Abstract
Background
Non-union in non-operatively managed humeral shaft fractures are associated with significant morbidity. Hence, developing a robust system that could help with early diagnosis is important. We aimed to evaluate the validity of the Radiographic Union Score for HUmeral fractures (RUSHU) at 6 weeks (RUSHU-6) and test whether a RUSHU at 12 weeks (RUSHU-12) would be a better predictor of non-union.
Methods
We retrospectively reviewed all non-operatively managed humeral diaphyseal fractures from 2012 to 2018. Statistical analysis was used to determine the cut-off RUSHU-12 and evaluate the effect of RUSHU-6 and RUSHU-12 on non-union prediction.
Results
In sum, 32 patients had radiographs at 6 weeks post-injury, 27 of which also had radiographs at 12 weeks. A RUSHU cut-off of 9 was the best predictor of non-union at 12 weeks. Only RUSHU-12 had a statistically significant influence predicting non-union (P = 0.011) and there was a significant correlation (P = 0.003) between score progression from RUSHU-6 to RUSHU-12 and the development of non-union.
Discussion
A RUSHU-12 of <9 and a low score progression between 6 and 12 weeks suggest superior predictive value in determining the likelihood of non-union. Further validation in the form of a large multicentred study is however required.
Keywords: Humerus, diaphysis, non-union, non-operative, RUSHU
Introduction
Fractures of the humeral shaft represent 1–3% of all fractures worldwide1–3 with an annual incidence of 13 per 100,000 per year reported in the United Kingdom. 4 The majority are treated successfully without operative intervention, often using a humeral brace.5,6 Nevertheless, a non-union can have a significant effect on a patient’s quality of life with the ensuing functional loss and pain leading to a loss of independence, especially in the elderly. 7 In addition to the increased morbidity, humeral shaft non-union patients have a lower probability of returning to full function even after subsequent union following delayed fixation. 8 With non-union rates as high as 39% reported in the literature, 9 there is an imperative to develop a robust system that can reliably predict humeral shaft non-unions at an earlier stage and thus guide intervention.
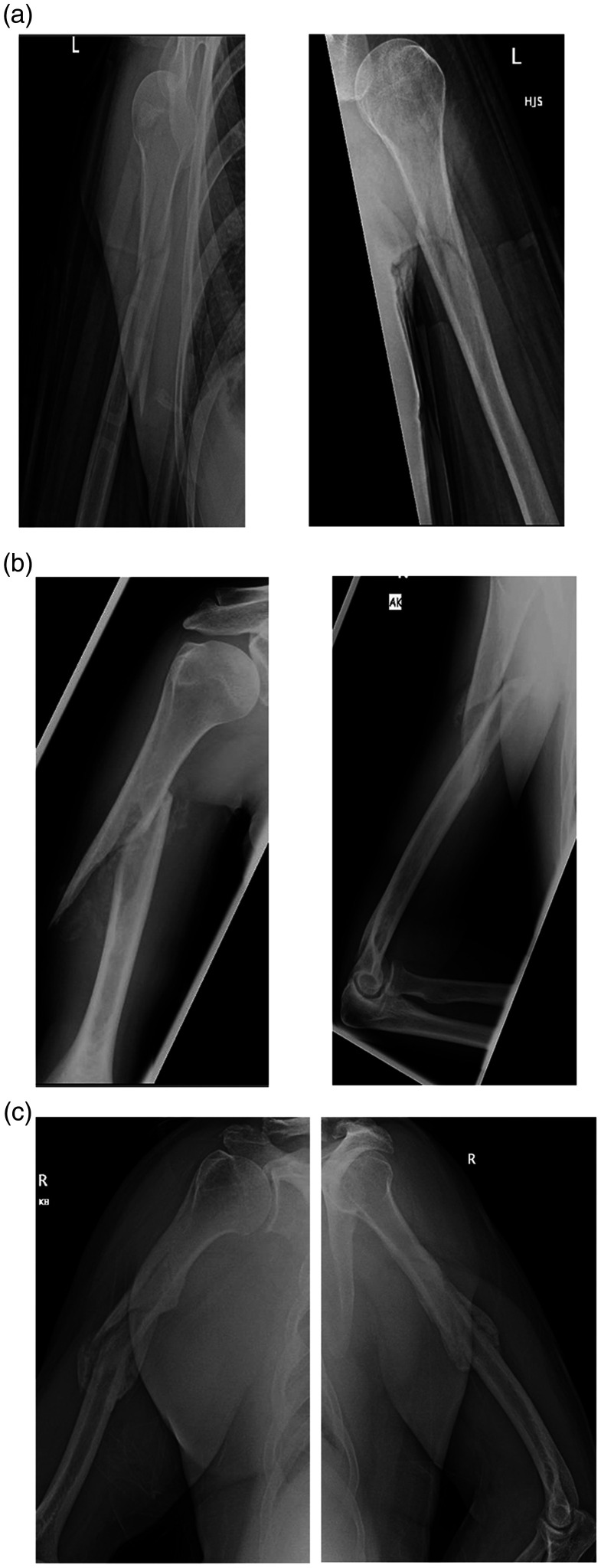
The Radiographic Union Score for HUmeral fractures (RUSHU) is an objective measurement to assess humeral diaphyseal fracture healing. 10 Based on the Radiographic Union Scale for Tibial fractures (RUST) score, 11 the recently published RUSHU 10 gives a score of 1–3 based on the presence or absence of callus on the four cortices seen on anteroposterior (AP) and lateral radiographic views (Table 1 and Figure 1). A RUSHU of <8 at six weeks was deemed to be predictive of non-union. To our knowledge, this score has not been validated by another unit to confirm its reliability. Given the false-positive rate of 20%, we tested the hypothesis that a 12-week RUSHU would be a better predictor of non-union and reduce the number of patients exposed to unnecessary surgery.
