Abstract
Context:
Given the high prevalence of burdensome symptoms in palliative care (PC) and increasing use of complementary and integrative medicine (CIM) therapies, research is needed to determine how often and what types of CIM therapies providers recommend to manage symptoms in PC.
Objective:
To document recommendation rates of CIM for target symptoms and assess if CIM use varies by provider characteristics.
Methods:
Nationwide survey of physicians (MD and DO), physician assistants, and nurse practitioners in PC.
Results:
Participants (N=404) were mostly female (71.3%), physicians (74.9%), and cared for adults (90.4%). Providers recommended CIM an average of 6.82 times per-month (95% CI: 6.04–7.60) and used an average of 5.13 (95% CI: 4.90–5.36) out of 10 CIM modalities. Respondents recommended mind-body medicines (e.g., meditation, biofeedback) most, followed by massage, and acupuncture/acupressure. The most targeted symptoms included pain; followed by anxiety, mood disturbance and distress. Recommendation frequencies for specific modality-for-symptom combinations ranged from little use (e.g., aromatherapy for constipation) to occasional use (e.g., mind-body interventions for psychiatric symptoms). Finally, recommendation rates increased as a function of pediatric practice, non-inpatient practice setting, provider age, and proportion of effort spent delivering palliative care.
Conclusion:
To the best of our knowledge, this is the first national survey to characterize PC providers’ CIM recommendation behaviors and assess specific therapies and common target symptoms. Providers recommended a broad range of CIM but do so less frequently than patients report using CIM. These findings should be of interest to any provider caring for patients with serious illness.
Keywords: complementary, integrative, alternative, nationwide survey, usage patterns, recommendation rates
Introduction
As the burden of prevalent symptoms in patients with serious illness is better recognized (1–4), palliative care continues to grow in an effort to address these needs (5,6). Symptoms such as pain, dyspnea, and nausea are common, contribute to significant distress, and negatively impact the quality of life of affected patients and their families (7). Americans increasingly use complementary and integrative medicine (CIM) modalities such as acupuncture, mind-body practices (e.g., meditation), and supplements alongside conventional medicines to address physical, psychosocial, and spiritual aspects of their health (8–10), a holistic goal similar to that of palliative care (5). Indeed, a growing body of evidence suggests that CIM can contribute to enhanced management of symptoms that are commonly encountered in the palliative care setting, such as pain, psychological symptoms, and sleep disturbance (11–18).
While patient use of CIM has been extensively researched (9,19,20), few studies have examined palliative care providers’ recommendation patterns regarding CIM use (21). In addition to studies of non-palliative-care providers (22–31), prior research has focused on palliative and end-of-life institutional rather than individual provider prescribing practices (32–35), specific geographic regions (26,33–36), the use of one or a few CIM modalities (31,37–39), or a few symptoms or a single disease at a time (29,37,39–41). To the best of our knowledge, there have been no U.S.-based studies that assembled a nationally representative sample of palliative care providers and assessed their recommendation patterns regarding the use of CIM therapies, nor the symptoms targeted in palliative care (21).
To address this knowledge gap, we surveyed physicians, physician assistants (PA), and advanced-practice nurses (NP) nationwide to document their CIM practice patterns and assess for differences in use based on providers’ demographic and practice characteristics.
Methods
Participants and Recruitment
This study was approved by the Weill Cornell Medicine Institutional Review Board. The target population included allopathic (MD) and osteopathic (DO) physicians and allied health professionals (i.e., PA and NP) who deliver palliative care to adults, children, or both in the United States. We focused on these 3 provider groups based on their ability to prescribe pharmacologic therapies. We first obtained a geographically representative random sample (the proportion of the invited participants from each U.S. census region matched that of the population of hospice and palliative care physicians in the U.S.) of MD/DO physicians, PAs, and NPs working in palliative care from IQVIA (42), a health information company that supplies healthcare provider contact information using multiple databases. We developed a second database of palliative care providers de novo, by searching the websites of the 5 largest institutions providing palliative care in each of the 50 states (as determined by hospital bed count) to identify publicly available email addresses. All providers identified by both sampling frames were invited to participate prior to collection of further information that determined their eligibility. After combining and de-duplicating addresses from the 2 sampling frames, we emailed 4,155 providers. No incentive was provided. After the initial email (day 0), we sent 3 reminders to non-responders and partial responders at days 10, 21, and 28. The survey was conducted in January-February 2021.
Eligibility Criteria and Method Used to Determine Eligibility
We assessed eligibility status by asking prospective participants whether they held an eligible professional degree (MD, DO, PA, or NP) and if any of their professional effort was spent delivering palliative care (yes/no). Of 442 providers who answered these 2 questions, 423 met eligibility criteria. Of these, 301 (71%) completed the survey and an additional 103 (24%) provided partial responses, yielding an analytic sample of 404. We closed the survey on day 46 after reaching an a priori quota of 300 complete responses. We achieved a response rate of 10.1%. The analytic sample size (depending on the model) ranged from 300 for multivariable analyses to 404 for univariate analyses.
Data Collection
We asked participants about the proportion of their effort devoted to delivering palliative care and the frequency with which they recommend CIM, irrespective of the specific type of therapy, to patients receiving palliative care. We collected data on respondents’ age, gender, race, ethnicity, years of experience in palliative care, professional degree, practice setting (e.g., hospice, academic center, outpatient clinic, etc.), state/territory in which they practiced, patient population density (i.e., urban, suburban, rural), and patient population served (i.e., adults, pediatrics, both).
We asked respondents to select any of the following 10 CIM therapies: 1) acupuncture / acupressure; 2) alternative medical systems (Ayurveda, traditional medicine, healers, Traditional Chinese Medicine, homeopathy, naturopathy, folk medicine); 3) chiropractic or osteopathic medicine; 4) massage; 5) yoga, tai-chi, or qigong; 6) mind-body interventions (meditation, relaxation, breathing, hypnosis, biofeedback); 7) natural products (non-vitamin, non-mineral dietary supplements); 8) nutrition or special diets; 9) creative arts therapies (art, dance, music); 10) aromatherapy that they had ever recommended to address: 1) pain; 2) nausea/vomiting; 3) constipation; 4) dyspnea; 5) anxiety, mood disturbance, and/or distress; or 6) sleep disturbance. We developed the list of CIM modalities based on prior surveys and systematic reviews of CIM (21–41), and in consultation with integrative medicine specialists. We chose the 6 symptoms based on their prevalence and burden, as well as on expert opinion (2–4). Then, for each of the 10 CIM modalities providers indicated they had recommended (either in the past or currently), we asked them to identify the symptoms targeted, e.g., aromatherapy for nausea/vomiting, massage for pain (Appendix 1). As the survey asked about the use of each of the 10 modalities to treat each of the 6 symptoms, respondents were able to select from 60 distinct clinical scenarios. For each of these 60 modality-for-symptom scenarios, participants who had recommended that modality for that symptom (e.g., natural products for constipation), were asked to estimate the frequency of making the recommendation using a 5-item Likert scale where responses ranged from “no longer recommend but have in the past” to “always.” We piloted the survey on a convenience sample of providers (N=12) and made adjustments based on their feedback.
