Abstract
Background
Push-ups (PU) are a common closed chain exercise used to enhance shoulder girdle stability, with variations that alter the difficulty or target specific muscles. To appropriately select and prescribe PU exercises, an understanding of muscle activity during variations of the PU is needed. The purpose of this scoping review was to identify common PU variations and describe their muscle activation levels.
Methods
Databases searched included PubMed, CINAHL, Scopus, and SPORTDiscus for articles published between January 2000 and November 2019.
Results
Three hundred three articles were screened for eligibility with 30 articles included in the analysis. Six PU types and five muscles met the criteria for analysis. Weighted mean electromyography (EMG) amplitude was calculated for each muscle across PU types and for each PU type as a measure of global muscle activity. Triceps and pectoralis major had the highest EMG amplitude during unstable, suspension, incline with hands on a ball and the standard PU. Serratus anterior had the highest EMG amplitude during PU plus and incline PU. The greatest global EMG amplitude occurred during unstable surface PU.
Discussion
These results provide clinicians with a framework for prescribing PU to target specific muscles and scale exercise difficulty to facilitate rehabilitation outcomes.
Keywords: Push-up, electromyography, rehabilitation, exercise
Introduction
Neuromuscular control, endurance, and strength are key components of many shoulder rehabilitation programs.1,2 Selection of appropriate exercises to address these components is an important determinant of successful rehabilitation outcomes.2–4 Axial loading during closed chain exercises enhances neuromuscular control through increased proprioceptive input and facilitates co-contraction to improve functional stability of the shoulder. 5 Therefore, upper extremity closed chain exercises can be an important component of a shoulder rehabilitation program.
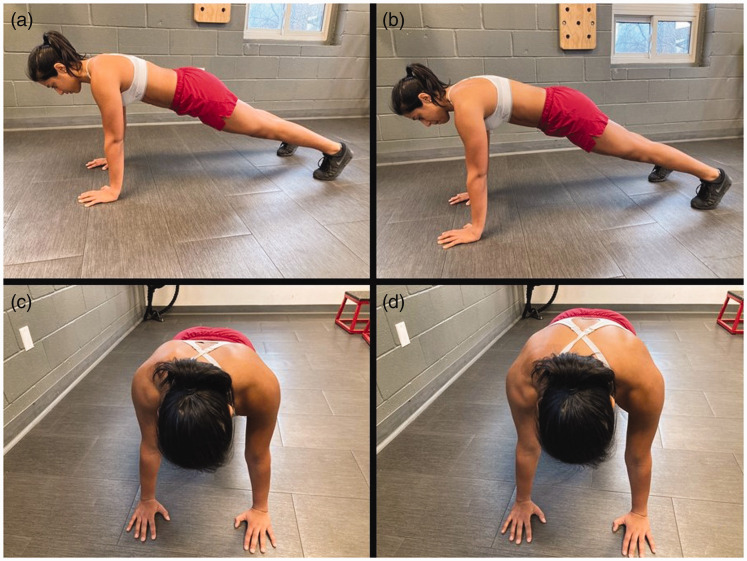
The standard push-up (PU) is a common closed chain exercise used to improve dynamic stability of the upper extremity through enhancement of proprioception, neuromuscular control, and shoulder girdle strength. 6 The starting position for the standard PU includes placing the hands directly below the glenohumeral joint, feet shoulder width apart, hips in a neutral position, and knees extended (Figure 1(a) and (c)). The body is then lowered to the ground until the elbows reach 90° of flexion, followed by a return back to the starting position. 7 The standard PU elicits high muscle activity in the serratus anterior (SA) and low activity in the upper fibers of the trapezius (UT), which may be helpful in restoring scapulothoracic muscle dysfunction seen in many shoulder pathologies.4,8 The standard PU position can be modified to alter muscle activation levels, target specific muscles, and scale exercise difficulty to facilitate successful rehabilitation outcomes.
Figure 1.
Standard push-up and push-up plus. (a) Starting position for standard push-up from lateral view. (b) Starting position for push-up plus from lateral view. (c) Starting position for standard push-up demonstrating scapulae in neutral position. (d) Starting position for push-up plus demonstrating scapular protraction.
There are countless variations of the standard PU; however, common modifications include altering body position,9,10 joint angles11,12 or stability of the external environment.13,14 To date, there has been no attempt to summarize the impact of variations to the standard PU on muscle activation levels. An overview of muscle activity during standard PU variations is needed to provide a framework for improved clinical decision making when selecting and prescribing PU exercises. The purpose of this scoping review was to identify commonly used PU variations within the literature and describe their muscle activation levels in healthy adults. Given the need for rehabilitation exercises and return to sport testing to match the functional demands of sport and work-related activities, knowledge of muscle activity during PU variations will assist in designing progressive, functional rehabilitation programs for individuals with closed chain upper extremity demands.
Materials and methods
A scoping review was selected for this study to gain an overview of the common clinically relevant PU variations examined in the literature and describe their muscle activation levels. The methodological framework for this scoping review followed recommendations of Levac et al. 15 and Colquhoun et al. 16 with the PRISMA Extension for Scoping Reviews checklist to guide reporting. 17
Data sources and searches
A database search was conducted in PubMed, CINAHL, Scopus, and SPORTDiscus to identify relevant peer-reviewed journal articles using the keywords [EMG OR electromyogra*] AND [“push up” OR “push-up”]. Reference lists of included studies and related systematic reviews were hand searched for additional relevant literature. The search was limited to full-text articles available in English and published between January 2000 and November 2019, to reflect contemporary exercise prescription practices.
