Abstract
Objectives:
To investigate trends in racial/ethnic differences in nursing home (NH) residents’ quality of life (QoL) and assess these patterns within and between facilities.
Method:
Data include resident-reported QoL surveys (n = 60,093), the Minimum Data Set, and facility-level characteristics (n = 376 facilities) for Minnesota. Hierarchical linear models were estimated to identify differences in QoL by resident race/ethnicity and facility racial/ethnic minority composition for 2011–2015.
Results:
White residents in low-proportion racial/ethnic minority facilities reported higher QoL than both minority and white residents in high-proportion minority facilities. While the year-to-year differences were not statistically significant, the point estimates for white–minority disparity widened over time.
Discussion:
Racial/ethnic differences in QoL are persistent and may be widening over time. The QoL disparity reported by minority residents and all residents in high-proportion minority facilities underscores the importance of examining NH structural characteristics and practices to ultimately achieve the goal of optimal, person-centered care in NHs.
Introduction
Nursing homes (NHs) are integral in the provision of long-term care for a growing population of older adults with complex health needs. The quality of services provided by NHs has been a consistent topic of concern for consumers, governmental agencies, and researchers. Major efforts at the federal and state levels have attempted to improve NH quality through initiatives such as public reporting of quality, pay-for-performance programs, and minimum nursing staff-level requirements (Bowblis, 2011; Unroe et al., 2018). The majority of these efforts have focused on improving quality of care (QoC), which refers to clinical care processes and outcomes (Cai et al., 2011; Castle & Ferguson, 2010; Hefele et al., 2017). Yet, quality of life (QoL) is a valuable aspect of NH quality and is different from QoC. QoL captures the person-reported aspects of resident well-being and experience of care in NHs and is an essential component in promoting person-centered care (Kane et al., 2003). Moreover, the Centers for Medicare and Medicaid Services (CMS) has increased focus on QoL by making regulatory changes which mandate person-centered care in NHs (42 C.F.R. § 483.24, 2016).
At the same time, as this increasing focus on QoL, another trend in the United States is the changing demographics and steady growth in the number of racially and ethnically diverse residents in NHs. Between 1999 and 2008, the number of older Hispanic, Asian, and black residents living in NHs grew by 54.9%, 54.1%, and 10.8%, respectively, while the number of white residents declined 10.2% (Feng et al., 2011). Complicating this growth are the findings that racial/ethnic minority residents (henceforth, “minority residents”) are more likely to be in NHs that are more reliant on Medicaid funding, have lower staffing levels, have more deficiencies in care, and that are more likely to be terminated from the Medicaid program (Mor et al., 2004; Smith et al., 2008). These are all factors associated with relatively worse QoC, and this combination of individual and facility characteristics has led to concerns that this growth in racial/ethnic minority NH residents could intensify already existing racial/ethnic disparities in NH QoC and QoL (Sharma et al., 2019).
Despite the shift in racial/ethnic minority compositions in NHs, there is a scarcity of studies examining the role of race and ethnicity for NH quality. The few existing studies on disparities in NH quality have focused on QoC (Castle & Ferguson, 2010), examining clinical and care process outcomes, and found that minority residents tend to have lower QoC than their non-Hispanic white counterparts (Hefele et al., 2017). Research on QoL is even more limited. For example a study examining facility-level disparities found that there is a positive association between NH deficiencies for QoL domains and minority resident composition (Campbell et al., 2016; Shippee et al., 2016). Another study using resident-reported QoL data found that while minority residents consistently reported lower QoL compared to their white counterparts, NHs with a high proportion of minority residents were more likely to report lower QoL even after controlling for case mix and facility structural and organizational characteristics (Shippee et al., 2016). Although almost all this work uses cross-sectional data, the findings highlight the need to examine the interaction of individual and contextual factors in shaping the racial/ethnic differences in QoL over time.
To further advance our understanding and insight into possible mechanisms for disparities in QoL in NHs, this study uses multiple years of data (2011–2015) to build a longitudinal dataset to examine racial/ethnic differences in QoL over time using a validated measure of resident-reported QoL. In doing so, we are able to document whether QoL trends worsen, increase, or remain persistent for residents of diverse racial/ethnic backgrounds. We also further advance the work on racial/ethnic disparities in QoL by measuring change in QoL over time within facilities via each resident’s racial/ethnic status versus between facilities via a measure for an NH’s racial/ethnic composition and testing the role of the interaction of the two.
Structural Resources, Social Context, and Stages of Addressing Health Disparities
This study draws on the cumulative inequality (CI) theory (Ferraro & Shippee, 2009) and social ecological theory (Stokols, 1992) to better understand the role of race/ethnicity for QoL at both individual and structural levels. The CI theory posits that inequality is structurally generated, and these stratified structures lead to diverse trajectories over the life course. Building on this concept (Ferraro & Shippee, 2009), we hypothesize that racial/ethnic disparities in NH QoL may result from disparate accumulated risks and available resources between older adults of different racial/ethnical groups. The accumulated risks of minority older adults are reflected by lower socioeconomic status and poorer health status which further impact the accessibility of long-term care, their choices of long-term care options, and a variety of health outcomes. Empirical evidence shows that, indeed, individual differences in physical and cognitive function help explain some of the disparity in QoL among NH residents (Shippee et al., 2016). The CI theory further explains that disadvantage increases exposure to risk, but advantage leads to opportunity. Resources such as higher level of education and higher income can provide for different choices of NHs to white residents, while minority residents are exposed to more health risks in selecting less desirable facilities (Ferraro & Shippee, 2009).
