Abstract
Study Design:
Retrospective review.
Objective:
Identify surgical complex adult spine deformity patients who are at increased risk for an unplanned postoperative 90-day readmission and/or reoperation.
Methods:
A total of 227 consecutive records of complex adult (≥18 years old) spine deformity surgeries from 2015 to 2018 were reviewed. Demographics, comorbidities, operative details, and postoperative complication data was collected. Chi-square/Fisher’s exact test and t tests were used for bivariate analysis. To determine independent predictors for readmissions/reoperations, stepwise multivariate logistic regressions were employed. The C-statistic and Hosmer-Lemeshow (HL) value was used to measure concordance and goodness of fit.
Results:
Average age was 50.5 ± 17.8 years and 67.8% were female. Ninety-day readmission and reoperation rates were 7.0% and 5.3%, respectively. Median number of days after index discharge date resulting in readmission and reoperation were 16.5 and 28, respectively. The multivariate regression for 90-day readmissions included pulmonary comorbidity, depression, history of deep vein thrombosis/pulmonary embolism (DVT/PE), and gastrointestinal comorbidity (C-statistic = 0.82; HL = 0.79). Pulmonary comorbidity, depression, and history of DVT/PE increased risk for 90-day readmission by 5-, 3.5-, and 10.2-fold, respectively. The multivariate regression for 90-day reoperations was similar to readmissions (C-statistic = 0.89; HL = 0.31). Operative time>7 hours and history of DVT/PE increased risk for early reoperation by 5.8- and 8.7-fold, respectively.
Conclusions:
An emphasis on medically optimizing patients with preexisting pulmonary comorbidities, depression, and history of DVT/PE may have a substantial impact on improving short-term outcomes in this population. The present study provides benchmark data and may serve as an initial model to predict unplanned reoperations and readmissions.
Keywords: adult spine deformity, spine surgery, readmission, reoperations, complications
Introduction
In the current literature, complex adult spinal deformity (ASD) surgery has been associated with an array of postoperative complications such as wound infections, proximal or distal junctional failure, pseudarthrosis, neurologic deficit, and acute blood loss anemia.1-3 With the continued evolution of bundled insurance payment plans, there has been a heightened focus on 90-day quality metrics postdischarge, especially with any complex surgery. Included in these quality metrics are unplanned readmission and reoperation rates, which may be markers for performance during the index admission and for an increased burden of cost on health care infrastructure. 4 Identifying predisposing risk factors for unplanned readmissions and reoperations remains an integral part of preoperative patient optimization. High-risk patients who have a greater potential for an unplanned 90-day readmission and/or reoperation can provide the opportunity for surgeons and other health care providers to ascertain and treat modifiable risk factors preoperatively, optimize patients for the planned surgical procedure, improve overall quality of care, and reduce costs to health care systems. The purpose of this study is to report on the 90-day readmission and reoperation rates of our institutional data and identify the associated risk factors for these outcomes.
Methods
Following institutional review board approval (Columbia University approved IRB protocol number AAAS0556), consecutive records of complex adult (≥18 years old) spine deformity surgeries between 2015 and 2018 from a single institution treated by 3 experienced spinal deformity surgeons were reviewed retrospectively. These “complex adult spine deformity” (ASD) patients had a primary diagnosis of ASD and underwent ≥6-level fusion surgery with posterior column osteotomy (PCO), pedicle subtraction osteotomy (PSO), vertebral column resection (VCR), pelvic fixation, interbody fusion, and/or prior spine surgery. Common ASD diagnoses included adult idiopathic scoliosis, degenerative lumbar scoliosis, congenital spine deformity, kyphoscoliosis, fixed sagittal imbalance, fixed coronal imbalance, flat back deformity, neuromuscular scoliosis, and Scheuermann’s kyphosis (Supplementary Table 1). Patients with a diagnosis of spinal trauma, active infection, and spinal tumor were excluded from this study. The minimum follow-up was 90 days after the index hospital discharge date.
Demographic information included sex, age, American Society of Anesthesiologists (ASA) grade, and body mass index (BMI, kg/m2). Comorbidities included cardiac (eg, myocardial infarction, hypertension, hyperlipidemia, coronary artery disease), pulmonary (eg, asthma, chronic obstruction pulmonary disease [COPD], obstructive sleep apnea, prior pneumonia), gastrointestinal (GI; eg, gastroesophageal reflux disease [GERD], peptic ulcer disease, ulcerative colitis, celiac disease), osteoporosis/osteopenia, diabetes, hypothyroidism, anemia, depression, history of deep vein thrombosis/pulmonary embolism (DVT/PE), and history of cancer (nonspine tumor).
