Abstract
Participant attrition in longitudinal studies can lead to substantial bias in study results, especially when attrition is nonrandom. A previous study of the Burn Model System (BMS) database prior to 2002 identified participant and study-related factors related to attrition. The purpose of the current study was to examine changes in attrition rates in the BMS longitudinal database since 2002 and to revisit factors associated with attrition. Individuals 18 years and older enrolled in the BMS database between 2002 and 2018 were included in this study. Stepwise logistic regression models identified factors significantly associated with attrition at 6, 12, and 24 months postburn injury. The percentage of individuals lost to follow-up was 26% at 6 months, 33% at 12 months, and 42% at 24 months. Factors associated with increased risk of loss to follow-up across two or more time points include male sex, lower TBSA burn size, being unemployed at the time of burn, shorter duration of acute hospital stay, younger age, not having private health insurance or workers’ compensation, and a history of drug abuse. Retention levels in the BMS have improved by at least 10% at all time points since 2002. The BMS and other longitudinal burn research projects can use these results to identify individuals at high risk for attrition who may require additional retention efforts. Results also indicate potential sources of bias in research projects utilizing the BMS database.
INTRODUCTION
Longitudinal studies have important advantages over cross-sectional studies, including the ability to examine causal relationships and evaluate patterns over time. However, they also present many significant challenges, including participant attrition. It is widely recognized that attrition in longitudinal studies can reduce both statistical power and cause bias. Specifically, attrition bias occurs when dropout of participants is not random, and variables associated with attrition are correlated with outcome variables under evaluation. Past research suggests that attrition of up to 20% may be acceptable and limit bias.1 However, studies have found when attrition is between 20 and 40%, there can be significant bias in study results, especially when attrition is nonrandom.2 In studies of individuals that last for years or decades, achieving follow-up rates of up to 80% are nearly impossible, even when significant study resources are available. When study resources are limited, this task becomes even more difficult and statistical methods that attempt to estimate the impact of attrition on study bias are the only available options.
Of key importance to both minimizing attrition and evaluating the effect of attrition on study outcomes is determining factors associated with attrition within and among longitudinal studies. By evaluating and identifying the characteristics of persons at highest risk of loss to follow-up, researchers can prioritize the use of resources and use recruitment and retention strategies that are tailored toward these high-risk individuals. In addition, by understanding which factors impact attrition within a study, researchers can better understand how attrition might bias-specific research outcomes and results and attempt to address those using statistical approaches.
Research indicates that a variety of participant factors can influence attrition. Several factors that have been consistently associated with dropout across populations include male sex, being single, low socioeconomic status, smoking, low education, minority ethnic group, substance abuse, and depression.3–7 Other factors, including age and poor health or co-morbidities, have been inconsistently associated with attrition and are more population dependent.3,4,8–10 For example, in persons with spinal cord injury or traumatic brain injury, participants with more medical conditions and higher injury severity are more likely to have follow-up data10,11; alternatively, a longitudinal study of women’s health found that those with poorer health had higher loss to follow-up3.
In addition to participant characteristics, many study-specific factors have also been found to be associated with attrition. These can vary widely and include things such as sensitive nature of the study topic, inadequate study resources for locating and following participants, inconvenience of study location or procedures, transportation barriers, amount and type of study compensation, and failure to achieve good rapport with study participants.12–14 Thus, improving retention must focus on both improving study-related factors where possible and identifying participants at highest risk of loss to follow-up so that efforts can be optimized for maximizing the number of retained study participants.
In this study, we sought to examine factors specifically associated with loss to follow-up in persons with burn injuries. To date, only three studies have examined attrition in persons with burn injuries.15–17 Findings based on data collected by the Burn Model System (BMS) National Longitudinal Database up until 2002 found that younger age, lower education, un-employment, prior drug abuse, and no health insurance were associated with lower rates of follow-up, while longer hospital stay was associated with increased likelihood of retention.16 Recruitment site was also significantly associated with attrition rates, signaling that study-related factors may also be of importance as data collection sites utilized different recruitment and retention methods. The findings of the previous BMS study16 resulted in the adoption of additional strategies to improve recruitment and retention, as well as standardization of procedures across BMS sites where possible.18 Some of these changes included implementation of locator services by all BMS centers in 2007, thank you letters sent upon completion of follow-up surveys, and in 2006 changes in recruitment criteria to require surgery for wound closure in 2006, leading to focused recruitment and retention of persons with more severe burns.19 The specific purpose of this study was to (i) examine changes in retention rates in the BMS longitudinal database since 2002; (ii) revisit factors associated with attrition found by a previous study of the BMS database16 in order to examine sources of bias in analyses done using BMS data and to identify participant subgroups that are most at risk for dropout and could benefit from additional retention efforts.
METHODS
Sample
The dataset used for the analyses in this paper includes records from the Burn Injury Model System National Longitudinal Database (BMS NDB). The BMS was established in 1994 and was funded by the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR). Beginning in 1994, funded BMS grantees began collecting information on survivors of burn injury, including demographics, clinical characteristics (such as cause of injury and days of hospital stay), and health outcomes using both medical record review and self-report survey. The goals and ideology behind the BMS program have been previously described20 and an overview of the type of data available has been published.18,20,21 A previously published study looking at loss to follow-up in the BMS database16 utilized records for individuals with a burn injury between 1994 and October 1, 2002. The current study sought to explore loss to follow-up between October 1, 2002 and September 30, 2018, and to examine predictors of loss to follow-up during this time period. All available data from four sites including the UW Medicine Regional Burn Center at Harborview Medical Center in Seattle, Washington (UW), the University of Texas Southwestern Medical Center at Dallas (UTSW), Texas, Boston-Harvard Burn Injury Model System (consisting of burn centers at Massachusetts General Hospital, Shriners Hospital for Children Boston, and Brigham and Women’s Hospital), and Johns Hopkins Regional Burn Center in Baltimore, Maryland (JH) were included. Excluded were data from the University of Texas Medical Branch/Shriners Hospital BMS center (site 5, Figure 1), as it almost exclusively recruits pediatric participants. The current study focuses on adult participants; reasons for loss to follow-up are potentially different in juvenile populations.22,23 All participants met the BMS inclusion criteria that were current at the time of their recruitment. The requirements and changes made to the recruitment criteria over time are detailed in Table 1. In addition, the principles outlined in the Declaration of Helsinki were followed and informed consent was obtained from all participants.
