Abstract
Background
Mobile health (mHealth) tools have emerged as a promising health care technology that may contribute to cost savings, better access to care, and enhanced clinical outcomes; however, it is important to ensure their acceptance and adoption to harness this potential. Patient adoption has been recognized as a key challenge that requires further exploration.
Objective
The aim of this review was to systematically investigate the literature to understand the factors affecting patients’ adoption of mHealth tools by considering sociotechnical factors (from technical, social, and health perspectives).
Methods
A structured search was completed following the participants, intervention, comparators, and outcomes framework. We searched the MEDLINE, PubMed, Cochrane Library, and SAGE databases for studies published between January 2011 and July 2021 in the English language, yielding 5873 results, of which 147 studies met the inclusion criteria. The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines and the Cochrane Handbook were followed to ensure a systematic process. Extracted data were analyzed using NVivo (QSR International), with thematic analysis and narrative synthesis of emergent themes.
Results
The technical factors affecting patients’ adoption of mHealth tools were categorized into six key themes, which in turn were divided into 20 subthemes: usefulness, ease of use, data-related, monetary factors, technical issues, and user experience. Health-related factors were categorized into six key themes: the disease or health condition, the care team’s role, health consciousness and literacy, health behavior, relation to other therapies, integration into patient journey, and the patients’ insurance status. Social and personal factors were divided into three key clusters: demographic factors, personal characteristics, and social and cultural aspects; these were divided into 19 subthemes, highlighting the importance of considering these factors when addressing potential barriers to mHealth adoption and how to overcome them.
Conclusions
This review builds on the growing body of research that investigates patients’ adoption of mHealth services and highlights the complexity of the factors affecting adoption, including personal, social, technical, organizational, and health care aspects. We recommend a more patient-centered approach by ensuring the tools’ fit into the overall patient journey and treatment plan, emphasizing inclusive design, and warranting comprehensive patient education and support. Moreover, empowering and mobilizing clinicians and care teams, addressing ethical data management issues, and focusing on health care policies may facilitate adoption.
Keywords: telemedicine, smartphone, mobile phone, electronic health record, public health practice, technology, perception, health education, mHealth, mobile health, telehealth, eHealth, patients
Introduction
Mobile health (mHealth) tools have emerged as a promising health care technology that may contribute to better access to health services, enhanced quality of care, and cost savings [1-6]. These novel technologies may also present an opportunity to enhance communication between patients and their health care providers and facilitate self-monitoring and self-management [7-9], leading to better treatment outcomes. Patients’ adoption is a key factor for mHealth success; however, it has been recognized as one of the key challenges.
Results from several trials showed that up to 70% of patients who were invited to use mHealth technologies either declined to participate or dropped using the tools prematurely [10]. Trials that reported higher retention rates were usually conducted over a short time frame and may not necessarily reflect the situation in real-world adoption [11]. A survey study on the topic stated that >50% of the surveyed clinicians cited patient resistance as one of the key barriers to adoption [12]. Furthermore, several studies have established that only a small fraction of patients kept using mHealth tools in the long term, and that up to 80% of users would only show minimal engagement, using the tools <2 times [13,14]. Another study conducted on a large real-world cohort of 189,770 people reported that only 2.58% of the people who downloaded the app sustained its active use, concluding that the impact of such apps may remain minimal if they fail to reach the patients who need them most [15].
The scope of this study is to build a better understanding of the different factors that may affect patients’ adoption of mHealth technologies. This study defines mHealth as “medical and public health practice supported by mobile devices, such as mobile phones, patient monitoring devices, Personal Digital Assistants (PDAs), and other wireless devices” as per the World Health Organization’s Global Observatory of eHealth, which considers mHealth a subcategory of eHealth. Telemedicine is, in turn, a subcategory of mHealth and defined as “the communication or consultation between health professionals about patients using voice, text, data, imaging, or video functions of a mobile device. But it can be applied to other situations; the management of chronic diseases of patients living at home being one example” [16].
Accordingly, a systematic review was conducted to provide a precise and up-to-date description of factors that affect patients’ adoption of mHealth tools from a technology, social, and health perspective. It also reflects on potential implications and suggests directions for relevant stakeholders to overcome barriers to adoption and thus facilitate the use of mHealth by a broader population. This work is part of an ongoing research project that explores the clinicians’ perspective and supplements its initial findings, which have already been published [17].
Findings from this study will help inform health care professionals, technology providers, and policy makers by presenting them with an up-to-date and comprehensive review of key factors affecting patients’ adoption of mHealth tools, as reported in the academic literature. This can guide them in making more informed decisions to promote adoption and harness the potential advantages of these tools.
Methods
Overview
The methods for this review were drawn from the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines [18] and the Cochrane Handbook [19], both of which provide guidance toward a rigorous and reliable literature review methodology. The review methods were defined in advance and the protocol was published in the PROSPERO (International Prospective Register of Systematic Reviews) and is available on the web [20]. The analysis did not require any major divergence from the initial protocol. The research question that guided this review was the following: “According to the literature, what are the social, technical and health factors impacting patients’ adoption of mHealth tools?”
Search Strategy
A search of MEDLINE, PubMed, Cochrane Library, and SAGE databases in July 2021 identified the relevant studies. The scope of this review was narrowed to studies published in English between January 2011 and July 2021. Only original, peer-reviewed, and published papers were included in this study. Other forms, such as editorials, unsystematic reviews, interviews, comments, unstructured observations, and position papers, were excluded. We decided not to include articles on the basis of manual searches of reference lists for causes summarized in the Cochrane Handbook: “positive studies are more likely to be cited” and “retrieving literature by scanning reference lists may thus produce a biased sample of studies” [19].
The search string shown in Figure 1 was developed according to the participants, intervention, comparators, and outcome framework [21]. There were no limitations to the types of conditions that qualified for inclusion, and both qualitative and quantitative studies were included. Comparators were not applicable to this study. Participants included studies that focused on patients. Interventions (mHealth) included studies involving smart device use such as mHealth apps or telehealth. Outcomes (adoption) included studies addressing the factors affecting mHealth technology adoption or use.
Figure 1.
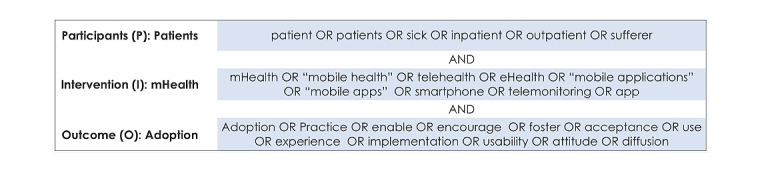
The search string according to the participants, intervention, comparator, and outcome (PICO) framework. mHealth: mobile health.
Study Selection
Two researchers (CJ and ES) were involved in the screening, eligibility, and inclusion phases, and any divergence was agreed upon in the discussion between them. In cases in which they could not reach an agreement, a third reviewer (ASV or CI) discussed it with them and made the final decision. The research team used the open-source app Rayyan QCRI (Qatar Computing Research Institute) to facilitate collaborative screening [22]. Screening lasted from June to September 2021.
The inclusion and exclusion criteria, detailed in Textbox 1, were developed according to the participants, intervention, comparators, and outcome framework. Studies were excluded if they did not involve the use of mHealth or smart devices; focused solely on, for example, clinicians, caregivers, or technology providers; did not include patients; were not peer-reviewed; were editorials, interviews, comments, unstructured observations, or position papers; did not address the factors affecting adoption; or if the full text was not available, freely available, or available in English.
Inclusion and exclusion criteria according to the PICO (participants, intervention, comparator, and outcome) framework.
Inclusion and exclusion criteria
Population
Include: focused on patients
Exclude: focused only on clinicians, caregivers, or technology providers
Intervention
Include: focused on solutions involving a smart device (eg, mobile health [mHealth] apps and telehealth)
Exclude: using other technologies (eg, virtual reality and machine learning)
Comparators
Does not apply
Outcome
Include: addresses factors impacting patients’ adoption, acceptance, use, experience, usability, or attitude of using mHealth, regardless of the condition
Exclude: focused only on mHealth success or development in general
Publication type
Include: original, peer-reviewed, and published paper
Exclude: editorials, interviews, comments, unstructured observations, and position papers
After completing the screening and resolving any conflicting views among the researchers, the selected full texts were assessed for eligibility independently by CJ and ES. Any disagreements were resolved through discussion with ASV or CI. The risk of bias was assessed using the Critical Appraisal Skills Program tool [23]. The checklist is included in Multimedia Appendix 1, and a Microsoft Excel sheet with the appraisal of the included studies can be accessed in Multimedia Appendix 2.
Data Collection and Synthesis
The variety of procedures and results that were identified in the included studies was not homogeneous enough to enable a quantitative analysis of the data. Therefore, a narrative synthesis was used and structured around the social, health, and technical factors affecting patients’ adoption of mHealth solutions. NVivo (QSR International), a computer-assisted qualitative data analysis software, was used to assist with this task.
Data coding began with a preliminary data extraction grid that included themes based on previous research and technology acceptance frameworks; the initial codebook was informed by our previous work that aggregated the factors used in the most used frameworks [24]. More codes were added as they emerged during the review process. Thematic analysis by Braun and Clarke [25] was used to identify and extract themes under social, technical, and health factors addressed in the research question. Social factors include any social-related elements, such as the effects of people and groups influencing one another through culture; technical factors include elements related to the material sides of the technology, such as its ease of use and usability; and health-related factors were linked to elements such as the health condition itself and the patient’s health literacy. The phases of the thematic analysis are explained in detail in Multimedia Appendix 3. This process lasted from September to November 2021.
Theoretical Framework
Health care technologies are generally more complex than tools that address individual user needs, as they usually support patients with comorbidities who are typically treated by multidisciplinary teams who might even work in different health care organizations. The special nature of how the health care sector operates and its high degree of regulation, normalized budget deficits, and the interdependence between health care organizations necessitate some crucial expansions to existing theoretical frameworks usually used when studying adoption.
Therefore, the authors were guided in their thinking about technology adoption by theoretical frameworks in the field of social studies of technology and sociotechnical theory; they view technology, roles, and practices and organizational structures as interacting parts of a mutually constituting ensemble of elements [26]. They used a consolidated model that the research team had previously published [24], in which they reviewed and aggregated the most used frameworks applied to technology adoption in health care. Most factors could be linked to one framework or another, but there was no single framework that could adequately cover all relevant and specific factors without some expansion. This led the authors to suggest a shift toward an extended framework that considers the complexity of the health care landscape, its highly regulated nature, and the interdependence between its different stakeholders [24]. This is aligned with what other scholars have also suggested, explaining that many of the broadly used frameworks adopt a technology-centered view focusing on the tool itself [27-30], and proposed a move to multidimensional models that go past usability to encompass the surrounding context, as well as societal and implementation challenges [27,28,30-33].
Results
Overview
As shown in the study selection flow diagram (Figure 2), the search string yielded 5873 studies, of which 5262 (89.6%) were from PubMed, 584 (9.9%) from SAGE, and 27 (0.5%) from the Cochrane database. Of these 5873 studies, 2540 (43.2%) were excluded after limiting the scope to studies published in English and published after January 2011, leaving 3333 (56.8%) studies for screening. Screening of the titles and abstracts excluded another 3032 articles because 37 of them did not involve mHealth or smart devices; 367 focused solely on nonpatient populations such as clinicians, caregivers, or technology providers; 438 were editorials, interviews, comments, unstructured observations, position, or non–peer-reviewed papers; and 2190 did not address factors affecting adoption.
Figure 2.
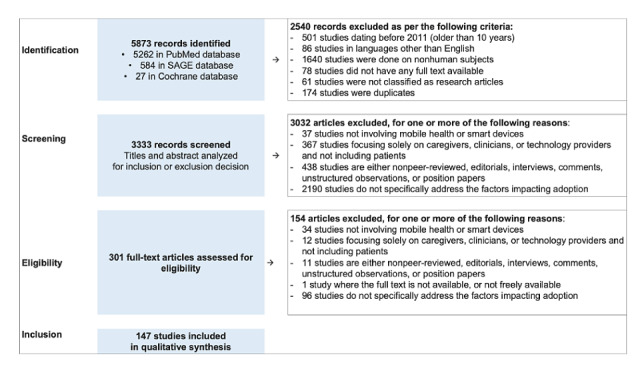
Study selection flow diagram on the basis of the PRISMA (Preferred Reporting Items for Systematic Review and Meta-Analysis) guidelines.
In the eligibility phase, 301 articles were included for full-text assessment. A total of 154 articles were excluded for the following reasons: 34 for not involving mHealth or smart devices; 12 for focusing solely on nonpatient populations such as clinicians, caregivers, or technology providers; 11 for being editorials, interviews, comments, unstructured observations, position, or non–peer-reviewed papers; 1 because the full text was not available; and 96 for not addressing the factors affecting adoption. This resulted in the inclusion of 147 articles for the qualitative synthesis [34-180].
Characteristics of Included Studies
Multimedia Appendix 4 presents the sample characteristics of the included articles. Overall, 85 studies focused on patients, 24 on both healthy and sick people, 24 on patients and health care professionals, 4 on patients and caregivers, and 10 included patients and other populations, such as clinicians, researchers, policy makers, and medical students. From a disease area perspective, some were more represented than others in the included studies; 16 studies focused on diabetes and obesity, 13 on cardiovascular disease and heart failure, 13 on mental health, 11 on surgery, 10 on oncology, 9 on chronic diseases, 8 on primary care, and 6 on neurology and neurosurgery, whereas the other disease areas were represented ≤4 times in the included studies.
Most of the publications did not mention the use of a theoretical framework. Among those that used one, the Unified Theory of Acceptance and Use of Technology was the most common (n=12), followed by the Technology Acceptance Model (n=11) and the Diffusion of Innovation Theory (n=2). Other models were used only once, as described in Multimedia Appendix 4. From a geographical perspective: 46 studies were conducted in the United States, 12 in China, 10 in the United Kingdom, 8 in Canada, 5 in Australia, 5 in Germany, 5 in Singapore, whereas other geographies were covered in ≤4 studies. From a sample size perspective, most of the included studies had a sample size >100 participants (n=80), whereas most studies that included smaller samples were qualitative in nature and did not necessitate the larger samples that are typically required in quantitative approaches.
Critical Appraisal
On the basis of the critical appraisal, 42.8% (63/147) studies did not clearly justify their choice of study design, but still used a design that is suitable for their objectives, 4.8% (7/147) did not report a clear participant recruitment strategy, 0.7% (1/147) did not provide sufficient details on the data collection techniques, 19% (28/147) did not report if the study procedure was reviewed for ethics approval, 18.4% (27/147) were not clear enough about their data analysis strategy and whether it was sufficiently rigorous, and 8.2% (12/147) did not sufficiently discuss the practical or policy implications of their findings. However, articles were not excluded based on technical quality to enable researchers to capture both theoretical and empirical contributions from the published studies.
Social and Personal Factors
The social and personal factors affecting patients’ adoption of mHealth were categorized into three key themes: demographic factors, personal characteristics, and cultural and social elements. These were, in turn, subdivided into 19 subthemes. Figure 3 provides an overview of these social and personal factor themes and subthemes and their respective occurrence.
Figure 3.
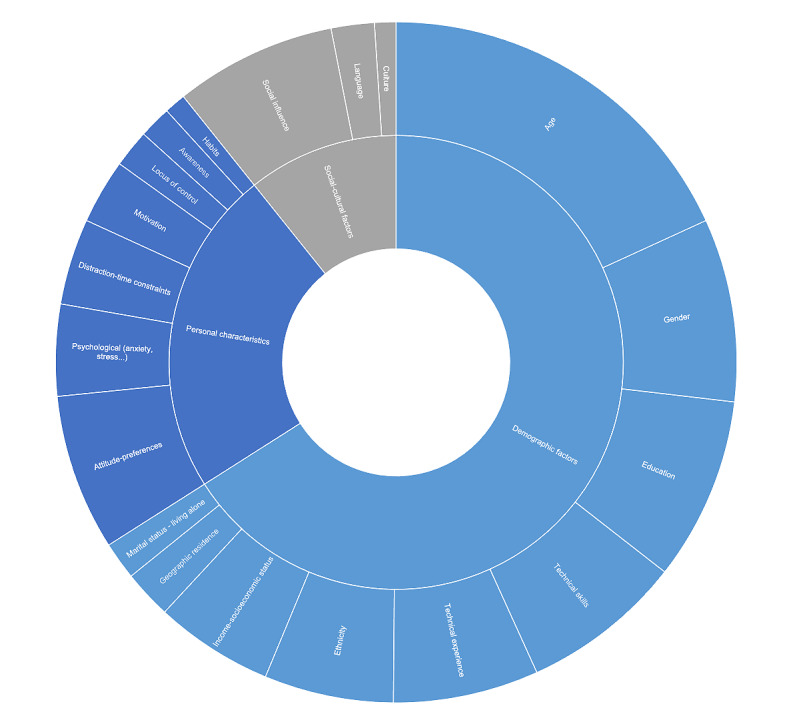
Overview of social and personal factors and their occurrence.