Operative variables included total instrumented levels (TIL), pelvic fixation, posterior column osteotomies (PCO), pedicle subtraction osteotomy (PSO), vertebral column resection (VCR), anterior lumbar interbody fusion (ALIF), oblique lumbar interbody fusion (OLIF), transforaminal lumbar interbody fusion (TLIF), estimated blood loss (EBL), operative and anesthesia durations, and prior spine surgery. We chose operative time >7 hours as a cutoff based on the mean operative time of the cohort.
Postoperative inpatient complications were collected as well. These included GI (eg, ileus, nausea/vomiting), cardiac (eg, cardiac/respiratory arrest, lower extremity edema, hypovolemic shock, pericardial effusion), pulmonary (eg, respiratory distress/failure, pneumonia, pleural effusion), DVT/PE, hyponatremia, neurologic (eg, weakness), infection (eg, skin, urinary tract infection), renal (eg, acute kidney injury), and packed red blood cell transfusion.
The primary outcome of interest was any readmission/reoperation within 90 days of the index hospital date of discharge. Chi-square or Fisher’s exact test (where appropriate) and t tests were used for categorical and continuous variables, respectively. A stepwise multivariate logistic regression, which is a modification of the forward selection method, was employed to identify the set of independent risk factors that would optimize model performance. Factors that had a P value <0.2 remained in the model. Statistical significance was defined as P < .05. The C-statistic and Hosmer-Lemeshow (HL) value was used to measure concordance and goodness of fit of the final models. SAS Studio Version 3.4 (SAS Institute Inc) was used for all statistical analyses.
Results
A total of 227 consecutive patients met inclusion/exclusion criteria, including having a minimum follow-up period of 90 days. The mean ± standard deviation age was 50.5 ± 17.8 years and 67.8% of the patients were female. The top primary diagnoses included adult idiopathic scoliosis (54.2%) and fixed sagittal imbalance (34.8%) (Supplementary Table 1). More than a third (37.9%) of these patients had a prior spine surgery. The mean TIL was 13.5 ± 4.7 with a range of 6 to 25 levels. The majority of patients had a pelvic fixation (72.7%) and PCO performed (85.5%, mean number of 5.4 per patient). A significant proportion of patients had a TLIF (46.7%), VCR (7.9%), PSO (5.7%), and ALIF/OLIF (1.7%). The overall mean operative time was 472 ± 134 minutes with a mean EBL of 1312 ± 808 mL.
The 90-day readmission and reoperation rates were 7.0% and 5.3%, respectively. The median number of days after index discharge date resulting in an early readmission and reoperation were 16.5 days (range 2-76) and 28 days (range 7-76), respectively. Four patients who were readmitted did not require a reoperation. These readmissions without reoperation were due to headache from a dural tear (0.4%), DVT/PE (0.4%), and poorly controlled pain (0.9%). Reoperations were due to wound complication (2.2%; wound infection, 0.9%; wound dehiscence, 1.3%), followed by acute proximal junctional kyphosis/implant failure (0.9%), lumbar radiculopathy (0.9%), dural tear requiring repair (0.9%), and unexplained upper extremity weakness (0.4%) (Table 1).
Table 1.
Overall Rates for 90-Day Readmission/Reoperation.
| n | % | Days after discharge, median (range) | |
|---|---|---|---|
| 90-day readmissiona | 16 | 7.0 | 16.5 (2-76) |
| 90-day reoperation | 12 | 5.3 | 28 (7-76) |
| Wound complication | 5 | 2.2 | 17 (7-50) |
| Dural tear | 3 | 1.3 | 6, 28 (28) |
| Proximal junctional kyphosis/implant failure | 2 | 0.9 | 9, 56 |
| Lumbar radiculopathy | 2 | 0.9 | 15, 48 |
| Other pain requiring admission | 2 | 0.9 | 6, 9 |
| Unexplained upper extremity weakness | 1 | 0.4 | 76 |
| Pulmonary embolism/deep vein thrombosis | 1 | 0.4 | 2 |
a Includes reoperations.