Variable Construction
We converted providers’ responses to the question about the frequency with which they recommend any CIM to patients (where response choices included never, less than once per month, several times a month, several times a week, and daily) to a quantitative variable coded as 0, 0.5, 5, 12, or 30 times per-month, respectively. We called this variable “frequency per month.”
From the list of CIM 10 modalities, participants were asked to select each therapy they had ever recommended in the past or were currently recommending to address any of the 6 symptoms. Using these data, we calculated the total number of unique modalities recommended per respondent (out of 10) and called this variable “usage index.” Finally, providers who indicated that they used a given therapy to address a specific symptom (e.g., mind-body interventions for sleep disturbance) were asked to provide the frequency of making this recommendation. This question was asked for each modality-for-symptom combination, i.e., up to a maximum of 60 times. Each respondent was asked the question for the subset of the 60 clinical scenarios they had used in the past or were currently using (Appendix 1). This variable had scores ranging from 0 (don’t currently recommend) to 4 (always recommend this modality when managing this symptom). Respondents who did not indicate that they had recommended a given modality-for-symptom combination (e.g., massage for pain) were recoded as 0. We called this variable “frequency-of-modality-for-symptomrecommendation.” In addition to examining this variable at the level of each of the 60 combinations, we also calculated frequencies of recommendation averaged across symptoms (i.e., average use of a particular modality to treat the 6 target symptoms), averaged across modalities (i.e., average use of the 10 modalities to treat a specific target symptom), and averaged across both modalities and symptoms (i.e., average use of the 10 modalities to treat the 6 symptoms).
Statistical Models
We examined means, variances, and ranges for all variables. We examined usage index and frequency-per-month as dependent variables in general linear models that included an a priori set of provider characteristics based on the literature and our previous research. These independent variables included gender, race/ethnicity, academic degree, the patient population (adult vs. peds vs. both, with the first and third combined to give a 2-level variable), the relative urban-nature of their practice (urban vs. suburban vs. rural), and the U.S. census region in which they practice as fixed classification factors; and participant age, years of experience in palliative care, and the percent of professional effort in palliative care as covariates (quantitative variables).
We examined the frequency-of-modality-for-symptom-recommendation outcome as a dependent variable in a general linear mixed model with repeated measures on symptom and modality. The core model included symptom (6 levels) and modality (10 levels) as fixed classification factors, the interaction of those 2 factors, and individuals (the providers) as levels of a random classification factor. A second model included additionally the same set of a priori fixed classification factors and covariate variables described in the preceding paragraph. These models provided unadjusted and adjusted estimates of mean frequency of recommendation for the 60 modality-for-symptom combinations. In these models, for covariates we specified overall regressions, resulting in an estimated frequency across all 60 modality-for-symptom combinations.
We examined interactions of each of the provider characteristics with symptom and modality. In the case of the covariates, this involved estimating the regressions of frequency-of-modality-for-symptom-recommendation on, for example, age specified separately by symptom and (in a separate model) by modality and testing the homogeneity of those regressions. No model that included interactions added coherence to the results, and they are not presented. Analyses were carried out using software from SAS Version 9.4 (43). Results reported in the text are those significant at a P level of .05 in a 2-sided test.
Results
Participant Characteristics
Table 1 shows that most participants (N=303) were female (71.3%), non-Hispanic-or-Latinx White (78.9%), physicians (74.9%), and provided care to adult patients (90.4%).
Table 1.
Characteristics of Study Samplea
| Percentage | ||
|---|---|---|
| Age | ||
| < = 30 years old | 2.6% | |
| 31–40 years old | 27.1% | |
| 41–50 years old | 30.0% | |
| 51–60 years old | 23.8% | |
| 60+ years old | 16.5% | |
| Gender | ||
| Female | 71.3% | |
| Male | 28.4% | |
| Other | 0.3% | |
| Race and Ethnicityb | ||
| White, Not Hispanic or Latino | 78.9% | |
| Asian | 13.2% | |
| Other | 7.9% | |
| Professional Degree | ||
| MD | 67.0% | |
| NP | 23.1% | |
| DO | 7.9% | |
| PA | 2.0% | |
| Years of Experience in Palliative Care | ||
| < 2 years | 10.2% | |
| 2–5 years | 22.8% | |
| 6–10 years | 25.1% | |
| 11–20 years | 24.8% | |
| >20 years | 17.2% | |
| Proportion of Effort in Palliative Care | ||
| 100% | 51.2% | |
| 75–99% | 13.6% | |
| 50–74% | 10.4% | |
| 25–49% | 10.4% | |
| 10–24% | 10.9% | |
| < 10% | 3.5% | |
| Patient Population | ||
| Adults | 90.4% | |
| Pediatrics | 5.3% | |
| Both | 4.3% | |
| Practice Settingc | ||
| Inpatient Academic Medical Center | 43.2% | |
| Outpatient Clinic | 42.9% | |
| Inpatient Community Hospital | 37.0% | |
| Hospice | 29.4% | |
| Long-Term Care | 13.9% | |
| Outpatient Private Office | 5.9% | |
| U.S. Census Region (N=301) | ||
| Northeast | 27.2% | |
| Midwest | 27.2% | |
| South | 26.9% | |
| West | 18.6% | |
| Patient Population Density | ||
| Urban | 55.4% | |
| Suburban | 32.7% | |
| Rural | 11.9% | |
N=303 for each category unless otherwise specified.
2 questions about race and ethnicity were used to construct a single race/ethnicity characteristic
Respondents could select multiple settings.