Demographic factors were the most prominent, often related to matters such as age (n=71), gender (n=34), education (n=34), technology skills (n=30), technology experience (n=27), ethnicity (n=24), socioeconomic factors (n=22), geographic residence (n=9), and marital status (n=7). An in-depth analysis of the demographic factors was also done to clarify which factors were mostly cited as barriers (they hinder adoption), facilitators (they facilitate adoption), mixed results (their relationship to adoption is not linear and may vary based on context), or had no impact on adoption according to the included studies, this subanalysis is visualized in Figure 4.
Figure 4.
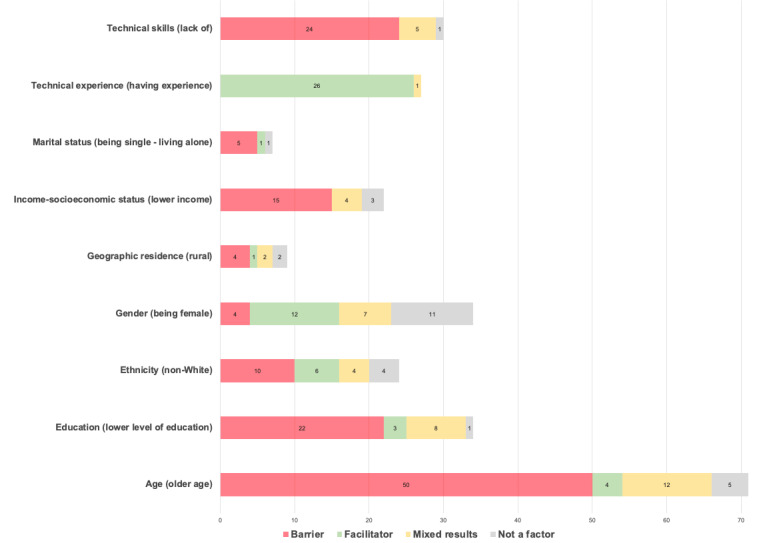
Subanalysis of the demographic factors according to their classification in the included studies.
Personal characteristics also played a central role, with factors such as patient attitudes and preferences (n=29), psychological factors (n=17), time constrain and distraction (n=16), and motivation (n=12) being in the center. Other personal characteristics were also mentioned, including the locus of control (n=7), awareness (n=6), and habits (n=5). These factors were complemented by cultural and social elements including social influence (n=30), language (n=8), and culture (n=4). Multimedia Appendix 5A details the social and personal factors affecting adoption, their occurrence, and the respective studies where they were identified.
Technical and Material Factors
The technical and material factors affecting patients’ adoption of mHealth were categorized into six key themes, which were in turn divided into 20 subthemes: usefulness, ease of use, data-related, monetary factors, technical issues, and user experience. Figure 5 provides an overview of these technical and material themes and subthemes and their respective occurrence.
Figure 5.
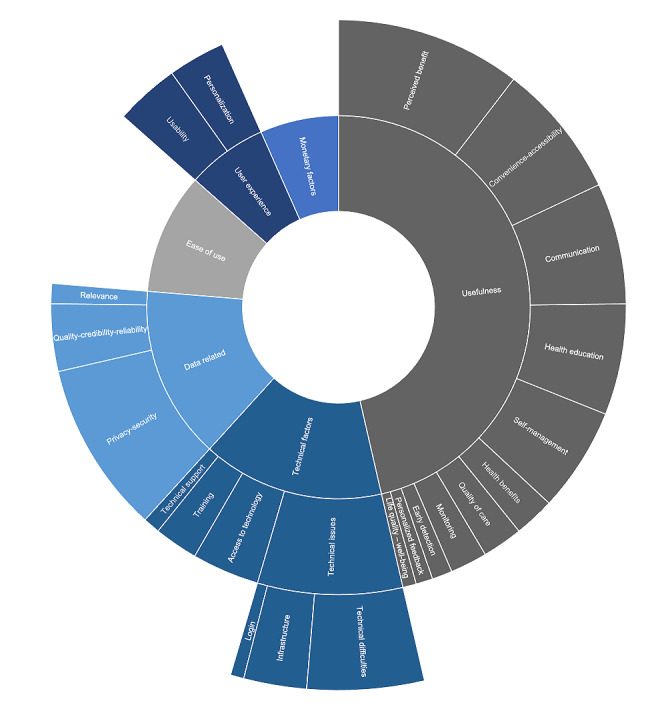
Overview of technical and material factors and their occurrence.
Usefulness was the most prominent factor in the technical and material clusters and was often related to matters such as perceived benefits and performance expectancy (n=55), convenience and accessibility (n=40), communication (n=36), health education (n=33), self-management (n=31), quality of care (n=12), health benefits (n=12), monitoring (n=11), early detection of symptoms (n=6), personalized feedback (n=5), and quality of life and well-being (n=4). Ease of use (n=54) was also very prevalent, as were data-related factors, mostly evolving around privacy and security (n=51), quality and credibility (n=20), and relevance (n=6).
There was also a frequent mention of monetary factors (n=35), such as cost and reimbursement, as well as user experience, where the focus was mostly on the usability of the tools (n=19) and personalization (n=17). Technical factors evolved around technical issues such as infrastructure and log-in problems (n=43), access to technology (n=20), training (n=13), and technical support (n=5). Multimedia Appendix 5B details the technical and material factors affecting adoption, their occurrence, and the respective studies where they were identified.
Health-Related Factors
Health-related factors affecting patients’ adoption of mHealth were categorized into six key themes: the disease or health condition, the care team’s role, health consciousness and literacy, health behavior, relation to other therapies and integration into patient journey, and the patients’ insurance status. Figure 6 provides an overview of these health-related themes and subthemes and their respective occurrences.
Figure 6.
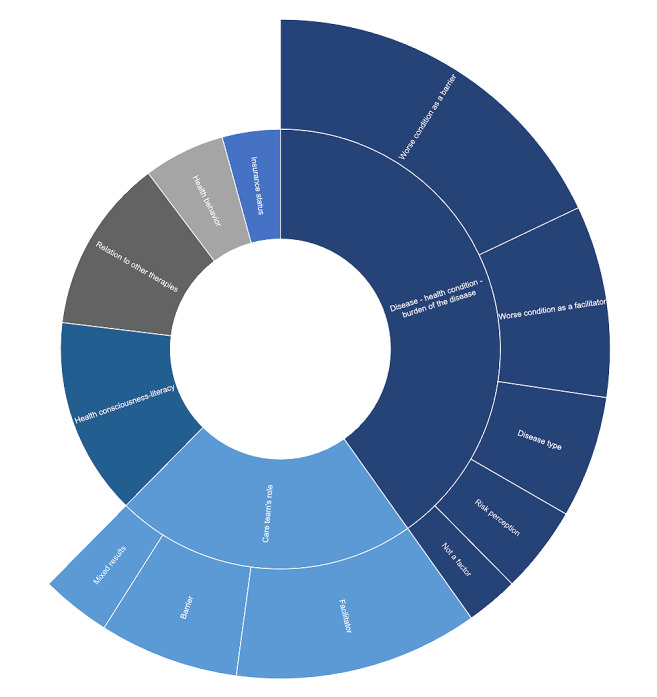
Overview of health-related factors and their occurrence.
The disease or health condition that the patient had was not only the most prominent factor, often related to matters such as perceiving the worse condition as a barrier to adoption (n=21), but also a facilitator in other contexts (n=11). The disease type itself may also be a factor (n=7) and the patient’s risk perception of their health condition (n=5), whereas other studies found that the health condition was not a factor (n=3). Similarly, the care team’s role was mostly reported as a facilitator (n=14), but also sometimes as a barrier (n=8), although some papers reported mixed results (n=4).
Other health-related aspects such as health consciousness and literacy (n=17), relation to other therapies, and the integration of mHealth into the patient journey (n=15), as well as the patient’s baseline health behavior (n=7) and insurance status (n=5) were cited as potential factors that may affect health technology adoption. Multimedia Appendix 5C details the health factors affecting adoption, their occurrence, and the respective studies where they were identified.
Principal Findings
The main findings of this review emphasize the central factors affecting patients’ adoption of mHealth tools. Analyzing the prevalence of the different factors sheds light on the significance of social and health-related factors that go beyond technical features, stressing their importance when developing and deploying these tools.
Social and Personal Factors
The prominence of social and personal factors in the included studies highlights how mHealth adoption is closely connected to and shaped by the societal dynamics in which they are embedded. Demographic factors, personal characteristics, and other social and cultural elements may play a key role in patients’ willingness to adopt an mHealth tool.
Demographic Factors
Age was the most prominent demographic factor, with older age mostly cited as a barrier, and many studies have reported a negative relationship between age and willingness to use such tools [34-55]. Some studies further explained that this may not be because of age per se but indirectly because of other factors such as older individuals facing physical or cognitive challenges [56,57], unfamiliarity with the use of technology or smartphones in general [58-63], or lack of phone ownership [64-66]. In the case of solutions dedicated to child patients, parents’ age was negatively associated with their willingness to use digital tools, whereas children’s age was positively associated with their willingness to adopt these tools [67].
Nevertheless, older age was cited as a facilitator in some studies, with older patients being among the highest adopters and the most adherent users [68-70], especially in cases where there is a clear need such as during the COVID-19 pandemic when a remote health service may help older patients minimize infection risk [71]. Other researchers have reported that age is not a factor, and that older patients are as interested as their younger counterparts, especially after adjusting for other factors, such as technology skills and experience [72-76]. This may explain why some studies concluded that increasing age should not necessarily be considered a limitation because it mostly depends on the context and other related factors [77-80], suggesting that ensuring ease of use and delivering better training could help close this gap [81-83], and that a better understanding of how the tools may help them improve their condition could motivate the adoption decision [84,85].
Gender was also a prominent demographic factor, with being female mostly cited as a facilitator, and many studies reporting on the positive relationship between being female and the willingness to use such tools [39,51,55,71,85-88], with some researchers describing that this may be because of gender-specific behavioral patterns, as women frequently undertook the role of health care liaison for their families [82], that mothers may experience more anxiety than fathers and are therefore more likely to seek alternative solutions [67]; therefore, these gender-related use patterns may very well be because of the care role that society assigns to women rather than gender per se [54,83]. Furthermore, this may be because of trial bias and self-selection bias presented by female participants, as seen in the patient characteristics of many mHealth studies. However, it is worth noting that an equally prevalent number of studies reported that gender was not significantly associated with the adoption decision [36,40,45,50,53,62,68,73,89-91].
Conversely, some studies have concluded that adoption is more widespread among male users [43,92,93], sometimes because of other related factors, such as more prevalent phone ownership among male members of a specific society [65]. Moreover, other researchers have established that gender is not necessarily a decisive factor, and that adoption may vary according to the context and other factors [49,94,95]. For instance, Abelson et al [77] explained that while women in their study were more likely than their male counterparts to be anxious about losing face-to-face communication with their care providers, they were also more likely to welcome the benefit of avoiding unwarranted clinic visits. Other studies noted that women may tend to be more adopters of specific types of digital tools compared with others. For example, Beard et al [35] noted that women are more likely to adopt mental health apps, but less likely to adopt other types of apps that use entertainment, for example, compared with men. Gender-specific behavior may also differ according to the health condition in question, as reported by Foster et al [69], where adopters were most likely females in the depression trial and most likely males in the cardiovascular disease risk trial.
Education was another prominent demographic factor, with lower levels of education mostly cited as a barrier, and many studies have reported a positive relationship between the level of education and the willingness to use mHealth tools [35,49,53,55,64,65,72,84,92,96-98]. This was explained in some studies by lower access to, and skills in using technology [89,90], and lower eHealth literacy among the less educated in some contexts [44]. Only one study reported that education was not significantly correlated with adoption [68].
Unexpectedly, some studies concluded that lower education may, in some cases, facilitate adoption [45]. For example, people with less education may have higher health information needs that, in turn, foster their digital information–seeking behaviors and consequently promote adoption [88], or they may be more likely to seek alternative or supplementary solutions when care problems occur [99]. Other researchers established that education is not necessarily a conclusive factor, and that adoption may vary according to the context and other factors [95], such as lower rates of computer and internet access among the less educated [82], lower technical skills [78], and differences depending on the type of solution at hand [39,51]. Furthermore, Torrent-Sellens [83] found that the relationship between education and adoption was not linear but rather U-shaped, with usage being greater among participants with a secondary education and lower among those with primary and tertiary education.
Technology-related skills were predictably among the most prominent factors, with the lack of technology skills being cited as a barrier, and numerous studies have reported a positive relationship between technology skills and the willingness to use mHealth tools [52,62,74,80,100-103], especially among older patients who may lack these skills [61,69,77,79,103-105]. Some studies concluded that a lack of technical skills may be the underlying cause of lower adoption in older age groups, not their age as such [72]. However, one study stated that self-efficacy and a person’s perception of their own skills did not have an impact on adoption [36]. Although the lack of technical skills was typically perceived as a hindrance to adoption in the included articles, some studies reported that it is not necessarily the case; for example, if the person believes that everything can be learned, it is no longer considered a hindrance, meaning that the adoption decision also depends on the person’s attitude and openness to learn new skills [106] and on other contextual factors such as the availability of training and some additional help or support [58,64,66,107].
Similarly, technological experience was prominent, with all studies except one reporting a positive relationship between previous technology experience and adoption decisions, stating that factors such as previous smartphone use or ownership [84,92,96,107], ownership of wearable devices [49], use of health apps [38,46,54,56,83,97,109-113] or apps in general [40,48,78,85], and broad experience with digital technologies [102,114-118] may increase the odds of mHealth acceptance and adoption. However, Zhang et al [127] pointed out that even users with previous technology experience may still choose not to adopt a tool that they perceive as irrelevant or less useful compared with their traditional methods in receiving health care.
Ethnicity came up in several studies, with being non-White mostly reported as a barrier to adoption, and a negative relationship between mHealth acceptance and being of non-White ethnicity [35,71,84,119,120], sometimes relating the impact of ethnicity to other indirect factors, such as socioeconomic factors [62], lower health literacy [121], less access to technology [64,66], and insurance status [122]. However, some studies have reported mixed results [95], with ethnicity being a significant factor in some contexts and not a factor in others, as described by Foster et al [69], who highlighted that the relevance of ethnicity varied in the different trials they conducted depending on the health condition in question. Other researchers who also reported mixed results pointed out that ethnicity itself may not be the real factor, but rather other underlying triggers such as systemic racism and the existing disparities in health services that may have increased the need for such alternative solutions among non-White patients [123]. In other contexts, being non-White was reported as a facilitator of adoption [43,51,124,125], which was sometimes linked to other contextual factors such as non-White patients being less concerned about privacy issues compared with their White counterparts [77], or more use of mobile apps in general and the perception that mobile phones are essential, predominantly because of the lack of home landlines [44]. However, some studies concluded that ethnicity had no impact on patients’ decisions to adopt mHealth [50,53,86,90].
Although some researchers have established that socioeconomic factors such as income have no impact on mHealth acceptance [48,50,52], lower or insufficient income has often been reported as a barrier to adoption [37,43,44,57,63,77,83,84,90,91,126], frequently citing other interrelated factors such as insurance status, skills and education, or access to technology [51,82,89,127]. There are also studies that have reported mixed results where income may be a factor in some contexts but not in others [41,95], sometimes depending on other elements such as the level of education [62] or the specific health condition [39].