The social ecological theory explains how contextual factors, such as cultural, organizational, physical, environmental, and community factors, may influence individual well-being (McLaren & Hawe, 2005; Stokols, 1992; Taplin et al., 2012). Empirical research has indicated contextual factors, such as activity staff level, minority composition, and number of private rooms, are associated with QoL scores (Shippee et al., 2016). However, no study has investigated the interaction between individual and context factors and its influence on disparities in QoL for NH residents. The social ecological theory is useful here because it not only pinpoints the importance of context factors in individual’s well-being but also delineates interrelations between individuals and their environment (particularly the psychosocial or cultural aspect of the environment) in shaping their well-being (McLaren & Hawe, 2005; Stokols, 1992). In this regard, we hypothesized that while resident’s individual minority racial/ethnic identity and percent racial/ethnic minority composition are independently associated with lower QoL, the interaction of these two factors will have a significant association with QoL on its own (e.g. minority residents in high-proportion minority NHs vs. lower proportion minority NHs). This hypothesis is based on research which shows that there may be a benefit for residents to live in an NH with others of similar cultural background due to shared cultural preferences and values (Petrov & Arnold, 2000; Runci, Redman, et al. 2005). In addition, the social ecological view also pertains to the influence of broader contextual factors such as political or societal environment on well-being (Stokols, 1992). This perspective necessitates an examination of changes in the disparities over time as NHs face constantly changing regulatory and payment environments. Therefore, we expected that residents’ QoL and racial/ethnic differences in QoL would not be static over time.
Our analytic approach is informed by Kilbourne’s framework for addressing healthcare disparities: (a) detecting, (b) understanding, and (c) reducing health disparities (Kilbourne et al., 2006). Progress through these three steps can help identify the interventions most likely to be useful for a particular issue. Thus, the first step is to identify how the prevalence of good QoL varies by race/ethnicity. Healthcare organizations, including NHs, must first detect disparities by systematically and accurately identifying the prevalence of racial/ethnic differences to be able to reduce them in the future. To that end, we aim to identify and detect racial/ethnic differences in QoL over time. Second, to understand disparities, it is vital to identify key resident (e.g. mental health status), facility (e.g. payment source), and system-level factors (e.g. racial bias) that affect NH care for minority residents. The long-term goal is to use these findings to influence care delivery for minority NH residents, with special attention to racial/ethnic differences, by providing the evidence necessary to develop a system-level intervention.
Methods
Data
This study combines four data sources from the state of Minnesota from 2011 through 2015: Minnesota Nursing Facility Quality of Life Survey, Minimum Data Set (MDS), Certification and Survey Provider Enhanced Reports (CASPER), and Minnesota Medicaid Cost Reports. Minnesota is one of only two states that routinely collects validated measures of QoL for NH residents and the only one that is currently linkable to the MDS. No other state has the available data to answer the questions of interest of this study.
QoL data on NH residents are obtained from the Minnesota Nursing Facility Quality of Life Survey. The annual survey consists of in-person interviews by an independent survey firm that randomly selects residents from every NH in the state. Therefore, the vast majority of sampled residents are different from year to year. The typical NH has 35 respondents, with a survey rate of about 85% (Vital Research, 2011). MDS is a required assessment of all NH residents upon admission, discharge, and various intervals in between. It contains each resident’s demographic, functional status, and medical conditions. To obtain facility-level characteristics, we used CASPER data, which are CMS-mandated inspections of NHs that are conducted by state inspectors on a regulator basis, and the Minnesota Medicaid Cost Reports which are annual reports submitted to the state contain numerous financial and NH characteristics.
In constructing our analytic sample that has a unit of analysis of a resident QoL survey, we linked the QoL survey to each NH respondent’s closest assessment in the MDS. We then merged in the CASPER and Medicaid Cost Report data corresponding to the year of the QoL survey. The final sample size for the regressions with no additional covariates includes 60,093 surveys from 376 NHs. When controls are included, the most restricted sample has 59,035 surveys from 375 NHs. By year, the number of surveys included in the most comprehensive regression ranges from 10,834 in 2015 to 12,466 in 2011.
Quality of Life Measures
In the Minnesota QoL survey, residents are asked a series of questions that map into six QoL domains: environmental adaptations, attention (from staff), food enjoyment, engagement (meaningful relationships and activities), positive mood, and lack of negative mood (Shippee et al., 2015). To calculate a QoL summary score, we first calculated domain scores by taking the mean of all questions answered in the domain. We then defined the QoL summary score as the unweighted average of each domain score. To make the summary score easier to interpret, it is standardized to percentage points (i.e. 0–100), with higher values indicating a respondent reported having higher QoL. The Minnesota QoL survey and its domains have demonstrated strong psychometric properties in prior research (Kane et al., 2004; Shippee et al., 2015).
Race/Ethnicity and High-Proportion Minority Facilities
To understand how a resident’s race/ethnicity and the facility minority composition impact QoL, we construct two sets of key variables: race/ethnicity of the respondent and the racial/ethnic minority composition of the facility the respondent lives in. The race/ethnicity of the respondent is an indicator variable for self-reported race/ethnicity and whether a resident is a member of a racial/ethnic minority group (aggregated due to small sample size). MDS reports whether a resident is white, Black, Hispanic, Native American, Asian American, other, or missing. Given the small number of minority NH residents in Minnesota, we created an indicator variable that aggregates residents into non-Hispanic white and minority, excluding residents with missing data on race/ethnicity. In sensitivity analyses, we examined differences by individual racial/ethnic group, and the directions of association were all unchanged for those in the minority group versus white respondents.
We used 100% of the MDS data from Minnesota each year to calculate the annual racial/ethnic minority composition of each NH, as measured by the proportion of minority residents. An indicator variable was constructed for whether the facility was a relatively high-proportion or low-proportion racial/ethnic minority facility (henceforth referred to as “high-minority” and “low-minority” facilities). Since the threshold for what is considered a relatively high-minority composition varies across states, we defined a facility as high minority if it was above the 90th percentile in the state of Minnesota for proportion of minority residents within the NH. For Minnesota, the 90th percentile facility had a minority composition of over 14% of nonwhite residents. Using this definition, high-minority facilities had an average of 25.8% minority residents, and low-minority facilities comprised 1.59% of minority residents on average in 2011. We conducted a number of sensitivity analyses to test for different thresholds to define high-minority facilities, in addition to treating the percent of minority residents as a continuous variable with linear and quadratic terms. None of these sensitivity analyses substantively changed our findings.
Control Variables
We identify a number of resident- and facility-level characteristics that are associated with QoL. Resident-level characteristics are from the MDS and include age, gender, length of stay, activities of daily living score (ADL, range 0–28), and a count of chronic conditions (i.e. congestive heart failure, diabetes, hip fracture, paralysis, pressure ulcers, and stroke). We separately created flags for severe mental illness (SMI, defined as a diagnosis of bipolar disorder, schizophrenia, or other psychotic disorders), behavioral symptoms, dementia diagnosis, and moderate or severe impairment to cognitive performance. Cognitive performance was obtained from the MDS Brief Interview for Mental Status if the resident can respond or the Cognitive Performance Scale if they cannot (Thomas et al., 2017).