Figure 1.
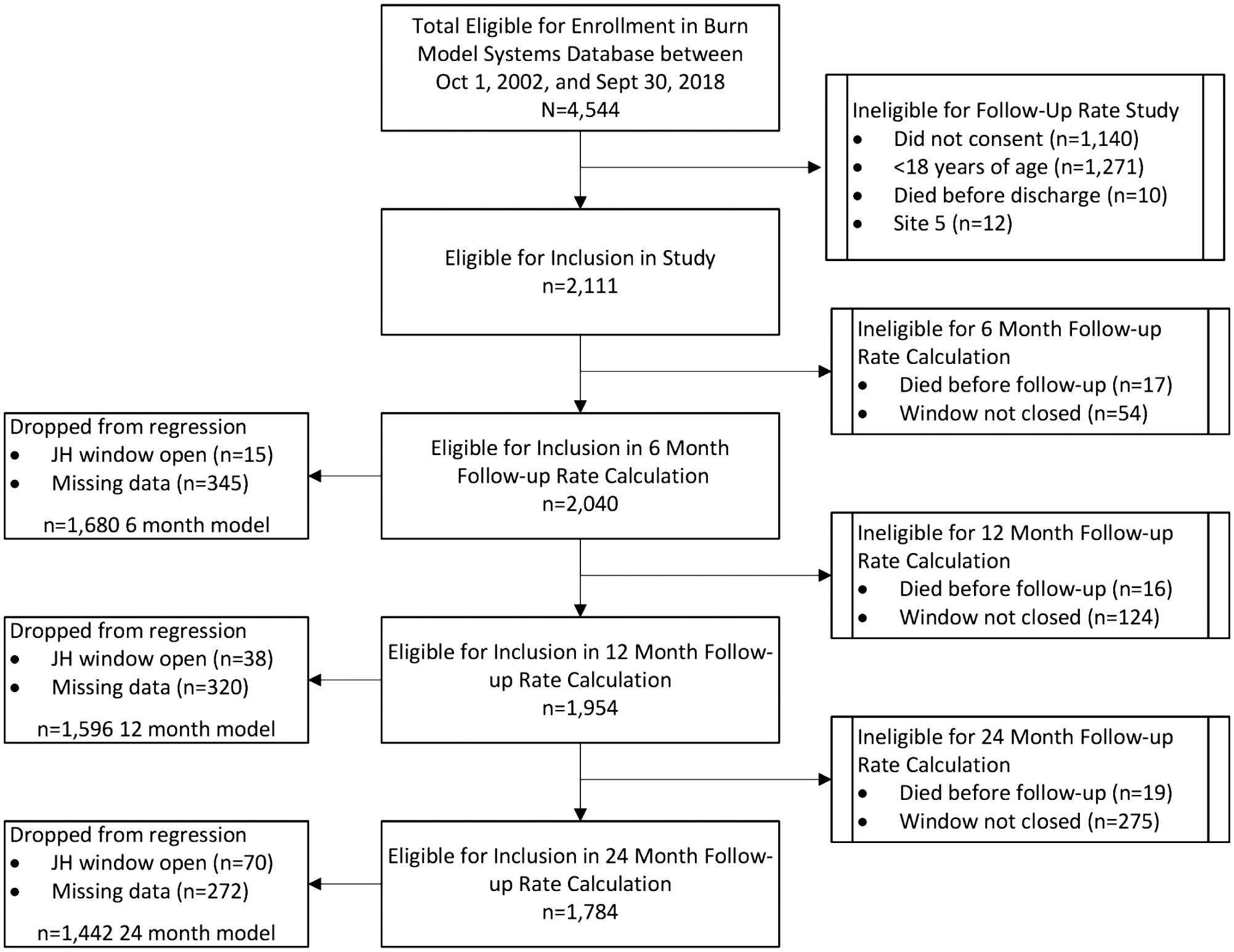
Flowchart of participant participation at each follow-up time point and reasons for loss to follow-up. Site 5 refers to the University of Texas Medical Branch/Shriners Hospital center and was excluded for reasons described in the text. JH refers to individuals from the Johns Hopkins Regional Burn Center with a follow-up window post September 30, 2012 (see text).
Table 1.