Study selection
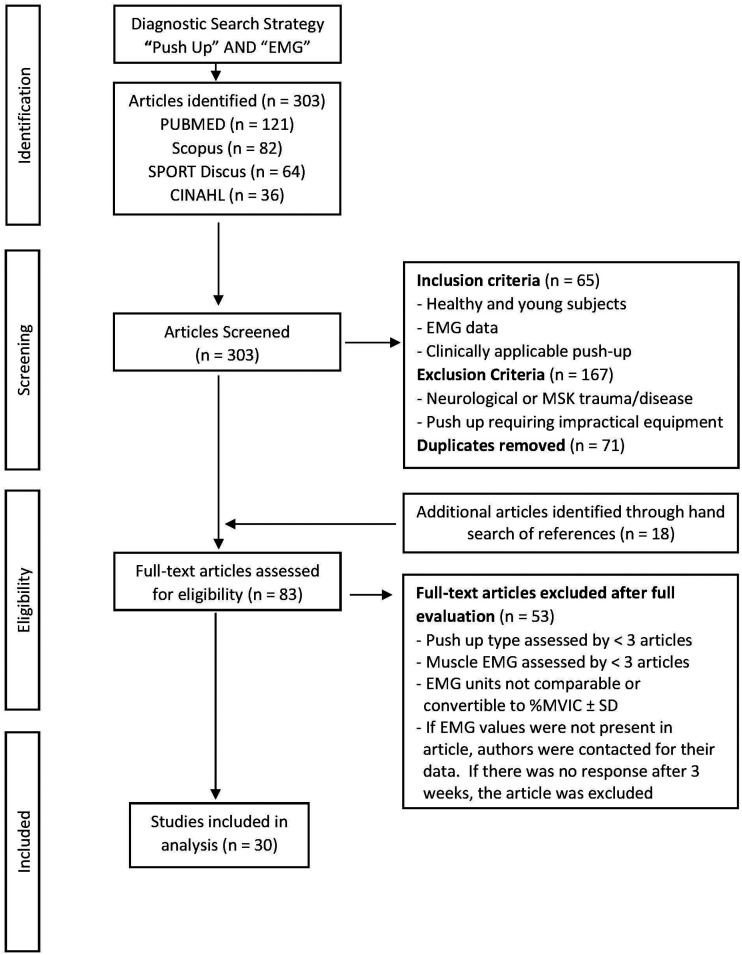
After identification of the relevant literature, each article was screened in duplicate by two study team members to ensure inclusion and exclusion criteria were met. Disagreement between reviewers was resolved through discussion to reach inclusion/exclusion consensus. Articles were included when the study population was young adults free of shoulder impairment and self-reported comorbidities, a PU variation was investigated in at least three articles and electromyography (EMG) values were expressed as a percent of maximum voluntary isometric contraction (%MVIC). If EMG values were not comparable or convertible to %MVIC from the reported values in the study, authors were contacted for their data. If there was no response after 3 weeks, the article was excluded. Articles were excluded from review if the study sample included subjects with neurological or musculoskeletal trauma or disease, PUs required expensive machinery or equipment (e.g. Stott Pilates® Reformer), or were deemed too difficult for the general population (e.g. clapping PU). Full texts were evaluated, using the same process as article screening, to identify articles for inclusion in the final analysis of PU variations and muscle activation levels. See Figure 2 for the article search and selection process flow diagram.
Figure 2.
Article search and selection flow diagram.
EMG: electromyography; MVIC: maximum voluntary isometric contraction.
Data extraction
Data extraction was completed in duplicate by two study team members. Data extracted from each full-text evaluation included: authors, year of publication, number of participants, participant age and sex, type of PU, muscles examined, mean EMG and standard deviation values represented as %MVIC. Where standard error was presented, standard deviation was calculated using the sample size.
Data synthesis and analysis
Study participant demographic information is reported as mean ± standard deviation, as appropriate. To determine average muscle activation levels across PU variations while accounting for unequal sample sizes, the weighted mean EMG amplitude was calculated using sample size as the weighting factor and expressed as %MVIC. To provide an estimate of total muscle activity for each PU type, a global EMG value was calculated as the weighted mean of all muscles for each PU variation. 14
Results
The literature search identified 303 articles to be screened (Figure 2). After removal of duplicates, 65 articles met inclusion criteria for full-text evaluation. Their reference lists were hand searched, and 18 additional articles were identified, leading to 83 articles that underwent full-text assessment for eligibility. Thirty articles were included in the final analysis, with a total of 606 participants and an average age of 23.1 ± 1.9 years. Females comprised 33.2% (n = 151) of study participants.
Six PU variations met inclusion criteria and included: standard PU (n = 17),7,9,13,14,18–30 PU plus (n = 11),11,12,18,20,29,31–36 suspension system (n = 7),10,13,14,24,27,30,37, hands on an unstable surface (n = 6),7,13,18,21,22,29 incline (n = 3),25,38,39 and incline with hands on an exercise ball (n = 3).25,38,39 Figures 1 and 3 provide representative images of these PU variations. Five muscles met inclusion criteria, including: SA (n = 17),9,11–13,18–24,28–30,34,35,38 UT (n = 17),10–12,14,18,19,21–23,29,30,32–34,36–38 pectoralis major (PM; n = 13),7,10–12,24–27,30,31,34,37,39 middle and lower fibers of trapezius (M/LT; n = 11),11,12,18,20–23,28,29,35,38 and triceps brachii (n = 11).7,10,11,14,19,24,26,27,30,37,39 MT and LT were grouped together as their scapular stabilization role is similar during the PU motion. 40 While other muscle groups (e.g. rotator cuff, deltoid, trunk stabilizers) are important for rehabilitation of the upper extremity, many did not meet inclusion criteria because they were not studied across all positions; the standard PU was the most common position for these muscles. A summary of all articles, including PU types, muscles assessed, and EMG values can be found in Table 1.
Figure 3.
Unstable, suspension, incline, incline on ball push-ups. (a) Unstable push-up on BOSU® ball. (b) Suspension push-up on TRX® with handles 10 cm from floor. (c) Incline push-up with hands elevated 65 cm. (d) Incline push-up on 65 cm ball.
Table 1.
Summary of push-up types, muscles assessed, and EMG amplitude.
| Author (year) | # participants | Age (years) | Type of PU | Muscles assessed | EMG (% MVIC) |
|---|---|---|---|---|---|
| Ashnagar (2016) | 0 M, 40 F | 23.9 ± 1.9 | Standard | Serratus anterior | 15.3 ± 16.7 |
| Standard | Upper trapezius | 4.3 ± 4.6 | |||
| Standard | Triceps | 23.7 ± 14.0 | |||
| Batbayar (2015) | 9 M, 0 F | 25 ± 2.7 | PU plus | Serratus anterior | 90.9 ± 40.5 |
| PU plus | Upper trapezius | 6.5 ± 3.3 | |||
| PU plus | Middle trapezius | 7.6 ± 7.9 | |||
| PU plus | Lower trapezius | 3.5 ± 1.5 | |||
| PU plus | Triceps | 48.1 ± 16.2 | |||
| PU plus | Pectoralis major | 13.3 ± 9.8 | |||
| Borreani (2015a) | 30 M, 0 F | 23 ± 1.1 | Standard | Serratus anterior | 29.1 ± 20.6 |
| Suspension | Serratus anterior | 75.5 ± 51.6 | |||
| Unstable | Serratus anterior | 95.8 ± 72.5 | |||
| Borreani (2015b) | 29 M, 0 F | 23.5 ± 3.1 | Suspension | Upper trapezius | 14.7 ± 10.3 |
| Suspension | Triceps | 37.0 ± 9.7 | |||
| Suspension | Pectoralis major | 30.8 ± 13.3 | |||
| Calatayud (2014a) | 29 M, 0 F | 23.5 ± 3.1 | Suspension | Upper trapezius | 20.4 ± 14.3 |
| Suspension | Triceps | 49.3 ± 15.5 | |||
| Suspension | Pectoralis major | 27.7 ± 13.0 | |||
| Calatayud (2014b) | 29 M, 0 F | 23.5 ± 3.1 | Standard | Upper trapezius | 5.9 ± 3.0 |
| Standard | Triceps | 17.1 ± 7.05 | |||