Table 1.
Scoring table for Radiographic Union Score for HUmeral fractures (RUSHU).
| Presence of callus (score per cortex) |
||||
|---|---|---|---|---|
| Radiographic view | Cortex | Absent (1) | Present, nonbridging (2) | Present, bridging (3) |
| Anteroposterior | Medial | |||
| Lateral | ||||
| Lateral | Anterior | |||
| Posterior | ||||
Figure 1.
Examples of different Radiographic Union Scores for HUmeral fractures (RUSHU). (a) RUSHU 4 (b) RUSHU 8 (c) RUSHU 12.
Materials and methods
After receiving local clinical governance approval, we used Accident and Emergency (A&E) coding data from our institution to retrospectively review all humeral fractures from 2012 to 2018. Inclusion criteria consisted of minimum age of 18 at time of injury, a humeral shaft fracture (humeral shaft defined as area distal to surgical neck and proximal to epicondyles 12 ), a minimum follow-up of six weeks and with adequate plain anteroposterior and lateral whole-humerus radiographs. Lateral humeral shaft views are taken with the patient standing and with the elbow flexed to 90 degrees at our institution. Exclusion criteria included operative fixation within six months of injury, pathological or periprosthetic fractures and proximal or distal humerus fractures. Appropriate radiographs were identified by clinicians EG (final year orthopaedic registrar) and FM (first-year orthopaedic registrar) on the Picture Archiving and Communications System (PACS). Radiographs were then scored sequentially by several clinicians, BG (first-year orthopaedic registrar), KG (final year orthopaedic registrar) and PD (fellowship trained orthopaedic consultant), who were blinded to the final outcome. Each radiograph was scored twice at different times and interobserver/intraobserver reliability was calculated. We determined a RUSHU score at 6 weeks (RUSHU-6) and 12 weeks (RUSHU-12) using the methodology described by Oliver et al. 10 The medial and lateral cortex was scored on the AP radiographs and the anterior/posterior cortices were scored on the lateral radiographs. Our radiographs are taken at 6 and 12 weeks for humeral shaft fractures as routine in our institution. Any discrepancy in the determination of RUSHU between the blinded clinicians was discussed with senior author (PD) before a final score was agreed on.