Summary of enrollment eligibility criteria for the Burn Model System (BMS) by year
| Prior to 2005 | 2006–2008 | 2009–2018 |
|---|---|---|
|
2005 criteria with the below changes:
|
2006 criteria with the below changes:
|
Participants’ data were included in this study if they were 18 years or older at the time of injury, received care from one of the four listed burn centers, and consented to participate in the BMS data collection process. Baseline data were collected from consenting participants within 30 days of their acute hospital discharge following their burn injury. Follow-up data were collected during specific follow-up windows as follows: 6 (±2)-month post injury, 12 (±3) months postinjury, and 24 (±6) months postinjury. Consistent with the previous study in this population,16 participants were considered lost to follow-up when phone calls, mailings, and clinic visits failed to result in data collection from the individual during the follow-up window. If a participant’s follow-up window had not yet closed on September 30, 2018, the data point was treated as missing and the participant was not included in the follow-up calculation rate. A participant was defined as not lost to follow-up if any part of the assessment was completed either in person, by mail, or over the phone, regardless of completeness of the assessment. In addition, participants were not considered lost to follow-up if at least some data were collected using medical record review for specific variables collected during the follow-up window. Consented individuals were still considered eligible for subsequent follow-up regardless of their participation at previous follow-up intervals unless they specifically requested to be withdrawn from the study. Individuals who died after admission for their initial injury were excluded from all calculations. Those who refused consent at initial contact were excluded from the study because they were not tracked and no effort was made to follow these individuals. Participants who died after consent were excluded from analyses for any subsequent follow-up visits, as the intention of this study was to examine other factors aside from mortality associated with loss to follow-up.
Measures
Since its inception in 1994, the information and instruments used to collect data in the BMS database have evolved, resulting in some inconsistency in outcome measures collected at specific time points or sites.18 Only variables available across participants, regardless of when they were enrolled, were utilized in this study. Information is collected using both medical record review and self-report surveys. Demographic variables utilized in this study included age in years, sex, employment status at time of burn, race/ethnicity, location of residence postacute discharge, and primary sponsor of care (ie, insurance type) at discharge. Employment status was recoded as a yes/no variable by recoding the initial response options as follows (1 = working; 2 = not working, homemaker/caregiver, volunteer, or retired). Ethnicity and race were combined to generate the categories of white non-Hispanic, Hispanic (white or nonwhite), Black non-Hispanic, and any other race (“other”). The insurance variable was collected with the following sponsor options: Medicare, Medicaid, Private Insurance, Workers’ Compensation/Labor and Industry, Health Maintenance Organization (HMO)/Preferred Provider Organization (PPO)/Prepaid/Managed care, Champus, Self-pay, Indigent, Public Support, Veterans Affairs (VA), Other, Philanthropy/Private Support, and Unknown. For all analyses, these insurance categories were collapsed based on similarity: category 1 includes “private insurance, HMO, PPO, VA, and Champus,” category 2 includes “Medicaid, self-pay, indigent, and philanthropy,” category 3 includes “Medicare,” and category 4, “Workers’ compensation.” Because marital status was not consistently recorded over time by the BMS, the variable which assessed that the participant was living with at the time of postacute injury release was used as a proxy. For living situation, participants who listed themselves as living with a spouse or partner were coded as “living with partner” and those living alone or in other situations were coded as “other.” Burn and injury-related variables considered in the analyses included site of recruitment location (ie, burn center site), burn size (percent TBSA burned), length of hospital stay in days, and if the injury was job-related or intentional. Additional variables considered in the analyses included concomitant medical problems and a past history of alcohol or drug abuse.
Analyses
Overall follow-up rates for each assessment period were calculated by comparing the number of individuals with or without follow-up out of those eligible for each assessment period and is consistent with the methodology used by Holavanahalli et al.16 Univariate analyses were completed for each variable considered for inclusion in the regression using chi-square tests for categorical variables and Wilcoxon rank-sum tests for continuous variables regardless of statistical significance in subsequent regression analyses. Logistic regression analyses with robust standard errors were completed by beginning with a full model that included all variables listed in Table 2 with the exception of participation in prior study assessment periods. Prior participation at 6 or 12 months was not included in the models as the purpose of the regression analyses was to determine whether demographic, medical, or burn-related variables were associated with loss to follow-up. In addition, individuals recruited by the JH site were dropped from the regression models if their follow-up window closed after September 30, 2012, because JH was no longer funded after this date and no follow-ups were attempted for individuals from that site after this date. Table 2 includes prior study participation in order to examine the likelihood of participation once a participant did not respond or participate at a previous time point and differentiate the rate of follow-up among those who had already participated in one or more prior assessment periods. The dependent variable, follow-up status at each assessment period, was coded as 1 for those lost to follow-up and 0 for those not lost to follow-up. Stepwise backward regression was completed for each of the three assessment periods (6, 12, and 24 months) and only variables statistically significant at the α level of 0.05 were kept in the final model. All models included the variables of sex and age regardless of their significance. Site of recruitment was included as a covariate in all models in order to adjust for operational disparities that might exist between the four included study sites. Individuals with complete data on all variables in the full model were included in the regression analyses. For all three regression models, unusual and influential data points as well as the regression assumption of linearity were investigated. High leverage individuals were identified through visual inspection of DFBETA statistics, which are measures of standardized differences between regression coefficients when a given observation is included or excluded. Model adequacy and goodness of fit were evaluated using the model specification linktest24and the Hosmer–Lemeshow goodness-of-fit test.25 A sensitivity analyses was completed to compare those excluded from the regression analyses (ie, those with complete vs partial missing data) on age, race/ethnicity, insurance, drug use, employment prior to burn, percent TBSA burned, and length of hospital stay using chi-squared or Student’s t-tests.
Table 2.