Geographic residence seems to also sometimes affect adoption, and several papers reported that living in a rural area is mostly considered a barrier to adoption [71,83], sometimes owing to lower technology access because of a less developed infrastructure in some rural areas [89]. Jaffe et al [50] reported that the prevalence of mHealth use in some regions more than others may also be related to other interrelated factors such as a lower number of COVID-19 infections in the regions that had lower adoption rates, most likely because there was less need for mHealth use in those regions with fewer cases. Rush et al [113] is the only study that concluded that living in a rural location may be a facilitator because of the long distances that a patient has to travel to access health care services and the life-saving effect that a remote service may have in such cases. Nevertheless, some studies have reported mixed results [76,95], whereas others have found that geographic residence was not a factor affecting adoption decisions [90,91].
Interestingly, marital status was also reported as a potential demographic factor affecting the adoption of these tools; seemingly, being single or living alone was usually a barrier [43,83,119], most likely because of the absence of accountability and support that a significant other may offer [82,95]. One study concluded that marital status has no impact on adoption [53], and another study reported that living alone or being single, divorced, or widowed may increase the odds of using mobile health [50].
Personal Characteristics
Patients’ attitudes and preferences are among the most prevalent personal characteristics that may affect mHealth acceptance. For instance, preference for face-to-face interactions with their care team [37,77,115,119,127,128], resistance or openness to change [36,45,129,130], negative or positive perceptions of mHealth [41,43,56,60,62,83,87,102,114,131-134], lack of interest [55,58,69,101,103], and fear of technology [135] are all elements that play a role in whether a patient is more or less receptive to these technologies.
There are also important psychological aspects to consider, such as individual-level processes and meanings that influence mental states. For instance, although mHealth may increase the feeling of safety for some patients as they know they are being monitored or have access to additional safety measures [67,80], it may trigger a sense of anxiety and stress in others for many reasons, such as being constantly reminded of their symptoms and so their disease [80,101,107,118,136-139], with these feelings sometimes subsiding when patients become more comfortable managing their own condition [112]. Furthermore, sometimes patients may give up the use of mHealth because they are overwhelmed or struggling to cope with their condition [140], they do not want the additional stress of managing their condition and prefer relying on their care team [73,79], or they may lack the emotional capacity to even try to use the tools [69]. Interestingly, users may also abandon digital tools and choose face-to-face examinations because of their emotional need to have physical contact and get out of the house [115]. Conversely, mHealth may help overcome some psychological challenges by enabling patients to receive health care services in a more private way, particularly in stigmatized areas such as mental health services [85].
Distraction and time constraints may also interfere with mHealth adoption, some patients drop the apps because they tend to forget to use them [100,110,133], get too busy with other competing priorities that take up all their time [69,80,91,100,112,115,116,137,138,140,141], find the tools too time consuming [55], or get annoyed by the interference of the app with their daily life through frequent reminders at unsuitable times that cannot be customized to their schedules [118,120]. This factor may also relate to a patient’s existing habits [57] and how a successful adoption is tied to the person’s willingness to embed the mHealth tools in their day-to-day routines to become a natural part of their existing agendas [70,140]. Haldane et al [110] pointed out that it might be easier for newly diagnosed patients to adopt these tools compared with established patients who have been managing their conditions using traditional methods for a long time. Conversely, other scholars have concluded that habit may not necessarily be a hindrance to adoption in the case of user-friendly tools that only require minimal effort and no major change in the user’s daily habits and routines [142].
Motivation is another personal characteristic that emerged as a noteworthy determining factor of behavioral intention to use new health technologies [140,142,143]; hence, motivating patients to use mHealth may be a challenge, especially if they perceive the tools as a burden or as not useful to them [130,144]. The lack of motivation in general [100,107,145] or lack of engaging mechanisms within the apps themselves may also be a challenge to adoption [146], whereas apps that include motivational elements such as rewards or interactivity may encourage adoption [101,114,147]. Similarly, self-efficacy and locus of control may also affect patients’ decisions to adopt mHealth; people who feel that they are more in control of their life and their condition are more intrinsically motivated to adopt self-management tools [80,140,148], and they are more likely to adhere to the tools when they feel responsible for their health and see it as an important purpose [110,143]. Furthermore, the lack of awareness and knowledge of mHealth apps may negatively affect patients’ intentions to use them [58,60,102,127], especially with the vast number of apps available, which makes it difficult for patients to choose the one that suits them most [78,135].
Social Influence and Cultural Factors
Several scholars argued that patients are often subject to the social influence surrounding them when making their health technology decisions [78,129,131,140,149,150], such as the presence or absence of caregivers who can encourage and support them in using the apps [70,107,108,115,128,132, 151,152], particularly in the case of people with less technology experience or those surrounded by a social circle that lacks technology experience [95,110,142]. Interestingly, the presence of strong social support and people who constantly care for the patient may sometimes discourage adoption as the person gets enough help from their caregiver and deems mHealth unnecessary [102]. It is also worth noting that social influence was not limited to the patient’s personal social network but also to the care team’s endorsement [81,153], input and support from other fellow patients who had undergone similar experiences through online communities and forums [104,113,118,154-157], or membership of a patient association [57]. Khalemsky et al [67] pointed out that this factor may also depend on the level of a person’s emotional autonomy, especially in the case of sick children and their relationship with their parents. In other contexts, researchers found no impact of social influence on adoption decisions [36].
Language barriers such as lack of language options in the tools may hinder adoption and compromise user experience [61,106,110,158], especially in the case of patients with low literacy [159,160]. This also applies to tools that use a complicated medical or technical language that is not easy for the patient to understand [78,158]. Conversely, Spooner et al [44] argued that the brevity and accessibility of some forms of mHealth tools, such as those using text messaging, may help overcome language barriers as they require less fluency compared with in-person or phone communication. Culture may also be an influencing factor, accounting for cultural nuances and tailoring the content to specific cultural beliefs and attitudes may foster adoption [95,118,121]. Gender issues in some cultural contexts may be a challenge; Duclos et al [115], for example, explains how male dominance may compromise mHealth implementation in some countries, as husbands prevent their wives from owning or using a phone.
Technical and Material Factors
It is no surprise that technical factors related to mHealth tool features and capabilities also played a central role in adoption. Factors such as usefulness and ease of use are crucial for patient acceptance, as well as user experience and personalization, data-related factors, monetary factors such as cost and funding, and technical factors including access to technology and technical challenges.
Usefulness
Perceived benefit and performance expectancy were among the key factors affecting patient acceptance of health care technologies, indicating that user adoption has much to do with the tool’s performance [40,76,78,81,92,94,101,110,114,129, 134,140,142,146,147,150,156,161,162], especially if they find it more useful compared with their current methods [87,106,117,141,157]. This perceived usefulness is not always related to the disease itself, but may also extend to other benefits such as better relaxation, an enhanced quality of sleep, or a sense of achievement [100,107,163]. In this context, it is important to note that a good understanding of the tool’s purpose and how it aims to help the patients may lead to higher adoption [60,132,137,164]. Furthermore, evidence of effectiveness may also encourage patients to start using the apps [43]. Similarly, lack of functionality or information [154] and lack of necessity or suitability [79,102,127,165,166] may lead to the tool’s abandonment. Surprisingly, Koivumäki et al [167] reported that their study found no impact of a tool’s performance on its adoption, contrary to most other studies.
Convenience and better access to care are typically facilitators to adoption [38,70,75,107,111,120,130,135,167,168], as mHealth tools may help save time and the cost of frequent clinic visits [77,105,128,137,151,169], are more flexible and may fit better in the patients’ schedule [61,92,115,170], and immediate access to care may also be convenient, especially when it is not easy to reach a physician on weekends or in the evening, for example [79,127,141,144]. Some studies specified that longer travel times [34,65,96,103,116] and difficulties accessing traditional care services are similarly positively related to health app adoption [54,74,99,113,152]. Conversely, Kemp et al [119] reported that travel distance does not have a significant impact on adoption decisions.
Communication between patients and their care team and whether it is positively or negatively affected by the use of mHealth apps also affects patient acceptance [70,75,152,160,171]. Several studies have reported that mHealth may positively affect communications [128,130,131,136,141, 154,171], for instance, by enabling a quicker and easier exchange with their care team [60,61,79,80,98,104,113, 116,118], and hence foster adoption. In contrast, other scholars concluded that in some contexts, users may perceive a negative impact on their communication with their care team [69,92,111,115,173], as it is less personal [52,107,146,165, 168,169], leading to lower acceptance and adoption. It is worth noting that some studies have pointed out the importance of combining web-based and offline communication to encourage adoption, suggesting that mHealth should complement traditional care and not replace it [79,137].
Health education was perceived as a facilitator of mHealth adoption in all included studies [88,105,107,113,116,118, 147,152], and the educational and informative content in the apps may address knowledge gaps, raise disease awareness, and encourage healthier behaviors. Such benefits may encourage patients to accept these tools as they help them better understand their medication and possible drug interactions [40,42,79,104,130], their symptoms [101,136], and their specific condition [38,53,80,102,141,149,154,155,170,174,175], and hence achieve better health results [140,145,157].
Self-management is another factor that is predominantly perceived as a facilitator [104], helping patients be more proactive in coping with their condition [43,164], more conscious of their health condition and behaviors [60,117,141,145,157], more engaged in self-care [61,70,75,79,80,101,109,113,118,139,140,152,163], and feeling more secure and confident in managing their disease [120,131,136,149,161]. This particularly applies in the case of newly diagnosed patients, as it may help them build and adopt new habits to better manage their condition [144]. Woo and Dowding [102] found that patients who have been successfully managing their condition using traditional methods for a long time may be reluctant to adopt mHealth tools as they may fail to see their value. Conversely, Fairbrother et al [175] reported that patients may not engage in self-management as they perceive this to be the responsibility of their care team, so they may choose to adopt mHealth to enable their care teams to better monitor them but not to engage in proactive management of their own condition.
Several studies have reported that mHealth adoption may improve health outcomes [42,55,114,149]. Patients who perceive potential health benefits such as better health effects and enhanced health behaviors resulting from the use of these apps are more likely to adopt them [49,58,98,107,117,138,140,141]. Similarly, tools that target a better overall quality of life that go beyond solely focusing on the disease or health condition are usually highly appreciated and may have better chances of being accepted by patients [70,103,135,176].
Continuous monitoring may encourage adoption as it increases patients’ feeling of safety because their care team constantly monitors them [77,79,80,120,170,174], allowing for treatment optimization and better control of the condition [107,145], and a clearer overview of patients’ development for better follow-up [104,155]. Early detection of symptoms and health care issues is another benefit closely related to monitoring and may foster adoption, as the tools allow the care team to stay in the loop between clinic visits and intervene in case of symptom deterioration [40,80,87,101,107,144].
Seeking a better quality of care as an outcome of mHealth adoption may motivate user acceptance, several studies reported on quality improvement and better continuity of care [42,118,168-170,172], streamlining the processes of follow-up and care management [61,113,163], enhanced documentation and evidence-based health decisions [174], and a more holistic and individualized care approach [79,135], as potential facilitators. Personalized feedback is a closely related factor that may also enhance the overall quality of care and facilitate adoption as it enables a more patient-centric approach tailored to each patient’s individual needs [95,101,147,170].
Ease of Use
Ease of use is one of the leading factors affecting mHealth adoption [70,104,107,117,150,160,161,163,177], patients would typically abandon tools that are complex or require a lot of effort [55,56,59,60,97,120,135,142,162,165,175], especially when they are already burdened by their condition [77,129]. In contrast, easy-to-use technologies that do not overburden patients have higher odds of being accepted and adopted [36,38,49,57,58,76,78,94,101,102,112,114,130,131,134,136,139,149,157,170]. Some studies have suggested that users’ perception of ease of use may be enhanced with good training material that shows the user how to optimize their use of these technologies [72,110,132,147], and by applying a more participatory approach to design that ensures the inclusion of patients in the development of tools [81,95].
User Experience
Usability was often mentioned in the included study, especially with the multitude of tools available to patients to choose from; they would most likely adopt tools that give them the best user experience [40,60,107,129,137,139,173]. Elements such as app appearance and attractiveness, including font size, navigation, layout, colors, text length, automated features, and interactive design, may play a role in the adoption decision [78,130,135,146,152,154,157,162,178]. Some studies have pointed out that design factors such as font size, color brightness, and screen size may play a particularly important role with more senior users and therefore must be tailored to their cognitive and physical capabilities [101,110,136].
Personalization has been specifically mentioned in several studies; for instance, the inability to personalize the app according to their specific needs (eg, diagnosis, symptoms, medication, stage of treatment) may lead to lower adoption or even abandonment of the tool [98,146,162,164]. Patients often prefer to be able to adjust the tools to their specific needs [101,104,107,118,130,138,154,157,160]; for instance, the timing of prompts and frequency of reminders [164], adjusting the app to their preferred goals and activities [147,165], and adjusting visual features such as colors and text size [78,118]. It is worth noting that Zhang et al [133] pointed out that patients’ desire to have more personalized solutions may be related to a decrease in their privacy concerns.
Data-Related Factors
Privacy and security are without a doubt very important factors; they were mostly perceived as a concern and a barrier to adoption, with many studies reporting on the importance patients put on the protection of their personal health information [38,40,43,52,55,61,85,87,97,101,108,128,130,137,139,168,169,175], typically requesting to know who will have access to their data and how the data will be protected against cybercrime [77,104,107,116-118,129,141,146,147,152,160,165], and sometimes voicing concerns or demanding control on whom to access their information, including other family members [58,155,157].
Conversely, some studies found that privacy may also facilitate adoption when patients perceive the apps to be secure and to offer a private way of sharing their health data [57,167], especially with users who already practice high privacy measures such as locking their phones with strong passwords [96]. Interestingly, van Heerden et al [174] pointed out that clinicians and patients are already using their smartphones to communicate and exchange information, which makes mHealth tools a more private and secure option compared with generic communication apps.
Other studies reported mixed outcomes regarding data privacy and security, expressing that not all participants perceived this factor as a barrier or as a facilitator but recognized both the advantages and the threats that it brings and highlighted the importance of securing the data [78,92,154,172]. For instance, Amann et al [144] explained that although some participants expressed concerns about data privacy, they also acknowledged that it is necessary to obtain the support they need through the app. Bauer et al [164] reported that although patients felt reassured knowing that their care team could access data about their symptoms through the app, they were simultaneously concerned about who else could have access to these data. Lupiáñez-Villanueva et al [93] concluded that patients do not have the same sensitivity to data privacy, and that their level of sensitivity may differ from one context to another. Interestingly, their study found that even users who are quite concerned about privacy are not necessarily willing to pay for it but rather would prefer their data to be protected by legal requirements [93]. Nonetheless, a few studies reported that they found no, or very minimal, impact of data privacy concerns on the adoption decision [69,94,120].
Quality, credibility, and reliability of the data available through mHealth tools may also play a role in the adoption decision [107,109,127,130,179]. The credibility of the information on the tool from the patients’ perspective often increases when it is provided or endorsed by trusted sources [40,58,78,93,110,116,154,175], reassurance that the information on the app is up-to-date to ensure its accuracy [144], and scientific evidence that warrants the app’s safety and reliability [57,59,101,113,118]. Relevance and appropriateness of the information offered by the app may also affect patient acceptance; content that is appropriate for users may foster adoption [118,146], whereas information that is not relevant, inappropriate, or not tailored to patients’ needs may discourage adoption [117,137,162]. For instance, Connor et al [154] explained that even an inappropriate tone, such as pushing too many tips through an app, could lead users to abandon it, especially if they are very sick.
Monetary Factors
Monetary factors such as app costs and lack of reimbursement were mostly perceived as barriers to adoption [61,91,131,169]. Several researchers have reported that patients may not be ready to pay for health apps or choose to pay only for the features that they find crucial for their perceived health benefits [78,104,106]. Hidden costs generated through extra data use were also mentioned as a potential barrier to adoption [55,58,97,118,152], which is particularly relevant in specific socioeconomic contexts where prepaid mobile services are the norm, and an overuse of the data package may result in service discontinuity [166]. Additional costs resulting from the patient’s need to buy new technology to facilitate mHealth use may also deter adoption [52]. Conversely, mHealth affordability was reported as one of the facilitating factors in other studies [111,116,167], and it could even help save costs, mostly by saving travel time and expenses [43,80,105,113,151,172]. Interestingly, other researchers have reported no impact of mHealth costs on patients’ intentions to use mHealth [81,129,142]. Other scholars reported mixed or inconclusive results, stating that some users may be more cost-sensitive than others [42,65,92,93,126,168], for instance, younger users may be less willing to pay for health apps [65,168].