| Suspension | Upper trapezius | 15.7 ± 11.3 | |||
| Suspension | Triceps | 37.0 ± 9.7 | |||
| Calatayud (2014c) | 29 M, 0 F | 22.6 ± 2.6 | Standard | Serratus anterior | 24.4 ± 12.3 |
| Standard | Upper trapezius | 5.3 ± 3.2 | |||
| Standard | Triceps | 14.0 ± 8.3 | |||
| Standard | Pectoralis major | 23.6 ± 9.4 | |||
| Suspension | Serratus anterior | 13.1 ± 7.1 | |||
| Suspension | Upper trapezius | 9.4 ± 7.3 | |||
| Suspension | Triceps | 33.0 ± 18.4 | |||
| Suspension | Pectoralis major | 29.5 ± 9.2 | |||
| Cho (2014) | 5 M, 10 F | 22.1 ± 2.9 | PU plus | Serratus anterior | 22.9 ± 17.5 |
| PU plus | Upper trapezius | 9.9 ± 5.0 | |||
| PU plus | Lower trapezius | 7.2 ± 5.1 | |||
| PU plus | Pectoralis major | 24.9 ± 17.2 | |||
| Cogley (2005) | 11 M, 29 F | 24.3 ± 13.2 | Standard | Triceps | 101.3 ± 85.4 |
| de Araujo (2018) | 18 M, 0 F | 21.5 ± 2.6 | Standard | Serratus anterior | 27.5 ± 12.9 |
| Standard | Upper trapezius | 17.0 ± 13.4 | |||
| Standard | Lower trapezius | 23.9 ± 11.9 | |||
| Unstable | Serratus anterior | 27.7 ± 11.9 | |||
| Unstable | Upper trapezius | 22.5 ± 18.4 | |||
| Unstable | Lower trapezius | 24.8 ± 12.1 | |||
| de Araujo (2019) | 23 M, 0 F | 21.7 ± 3.0 | Standard | Serratus anterior | 92.3 ± 67.2 |
| Standard | Upper trapezius | 51.2 ± 43.6 | |||
| Standard | Middle trapezius | 21.9 ± 13.0 | |||
| Standard | Lower trapezius | 58.7 ± 48.4 | |||
| Unstable | Serratus anterior | 76.9 ± 20.7 | |||
| Unstable | Upper trapezius | 56.6 ± 37.3 | |||
| Unstable | Middle trapezius | 44.1 ± 29.5 | |||
| Unstable | Lower trapezius | 59.3 ± 34.6 | |||
| Decker (2003) | 9 M, 6 F | 26.8 ± 4.0 | PU plus | Pectoralis major | 94.3 ± 27.2 |
| Freeman (2006) | 9 M, 1 F | 24, SD not given | Standard | Triceps | 66.0 ± 17.6 |
| Standard | Pectoralis major | 61.2 ± 38.3 | |||
| Unstable | Triceps | 68.9 ± 16.2 | |||
| Unstable | Pectoralis major | 68.7 ± 39.9 | |||
| Gioftsos (2016) | 13 M, 0 F | 20.5 ± 1.0 | Standard | Serratus anterior | 49.0 ± 20.5 |
| Standard | Upper trapezius | 35.9 ± 14.0 | |||
| Standard | Lower trapezius | 12.8 ± 10.1 | |||
| PU plus | Serratus anterior | 60.7 ± 17.1 | |||
| PU plus | Upper trapezius | 28.6 ± 9.2 | |||
| PU plus | Lower trapezius | 9.1 ± 8.7 | |||
| Unstable | Serratus anterior | 45.7 ± 14.0 | |||
| Unstable | Upper trapezius | 35.8 ± 16.4 | |||
| Unstable | Lower trapezius | 12.6 ± 15.1 | |||
| Hwang (2015) | 29 M, 0 F | 24.7 ± 2.5 | PU plus | Serratus anterior | 59.2 ± 13.9 |
| PU plus | Upper trapezius | 9.9 ± 7.1 | |||
| PU plus | Pectoralis major | 10.7 ± 7.6 | |||
| Kang (2014) | 15 M, 0 F | 21.2 ± 2.4 | Standard | Serratus anterior | 45.5 ± 19.4 |
| Lehman (2006) | 13 M, 0 F | 26.3 ± 1.5 | Incline | Triceps | 22.2 ± 8.8 |
| Incline | Pectoralis major | 21.4 ± 11.8 | |||
| Incline, hands on ball | Triceps | 43.1 ± 17.3 | |||
| Incline, hands on ball | Pectoralis major | 26.7 ± 14.5 | |||
| Lehman (2008) | 10 M, 0 F | 26.1 ± 1.1 | Incline | Serratus anterior | 24.2 ± 14.5 |
| Incline | Upper trapezius | 5.2 ± 6.4 | |||
| Incline | Lower trapezius | 10.5 ± 12.2 | |||
| Incline, hands on ball | Serratus anterior | 19.7 ± 11.5 | |||
| Incline, hands on ball | Upper trapezius | 10.5 ± 6.9 | |||
| Incline, hands on ball | Lower trapezius | 9.5 ± 11.9 | |||
| Ludewig (2004) | 7 M, 12 F | 25.2 ± 3.7 | PU plus | Upper trapezius | 14.5 ± 11.8 |
| Marshall (2006) | 8 M, 4 F | 22.1 ± 2.4 | Standard | Pectoralis major | 34.1 ± 25.5 |
| Incline | Pectoralis major | 25.5 ± 13.6 | |||
| Incline, hands on ball | Pectoralis major | 39.2 ± 27.2 | |||
| McGill (2014) | 14 M, 0 F | 21.1 ± 2.0 | Standard | Serratus anterior | 72.1 ± 60.2 |
| Standard | Triceps | 23.0 ± 22.7 | |||
| Standard | Pectoralis major | 46.6 ± 40.6 | |||
| Suspension | Serratus anterior | 55.6 ± 60.3 | |||
| Suspension | Triceps | 29.6 ± 19.4 | |||
| Suspension | Pectoralis major | 42.3 ± 32.8 | |||
| Park (2013) | 20 M, 0 F | 21–26, no mean given | PU plus | Upper trapezius | 3.6 ± 1.9 |
| Park (2015) | 10 M, 0 F | 23.9 ± 1.8 | PU plus | Upper trapezius | 8.0 ± 3.5 |
| Santos (2018) | 18 M, 0 F | 22.0 ± 2.0 | Standard | Serratus anterior | 49.7 ± 38.0 |
| Standard | Upper trapezius | 3.4 ± 2.6 | |||
| Standard | Middle trapezius | 6.3 ± 11.4 | |||
| Standard | Lower trapezius | 10.0 ± 6.5 | |||
| Snarr (2013) | 15 M, 6 F | 25.2 ± 3.4 | Standard | Triceps | 74.3 ± 16.9 |
| Standard | Pectoralis major | 63.6 ± 16.4 | |||
| Suspension | Triceps | 105.8 ± 18.5 | |||
| Suspension | Pectoralis major | 69.5 ± 27.6 | |||
| Stoelting (2008) | 0 M, 19 F | 20.7 ± 2.3 | Standard | Serratus anterior | 91.9 ± 52.2 |
| Standard | Middle trapezius | 32.6 ± 16.2 | |||
| Standard | Lower trapezius | 28.2 ± 15.0 | |||
| PU plus | Serratus anterior | 83.0 ± 44.6 | |||
| PU plus | Middle trapezius | 34.8 ± 18.8 | |||
| PU plus | Lower trapezius | 26.8 ± 9.8 | |||
| Tucker (2008) | 15 M, 13 F | 20.9 ± 2.8 | Standard | Serratus anterior | 68.5 ± 32.8 |
| Standard | Middle trapezius | 27.0 ± 20.4 | |||
| Standard | Lower trapezius | 36.1 ± 19.0 | |||
| Tucker (2009) | 19 M, 0 F | 20.7 ± 2.9 | PU plus | Serratus anterior | 48.6 ± 16.8 |
| PU plus | Lower trapezius | 29.4 ± 12.8 | |||
| Tucker (2010) | 4 M, 11 F | 20.4 ± 3.8 | Standard | Serratus anterior | 56.2 ± 24.4 |
| Standard | Upper trapezius | 44.7 ± 30.2 | |||
| Standard | Middle trapezius | 18.0 ± 7.3 | |||
| Standard | Lower trapezius | 27.0 ± 13.1 | |||
| Unstable | Serratus anterior | 48.3 ± 21.7 | |||
| Unstable | Upper trapezius | 61.6 ± 47.4 | |||
| Unstable | Middle trapezius | 19.5 ± 7.3 | |||
| Unstable | Lower trapezius | 27.5 ± 11.2 |
EMG values are weighted mean ± SD. Unstable push-up includes BOSU® balls, stability discs, balance boards, foam mats, and unstable push-up bars.