Distributions and statistical tests of association of characteristics for Burn Model System participants discharged alive, consented and 18-year-old or older participants lost to follow-up
| 6 Months | 12 Months | 24 Months | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Followed | Lost | % Lost | P-value | Followed | Lost | % Lost | P-value | Followed | Lost | % Lost | P-value | |
| Number of eligible participants | 2040 | 1954 | 1784 | |||||||||
| Overall sample follow-up status | 1508 | 532 | 26% | 1302 | 652 | 33% | 1029 | 755 | 42% | |||
| Participants lost to follow-up by site | ||||||||||||
| Site 1 | 521 | 164 | 24% | <.001 | 448 | 209 | 32% | <.001 | 353 | 241 | 41% | <.001 |
| Site 2 | 632 | 121 | 16% | 549 | 176 | 24% | 420 | 251 | 37% | |||
| Site 3 | 184 | 197 | 52% | 164 | 213 | 57% | 156 | 219 | 58% | |||
| Site 4 | 171 | 50 | 23% | 141 | 54 | 28% | 100 | 44 | 31% | |||
| Ethnicity | ||||||||||||
| White | 1011 | 323 | 24% | .001 | 871 | 410 | 32% | .023 | 696 | 476 | 41% | .112 |
| Black | 198 | 103 | 34% | 174 | 117 | 40% | 138 | 130 | 49% | |||
| Hispanic | 208 | 56 | 21% | 177 | 72 | 29% | 135 | 90 | 40% | |||
| Other | 80 | 31 | 28% | 72 | 32 | 31% | 54 | 41 | 43% | |||
| Sex | ||||||||||||
| Male | 1068 | 391 | 27% | .24 | 916 | 489 | 35% | .031 | 722 | 562 | 44% | .047 |
| Female | 440 | 141 | 24% | 386 | 163 | 30% | 307 | 193 | 39% | |||
| Employed at time of burn | ||||||||||||
| No | 531 | 198 | 27% | .032 | 444 | 256 | 37% | .002 | 340 | 301 | 47% | <.001 |
| Yes | 962 | 285 | 23% | 841 | 355 | 30% | 676 | 415 | 38% | |||
| History alcohol abuse | ||||||||||||
| No | 1274 | 379 | 23% | .004 | 1107 | 478 | 30% | .001 | 882 | 574 | 39% | .001 |
| Yes | 188 | 84 | 31% | 156 | 105 | 40% | 114 | 119 | 51% | |||
| History drug abuse | ||||||||||||
| No | 1309 | 381 | 23% | <.001 | 1139 | 480 | 30% | <.001 | 916 | 566 | 38% | <.001 |
| Yes | 142 | 77 | 35% | 116 | 97 | 46% | 77 | 116 | 60% | |||
| Non-intentional injury | ||||||||||||
| No | 90 | 40 | 31% | .104 | 80 | 43 | 35% | .502 | 64 | 50 | 44% | .571 |
| Yes | 1394 | 450 | 24% | 1201 | 566 | 32% | 945 | 661 | 41% | |||
| Job-related injury | ||||||||||||
| No | 1133 | 399 | 26% | .019 | 968 | 493 | 34% | .009 | 747 | 576 | 44% | .001 |
| Yes | 351 | 91 | 21% | 313 | 116 | 27% | 262 | 135 | 34% | |||
| Where living at release | ||||||||||||
| Other | 435 | 163 | 27% | .138 | 366 | 201 | 35% | .07 | 298 | 228 | 43% | .374 |
| Personal residence | 1045 | 332 | 24% | 911 | 413 | 31% | 705 | 491 | 41% | |||
| Who living with at release | ||||||||||||
| Alone | 156 | 60 | 28% | .005 | 125 | 78 | 38% | <.001 | 102 | 79 | 44% | <.001 |
| Spouse/partner | 630 | 164 | 21% | 587 | 194 | 25% | 480 | 261 | 35% | |||
| Other | 625 | 231 | 27% | 509 | 295 | 37% | 380 | 330 | 46% | |||
| Primary sponsor of care (i.e., insurance) | ||||||||||||
| Private, HMO, PPO, VA, and Champus | 487 | 114 | 19% | <.001 | 420 | 162 | 28% | <.001 | 336 | 190 | 36% | <.001 |
| Medicaid, self-pay, indigent, philanthropy | 498 | 230 | 32% | 412 | 283 | 41% | 315 | 317 | 50% | |||
| Medicare | 220 | 70 | 24% | 197 | 72 | 27% | 145 | 94 | 39% | |||
| Workers compensation | 248 | 50 | 17% | 227 | 59 | 21% | 187 | 81 | 30% | |||
| Followed at 6 months | ||||||||||||
| No | 113 | 388 | 77% | <.001 | 102 | 362 | 78% | <.001 | ||||
| Yes | 1189 | 264 | 18% | 927 | 393 | 30% | ||||||
| Followed at 12 months | ||||||||||||
| No | 109 | 481 | 82% | <.001 | ||||||||
| Yes | 920 | 274 | 23% | |||||||||
| Mean TBSA burned (%) | 19.2 | 16.3 | <.001 | 20.3 | 15.1 | <.001 | 20.3 | 16.6 | <.001 | |||
| Mean age at follow-up (years) | 44.5 | 42.4 | .003 | 45.6 | 41.8 | <.001 | 46.6 | 43.0 | <.001 | |||
| Length of acute hospital stay (days) | 30.8 | 29.9 | <.001 | 33.5 | 25.1 | <.001 | 34.0 | 27.0 | <.001 | |||
HMO: Health Maintenance Organization; PPO: Preferred Provider Organization; VA: Veterans Administration.
RESULTS
The final dataset included the following number of eligible individuals with closed follow-up windows for each of the follow-up time periods (Figure 1): 2040 at 6 months, 1954 at 12 months, and 1784 at 24 months. Of the 2040 individuals eligible for follow-up at 6 months 532 (26%) were lost to follow-up. This number increased to 652 of 1954 (33%) at 12 months and 755 of 1784 (42%) at 24 months.
Univariate Analyses
The results of the univariate analyses indicated that recruitment site location, previous participation at 6 or 12 months, no history of drug or alcohol abuse, living with a spouse/partner after discharge, workers compensation or private insurance, being employed at time of burn, having a job-related injury, larger % TBSA burn size, older age, and longer length of hospital stay at acute injury were all consistently associated with lower loss to follow-up at all time points at the α level of 0.05 (Table 2). There was no association between follow-up status and nonintentional injury or residence at discharge from acute hospital stay at all three time points. Ethnicity and sex were inconsistently associated with loss to follow-up across the three time points.