Non-union was defined after a period of six months as a lack of clinical or radiographic union at the fracture site. Non-operative treatment of humeral shaft fractures at our centre consists of applying a U-slab at initial presentation to A&E followed by conversion to a humeral brace at the first clinical follow-up (usually 5–7 days after the injury), although the exact mode and length of immobilisation was at the discretion of the treating clinician. Patient demographic data including relevant comorbidities and smoking status, injury characteristics (location and pattern of fracture), time to union and complications were noted from the medical records and PACS.
Statistical analysis
Statistical analysis was performed using R version 4.0.0 (R Foundation for Statistical Computing, Vienna, Austria). A receiver operating characteristic (ROC) curve was used to help determine the cut-off RUSHU-12 score for predicting non-union. We then used a logistic regression model to compare the effect of the RUSHU-6 and RUSHU-12 cut-off scores on the likelihood of predicting non-union. Logistic regression was also used to determine whether progression of the scores between 6 and 12 weeks had a significant effect on eventual union. Interobserver/intraobserver reliability was calculated using a two-way mixed model single measure intraclass correlation coefficient (ICC) with 95% CI. ICC score ranges from 0 to 1 with 1 indicating perfect agreement and 0 indicating no agreement.
Results
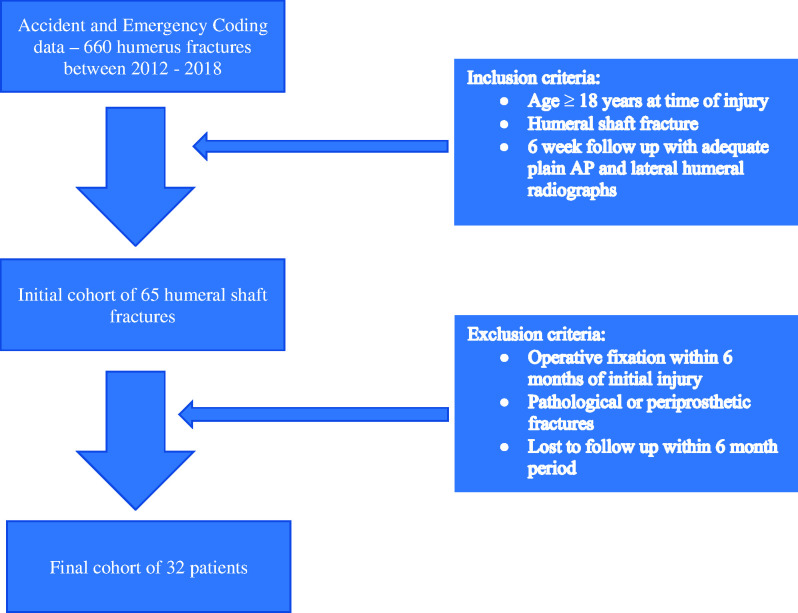
Our database revealed 660 humerus fractures, and after applying our inclusion and exclusion criteria, we had 32 eligible patients with a 6-week follow-up radiograph of which 27 also had radiographs at 12-week follow-up (Figure 2); 48% of the fractures were sustained on the dominant arm. The mean age was 59 years (range 19-92, SD 19, 95% CI 53–66) with a female to male ratio of 3:1.
Figure 2.
Flow chart depicting the use of inclusion and exclusion criteria on selecting final patient cohort.
The overall non-union rate was 28% (n = 9). The average time to union for the union group was 15 weeks (range 8–24, SD 6, 95% CI 12–17). The average time to eventual union for the non-union group was 79 weeks (range 52–108, SD 28, 95% CI 9–148). The overall (union and non-union) mean RUSHU score at 6 weeks was 7.8 (range 4–12, SD 3, 95% CI 7–9) and at 12 weeks was 9.1 (range 5–12, SD 2, 95% CI 8–10). Patient and fracture characteristics of union versus non-union groups are shown in Table 2 and the intraobserver/interobserver ICC in Table 3.
Table 2.