Univariate Analysis
Providers recommended any CIM, irrespective of therapy, an average of 6.82 times per-month (95% CI: 6.04–7.60, N=404) and had used an average of 5.13 (95% CI: 4.90–5.36, N=394) out of the 10 modalities examined. We estimated participants’ recommendation patterns regarding use of the 10 therapies to mitigate any of the 6 symptoms. Table 2 shows the results for each of these 60 modality-for-symptom combinations (e.g., massage for pain). The table entries represent an average frequency of recommendation that ranges from 0 (don’t currently recommend) to 4 (always recommend this modality when managing this symptom). Figure 1 shows the same data in a heatmap form. The frequency of recommendation averaged across all 60 modality-for-symptom combinations was 0.39 (95% CI: 0.38–0.40, N=22902).
Table 2.
Frequency of Recommending CIM Modalities for the Management of Specific Palliative Care Symptoms
| Psychiatric | GI | ||||||
|---|---|---|---|---|---|---|---|
| Pain | Dyspnea | Anxiety, Mood and/or Distress | Sleep Disturbance | Nausea and Vomiting | Constipation | ||
| Alternative Medical System | Alternative Medical Systems (Ayurveda, Traditional Medicine, Healers, Traditional Chinese Medicine, Homeopathy, Naturopathy, Folk Medicine) | 0.24 | 0.05 | 0.20 | 0.16 | 0.18 | 0.11 |
| Mind-Body | Meditation, Relaxation, Hypnosis, or Biofeedback | 1.43 | 0.85 | 1.73 | 1.38 | 0.57 | 0.04 |
| Yoga, Tai Chi, or Qigong | 0.65 | 0.10 | 0.73 | 0.45 | 0.03 | 0.08 | |
| Creative Arts Therapies (art, dance, music) | 0.60 | 0.23 | 0.90 | 0.40 | 0.14 | 0.02 | |
| Aromatherapy | 0.27 | 0.08 | 0.57 | 0.47 | 0.59 | 0.02 | |
| Biologically-Based | Natural Products (non-vitamin, non-mineral dietary supplements) | 0.30 | 0.07 | 0.29 | 0.51 | 0.38 | 0.40 |
| Nutrition or Special Diets | 0.11 | 0.02 | 0.11 | 0.14 | 0.48 | 0.63 | |
| Manipulative/Body-Based | Acupuncture / Acupressure | 1.13 | 0.12 | 0.52 | 0.26 | 0.66 | 0.12 |
| Massage | 1.48 | 0.04 | 1.08 | 0.57 | 0.09 | 0.13 | |
| Chiropractic or Osteopathic Medicine | 0.59 | 0.02 | 0.07 | 0.02 | 0.03 | 0.08 | |
Results of a mixed model, unadjusted for covariates. Entries in each cell represent average frequency of recommendation from 0 (don’t currently recommend) to 4 (always recommend this modality when managing this symptom). Cell sizes range from 353 to 393 due to missing data.
Figure 1. Frequency of Recommending CIM Modalities for the Management of Specific Palliative Care Symptoms.
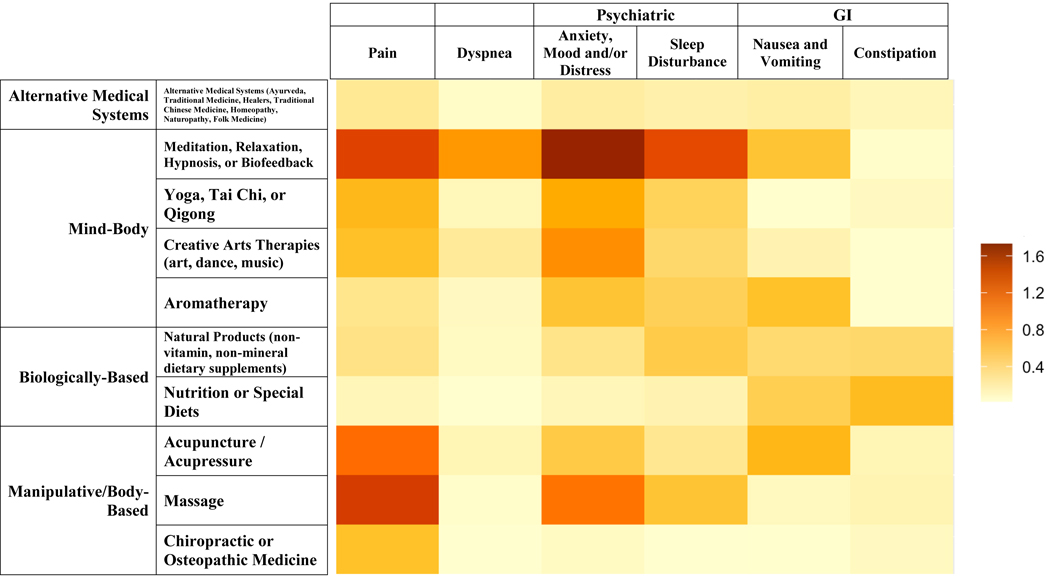
Results of a mixed model, unadjusted for covariates. Entries in each cell represent average frequency of recommendation from 0 (don’t currently recommend) to 4 (always recommend this modality when managing this symptom). Cell sizes range from 353 to 393 due to missing data.
We examined recommendation patterns of specific modalities regardless of symptom addressed and use of any modality for managing each symptom. The results represent an average frequency of recommendation ranging from 0 (don’t currently recommend) to 4 (always recommend this modality when managing this symptom). The most frequently employed treatments were mind-body medicines (1.00), massage (0.56), and acupuncture/acupressure (0.47), while the least frequently recommended were alternative medical systems (0.16) and chiropractic or osteopathic medicine (0.13). Symptoms most frequently addressed with CIM included pain (0.68) and psychological sequelae including anxiety, mood disturbance, and distress (0.62), while the least frequently addressed was dyspnea (0.16).
Frequencies of use for specific modality-for-symptom combinations ranged from little use (e.g., aromatherapy for constipation [0.02]), to occasional use (e.g., mind-body interventions for psychiatric symptoms [1.73]).