Multivariate Analyses:
Linearity, model adequacy. and goodness of fit were acceptable for all three models. Two high leverage individuals were identified for the 12-month model and were dropped from the analyses. Further examination of these individuals indicated that they had extreme values of TBSA burn size (>90%).26
The sensitivity analysis indicated that individuals with partial missing data excluded from the regression models were not statistically different with respect to sex, age, insurance payer, or duration of hospital stay. However, differences were significant with respect to race/ethnicity, TBSA burned, and preburn employment at all three time points and prior drug use at 6 and 12 months. Individuals dropped due to partial missing data were less likely (all P ≤ .003) to be Hispanic (6% vs 15% at 6 months), less likely (all P ≤ .03) to be employed prior to burn (43% vs 36% at 6 months), report lower average TBSA burned (19% vs 15% at 6 months) (all P ≤ .003), and more likely (both P = .01) to report prior drug use (16% vs 11% at 6 months).
Six-Month Follow-Up
Age, sex, and site were included in the model regardless of their statistical significance in univariate analyses. Male sex, recruitment site, race/ethnicity, primary insurance, and prior history of drug abuse were the only variables statistically significantly associated with probability of loss to follow-up at 6 months. Specifically, individuals in the Medicaid/Self-Pay/Indigent/Philanthropy or Medicare groups had odds of loss to follow-up that were nearly twice that of individuals who had private insurance/HMO/PPO/VA/Champus (odds ratio (OR):2.13 and 1.92, respectively; Table 3). Conversely, individuals who listed workers’ compensation as their insurance had lower odds of loss to follow-up (OR: 0.82) than the private insurance reference group. Those with “other” race or ethnicity had odds of loss to follow-up twice that of non-Hispanic White individuals (OR: 2.13). For the drug abuse variable, individuals who reported prior drug abuse had higher odds of loss to follow-up (OR: 1.62).
Table 3.
Logistic regression results examining variables significantly associated with loss to follow-up at 6, 12, and 24 months postburn injury in the BMS database
| 6 Months | 12 Months | 24 Months | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N = 1680, pseudo R2 = 0.098 | N = 1596, pseudo R2 = 0.112 | N = 1442, pseudo R2 = 0.086 | ||||||||||
| OR | z | P-value | (95% CI) | OR | z | P-value | (95% CI) | OR | z | P-value | (95% CI) | |
| Male Sex | 1.34 | 2.09 | 0.037 | (1.02, 1.79) | 1.71 | 3.75 | <0.001 | (1.29, 2.27) | 1.57 | 3.34 | 0.001 | (1.21, 2.06) |
| Age (10-year increment) | 0.94 | −1.28 | 0.199 | (0.85, 1.03) | 0.85 | −3.63 | <0.001 | (0.77, 0.93) | 0.83 | −4.09 | <0.001 | (0.76, 0.91) |
| Site 2* | 0.50 | −4.25 | <0.001 | (0.37, 0.69) | 0.55 | −4.18 | <0.001 | (0.41, 0.73) | 0.73 | −2.31 | 0.021 | (0.56, 0.95) |
| Site 3* | 3.69 | 7.13 | <0.001 | (2.58, 5.28) | 1.85 | 3.35 | 0.001 | (1.29, 2.65) | 1.53 | 2.32 | 0.021 | (1.07, 2.19) |
| Site 4* | 0.61 | −1.95 | 0.052 | (0.37, 1.00) | 0.53 | −2.55 | 0.011 | (0.33, 0.87) | 0.54 | −2.43 | 0.015 | (0.33, 0.89) |
| Blackα | 1.08 | 0.43 | 0.664 | (0.76, 1.53) | ||||||||
| Hispanicα | 0.85 | −0.83 | 0.407 | (0.57, 1.26) | ||||||||
| Other race/ethnicityα | 2.16 | 3.04 | 0.002 | (1.31, 3.55) | ||||||||
| Medicaid, self-pay, indigent, philanthropyß | 2.13 | 4.65 | <0.001 | (1.55, 2.94) | 1.50 | 2.64 | 0.008 | (1.11, 2.02) | 1.51 | 2.79 | 0.005 | (1.13, 2.01) |
| Medicareß | 1.92 | 2.86 | 0.004 | (1.23, 3.00) | 1.26 | 0.99 | 0.320 | (0.80, 1.98) | 1.41 | 1.56 | 0.119 | (0.91, 2.18) |
| Workers compensationß | 0.81 | −1 | 0.316 | (0.54, 1.22) | 0.55 | −2.93 | 0.003 | (0.37, 0.82) | 0.59 | −2.79 | 0.005 | (0.41, 0.86) |
| Prior drug abuse | 1.62 | 2.46 | 0.014 | (1.10, 2.39) | 1.54 | 2.18 | 0.029 | (1.04, 2.27) | 2.31 | 4.44 | <0.001 | (1.60, 3.35) |
| Prior alcohol abuse | 1.60 | 2.52 | 0.012 | (1.11, 2.30) | ||||||||
| Unemployed at time of burn | 1.36 | 2.14 | 0.033 | (1.03, 1.81) | 1.48 | 2.74 | 0.006 | (1.12, 1.95) | ||||
| Not living with partner | 1.55 | 3.42 | 0.001 | (1.20, 1.98) | ||||||||
| Length of acute hospital stay | 0.90 | −2.48 | 0.013 | (0.83, 0.98) | 0.93 | −2.84 | 0.005 | (0.89, 0.98) | ||||
| (10-day increment) | ||||||||||||
| TBSA burned (10% increment) | 0.88 | −2.47 | 0.014 | (0.79, 0.97) | 0.88 | −2.88 | 0.004 | (0.81, 0.96) | ||||
OR: odds ratio; CI: confidence interval.