When comparing readmitted versus nonreadmitted patients in the bivariate analyses, patients had statistically similar age (55.4 vs 50.1 years, P = .241), BMI > 30 kg/m2 (64.7% vs 45.7%, P = .131), and comorbidity burden/ASA > 2 (41.2% vs 26.6%, P = .234). Patients with preoperative pulmonary and GI comorbidities, depression, and history of DVT/PE were more likely to require a readmission within 90 days. Of note, 83.3% of the GI complications were in patients with a history of GERD, and 85.0% of the pulmonary comorbidities were in patients with known asthma/COPD. The most relevant operative factor for readmission was operative duration (563 ± 121 vs 464 ± 133 minutes; P = .003). About 75% of patients with a readmission had an operative time >7 hours (vs 42% of those without a readmission). Length of stay of the index admission was nearly 50% longer in the reoperation group compared with those who did not require a reoperation (11.2 ± 11.0 vs 7.5 ± 7.0 days; P = .045) (Table 2).
Table 2.
Patient Clinical Characteristics by Readmission.
| 90-day readmission | |||
|---|---|---|---|
| No | Yes | P | |
| n | 211 | 16 | |
| Female, % | 67.6 | 70.6 | .801 |
| Age, y, mean (SD) | 50.1 (17.9) | 55.4 (17.5) | .241 |
| Age, y, % | |||
| ≤40 | 28.6 | 17.7 | .692 |
| 41-50 | 9.5 | 5.9 | |
| 51-60 | 25.2 | 23.5 | |
| 61-70 | 30.5 | 41.2 | |
| ≥71 | 6.2 | 11.8 | |
| ASA grade >2, % | 26.6 | 41.2 | .234 |
| BMI >30 kg/m2, % | 45.7 | 64.7 | .131 |
| Comorbidities, % | |||
| Cardiac | 35.7 | 52.9 | .157 |
| Pulmonary | 14.7 | 41.2 | .005 |
| Gastrointestinal | 6.7 | 23.5 | .013 |
| Osteoporosis/osteopenia | 21.4 | 29.4 | .445 |
| Diabetes | 3.3 | 5.9 | .584 |
| Hypothyroidism | 11.9 | 23.5 | .167 |
| Anemia | 2.9 | 5.9 | .488 |
| Prior transient ischemic attack/stroke | 0.48 | 0 | .776 |
| Anxiety | 16.7 | 29.4 | .185 |
| Depression | 18.1 | 47.1 | .004 |
| DVT/PE | 2.9 | 17.7 | .003 |
| History of cancer | 7.1 | 17.7 | .123 |
| Operative characteristics | |||
| Total instrumented level, mean (SD) | 13.3 (3.9) | 14.9 (3.9) | .103 |
| PCO, mean (SD) | 4.7 (3.2) | 4.5 (2.8) | .795 |
| PCO, % patients | 85.2 | 88.2 | .736 |
| PSO, % patients | 5.7 | 5.9 | .977 |
| VCR, % patients | 7.1 | 17.6 | .123 |
| ALIF/OLIF, % patients | 2.4 | 0 | .686 |
| TLIF, % patients | 45.2 | 64.7 | .122 |
| Pelvic fixation, % patients | 71.9 | 82.4 | .352 |
| Estimated blood loss, mL, mean (SD) | 1286 (801) | 1642 (875) | .081 |
| Operative time, min, mean (SD) | 464 (133) | 563 (121) | .003 |
| Anesthesia time, min, mean (SD) | 560 (135) | 657 (125) | .005 |
| Prior spine surgery, % patients | 37.1 | 47.1 | .418 |
| Postoperative inpatient complications | |||
| Cardiac | 10 | 5.9 | .581 |
| DVT/PE | 2.4 | 5.9 | .387 |
| Gastrointestinal | 3.3 | 0 | .445 |
| Hyponatremia | 0.95 | 0 | .686 |
| Neurologic | 0 | 5.9 | <.001 |
| Infection | 0.48 | 0 | .776 |
| Pulmonary | 8.6 | 5.9 | .7 |
| Renal | 1.9 | 5.9 | .283 |
| Postoperative transfusion | 57.6 | 76.5 | .129 |
| Length of stay, d, mean (SD) | 7.5 (7.0) | 11.2 (11.0) | .045 |
Abbreviations: ASA, American Society of Anesthesiologists; BMI, body mass index; DVT/PE, deep vein thrombosis/pulmonary embolism; PCO, posterior column osteotomy; PSO, pedicle subtraction osteotomy; VCR, vertebral column resection; ALIF, anterior lumbar interbody fusion; OLIF, oblique lumbar interbody fusion; TLIF, transforaminal lumbar interbody fusion.