Primary Analyses
We investigated correlates of the frequency-per-month variable (Table 3). Female respondents recommended any CIM 27% more often than male providers (p=0.045), while providers of pediatric-only palliative care recommended any CIM 100% more often than adult-only or both adult and pediatric providers (p=0.006). Finally, providers working in outpatient-only settings recommended any CIM 135% more often than inpatientonly providers (p<0.001), 100% more often than providers in hospice-only settings (p=0.002), 240% more often than long-term-care-only providers (p<0.001), and 90% more often than providers working in multiple settings (p<0.001). There were no significant associations between the recommendation frequency-per-month variable and provider race and ethnicity, degree, census region, age, years of experience, or proportion of effort in palliative care.
Table 3.
Results of General Linear Mixed Models for Primary Outcomes
| Provider Characteristic | Frequency-Per-Month (Recommendations/Month) | Usage Index (No. Modalities Recommended) | Frequency of Modalityfor-Symptom Recommendation (Recommendation Score) | ||||
|---|---|---|---|---|---|---|---|
| Estimate | P-Value | Estimate | P-Value | Estimate | P-Value | ||
| Gender | Male | 7.19 | 0.0447 | 5.77 | 0.1455 | 0.49 | 0.1114 |
| Female | 9.15 | 6.18 | 0.56 | ||||
|
Race and
Ethnicity |
Non-Hispanic-or-Latinx White |
7.65 | 0.7728 | 5.91 | 0.8145 | 0.49 | 0.4226 |
| Asian | 8.51 | 5.83 | 0.57 | ||||
| Other | 8.33 | 6.18 | 0.50 | ||||
|
Professional
Degree |
PA or NP | 8.74 | 0.7597 | 5.54 | 0.1198 | 0.56 | 0.3593 |
| MD | 7.92 | 5.76 | 0.48 | ||||
| DO | 7.83 | 6.62 | 0.53 | ||||
|
Patient
Population |
Pediatrics Only | 12.25 | 0.0059 | 7.19 | 0.0152 | 0.72 | 0.0057 |
| Any Adults | 6.13 | 5.37 | 0.42 | ||||
|
Patient
Population Density |
Urban | 9.10 | 0.1170 | 6.10 | 0.7069 | 0.53 | 0.3044 |
| Suburban | 7.06 | 6.07 | 0.57 | ||||
| Rural | 8.34 | 5.76 | 0.47 | ||||
|
U.S. Census
Region |
Northeast | 7.95 | 0.7216 | 5.75 | 0.0620 | 0.49 | 0.2500 |
| Midwest | 7.46 | 5.84 | 0.50 | ||||
| South | 8.41 | 5.68 | 0.51 | ||||
| West | 8.84 | 6.63 | 0.60 | ||||
| Practice Setting | Hospice Only | 7.43 | <.0001 | 7.10 | 0.0002 | 0.61 | 0.0268 |
| Long-Term Care Only | 4.37 | 5.39 | 0.35 | ||||
| Inpatient Only | 6.34 | 5.00 | 0.46 | ||||
| Outpatient Only | 14.87 | 6.77 | 0.64 | ||||
| Mixed | 7.82 | 5.62 | 0.56 | ||||
| Coefficient | P-Value | Coefficient | P-Value | Coefficient |
P-
Value |
||
| Provider Age | 0.42 | 0.4176 | 0.37 | 0.0160 | 0.05 | 0.0268 | |
| Years of Experience in Palliative Care | 0.28 | 0.5310 | 0.13 | 0.3333 | 0.00 | 0.8668 | |
| Proportion of Professional Effort in Palliative | 1.00 | 0.0011 | 0.30 | 0.0009 | 0.03 | 0.0323 | |
| Care | |||||||
Results of a mixed model, adjusted for covariates. Rows show provider characteristics (independent variables), and columns show study outcomes. The first 7 provider characteristics are classification factors; estimated least-squared means are shown for each level for of each outcome with the significance for each variable. The final 3 provider characteristics are covariates, and the estimates of regressions of each outcome on the covariates are given. Original categories were retained for categorical sociodemographic and clinical variables (Table 1) except for collapsing or excluding as follows: given a low count in the Other gender category (N=1), this individual was not used in multivariable analyses; professional degree was collapsed into MD, DO, and PA/NP providers; the patient population variable was collapsed into pediatrics-only and any-adult-patients; and practice setting was collapsed into hospice-only, long-term care-only, inpatient-only, outpatient-only, or mixed. In the first column, least-squared means represent the number of times per-month that providers recommended any CIM modality to patients receiving palliative care. In the second column, least-squared means represent the number of unique CIM modalities that providers had ever recommended to palliative care patients. In the final column, least-squared means represent average frequency-of-recommendation of the 10 CIM modalities for the 6 palliative care symptoms, ranging from 0 (don’t currently recommend) to 4 (always recommend this modality when managing this symptom). For all outcomes, N=300.
Respondent characteristics associated with the usage index variable appear in Table 3. DO physicians used 20% more CIM therapies than PAs/NPs (p=0.043). Providers of pediatric-only palliative care used 34% more unique modalities compared to adult-only or both adult and pediatric providers (p=0.005). Participants in the Western U.S. census region used 15% more CIM modalities than those in the Northeast (p=0.021), 14% more modalities than those in the Midwest (p=0.038), and 17% more modalities than those in the South (p=0.014). Palliative care providers working solely in the hospice setting recommended 42% more modalities than those working only in inpatient settings (p=0.001), and 26% more modalities than providers working in multiple settings (p=0.018). Respondent age was positively associated with the number of unique modalities recommended (p=0.016) as was the proportion of their effort in palliative care (p<0.001). Other independent variables, including participant gender, race/ethnicity, and years of experience in palliative care, were not associated with this variable.
Finally, we examined factors associated with the frequency-of-modality-for-symptom-recommendation variable (Table 3). Providers treating only pediatric patients recommended CIM in these 60 clinical scenarios 140% more frequently than providers seeing adults in any capacity (p=0.003). Providers working only in the outpatient setting used the 10 modalities for managing the 6 symptoms 83% more often than those working only in long-term care facilities (p=0.041) and 37% more often than those working only in inpatient settings (p=0.011). Finally, provider age was positively associated with this variable (p=0.027), as was the proportion of effort spent delivering palliative care (p=0.032).