Reference group is site 1;
Reference group is White non-Hispanic;
References group is private, HMO, PPO, VA, or Champus.
Twelve-Month Follow-Up
At the 12-month follow-up, age, sex, and site were all statistically significant predictors of loss to follow-up with male sex and younger age associated with higher odds of loss to follow-up (Table 3). As with 6 months, insurance and prior drug abuse history were both associated with probability of loss to follow-up. However, in addition, length of acute hospital stay in days, TBSA burn, prior alcohol abuse history, employment status at time of burn, and living situation were also significantly associated with follow-up status. More specifically, those with smaller burns, shorter hospital stays, a history of prior alcohol abuse, living without a partner, and being unemployed at the time of burn were more likely to be lost to follow-up (Table 3).
Twenty-Four-Month Follow-Up
Age, sex, and recruitment site were all significantly associated with the probability of loss to follow-up, with younger age and male sex having higher odds of loss to follow-up, similar to the 12-month model. Prior drug abuse, having shorter length of acute hospital stay, smaller TBSA burn, being unemployed at the time of burn, and having Medicaid/Self-pay/Indigent/Philanthropy or Medicare listed as insurance were all associated with increased odds of loss to follow-up (see Table 3).
DISCUSSION
The results of this study indicate that loss to follow-up rates in the BMS database have improved by at least 10% since 2002 at all time points, ranging from 26% (at 6 months) to 42% (at 24 months) between 2002 and 2018. The improved lost-to-follow-up rates suggest that strategies aimed at minimizing attrition have been effective. The results of the analyses suggest that those at highest risk of loss to follow-up across two or more time points include males, persons of younger age, shorter duration of acute hospital stay, individuals without private health insurance or workers’ compensation, persons with a history of drug abuse, being unemployed at the time of burn, and lower TBSA burn size. Factors less consistently associated with being lost to follow-up (ie, only one time points) were ethnicity/race (6 months), prior alcohol abuse (12 and 24 months), and not living with a partner or spouse postinjury (12 months).
The findings of this study support the prior study looking at pre-2002 data collected by the BMS16 in that all of the factors associated at one or more time points in this study were also associated with loss to follow-up at one or more time points in the previous study, with the exception of sex. Results of both studies can be used to develop targeted recruitment efforts to burn survivors with characteristics associated with greater risk of dropping out. In addition, BMS centers could create a nomogram, such as the one created by the SCI model system,27 which would allow study staff to assess a new participant’s risk of loss to follow-up at the time of enrollment and individualize recruitment efforts. Study site also continues to play a significant role in retention of participants and exploring site differences in patient populations and recruitment strategies may be informative.
Our findings also indicate that once participants miss one data collection they are unlikely to respond to subsequent requests. Of those who did not respond or participate at 6 months, only 21 to 22% had follow-up data at future time points while 83 and 68% of those followed at 6 months had follow-up data at 12 or 24 months, respectively. Similarly, of those followed at 12 months, 76% had follow-up data 1 year later. This finding is to be expected as the reasons for loss to follow-up at 6 months are similar if not the same as reasons for loss to follow-up at later time points. For example, if a participant has moved and cannot be located by study staff at 6 months, it is unlikely that they would be located after additional time has passed. In addition, if the participant no longer needs or seeks burn care at a burn center at 6 or 12 months, it is unlikely they would need or seek burn care at a future time point. Thus, medical record abstraction of follow-up data would be impossible for these individuals and contact with study staff further limited because participants are no longer receiving clinical care. These findings imply that the earlier time points are important for retention efforts, and that the BMS may be better served by focusing limited resources on locating participants and collecting data at earlier time points.
The recommendations for follow-up rates for cohort studies range from 50 to 80%,1,2 and in the literature cohort studies in other populations report response rates of anywhere between 46 and 92% at 1-year,14 though survey rates have been shown to be declining significantly worldwide in recent years.28 The current BMS follow-up rates fall between the rates of follow-up in the Traumatic Brain Injury (TBI) and Spinal Cord Injury (SCI) model systems databases, which have different eligibility criteria29,30 but are similarly managed, have multiple sites contributing data to the database, and report 41 and 23% attrition rates at 1-year follow-up, respectively.10, 27 This study also indicates that there are many overlapping factors that are associated with loss to follow-up across the three model systems databases. These factors include age, marital status, alcohol use/abuse, race/ethnicity, employment, severity of injury, and insurance payer.10, 27 Retention efforts should focus on groups that may exhibit a higher attrition rate, and researchers who include these traumatic injury populations in longitudinal studies should design their tracking and follow-up procedures accordingly. In addition, researchers in the BMS could consider additional tools and resources for further reducing attrition where feasible. For example, monetary or nonmonetary incentives, prenotification of survey, offering survey results, reducing the length of the survey to reduce participant burden or consideration of a core subset of measures to be administered to some or all participants may increase participation rates.31 The use of online survey administration and/or Computer Adaptive Testing also has the potential to reduce burden and increase participation, both of which recently have been or are currently being implemented by the BMS.