Facility characteristics are obtained from CASPER or Medicaid Cost Reports and include geographic location (i.e. Twin Cities metropolitan area, other metropolitan area, micropolitan area, or rural), ownership (i.e. nonprofit, for profit, or government), affiliation with a chain, number of beds, occupancy rate, facility-level acuity (Minnesota Department of Health, 2015), and payer mix. We also included a number of staffing variables. Staffing levels, in hours per resident day, are calculated for registered nurses, licensed practical nurses, certified nursing assistants, activities staff, social workers, and mental health workers. We also included the retention rate for all NH staff and an indicator variable for whether the NHs had a high use of temporary staff from employment agencies. The cutoff used for the high use of temporary staff was the 99th percentile (or 11.1% of all staff hours) for the entire sample.
Analytical Approach
To examine whether there were racial/ethnic disparities in QoL over time, we compare summary statistics for non-Hispanic white (henceforth referred to as “white”) and minority residents. Next, we implement a set of linear mixed-effects models where the dependent variable was the QoL summary score for each respondent. To capture the disparity, we divided NH residents into four groups based on their race/ethnicity and facility minority composition: (1) white, low-minority facility, (2) white, high-minority facility, (3) minority, low-minority facility, and (4) minority, high-minority facility. For all our analyses, we use the first group, white residents in low-minority facilities, as a reference group. To account for variation in time, we also include indicator variable for each year and interact these year indicators with the four groups. By doing this, we are able to identify the average QoL score for respondents in each group in each year.
We consider three specifications for our linear mixed-effects regression models. The first model does not include any additional control variables to calculate unadjusted QoL scores. The second model includes resident-level controls to determine whether the measured disparities are different after accounting for differences in resident characteristics. Finally, a model that includes both resident- and facility-level controls. All regression models are estimated using Stata 13/MP (StataCorp, 2013) and also include a normally distributed random intercept for each facility to account for between-facility heterogeneity and standard errors account for heteroscedasticity. We also fitted GEE models with independence correlation structure, and it did not qualitatively change the results (not shown).
Results
Descriptive Statistics
Table 1 reports descriptive statistics and tests that compare white and minority respondents in 2011 and 2015. QoL summary scores for white respondents were stable at about 80 points but declined for minority respondents from 75.9 points in 2011 to 73.7 points in 2015. More importantly, minority respondents reported lower average QoL in both years. Nearly 9% of white respondents were in high-minority facilities. In comparison, 64.0% of minority respondents were in high-minority facilities in 2011 compared to 57.9% in 2015.
Table 1.
Sample by Race/Ethnicity for 2011 and 2015.
| 2011 |
2015 |
|||
|---|---|---|---|---|
| White Resident | Minority Resident | White Resident | Minority Resident | |
| Key variables | ||||
| Quality of life summary score | 80.324 | 75.893 | 80.015 | 73.691 |
| High-minority facility (%) | 9.047 | 63.975 | 8.723 | 57.948 |
| Resident-level characteristics | ||||
| Age (years) | 82.898 | 67.615 | 83.118 | 69.592 |
| Activities of daily living score long-form scale (0–28) | 14.251 | 10.996 | 14.670 | 12.409 |
| Length of stay (years) | 1.741 | 2.199 | 2.623 | 3.175 |
| Married | 22.305% | 12.422% | 21.195% | 11.398% |
| Count of chronic conditions (0–5) | .799 | .983 | .699 | .834 |
| Depression diagnosis (%) | 52.760 | 48.240 | 50.399 | 46.233 |
| Anxiety diagnosis (%) | 23.508 | 17.805 | 25.031 | 18.353 |
| Moderate or severe cognitive impairment (%) | 31.835 | 28.986 | 29.460 | 29.913 |
| Dementia diagnosis (%) | 43.957 | 38.095 | 46.694 | 39.291 |
| Serious mental illness diagnosis (%) | 14.292 | 24.224 | 13.288 | 27.457 |
| Behavioral symptoms (%) | 21.099 | 32.505 | 15.619 | 22.721 |
| Facility-level characteristics | ||||
| Location | ||||
| Twin Cities (%) | 37.894 | 74.741 | 37.733 | 80.202 |
| Other metro (%) | 18.585 | 5.797 | 18.824 | 3.902 |
| Micropolitan (%) | 21.199 | 12.008 | 20.191 | 9.682 |
| Rural (%) | 22.322 | 7.453 | 23.252 | 6.214 |
| Ownership | ||||
| Nonprofit (%) | 64.786 | 49.275 | 63.577 | 38.728 |
| For profit (%) | 26.309 | 47.412 | 28.752 | 54.046 |
| Government (%) | 8.906 | 3.313 | 7.671 | 7.225 |
| Chain affiliation (%) | 54.856 | 50.932 | 54.012 | 53.468 |
| Minnesota acuity index | 1.046 | 1.010 | 1.015 | .979 |
| Number of beds | 92.266 | 104.959 | 88.923 | 123.409 |
| Occupancy (%) | 90.040 | 88.805 | 88.228 | 87.604 |
| Medicare resident days (%) | 8.977 | 6.749 | 9.027 | 7.404 |
| Medicaid resident days (%) | 56.701 | 70.922 | 54.056 | 65.756 |
| Staffing levels (hours per resident day) | ||||
| Registered nurse | .488 | .561 | .541 | .603 |
| Licensed practical nurse | .722 | .725 | .692 | .693 |
| Certified nursing assistant | 2.204 | 1.859 | 2.168 | 1.856 |
| Activities | .242 | .211 | .253 | .204 |
| Social service and mental health staff | .118 | .143 | .124 | .191 |
| All staff retention rate (%) | 72.179 | 74.511 | 67.443 | 66.018 |
| High use of temporary staff (%) | .499 | .207 | 2.162 | 5.058 |
| N | 12,015 | 483 | 10,455 | 692 |
The table reports the means for key variables, resident-level characteristics, and facility-level characteristics for 2011 and 2015 for white and racial/ethnic minority residents.