Discussion
To the best of our knowledge, this is the first national survey to characterize palliative care providers’ practice patterns related to the use of complementary and integrative medicine, as well as the first to assess the types of CIM therapies they recommend for the management of common and morbid symptoms in the palliative care setting (21). Providers reported recommending any CIM approximately 7 times a month and used, on average, half of the 10 CIM modalities examined in this study, principally recommending mind-body medicines to manage pain, psychiatric symptoms, and sleep disturbance. We also identified pediatric practice, outpatient practice, provider age, and proportion of effort spent delivering palliative care as factors independently associated with study outcomes of 1) frequency-per-month, 2) usage index, and 3) frequency of modality-forsymptom recommendation. These results serve as a baseline that future studies can use to assess for change in CIM recommendation behaviors over time.
Our major findings should be of interest to all providers caring for patients with advanced illness, a significant proportion of whom likely use CIM. We found that providers, on average, had recommended over 50% of the modalities included in the study, demonstrating recommendation behaviors that reflect use of a broad range of CIM modalities, corresponding with prior studies of non-palliative care providers. For example, one survey found rheumatologists had used 36% of the included modalities (23), and another showed generalists had recommended 47% of the suggested therapies (22). However, we found providers only recommended CIM twice-weekly, on average, while studies have shown that 5%−95% of these patients use CIM therapies, depending on the illness/target symptom, phase of illness, and CIM modality (44–49). This difference suggests that patients (not providers) may be initiating CIM use in this setting. Common barriers to providers employing CIM include perceived lack of evidence or clinical benefit, poor cost-effectiveness, limited access, and lack of familiarity with modalities and indications (21). Data from this study will provide the basis for future work assessing how often CIM recommendations are provider- vs. patient-initiated, whether recommendation rates of particular modalities differ from previously reported rates in other provider groups, as well as correlations between common barriers and recommendation rates of specific modalities. Additionally, future studies should examine where in the line-of-treatment these modalities fall, i.e., are they being used in an integrative manner alongside conventional therapies, or in an alternative fashion solely when customary methods for managing symptoms do not provide the desired results. It will also be important to discern how behaviors correlate with current safety and efficacy data, and current insurance coverage practices given the coverage of some but not all efficacious modalities. Finally, future research should expand the types of providers studied to include other multi-disciplinary team members (e.g., social work, chaplaincy) who are also likely to recommend use of CIM.
Our study sheds light on the modalities employed and types of symptoms targeted by palliative care providers. Providers employed mind-body interventions nearly twice as often as the next two most common modalities (acupuncture and massage), a finding that deviates from studies of non-palliative care providers (22,23,25,30,50). Factors that may explain the greater use of mind-body interventions for symptom management in palliative care include the high prevalence of psychological symptoms experienced by patients receiving palliative care (51), and ease of delivery (e.g., not requiring a licensed provider or self-administered digitally [52,53]) to patients with advanced illness. Future research is needed to investigate motivations behind provider recommendation of mind-body medicines and expand on existing efficacy studies to include head-to-head comparisons between these modalities and conventional treatments for symptom management.
Our study further documents that pain and psychological sequelae of advanced illness, including anxiety, mood disturbance, and distress, as well as sleep disturbance are symptoms palliative care providers target most using CIM modalities. These findings align with patient-reported symptoms from which they most often seek relief with CIM (19,54). Given concerns about misuse of opioids in palliative care populations (55), research is also needed to investigate whether CIM use has an opioid-sparing effect. All healthcare providers, irrespective of specialty, caring for patients in this stage of illness should be aware of these common modalities and target symptoms, as their patients may be using CIM alongside conventional therapies.
We also demonstrated significant practice variation regarding CIM use as a function of providers’ demographic and practice characteristics. Pediatric providers reported greater use of CIM relative to those caring for adults only. Our results contrast with prior studies that demonstrate pediatricians recommend CIM less than adult providers (22,50). These studies examined primary care pediatricians seeing healthy children and their families, while our study likely captured behaviors of palliative care providers caring for a chronically ill population (44, 56,57). Prior research has also shown that female physicians are more likely to recommend CIM (50), whereas we did not find a gender association for two of our three outcomes. We also found that increased age correlated with an increased rate of recommending CIM, contrasting with prior research showing increased CIM use among younger providers across specialty and practice settings (23,50,58). We suspect these contrasts in age and gender associations are due to greater homogeneity in CIM behaviors among palliative care providers compared to non-palliative-care specialties. Increased use among outpatient and hospice providers suggests that future research should examine how patient illness severity and access and availability to CIM affect provider recommendation behavior.
CIM uptake continues to expand among patients (9,16,19), particularly in populations with advanced illness (45,59). This trend may reflect efforts on the part of patients with advanced illness to achieve symptom management (53), especially given limited access to palliative care services (60). It may also reflect patient distrust of customary methods of symptom management (e.g., use of opioids) in the palliative care setting (61–63). However, we show that provider recommendations of CIM in the palliative care setting fall significantly below patient-reported prevalence of use (44–49). The overall low frequency of recommendation also suggests the need to examine whether perceived lack of evidence related to CIM efficacy and lack of familiarity constitute barriers to the recommendation of CIM. Our findings support the need to study existing CIM education paradigms within palliative care institutions, and to assess providers’ sources of information on CIM. The disagreement in provider recommendation and patient-reported use rates support routine screening by all providers for CIM use in patients with advanced illness to assess modalities used, symptoms targeted, motivations for use, and perceived efficacy in managing symptoms. Future research should ascertain the frequency with which providers across different specialties recommend CIM modalities to mitigate burdensome symptoms among patients with advanced illness and to compare these patterns to those of palliative care providers, and to the use of conventional therapies. These future directions can enhance the safe and efficacious use of CIM by patients, as can improved communication with patients about their use and increased knowledge of the growing evidence surrounding CIM efficacy and safety as compiled by the National Institutes of Health (64).
This study has several limitations. The response rate was low (~10%) raising concerns about selection bias in the absence of a known list of all multidisciplinary palliative care providers, making it difficult to assess the size of the target population. Further, we do not have data to characterize non-responders to compare their demographics to those of responders; we acknowledge the limitations of reaching out to palliative care physicians, physician assistants, and nurse practitioners during the COVID-19 pandemic. Our focus on providers with prescribing ability limits the ability to capture behaviors of other key palliative-care team members that often make recommendations regarding the use of various CIM, including social workers, chaplains, and nurses. There are also many more CIM modalities than the 10 included in this survey, and more symptoms that palliative care providers likely address with CIM than the 6 we examined. Finally, as with any survey, we relied on participant self-report and cannot verify the accuracy of the data reported in the current study. One of our variables of interest is the frequency with which the providers recommend any CIM to patients. This was asked about using a 1–5 scale and not directly on the basis of number of times per month (or other timeframe). We made a transformation of the original scale to put the variable on the more interpretable scale of times per month; the transformation is, of course, only approximate but does not alter results from the results when the original scale (1–5) is used.