The same factors that put participants at higher risk of loss to follow-up in this study have also been shown to be associated with poorer health outcomes in persons with burn injuries.18 For example, lower satisfaction with life postburn injury is associated with prior alcohol abuse, marital status, and days in intensive care,32 all three of which are associated with loss to follow-up in this study. In addition, Esselman et al found that self-reported community integration is associated with sex, living situation, age, and preinjury employment.33 Selective attrition due to for instance, substance abuse, may distort the relationship between predictive factors and outcomes, leading to the under or over-estimate of the impact of a particular factor on a specific outcome or limiting the generalizability of the results to the larger population of individuals with a burn injury. Thus, nonrandom attrition of individuals with these characteristics may have biased estimates of rates of community integration and levels of satisfaction with life postburn injury. The results of this study are of value to researchers who might wish to study health outcomes using the BMS data that may also be related to loss to follow-up. Researchers may wish to use statistical approaches and/or data imputation methods to handle missing data due to nonrandom loss to follow-up. Multiple methods for imputing missing data or for evaluating the impact of missing data on risk estimates exist,34 though there is currently no recommended robust method35 and incorrect application of statistical approaches may introduce additional bias.36, 37 However, at a minimum, researchers who use the BMS data can evaluate the potential for bias in their study based on these loss to follow-up results and provide adequate discussion and warning to those who wish to use or generalize their findings. Our data indicate that researchers presenting longitudinal patient-reported outcome data must address issues related to the characteristics of the groups who were lost to follow-up, whether the attrition is likely to have affected the generalizability of their results and provide appropriate sensitivity analyses if possible.1
Study Limitations
This study has several limitations. First, analyses did not include participants who were lost to follow-up due to death, and therefore the results of these analyses are not as informative for studies looking at outcomes related to mortality. Second, a subset of individuals were included in the regression analyses because of missing data and therefore the regression results are not representative of the entire BMS sample. Third, types of attrition are not analyzed in depth. Loss to follow-up due to refusal vs inability to locate vs nonresponse are potentially different and warrant additional research.
CONCLUSIONS
The current study highlights factors associated with loss to follow-up in the BMS national database and provides BMS researchers with information for identifying participants who may require additional retention efforts. Furthermore, this study indicates that attrition has decreased over time, suggesting improvements can be made. However, reaching loss to follow-up rates <20% over an extended follow-up period is an extremely challenging task and success will depend on numerous factors, many of which are outside the control of the BMS researchers, including the clinical population in focus. In addition, some have suggested that trying to achieve a fixed level of “acceptable” follow-up is unhelpful and unnecessary as it could curtail research in the field.1 Future efforts should focus on innovative follow-up methods, including use of social media and tracking databases, when approved by institutional review boards. Statistical techniques to minimize the impact of missing data should also be considered.
ACKNOWLEDGMENTS
The contents of this manuscript were developed under a grant from the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR grant no. 90DP0053). NIDILRR is a Center within the Administration for Community Living (ACL), Department of Health and Human Services (HHS). The contents of this manuscript do not necessarily represent the policy of NIDILRR, ACL, HHS, and you should not assume endorsement by the Federal Government.
Footnotes
Conflict of interest statement. The authors have no conflicts of interest to report.
REFERENCES
- 1.Fewtrell MS, Kennedy K, Singhal A, et al. How much loss to follow-up is acceptable in long-term randomised trials and prospective studies? Arch Dis Child 2008;93:458–61. [DOI] [PubMed] [Google Scholar]
- 2.Kristman V, Manno M, Côté P. Loss to follow-up in cohort studies: how much is too much? Eur J Epidemiol 2004;19:751–60. [DOI] [PubMed] [Google Scholar]
- 3.Young AF, Powers JR, Bell SL. Attrition in longitudinal studies: who do you lose? Aust N Z J Public Health 2006;30:353–61. [DOI] [PubMed] [Google Scholar]
- 4.Goldberg M, Chastang JF, Zins M, Niedhammer I, Leclerc A. Health problems were the strongest predictors of attrition during follow-up of the GAZEL cohort. J Clin Epidemiol 2006;59:1213–21. [DOI] [PubMed] [Google Scholar]
- 5.Lamers F, Hoogendoorn AW, Smit JH, et al. Sociodemographic and psychiatric determinants of attrition in the Netherlands Study of Depression and Anxiety (NESDA). Compr Psychiatry 2012;53:63–70. [DOI] [PubMed] [Google Scholar]
- 6.Fröjd SA, Kaltiala-Heino R, Marttunen MJ. Does problem behaviour affect attrition from a cohort study on adolescent mental health? Eur J Public Health 2011;21:306–10. [DOI] [PubMed] [Google Scholar]
- 7.Hansten ML, Downey L, Rosengren DB, Donovan DM. Relationship between follow-up rates and treatment outcomes in substance abuse research: more is better but when is “enough” enough? Addiction 2000;95:1403–16. [DOI] [PubMed] [Google Scholar]
- 8.Chatfield MD, Brayne CE, Matthews FE. A systematic literature review of attrition between waves in longitudinal studies in the elderly shows a consistent pattern of dropout between differing studies. J Clin Epidemiol 2005;58:13–9. [DOI] [PubMed] [Google Scholar]
- 9.Mihelic AH, Crimmins EM. Loss to follow-up in a sample of Americans 70 years of age and older: the LSOA 1984–1990. J Gerontol B Psychol Sci Soc Sci 1997;52B:S37–48. [DOI] [PubMed] [Google Scholar]