Patient and fracture characteristics for final cohort.
| Demographic | Union (n = 23) | Non-union (n = 9) |
|---|---|---|
| Age (years) | 56 (19–92) | 68 (52–82) |
| Gender (n) | ||
| Female | 15 | 6 |
| Male | 7 | 0 |
| Fracture location | ||
| Proximal % | 52% (12) | 55% (5) |
| Middle % | 39% (9) | 44% (4) |
| Distal % | 9% (2) | 0% |
| Fracture configuration | ||
| Transverse % | 13% (3) | 11 % (1) |
| Spiral % | 74% (17) | 77% (7) |
| Oblique % | 13% (3) | 11% (1) |
| Fracture comminution | ||
| Yes | 52% (12) | 67% (6) |
| No | 48% (11) | 33 % (3) |
Table 3.
Reliability of Radiographic Union Scores of HUmeral (RUSHU) fractures at 6 weeks and 12 weeks.
| 6 Weeks | 12 Weeks | |
|---|---|---|
| Interobserver ICC (95% CI) | 0.808 (95% CI 0.687–0.894) | 0.880 (95% CI 0.794–0.937) |
| Intraobserver ICC (95% CI) | 0.69 (95% CI 0.454–0.836) | 0.838 (95% CI 0.687–0.919) |
ICC: Intraclass correlation coefficient; CI: confidence interval.
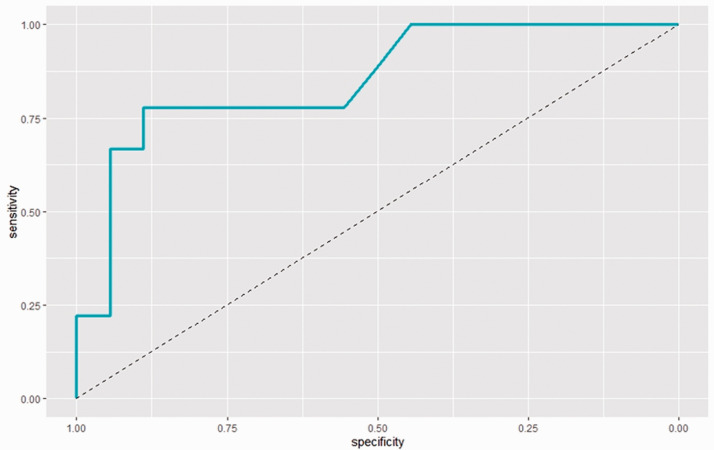
We plotted ROC curves for each reported RUSHU-12 value in the dataset (score range 5–12) and calculated the area under the curve (AUC) for each. Based on this, we found that a cut-off of 9 (AUC 0.85, specificity 0.89, sensitivity 0.78) was the best predictor for non-union (Table 4 and Figure 3) with a positive predictive value (PPV) of 64% and a negative predictive value (NPV) of 88%. In addition, 18 patients in RUSHU-12 group went on to union; 4 of these had a RUSHU-12 score of <9, giving a false-positive rate of 22%.
Table 4.
Area under the curve for the different Radiographic Union Scores for Humeral fractures (RUSHU) cut-offs at 12-week follow-up.
| RUSHU cut-off | Area under the curve | Specificity | Sensitivity |
|---|---|---|---|
| 5 | 0.75 | 0.83 | 0.33 |
| 6 | 0.76 | 0.83 | 0.44 |
| 7 | 0.81 | 0.89 | 0.44 |
| 8 | 0.84 | 0.89 | 0.56 |
| 9 | 0.85 | 0.89 | 0.78 |
| 10 | 0.81 | 0.83 | 0.78 |
| 11 | 0.79 | 0.89 | 0.44 |
| 12 | 0.78 | 0.89 | 0.44 |
Figure 3.
Receiver operating characteristic (ROC) curve for the Radiographic Union Score for HUmeral fracture (RUSHU) cut-off score of 9.
In the RUSHU-6 group, 23 patients went on to union; 9 of these patients had a RUSHU-6 score of <8 giving a false-positive rate of 39%. This cut-off score of 8 at 6 weeks had a PPV of 44% and a NPV of 88%.
Using a logistic regression model, the effect of age had an effect on the probability of developing a non-union but did not reach statistical significance (p = 0.087). Using the previously quoted RUSHU-6 cut-off score of <810 did not have a significant effect on observing a non-union (p = 0.062). A RUSHU-12 score of <9 did have a significant effect of observing an eventual non-union (p = 0.011).