Technical Factors
Technical issues were frequently cited as a barrier, with issues such as technology failure, insufficient phone storage, battery drain, syncing, and technical difficulties creating frustration and discouraging adoption [37,68,70,77,80,100,114,118-120, 130-132,135,137,138,141,151,178]. Poor technology infrastructure, including connectivity, network availability, and Wi-Fi issues [65,77,78,102,112,116,118,120,132,148,152, 155,158,166] as well as log-in difficulties [78,152,170] were also prevalent in the included studies. Access to technology is another important technical factor that should not be overlooked. Several studies have reported that the lack of patient access to technologies such as smartphones, computers, or specific apps [34,43,66,85,92,100,103,107,108,115,128,132,166], or lack of internet access [37,52,69,95,127], especially among older patients [135,157] could be barriers to mHealth adoption.
Training emerged in several studies as a particularly important factor for adoption given the disparity of technical skills among patients, especially in the older age groups and users with low levels of education [70,79,80,100,108,116,117,131,157,162]. The lack of such training may be a major concern and a real barrier to adoption [61,171,174]. Furthermore, technical support has often been cited as a facilitator to patient adoption if it is available and efficient in helping users overcome their technical issues [70,102,131], but it could also be a barrier if it is not adequate, leading users to abandon the tools when they do not feel supported when they face technical difficulties [55,117].
Health-Related Factors
Health- and health care–related factors were equally central in the included studies. Elements such as the specific disease a patient has, the severity of their health condition, their health behavior, health consciousness and literacy, the relation of the mHealth tool to other therapies, and the role that the care team plays may affect a patient’s willingness to use mHealth tools. The patients’ disease and health condition may affect their decision to adopt mHealth. The severity of symptoms and complexity of the health condition were prevalent factors in the included studies; however, there were mixed results on whether they were a barrier or a facilitator. It is worth noting that the studies that established that more severe disease could be a barrier to adoption were about twice the number of studies that found it to be a facilitator.
Several researchers have reported that their studies found that patients with low baseline health, worse baseline clinical disease activity, higher prevalence of chronic conditions, high level of comorbidity, higher levels of pain and fatigue, higher frequency of hospital readmission, and those who were hospitalized or in the end-of-life phase were less likely to use the apps [52,64-66,68,73,76,80,107,112,114,115,119,148,159,161]. This could sometimes be explained by the closer follow-up usually needed by patients with a worse condition, resulting in a reduced need for mHealth [57]. In some specific cases, such as mental health disease, patients having a depressive episode, or those with more depressive symptoms, for example, may experience a sense of hopelessness that makes them disengaged in many aspects of life, including health care apps [104,121]; similarly, patients with severe psychotic symptoms may have an exaggerated sense of fear of the potential surveillance resulting from remote monitoring apps [117].
Conversely, other studies found that patients who are more affected by their disease or health state may be more motivated to use mHealth to manage their condition better [39,41,49,83,89,98,132]. For instance, Ross et al [138] reported that patients with higher pain ratings had a higher adoption rate, most likely because their perceived benefit from the app is higher compared with those who have pain levels under control. Similarly, Runz-Jørgensen et al [79] explained that patients with a higher burden of illness placed a higher value on the benefits that they could obtain from mHealth. Interestingly, 3 studies concluded that disease and health condition did not have a significant impact on patients’ decision to use mHealth [35,48,100].
Some studies have also reported that the disease type may be a factor that affects patients’ intentions to adopt health apps [83,90,91,120]. For instance, health care technologies seem to be more accepted among mental health patients compared with other conditions [50,74]. Bauer et al [86] reported that mHealth use appears to be more common among primary care patients compared with those with chronic conditions; however, they rationalized that this pattern may be explained by other factors such as older age in chronic disease patients and not their health condition as such. Torrent-Sellens et al [83] affirmed that the presence of specific types of diseases such as diabetes, stroke or cerebral hemorrhage, cancer, and cataract may increase the odds of mHealth adoption. Patients’ perception of the risk or health threat caused by their disease could also play a role in their adoption decision. A higher perception of risk or health threat may positively affect the adoption of health care technologies [36,110,123,129]. In addition, a higher stigma perception of the disease, such as in the case of HIV, may foster mHealth adoption [92].
The role of the care team is also central for adoption. It has mostly been reported as a facilitator, especially when the health app has been recommended by the health care provider [59,60,70,78,81,93,97,180], when patients notice how their care team responds to the data they feed into the apps and integrate it into their care [136,164], and when the care team offers coaching and support toward patients’ self-management [132,134,143]. However, Gupta et al [85] warned that clinicians should be careful not to overdo the reminders to use the tools, especially with patients with high disease burden, such as patients with cancer, to avoid overwhelming them. Several studies concluded that the care team could be a barrier to adoption if they lacked the necessary skills [107,168], if they did not proactively support mHealth use [44,62,101,118,154], or if they did not monitor the information that patients submit to the apps [80].
Interestingly, some studies reported mixed results; for example, clinician engagement and support of mHealth use may depend on their medical specialty, with specialists more engaged than general practitioners in health care app use, perhaps because of their higher involvement in shared decision-making and clinician-patient communication [135,153]. It may also be confusing to patients when the care team encourages them to use the technology, but then fails to actively monitor the data they feed into the apps, which eventually leads to app abandonment even if the user initially agrees to adopt the tool [145]. Magnol et al [57] explained that although physician’s recommendation could initially foster mHealth adoption, their potential lack of information on the range of available apps may also be a limitation.
Health consciousness and literacy could play a role in patients’ adoption of health care technologies [40,49,51,65,72,98,107,121, 134,159], as people with higher levels of health consciousness and literacy are typically more cognizant of their health issues and behaviors [93,110,142,156]. However, some studies have concluded that health literacy is not necessarily a significant predictor of mHealth use [73,81,86]. Health behavior is another factor with mixed results. Studies have reported that patients with a positive baseline health behavior, such as better medication adherence rate or a higher physical activity level, were more likely to adopt the tools [41,49,75,106]. Conversely, other researchers found that users with poorer baseline health behavior, such as a lower treatment adherence rate, felt a higher need for the app and used it more frequently [67]. Although Meyerowitz-Katz et al [98] reported a low adoption rate among those who were already healthy eaters before the initiation of mHealth use; Browning et al [48] found no correlation between baseline health behavior and mHealth use in their research.
Relation to other therapies and how the app fits into the overall patient journey and treatment path could play a role in the adoption decision. Several researchers have pointed out that although patients may appreciate the benefits they receive from mHealth, they still perceive it as a complement rather than a replacement for other components and modes of treatment [100]. When mHealth apps are used in isolation from other parts of the treatment and are not integrated into the overall patient journey, adoption rates may suffer [112-114,141,162]. Similarly, it is very important to consider any underlying comorbidities that the patients may have from before using mHealth to ensure a holistic understanding of the data they submit in the apps [80]. The type and burden of other medications may also play a role; for instance, the high burden of cancer treatment can be overwhelming, preventing patients from using an additional tool such as a health app [85]. Furthermore, patients who take multiple long-term medications and those who engage in multiple interventions may be less likely to adopt these tools [52,98]. Jemere et al [96] found that study participants who took medication in the form of a pill were over 3 times more likely to adopt mHealth compared with those who took medication in the form of an injection. It is also worth noting that some studies found that patients who have easy access to satisfactory care services or those who need frequent hospital follow-ups or hospitalization may have a lower mHealth adoption rate because they are often in direct contact with their care team [54,57,102,179].
Insurance status and its impact on mHealth adoption was inconclusive in the included studies. For instance, being publicly insured has been reported as a facilitator in a study by Pierce et al [71] but as a barrier in a study by Warinner et al [90]. Similarly, Anosike et al [126] found that some insured patients are less likely to use mHealth tools if they are not covered by their insurance, and Pierce et al [71] reported that privately insured patients are less likely to use these tools compared with Medicare, Medicaid, and self-pay patients. Others reported that patients who had commercial insurance or preferred provider organization insurance were more likely to use these services [37,82]. It is worth noting that adoption decisions related to patients’ insurance status may differ from one country to another depending on elements such as the legal requirements of minimum insurance cover and local policies on mHealth reimbursement.
Discussion
Practical Implications
This review builds on the growing body of research that investigates patients’ adoption of mHealth services and highlights the complexity of the factors affecting adoption, spanning personal, social, technical, organizational, and health care aspects. This implies that to achieve successful adoption and implementation of these tools, the different players in the health care landscape need to work together to overcome the barriers and harness the potential benefits of novel technologies in health care. Our findings show that mHealth developers and technology providers alone are not likely to achieve success by focusing on creating tools that are technically superior; there are social, organizational, health care, and policy-related factors that must be considered, underlining the central role of care teams and health care policy in promoting adoption.
Although some factors may be very hard to influence (eg, intrinsic motivation or a person’s locus of control), others could be shifted. Figure 7 summarizes our recommendations for a more patient-centered approach to mHealth adoption, covering aspects that may help overcome some of the key barriers reported in this systematic review. This shift may be possible by ensuring the tools’ fit into the overall patient journey and treatment plan, emphasizing inclusive design, warranting comprehensive patient education and support, empowering and mobilizing clinicians and care teams, addressing ethical data management issues, and focusing on health care policies that may facilitate adoption.
Figure 7.
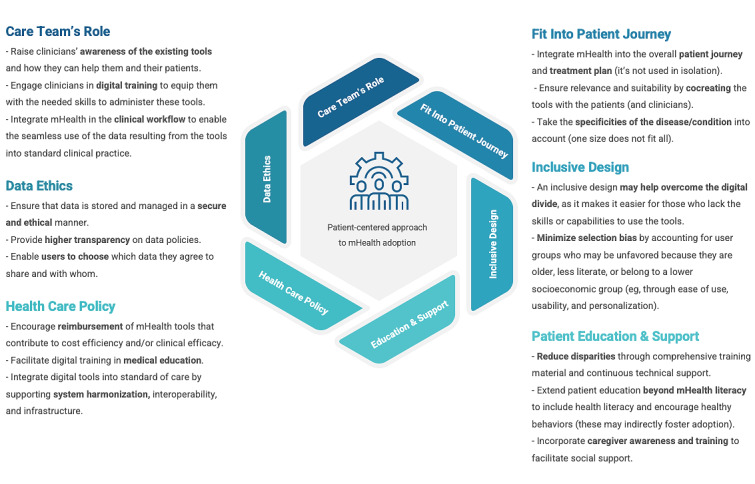
Recommendations for a patient-centered approach to mobile health (mHealth) adoption.
Ensuring the tools’ fit into the overall patient journey and treatment plan, based on the understanding that mHealth apps are not used in isolation, is crucial for sustainable adoption. Technology providers may opt to co-create the tools with patients (and clinicians) to ensure that they have taken their overall journey into account and established how their tool relates to other treatments that the patients are receiving, any comorbidities, and how their specific health condition may influence the way they use the technology [181]. Embedding users as equal partners in all phases of the development process may increase the usefulness, relevance, and appropriateness of the resulting tools, ensuring that they reflect the specificities of each disease and the overall context of the patients, increasing the odds of their adoption.
Inclusive design principles may help developers address the needs of the most vulnerable patient populations who may not be engaging with mHealth owing to their age or health-related physical and cognitive challenges, educational level, socioeconomic status, or their technological skills and experience. Numerous studies have concluded that many demographic factors are typically not the root cause for the lack of adoption per se, but rather other underlying causes were at play, mainly pointing back to a lack of skills and literacy that were typically correlated to more older patients, those with a lower level of education, or those belonging to lower socioeconomic classes. Designing for inclusivity does not ignore the unique features, environments, and cultural contexts of users. Research has shown that many aspects of the digital divide may be addressed through an inclusive design that incorporates cultural appropriateness, easy-to-understand lay language that does not need high literacy levels, and ease-of-use that does not require any sophisticated technical skills. For instance, a design that enables offline use may encourage patients in lower socioeconomic classes who are weary of the overuse of their data package to use the tool. Increasing the personal relevance of tools through personalization may also help address the varying needs of different users, allowing technology providers to cater to different patient populations that may vary in their level of skills, physical or mental capabilities, and literacy.
Another element that may help to reduce disparities in adoption is patient education and support. Comprehensive training materials and continuous technical support may assist some of the most unfavorable patient populations to benefit from these tools. Several studies have reported that the availability of training enables user groups that do not necessarily have the skills or literacy levels to acquire the knowledge that they need to use the tools more easily, especially when it increases their understanding of how the tool may help them improve their condition, step-by-step instructions on how it works, and knowing whom to contact in case of issues or questions. It is worth noting that extending patient education and awareness programs to go beyond mHealth literacy to include health literacy in general and encourage healthy behaviors may foster adoption, as research has shown that these factors may indirectly promote the tools’ uptake. Furthermore, given the important role of social influence, raising caregivers’ awareness may contribute to more successful adoption.
Data ethics is one of the most prominent factors in almost all health technology–related discussions, mostly as a barrier to adoption. Fostering patient adoption necessitates addressing their main fears and concerns by ensuring that their health data are stored and managed in a secure and ethical manner, providing higher transparency on data policies, and, whenever possible, enabling users to choose which data they agree to share and with whom.
Care teams’ role is central to patient adoption, as research shows that the endorsement of the clinician is a key facilitator of patient acceptance of the tools. However, lack of knowledge, skills, or active engagement with mHealth from the care team may discourage patient adoption. Therefore, raising clinicians’ awareness of the existing tools and how they can help them and their patients and engaging them in digital training to equip them with the necessary skills to administer these tools is central to success. Moreover, integrating mHealth in the clinical workflow to enable the seamless use of the data resulting from the tools in standard clinical practice is crucial, as previous studies have reported that patients would often abandon the tools if they feel that their care team is not actively engaging with the data that they feed on these apps.
Furthermore, recognizing potential barriers has essential policy implications for mHealth adoption to improve access to health care services and patient support. Encouraging the reimbursement of mHealth tools that contribute to cost efficiency and clinical efficacy may help overcome the cost-related barriers that were often reported in the studies. Facilitating digital training in medical education may help equip care teams with the necessary skills to implement and administer new technologies. Facilitating the integration of digital tools into the standard of care by supporting system harmonization, interoperability, and infrastructure may play a vital role in overcoming some of the key technical barriers that hinder adoption.
Limitations and Recommendations for Future Research
Although this study contributes to the understanding of the factors affecting patients’ adoption of mHealth services, some limitations must be acknowledged. This review may not have included relevant studies that were not indexed in the searched databases, written in a language other than English, and gray literature searches that could have also allowed the identification of additional relevant insights. However, this study focused on peer-reviewed scientific papers.
In addition, this analysis only considered published studies, and no further contacts were made with the authors of the papers to obtain additional information or to validate our thematic analysis. Consequently, it is possible that other mHealth adoption factors may have been missed. Future reviews could include studies in other languages to gain a better grasp of any interregional or intercultural differences, and to have more studies in developed countries.
Conclusions
This systematic literature review and narrative synthesis builds on and expands the growing body of literature investigating patients’ adoption of mHealth services. Our findings highlight the complexity of the factors affecting adoption, including personal, social, technical, organizational, and health care aspects. We recommend improving patient-centered approaches and taking a more holistic view of adoption factors beyond technical aspects by ensuring the tools’ fit into the overall patient journey and treatment plan. We emphasize the crucial role of inclusive design, which enables comprehensive patient education and support programs. Moreover, we stress the importance of empowering and mobilizing clinicians and care teams, addressing ethical data management issues, and focusing on health care policies that may facilitate adoption such as mHealth reimbursement.
Abbreviations
- mHealth
mobile health
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- QCRI
Qatar Computing Research Institute
Critical Appraisal Skills Program checklist.
Critical appraisal of the included studies.
Phases of thematic analysis based on Braun and Clarke [25].
Characteristics of included studies.
(A) Social and personal factors and their occurrence. (B) Technical and material factors and their occurrence. (C) Health-related factors and their occurrence.
Footnotes
Conflicts of Interest: None declared.