While there were some changes in resident- and facility-level characteristics from 2011 to 2015, the general pattern between white and minority respondents was consistent over time. Minority respondents were on average younger, had shorter lengths of stays, and had more chronic conditions. Minority respondents were also less likely to have age-associated cognitive decline (e.g. dementia) and mental health condition (depression) but were more likely to have serious mental illness and behavioral symptoms. In terms of facility characteristics, minority respondents were more likely to be in larger for-profit NHs in the Twin Cities metropolitan area.
Regression Results
The linear mixed-effects regression results adjusting for varying levels of control variables are reported in Table 2. Most resident-level controls were found to significantly predict QoL. The direction of the effects and statistical significance of resident-level controls was generally similar whether or not facility-level controls were included. Respondents who were older, had longer lengths of stay, and had better physical functional status reported higher QoL. Respondents in smaller, nonprofit facilities located in rural areas reported higher QoL. Interestingly, higher nursing staff level had no statistically significant effect on QoL, but NHs with more activities staff, social service/mental health staff, and those with higher staff retention rates reported higher QoL scores.
Table 2.
Racial/Ethnic Disparities in Quality of Life Summary Scores: Hierarchical Linear Model Results.
| Unadjusted |
Resident Covariates |
Resident and Facility Covariates |
||||
|---|---|---|---|---|---|---|
| b | se | b | se | b | se | |
| Key explanatory variables | ||||||
| Group (reference = white, low-minority facility) | ||||||
| White, high-minority facility | −4.077*** | 1.013 | −4.172*** | .85 | −2.282** | .779 |
| Minority, low-minority facility | −2.624* | 1.323 | −2.409 | 1.323 | −2.105 | 1.300 |
| Minority, high-minority facility | −5.420*** | 1.294 | −5.732*** | 1.303 | −4.033** | 1.298 |
| Year (reference = 2011) | ||||||
| 2012 | −.296 | .204 | −.322 | .199 | −.308 | .204 |
| 2013 | .293 | .226 | .266 | .223 | .314 | .225 |
| 2014 | .022 | .246 | −.549* | .247 | −.426 | .244 |
| 2015 | −.311 | .257 | −.593* | .251 | −.480 | .252 |
| Group–year interactions | ||||||
| White, high-minority facility # 2012 | −.558 | .760 | −.552 | .732 | −.435 | .745 |
| White, high-minority facility # 2013 | −1.436 | .765 | −1.147 | .668 | −1.150 | .663 |
| White, high-minority facility # 2014 | −1.534 | .877 | −1.338 | .856 | −1.481 | .855 |
| White, high-minority facility # 2015 | −.758 | .963 | −1.129 | .905 | −1.006 | .849 |
| Minority, low-minority facility # 2012 | −1.795 | 1.977 | −2.004 | 1.901 | −1.804 | 1.886 |
| Minority, low-minority facility # 2013 | −1.081 | 1.944 | −.606 | 1.911 | −.568 | 1.885 |
| Minority, low-minority facility # 2014 | −.741 | 1.718 | −.596 | 1.757 | −.455 | 1.732 |
| Minority, low-minority facility # 2015 | −1.954 | 1.654 | −2.050 | 1.667 | −1.741 | 1.640 |
| Minority, high-minority facility # 2012 | .353 | 1.466 | .350 | 1.460 | .353 | 1.449 |
| Minority, high-minority facility # 2013 | −1.553 | 1.383 | −1.390 | 1.377 | −1.376 | 1.420 |
| Minority, high-minority facility # 2014 | −1.292 | 1.500 | −1.270 | 1.444 | −1.418 | 1.448 |
| Minority, high-minority facility # 2015 | −1.602 | 1.421 | −1.686 | 1.471 | −1.455 | 1.390 |
| Resident-level characteristics | ||||||
| Age (years) | .057*** | .010 | .047*** | .010 | ||
| Activities of daily living score long-form scale (0–28) | −.415*** | .013 | −.404*** | .012 | ||
| Length of stay (years) | .309*** | .034 | .299*** | .034 | ||
| Married | .173 | .192 | .111 | .191 | ||
| Count of chronic conditions (0–5) | −.540*** | .100 | .527*** | .099 | ||
| Depression diagnosis | −2.479*** | .162 | −2.470*** | .161 | ||
| Anxiety diagnosis | −1.699*** | .193 | −1.710*** | .194 | ||
| Moderate or severe cognitive impairment | 1.840*** | .198 | 1.790*** | .197 | ||
| Dementia diagnosis | 1.370*** | .178 | 1.504*** | .179 | ||
| Serious mental illness diagnosis | −1.355*** | .286 | −1.210*** | .286 | ||
| Behavioral symptoms | −2.675*** | .227 | −2.748*** | .222 | ||
| Facility-level characteristics | ||||||
| Location (reference = Twin Cities) | ||||||
| Other metro | 1.349*** | .372 | ||||
| Micropolitan | 1.585*** | .381 | ||||
| Rural | 2.514*** | .377 | ||||
| Ownership (reference = nonprofit) | ||||||
| For profit | −1.359*** | .361 | ||||
| Government | .412 | .433 | ||||
| Chain affiliation | −.127 | .273 | ||||
| Minnesota acuity index | −1.676 | 1.542 | ||||
| Number of beds, each 10 | −.130*** | .029 | ||||
| Occupancy, each 10 percentage points | .575*** | .153 | ||||
| Proportion of Medicare resident days, each 10 percentage points | .162 | .279 | ||||
| Proportion of Medicaid resident days, each 10 percentage points | −.200 | .131 | ||||
| Staffing levels (hours per resident day) | ||||||
| Registered nurse | .151 | .474 | ||||
| Licensed practical nurse | .518 | .641 | ||||
| Certified nursing assistant | −.159 | .336 | ||||
| Activities | 4.040** | 1.289 | ||||
| Social service and mental health staff | 3.622* | 1.806 | ||||
| High use of temporary staff | 1.568* | .631 | ||||
| All staff retention rate, each 10 percentage points | .389*** | .099 | ||||
| Random intercept variance | 10.381 | 8.365 | 5.033 | |||
| Residual variance | 231.829 | 219.203 | 219.203 | |||
| Intraclass correlation | .043 | .037 | .022 | |||
| Number of surveys | 60,903 | 59,103 | 59,035 | |||
| Number of NFs | 376 | 376 | 375 | |||
The table reports the coefficient estimates and standard errors from nested random intercept regression models where the dependent variable is a quality of life summary score. The key variables are indicators for whether the resident is a minority interacted with whether they reside in a high-minority facility. We also fitted GEE models with independence correlation structure, and it did not qualitatively change the results (not shown).
p < .01,
p < .05,
p < .10.