EMG: electromyography; MVIC: maximum voluntary isometric contraction; PU: push-up.
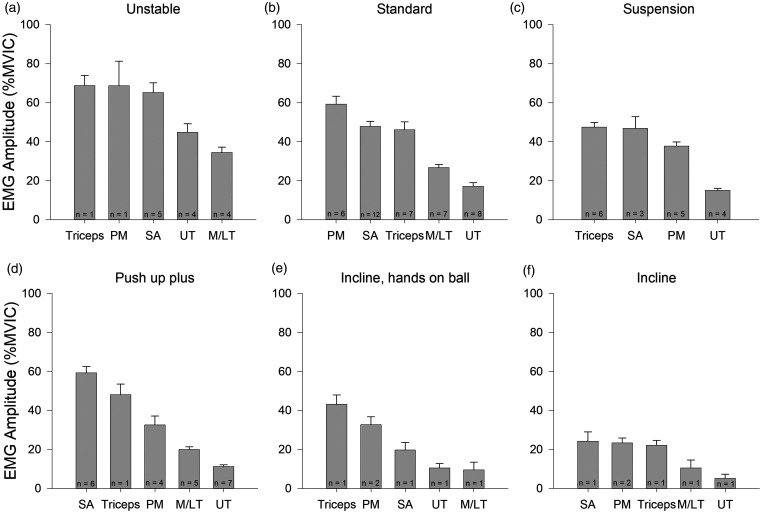
The weighted mean EMG amplitude for each muscle across PU variations is presented graphically in Figure 4, and numerical data are available as a supplemental appendix. PM and triceps demonstrated the highest EMG amplitude in four of the six PU types. SA had the highest EMG amplitude during the PU plus and incline PU. UT demonstrated the lowest EMG amplitude in four of the six PU types. There were no studies assessing M/LT activation during suspension PUs.
Figure 4.
EMG amplitude across muscles and push-up type. Weighted mean EMG amplitude for each muscle group during identified push-up variations. Data are presented as weighted mean ± SE.
EMG: electromyography; M/LT: middle/lower trapezius; MVIC: maximum voluntary isometric contraction; n: number of studies evaluated for each muscle; PM: pectoralis major; SA: serratus anterior; UT: upper trapezius.
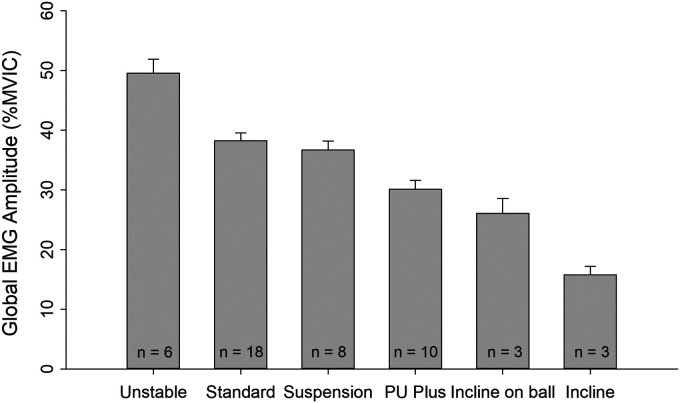
The greatest global EMG activity occurred during PU on an unstable surface (49.6 ± 40.5 %MVIC). The standard PU had the next highest global EMG activity (38.2 ± 41.8 %MVIC), followed by suspension systems (36.7 ± 31.9 %MVIC), PU plus (30.1 ± 30.6 %MVIC), incline on a ball (26.1 ± 20.7 %MVIC) and incline on a stable surface (15.8 ± 13.4 %MVIC). Global EMG activity for each PU type is presented in Figure 5.
Figure 5.
Global EMG amplitude for each push-up type. Combined weighted mean EMG amplitude of pectoralis major, serratus anterior, middle/lower trapezius, upper trapezius, and triceps for each push-up movement. Data are presented as weighted mean ± SE.
EMG: electromyography; MVIC: maximum voluntary isometric contraction; n: number of studies evaluated per push-up movement; PU: push-up.
Discussion
Multiple variations of the standard PU exist in rehabilitation and strengthening of the upper quadrant in weight bearing. The purpose of this scoping review was to identify commonly researched PU variations and describe their muscle activation levels. Six PU variations were identified (standard, unstable, suspension, PU plus, incline, incline on a ball) with muscle activity in five muscles (SA, PM, triceps, UT, M/LT) described during the PU variations. This EMG-based review of PU variations can assist in developing rehabilitation programs for individuals with closed chain upper extremity work or sport demands. This could include progressively challenging the shoulder girdle to prepare for return to sport testing, such as the Upper Quarter Y Balance Test. 41 Further, this review advances the existing framework for upper extremity weight bearing exercise prescription which may be implemented within the context of the Derby Shoulder Instability Rehabilitation Program for atraumatic recurrent shoulder instability 42 or late to end-stage rehabilitation in individuals who have work or sport-related upper extremity weight bearing demands. However, clinical reasoning regarding exercise prescription should always include an analysis of the functional capacities of the patient, which includes assessment for other musculoskeletal impairments which may become exacerbated by high-level exercises, especially those performed on unstable surfaces.
To facilitate contextualization of normalized EMG amplitude, categories of muscle activity intensity have been developed and include: low ( < 20% MVIC), moderate (21%–40% MVIC), high (41%–60% MVIC), and very high ( > 60% MVIC).43,44 Low levels of muscle activity are generally recommended for early rehabilitation or when minimal muscle activity is desired, while high levels of activity are reserved for later rehabilitation exercises and general strengthening.43,45 This convention will be used in the following discussion of muscle activity during each PU variations.