A RUSHU score of <9 at 12 weeks was more likely to develop a non-union (Odds ratio 1.43) than a RUSHU score of <8 at 6 weeks. Patients with a RUSHU-12 score of <9 were five times more likely to develop a non-union than those with a score of ≥ 9 at 12 weeks (Odds ratio 5.12).
The logistic regression model found a significant effect on change in score between RUSHU-6 and RUSHU-12 (p = 0.003) and the development of non-union, but it was also dependent on the starting RUSHU-6 score (Table 5). For instance, a RUSHU-6 score of 4 and an interval progression score of 0 had a 92% chance of progressing to non-union but a RUSHU-6 score of 10 and an interval progression score of 0 only had a 36% chance of progression to non-union.
Table 5.
Probabilities of non-union at different values of RUSHU-6 and change in score between 6 and 12 weeks (RUSHU progression).
| Rushu6 score | RUSHU progression | Probability | SD | Lower CI | Upper CI |
|---|---|---|---|---|---|
| Rushu6 = 4 | 0 | 0.922 | 0.0947 | 0.4722 | 0.9936 |
| 1 | 0.8027 | 0.1616 | 0.3551 | 0.9678 | |
| 2 | 0.5834 | 0.2217 | 0.1899 | 0.8933 | |
| 3 | 0.3252 | 0.2309 | 0.0578 | 0.7912 | |
| 4 | 0.1423 | 0.1667 | 0.0113 | 0.7071 | |
| 5 | 0.054 | 0.0901 | 0.0018 | 0.6441 | |
| Rushu6 = 6 | 0 | 0.8112 | 0.1457 | 0.3996 | 0.9652 |
| 1 | 0.5965 | 0.1559 | 0.2934 | 0.8403 | |
| 2 | 0.3372 | 0.1445 | 0.1253 | 0.6438 | |
| 3 | 0.149 | 0.1204 | 0.0265 | 0.5295 | |
| 4 | 0.0568 | 0.0733 | 0.0041 | 0.4676 | |
| 5 | 0.0203 | 0.0363 | 0.0006 | 0.4245 | |
| Rushu6 = 8 | 0 | 0.6095 | 0.177 | 0.2665 | 0.8702 |
| 1 | 0.3494 | 0.1193 | 0.1611 | 0.6003 | |
| 2 | 0.156 | 0.0914 | 0.0453 | 0.4188 | |
| 3 | 0.0598 | 0.0609 | 0.0076 | 0.3469 | |
| 4 | 0.0214 | 0.0321 | 0.0011 | 0.3061 | |
| 5 | 0.0075 | 0.0149 | 0.0001 | 0.2759 | |
| Rushu6 = 10 | 0 | 0.3618 | 0.1901 | 0.1014 | 0.7401 |
| 1 | 0.1633 | 0.1065 | 0.0406 | 0.4736 | |
| 2 | 0.0629 | 0.0596 | 0.0092 | 0.3276 | |
| 3 | 0.0226 | 0.0306 | 0.0015 | 0.2591 | |
| 4 | 0.0079 | 0.0142 | 0.0002 | 0.219 | |
| 5 | 0.0027 | 0.0062 | 0 | 0.191 | |
| Rushu6 = 12 | 0 | 0.1708 | 0.1602 | 0.0219 | 0.6542 |
| 1 | 0.0662 | 0.0736 | 0.0068 | 0.4225 | |
| 2 | 0.0238 | 0.0332 | 0.0015 | 0.2863 | |
| 3 | 0.0083 | 0.0146 | 0.0003 | 0.2137 | |
| 4 | 0.0029 | 0.0063 | 0 | 0.1707 | |
| 5 | 0.001 | 0.0026 | 0 | 0.1422 |
CI: confidence intervals, set at 0.95; SD: standard deviation.
The average increase in RUSHU from 6 to 12 weeks was 1.7. For fractures that went on to union the average increase in score was 2.17 compared to 0.78 for non-union; 100% of fractures that had an increase in RUSHU of 3 or more went on to unite while 78% of the non-union patients had a change in score of 1 or less. Figure 4 depicts the change in RUSHU from 6 to 12 weeks comparing union to non-union.
