated the appropriate degree of endothelialization. Additionally, the cumulative detrimental effect of the regurgitant flow around the vascular plug should be taken into consideration. As these plugs sometimes are not well visualized by transthoracic echocardiography, TEE is required in symptomatic patients for diagnosis. When the embolization of the vascular plug was identified, the severe paravalvular regurgitation through an irregularly shaped orifice was treated with a high degree of expertise using two vascular plugs side by side.
Conclusion
Redo percutaneous PVL closure can be challenging but should be strongly considered in patients at high surgical risk when a redo sternotomy is the sole alternative. Serial echocardiographic monitoring with a low threshold for performing TEE, as demonstrated in this case, is highly recommended to assess device displacement, especially if the patient develops heart failure symptoms.
Footnotes
Conflicts Interest: The authors reported no actual or potential conflicts of interest relative to this document.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.case.2021.11.003.
Supplementary Data
Transesophageal echocardiogram at 11-month follow-up after initial deployment of vascular plug. (A) Three-dimensional TEE “surgeon's view” of the mitral valve showing the vascular plug at the 11 o'clock position. (B) Three-dimensional TEE volume-rendered view of the mitral valve with significant paravalvular mitral regurgitant jet (color flow Doppler) around the vascular plug at the 12 o'clock position.
Transesophageal echocardiogram at 11-month follow-up after initial deployment of vascular plug with a two-dimensional view at 130° demonstrating the significant paravalvular mitral regurgitant jet (color flow) around the vascular plug hugging the wall of the left atrium.
Transesophageal echocardiogram at 17 months after initial deployment of vascular plug. (A) Three-dimensional TEE “surgeon's view” of the mitral valve demonstrating the absence of the vascular plug at the 10 o'clock position. (B) Three-dimensional TEE volume-rendered view of the mitral valve demonstrating a significant PVL (color flow Doppler at the 10 o'clock position) through the orifice where the vascular plug should have been noted.
Transesophageal echocardiogram three-dimensional volume-rendered view of the mitral valve after deployment of the two side-by-side vascular plugs (10 o'clock) with mild residual leak around the device (color flow Doppler at 11 o'clock).
References
- 1.Ruiz C.E., Jelnin V., Kronzon I., Dudiy Y., Del Valle-Fernandez R., Einhorn B.N., et al. Clinical outcomes in patients undergoing percutaneous closure of periprosthetic paravalvular leaks. J Am Coll Cardiol. 2011;58:2210–2217. doi: 10.1016/j.jacc.2011.03.074. [DOI] [PubMed] [Google Scholar]
- 2.Sorajja P., Cabalka A.K., Hagler D.J., Rihal C.S. Long-term follow-up of percutaneous repair of paravalvular prosthetic regurgitation. J Am Coll Cardiol. 2011;58:2218–2224. doi: 10.1016/j.jacc.2011.07.041. [DOI] [PubMed] [Google Scholar]
- 3.Arzamendi D., Li C.H., Serra A. Late embolization of a vascular plug III device after mitral paravalvular leak closure. Catheter Cardiovasc Interv. 2013;82:E831–E834. doi: 10.1002/ccd.25039. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Transesophageal echocardiogram at 11-month follow-up after initial deployment of vascular plug. (A) Three-dimensional TEE “surgeon's view” of the mitral valve showing the vascular plug at the 11 o'clock position. (B) Three-dimensional TEE volume-rendered view of the mitral valve with significant paravalvular mitral regurgitant jet (color flow Doppler) around the vascular plug at the 12 o'clock position.
Transesophageal echocardiogram at 11-month follow-up after initial deployment of vascular plug with a two-dimensional view at 130° demonstrating the significant paravalvular mitral regurgitant jet (color flow) around the vascular plug hugging the wall of the left atrium.
Transesophageal echocardiogram at 17 months after initial deployment of vascular plug. (A) Three-dimensional TEE “surgeon's view” of the mitral valve demonstrating the absence of the vascular plug at the 10 o'clock position. (B) Three-dimensional TEE volume-rendered view of the mitral valve demonstrating a significant PVL (color flow Doppler at the 10 o'clock position) through the orifice where the vascular plug should have been noted.
Transesophageal echocardiogram three-dimensional volume-rendered view of the mitral valve after deployment of the two side-by-side vascular plugs (10 o'clock) with mild residual leak around the device (color flow Doppler at 11 o'clock).