Standard push-up
The standard PU (Figure 1(a) and (c)) led to high activity levels in the prime movers of the PU movement (i.e. triceps, PM) and the SA. While the scapula demonstrates some three-dimensional movement during the standard PU, 46 there is less scapular movement during a PU compared to open chain upper extremity elevation, for a similar degree of humeral elevation. 47 Thus, high SA activity during the standard PU can be presumed to facilitate scapular stabilization, allowing for dynamic control of the glenohumeral joint. Given the high muscle activity in the triceps, PM, and SA, the standard PU could be considered an appropriate end-stage rehabilitation exercise, particularly if triceps, PM or SA strengthening is desired.
SA also functions as a force couple with the trapezius to assist with scapular positioning and movement.48,49 The standard PU led to moderate activity in M/LT and low activity in UT. Low UT activity relative to higher M/LT and SA activity can be a desirable muscle activity combination as individuals with scapular and shoulder dysfunction often demonstrate weak or underactive SA and M/LT with overactive UT.4,50 Thus, the standard PU may be an effective exercise for patients with scapulothoracic muscle imbalance.
The global EMG amplitude of the standard PU was nearly 40% MVIC, bordering on high activity. This activity level is consistent with the recommendation that PU progressions are added to end-stage rehabilitation programs when muscles are able to tolerate higher loads2,51 or prescribed to individuals interested in building general upper extremity strength.
Unstable push-up
EMG activity during unstable PU (Figure 3(a)) was higher in all muscles compared to other PU variations with global EMG in the high activity category. In comparison to the standard PU, PM, triceps, and SA activity increased from the high to very high activity category, UT activity more than doubled and moved from the low to high activity category, while M/LT had a modest increase in EMG activity but stayed in the moderate category. Given these high and very high levels of muscle activity, PU on an unstable surface should be reserved for end-stage rehabilitation or for individuals seeking to enhance upper extremity strength.
The increase in EMG activity during an unstable PU could be due to increased co-contraction to control the upper limb and scapular position, improve joint stiffness and stability.52,53 Indeed, long-term training on an unstable surface leads to improved coordination between synergists and antagonists as well as faster activation of stabilizing muscles, further enhancing joint stability and reducing the risk of injury.52,53 Therefore, the unstable PU may be an effective exercise to enhance joint proprioception and neuromuscular control of the shoulder joint complex.
The unstable PU was one of two PU variations (unstable and incline, hands on ball) in which UT EMG activity was not the lowest of the muscles reviewed. This is consistent with a systematic review in which all unstable pushing exercises had high UT to SA activity ratios. 54 As many individuals with shoulder pathology demonstrate increased UT activity and SA weakness or underactivity during arm elevation, unstable PU are not the preferred PU variation. The standard PU or PU plus, as noted below, may be more appropriate due to their low UT and high SA activity.
Studies in this review which investigated an unstable PU used a variety of equipment to create an unstable surface, such as BOSU® balls, stability discs, balance boards, foam mats, and unstable PU bars. While different unstable surfaces could introduce variability into the EMG results, this equipment likely reflects that which is available within a clinical environment and allows the results to be more generalizable. Additionally, when the hands are placed on an unstable surface while the feet are kept on the ground, there is an increase in the body inclination angle. As this angle is increased, there is a reduction in body weight placed through the upper extremities, leading to a decline in muscle activity. 55 Not all studies accounted for this change in body angle which could impact the results. However, given most muscle activity levels were in the high or very high categories, the influence of body inclination angle was likely minimal.
Suspension push-up
Most studies investigating a suspension PU used a TRX® (Figure 3(b)). During this PU variant, SA and triceps activity remained high while UT remained low, in comparison to the standard PU. This indicates that the suspension PU is a good option to target triceps and SA, particularly if one is looking to keep UT activity low.
While a suspension device is an unstable surface, which generally leads to increased muscle activity, individual muscle and global EMG in the suspension PU were less than the unstable PU. During a suspension PU, the body is often in a more inclined position than a standard PU, leading to less body weight placed through the upper extremities and consequently less muscle demand. 56 Therefore, it is possible the greater body inclination angle in the suspension PU mitigated an increase in muscle activity due to the unstable surface created by the suspension system.
Alternatively, previous work has demonstrated that moderately unstable surfaces increase muscle activity while highly unstable surfaces decrease muscle activity,52,53 suggesting unstable surfaces, such as rocker boards and BOSU® balls, may serve as moderately unstable surfaces while suspension devices are highly unstable surfaces. The authors of this previous work interpret these findings to suggest that highly unstable environments lead to a decline in muscle activity of the primary movers of a motion with transfer of activity to greater stabilizing functions. 52 Under this framework, the suspension PU would lead to lower activation of the PM and triceps with greater activation of the shoulder and trunk stabilizers, and lower extremity posterior chain musculature compared to unstable PU. In alignment with this theory, we identified lower muscle activity in the PM and triceps during the suspension PU compared to the unstable PU. However, we also noted a decline in SA and UT activity, which would likely be functioning as stabilizers. We were unable to assess M/LT activity during suspension PU as this investigation was notably absent from the literature. Muscle activity of the trunk and lower extremities during PU variations was also not included in this review, because there were too few studies from the body of literature considering muscle activity. Trunk and lower extremity muscle activation during exercises targeting the upper extremity is an important area for future study as much of the upper extremity torque is generated in the lower quadrant and transferred to the upper extremity through the trunk and shoulder girdle. Future research should incorporate more scapular, trunk, and lower extremity muscles, such as the M/LT, erector spine, and gluteals, into investigations of EMG activity during upper extremity exercise. This will facilitate a better understanding of optimal exercise prescription for upper extremity athletes in preparation for return to sport.
In addition, while the body inclination angle was not reported in most suspension PU studies, those that did, set the suspension handles 10 cm from the floor. Strap height is an important consideration when prescribing suspension PU as it is an easily modifiable variable to scale the exercise difficulty and modulate EMG activity. Future research should ensure to account for and report suspension strap height to assist in determining the differential influence of changes in body inclination angle and the unstable surface created by the suspension system in muscle activity.
Push-up plus
The PU plus is performed similar to the standard PU, with the addition of scapular protraction at full elbow extension (Figure 1(b) and (d)). During this PU variation, SA is not only providing scapular stabilization, but is also working dynamically to produce scapular protraction. Indeed, SA activity increased during the PU plus in comparison to the standard PU, with activity levels bordering on very high. This occurred in conjunction with a slight decline in UT activity in comparison to the standard PU, highlighting the low UT to SA activity ratio of the PU plus. Therefore, the PU plus is an effective exercise to target the SA and may be a more ideal PU variation than the standard PU for individuals who have overactive UT.
M/LT activity declined during the PU plus in comparison to the standard PU, with activity levels bordering on low to moderate. This could have occurred as a result of M/LT acting as antagonists to scapular protraction during the ‘plus’ phase of the PU or due to scapular protraction placing the M/LT in a lengthened position, thereby decreasing the available active force generation and EMG activity of the M/LT. Thus, for individuals with weak, underactive M/LT, the PU plus is not a recommended exercise due to low activity levels. However, it is interesting to note that LT activity can be increased during a PU plus by using a narrow hand placement, which alters scapular positioning and creates a more favorable LT length-tension relationship. 35 Therefore, to facilitate LT activity, it may be worthwhile to consider a narrow hand placement.