References
- 1.Armstrong AW, Kwong MW, Chase EP, Ledo L, Nesbitt TS, Shewry SL. Teledermatology operational considerations, challenges, and benefits: the referring providers' perspective. Telemed J E Health. 2012 Oct;18(8):580–4. doi: 10.1089/tmj.2011.0241. [DOI] [PubMed] [Google Scholar]
- 2.Avey JP, Hobbs RL. Dial in: fostering the use of telebehavioral health services in frontier Alaska. Psychol Serv. 2013 Aug;10(3):289–97. doi: 10.1037/a0028231.2012-23377-001 [DOI] [PubMed] [Google Scholar]
- 3.Anderson K, Francis T, Ibanez-Carrasco F, Globerman J. Physician's perceptions of telemedicine in HIV care provision: a cross-sectional web-based survey. JMIR Public Health Surveill. 2017 May 30;3(2):e31. doi: 10.2196/publichealth.6896. https://publichealth.jmir.org/2017/2/e31/ v3i2e31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bhatta R, Aryal K, Ellingsen G. Opportunities and challenges of a rural-telemedicine program in Nepal. J Nepal Health Res Counc. 2015;13(30):149–53. [PubMed] [Google Scholar]
- 5.Mileski M, Kruse CS, Catalani J, Haderer T. Adopting telemedicine for the self-management of hypertension: systematic review. JMIR Med Inform. 2017 Oct 24;5(4):e41. doi: 10.2196/medinform.6603. https://medinform.jmir.org/2017/4/e41/ v5i4e41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Puszka S, Dingwall KM, Sweet M, Nagel T. E-mental health innovations for aboriginal and Torres Strait Islander Australians: a qualitative study of implementation needs in health services. JMIR Ment Health. 2016 Sep 19;3(3):e43. doi: 10.2196/mental.5837. https://mental.jmir.org/2016/3/e43/ v3i3e43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Talboom-Kamp EP, Verdijk NA, Kasteleyn MJ, Numans ME, Chavannes NH. From chronic disease management to person-centered eHealth; a review on the necessity for blended care. Clin eHealth. 2018 Mar;1(1):3–7. doi: 10.1016/j.ceh.2018.01.001. [DOI] [Google Scholar]
- 8.Tistad M, Lundell S, Wiklund M, Nyberg A, Holmner A, Wadell K. Usefulness and relevance of an ehealth tool in supporting the self-management of chronic obstructive pulmonary disease: explorative qualitative study of a cocreative process. JMIR Hum Factors. 2018 Oct 26;5(4):e10801. doi: 10.2196/10801. https://humanfactors.jmir.org/2018/4/e10801/ v5i4e10801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stellefson M, Chaney B, Barry AE, Chavarria E, Tennant B, Walsh-Childers K, Sriram PS, Zagora J. Web 2.0 chronic disease self-management for older adults: a systematic review. J Med Internet Res. 2013 Feb 14;15(2):e35. doi: 10.2196/jmir.2439. https://www.jmir.org/2013/2/e35/ v15i2e35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Achelrod D. Policy expectations and reality of telemedicine – a critical analysis of health care outcomes, costs and acceptance for congestive heart failure. J Telemed Telecare. 2014 May 06;20(4):192–200. doi: 10.1177/1357633x14533894. [DOI] [PubMed] [Google Scholar]
- 11.Wang Y, Xue H, Huang Y, Huang L, Zhang D. A systematic review of application and effectiveness of mHealth interventions for obesity and diabetes treatment and self-management. Adv Nutr. 2017 May 15;8(3):449–62. doi: 10.3945/an.116.014100. http://europepmc.org/abstract/MED/28507010 .8/3/449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shivkumar V, Subramanian T, Agarwal P, Mari Z, Mestre TA, Parkinson Study Group Uptake of telehealth in Parkinson's disease clinical care and research during the COVID-19 pandemic. Parkinsonism Relat Disord. 2021 May;86:97–100. doi: 10.1016/j.parkreldis.2021.03.032.S1353-8020(21)00125-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pfammatter AF, Mitsos A, Wang S, Hood SH, Spring B. Evaluating and improving recruitment and retention in an mHealth clinical trial: an example of iterating methods during a trial. Mhealth. 2017 Nov 01;3:49. doi: 10.21037/mhealth.2017.09.02. doi: 10.21037/mhealth.2017.09.02.mh-03-2017.09.02 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fleming T, Bavin L, Lucassen M, Stasiak K, Hopkins S, Merry S. Beyond the trial: systematic review of real-world uptake and engagement with digital self-help interventions for depression, low mood, or anxiety. J Med Internet Res. 2018 Jun 06;20(6):e199. doi: 10.2196/jmir.9275. https://www.jmir.org/2018/6/e199/ v20i6e199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Helander E, Kaipainen K, Korhonen I, Wansink B. Factors related to sustained use of a free mobile app for dietary self-monitoring with photography and peer feedback: retrospective cohort study. J Med Internet Res. 2014 Apr 15;16(4):e109. doi: 10.2196/jmir.3084. https://www.jmir.org/2014/4/e109/ v16i4e109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.MHealth New Horizons for Health Through Mobile Technologies. Geneva: World Health Organization; 2011. [Google Scholar]
- 17.Jacob C, Sanchez-Vazquez A, Ivory C. Social, organizational, and technological factors impacting clinicians’ adoption of mobile health tools: systematic literature review. JMIR Mhealth Uhealth. 2020 Feb 20;8(2):e15935. doi: 10.2196/15935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009 Jul 21;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. https://dx.plos.org/10.1371/journal.pmed.1000097 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Higgins J. Cochrane Handbook for Systematic Reviews of Interventions: Cochrane Book Series. Hoboken, New Jersey: Wiley; 2011. [Google Scholar]
- 20.Jacob C, Ivory C, Sezgin E. Sociotechnical factors impacting patients’ adoption of mHealth tools: a systematic review of the literature [Internet] PROSPERO. 2021. https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=266484 . [DOI] [PMC free article] [PubMed]
- 21.Richardson WS, Wilson MC, Nishikawa J, Hayward RS. The well-built clinical question: a key to evidence-based decisions. ACP J Club. 1995;123(3):A12–3. [PubMed] [Google Scholar]
- 22.Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016 Dec 05;5(1):210. doi: 10.1186/s13643-016-0384-4. https://systematicreviewsjournal.biomedcentral.com/articles/10.1186/s13643-016-0384-4 .10.1186/s13643-016-0384-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.CASP Checklist. CASP. [2022-04-09]. https://casp-uk.net/casp-tools-checklists/
- 24.Jacob C, Sanchez-Vazquez A, Ivory C. Understanding clinicians' adoption of mobile health tools: a qualitative review of the most used frameworks. JMIR Mhealth Uhealth. 2020 Jul 06;8(7):e18072. doi: 10.2196/18072. https://mhealth.jmir.org/2020/7/e18072/ v8i7e18072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006 Jan;3(2):77–101. doi: 10.1191/1478088706qp063oa. [DOI] [Google Scholar]
- 26.Leonardi P. The Routledge Companion to Qualitative Research in Organization Studies. Milton Park, Abingdon-on-Thames, Oxfordshire, England, UK: Routledge; 2017. Methodological guidelines for the study of materiality and affordances. [Google Scholar]
- 27.Ammenwerth E. Technology acceptance models in health informatics: TAM and UTAUT. Stud Health Technol Inform. 2019 Jul 30;263:64–71. doi: 10.3233/SHTI190111.SHTI190111 [DOI] [PubMed] [Google Scholar]
- 28.Ward R. The application of technology acceptance and diffusion of innovation models in healthcare informatics. Health Policy Technol. 2013 Dec;2(4):222–8. doi: 10.1016/j.hlpt.2013.07.002. [DOI] [Google Scholar]
- 29.Rahimi B, Nadri H, Lotfnezhad Afshar H, Timpka T. A systematic review of the technology acceptance model in health informatics. Appl Clin Inform. 2018 Jul 15;9(3):604–34. doi: 10.1055/s-0038-1668091. http://europepmc.org/abstract/MED/30112741 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shachak A, Kuziemsky C, Petersen C. Beyond TAM and UTAUT: future directions for HIT implementation research. J Biomed Inform. 2019 Dec;100:103315. doi: 10.1016/j.jbi.2019.103315. https://linkinghub.elsevier.com/retrieve/pii/S1532-0464(19)30234-5 .S1532-0464(19)30234-5 [DOI] [PubMed] [Google Scholar]
- 31.Sittig DF, Singh H. A new sociotechnical model for studying health information technology in complex adaptive healthcare systems. Qual Saf Health Care. 2010 Oct;19 Suppl 3:68–74. doi: 10.1136/qshc.2010.042085. http://europepmc.org/abstract/MED/20959322 .19/Suppl_3/i68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Riley WT, Rivera DE, Atienza AA, Nilsen W, Allison SM, Mermelstein R. Health behavior models in the age of mobile interventions: are our theories up to the task? Transl Behav Med. 2011 Mar;1(1):53–71. doi: 10.1007/s13142-011-0021-7. http://europepmc.org/abstract/MED/21796270 .21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Karsh B. Beyond usability: designing effective technology implementation systems to promote patient safety. Qual Saf Health Care. 2004 Oct;13(5):388–94. doi: 10.1136/qhc.13.5.388. https://qhc.bmj.com/lookup/pmidlookup?view=long&pmid=15465944 .13/5/388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dai M, Xu J, Lin J, Wang Z, Huang W, Huang J. Willingness to use mobile health in Glaucoma patients. Telemed J E Health. 2017 Oct;23(10):822–7. doi: 10.1089/tmj.2016.0254. [DOI] [PubMed] [Google Scholar]
- 35.Beard C, Silverman AL, Forgeard M, Wilmer MT, Torous J, Björgvinsson T. Smartphone, social media, and mental health app use in an acute transdiagnostic psychiatric sample. JMIR Mhealth Uhealth. 2019 Jun 07;7(6):e13364. doi: 10.2196/13364. https://mhealth.jmir.org/2019/6/e13364/ v7i6e13364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Breil B, Kremer L, Hennemann S, Apolinário-Hagen J. Acceptance of mHealth apps for self-management among people with hypertension. Stud Health Technol Inform. 2019 Sep 03;267:282–8. doi: 10.3233/SHTI190839.SHTI190839 [DOI] [PubMed] [Google Scholar]
- 37.Darcourt JG, Aparicio K, Dorsey PM, Ensor JE, Zsigmond EM, Wong ST, Ezeana CF, Puppala M, Heyne KE, Geyer CE, Phillips RA, Schwartz RL, Chang JC. Analysis of the implementation of telehealth visits for care of patients with cancer in Houston during the COVID-19 pandemic. JCO Oncol Pract. 2021 Jan;17(1):e36–43. doi: 10.1200/OP.20.00572. http://europepmc.org/abstract/MED/33026951 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.de Vries ST, Denig P, Lasheras Ruiz C, Houÿez F, Wong L, Sutcliffe A, Mol PG, IMI Web-RADR Work Package 3b Consortium Interest in a mobile app for two-way risk communication: a survey study among European healthcare professionals and patients. Drug Saf. 2018 Jul 2;41(7):697–712. doi: 10.1007/s40264-018-0648-0. http://europepmc.org/abstract/MED/29500800 .10.1007/s40264-018-0648-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hansen AH, Bradway M, Broz J, Claudi T, Henriksen O, Wangberg SC, Årsand E. Inequalities in the use of eHealth between socioeconomic groups among patients with type 1 and type 2 diabetes: cross-sectional study. J Med Internet Res. 2019 May 29;21(5):e13615. doi: 10.2196/13615. https://www.jmir.org/2019/5/e13615/ v21i5e13615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Knitza J, Simon D, Lambrecht A, Raab C, Tascilar K, Hagen M, Kleyer A, Bayat S, Derungs A, Amft O, Schett G, Hueber AJ. Mobile health usage, preferences, barriers, and eHealth literacy in rheumatology: patient survey study. JMIR Mhealth Uhealth. 2020 Aug 12;8(8):e19661. doi: 10.2196/19661. https://mhealth.jmir.org/2020/8/e19661/ v8i8e19661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lee K, Bejerano IL, Han M, Choi HS. Willingness to use smartphone apps for lifestyle management among patients with schizophrenia. Arch Psychiatr Nurs. 2019 Aug;33(4):329–36. doi: 10.1016/j.apnu.2019.01.002.S0883-9417(18)30335-2 [DOI] [PubMed] [Google Scholar]
- 42.Reinecke F, Dittrich F, Dudda M, Stang A, Polan C, Müller R, Beck P, Kauther MD. Acceptance, barriers, and future preferences of mobile health among patients receiving trauma and orthopedic surgical care: paper-based survey in a prospective multicenter study. JMIR Mhealth Uhealth. 2021 Apr 21;9(4):e23784. doi: 10.2196/23784. https://mhealth.jmir.org/2021/4/e23784/ v9i4e23784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sin DY, Guo X, Yong DW, Qiu TY, Moey PK, Falk M, Tan NC. Assessment of willingness to tele-monitoring interventions in patients with type 2 diabetes and/or hypertension in the public primary healthcare setting. BMC Med Inform Decis Mak. 2020 Jan 28;20(1):11. doi: 10.1186/s12911-020-1024-4. https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/s12911-020-1024-4 .10.1186/s12911-020-1024-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Spooner KK, Salemi JL, Salihu HM, Zoorob RJ. eHealth patient-provider communication in the United States: interest, inequalities, and predictors. J Am Med Inform Assoc. 2017 Apr 01;24(e1):e18–27. doi: 10.1093/jamia/ocw087. http://europepmc.org/abstract/MED/27497797 .ocw087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Su J, Dugas M, Guo X, Gao G. Influence of personality on mHealth use in patients with diabetes: prospective pilot study. JMIR Mhealth Uhealth. 2020 Aug 10;8(8):e17709. doi: 10.2196/17709. https://mhealth.jmir.org/2020/8/e17709/ v8i8e17709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sun L, Jiao C, Wang Y, Xiao Q, Zhang Y, Wu Y. A survey on the willingness to use physical activity smartphone applications (Apps) in patients with chronic diseases. Stud Health Technol Inform. 2016;225:1032–3. [PubMed] [Google Scholar]
- 47.Aghazadeh H, Crump T, Tennant M, Weis E. Use of mobile health (mHealth) technologies in ophthalmology patients in Alberta. Can J Ophthalmol. 2019 Apr;54(2):164–70. doi: 10.1016/j.jcjo.2018.05.010.S0008-4182(17)31126-2 [DOI] [PubMed] [Google Scholar]
- 48.Browning RB, McGillicuddy JW, Treiber FA, Taber DJ. Kidney transplant recipients' attitudes about using mobile health technology for managing and monitoring medication therapy. J Am Pharm Assoc (2003) 2016;56(4):450–4.e1. doi: 10.1016/j.japh.2016.03.017. http://europepmc.org/abstract/MED/27450140 .S1544-3191(16)30032-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ernsting C, Stühmann LM, Dombrowski SU, Voigt-Antons J, Kuhlmey A, Gellert P. Associations of health app use and perceived effectiveness in people with cardiovascular diseases and diabetes: population-based survey. JMIR Mhealth Uhealth. 2019 Mar 28;7(3):e12179. doi: 10.2196/12179. https://mhealth.jmir.org/2019/3/e12179/ v7i3e12179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Jaffe DH, Lee L, Huynh S, Haskell TP. Health inequalities in the use of telehealth in the United States in the lens of COVID-19. Popul Health Manag. 2020 Oct 01;23(5):368–77. doi: 10.1089/pop.2020.0186. [DOI] [PubMed] [Google Scholar]
- 51.Kontos E, Blake KD, Chou WS, Prestin A. Predictors of eHealth usage: insights on the digital divide from the health information national trends survey 2012. J Med Internet Res. 2014 Jul 16;16(7):e172. doi: 10.2196/jmir.3117. https://www.jmir.org/2014/7/e172/ v16i7e172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mangin D, Parascandalo J, Khudoyarova O, Agarwal G, Bismah V, Orr S. Multimorbidity, eHealth and implications for equity: a cross-sectional survey of patient perspectives on eHealth. BMJ Open. 2019 Feb 12;9(2):e023731. doi: 10.1136/bmjopen-2018-023731. https://bmjopen.bmj.com/lookup/pmidlookup?view=long&pmid=30760515 .bmjopen-2018-023731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Potdar R, Thomas A, DiMeglio M, Mohiuddin K, Djibo DA, Laudanski K, Dourado CM, Leighton JC, Ford JG. Access to internet, smartphone usage, and acceptability of mobile health technology among cancer patients. Support Care Cancer. 2020 Nov 12;28(11):5455–61. doi: 10.1007/s00520-020-05393-1.10.1007/s00520-020-05393-1 [DOI] [PubMed] [Google Scholar]