Figure 4.
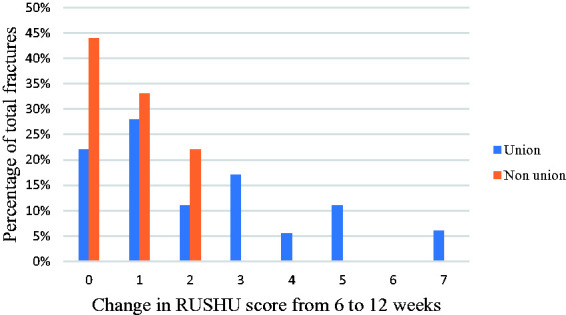
Interval change between 6- and 12-week Radiographic Union Scores for HUmeral Fractures (RUSHU) scores for union and non-union.
Discussion
We found the RUSHU to be a good predictor of eventual non-union with excellent interobserver and intraobserver reliability. Scores of 0.88 and 0.83, respectively, at 12 weeks indicated substantial agreement and were similar to the scores published in the study of Oliver et al. 10 As hypothesised, using a RUSHU at 12 weeks rather than at 6 weeks proved to be a significantly better predictor of non-union. In the original RUSHU study, the authors alluded to a reduced diagnostic certainty when predicting non-union at a six-week mark; our study has addressed this through an improved and more predictable RUSHU. Exposing someone to the risks of humeral shaft fracture surgery, which include a 6.5–12% risk of radial nerve palsy, 13 unnecessarily is difficult to justify and something one would want to avoid. Similarly identifying those patients who will progress to non-union at an early stage can prevent the significant morbidity and cost associated with established non-union and its management. 14 We have shown that the 12-week mark is a better time point to make a decision about operative fixation of these fracture types, with a lower risk of exposing someone to an unnecessary operation whilst at an early enough timeframe to operate before the fracture develops into an established non-union. The accepted timeline before one can diagnose a humeral shaft non-union is six months; 9 yet, the majority of humeral shaft fractures should unite between 12 and 16 weeks. 9 We believe therefore that 12 weeks is an appropriate timeline to decide on whether a humeral shaft fracture will go on to non-union or not. By using RUSHU-12 to help guide that decision at 12 weeks, one can stop the patient suffer from the increasing loss of function and independence that further months of brace immobilisation will bring.8,9 The functional loss and osteopaenia associated with prolonged brace immobilisation is also likely to contribute to poorer outcomes post non-union humerus fracture surgery. 8
Our demographic data was in line with previously published epidemiological studies on humeral shaft fractures.1,3 A higher proportion of our patients were female, and the majority had fractures within the proximal to middle third of the humeral shaft. The non-union group had a higher average age of 68 compared to 56 in the union group, which in our statistical model did not reach significance (P = 0.087). Our average time to union was 14 weeks, similar to the study by Harkin and Large 15 and our non-union rate of 28% was in the mid-range between studies such as Sarmiento et al. 6 which quoted a 2% non-union rate and Foulk and Szabo 9 with a 39% non-union rate.
Other radiological scoring systems such as the radiographic union score for tibial (RUST) fractures 11 and radial union scoring system (RUSS) 16 have been previously shown to be successful in predicting union and non-union. 17 In a study of 323 patients, Ross et al. 18 found a statistically significant association between RUST scores and non-union in tibial fractures with 69% of patients with RUST score < 6 developing non-union. In our study, 64% of patients with a RUSHU score of <9 at 12 weeks proceeded to develop non-union and they were five times more likely to develop non-union than those with a RUSHU score of ≥ 9.
In our study, the RUSHU cut-off score of 8 at six weeks, as previously recommended by Oliver et al, 10 had a high false-positive rate of 39% with a PPV of 44%. Using ROC curves and logistic regression modelling for 12-week RUSHU scores, the data suggests that a cut-off score of 9 would be optimal, although our dataset was not large enough to confirm this. This cut-off score is in keeping with the Radiographic Humerus Union Measurement (RHUM), a slight variation on the RUSHU scoring system albeit using the same principles, which found that all patients with a score of 9 or above at 12 weeks went on to unite. 19 The main difference between RHUM and RUSHU was that the RHUM score also included data on whether a fracture line is visible and as well as the presence/absence of callus whereas RUSHU purely focused on callus. The original RUSHU study 10 also went into more detail on what they defined as bridging callus and based on this and ease of use we decided to opt for RUSHU in this study.