Given the complexity of interpreting the interaction terms, reporting the disparity across the four groups and across time is difficult. Therefore, Table 3 reports the size of the disparity in each year relative to white respondents in low-minority facilities. Relative to this group, minority respondents in high-minority facilities had unadjusted QoL scores that were 4.1–5.6 points lower, minority respondents in low-minority facilities had unadjusted QoL scores that were 2.6–4.6 points lower, and minority respondents in high-minority facilities had the largest disparity (5.1–7.0 points). Adjusting for individual covariates did not appreciably reduce the disparity, but including facility characteristics results in narrowing of the disparity. For white respondents in high-minority facilities, the size of the disparity ranged from 2.3 to 3.7 points relative to white residents in low-minority facilities when resident- and facility-level controls were included in the model. This is a reduction of 32–44%. Minorities also experienced narrowing of reported disparities, but the declines were smaller in magnitude. For example the disparity for minority respondents in low-minority facilities declined by 16–28%, and minority respondents in high-minority facilities declined by 19–27%.
Table 3.
Disparity in Quality of Life Relative to a White Resident in a Low-Minority Facility.
| Unadjusted | Resident Covariates | Resident and Facility Covariates | |
|---|---|---|---|
| White resident in high-minority facility | |||
| 2011 | −4.077*** | −4.172*** | −2.282*** |
| 2012 | −4.635*** | −4.724*** | −2.717*** |
| 2013 | −5.513*** | −5.319*** | −3.432*** |
| 2014 | −5.611*** | −5.509*** | −3.764*** |
| 2015 | −4.835*** | −5.300*** | −3.288*** |
| Minority resident in low-minority facility | |||
| 2011 | −2.624* | −2.409* | −2.105 |
| 2012 | −4419*** | −4.414*** | −3.908*** |
| 2013 | −3.705*** | −3.016** | −2.673* |
| 2014 | −3.366** | −3.005** | −2.559* |
| 2015 | −4.578*** | −4.459*** | −3.846*** |
| Minority resident in high-minority facilit | |||
| 2011 | −5.420*** | −5.732*** | −4.033*** |
| 2012 | −5.066*** | −5.382*** | −3.680*** |
| 2013 | −6.973*** | −7.122*** | −5.410*** |
| 2014 | −6.711*** | −7.003*** | −5.451*** |
| 2015 | 7.022*** | −7.418*** | −5.488*** |
The table reports the disparity by year for each group listed relative to white residents in a low-minority facility. The disparity and corresponding standard errors for statistical tests were calculated using the regression results from Table 2. Each column reports the disparity with varying number of controls, starting from no additional controls, resident-level controls, and the fully controlled model which includes resident- and facility-level controls.
p < .01,
p < .05,
p < .10.
To visualize these disparities over time, Figure 1 shows the predicted mean QoL score holding all covariates at the overall sample mean for each race/ethnicity, facility minority composition, and year. Overall, the QoL did not significantly change for white residents in low-minority facilities over time. Regardless of which additional covariates are included in the model, mean QoL scores are declining over time for minority respondents, regardless if they are in a low- or high-minority facility. This finding is an indication that the disparity is increasing over time. However, almost all the interaction terms with year are not statistically significant in Table 2.
Figure 1.
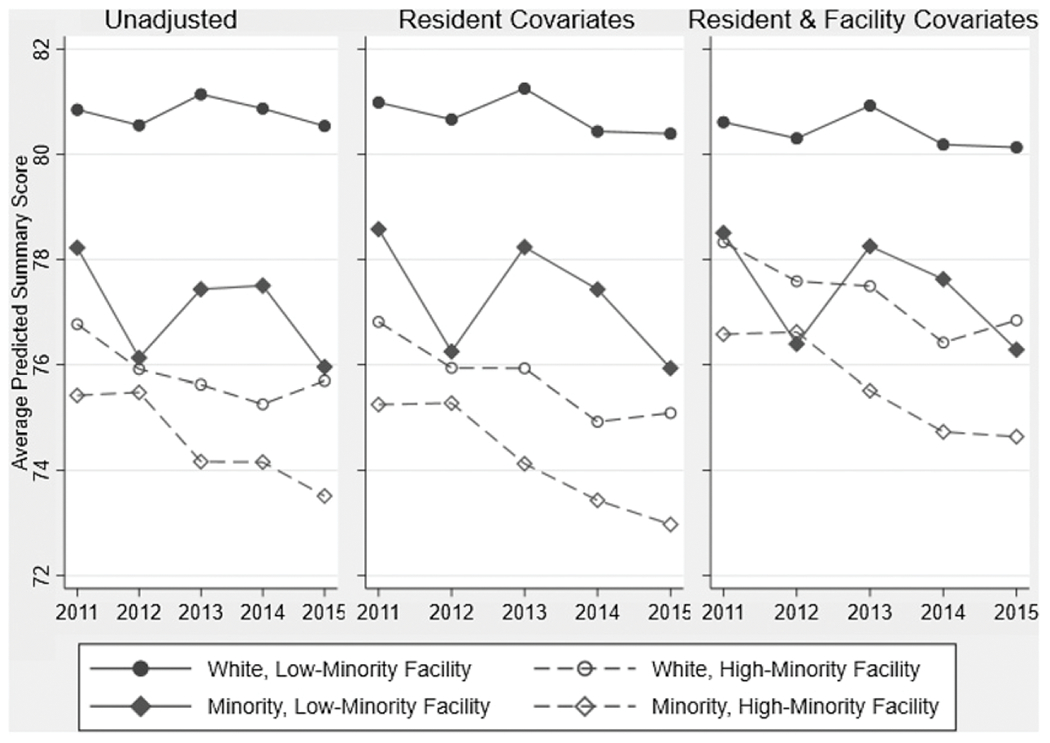
Predicted mean summary scores by race, facility minority composition, and year.