During PU plus, PM activity declined from the high to moderate category, in comparison to the standard PU. As scapular protraction occurs through protraction of the clavicle, the clavicular head of the PM may act as a synergist to SA through facilitating clavicular protraction.57,58 Therefore, if PM and SA are acting synergistically, it is possible PM activity declined due to the increase in SA activity during the PU plus. If PM is the muscle of interest for strengthening, then the standard PU or PU on an unstable surface is a better choice than the PU plus.
PU plus global EMG activity declined slightly compared to the standard PU, though remained in the moderate muscle activity category. However, given the high levels of activity in SA and triceps, PU plus should still be considered an advanced exercise and reserved for end-stage rehabilitation and general upper extremity strengthening.
Incline push-up
Incline PU consisted of a standard PU performed with hands placed on a stable box or bench (Figure 3(c)). In comparison to the standard PU, incline PU led to a reduction in muscle activity in all muscles included in this review. PM, SA, and triceps activity declined from the high to low category, M/LT activity declined from the moderate to low category while UT activity declined and remained in the low category. These changes led incline PU global EMG amplitude to be the lowest of all PU variations. These results suggest that performing an incline PU may be incorporated earlier in the rehabilitation process if low grade muscle activity is desired in a closed chain position. However, compared to other PU variations examined in this review, there were fewer studies investigating muscle activity during an incline PU with fewer muscles assessed. This could limit the interpretation and application of these findings. Future studies should ensure that there is a broad, comprehensive, and consistent examination of muscle activity when analyzing PU variations for rehabilitation.
Lower levels of muscle activity during the incline PU likely reflects a reduction in weight bearing through the upper extremities as the body inclination angle is increased and less muscle activity is required to support the body. 55 Therefore, the height of the inclined surface can therefore be manipulated to modulate muscle activity. Of the studies investigating incline PU, two used boxes 65 cm tall while height was not mentioned in the third study. Future research should ensure reporting of elevation height to facilitate comparison between studies and application to clinical environments.
Incline on ball
All studies that examined an incline PU on an unstable surface used an exercise ball (Figure 3(d)). In comparison to the stable incline PU, incline PU on a ball increased EMG activity in muscles acting as prime movers. PM had a small increase in activity and remained in the moderate category while triceps had a large increase in activity and moved into the high category. This pattern is similar to that observed when comparing the standard to the unstable PU. Thus, it appears that adding instability to the PU, no matter what the position, increases activity in the prime movers, and particularly the triceps.
This contrasts with the activity of the scapular stabilizers during unstable incline PU, which demonstrated minimal changes in comparison to the stable incline PU. SA activity declined slightly and fell into the low category while M/LT and LT activity remained unchanged in the low category. Therefore, it appears that incline PU on a ball is not an effective exercise to strengthen the scapular stabilizers. However, if low levels of muscle activity in the scapular stabilizers are desired in combination with a dynamic surface to train proprioception and neuromuscular control, then incline PU on a ball may be an effective exercise.
Incline PU on a ball demonstrated moderate global EMG activity and was greater than global EMG during the stable incline PU. This further demonstrates the impact of an unstable surface on increasing global muscle activity. PU on an unstable surface, such as an exercise ball, may be an appropriate progression from a stable incline PU prior to lowering the inclination of the body to a standard PU position. However, similar to incline PU on a stable surface, the number of studies we identified examining muscle activity during PU on a ball was limited, as was the number of muscle groups assessed within this PU variation. Therefore, caution should be exercised with implementation of these findings, and future research should ensure muscles assessed during PU variation exercises are thorough and align with those previously reported within the literature.
Limitations
While EMG studies assist in guiding clinical decision making regarding therapeutic exercise prescription, there are limitations in interpreting EMG studies. To allow for comparisons between studies, we selected articles which normalized EMG values to an isolated MVIC. Informed by the methodology within each paper, we assumed participants were able to perform a true isolated MVIC, PU modifications were performed in a similar manner and comparable placement of EMG electrodes. The phase of the PU motion in which EMG data was reported was not always consistent or mentioned, which could impact the results of each study. To enhance the ability to compare EMG results across studies, improvements in reporting of EMG methodology are warranted.
Of the 606 participants in this review, only 151 (33%) were female, representing a large disparity between male and female participants in EMG-based research. More work is required to ensure females are adequately represented in EMG-based research studies. This becomes important as physiological sex-specific differences, such as muscle fiber type composition, 59 force steadiness 60 and fatigue, 61 can impact EMG assessments of muscle activity and are related to neck and shoulder musculoskeletal disorders. 62
We only included studies which obtained data from young, healthy participants who were free of shoulder impairments and may have different muscle activation levels than individuals with shoulder pain, weakness, or other pathology. This should be considered when extrapolating our results to a patient population. Further, studies included in this review only assessed muscle activity in a non-fatigued state. As muscle activation levels can change with fatigue 63 and key priorities for return to sport rehabilitation include addressing fatigability and enhancing endurance capacity, caution should be used when applying our results to exercises performed in a fatigued state. However, this review is a necessary first step in understanding the expected muscle activation levels during variations of the standard PU, from which future research with patient populations can be compared. Further, this review highlights the need for future research to investigate rotator cuff, deltoid, and trunk stabilizer muscle activity during variations of the standard PU, as these muscle groups can play an important role in upper extremity rehabilitation.
Conclusion
This scoping review provides clinicians and other exercise or sport performance professionals with an EMG-based framework from which PU variations can be prescribed to target specific muscles. Prescribing PU variations with progressively greater muscle activation levels will prepare individuals for the upper extremity control and strength demands of safe return to work or sport. This review advances the existing framework for upper extremity weight bearing exercise prescription, which may be incorporated into established rehabilitation protocols, such as the Derby Shoulder Instability Rehabilitation Program for atraumatic recurrent shoulder instability 42 or late to end-stage rehabilitation in individuals with work or sport-related upper extremity weight bearing demands. However, further investigation is required to determine if these muscle activation levels during PU variations are similar in individuals with shoulder pain or pathology.
Supplementary Material
Acknowledgements
The authors thank A Dib, N Dua, S Hasan and A Younes for their efforts in the literature search, selection and data extraction process, as well as J Mistry for being a model in the PU figures. This paper is not based on a previous communication to a society or meeting.
Contributorship: JS and DC conceived the study; KK, DC, JS and JJ reviewed the literature and extracted data; KK performed the analysis; KK, JS, DC and JJ interpreted the data; KK drafted the manuscript and created figures; JS, DC and JJ critically reviewed and edited the manuscript; all authors approved the final version of the manuscript.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Guarantor: DC
ORCID iD: Denise M Connelly https://orcid.org/0000-0001-8138-1746
Supplemental material: Supplemental material for this article is available online.
Ethical Review and Patient Consent
N/A for this scoping review.