Conclusions
We identified the CIM modalities palliative care providers recommend and symptoms most frequently targeted, as well as the provider characteristics associated with these outcomes. We document this current use against which future survey data can be compared. These findings should be of interest to any provider caring for patients with serious illness as well as those receiving palliative care.
Supplementary Material
Key Message.
This is the first national survey assessing palliative care providers’ recommendation patterns regarding complementary and integrative medicine (CIM) to manage symptoms. Providers recommend a broad range of CIM twice per-week, varying by patient age, practice setting, and provider age. Provider recommendation rates appear modest compared to patient-reported use.
Acknowledgements
We thank our 12 survey pilot participants, all of whom are clinical faculty in the Weill Cornell Medicine Joan and Sanford I. Weill Department of Medicine, for their thoughtful contribution to our survey design; members of the Weill Cornell Medicine Division of Geriatrics and Palliative Medicine for their input on our data analysis and thoughtful comments on earlier drafts of this manuscript; and Patricia Kim, MSW, for her guidance and organizational support throughout this study. Anurag Goel conducted this research as part of the Areas of Concentration (AOC) Program of the Weill Cornell Medicine MD Program curriculum.
Funding
MCR is supported by grants from the National Institute on Aging [K24AGO53462, P30AG022845]
Footnotes
Disclosure
The authors declare no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Bookbinder M, McHugh ME. Symptom Management in Palliative Care and End of Life Care. Nursing Clinics of North America. 2010;45(3):271–327. doi: 10.1016/j.cnur.2010.04.002 [DOI] [PubMed] [Google Scholar]
- 2.Glare P, Miller J, Nikolova T, Tickoo R. Treating nausea and vomiting in palliative care: a review. Clin Interv Aging. 2011;6:243–259. doi: 10.2147/CIA.S13109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mercadante S, Adile C, Ferrera P, Masedu F, Valenti M, Aielli F. Sleep disturbances in advanced cancer patients admitted to a supportive/palliative care unit. Support Care Cancer. 2017;25(4):1301–1306. doi: 10.1007/s00520-016-3524-4 [DOI] [PubMed] [Google Scholar]
- 4.Moens K, Higginson IJ, Harding R, et al. Are There Differences in the Prevalence of Palliative Care-Related Problems in People Living With Advanced Cancer and Eight Non-Cancer Conditions? A Systematic Review. Journal of Pain and Symptom Management. 2014;48(4):660–677. doi: 10.1016/j.jpainsymman.2013.11.009 [DOI] [PubMed] [Google Scholar]
- 5.Center to Advance Palliative Care. America’s Care of Serious Illness: 2019 State-by-State Report Care on Access to Palliative Care in our Nation’s Hospitals. Palliative Care, Report Card. Accessed July 2, 2020. https://reportcard.capc.org/
- 6.National Hospice and Palliative Care Organization. NHPCO’s Facts & Figures on Hospice Care in America. NHPCO. Accessed May 26, 2020. https://www.nhpco.org/factsfigures/ [Google Scholar]
- 7.Blinderman CD, Billings JA. Comfort Care for Patients Dying in the Hospital. N Engl J Med. 2015;373(26):2549–2561. doi: 10.1056/NEJMra1411746 [DOI] [PubMed] [Google Scholar]
- 8.Astin JA. Why patients use alternative medicine: results of a national study. JAMA. 1998;279(19):1548–1553. doi: 10.1001/jama.279.19.1548 [DOI] [PubMed] [Google Scholar]
- 9.Clarke TC, Black LI, Stussman BJ, Barnes PM, Nahin RL. Trends in the use of complementary health approaches among adults: United States, 2002–2012. Natl Health Stat Report. 2015;(79):1–16. [PMC free article] [PubMed] [Google Scholar]
- 10.Mbizo J, Okafor A, Sutton MA, Leyva B, Stone LM, Olaku O. Complementary and alternative medicine use among persons with multiple chronic conditions: results from the 2012 National Health Interview Survey. BMC Complement Altern Med. 2018;18(1):281. doi: 10.1186/s12906-018-2342-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Aalbers S, Fusar-Poli L, Freeman RE, et al. Music therapy for depression. Cochrane Database Syst Rev. 2017;11:CD004517. doi: 10.1002/14651858.CD004517.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cramer H, Lauche R, Klose P, Lange S, Langhorst J, Dobos GJ. Yoga for improving health-related quality of life, mental health and cancerrelated symptoms in women diagnosed with breast cancer. Cochrane Database Syst Rev. 2017;1:CD010802. doi: 10.1002/14651858.CD010802.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goyal M, Singh S, Sibinga EMS, et al. Meditation programs for psychological stress and well-being: a systematic review and meta-analysis. JAMA Intern Med. 2014;174(3):357–368. doi: 10.1001/jamainternmed.2013.13018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lin Y-C, Wan L, Jamison RN. Using Integrative Medicine in Pain Management: An Evaluation of Current Evidence. Anesth Analg. 2017;125(6):2081–2093. doi: 10.1213/ANE.0000000000002579 [DOI] [PubMed] [Google Scholar]
- 15.Linde K, Kriston L, Rücker G, et al. Efficacy and acceptability of pharmacological treatments for depressive disorders in primary care: systematic review and network meta-analysis. Ann Fam Med. 2015;13(1):69–79. doi: 10.1370/afm.1687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nahin RL, Barnes PM, Stussman BJ. Expenditures on Complementary Health Approaches: United States, 2012. Natl Health Stat Report. 2016;(95):1–11. [PubMed] [Google Scholar]
- 17.Sarris J, Panossian A, Schweitzer I, Stough C, Scholey A. Herbal medicine for depression, anxiety and insomnia: a review of psychopharmacology and clinical evidence. Eur Neuropsychopharmacol. 2011;21(12):841–860. doi: 10.1016/j.euroneuro.2011.04.002 [DOI] [PubMed] [Google Scholar]