Note. The figure reports predicted mean quality of life scores which hold all covariates except race, facility composition, and year at the overall sample mean and random effects at zero using the regression as reported in Table 2.
Discussion
As the United States has become more ethnically and racially diverse, so have America’s NHs. This makes understanding and monitoring of racial and ethnic disparities in the NH setting all the more important. While existing work has established the existence of racial/ethnic disparities (Campbell et al., 2016; Shippee et al. 2016), many of these studies have been cross-sectional and rely on only one year of data. This is the first article to use a multisource longitudinal dataset that provides us with the ability to examine the trends in racial/ethnic disparities in QoL over time.
We find facility characteristics are importantly related to white and minority NH residents’ QoL. White residents tend to be more traditional NH residents—older, with dementia, and greater needs in terms of ADLs. In contrast, minority residents tend to be younger, have SMI, and have fewer ADL deficits. This is changing, as minority residents had significant increases in the ADL acuity levels over the study period. Minority residents are more likely to live in for-profit NHs that have fewer activities staff, use more temporary staff, and are located in the most urban areas of the state. All of these are consistent with minority residents being more likely to reside in NHs that have characteristics known to be associated with lower QoC and QoL (Mor et al., 2004). Examination of trends over time showed that the frequency of these factors is increasing. For example NHs that made frequent use of temporary staff, which create the potential for the lack of consistent care—a factor known to be associated with lower quality (Bowblis, 2011)—were classified as having a high proportion of minority residents 15.4% of the time, versus 9.9% of facilities which did not have high temporary staff use.
We found that the unadjusted QoL scores indicate the existence of a disparity between white and minority residents. For the average white NH resident, QoL score was stable between 2011–2015, with a mean score of just over 80 (out of possible 100). Over this same period, minority residents saw a decline in QoL from 75.9 to 73.7. These results clearly indicate the existence of a disparity in 2011, but more importantly, that the disparity was larger by 2015. Moreover, some non-US research has suggested that there may be a benefit for residents to live in an NH with others of similar cultural background (Petrov & Arnold, 2000; Runci, O’Connor, et al., 2005). If this applied to our setting, we would expect that minority residents in facilities with a greater composition of racial/ethnic minorities to have relatively higher QoL scores than minorities in NHs with a low proportion of minority residents. We find that this is not the case for racial/ethnic minority NH residents in our study and in fact, facilities with a high proportion of minority residents have a negative association with QoL for both minority and white residents.
This difference in findings is likely due to racial segregation of long-term care in the Unites States, one of the most racially segregated sectors of health care (Rahman & Foster, 2014). System-level disparities in where care can be received and what services are available have resulted in worse outcomes for older adults from minority communities and indigenous people (Mack et al., 2020; Smith et al., 2008) that are not attenuated by greater racial/ethnic diversity of residents in the facility. Moreover, the United States has great diversity within and across minority communities, in terms of cultural, religious preferences, and other factors. Thus, it would be more meaningful to examine not only overall racial/ethnic diversity at the facility but specific presence of those from one’s cultural group. The NHs themselves contribute to this picture, as racial and ethnic minorities reside in facilities with characteristics associated with poorer QoL (e.g. activities staffing, larger size, and for-profit status).
Our study was informed by the CI theory (Ferraro et al., 2009) and social ecological theory (Stokols, 1992) to better understand the interaction between individual and context factors for racial disparities in NH residents’ QoL. Our findings show that individual’s minority race/ethnicity placed them at a systemic disadvantage for receiving higher quality of life in NHs and facility characteristics, such as the use of temporary staff and reliance on Medicaid reflected these disparities. Our finding that racial/ethnic disparity has increased over time speaks to the need of applying Kilbourne’s stages of addressing health disparities to this work. The first stage is to identify how the prevalence of good QoL varies by race/ethnicity and trends over time. Indeed, accurately identifying the prevalence of racial/ethnic differences is the first step necessary to identify the need for system-level response. Second, we aimed to understand the role of individual and facility factors in these disparities, by examining key resident and facility factors that affect NH care for minority residents. We hope that the findings from this work can lay the foundation for the third stage to ultimately impact policy in Minnesota but also in other states to improve outcomes for minority NH residents.
Indeed, as per Kilbourne’s stages, we should not stop at the first two steps because we need to ultimately progress to stage three, which includes a policy response if these disparities are to be reversed. Efforts such as public reporting of quality (Konetzka & Werner, 2009) will help families and policy makers alike recognize under-resourced facilities that may not be able to provide high-quality care. States will also have to consider whether Medicaid payment levels are sufficient to meet the varied needs of contemporary NH residents. Minnesota’s Eliminating Health Disparities Initiative is an example of a state effort to address racial/ethnic disparities in NH quality. The program provides grants to programs designed to improve outcomes for populations of color and American Indians. While appealing, thus far, these efforts, in which QoL is not a priority area, do not seem to have been effective in addressing disparities in NH residents’ QoL. Finally, both states and the federal government have a role in setting Medicaid policies and broader regulations. Thus, policies focusing on increasing NH quality should focus on addressing the needs of racial/ethnic minority residents.
Our study has many strengths, and the most notable one is the use of a validated, resident-reported measure of QoL that can be linked with MDS to study the racial/ethnic disparities within and between NHs. However, there are some weaknesses we must also acknowledge. We do not know how residents chose their NH residences, or how much information residents have regarding the QoL in the NHs prior to admission, or whether there are other factors that are of sufficient importance to the resident to offset QoL or QoC concerns. While proximity and quality are important factors in NH choice, recent work has found that minority residents are willing to seek care at a facility with residents that better reflect their respective community, even if closer NHs have better clinical quality (Rahman & Foster, 2014).
Finally, the racial and ethnic composition of Minnesota does not allow us to have enough power to study specific racial and ethnic groups, and therefore, associations observed in Minnesota may not apply to other states with different demographic compositions. Yet, it is also likely that findings about racial/ethnic disparities are transferable to other states because Minnesota has a more generous nursing home payment policy (Medicaid equalization rate). In spite of these limitations, we feel the strengths of our study outweigh any limitations.