References
- 1.Reinold MM, Escamilla R, Wilk KE. Current concepts in the scientific and clinical rationale behind exercises for glenohumeral and scapulothoracic musculature. J Orthop Sports Phys Ther 2009; 39: 105–117. [DOI] [PubMed] [Google Scholar]
- 2.Bleichert S, Renaud G, MacDermid J, et al. Rehabilitation of symptomatic atraumatic degenerative rotator cuff tears: a clinical commentary on assessment and management. J Hand Ther 2017; 30: 125–135. [DOI] [PubMed] [Google Scholar]
- 3.Steuri R, Sattelmayer M, Elsig S, et al. Effectiveness of conservative interventions including exercise, manual therapy and medical management in adults with shoulder impingement: a systematic review and meta-analysis of RCTs. Br J Sport Med 2017; 51: 1340–1347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Castelein B, Cagnie B, Cools A. Scapular muscle dysfunction associated with subacromial pain syndrome. J Hand Ther 2017; 30: 136–146. [DOI] [PubMed] [Google Scholar]
- 5.Lephart SM, Pincivero DM, Giraldo JL, et al. The role of proprioception in the management and rehabilitation of athletic injuries. Am J Sports Med 1997; 25: 130–137. [DOI] [PubMed] [Google Scholar]
- 6.Wright AA, Hegedus EJ, Tarara DT, et al. Exercise prescription for overhead athletes with shoulder pathology: a systematic review with best evidence synthesis. Br J Sport Med 2018; 52: 231–237. [DOI] [PubMed] [Google Scholar]
- 7.Freeman S, Karpowicz A, Gray J, et al. Quantifying muscle patterns and spine load during various forms of the push-up. Med Sci Sports Exerc 2006; 38: 570–577. [DOI] [PubMed] [Google Scholar]
- 8.Cricchio M, Frazer C. Scapulothoracic and scapulohumeral exercises: a narrative review of electromyographic studies. J Hand Ther 2011; 24: 322–334. [DOI] [PubMed] [Google Scholar]
- 9.Kang DH, Jung SY, Nam DH, et al. The effects of push-ups with the trunk flexed on the shoulder and trunk muscles. J Phys Ther Sci 2014; 26: 909–910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Borreani S, Calatayud J, Colado JC, et al. Shoulder muscle activation during stable and suspended push-ups at different heights in healthy subjects. Phys Ther Sport 2015; 16: 248–254. [DOI] [PubMed] [Google Scholar]
- 11.Batbayar Y, Uga D, Nakazawa R, et al. Effect of various hand position widths on scapular stabilizing muscles during the push-up plus exercise in healthy people. J Phys Ther Sci 2015; 27: 2573–2576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cho SH, Baek IH, Cheon JY, et al. Effect of the push-up plus (PUP) exercise at different shoulder rotation angles on shoulder muscle activities. J Phys Ther Sci 2014; 26: 1737–1740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Borreani S, Calatayud J, Colado JC, et al. Muscle activation during push-ups performed under stable and unstable conditions. J Exerc Sci Fit 2015; 13: 94–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Calatayud J, Borreani S, Colado JC, et al. Muscle activation during push-ups with different suspension training systems. J Sport Sci Med 2014; 13: 502–510. [PMC free article] [PubMed] [Google Scholar]
- 15.Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci 2010; 5: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Colquhoun HL, Levac D, O’Brien KK, et al. Scoping reviews: time for clarity in definition, methods, and reporting. J Clin Epidemiol 2014; 67: 1291–1294. [DOI] [PubMed] [Google Scholar]
- 17.Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 2018; 169: 467–473. [DOI] [PubMed] [Google Scholar]
- 18.Tucker WS, Armstrong CW, Gribble PA, et al. Scapular muscle activity in overhead athletes with symptoms of secondary shoulder impingement during closed chain exercises. Arch Phys Med Rehabil 2010; 91: 550–556. [DOI] [PubMed] [Google Scholar]
- 19.Ashnagar Z, Shadmehr A, Hadian M, et al. The effects of whole body vibration on EMG activity of the upper extremity muscles in static modified push up position. J Back Musculoskelet Rehabil 2016; 29: 557–563. [DOI] [PubMed] [Google Scholar]
- 20.Stoelting KJ. The effects of hand placement on muscle activation during a closed kinetic chain exercise in physically active females, Toledo: University of Toledo, 2008. [Google Scholar]
- 21.de Araújo RC, Pirauá ALT, Beltrão NB, et al. Activity of periscapular muscles and its correlation with external oblique during push-up: does scapular dyskinesis change the electromyographic response? J Sports Sci 2018; 36: 571–577. [DOI] [PubMed] [Google Scholar]
- 22.de Araújo RC, Nascimento VYS, Torres RJB, et al. Can the use of unstable surfaces and instruction for conscious abdominal contraction increase the EMG activity of the periscapular muscles during the dynamic push-up? J Sport Rehabil 2019; 29: 225–230. [DOI] [PubMed] [Google Scholar]
- 23.Santos MR, Cavalcante BR, Ferreira FLS, et al. Effects of conscious abdominal contraction on periscapular muscle activity. Clin Kinesiol 2018; 72: 23–28. [Google Scholar]
- 24.McGill SM, Cannon J, Andersen JT. Analysis of pushing exercises: muscle activity and spine load while contrasting techniques on stable surfaces with a labile suspension strap training system. J Strength Cond Res 2014; 28: 105–116. [DOI] [PubMed] [Google Scholar]
- 25.Marshall P, Murphy B. Changes in muscle activity and perceived exertion during exercises performed on a Swiss ball. Appl Physiol Nutr Metab 2006; 31: 376–383. [DOI] [PubMed] [Google Scholar]
- 26.Cogley RM, Archambault TA, Fibeger JF, et al. Comparison of muscle activation using various hand positions during the push-up exercise. J Strength Cond Res 2005; 19: 628–633. [DOI] [PubMed] [Google Scholar]
- 27.Snarr RL, Esco MR. Electromyographic comparison of traditional and suspension push-ups. J Hum Kinet 2013; 39: 75–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tucker WS, Campbell BM, Swartz EE, et al. Electromyography of 3 scapular muscles: a comparative analysis of the cuff link device and a standard push-up. J Athl Train 2008; 43: 464–469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gioftsos G, Arvanitidis M, Tsimouris D, et al. EMG activity of the serratus anterior and trapezius muscles during the different phases of the push-up plus exercise on different support surfaces and different hand positions. J Phys Ther Sci 2016; 28: 2114–2118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Calatayud J, Borreani S, Colado JC, et al. Muscle activity levels in upper-body push exercises with different loads and stability conditions. Phys Sportsmed 2014; 42: 106–118. [DOI] [PubMed] [Google Scholar]