- 10.Corrigan JD, Harrison-Felix C, Bogner J, Dijkers M, Terrill MS, Whiteneck G. Systematic bias in traumatic brain injury outcome studies because of loss to follow-up. Arch Phys Med Rehabil 2003;84:153–60. [DOI] [PubMed] [Google Scholar]
- 11.Richards JS, Go BK, Rutt RD, et al. The National Spinal Cord Injury Collaborative Database. In: Stover SL, DeLisa JA, Whiteneck GG, editors. Spinal cord injury: clinical outcomes from the model system. Gaithersburg, MD: Aspen Publishers; 1995. p. 10–20. [Google Scholar]
- 12.McKenzie M, Tulsky JP, Long HL, Chesney M, Moss A. Tracking and follow-up of marginalized populations: a review. J Health Care Poor Underserved 1999;10:409–29. [DOI] [PubMed] [Google Scholar]
- 13.Tansey CM, Matté AL, Needham D, Herridge MS. Review of retention strategies in longitudinal studies and application to follow-up of ICU survivors. Intensive Care Med 2007;33:2051–7. [DOI] [PubMed] [Google Scholar]
- 14.Booker CL, Harding S, Benzeval M. A systematic review of the effect of retention methods in population-based cohort studies. BMC Public Health 2011;11:249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fauerbach JA, Lawrence J, Stevens S, Munster A. Work status and attrition from longitudinal studies are influenced by psychiatric disorder. J Burn Care Rehabil 1998;19:247–52. [PubMed] [Google Scholar]
- 16.Holavanahalli RK, Lezotte DC, Hayes MP, et al. Profile of patients lost to follow-up in the Burn Injury Rehabilitation Model Systems’ longitudinal database. J Burn Care Res 2006;27:703–12. [DOI] [PubMed] [Google Scholar]
- 17.Ohrtman EA, Zaninotto AL, Carvalho S, et al. Longitudinal clinical trial recruitment and retention challenges in the burn population: lessons learned from a trial examining a novel intervention for chronic neuropathic symptoms. J Burn Care Res 2019;40:792–5. [DOI] [PubMed] [Google Scholar]
- 18.Goverman J, Mathews K, Holavanahalli RK, et al. The National Institute on Disability, Independent Living, and Rehabilitation Research burn model system: twenty years of contributions to clinical service and research. J Burn Care Res 2017;38:e240–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.National Data and Statistical Center for the Burn Model System. BMS Procedures. Accessed 1 August, 2019. Available from http://burndata.washington.edu/standard-operating-procedures
- 20.Klein MB, Lezotte DL, Fauerbach JA, et al. The national institute on disability and rehabilitation research burn model system database: a tool for the multicenter study of the outcome of burn injury. J Burn Care Res 2007;28:84–96. [DOI] [PubMed] [Google Scholar]
- 21.Goverman J, Mathews K, Nadler D, et al. Satisfaction with life after burn: a Burn Model System National Database Study. Burns 2016;42:1067–1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Launes J, Hokkanen L, Laasonen M, et al. Attrition in a 30-year follow-up of a perinatal birth risk cohort: factors change with age. PeerJ 2014;2:e480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Karlson CW, Rapoff MA. Attrition in randomized controlled trials for pediatric chronic conditions. J Pediatr Psychol 2009;34:782–93. [DOI] [PubMed] [Google Scholar]
- 24.StataCorp. Stata 12 base reference manual. College Station, TX: Stata Press; 2011. [Google Scholar]
- 25.Hosmer DW, Lemeshow SA. Goodness-of-fit tests for the multiple logistic regression model. Communications in statistics. 1980;A9:1043–69. [Google Scholar]
- 26.Vittinghoff E, Glidden DV, Shiboski SC, et al. Regression methods in biostatistics: linear, logistic, survival, and repeated measures models. New York, NY: Springer Science+Business Media; 2005. [Google Scholar]
- 27.Kim H, Cutter GR, George B, Chen Y. Understanding and preventing loss to follow-up: experiences from the spinal cord injury model systems. Top Spinal Cord Inj Rehabil 2018;24:97–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mindell JS, Giampaoli S, Goesswald A, et al. ; HES Response Rate Group. Sample selection, recruitment and participation rates in health examination surveys in Europe–experience from seven national surveys. BMC Med Res Methodol 2015;15:78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chen Y, DeVivo MJ, Richards JS, SanAgustin TB. Spinal cord injury model systems: review of program and national database from 1970 to 2015. Arch Phys Med Rehabil 2016;97:1797–804. [DOI] [PubMed] [Google Scholar]
- 30.Corrigan JD, Cuthbert JP, Whiteneck GG, et al. Representativeness of the Traumatic Brain Injury Model Systems National Database. J Head Trauma Rehabil 2012;27:391–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Edwards PJ, Roberts I, Clarke MJ, et al. Methods to increase response to postal and electronic questionnaires. Cochrane Database Syst Rev 2009;(3):MR000008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Patterson DR, Ptacek JT, Cromes F, Fauerbach JA, Engrav L. The 2000 Clinical Research Award. Describing and predicting distress and satisfaction with life for burn survivors. J Burn Care Rehabil 2000;21:490–8. [PubMed] [Google Scholar]
- 33.Esselman PC, Ptacek JT, Kowalske K, Cromes GF, deLateur BJ, Engrav LH. Community integration after burn injuries. J Burn Care Rehabil 2001;22:221–7. [DOI] [PubMed] [Google Scholar]
- 34.Graham JW. Missing data analysis: making it work in the real world. Annu Rev Psychol 2009;60:549–76. [DOI] [PubMed] [Google Scholar]
- 35.Panel on Handling Missing Data in Clinical Trials, Committee on National Statistics Division of Behavioral and Social Sciences and Education. The prevention and treatment of missing data in clinical trials. Washington, DC: National Research Council; 2010. [Google Scholar]
- 36.White IR, Carlin JB. Bias and efficiency of multiple imputation compared with complete-case analysis for missing covariate values. Stat Med 2010;29:2920–31. [DOI] [PubMed] [Google Scholar]
- 37.Vach W, Blettner M. Biased estimation of the odds ratio in case-control studies due to the use of ad hoc methods of correcting for missing values for confounding variables. Am J Epidemiol 1991;134:895–907. [DOI] [PubMed] [Google Scholar]