In conclusion, our study identified racial and ethnic disparities in NH residents’ QoL and that the gap has been increasing over time. While this trend is occurring in all NHs, our study highlights the particular role of NHs serving a high proportion of minority residents, as residents in these facilities report worse QoL among all ethnic and racial groups, including white residents. The government has many policy tools available to help reduce disparities, such as overall payment rates and quality improvement bonus payments, mandated staffing level, public quality reporting, and educating consumers. Yet, as a society, if we want to address these issues, we need to tailor policies to the specific needs of minority communities. This study has documented the issue and potential target—NHs with a high proportion of minority resident—but not all these facilities are the same. Given the diversity of minority population, eliminating disparities in NHs is unlikely to come from a one-size-fits-all policy. New policies and resources are needed in order to achieve equitable QoL in long-term care that are culturally sensitive and are based on the needs and input of the communities that these policies are meant to help.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: National Institute on Minority Health and Health Disparities (5R01MD010729-04).
Appendix A
Table A1.
Summary Statistics by Race/Ethnicity.
| White | Black/African American | American Indian/Alaska Native | All Others | p-Value for Difference | |
|---|---|---|---|---|---|
| Key variables | |||||
| Quality of life summary score | 80.015 | 72.935 | 74.435 | 75.155 | <.001 |
| High-minority facility | 8.723% | 64.337% | 50.820% | 46.452% | <.001 |
| Resident-level characteristics | |||||
| Age (years) | 83.118 | 68.624 | 69.115 | 72.561 | <.001 |
| Activities of daily living score long-form scale (0–28) | 14.670 | 13.039 | 11.770 | 11.226 | <.001 |
| Length of stay (years) | 2.623 | 2.897 | 3.338 | 3.790 | <.001 |
| Married | 21.195% | 8.437% | 8.696% | 22.143% | <.001 |
| Count of chronic conditions (0–5) | .699 | .795 | .926 | .865 | <.001 |
| Depression diagnosis | 50.399% | 43.243% | 52.542% | 49.342% | .040 |
| Anxiety diagnosis | 25.031% | 14.699% | 22.951% | 24.516% | <.001 |
| Moderate or severe cognitive impairment | 29.460% | 30.602% | 30.328% | 27.742% | .91 |
| Dementia diagnosis | 46.694% | 41.523% | 37.288% | 34.868% | .001 |
| Serious mental illness diagnosis | 13.288% | 28.434% | 21.311% | 29.677% | <.001 |
| Behavioral symptoms | 15.619% | 21.446% | 27.049% | 22.727% | <.001 |
| Facility-level characteristics | |||||
| Location | |||||
| Twin Cities | 37.733% | 96.145% | 30.328% | 76.774% | <.001 |
| Other metro | 18.824% | 1.687% | 9.016% | 5.806% | |
| Micropolitan | 20.191% | 2.169% | 36.885% | 8.387% | |
| Rural | 23.252% | .000% | 23.770% | 9.032% | |
| Ownership | |||||
| Nonprofit | 63.577% | 40.241% | 28.689% | 42.581% | <.001 |
| For profit | 28.752% | 57.590% | 40.984% | 54.839% | |
| Government | 7.671% | 2.169% | 30.328% | 2.581% | |
| Chain affiliation | 54.012% | 58.554% | 40.984% | 49.677% | .005 |
| Minnesota acuity index | 1.015 | .996 | .960 | .948 | <.001 |
| Number of beds | 88.923 | 138.761 | 83.451 | 113.755 | <.001 |
| Occupancy | 88.228% | 88.417% | 82.020% | 89.830% | <.001 |
| Medicare resident days | 9.027% | 7.667% | 6.384% | 7.504% | <.001 |
| Medicaid resident days | 54.056% | 65.642% | 71.318% | 61.490% | <.001 |
| Staffing levels (hours per resident day) | |||||
| Registered nurse | .541 | .652 | .463 | .582 | <.001 |
| Licensed practical nurse | .692 | .694 | .756 | .640 | <.001 |
| Certified nursing assistant | 2.168 | 1.884 | 1.952 | 1.706 | <.001 |
| Activities | .253 | .180 | .293 | .200 | <.001 |
| Social service and mental health staff | .124 | .202 | .130 | .209 | <.001 |
| All staff retention rate | 67.443% | 67.480% | 58.267% | 67.423% | <.001 |
| High use of temporary staff | 2.162% | .000% | 24.590% | 3.226% | <.001 |
| N | 10,455 | 415 | 122 | 155 |
Footnotes
Declaration of Conflicting Interests
John R. Bowblis provides litigation consulting services to the health care industry, which has included long-term care providers. All other author(s) declared no conflicts of interest with respect to research, authorship, and/or publciation of this article.