- 31.Decker MJ, Tokish JM, Ellis HB, et al. Subscapularis muscle activity during selected rehabilitation exercises. Am J Sports Med 2003; 31: 126–134. [DOI] [PubMed] [Google Scholar]
- 32.Park SY, Yoo WG. Activation of the serratus anterior and upper trapezius in a population with winged and tipped scapulae during push-up-plus and diagonal shoulder-elevation. J Back Musculoskelet Rehabil 2015; 28: 7–12. [DOI] [PubMed] [Google Scholar]
- 33.Park S, Yoo W, Kim M, et al. Differences in EMG activity during exercises targeting the scapulothoracic region: a preliminary study. Man Ther 2013; 18: 512–518. [DOI] [PubMed] [Google Scholar]
- 34.Hwang U-J, Kwon O-Y, Jeon I-C, et al. Effect of humeral elevation angle on electromyographic activity in the serratus anterior during the push-up plus exercise. J Sport Rehabil 2015; 26: 57–64. [DOI] [PubMed] [Google Scholar]
- 35.Tucker WS, Gilbert ML, Gribble PA, et al. Effects of hand placement on scapular muscle activation during the push-up plus exercise. Athl Train Sport Heal Care 2009; 1: 107–113. [Google Scholar]
- 36.Ludewig PM, Hoff MS, Osowski EE, et al. Relative balance of serratus anterior and upper trapezius muscle activity during push-up exercises. Am J Sports Med 2004; 32: 484–493. [DOI] [PubMed] [Google Scholar]
- 37.Calatayud J, Borreani S, Colado JC, et al. Muscle activation differences between stable push-ups and push-ups with a unilateral v-shaped suspension system at different heights. Motricidade 2014; 10: 84–93. [Google Scholar]
- 38.Lehman GJ, Gilas D, Patel U. An unstable support surface does not increase scapulothoracic stabilizing muscle activity during push up and push up plus exercises. Man Ther 2008; 13: 500–506. [DOI] [PubMed] [Google Scholar]
- 39.Lehman GJ, MacMillan B, MacIntyre I, et al. Shoulder muscle EMG activity during push up variations on and off a Swiss ball. Dyn Med 2006; 5: 11–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Torres RJB, Piraua ALT, Nascimento VYS, et al. Shoulder muscle activation levels during the push-up-plus exercise on stable and unstable surfaces. J Sport Rehabil 2017; 26: 281–286. [DOI] [PubMed] [Google Scholar]
- 41.Westrick RB, Miller JM, Carow SD, et al. Exploration of the Y-balance test for assessment of upper quarter closed kinetic chain performance. Int J Sports Phys Ther 2012; 7: 139–147. [PMC free article] [PubMed] [Google Scholar]
- 42.Bateman M, Osborne SE, Smith BE. Physiotherapy treatment for atraumatic recurrent shoulder instability: updated results of the Derby Shoulder Instability Rehabilitation Programme. J Arthrosc Jt Surg 2019; 6: 35–41. [Google Scholar]
- 43.Escamilla RF, Yamashiro K, Paulos L, et al. Shoulder muscle activity and function in common shoulder rehabilitation exercises. Sport Med 2009; 39: 663–685. [DOI] [PubMed] [Google Scholar]
- 44.DiGiovine NM, Jobe FW, Marilyn P, et al. An electromyographic analysis of the upper extremity in pitching. J Shoulder Elbow Surg 1992; 1: 15–25. [DOI] [PubMed] [Google Scholar]
- 45.Uhl TL, Muir TA, Lawson L. Electromyographical assessment of passive, active assistive, and active shoulder rehabilitation exercises. PM R 2010; 2: 132–141. [DOI] [PubMed] [Google Scholar]
- 46.Suprak DN, Bohannon J, Morales G, et al. Scapular kinematics and shoulder elevation in a traditional push-up. J Athl Train 2013; 48: 826–835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lunden JB, Braman JP, Laprade RF, et al. Shoulder kinematics during the push-up plus exercise. J Shoulder Elbow Surg 2010; 19: 216–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Johnson G, Bogduk N, Nowitzke A, et al. Anatomy and actions of the trapezius muscle. Clin Biomech 1994; 9: 44–50. [DOI] [PubMed] [Google Scholar]
- 49.Kibler BW, Sciascia A, Wilkes T. Scapular dyskinesis and its relation to shoulder injury. J Am Acad Orthop Surg 2012; 20: 364–372. [DOI] [PubMed] [Google Scholar]
- 50.Cools AM, Dewitte V, Lanszweert F, et al. Rehabilitation of scapular muscle balance: which exercises to prescribe? Am J Sports Med 2007; 35: 1744–1751. [DOI] [PubMed] [Google Scholar]
- 51.Uhl TL, Carver TJ, Mattacola CG, et al. Shoulder muscle activation during upper extremity weight-bearing exercise. J Orthop Sport Phys Ther 2003; 33: 109–117. [DOI] [PubMed] [Google Scholar]
- 52.Behm D, Colado JC. The effectiveness of resistance training using unstable surfaces and devices for rehabilitation. Int J Sports Phys Ther 2012; 7: 226–241. [PMC free article] [PubMed] [Google Scholar]
- 53.Behm DG, Colado Sanchez JC. Instability resistance training across the exercise continuum. Sports Health 2013; 5: 500–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Karabay D, Emük Y, Özer Kaya D. Muscle activity ratios of scapular stabilizers during closed kinetic chain exercises in healthy shoulders: a systematic review. J Sport Rehabil 2019; 29: 1001–1018. [DOI] [PubMed] [Google Scholar]
- 55.Ebben WP, Wurm B, Vanderzanden TL, et al. Kinetic analysis of several variations of push-ups. J Strength Cond Res 2011; 25: 2891–2894. [DOI] [PubMed] [Google Scholar]
- 56.Giancotti GF, Fusco A, Varalda C, et al. Biomechanical analysis of suspension training push-up. J Strength Cond Res 2018; 32: 602–609. [DOI] [PubMed] [Google Scholar]
- 57.Decker MJ, Hintermeister RA, Faber KJ, et al. Serratus anterior muscle activity during selected rehabilitation exercises. Am J Sports Med 1999; 27: 784–791. [DOI] [PubMed] [Google Scholar]
- 58.Park K-M, Cynn H-S, Kwon O-Y, et al. Comparison of pectoralis major and serratus anterior muscle activities during different push-up plus exercises in subjects with and without scapular winging. J Strength Cond Res 2014; 28: 2546–2551. [DOI] [PubMed] [Google Scholar]
- 59.Simoneau JA, Lortie G, Boulay MR, et al. Skeletal muscle histochemical and biochemical characteristics in sedentary male and female subjects. Can J Physiol Pharmacol 1985; 63: 30–35. [DOI] [PubMed] [Google Scholar]
- 60.Jakobi JM, Haynes EMK, Smart RR. Is there sufficient evidence to explain the cause of sexually dimorphic behaviour in force steadiness? Appl Physiol Nutr Metab 2018; 43: 1207–1214. [DOI] [PubMed] [Google Scholar]
- 61.Hunter SK. Sex differences in human fatigability: mechanisms and insight to physiological responses. Acta Physiol (Oxf) 2014; 210: 768–789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Côté JN. A critical review on physical factors and functional characteristics that may explain a sex/gender difference in work-related neck/shoulder disorders. Ergonomics 2012; 55: 173–182. [DOI] [PubMed] [Google Scholar]
- 63.Enoka RM, Duchateau J. Muscle fatigue: what, why and how it influences muscle function. J Physiol 2008; 586: 11–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.