- 18.Smith CA, Armour M, Lee MS, Wang L-Q, Hay PJ. Acupuncture for depression. Cochrane Database of Systematic Reviews. 2018;(3). doi: 10.1002/14651858.CD004046.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States, 2007. Natl Health Stat Report. 2008;(12):1–23. [PubMed] [Google Scholar]
- 20.Eisenberg DM, Davis RB, Ettner SL, et al. Trends in alternative medicine use in the United States, 1990–1997: results of a follow-up national survey. JAMA. 1998;280(18):1569–1575. doi: 10.1001/jama.280.18.1569 [DOI] [PubMed] [Google Scholar]
- 21.Goel AR, Elhassan H, Patterson M, Reid MC. Characteristics of Provider-Focused Research on Complementary and Integrative Medicine in Palliative Care: A Scoping Review. Am J Hosp Palliat Care. Published online April 23, 2021:10499091211011708. doi: 10.1177/10499091211011708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Berman BM, Singh BB, Hartnoll SM, Singh BK, Reilly D. Primary care physicians and complementary-alternative medicine: training, attitudes, and practice patterns. J Am Board Fam Pract. 1998;11(4):272–281. doi: 10.3122/jabfm.11.4.272 [DOI] [PubMed] [Google Scholar]
- 23.Berman BM, Bausell RB, Lee W-L. Use and referral patterns for 22 complementary and alternative medical therapies by members of the American College of Rheumatology: results of a national survey. Arch Intern Med. 2002;162(7):766–770. doi: 10.1001/archinte.162.7.766 [DOI] [PubMed] [Google Scholar]
- 24.Kemper KJ, O’Connor KG. Pediatricians’ recommendations for complementary and alternative medical (CAM) therapies. Ambul Pediatr. 2004;4(6):482–487. doi: 10.1367/A04-050R.1 [DOI] [PubMed] [Google Scholar]
- 25.Kent JB, Tanabe KO, Muthusubramanian A, Statuta SM, MacKnight JM. Complementary and Alternative Medicine Prescribing Practices Among Sports Medicine Providers. Altern Ther Health Med. 2020;26(5):28–32. [PubMed] [Google Scholar]
- 26.Kundu A, Tassone RF, Jimenez N, Seidel K, Valentine JK, Pagel PS. Attitudes, patterns of recommendation, and communication of pediatric providers about complementary and alternative medicine in a large metropolitan children’s hospital. Clin Pediatr (Phila). 2011;50(2):153–158. doi: 10.1177/0009922810384724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kurtz ME, Nolan RB, Rittinger WJ. Primary care physicians’ attitudes and practices regarding complementary and alternative medicine. J Am Osteopath Assoc. 2003;103(12):597–602. [PubMed] [Google Scholar]
- 28.Manek NJ, Crowson CS, Ottenberg AL, Curlin FA, Kaptchuk TJ, Tilburt JC. What rheumatologists in the United States think of complementary and alternative medicine: results of a national survey. BMC Complementary and Alternative Medicine. 2010;10(1):5. doi: 10.1186/1472-6882-10-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rhode JM, Patel DA, Sen A, Schimp VL, Johnston CM, Liu JR. Perception and use of complementary and alternative medicine among gynecologic oncology care providers. Int J Gynaecol Obstet. 2008;103(2):111–115. doi: 10.1016/j.ijgo.2008.06.001 [DOI] [PubMed] [Google Scholar]
- 30.Sawni A, Thomas R. Pediatricians’ attitudes, experience and referral patterns regarding Complementary/Alternative Medicine: a national survey. BMC Complement Altern Med. 2007;7:18. doi: 10.1186/1472-6882-7-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sierpina V, Levine R, Astin J, Tan A. Use of mind-body therapies in psychiatry and family medicine faculty and residents: attitudes, barriers, and gender differences. Explore (NY). 2007;3(2):129–135. doi: 10.1016/j.explore.2006.12.001 [DOI] [PubMed] [Google Scholar]
- 32.Demmer C. A Survey of Complementary Therapy Services Provided by Hospices. Journal of Palliative Medicine. 2004;7(4):510–516. doi: 10.1089/jpm.2004.7.510 [DOI] [PubMed] [Google Scholar]
- 33.Kozak LE, Kayes L, McCarty R, et al. Use of Complementary and Alternative Medicine (CAM) by Washington State Hospices. Am J Hosp Palliat Care. 2009;25(6):463–468. doi: 10.1177/1049909108322292 [DOI] [PubMed] [Google Scholar]
- 34.Olotu BS, Brown CM, Lawson KA, Barner JC. Complementary and Alternative Medicine Utilization in Texas Hospices: Prevalence, Importance, and Challenges. Am J Hosp Palliat Care. 2014;31(3):254–259. doi: 10.1177/1049909113486535 [DOI] [PubMed] [Google Scholar]
- 35.Van Hyfte GJ, Kozak LE, Lepore M. A Survey of the Use of Complementary and Alternative Medicine in Illinois Hospice and Palliative Care Organizations. Am J Hosp Palliat Care. 2014;31(5):553–561. doi: 10.1177/1049909113500378 [DOI] [PubMed] [Google Scholar]
- 36.Chan P-S, Wong MM. Physicians and complementary-alternative medicine: training, attitudes, and practices in Hawaii. Hawaii Med J. 2004;63(6):176–181. [PubMed] [Google Scholar]
- 37.Esplen MJ, Foster B, Pearson S, et al. A survey of oncology healthcare professionals’ knowledge and attitudes toward the use of music as a therapeutic tool in healthcare. Support Care Cancer. 2020;28(1):381–388. doi: 10.1007/s00520-019-04812-2 [DOI] [PubMed] [Google Scholar]
- 38.Greene BR, Smith M, Allareddy V, Haas M. Referral patterns and attitudes of primary care physicians towards chiropractors. BMC Complement Altern Med. 2006;6:5. doi: 10.1186/1472-6882-6-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lee RT, Barbo A, Lopez G, et al. National survey of US oncologists’ knowledge, attitudes, and practice patterns regarding herb and supplement use by patients with cancer. J Clin Oncol. 2014;32(36):4095–4101. doi: 10.1200/JCO.2014.55.8676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Klein E, Beckmann MW, Bader W, et al. Gynecologic oncologists’ attitudes and practices relating to integrative medicine: results of a nationwide AGO survey. Arch Gynecol Obstet. 2017;296(2):295–301. doi: 10.1007/s00404-017-4420-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Risberg T, Kolstad A, Bremnes Y, et al. Knowledge of and attitudes toward complementary and alternative therapies; a national multicentre study of oncology professionals in Norway. Eur J Cancer. 2004;40(4):529–535. doi: 10.1016/j.ejca.2003.11.011 [DOI] [PubMed] [Google Scholar]