References
- 42 C.F.R. § 483.24. (2016). State operations manual, Appendix PP - Guidance to surveyors for long term care facilities” (hereinafter “CMS guidance”). Available at: http://www.cms.gov/RegulationsandGuidance/Guidance/Manuals/downloads/som107ap_pp_guidelines_ltcf.pdf
- Bowblis JR (2011). Staffing ratios and quality: An analysis of minimum direct care staffing requirements for nursing homes. Health Services Research, 46(5), 1495–1516. doi: 10.1111/j.1475-6773.2011.01274.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai S, Feng Z, Fennell ML, & Mor V (2011). Despite small improvement, black nursing home residents remain less likely than whites to receive flu vaccine. Health Affairs, 30(10), 1939–1946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell LJ, Cai X, Gao S, & Li Y (2016). Racial/ethnic disparities in nursing home quality of life deficiencies, 2001 to 2011. Gerontology and Geriatric Medicine, 2, 233372141665356. doi: 10.1177/2333721416653561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castle NG, & Ferguson JC (2010). What is nursing home quality and how is it measured? The Gerontologist, 50(4), 426–442. doi: 10.1093/geront/gnq052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng Z, Fennell ML, Tyler DA, Clark M, & Mor V (2011). Growth of racial and ethnic minorities in US nursing homes driven by demographics and possible disparities in options. Health Affairs, 30(7), 1358–1365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferraro KF, & Shippee TP (2009). Aging and cumulative inequality: How does inequality get under the skin? The Gerontologist, 49(3), 333–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferraro KF, Shippee TP, & Schafer MH (2009). Cumulative inequality theory for aging and the life course. In Bengston VL, Silverstein M, Putney NM,& Gans D (Eds.), Handbook of theories of aging (pp. 413–434). New York: Springer Publishing Company. [Google Scholar]
- Hefele JG, Ritter GA, Bishop CE, Acevedo A, Ramos C, Nsiah-Jefferson LA, & Katz G (2017). Examining racial and ethnic differences in nursing home quality. The Joint Commission Journal on Quality and Patient Safety, 43(11), 554–564. doi: 10.1016/j.jcjq.2017.06.003 [DOI] [PubMed] [Google Scholar]
- Kane RA, Kane RL, Bershadsky B, Cutler LJ, Giles K, Liu J, & Degenholtz HB (2004). Measures, indicators, and improvement of quality of life in nursing homes: Final report. http://www.hpm.umn.edu/ltcresourcecenter/research/QOL/Final_Report_to_CMS_Volume_1.pdf
- Kane RA, Kling KC, Bershadsky B, Kane RL, Giles K, Degenholtz HB, & Cutler LJ (2003). Quality of life measures for nursing home residents. The Journals Of Gerontology. Series A, Biological Sciences And Medical Sciences, 58(3), 240–248. [DOI] [PubMed] [Google Scholar]
- Kilbourne AM, Switzer G, Hyman K, Crowley-Matoka M, & Fine MJ (2006). Advancing health disparities research within the health care system: A conceptual framework. American Journal of Public Health, 96(12), 2113–2121. doi: 10.2105/AJPH.2005.077628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konetzka RT, & Werner RM (2009). Review: Disparities in long-term care. Medical Care Research and Review, 66(5), 491–521. [DOI] [PubMed] [Google Scholar]
- Mack DS, Jesdale BM, Ulbricht CM, Forrester SN, Michener PS, & Lapane KL 2020. Racial segregation across U.S. nursing homes: A systematic review of measurement and outcomes. The Gerontologist, 60. e218–e231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaren L, & Hawe P (2005). Ecological perspectives in health research. Journal of Epidemiology & Community Health, 59(1), 6–14. doi: 10.1136/jech.2003.018044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minnesota Department of Health. (2015). Case mix classification manual for nursing facilities. Saint Paul, MN: Minnesota Department of Health. http://www.health.state.mn.us/divs/fpc/profinfo/cms/cmrmanual.pdf. [Google Scholar]
- Mor V, Zinn J, Angelelli J, Teno JM, & Miller SC (2004). Driven to tiers: Socioeconomic and racial disparities in the quality of nursing home care. The Milbank Quarterly, 82(2), 227–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petrov L, & Arnold L (2000). Special needs, special wants. Australasian Journal on Ageing, 19(1), 43–44. doi: 10.1111/j.1741-6612.2000.tb00138.x [DOI] [Google Scholar]
- Rahman M, & Foster AD (2015). Racial segregation and quality of care disparity in US nursing homes. Journal of Health Economics, 39, 1–16. doi: 10.1016/j.jhealeco.2014.09.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Runci SJ, O’Connor DW, & Redman JR (2005). Language needs and service provision for older persons from culturally and linguistically diverse backgrounds in south-east Melbourne residential care facilities. Australasian Journal on Ageing, 24(3), 157–161. doi: 10.1111/j.1741-6612.2005.00106.x [DOI] [Google Scholar]
- Runci SJ, Redman JR, & O’Connor DW (2005). Language use of older Italian-background persons with dementia in mainstream and ethno-specific residential care. International Psychogeriatrics, 17(4), 699–708. doi: 10.1017/S1041610205002309 [DOI] [PubMed] [Google Scholar]
- Sharma H, Perraillon MC, Werner RM, Grabowski DC, Konetzka RT (2019). Medicaid and nursing home choice: Why do duals end up in low-quality facilities? Journal of Applied Gerontology, doi: 10.1177/0733464819838447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shippee TP, Henning-Smith C, Kane RL, & Lewis T (2015). Resident- and facility-level predictors of quality of life in long-term care. The Gerontologist, 55(4), 645–655. doi: 10.1093/geront/gnt148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shippee TP, Henning-Smith C, Rhee GT, Held RN, & Kane RL (2016). Racial differences in Minnesota nursing home residents’ quality of life: The importance of looking beyond individual predictors. Journal of aging and health, 28, 199–224. [DOI] [PubMed] [Google Scholar]
- Smith DB, Feng Z, Fennell ML, Zinn J, & Mor V (2008). Racial disparities in access to long-term care: The illusive pursuit of equity. Journal of Health Politics, Policy and Law, 33(5), 861–881. [DOI] [PubMed] [Google Scholar]
- StataCorp. 2013. Stata Statistical Software: Release 13. Stata-Corp LP. [Google Scholar]
- Stokols D (1992). Establishing and maintaining healthy environments: Toward a social ecology of health promotion. American Psychologist, 47(1), 6–22. doi: 10.1037/0003-066X.47.1.6 [DOI] [PubMed] [Google Scholar]
- Taplin SH, Anhang Price R, Edwards HM, Foster MK, Breslau ES, Chollette V, Prabhu Das I, Clauser SB, Fennell ML, & Zapka J 2012). Introduction: Understanding and influencing multilevel factors across the cancer care continuum. JNCI Monographs, 2012(44), 2–10. doi: 10.1093/jncimonographs/lgs008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas KS, Dosa D, Wysocki A, & Mor V (2017). The minimum data set 3.0 cognitive function scale. Medical Care, 55(9), e68–e72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Unroe KT, Ouslander JG, & Saliba D (2018). Nursing home regulations redefined: Implications for providers. Journal of the American Geriatrics Society, 66(1), 191–194. [DOI] [PubMed] [Google Scholar]
- Vital Research (2011). Implementation of the 2010 consumer satisfaction and quality of life survey in Minnesota nursing homes and satisfaction survey of family members of residents in Minnesota nursing homes: final report (Prepared for the Minnesota Department of Human Services). Los Angeles, CA: Vital Research. [Google Scholar]