The final multivariate regression for 90-day readmissions included pulmonary comorbidity, depression, history of DVT/PE, and GI comorbidity (C-statistic = 0.82, HL = 0.79). Pulmonary comorbidity, depression, and history of DVT/PE increased risk for 90-day readmission by 5-, 3.5-, and 10.2-fold, respectively. GI comorbidity increased readmissions risk by 4-fold, but only trended toward statistical significance (P = .064). The final multivariate regression for 90-day reoperations was similar to readmissions and included history of DVT/PE, operative time >7 hours, depression, cardiac comorbidity, pulmonary comorbidity, and osteopenia/osteoporosis (C-statistic = 0.89, HL = 0.31). Operative time >7 hours and history of DVT/PE increased risk for early reoperation by 5.8- and 8.7-fold, respectively (Table 3).
Table 3.
Stepwise Multivariate Logistic Regression Analysis For 90-Day Readmissions and Reoperations.
| 90-day readmission (C-stat = 0.82; HL = 0.79) | Odds ratio | 95% CI | P | |
|---|---|---|---|---|
| Lower limit | Upper limit | |||
| Pulmonary comorbidity | 5.0 | 1.4 | 17.3 | .012 |
| Depression | 3.5 | 1.1 | 11.0 | .036 |
| History of DVT/PE | 10.2 | 1.9 | 55.3 | .007 |
| GI comorbidity | 4.0 | 0.9 | 17.4 | .064 |
| 95% CI | ||||
| 90-day reoperation (C-stat = 0.89; HL = 0.31) | Odds ratio | Lower limit | Upper limit | P |
| History of DVT/PE | 8.7 | 1.3 | 58.2 | .025 |
| Operative time >7 hours | 5.8 | 1.1 | 31.5 | .043 |
| Depression | 3.4 | 0.8 | 13.6 | .085 |
| Cardiac comorbidity | 3.1 | 0.8 | 12.6 | .114 |
| Pulmonary comorbidity | 3.1 | 0.7 | 13.8 | .133 |
| Osteopenia/osteoporosis | 3.1 | 0.7 | 12.8 | .126 |
Abbreviations: HL, Hosmer-Lemeshow value; DVT/PE, deep vein thrombosis/pulmonary embolism; GI, gastrointestinal.
Discussion
The majority of readmissions (75%) involved a reoperation to address a wound complication, dural tear, acute proximal junctional kyphosis/instrumentation failure, or extremity pain/weakness of unclear etiology. Therefore, finding opportunities to mitigate and avoid an unplanned reoperation are imperative. One potential technique related variable is avoiding 3 column osteotomies (3CO: PSO and VCR) when possible as those are known to have higher perioperative complication rates than those with ASD not having 3COs.5,6 In this current series, 13.6% of patients underwent a 3CO, which is less than the Scoli-Risk-1 study, which had nearly 75% of patients with a 3CO. 7 To the authors’ knowledge, no prior study has investigated the 90-day readmission and reoperation data after index complex spine deformity surgery.
In the multivariate analyses, pulmonary comorbidity appeared in the final regression models for both 90-day readmission and 90-day reoperation. In prior literature, lung disease has been found to be an important risk factor for postoperative complications after ASD.8,9 The association between complication and pulmonary comorbidity is likely multifactorial. The majority of pulmonary comorbidities in this study were due to asthma/COPD. Literature has shown that COPD is associated with decreased bone mineral density and increased vertebral deformities/fractures. 10 Furthermore, it is possible that concomitant use of steroids to treat lung disease may have contributed to readmission/reoperation risk as steroids are known to be associated with lower bone mineral density and poor wound healing.11-13 Interestingly, the 2 patients with pseudarthroses/implant failure also had severe lung disease.
In a retrospective multicentered database, Manoharan et al 14 used the National Surgical Quality Improvement Program database (NSQIP) to review the 30-day readmission rate following adult spinal deformity surgery. In 747 patients, they found a readmission rate of 7.5% within 30 days of index surgery date, most commonly due to infection, hematoma/seroma, and postoperative pain. Risk factors were obesity, peripheral vascular disease, pulmonary embolism prior to discharge, and total or partial dependent preoperative functional health status. 14
Schairer et al 15 used single institutional data to review hospital readmission after spine fusion for adult spinal deformity. The 836 patients had either short (<4 level fusion), medium (4-7 levels) or long (>7 level) fusions. Overall unplanned readmission rates were 8.4% for 30 days, and 12.3% at 90 days. Surgical site infection accounted for 45.6% of readmissions. Risk for readmission include longer fusion length, higher patient severity of illness, and specific medical comorbidities. Proximal junctional kyphosis accounted for more than half of surgical readmissions with an overall rate of 1.7% within 90 days of discharge. 15 As demonstrated in these prior studies, infection and proximal junctional kyphosis may be one of the most common reasons for early unplanned revision surgery.