The cut-off score of 9 at 12 weeks gave a much-improved false-positive rate of 22% with a higher PPV of 64% and was an independent predictor of non-union in our logistic regression model.
The overall trend for false positives in our study was higher compared to the Oliver et al.’s paper, 10 which quoted a 20% false-positive rate for a RUSHU of <8 at six weeks compared to 39% in our study. Nevertheless, our false-positive rate of 22% for RUSHU-12 of <9 remained high. We therefore investigated whether an interval change in score between RUSHU-6 and RUSHU-12 could help with our prediction. Our logistic regression model showed there was a statistically significant effect of low RUSHU progression on the development of non-union. The model also highlighted the importance of taking into consideration the starting RUSHU-6 scores, with higher scores less likely to progress to non-union regardless of the interval progression (Table 4). The presence of bridging callus indicates that there is a suitable mechanical and biological environment for the fracture to unite and although it is less likely to be apparent at six weeks in the rare occasions where the fracture has a high RUSHU-6 score, such as 10 or above, a repeat RUSHU-12 score may be less necessary; 78% of the non-union group had a RUSHU interval score of 1 or less whereas 100% of the fractures with an interval score of 3 or more went on to union. Therefore, we suggest that a RUSHU-12 of less than 9 and an interval progression score of 1 or less indicate that the fracture is likely to progress to non-union. We recommend calculating a RUSHU-6 in conjunction with RUSHU-12 at follow-up to guide final management.
The strength of our study was the strict adherence to our inclusion and exclusion criteria as well as the fact we had several blinded reviewers assessing RUSHU to reduce intraobserver and interobserver variability. Radiographs are widely available and RUSHU does not require any advanced imaging such as CT/MRI or imaging which is very operator dependent such as ultrasound. This makes it more accessible worldwide especially in low-income settings. Our study was limited by its retrospective nature and size of dataset. Due to our robust inclusion and exclusion criteria, the variation in timing and frequency of follow-up radiographs affected the total number of patients we could include in our final cohort. Making a verdict about whether a fracture is going to proceed to non-union is multifactorial and our study was purely radiological in nature. Other factors such as clinical assessment is essential to augment decision-making and, in particular, mobility at the fracture site at six weeks, as shown by Driesman et al., 20 which helps predict non-union can be integrated into future studies.
A prospective study with larger patient numbers, pre-determined follow-up and radiograph timings as well as specific clinical findings such as fracture site mobility would enhance our understanding of the fractures which progress to non-union. Other imaging modalities, such as ultrasound or CT scanning, have yet to be formally investigated as an early predictor of humeral shaft non-union and these could also be explored in the future.
Conclusion
This study indicates promise for the use of RUSHU-12 in predicting non-union. The use of RUSHU at 12 weeks, a score of <9 and a low interval score between 6 and 12 weeks suggest superior predictive value in determining the likelihood of non-union in humeral diaphyseal fractures. A larger multicentred study is however required to fully validate the scoring system and our recommendations.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Contributorship: BG wrote the first draft of the manuscript. All authors reviewed and edited the manuscript and approved the final version of the manuscript.
Ethical Review and Patient Consent
Written informed consent was obtained from the patients for their anonymised information to be published in this article. The Royal Free Foundation NHS Trust does not require ethical approval for individual case series.