- 54.Ye Q, Deng Z, Chen Y, Liao J, Li G, Lu Y. How resource scarcity and accessibility affect patients' usage of mobile health in China: resource competition perspective. JMIR Mhealth Uhealth. 2019 Aug 09;7(8):e13491. doi: 10.2196/13491. https://mhealth.jmir.org/2019/8/e13491/ v7i8e13491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Qan'ir Y, Khalifeh A, Eid M, Hammad B, Al-Batran M. Mobile health apps use among Jordanian outpatients: a descriptive study. Health Informatics J. 2021;27(2):14604582211017940. doi: 10.1177/14604582211017940. https://journals.sagepub.com/doi/10.1177/14604582211017940?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed . [DOI] [PubMed] [Google Scholar]
- 56.Ali EE, Leow JL, Chew L, Yap KY. Patients' perception of app-based educational and behavioural interventions for enhancing oral anticancer medication adherence. J Cancer Educ. 2018 Dec 14;33(6):1306–13. doi: 10.1007/s13187-017-1248-x.10.1007/s13187-017-1248-x [DOI] [PubMed] [Google Scholar]
- 57.Magnol M, Eleonore B, Claire R, Castagne B, Pugibet M, Lukas C, Tournadre A, Vergne-Salle P, Barnetche T, Truchetet M, Ruyssen-Witrand A. Use of ehealth by patients with rheumatoid arthritis: observational, cross-sectional, multicenter study. J Med Internet Res. 2021 Jan 29;23(1):e19998. doi: 10.2196/19998. https://www.jmir.org/2021/1/e19998/ v23i1e19998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Alwashmi MF, Fitzpatrick B, Farrell J, Gamble J, Davis E, Nguyen HV, Farrell G, Hawboldt J. Perceptions of patients regarding mobile health interventions for the management of chronic obstructive pulmonary disease: mixed methods study. JMIR Mhealth Uhealth. 2020 Jul 23;8(7):e17409. doi: 10.2196/17409. https://mhealth.jmir.org/2020/7/e17409/ v8i7e17409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Byambasuren O, Beller E, Hoffmann T, Glasziou P. Barriers to and facilitators of the prescription of mHealth apps in Australian general practice: qualitative study. JMIR Mhealth Uhealth. 2020 Jul 30;8(7):e17447. doi: 10.2196/17447. https://mhealth.jmir.org/2020/7/e17447/ v8i7e17447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Cook EJ, Randhawa G, Sharp C, Ali N, Guppy A, Barton G, Bateman A, Crawford-White J. Exploring the factors that influence the decision to adopt and engage with an integrated assistive telehealth and telecare service in Cambridgeshire, UK: a nested qualitative study of patient 'users' and 'non-users'. BMC Health Serv Res. 2016 Apr 19;16:137. doi: 10.1186/s12913-016-1379-5. https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-016-1379-5 .10.1186/s12913-016-1379-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Eno AK, Ruck JM, Van Pilsum Rasmussen SE, Waldram MM, Thomas AG, Purnell TS, Garonzik Wang JM, Massie AB, Al Almmary F, Cooper LM, Segev DL, Levan MA, Henderson ML. Perspectives on implementing mobile health technology for living kidney donor follow-up: in-depth interviews with transplant providers. Clin Transplant. 2019 Aug 26;33(8):e13637. doi: 10.1111/ctr.13637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Fischer SH, Ray KN, Mehrotra A, Bloom EL, Uscher-Pines L. Prevalence and characteristics of telehealth utilization in the United States. JAMA Netw Open. 2020 Oct 01;3(10):e2022302. doi: 10.1001/jamanetworkopen.2020.22302. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2020.22302 .2772162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Reddy R, Majmudar M, Dhopeshwarkar N, Vacaro V, Isselbacher E, Bhatt AB. Mobile health apps preferences and practice among ambulatory cardiovascular patients. Future Cardiol. 2018 Sep;14(5):381–8. doi: 10.2217/fca-2018-0005. [DOI] [PubMed] [Google Scholar]
- 64.Gordon NP, Hornbrook MC. Differences in access to and preferences for using patient portals and other eHealth technologies based on race, ethnicity, and age: a database and survey study of seniors in a large health plan. J Med Internet Res. 2016 Mar 04;18(3):e50. doi: 10.2196/jmir.5105. https://www.jmir.org/2016/3/e50/ v18i3e50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kamis K, Janevic MR, Marinec N, Jantz R, Valverde H, Piette JD. A study of mobile phone use among patients with noncommunicable diseases in La Paz, Bolivia: implications for mHealth research and development. Global Health. 2015 Jul 04;11:30. doi: 10.1186/s12992-015-0115-y. https://globalizationandhealth.biomedcentral.com/articles/10.1186/s12992-015-0115-y .10.1186/s12992-015-0115-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Gordon NP, Hornbrook MC. Older adults' readiness to engage with eHealth patient education and self-care resources: a cross-sectional survey. BMC Health Serv Res. 2018 Mar 27;18(1):220. doi: 10.1186/s12913-018-2986-0. https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-018-2986-0 .10.1186/s12913-018-2986-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Khalemsky M, Schwartz DG, Silberg T, Khalemsky A, Jaffe E, Herbst R. Childrens' and parents' willingness to join a smartphone-based emergency response community for anaphylaxis: survey. JMIR Mhealth Uhealth. 2019 Aug 27;7(8):e13892. doi: 10.2196/13892. https://mhealth.jmir.org/2019/8/e13892/ v7i8e13892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Colls J, Lee Y, Xu C, Corrigan C, Lu F, Marquez-Grap G, Murray M, Suh D, Solomon D. Patient adherence with a smartphone app for patient-reported outcomes in rheumatoid arthritis. Rheumatology (Oxford) 2021 Jan 05;60(1):108–12. doi: 10.1093/rheumatology/keaa202.5861028 [DOI] [PubMed] [Google Scholar]
- 69.Foster A, Horspool KA, Edwards L, Thomas CL, Salisbury C, Montgomery AA, O'Cathain A. Who does not participate in telehealth trials and why? A cross-sectional survey. Trials. 2015 Jun 05;16(1):258. doi: 10.1186/s13063-015-0773-3. https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-015-0773-3 .10.1186/s13063-015-0773-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ware P, Dorai M, Ross HJ, Cafazzo JA, Laporte A, Boodoo C, Seto E. Patient adherence to a mobile phone-based heart failure telemonitoring program: a longitudinal mixed-methods study. JMIR Mhealth Uhealth. 2019 Feb 26;7(2):e13259. doi: 10.2196/13259. https://mhealth.jmir.org/2019/2/e13259/ v7i2e13259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Pierce R, Stevermer J. Disparities in use of telehealth at the onset of the COVID-19 public health emergency. J Telemed Telecare. 2020 Oct 21;:1357633X2096389. doi: 10.1177/1357633X20963893. doi: 10.1177/1357633X20963893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Jiang J, Zhu Q, Zheng Y, Zhu Y, Li Y, Huo Y. Perceptions and acceptance of mHealth in patients with cardiovascular diseases: a cross-sectional study. JMIR Mhealth Uhealth. 2019 Feb 04;7(2):e10117. doi: 10.2196/10117. https://mhealth.jmir.org/2019/2/e10117/ v7i2e10117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Wiggers A, Peek N, Kraaijenhagen R, Jaspers M. Determinants of eligibility and use of ehealth for cardiac rehabilitation patients: preliminary results. Stud Health Technol Inform. 2014;205:818–22. [PubMed] [Google Scholar]
- 74.Edwards L, Thomas C, Gregory A, Yardley L, O'Cathain A, Montgomery AA, Salisbury C. Are people with chronic diseases interested in using telehealth? A cross-sectional postal survey. J Med Internet Res. 2014 May 08;16(5):e123. doi: 10.2196/jmir.3257. https://www.jmir.org/2014/5/e123/ v16i5e123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hasenöhrl T, Windschnurer T, Dorotka R, Ambrozy C, Crevenna R. Prescription of individual therapeutic exercises via smartphone app for patients suffering from non-specific back pain : a qualitative feasibility and quantitative pilot study. Wien Klin Wochenschr. 2020 Mar 14;132(5-6):115–23. doi: 10.1007/s00508-020-01616-x. http://europepmc.org/abstract/MED/32060724 .10.1007/s00508-020-01616-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Jaana M, Paré G. Comparison of mobile health technology use for self-tracking between older adults and the general adult population in Canada: cross-sectional survey. JMIR Mhealth Uhealth. 2020 Nov 27;8(11):e24718. doi: 10.2196/24718. https://mhealth.jmir.org/2020/11/e24718/ v8i11e24718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Abelson J, Kaufman E, Symer M, Peters A, Charlson M, Yeo H. Barriers and benefits to using mobile health technology after operation: a qualitative study. Surgery. 2017 Sep;162(3):605–11. doi: 10.1016/j.surg.2017.05.007.S0039-6060(17)30331-8 [DOI] [PubMed] [Google Scholar]
- 78.de Vries ST, Wong L, Sutcliffe A, Houÿez F, Ruiz CL, Mol PG, IMI Web-RADR Work Package 3b Consortium Factors influencing the use of a mobile app for reporting adverse drug reactions and receiving safety information: a qualitative study. Drug Saf. 2017 May;40(5):443–55. doi: 10.1007/s40264-016-0494-x. http://europepmc.org/abstract/MED/28035492 .10.1007/s40264-016-0494-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Runz-Jørgensen SM, Schiøtz ML, Christensen U. Perceived value of eHealth among people living with multimorbidity: a qualitative study. J Comorb. 2017;7(1):96–111. doi: 10.15256/joc.2017.7.98. https://journals.sagepub.com/doi/10.15256/joc.2017.7.98?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed .joc.2017.7.98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.De La Cruz Monroy MF, Mosahebi A. The use of smartphone applications (apps) for enhancing communication with surgical patients: a systematic review of the literature. Surg Innov. 2019 Apr;26(2):244–59. doi: 10.1177/1553350618819517. [DOI] [PubMed] [Google Scholar]
- 81.Cajita MI, Hodgson NA, Budhathoki C, Han H. Intention to use mHealth in older adults with heart failure. J Cardiovasc Nurs. 2017;32(6):E1–7. doi: 10.1097/JCN.0000000000000401. http://europepmc.org/abstract/MED/28248747 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Darrat I, Tam S, Boulis M, Williams AM. Socioeconomic disparities in patient use of telehealth during the Coronavirus disease 2019 surge. JAMA Otolaryngol Head Neck Surg. 2021 Mar 01;147(3):287–95. doi: 10.1001/jamaoto.2020.5161. http://europepmc.org/abstract/MED/33443539 .2775067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Torrent-Sellens J, Díaz-Chao Á, Soler-Ramos I, Saigí-Rubió F. Modelling and predicting eHealth usage in Europe: a multidimensional approach from an online survey of 13,000 European Union internet users. J Med Internet Res. 2016 Jul 22;18(7):e188. doi: 10.2196/jmir.5605. https://www.jmir.org/2016/7/e188/ v18i7e188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Abelson JS, Symer M, Peters A, Charlson M, Yeo H. Mobile health apps and recovery after surgery: what are patients willing to do? Am J Surg. 2017 Oct;214(4):616–22. doi: 10.1016/j.amjsurg.2017.06.009.S0002-9610(17)30230-1 [DOI] [PubMed] [Google Scholar]
- 85.Gupta A, Ocker G, Chow P. Recruiting breast cancer patients for mHealth research: obstacles to clinic-based recruitment for a mobile phone app intervention study. Clin Trials. 2020 Dec;17(6):675–83. doi: 10.1177/1740774520939247. doi: 10.1177/1740774520939247. [DOI] [PubMed] [Google Scholar]
- 86.Bauer AM, Rue T, Keppel GA, Cole AM, Baldwin L, Katon W. Use of mobile health (mHealth) tools by primary care patients in the WWAMI region Practice and Research Network (WPRN) J Am Board Fam Med. 2014 Nov 07;27(6):780–8. doi: 10.3122/jabfm.2014.06.140108. http://www.jabfm.org/cgi/pmidlookup?view=long&pmid=25381075 .27/6/780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Scherer J, Keller F, Pape H, Osterhoff G. Would patients undergo postoperative follow-up by using a smartphone application? BMC Surg. 2020 Oct 07;20(1):229. doi: 10.1186/s12893-020-00889-3. https://bmcsurg.biomedcentral.com/articles/10.1186/s12893-020-00889-3 .10.1186/s12893-020-00889-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Theis S, Schäfer D, Bröhl C, Schäfer K, Rasche P, Wille M, Brandl C, Jochems N, Nitsch V, Mertens A. Predicting technology usage by health information need of older adults: implications for eHealth technology. Work. 2019 Mar 19;62(3):443–57. doi: 10.3233/WOR-192878.WOR192878 [DOI] [PubMed] [Google Scholar]
- 89.Liu X, Wang R, Zhou D, Hong Z. Feasibility and acceptability of smartphone applications for seizure self-management in China: questionnaire study among people with epilepsy. Epilepsy Behav. 2016 Feb;55:57–61. doi: 10.1016/j.yebeh.2015.11.024.S1525-5050(15)00649-6 [DOI] [PubMed] [Google Scholar]
- 90.Warinner C, Hayirli T, Bergmark R, Sethi R, Rettig E. Patterns of technology use among patients with head and neck cancer and implications for telehealth. OTO Open. 2021 Jun 07;5(2):2473974X2110186. doi: 10.1177/2473974X211018612. doi: 10.1177/2473974X211018612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Zhang Y, Li X, Luo S, Liu C, Xie Y, Guo J, Liu F, Zhou Z. Use, perspectives, and attitudes regarding diabetes management mobile apps among diabetes patients and diabetologists in China: national web-based survey. JMIR Mhealth Uhealth. 2019 Feb 08;7(2):e12658. doi: 10.2196/12658. https://mhealth.jmir.org/2019/2/e12658/ v7i2e12658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Dandachi D, Dang BN, Lucari B, Teti M, Giordano TP. Exploring the attitude of patients with HIV about using telehealth for HIV care. AIDS Patient Care STDS. 2020 Apr 01;34(4):166–72. doi: 10.1089/apc.2019.0261. [DOI] [PubMed] [Google Scholar]
- 93.Lupiáñez-Villanueva F, Folkvord F, Vanden Abeele M. Influence of the business revenue, recommendation, and provider models on mobile health app adoption: three-country experimental vignette study. JMIR Mhealth Uhealth. 2020 Jun 04;8(6):e17272. doi: 10.2196/17272. https://mhealth.jmir.org/2020/6/e17272/ v8i6e17272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Hoque MR, Bao Y, Sorwar G. Investigating factors influencing the adoption of e-Health in developing countries: a patient's perspective. Inform Health Soc Care. 2017 Jan;42(1):1–17. doi: 10.3109/17538157.2015.1075541. [DOI] [PubMed] [Google Scholar]