Diebo et al 16 performed a retrospective analysis on a New York statewide database for those with adult spinal deformity who underwent at least a 4-level thoracolumbar fusion surgery with a 2-year minimum follow up. They found that patients with mental health disorders (including depression, sleep disorders, anxiety, and stress disorder) had higher rates of any readmission and revision surgery (P < .002). In their study, mental health disease was the strongest predictor for any revision (OR 1.56, P < .001) and readmission (OR 1.32 P < .001). Depression is the most common mental health disorder in the United States and is known to be associated with greater postoperative functional disability and pain after adult spinal deformity surgery. 17 It is possible that patients with depression are at higher risk for falls after surgery 18 and poorer medical compliance to postoperative therapy and rehabilitation, which may lead to an unplanned readmission.
In our study, 26.4% of patients had either anxiety (17.6%) and/or depression (20.2%). Spine surgeons should be aware of the associated risks of mental health status and outcomes after spine deformity surgery. Multiple studies in various orthopedic subspecialties show increased association with extended length of stay as well as revision surgery.19,20 It is unclear what the underlying mechanism or link between depression and reoperation/readmission. This does not imply that poor preoperative mental status should be a contraindication for surgery, but rather an opportunity to recognize that depression is multifaceted and to optimize preoperative mental health status. There is evidence to suggest that pre- and postoperative mental health counseling may benefit patient recovery more than physical therapy alone. Such as the “back-café” concept, in which patients who met with other patients to discuss their fusion surgery recovery in addition to physical therapy had better overall outcomes.16,21
There are several key differences between our results and those already published. First, one of the main objectives of our study was to focus on complex spine deformity surgeries. Few prior studies have reviewed readmissions and reoperations on this population in isolation. Nevertheless, the literature describes a range of “complex” ASD patients. With exception to the Scoli-Risk-1 study, many studies define ASD as having >2 spinal fusion levels and/or based on certain radiographic parameters.22-26 In comparison to the Schairer et al 15 study, which included patients who had less than 4 fusion levels, we report a significantly lower 90-day readmission rate (7.0% vs. 12.3%). This variability may partly be due to surgeon technique and patient selection. However, it is important to note that our patient population appeared to be considerably more complex given the range and minimum fusion level criteria as well as the concomitant procedures. It may be beneficial in future studies to create a case-mix index when analyzing “complex” ASD so that the comparisons in complication/reoperation rates between studies may be better controlled. Second, many prior studies use a 30-day follow-up period after discharge. However, many short-term complications occur beyond this window and may lead to failure in identifying up to 30% to 40% of potential total readmissions in comparison with the 90-day follow-up period. 27 Third, large database studies have the power to elucidate risk factors for relatively rare complications; however, as shown in this study, our risk factors for readmission were dissimilar to those reviewed by Manoharan et al’s study. Models derived from large databases may not always apply for every surgeon or practice due to the variability in surgeon-specific variables and/or the lack of surgery-specific variables in these databases. With regard to other key findings of this study, operative time >7 hours increased risk for reoperation by nearly 6-fold. Interestingly, all reoperations for wound complications also had prolonged operative time. Results demonstrated that pulmonary comorbidity and depression increased risk for 90-day readmissions. A history of DVT/PE was also a significant risk factor for reoperation. It is possible that patients who are on long-standing anticoagulation medication may be at higher risk postoperative wound complications as it is possible that relatively poorer hemostasis can result in worse postoperative seroma and hematoma. Furthermore, results demonstrated that pulmonary comorbidity and depression increased the risk for 90-day readmissions. When inspecting the reasons for readmissions for both of these comorbidities, it was difficult to decipher any clear pattern since both cohorts included a myriad of reasons with many patients having more than one reason for readmission, that is, the reasons for readmission for patients with depression (n = 14) included proximal junctional kyphosis (n = 4), implant failure (n = 4), wound complication (n = 3), dural tears (n = 2), pain (n = 2), PE (n = 1), and postoperative trauma (n = 1); the reasons for readmission for patients with pulmonary comorbidities (n = 11) included dural tear (n = 1), pain (n = 2), proximal junctional kyphosis (n = 1), implant failure (n = 1), weakness (n = 3), prominence of incision (n = 1), and wound complication (n = 2).