- 42.IQVIA. Accessed April 27, 2021. https://www.iqvia.com/
- 43.SAS Institute Inc. 2013. SAS 9.4 Statements: Reference. Cary, NC: SAS Institute Inc. [Google Scholar]
- 44.Tomlinson D, Hesser T, Ethier M-C, Sung L. Complementary and alternative medicine use in pediatric cancer reported during palliative phase of disease. Support Care Cancer. 2011;19(11):1857–1863. doi: 10.1007/s00520-010-1029-0 [DOI] [PubMed] [Google Scholar]
- 45.Bercovitz A, Sengupta M, Jones A, Harris-Kojetin LD. Complementary and alternative therapies in hospice: The national home and hospice care survey: United States, 2007. Natl Health Stat Report. 2011;(33):1–20. [PubMed] [Google Scholar]
- 46.Axtner J, Steele M, Kröz M, Spahn G, Matthes H, Schad F. Health services research of integrative oncology in palliative care of patients with advanced pancreatic cancer. BMC Cancer. 2016;16:579. doi: 10.1186/s12885-016-2594-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Horneber M, Bueschel G, Dennert G, Less D, Ritter E, Zwahlen M. How Many Cancer Patients Use Complementary and Alternative Medicine: A Systematic Review and Metaanalysis. Integr Cancer Ther. 2012;11(3):187–203. doi: 10.1177/1534735411423920 [DOI] [PubMed] [Google Scholar]
- 48.Muecke R, Paul M, Conrad C, et al. Complementary and Alternative Medicine in Palliative Care: A Comparison of Data From Surveys Among Patients and Professionals. Integr Cancer Ther. 2016;15(1):10–16. doi: 10.1177/1534735415596423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Steel A, Schloss J, Diezel H, Palmgren PJ, Maret JB, Filbet M. Complementary medicine visits by palliative care patients: a cross-sectional survey. BMJ Supportive & Palliative Care. Published online August 9, 2020. doi: 10.1136/bmjspcare-2020-002269 [DOI] [PubMed] [Google Scholar]
- 50.Stussman BJ, Nahin RR, Barnes PM, Ward BW. U.S. Physician Recommendations to Their Patients About the Use of Complementary Health Approaches. J Altern Complement Med. 2020;26(1):25–33. doi: 10.1089/acm.2019.0303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mitchell AJ, Chan M, Bhatti H, et al. Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: a meta-analysis of 94 interview-based studies. Lancet Oncol. 2011;12(2):160–174. doi: 10.1016/S1470-2045(11)70002-X [DOI] [PubMed] [Google Scholar]
- 52.Weisel KK, Fuhrmann LM, Berking M, Baumeister H, Cuijpers P, Ebert DD. Standalone smartphone apps for mental health-a systematic review and meta-analysis. NPJ Digit Med. 2019;2:118. doi: 10.1038/s41746-019-0188-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Chiaramonte DR, Adler SR. Integrative Palliative Care: A New Transformative Field to Alleviate Suffering. J Altern Complement Med. 2020;26(9):761–765. doi: 10.1089/acm.2020.0366 [DOI] [PubMed] [Google Scholar]
- 54.Frass M, Strassl RP, Friehs H, Müllner M, Kundi M, Kaye AD. Use and Acceptance of Complementary and Alternative Medicine Among the General Population and Medical Personnel: A Systematic Review. Ochsner J. 2012;12(1):45–56. [PMC free article] [PubMed] [Google Scholar]
- 55.Gabbard J, Jordan A, Mitchell J, Corbett M, White P, Childers J. Dying on Hospice in the Midst of an Opioid Crisis: What Should We Do Now? Am J Hosp Palliat Care. 2019;36(4):273–281. doi: 10.1177/1049909118806664 [DOI] [PubMed] [Google Scholar]
- 56.Valderas JM, Starfield B, Forrest CB, Rajmil L, Roland M, Sibbald B. Routine care provided by specialists to children and adolescents in the United States (2002–2006). BMC Health Serv Res. 2009;9:221. doi: 10.1186/1472-6963-9-221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bishop FL, Prescott P, Chan YK, Saville J, von Elm E, Lewith GT. Prevalence of complementary medicine use in pediatric cancer: a systematic review. Pediatrics. 2010;125(4):768–776. doi: 10.1542/peds.2009-1775 [DOI] [PubMed] [Google Scholar]
- 58.Wahner-Roedler DL, Lee MC, Chon TY, Cha SS, Loehrer LL, Bauer BA. Physicians’ attitudes toward complementary and alternative medicine and their knowledge of specific therapies: 8-year follow-up at an academic medical center. Complement Ther Clin Pract. 2014;20(1):54–60. doi: 10.1016/j.ctcp.2013.09.003 [DOI] [PubMed] [Google Scholar]
- 59.Corbin LW, Mellis BK, Beaty BL, Kutner JS. The use of complementary and alternative medicine therapies by patients with advanced cancer and pain in a hospice setting: a multicentered, descriptive study. J Palliat Med. 2009;12(1):7–8. doi: 10.1089/jpm.2008.0198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.World Health Organization. International Classification of Diseases for Mortality and Morbidity Statistics (11th Revision). Published 2018. Accessed June 18, 2021. https://icd-who-int.revproxy.brown.edu/browse11/l-m/en
- 61.Astin JA. Why patients use alternative medicine: results of a national study. JAMA. 1998;279(19):1548–1553. doi: 10.1001/jama.279.19.1548 [DOI] [PubMed] [Google Scholar]
- 62.Penney LS, Ritenbaugh C, DeBar LL, Elder C, Deyo RA. Provider and patient perspectives on opioids and alternative treatments for managing chronic pain: a qualitative study. BMC Fam Pract. 2017;17(1):164. doi: 10.1186/s12875-016-0566-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Thorne S, Paterson B, Russell C, Schultz A. Complementary/alternative medicine in chronic illness as informed self-care decision making. Int J Nurs Stud. 2002;39(7):671–683. doi: 10.1016/s0020-7489(02)00005-6 [DOI] [PubMed] [Google Scholar]
- 64.Health Topics A-Z. National Center for Complementary and Integrative Health. Accessed June 11, 2021. https://www.nccih.nih.gov/health/atoz
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