- 95.Reiners F, Sturm J, Bouw LJ, Wouters EJ. Sociodemographic factors influencing the use of eHealth in people with chronic diseases. Int J Environ Res Public Health. 2019 Feb 21;16(4):645. doi: 10.3390/ijerph16040645. https://www.mdpi.com/resolver?pii=ijerph16040645 .ijerph16040645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Jemere AT, Yeneneh YE, Tilahun B, Fritz F, Alemu S, Kebede M. Access to mobile phone and willingness to receive mHealth services among patients with diabetes in Northwest Ethiopia: a cross-sectional study. BMJ Open. 2019 Jan 24;9(1):e021766. doi: 10.1136/bmjopen-2018-021766. https://bmjopen.bmj.com/lookup/pmidlookup?view=long&pmid=30679284 .bmjopen-2018-021766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Sun L, Wang Y, Greene B, Xiao Q, Jiao C, Ji M, Wu Y. Facilitators and barriers to using physical activity smartphone apps among Chinese patients with chronic diseases. BMC Med Inform Decis Mak. 2017 Apr 19;17(1):44. doi: 10.1186/s12911-017-0446-0. https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/s12911-017-0446-0 .10.1186/s12911-017-0446-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Meyerowitz-Katz G, Ravi S, Arnolda L, Feng X, Maberly G, Astell-Burt T. Rates of attrition and dropout in app-based interventions for chronic disease: systematic review and meta-analysis. J Med Internet Res. 2020 Sep 29;22(9):e20283. doi: 10.2196/20283. https://www.jmir.org/2020/9/e20283/ v22i9e20283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Senft N, Everson J. eHealth engagement as a response to negative healthcare experiences: cross-sectional survey analysis. J Med Internet Res. 2018 Dec 05;20(12):e11034. doi: 10.2196/11034. https://www.jmir.org/2018/12/e11034/ v20i12e11034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Ball E, Newton S, Rohricht F, Steed L, Birch J, Dodds J, Cantalapiedra Calvete C, Taylor S, Rivas C. mHealth: providing a mindfulness app for women with chronic pelvic pain in gynaecology outpatient clinics: qualitative data analysis of user experience and lessons learnt. BMJ Open. 2020 Mar 12;10(3):e030711. doi: 10.1136/bmjopen-2019-030711. https://bmjopen.bmj.com/lookup/pmidlookup?view=long&pmid=32165550 .bmjopen-2019-030711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Korpershoek YJ, Vervoort SC, Trappenburg JC, Schuurmans MJ. Perceptions of patients with chronic obstructive pulmonary disease and their health care providers towards using mHealth for self-management of exacerbations: a qualitative study. BMC Health Serv Res. 2018 Oct 04;18(1):757. doi: 10.1186/s12913-018-3545-4. https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-018-3545-4 .10.1186/s12913-018-3545-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Woo K, Dowding DW. Decision-making factors associated with telehealth adoption by patients with heart failure at home: a qualitative study. Comput Inform Nurs. 2020 Apr;38(4):204–14. doi: 10.1097/CIN.0000000000000589. http://europepmc.org/abstract/MED/31929355 .00024665-202004000-00007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Hawley CE, Genovese N, Owsiany MT, Triantafylidis LK, Moo LR, Linsky AM, Sullivan JL, Paik JM. Rapid integration of home telehealth visits amidst COVID-19: what do older adults need to succeed? J Am Geriatr Soc. 2020 Nov 04;68(11):2431–9. doi: 10.1111/jgs.16845. http://europepmc.org/abstract/MED/32930391 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Patoz M, Hidalgo-Mazzei D, Blanc O, Verdolini N, Pacchiarotti I, Murru A, Zukerwar L, Vieta E, Llorca P, Samalin L. Patient and physician perspectives of a smartphone application for depression: a qualitative study. BMC Psychiatry. 2021 Jan 29;21(1):65. doi: 10.1186/s12888-021-03064-x. https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-021-03064-x .10.1186/s12888-021-03064-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Smith R, Menon J, Rajeev JG, Feinberg L, Kumar RK, Banerjee A. Potential for the use of mHealth in the management of cardiovascular disease in Kerala: a qualitative study. BMJ Open. 2015 Nov 17;5(11):e009367. doi: 10.1136/bmjopen-2015-009367. https://bmjopen.bmj.com/lookup/pmidlookup?view=long&pmid=26576813 .bmjopen-2015-009367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Ali E, Chan S, Leow J, Chew L, Yap KY. User acceptance of an app-based adherence intervention: perspectives from patients taking oral anticancer medications. J Oncol Pharm Pract. 2019 Mar;25(2):390–7. doi: 10.1177/1078155218778106. https://journals.sagepub.com/doi/10.1177/1078155218778106?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Simblett S, Matcham F, Siddi S, Bulgari V, Barattieri di San Pietro C, Hortas López J, Ferrão J, Polhemus A, Haro JM, de Girolamo G, Gamble P, Eriksson H, Hotopf M, Wykes T, RADAR-CNS Consortium Barriers to and facilitators of engagement with mHealth technology for remote measurement and management of depression: qualitative analysis. JMIR Mhealth Uhealth. 2019 Jan 30;7(1):e11325. doi: 10.2196/11325. https://mhealth.jmir.org/2019/1/e11325/ v7i1e11325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Wiseman JT, Fernandes-Taylor S, Barnes ML, Tomsejova A, Saunders RS, Kent KC. Conceptualizing smartphone use in outpatient wound assessment: patients' and caregivers' willingness to use technology. J Surg Res. 2015 Sep;198(1):245–51. doi: 10.1016/j.jss.2015.05.011. http://europepmc.org/abstract/MED/26025626 .S0022-4804(15)00579-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Chen P, Xiao L, Gou Z, Xiang L, Zhang X, Feng P. Telehealth attitudes and use among medical professionals, medical students and patients in China: a cross-sectional survey. Int J Med Inform. 2017 Dec;108:13–21. doi: 10.1016/j.ijmedinf.2017.09.009.S1386-5056(17)30232-0 [DOI] [PubMed] [Google Scholar]
- 110.Haldane V, Tan YG, Teo KW, Koh JJK, Srivastava A, Cheng RX, Yap YC, Ong P, van Dam RM, Foo JM, Müller-Riemenschneider F, Koh GC, Perel P, Legido-Quigley H. Perspectives on acceptance and use of a mobile health intervention for the prevention of atherosclerotic cardiovascular disease in Singapore: mixed-methods study. JMIR Mhealth Uhealth. 2019 Mar 14;7(3):e11108. doi: 10.2196/11108. https://mhealth.jmir.org/2019/3/e11108/ v7i3e11108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Javanparast S, Roeger L, Kwok Y, Reed RL. The experience of Australian general practice patients at high risk of poor health outcomes with telehealth during the COVID-19 pandemic: a qualitative study. BMC Fam Pract. 2021 Apr 08;22(1):69. doi: 10.1186/s12875-021-01408-w. https://bmcfampract.biomedcentral.com/articles/10.1186/s12875-021-01408-w .10.1186/s12875-021-01408-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Papoutsi C, A'Court C, Wherton J, Shaw S, Greenhalgh T. Explaining the mixed findings of a randomised controlled trial of telehealth with centralised remote support for heart failure: multi-site qualitative study using the NASSS framework. Trials. 2020 Oct 27;21(1):891. doi: 10.1186/s13063-020-04817-x. https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-020-04817-x .10.1186/s13063-020-04817-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Rush K, Hatt L, Gorman N, Janicki L, Polasek P, Shay M. Planning telehealth for older adults with atrial fibrillation in rural communities: understanding stakeholder perspectives. Clin Nurs Res. 2019 Feb;28(2):130–49. doi: 10.1177/1054773818758170. doi: 10.1177/1054773818758170. [DOI] [PubMed] [Google Scholar]
- 114.Bentley CL, Powell L, Potter S, Parker J, Mountain GA, Bartlett YK, Farwer J, O'Connor C, Burns J, Cresswell RL, Dunn HD, Hawley MS. The use of a smartphone app and an activity tracker to promote physical activity in the management of chronic obstructive pulmonary disease: randomized controlled feasibility study. JMIR Mhealth Uhealth. 2020 Jun 03;8(6):e16203. doi: 10.2196/16203. https://mhealth.jmir.org/2020/6/e16203/ v8i6e16203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.James N, Power E, Hogden A, Vucic S. Patients' perspectives of multidisciplinary home-based e-Health service delivery for motor neurone disease. Disabil Rehabil Assist Technol. 2019 Oct;14(7):737–43. doi: 10.1080/17483107.2018.1499139. [DOI] [PubMed] [Google Scholar]
- 116.Margineanu I, Louka C, Vincenti-Gonzalez M, Saktiawati AM, Schierle J, Abass KM, Akkerman O, Alffenaar J, Ranchor AV, Stienstra Y. Patients and medical staff attitudes toward the future inclusion of ehealth in tuberculosis management: perspectives from six countries evaluated using a qualitative framework. JMIR Mhealth Uhealth. 2020 Nov 02;8(11):e18156. doi: 10.2196/18156. https://mhealth.jmir.org/2020/11/e18156/ v8i11e18156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Steare T, Giorgalli M, Free K, Harju-Seppänen J, Akther S, Eskinazi M, O'Hanlon P, Rostill H, Amani S, Lloyd-Evans B, Osborn D, Johnson S. A qualitative study of stakeholder views on the use of a digital app for supported self-management in early intervention services for psychosis. BMC Psychiatry. 2021 Jun 19;21(1):311. doi: 10.1186/s12888-021-03317-9. https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-021-03317-9 .10.1186/s12888-021-03317-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Vo V, Auroy L, Sarradon-Eck A. Patients' perceptions of mHealth apps: meta-ethnographic review of qualitative studies. JMIR Mhealth Uhealth. 2019 Jul 10;7(7):e13817. doi: 10.2196/13817. https://mhealth.jmir.org/2019/7/e13817/ v7i7e13817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Kemp MT, Williams AM, Sharma SB, Biesterveld BE, Wakam GK, Matusko N, Wilson JK, Cohen MS, Alam HB. Barriers associated with failed completion of an acute care general surgery telehealth clinic visit. Surgery. 2020 Nov;168(5):851–8. doi: 10.1016/j.surg.2020.06.029.S0039-6060(20)30422-0 [DOI] [PubMed] [Google Scholar]
- 120.Thomas NA, Drewry A, Racine Passmore S, Assad N, Hoppe KK. Patient perceptions, opinions and satisfaction of telehealth with remote blood pressure monitoring postpartum. BMC Pregnancy Childbirth. 2021 Feb 19;21(1):153. doi: 10.1186/s12884-021-03632-9. https://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/s12884-021-03632-9 .10.1186/s12884-021-03632-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Nelson LA, Mulvaney SA, Gebretsadik T, Ho Y, Johnson KB, Osborn CY. Disparities in the use of a mHealth medication adherence promotion intervention for low-income adults with type 2 diabetes. J Am Med Inform Assoc. 2016 Jan;23(1):12–8. doi: 10.1093/jamia/ocv082. http://europepmc.org/abstract/MED/26186935 .ocv082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Weber E, Miller S, Astha V, Janevic T, Benn E. Characteristics of telehealth users in NYC for COVID-related care during the coronavirus pandemic. J Am Med Inform Assoc. 2020 Dec 09;27(12):1949–54. doi: 10.1093/jamia/ocaa216. http://europepmc.org/abstract/MED/32866249 .5899728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Campos-Castillo C, Anthony D. Racial and ethnic differences in self-reported telehealth use during the COVID-19 pandemic: a secondary analysis of a US survey of internet users from late March. J Am Med Inform Assoc. 2021 Jan 15;28(1):119–25. doi: 10.1093/jamia/ocaa221. http://europepmc.org/abstract/MED/32894772 .5902454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Almandoz J, Xie L, Schellinger J, Mathew M, Edwards K, Ofori A, Kukreja S, Schneider B, Messiah S. Telehealth utilization among multi-ethnic patients with obesity during the COVID-19 pandemic. J Telemed Telecare. 2021 Mar 04;:1357633X2199821. doi: 10.1177/1357633X21998211. doi: 10.1177/1357633X21998211. [DOI] [PubMed] [Google Scholar]
- 125.Raghunathan NJ, Korenstein D, Li QS, Tonorezos ES, Mao JJ. Determinants of mobile technology use and smartphone application interest in cancer patients. Cancer Med. 2018 Nov;7(11):5812–9. doi: 10.1002/cam4.1660. doi: 10.1002/cam4.1660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Anosike C, Adibe M, Isah A, Ukoha-Kalu O. Willingness to pay for pharmacist-provided home telemonitoring among patients with chronic diseases in Enugu metropolis. Health Informatics J. 2020 Jun;26(2):829–40. doi: 10.1177/1460458219852534. https://journals.sagepub.com/doi/10.1177/1460458219852534?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed . [DOI] [PubMed] [Google Scholar]
- 127.Zhang X, Yu P, Yan J, Ton A M Spil I. Using diffusion of innovation theory to understand the factors impacting patient acceptance and use of consumer e-health innovations: a case study in a primary care clinic. BMC Health Serv Res. 2015 Feb 21;15:71. doi: 10.1186/s12913-015-0726-2. https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-015-0726-2 .10.1186/s12913-015-0726-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Geronimo A, Wright C, Morris A, Walsh S, Snyder B, Simmons Z. Incorporation of telehealth into a multidisciplinary ALS Clinic: feasibility and acceptability. Amyotroph Lateral Scler Frontotemporal Degener. 2017 Nov 05;18(7-8):555–61. doi: 10.1080/21678421.2017.1338298. [DOI] [PubMed] [Google Scholar]
- 129.Alaiad A, Alsharo M, Alnsour Y. The determinants of m-health adoption in developing countries: an empirical investigation. Appl Clin Inform. 2019 Oct 30;10(5):820–40. doi: 10.1055/s-0039-1697906. http://europepmc.org/abstract/MED/31667819 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.DiDonato KL, Liu Y, Lindsey CC, Hartwig DM, Stoner SC. Community pharmacy patient perceptions of a pharmacy-initiated mobile technology app to improve adherence. Int J Pharm Pract. 2015 Oct 09;23(5):309–19. doi: 10.1111/ijpp.12168. [DOI] [PubMed] [Google Scholar]
- 131.Helleman J, Kruitwagen ET, van den Berg LH, Visser-Meily JM, Beelen A. The current use of telehealth in ALS care and the barriers to and facilitators of implementation: a systematic review. Amyotroph Lateral Scler Frontotemporal Degener. 2020 May;21(3-4):167–82. doi: 10.1080/21678421.2019.1706581. [DOI] [PubMed] [Google Scholar]
- 132.Louissaint J, Lok AS, Fortune BE, Tapper EB. Acceptance and use of a smartphone application in cirrhosis. Liver Int. 2020 Jul;40(7):1556–63. doi: 10.1111/liv.14494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Zhang X, Guo X, Guo F, Lai K. Nonlinearities in personalization-privacy paradox in mHealth adoption: the mediating role of perceived usefulness and attitude. Technol Health Care. 2014 Aug 01;22(4):515–29. doi: 10.3233/thc-140811. [DOI] [PubMed] [Google Scholar]
- 134.Zolait A, Radhi N, Alhowaishi MM, Sundram VP, Aldoseri LM. Can Bahraini patients accept e-health systems? Int J Health Care Qual Assur. 2019 May 13;32(4):720–30. doi: 10.1108/ijhcqa-05-2018-0106. [DOI] [PubMed] [Google Scholar]
- 135.Nabi J, Cone EB, Vasavada A, Sun M, Kilbridge KL, Kibel AS, Berry DL, Trinh Q. Mobile health app for prostate cancer patients on androgen deprivation therapy: qualitative usability study. JMIR Mhealth Uhealth. 2020 Nov 03;8(11):e20224. doi: 10.2196/20224. https://mhealth.jmir.org/2020/11/e20224/ v8i11e20224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Li J, Varnfield M, Jayasena R, Celler B. Home telemonitoring for chronic disease management: perceptions of users and factors influencing adoption. Health Informatics J. 2021;27(1):1460458221997893. doi: 10.1177/1460458221997893. https://journals.sagepub.com/doi/10.1177/1460458221997893?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed . [DOI] [PubMed] [Google Scholar]
- 137.Lie SS, Karlsen B, Oord ER, Graue M, Oftedal B. Dropout from an eHealth intervention for adults with type 2 diabetes: a qualitative study. J Med Internet Res. 2017 May 30;19(5):e187. doi: 10.2196/jmir.7479. https://www.jmir.org/2017/5/e187/ v19i5e187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Ross EL, Jamison RN, Nicholls L, Perry BM, Nolen KD. Clinical integration of a smartphone app for patients with chronic pain: retrospective analysis of predictors of benefits and patient engagement between clinic visits. J Med Internet Res. 2020 Apr 16;22(4):e16939. doi: 10.2196/16939. https://www.jmir.org/2020/4/e16939/ v22i4e16939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Leenen LA, Wijnen BF, de Kinderen RJ, van Heugten CM, Evers SM, Majoie MH. Are people with epilepsy using eHealth-tools? Epilepsy Behav. 2016 Nov;64(Pt A):268–72. doi: 10.1016/j.yebeh.2016.08.007.S1525-5050(16)30351-1 [DOI] [PubMed] [Google Scholar]