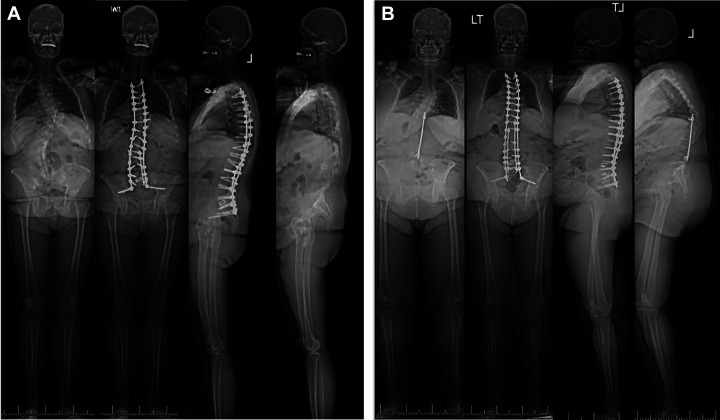
The current study’s findings can be appreciated through the following case examples: patient A (nonreadmitted) and patient B (readmitted) (Figure 1). Both patients underwent spinal fusion surgery from T3 to pelvis for adult idiopathic scoliosis. Patient A was a 38-year-old woman with obesity, diabetes, and hypothyroidism. Her surgery involved multiple PCOs (10), a TLIF L5-S1, with an operative duration of 500 minutes and an EBL of 1600 mL. Her hospital course was uncomplicated, and she was discharged after 6 days in the hospital. She did not have any issues during the 3-month postoperative period. On the other hand, patient B was a 58-year old woman with GERD, hypertension, hyperlipidemia, diabetes, and obesity. She had a prior Harrington rod procedure >20 years ago. Similar to patient A, her surgery involved multiple PCOs (7), TLIF L4-5, L5-S1, with an operative duration of 687 minutes and an EBL of 1200 mL. Her hospital course was complicated by an intraoperative dural tear, which was repaired during the index procedure. Her hospital length of stay was 8 days. At her rehabilitation facility, she was found to have a wound infection and subsequently brought to the operating room for an irrigation and debridement (I&D) on postoperative day 16. At her most recent follow-up (about 6 months status post I&D), her wound has resolved and healed well. Although patient A had a number of comorbidities, including obesity and diabetes, it is possible, based on our analyses, that those factors had less effect compared with extended operative time in influencing reoperation risk. Dural tear and revision surgery were likely accounted for in the operative duration variable in our multivariate analysis.
Figure 1.
(A) Patient A: 38-year-old woman with a past medical history of obesity, diabetes, and hypothyroidism presented with AdIS. Patient had a primary T3 to ilium with PCOs, 1 TLIF at L5-S1, 1600 mL EBL, 6-day length of stay, and was not readmitted postoperatively. (B) Patient B: 58 year-old female status post Harrington Rod T10 to L4. Patient presented with AdIS with PJK and coronal and sagittal imbalance and a past medical history of GERD, obesity, diabetes, and hypertension. Readmitted for wound dehiscence (OR cultures grew pseudomonas, Morganell morganii) 16 days status post revision T3 to ilium with PCOs, 2 TLIFs at L4-5 and L5-S1, 1200 mL EBL, and an 8-day length of stay postoperatively. AdIS, adult idiopathic scoliosis; PJK, proximal junction kyphosis; PCO, posterior column osteotomy; TLIF, transforaminal lumbar interbody fusion; EBL, estimated blood loss.
There are a number of limitations for this study. The minimum follow-up was 90 days after index discharge date; however, complications such as proximal junctional kyphosis are known to occur beyond this follow up period. As demonstrated in this study, the 90-day follow up rate was 92.3%. This loss to follow-up could suggest that some patients were readmitted to other hospitals/health care systems. The current study relied on data derived from a single institution, which may not be generalizable to all spine surgery practices. Furthermore, inclusion of more radiographic parameters such as the amount of coronal and sagittal correction may account for the variability in readmission risk from the complexity of surgery and may improve regression performance. Future studies could account for cost analyses which would improve our understanding of the financial impact of unplanned reoperations and readmissions on patients and providers.
Conclusion
The 90-day readmission and reoperation rates after complex ASD surgery in this single institutional study were relatively low, with a significant proportion that appear to be potentially modifiable and/or avoidable. Half of the readmissions were due to wound complications and dural tears. Several patient and operative risk factors were identified as well. An emphasis on medically optimizing patients with preexisting pulmonary comorbidities, depression, and history of DVT/PE may have a substantial impact in improving short term outcomes in this population. These multivariate regression analyses show excellent model performance at our institution, but they need to be tested on prospective patients to determine model accuracy and reliability. The present study provides benchmark data and may serve as an initial model to predict unplanned reoperations and readmissions for this study population.