ORCID iDs
Borna Guevel https://orcid.org/0000-0002-7750-3197
Frederik Sorensen https://orcid.org/0000-0003-4223-7463
References
- 1.Ekholm R, Adami J, Tidermark J, et al. Fractures of the shaft of the humerus. An epidemiological study of 401 fractures. J Bone Joint Surg Br 2006; 88: 1469–1473. [DOI] [PubMed] [Google Scholar]
- 2.Tsai C-H, Fong Y-C, Chen Y-H, et al. The epidemiology of traumatic humeral shaft fractures in Taiwan. Int Orthop 2009; 33: 463–467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tytherleigh-Strong G, Walls N, McQueen MM. The epidemiology of humeral shaft fractures. J Bone Joint Surg Br 1998; 80: 249–253. [DOI] [PubMed] [Google Scholar]
- 4.Court-Brown CM, Caesar B. Epidemiology of adult fractures: a review. Injury 2006; 37: 691–697. [DOI] [PubMed] [Google Scholar]
- 5.Koch PP, Gross DFL, Gerber C. The results of functional (Sarmiento) bracing of humeral shaft fractures. J Shoulder Elbow Surg 2002; 11: 143–150. [DOI] [PubMed] [Google Scholar]
- 6.Sarmiento A, Zagorski JB, Zych GA, et al. Functional bracing for the treatment of fractures of the humeral diaphysis. J Bone Joint Surg Am 2000; 82: 478–486. [DOI] [PubMed] [Google Scholar]
- 7.Pugh DMW, Mckee MD. Advances in the management of humeral non-union. J Am Acad Orthop Surg 2003; 11: 48–59. [DOI] [PubMed] [Google Scholar]
- 8.Ekholm R, Tidermark J, Tornkvist H, et al. Outcome after closed functional treatment of humeral shaft fractures. J Orthop Trauma 2006; 20: 591–596. [DOI] [PubMed] [Google Scholar]
- 9.Foulk DA, Szabo RM. Diaphyseal humerus fractures: natural history and occurrence of nonunion. Orthopedics 1995; 18: 33–35. [DOI] [PubMed] [Google Scholar]
- 10.Oliver WM, Smith TJ, Nicholson JA, et al. The radiographic union score for humeral fractures (RUSHU) predicts humeral shaft nonunion. Bone Joint J 2019; 101: 1300–1306. [DOI] [PubMed] [Google Scholar]
- 11.Whelan DB, Bhandari M, Stephen D, et al. Development of the radiographic union score for tibial fractures for the assessment of tibial fracture healing after intramedullary fixation. J Trauma 2010; 68: 629–632. [DOI] [PubMed] [Google Scholar]
- 12.Klenerman L. Fractures of the shaft of the humerus. J Bone Joint Surg Br 1966; 48: 105–111. [PubMed] [Google Scholar]
- 13.Pidhorz L. Acute and chronic humeral shaft fractures in adults. Orthop Traumatol Surg Res 2015; 101: S41–S49. [DOI] [PubMed] [Google Scholar]
- 14.Hak DJ, Fitzpatrick D, Bishop J, et al. Delayed union and nonunions: epidemiology, clinical issues, and financial aspects. Injury 2014; 45: S3–S7. [DOI] [PubMed] [Google Scholar]
- 15.Harkin FE, Large RJ. Humeral shaft fractures: union outcomes in a large cohort. J Shoulder Elbow Surg 2017; 26: 1881–1888. [DOI] [PubMed] [Google Scholar]
- 16.Patel SP, Anthony SG, Zurakowski D, et al. Radiographic scoring system to evaluation union of distal radius fractures. J Hand Surg Am 2014; 39: 1471–1479. [DOI] [PubMed] [Google Scholar]
- 17.Van Houten AH, Heesterbeek PJC, Van Heerwaarden RJV, et al. Medial open wedge high tibial osteotomy: can delayed or nonunion be predicted? Clin Orthop Relat Res 2014; 472: 1217–1223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ross KA, O’Halloran K, Castillo RC, et al. Prediction of tibial nonunion at the 6-week time point. Injury 2018; 49: 2075–2082. [DOI] [PubMed] [Google Scholar]
- 19.Christiano AV, Pean CA, Leucht P, et al. Scoring of radiographic cortical healing with the radiographic humerus union measurement predicts union in humeral shaft fractures. Eur J Orthop Surg Traumatol 2020; 30: 835–838. [DOI] [PubMed] [Google Scholar]
- 20.Driesman AS, Fisher N, Karia R, et al. Fracture site mobility at 6 weeks after humeral shaft fracture predicts nonunion without surgery. J Orthop Trauma 2017; 31: 657–662. [DOI] [PubMed] [Google Scholar]