- 140.Desveaux L, Shaw J, Saragosa M, Soobiah C, Marani H, Hensel J, Agarwal P, Onabajo N, Bhatia RS, Jeffs L. A mobile app to improve self-management of individuals with type 2 diabetes: qualitative realist evaluation. J Med Internet Res. 2018 Mar 16;20(3):e81. doi: 10.2196/jmir.8712. https://www.jmir.org/2018/3/e81/ v20i3e81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Edbrooke-Childs J, Edridge C, Averill P, Delane L, Hollis C, Craven MP, Martin K, Feltham A, Jeremy G, Deighton J, Wolpert M. A feasibility trial of power up: smartphone app to support patient activation and shared decision making for mental health in young people. JMIR Mhealth Uhealth. 2019 Jun 04;7(6):e11677. doi: 10.2196/11677. https://mhealth.jmir.org/2019/6/e11677/ v7i6e11677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Alam MM, Alam MZ, Rahman SA, Taghizadeh SK. Factors influencing mHealth adoption and its impact on mental well-being during COVID-19 pandemic: a SEM-ANN approach. J Biomed Inform. 2021 Apr;116:103722. doi: 10.1016/j.jbi.2021.103722. https://linkinghub.elsevier.com/retrieve/pii/S1532-0464(21)00051-4 .S1532-0464(21)00051-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Graffigna G, Barello S, Bonanomi A, Menichetti J. The motivating function of healthcare professional in eHealth and mHealth interventions for type 2 diabetes patients and the mediating role of patient engagement. J Diabetes Res. 2016;2016:2974521. doi: 10.1155/2016/2974521. doi: 10.1155/2016/2974521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Amann J, Fiordelli M, Scheel-Sailer A, Brach M, Rubinelli S. Opportunities and challenges of a self-management app to support people with spinal cord injury in the prevention of pressure injuries: qualitative study. JMIR Mhealth Uhealth. 2020 Dec 09;8(12):e22452. doi: 10.2196/22452. https://mhealth.jmir.org/2020/12/e22452/ v8i12e22452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Chang C, Lee T, Mills ME. Experience of home telehealth technology in older patients with diabetes. Comput Inform Nurs. 2017 Oct;35(10):530–7. doi: 10.1097/CIN.0000000000000341. [DOI] [PubMed] [Google Scholar]
- 146.Anastasiadou D, Folkvord F, Serrano-Troncoso E, Lupiañez-Villanueva F. Mobile health adoption in mental health: user experience of a mobile health app for patients with an eating disorder. JMIR Mhealth Uhealth. 2019 May 31;7(6):e12920. doi: 10.2196/12920. https://mhealth.jmir.org/2019/6/e12920/ v7i6e12920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Blonigen D, Harris-Olenak B, Kuhn E, Humphreys K, Timko C, Dulin P. From "Step away" to "Stand down": tailoring a smartphone app for self-management of hazardous drinking for veterans. JMIR Mhealth Uhealth. 2020 Feb 13;8(2):e16062. doi: 10.2196/16062. https://mhealth.jmir.org/2020/2/e16062/ v8i2e16062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Shaw RJ, Steinberg DM, Bonnet J, Modarai F, George A, Cunningham T, Mason M, Shahsahebi M, Grambow SC, Bennett GG, Bosworth HB. Mobile health devices: will patients actually use them? J Am Med Inform Assoc. 2016 May 17;23(3):462–6. doi: 10.1093/jamia/ocv186. http://europepmc.org/abstract/MED/26911820 .ocv186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Jaana M, Sherrard H, Paré G. A prospective evaluation of telemonitoring use by seniors with chronic heart failure: adoption, self-care, and empowerment. Health Informatics J. 2019 Dec;25(4):1800–14. doi: 10.1177/1460458218799458. https://journals.sagepub.com/doi/10.1177/1460458218799458?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed . [DOI] [PubMed] [Google Scholar]
- 150.Rho MJ, Kim H, Sun C, Wang G, Yoon K, Choi IY. Comparison of the acceptance of telemonitoring for glucose management between South Korea and China. Telemed J E Health. 2017 Nov;23(11):881–90. doi: 10.1089/tmj.2016.0217. [DOI] [PubMed] [Google Scholar]
- 151.Powell RE, Henstenburg JM, Cooper G, Hollander JE, Rising KL. Patient perceptions of telehealth primary care video visits. Ann Fam Med. 2017 May;15(3):225–9. doi: 10.1370/afm.2095. http://www.annfammed.org/cgi/pmidlookup?view=long&pmid=28483887 .15/3/225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Serafica R, Inouye J, Lukkahatai N, Braginsky N, Pacheco M, Daub K. The use of mobile health to assist self-management and access to services in a rural community. Comput Inform Nurs. 2019 Feb;37(2):62–72. doi: 10.1097/CIN.0000000000000494. [DOI] [PubMed] [Google Scholar]
- 153.Brew-Sam N, Chib A, Rossmann C. Differential influences of social support on app use for diabetes self-management - a mixed methods approach. BMC Med Inform Decis Mak. 2020 Jul 07;20(1):151. doi: 10.1186/s12911-020-01173-3. https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/s12911-020-01173-3 .10.1186/s12911-020-01173-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Connor K, Wambach K, Baird MB. Descriptive, qualitative study of women who use mobile health applications to obtain perinatal health information. J Obstet Gynecol Neonatal Nurs. 2018 Nov;47(6):728–37. doi: 10.1016/j.jogn.2018.04.138.S0884-2175(18)30232-6 [DOI] [PubMed] [Google Scholar]
- 155.Duclos V, Yé M, Moubassira K, Sanou H, Sawadogo NH, Bibeau G, Sié A. Situating mobile health: a qualitative study of mHealth expectations in the rural health district of Nouna, Burkina Faso. Health Res Policy Syst. 2017 Jul 12;15(Suppl 1):47. doi: 10.1186/s12961-017-0211-y. https://health-policy-systems.biomedcentral.com/articles/10.1186/s12961-017-0211-y .10.1186/s12961-017-0211-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Guo X, Chen S, Zhang X, Ju X, Wang X. Exploring patients' intentions for continuous usage of mHealth services: elaboration-likelihood perspective study. JMIR Mhealth Uhealth. 2020 Apr 06;8(4):e17258. doi: 10.2196/17258. https://mhealth.jmir.org/2020/4/e17258/ v8i4e17258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Schulte M, Liang D, Wu F, Lan Y, Tsay W, Du J, Zhao M, Li X, Hser Y- A smartphone application supporting recovery from heroin addiction: perspectives of patients and providers in China, Taiwan, and the USA. J Neuroimmune Pharmacol. 2016 Sep 4;11(3):511–22. doi: 10.1007/s11481-016-9653-1. http://europepmc.org/abstract/MED/26846506 .10.1007/s11481-016-9653-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Aisyah DN, Ahmad RA, Artama WT, Adisasmito W, Diva H, Hayward AC, Kozlakidis Z. Knowledge, attitudes, and behaviors on utilizing mobile health technology for TB in Indonesia: a qualitative pilot study. Front Public Health. 2020;8:531514. doi: 10.3389/fpubh.2020.531514. doi: 10.3389/fpubh.2020.531514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Hinami K, Harris BA, Uriostegui R, Jasmin W, Lopez M, Trick WE. Patient-level exclusions from mHealth in a safety-net health system. J Hosp Med. 2017 Feb 01;12(2):90–3. doi: 10.12788/jhm.2686. [DOI] [PubMed] [Google Scholar]
- 160.Kumar AA, De Costa A, Das A, Srinivasa G, D'Souza G, Rodrigues R. Mobile health for tuberculosis management in South India: is video-based directly observed treatment an acceptable alternative? JMIR Mhealth Uhealth. 2019 Apr 03;7(4):e11687. doi: 10.2196/11687. https://mhealth.jmir.org/2019/4/e11687/ v7i4e11687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Salgado T, Tavares J, Oliveira T. Drivers of mobile health acceptance and use from the patient perspective: survey study and quantitative model development. JMIR Mhealth Uhealth. 2020 Jul 09;8(7):e17588. doi: 10.2196/17588. https://mhealth.jmir.org/2020/7/e17588/ v8i7e17588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Zini EM, Lanzola G, Quaglini S, Bossi P, Licitra L, Resteghini C. A pilot study of a smartphone-based monitoring intervention on head and neck cancer patients undergoing concurrent chemo-radiotherapy. Int J Med Inform. 2019 Sep;129:404–12. doi: 10.1016/j.ijmedinf.2019.06.004.S1386-5056(18)30622-1 [DOI] [PubMed] [Google Scholar]
- 163.Su Y, Huang S, Wu Y, Chen C. Factors affecting patients' acceptance of and satisfaction with cloud-based telehealth for chronic disease management: a case study in the workplace. Appl Clin Inform. 2020 Mar 15;11(2):286–94. doi: 10.1055/s-0040-1708838. http://europepmc.org/abstract/MED/32294772 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Bauer AM, Iles-Shih M, Ghomi RH, Rue T, Grover T, Kincler N, Miller M, Katon WJ. Acceptability of mHealth augmentation of collaborative care: a mixed methods pilot study. Gen Hosp Psychiatry. 2018;51:22–9. doi: 10.1016/j.genhosppsych.2017.11.010. http://europepmc.org/abstract/MED/29272712 .S0163-8343(17)30287-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Čuš A, Edbrooke-Childs J, Ohmann S, Plener PL, Akkaya-Kalayci T. "Smartphone Apps Are Cool, But Do They Help Me?": a qualitative interview study of adolescents' perspectives on using smartphone interventions to manage nonsuicidal self-injury. Int J Environ Res Public Health. 2021 Mar 22;18(6):3289. doi: 10.3390/ijerph18063289. https://www.mdpi.com/resolver?pii=ijerph18063289 .ijerph18063289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Jain N, Singh H, Koolwal GD, Kumar S, Gupta A. Opportunities and barriers in service delivery through mobile phones (mHealth) for Severe Mental Illnesses in Rajasthan, India: a multi-site study. Asian J Psychiatr. 2015 Apr;14:31–5. doi: 10.1016/j.ajp.2015.01.008.S1876-2018(15)00009-X [DOI] [PubMed] [Google Scholar]
- 167.Koivumäki T, Pekkarinen S, Lappi M, Väisänen J, Juntunen J, Pikkarainen M. Consumer adoption of future MyData-based preventive eHealth services: an acceptance model and survey study. J Med Internet Res. 2017 Dec 22;19(12):e429. doi: 10.2196/jmir.7821. https://www.jmir.org/2017/12/e429/ v19i12e429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Caplan S, Sosa Lovera A, Veloz Comas E, Attilus J. A mobile app to prevent depression among low-income primary care patients in the Dominican Republic: sociocultural adaptations. J Transcult Nurs. 2020 Jul 19;31(4):413–24. doi: 10.1177/1043659620912315. [DOI] [PubMed] [Google Scholar]
- 169.Muigg D, Duftschmid G, Kastner P, Modre-Osprian R, Haluza D. Telemonitoring readiness among Austrian diabetic patients: a cross-sectional validation study. Health Informatics J. 2020 Dec;26(4):2332–43. doi: 10.1177/1460458219894094. https://journals.sagepub.com/doi/10.1177/1460458219894094?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed . [DOI] [PubMed] [Google Scholar]
- 170.Muigg D, Kastner P, Modre-Osprian R, Haluza D, Duftschmid G. Is Austria ready for telemonitoring? A readiness assessment among doctors and patients in the field of diabetes. Stud Health Technol Inform. 2018;248:322–9. [PubMed] [Google Scholar]
- 171.Helleman J, Van Eenennaam R, Kruitwagen ET, Kruithof WJ, Slappendel MJ, Van Den Berg LH, Visser-Meily JM, Beelen A. Telehealth as part of specialized ALS care: feasibility and user experiences with "ALS home-monitoring and coaching". Amyotroph Lateral Scler Frontotemporal Degener. 2020 May;21(3-4):183–92. doi: 10.1080/21678421.2020.1718712. [DOI] [PubMed] [Google Scholar]
- 172.Müller SD, Wehner D, Konzag H, Vesterby M, Høybye MT. The paradox of project success despite lack of the "My Pathway" telehealth platform usage. Health Informatics J. 2021;27(1):1460458220976734. doi: 10.1177/1460458220976734. https://journals.sagepub.com/doi/10.1177/1460458220976734?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed . [DOI] [PubMed] [Google Scholar]
- 173.Chang LW, Njie-Carr V, Kalenge S, Kelly JF, Bollinger RC, Alamo-Talisuna S. Perceptions and acceptability of mHealth interventions for improving patient care at a community-based HIV/AIDS clinic in Uganda: a mixed methods study. AIDS Care. 2013 May 08;25(7):874–80. doi: 10.1080/09540121.2013.774315. http://europepmc.org/abstract/MED/23452084 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.van Heerden A, Harris DM, van Rooyen H, Barnabas RV, Ramanathan N, Ngcobo N, Mpiyakhe Z, Comulada WS. Perceived mHealth barriers and benefits for home-based HIV testing and counseling and other care: qualitative findings from health officials, community health workers, and persons living with HIV in South Africa. Soc Sci Med. 2017 Jun;183:97–105. doi: 10.1016/j.socscimed.2017.04.046. http://europepmc.org/abstract/MED/28475904 .S0277-9536(17)30276-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Fairbrother P, Ure J, Hanley J, McCloughan L, Denvir M, Sheikh A, McKinstry B, Telescot programme team Telemonitoring for chronic heart failure: the views of patients and healthcare professionals - a qualitative study. J Clin Nurs. 2014 Jan;23(1-2):132–44. doi: 10.1111/jocn.12137. [DOI] [PubMed] [Google Scholar]
- 176.Schnall R, Higgins T, Brown W, Carballo-Dieguez A, Bakken S. Trust, perceived risk, perceived ease of use and perceived usefulness as factors related to mHealth technology use. Stud Health Technol Inform. 2015;216:467–71. http://europepmc.org/abstract/MED/26262094 . [PMC free article] [PubMed] [Google Scholar]
- 177.Siebenhüner AR, Mikolasek M, Witt C, Barth J. Improvements in health might contradict adherence to mobile health interventions: findings from a self-care cancer app study. J Altern Complement Med. 2021 Mar;27(S1):S115–23. doi: 10.1089/acm.2020.0111. [DOI] [PubMed] [Google Scholar]
- 178.Murphy J, Uttamlal T, Schmidtke KA, Vlaev I, Taylor D, Ahmad M, Alsters S, Purkayastha P, Scholtz S, Ramezani R, Ahmed AR, Chahal H, Darzi A, Blakemore AI. Tracking physical activity using smart phone apps: assessing the ability of a current app and systematically collecting patient recommendations for future development. BMC Med Inform Decis Mak. 2020 Feb 03;20(1):17. doi: 10.1186/s12911-020-1025-3. https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/s12911-020-1025-3 .10.1186/s12911-020-1025-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Zhou M, Zhao L, Kong N, Campy KS, Qu S, Wang S. Factors influencing behavior intentions to telehealth by Chinese elderly: an extended TAM model. Int J Med Inform. 2019 Jun;126:118–27. doi: 10.1016/j.ijmedinf.2019.04.001.S1386-5056(18)30319-8 [DOI] [PubMed] [Google Scholar]
- 180.Bennett BL, Goldstein CM, Gathright EC, Hughes JW, Latner JD. Internal health locus of control predicts willingness to track health behaviors online and with smartphone applications. Psychol Health Med. 2017 Dec 17;22(10):1224–9. doi: 10.1080/13548506.2017.1317354. http://europepmc.org/abstract/MED/28415852 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Sezgin E, Weiler M, Weiler A, Lin S. Proposing an ecosystem of digital health solutions for teens with chronic conditions transitioning to self-management and independence: exploratory qualitative study. J Med Internet Res. 2018 Sep 06;20(9):e10285. doi: 10.2196/10285. https://www.jmir.org/2018/9/e10285/ v20i9e10285 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Critical Appraisal Skills Program checklist.
Critical appraisal of the included studies.
Phases of thematic analysis based on Braun and Clarke [25].
Characteristics of included studies.
(A) Social and personal factors and their occurrence. (B) Technical and material factors and their occurrence. (C) Health-related factors and their occurrence.