Supplementary Materials
Supplemental_Table for The 90-Day Reoperations and Readmissions in Complex Adult Spinal Deformity Surgery by Nathan J. Lee, Lawrence G. Lenke, Meghan Cerpa, Joseph Lombardi, Alex Ha, Paul Park, Eric Leung, Zeeshan M. Sardar and Ronald A. Lehman in Global Spine Journal
Footnotes
Authors’ Note: Results of this study were presented at the 2019 International Meeting of Advanced Spine Techniques.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Nathan J. Lee, MD  https://orcid.org/0000-0001-9572-5968
https://orcid.org/0000-0001-9572-5968
Meghan Cerpa, MPH  https://orcid.org/0000-0002-5931-7067
https://orcid.org/0000-0002-5931-7067
Alex Ha, MD  https://orcid.org/0000-0001-8057-9996
https://orcid.org/0000-0001-8057-9996
Supplementary Materials: Supplemental material for this article is available online.
References
- 1.Burton DC, Sethi RK, Wright AK, et al. The role of potentially modifiable factors in a standard work protocol to decrease complications in adult spinal deformity surgery: a systematic review, part 1. Spine Deform. 2019;7:669–683. [DOI] [PubMed] [Google Scholar]
- 2.Segreto FA, Passias PG, Lafage R, et al. Incidence of acute, progressive, and delayed proximal junctional kyphosis over an 8-year period in adult spinal deformity patients. Oper Neurosurg (Hagerstown). 2020;18:75–82. [DOI] [PubMed] [Google Scholar]
- 3.Lee NJ, Kothari P, Kim JS, et al. Early complications and outcomes in adult spinal deformity surgery: an NSQIP study based on 5803 patients. Global Spine J. 2017;7:432–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yeramaneni S, Gum JL, Carreon LY, et al. Impact of readmissions in episodic care of adult spinal deformity: event-based cost analysis of 695 consecutive cases. J Bone Joint Surg Am, 2018;100:487–495. [DOI] [PubMed] [Google Scholar]
- 5.Auerbach JD, Lenke LG, Bridwell KH, et al. Major complications and comparison between 3-column osteotomy techniques in 105 consecutive spinal deformity procedures. Spine (Phila Pa 1976). 2012;37:1198–1210. [DOI] [PubMed] [Google Scholar]
- 6.Smith JS, Shaffrey CI, Klineberg E, et al. Complication rates associated with 3-column osteotomy in 82 adult spinal deformity patients: retrospective review of a prospectively collected multicenter consecutive series with 2-year follow-up. J Neurosurg Spine. 2017;27:444–457. [DOI] [PubMed] [Google Scholar]
- 7.Lenke LG, Shaffrey CI, Carreon LY, et al. Lower extremity motor function following complex adult spinal deformity surgery: two-year follow-up in the Scoli-RISK-1 prospective, multicenter, international study. J Bone Joint Surg Am. 2018;100:656–665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.De la Garza Ramos R, Passias PG, Schwab F, Bydon A, Lafage V, Sciubba DM. Incidence, risk factors, and mortality of reintubation in adult spinal deformity surgery. Clin Spine Surg. 2017;30:E896–E900. [DOI] [PubMed] [Google Scholar]
- 9.Tang H, Zhu J, Ji F, Wang S, Xie Y, Fei H. Risk factors for postoperative complication after spinal fusion and instrumentation in degenerative lumbar scoliosis patients. J Orthop Surg Res. 2014;9:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kjensli A, Falch JA, Ryg M, et al. High prevalence of vertebral deformities in COPD patients: relationship to disease severity. Eur Respir J. 2009;33:1018–1024. [DOI] [PubMed] [Google Scholar]
- 11.White SJW, Ranson WA, Cho B, et al. The effects of preoperative steroid therapy on perioperative morbidity and mortality after adult spinal deformity surgery. Spine Deform. 2019;7:779–787. [DOI] [PubMed] [Google Scholar]
- 12.De la Garza-Ramos R, Abt NB, Kerezoudis P, et al. Deep-wound and organ-space infection after surgery for degenerative spine disease: an analysis from 2006 to 2012. Neurol Res. 2016;38:117–123. [DOI] [PubMed] [Google Scholar]
- 13.de Nijs RN, Jacobs JW, Bijlsma JW, et al. Prevalence of vertebral deformities and symptomatic vertebral fractures in corticosteroid treated patients with rheumatoid arthritis. Rheumatology (Oxford). 2001;40:1375–1383. [DOI] [PubMed] [Google Scholar]
- 14.Manoharan SR, Baker DK, Pasara SM, Ponce B, Deinlein D, Theiss SM. Thirty-day readmissions following adult spinal deformity surgery: an analysis of the National Surgical Quality Improvement Program (NSQIP) database. Spine J. 2016;16:862–866. [DOI] [PubMed] [Google Scholar]
- 15.Schairer WW, Carrer A, Deviren V, et al. Hospital readmission after spine fusion for adult spinal deformity. Spine (Phila Pa 1976). 2013;38:1681–1689. [DOI] [PubMed] [Google Scholar]
- 16.Diebo BG, Lavian JD, Murray DP, et al. The impact of comorbid mental health disorders on complications following adult spinal deformity surgery with minimum 2-year surveillance. Spine (Phila Pa 1976). 2018;43:1176–1183. [DOI] [PubMed] [Google Scholar]
- 17.Theologis AA, Ailon T, Scheer JK, et al. Impact of preoperative depression on 2-year clinical outcomes following adult spinal deformity surgery: the importance of risk stratification based on type of psychological distress. J Neurosurg Spine. 2016;25:477–485. [DOI] [PubMed] [Google Scholar]
- 18.Whooley MA, Kip KE, Cauley JA, Ensrud KE, Nevitt MC, Browner MS. Depression, falls, and risk of fracture in older women. Study of Osteoporotic Fractures Research Group. Arch Intern Med. 1999;159:484–490. [DOI] [PubMed] [Google Scholar]
- 19.Jorgensen CC, Knop J, Nordentoft M, et al. Psychiatric disorders and psychopharmacologic treatment as risk factors in elective fast-track total hip and knee arthroplasty. Anesthesiology. 2015;123:1281–1291. [DOI] [PubMed] [Google Scholar]
- 20.Bozic KJ, Lau E, Ong K, et al. Risk factors for early revision after primary total hip arthroplasty in Medicare patients. Clin Orthop Relat Res. 2014;472:449–454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Christensen FB, Laurberg I, Bunger CE. Importance of the back-cafe concept to rehabilitation after lumbar spinal fusion: a randomized clinical study with a 2-year follow-up. Spine (Phila Pa 1976). 2003;28:2561–2569. [DOI] [PubMed] [Google Scholar]
- 22.Soroceanu A, Burton DC, Oren JH, et al. Medical complications after adult spinal deformity surgery: incidence, risk factors, and clinical impact. Spine (Phila Pa 1976). 2016;41:1718–1723. [DOI] [PubMed] [Google Scholar]
- 23.Faldini C, Di Martino A, Borghi R, Perna F, Toscano A, Traina F. Long vs. short fusions for adult lumbar degenerative scoliosis: does balance matters? Eur Spine J. 2015;24(suppl 7):887–892. [DOI] [PubMed] [Google Scholar]
- 24.Elsamadicy AA, Adogwa O, Vuong VD, et al. Impact of alcohol use on 30-day complication and readmission rates after elective spinal fusion (≥2 levels) for adult spine deformity: a single institutional study of 1010 patients. J Spine Surg. 2017;3:403–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Elsamadicy AA, Adogwa O, Sergesketter A, et al. Reduced impact of smoking status on 30-day complication and readmission rates after elective spinal fusion (≥3 levels) for adult spine deformity: a single institutional study of 839 patients. World Neurosurg. 2017;107:233–238. [DOI] [PubMed] [Google Scholar]
- 26.Elsamadicy AA, Adogwa O, Behrens S, et al. Impact of surgical approach on complication rates after elective spinal fusion (≥3 levels) for adult spine deformity. J Spine Surg. 2017;3:31–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Avinash M, Rajasekaran S, Aiyer SN. Unplanned 90-day readmissions in a specialty orthopaedic unit—a prospective analysis of consecutive 12729 admissions. J Orthop. 2017;14:236–240. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental_Table for The 90-Day Reoperations and Readmissions in Complex Adult Spinal Deformity Surgery by Nathan J. Lee, Lawrence G. Lenke, Meghan Cerpa, Joseph Lombardi, Alex Ha, Paul Park, Eric Leung, Zeeshan M. Sardar and Ronald A. Lehman in Global Spine Journal